Effect of Different Crestal Sinus Lift Techniques for Implant Placement in the Posterior Maxilla of Deficient Height: A Randomized Clinical Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Aspect and Patient Induction
2.2. Presurgical Therapy and Grouping
2.3. Randomization and Allocation
