Laminoplasty on Kyphotic Cervical Alignments Suggests Poor Surgical Outcomes: A Comparative Finite Element Analysis of Laminoplasty on Different Alignments
Abstract
:1. Introduction
2. Materials and Methods
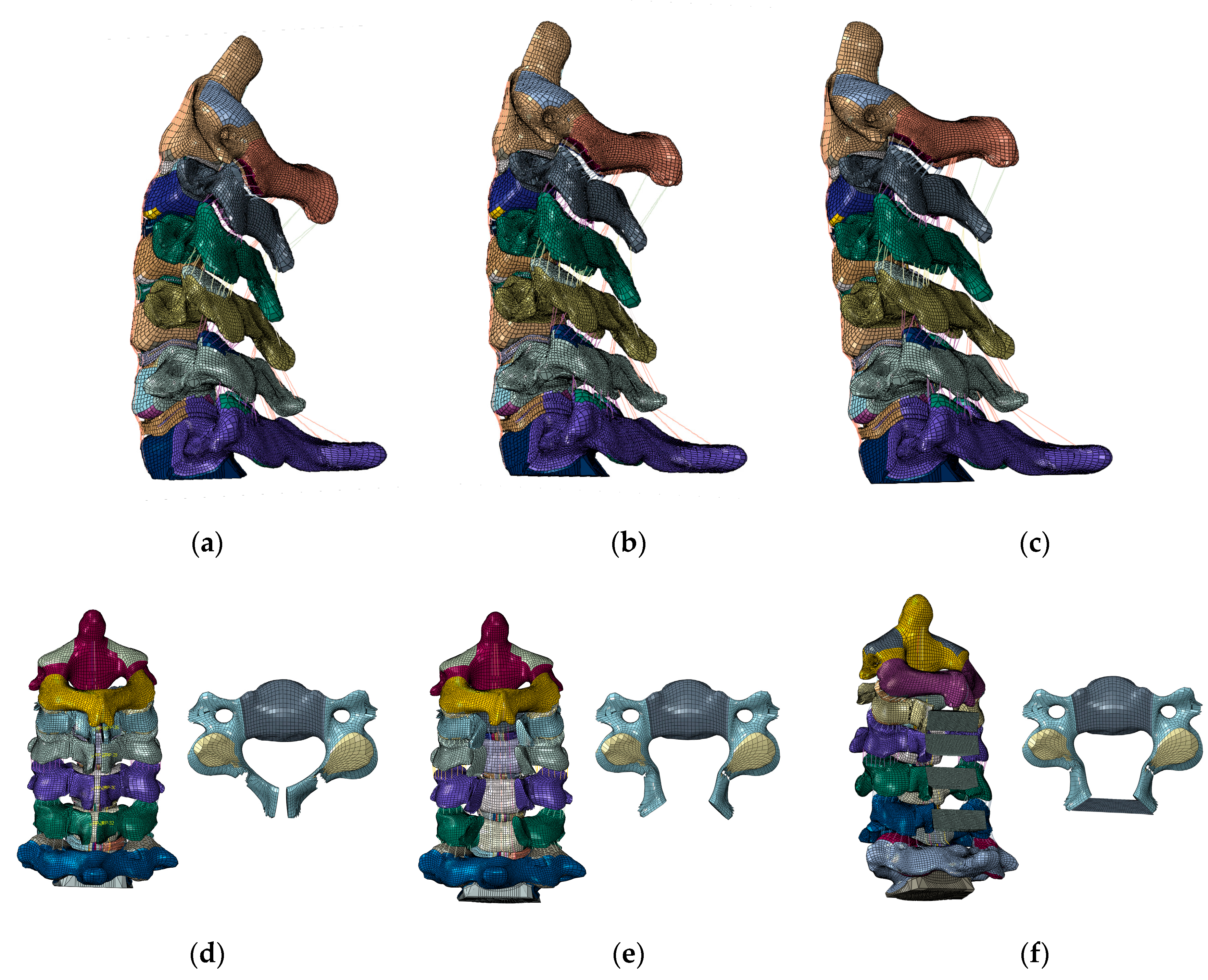
2.1. Model Development
2.2. Cervical Alignments
2.3. Cervical Laminoplasty
2.4. Loads and Boundary Conditions
2.5. Data Analyses
3. Results
3.1. ROM
3.2. Annular Stress
3.3. Nucleus Stresses
3.4. Facet Contact Forces
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Boody, B.S.; Lendnerm, M.; Vaccaro, A.R. Ossification of the posterior longitudinal ligament in the cervical spine: A review. Int. Orthop. 2019, 43, 797–805. [Google Scholar] [CrossRef] [PubMed]
- Hirabayashi, S.; Kitagawa, T.; Yamamoto, I.; Yamada, K.; Kawano, H. Development and Achievement of Cervical Laminoplasty and Related Studies on Cervical Myelopathy. Spine Surg. Relat. Res. 2020, 4, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.J.; Kim, J.S.; Park, P.; Riew, K.D. A Comparison of Various Surgical Treatments for Degenerative Cervical Myelopathy: A Propensity Score Matched Analysis. Glob. Spine J. 2022, 12, 1109–1118. [Google Scholar] [CrossRef]
- Yoshii, T.; Egawa, S.; Chikuda, H.; Kaito, T.; Mori, K.; Koda, M.; Egawa, S.; Hasegawa, T.; Imagama, S.; Yoshida, M.; et al. A systematic review and meta-analysis comparing anterior decompression with fusion and posterior laminoplasty for cervical spondylotic myelopathy. J. Orthop. Sci. 2021, 26, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.A.; Scheer, J.K.; Smith, J.S.; Deviren, V.; Bess, S.; Hart, R.A.; Lafage, V.; Shaffrey, C.I.; Schwab, F.; Ames, C.P. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 2015, 76 (Suppl. 1), S14–S21; Discussion S. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.W.; Jang, S.B.; Lee, H.M.; Lee, J.H.; Lee, M.U.; Kim, J.W.; Yee, J.S. Analysis of Cervical Spine Alignment and its Relationship with Other Spinopelvic Parameters after Laminoplasty in Patients with Degenerative Cervical Myelopathy. J. Clin. Med. 2020, 9, 713. [Google Scholar] [CrossRef] [PubMed]
- Machino, M.; Yukawa, Y.; Hida, T.; Ito, K.; Nakashima, H.; Kanbara, S.; Morita, D.; Kato, F. Cervical alignment and range of motion after laminoplasty: Radiographical data from more than 500 cases with cervical spondylotic myelopathy and a review of the literature. Spine 2012, 37, E1243–E1250. [Google Scholar] [CrossRef]
- Kurokawa, R.; Kim, P. Cervical Laminoplasty: The History and the Future. Neurol. Med. -Chir. 2015, 55, 529–539. [Google Scholar] [CrossRef]
- Nishida, N.; Mumtaz, M.; Tripathi, S.; Kelkar, A.; Sakai, T.; Goel, V.K. Biomechanical Analysis of Posterior Ligaments of Cervical Spine and Laminoplasty. Appl. Sci. 2021, 11, 7645. [Google Scholar] [CrossRef]
- Kallemeyn, N.; Gandhi, A.; Kode, S.; Shivanna, K.; Smucker, J.; Grosland, N. Validation of a C2-C7 cervical spine finite element model using specimen-specific flexibility data. Med. Eng. Phys. 2010, 32, 482–489. [Google Scholar] [CrossRef]
- Mumtaz, M.; Zafarparandeh, I.; Erbulut, D.U. Investigation into Cervical Spine Biomechanics Following Single, Multilevel and Hybrid Disc Replacement Surgery with Dynamic Cervical Implant and Fusion: A Finite Element Study. Bioengineering 2022, 9, 16. [Google Scholar] [CrossRef] [PubMed]
- Finn, M.A.; Brodke, D.S.; Daubs, M.; Patel, A.; Bachus, K.N. Local and global subaxial cervical spine biomechanics after single-level fusion or cervical arthroplasty. Eur. Spine J. 2009, 18, 1520–1527. [Google Scholar] [CrossRef] [PubMed]
- Goel, V.K.; Clausen, J.D. Prediction of load sharing among spinal components of a C5-C6 motion segment using the finite element approach. Spine 1998, 23, 684–691. [Google Scholar] [CrossRef] [PubMed]
- Little, J.P.; Adam, C.J.; Evans, J.H.; Pettet, G.J.; Pearcy, M.J. Nonlinear finite element analysis of anular lesions in the L4/5 intervertebral disc. J. Biomech. 2007, 40, 2744–2751. [Google Scholar] [CrossRef]
- Ling, F.P.; Chevillotte, T.; Leglise, A.; Thompson, W.; Bouthors, C.; Le Huec, J.C. Which parameters are relevant in sagittal balance analysis of the cervical spine? A literature review. Eur. Spine J. 2018, 27 (Suppl. 1), 8–15. [Google Scholar] [CrossRef]
- Harrison, D.E.; Harrison, D.D.; Cailliet, R.; Troyanovich, S.J.; Janik, T.J.; Holland, B. Cobb method or Harrison posterior tangent method: Which to choose for lateral cervical radiographic analysis. Spine 2000, 25, 2072–2078. [Google Scholar] [CrossRef]
- Patwardhan, A.G.; Havey, R.M.; Carandang, G.; Simonds, J.; Voronov, L.I.; Ghanayem, A.J.; Meade, K.P.; Gavin, T.M.; Paxinos, O. Effect of compressive follower preload on the flexion-extension response of the human lumbar spine. J. Orthop. Res. 2003, 21, 540–546. [Google Scholar] [CrossRef]
- Seichi, A.; Takeshita, K.; Ohishi, I.; Kawaguchi, H.; Akune, T.; Anamizu, Y.; Kitagawa, T.; Nakamura, K. Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine 2001, 26, 479–487. [Google Scholar] [CrossRef]
- Ratliff, J.K.; Cooper, P.R. Cervical laminoplasty: A critical review. J. Neurosurg. 2003, 98 (Suppl. 3), 230–238. [Google Scholar] [CrossRef]
- Lee, J.Y.; Sharan, A.; Baron, E.M.; Lim, M.R.; Grossman, E.; Albert, T.J.; Vaccaro, A.R.; Hilibrand, A.S. Quantitative prediction of spinal cord drift after cervical laminectomy and arthrodesis. Spine 2006, 31, 1795–1798. [Google Scholar] [CrossRef]
- Inose, H.; Yoshii, T.; Kimura, A.; Takeshita, K.; Inoue, H.; Maekawa, A.; Endo, K.; Furuya, T.; Nakamura, A.; Mori, K.; et al. Factors Negatively Influencing Postoperative Improvement after Laminoplasty in Degenerative Cervical Myelopathy. Clin. Spine Surg. 2021, 35, E230–E235. [Google Scholar] [CrossRef]
- Bridges, K.J.; Simpson, L.N.; Bullis, C.L.; Rekito, A.; Sayama, C.M.; Than, K.D. Combined Laminoplasty and Posterior Fusion for Cervical Spondylotic Myelopathy Treatment: A Literature Review. Asian Spine J. 2018, 12, 446–458. [Google Scholar] [CrossRef] [PubMed]
- Azimi, P.; Yazdanian, T.; Benzel, E.C.; Hai, Y.; Montazeri, A. Sagittal balance of the cervical spine: A systematic review and meta-analysis. Eur. Spine J. 2021, 30, 1411–1439. [Google Scholar] [CrossRef] [PubMed]
- Matsunaga, S.; Sakou, T.; Nakanisi, K. Analysis of the cervical spine alignment following laminoplasty and laminectomy. Spinal Cord 1999, 37, 20–24. [Google Scholar] [CrossRef]
- Khuyagbaatar, B.; Kim, K.; Park, W.M.; Lee, S.; Kim, Y.H. Increased stress and strain on the spinal cord due to ossification of the posterior longitudinal ligament in the cervical spine under flexion after laminectomy. Proc. Inst. Mech. Eng. H 2017, 231, 898–906. [Google Scholar] [CrossRef] [PubMed]
- Hashiguchi, A.; Kanchiku, T.; Nishida, N.; Taguchi, T. Biomechanical Study of Cervical Posterior Decompression. Asian Spine J. 2018, 12, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Kode, S.; Kallemeyn, N.A.; Smucker, J.D.; Fredericks, D.C.; Grosland, N.M. The effect of multi-level laminoplasty and laminectomy on the biomechanics of the cervical spine: A finite element study. Iowa Orthop. J. 2014, 34, 150–157. [Google Scholar] [PubMed]
- Kubo, S.; Goel, V.K.; Yang, S.J.; Tajima, N. The biomechanical effects of multilevel posterior foraminotomy and foraminotomy with double-door laminoplasty. J. Spinal Disord. Tech. 2002, 15, 477–485. [Google Scholar] [CrossRef]
- Subramaniam, V.; Chamberlain, R.H.; Theodore, N.; Baek, S.; Safavi-Abbasi, S.; Senoglu, M.; Sonntag, V.K.H.; Crawford, N.R. Biomechanical effects of laminoplasty versus laminectomy: Stenosis and stability. Spine 2009, 34, E573–E578. [Google Scholar] [CrossRef] [Green Version]





| Component | Material Properties | Constitute Relation | Element Type | Area (mm2) |
|---|---|---|---|---|
| Bone | ||||
| Vertebral cortical bone | E = 10,000 Mpa | Isotropic, Elastic | C3D8 | - |
| v = 0.3 | ||||
| Vertebral cancellous bone | E = 450 Mpa | Isotropic, Elastic | C3D9 | - |
| v = 0.25 | ||||
| Vertebrae-Posterior | E = 3500 Mpa | Isotropic, Elastic | C3D10 | - |
| v = 0.25 | ||||
| Artificial bone | E = 10,000 Mpa | Isotropic, Elastic | C3D8 | - |
| v = 0.3 | ||||
| Intervertebral Disc | ||||
| Ground substance of annulus fibrosis | C10 = 0.7 | Hyper-elastic, Mooney-Rivlin | C3D8 | - |
| C01 = 0.2 | ||||
| Nucleus pulposus | C10 = 0.12 | Incompressible Hyper-elastic, Mooney-Rivlin | C3D8 | - |
| C01 = 0.03 | ||||
| D1 = 0 | ||||
| Ligaments | ||||
| Anterior Longitudinal Ligament | 15.0 (<12%), 30.0 (>12%) | Non-linear, Hypoelastic | T3D2 | 6.1 |
| v = 0.3 | ||||
| Posterior Longitudinal Ligament | 10.0 (<12%), 20.0 (>12%) | Non-linear, Hypoelastic | T3D3 | 5.4 |
| v = 0.3 | ||||
| Capsular Ligament | 7.0 (<30%), 30 (>12%) | Non-linear, Hypoelastic | T3D4 | 46.6 |
| v = 0.3 | ||||
| Ligamentum Flavum | 5.0 (<25%), 10.0 (>25%) | Non-linear, Hypoelastic | T3D5 | 50.1 |
| v = 0.3 | ||||
| Interspinous Ligament | 4.0 (20–40%), 8.0 (>40%) | Non-linear, Hypoelastic | T3D6 | 13.1 |
| v = 0.3 | ||||
| Facet Joints | ||||
| Apophyseal Joints | Non-linear Soft contact, GAPPUNI elements | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nishida, N.; Mumtaz, M.; Tripathi, S.; Kelkar, A.; Mendoza, J.; Kumaran, Y.; Goel, V.K. Laminoplasty on Kyphotic Cervical Alignments Suggests Poor Surgical Outcomes: A Comparative Finite Element Analysis of Laminoplasty on Different Alignments. Appl. Sci. 2022, 12, 9089. https://doi.org/10.3390/app12189089
Nishida N, Mumtaz M, Tripathi S, Kelkar A, Mendoza J, Kumaran Y, Goel VK. Laminoplasty on Kyphotic Cervical Alignments Suggests Poor Surgical Outcomes: A Comparative Finite Element Analysis of Laminoplasty on Different Alignments. Applied Sciences. 2022; 12(18):9089. https://doi.org/10.3390/app12189089
Chicago/Turabian StyleNishida, Norihiro, Muzammil Mumtaz, Sudharshan Tripathi, Amey Kelkar, Justin Mendoza, Yogesh Kumaran, and Vijay K. Goel. 2022. "Laminoplasty on Kyphotic Cervical Alignments Suggests Poor Surgical Outcomes: A Comparative Finite Element Analysis of Laminoplasty on Different Alignments" Applied Sciences 12, no. 18: 9089. https://doi.org/10.3390/app12189089
APA StyleNishida, N., Mumtaz, M., Tripathi, S., Kelkar, A., Mendoza, J., Kumaran, Y., & Goel, V. K. (2022). Laminoplasty on Kyphotic Cervical Alignments Suggests Poor Surgical Outcomes: A Comparative Finite Element Analysis of Laminoplasty on Different Alignments. Applied Sciences, 12(18), 9089. https://doi.org/10.3390/app12189089







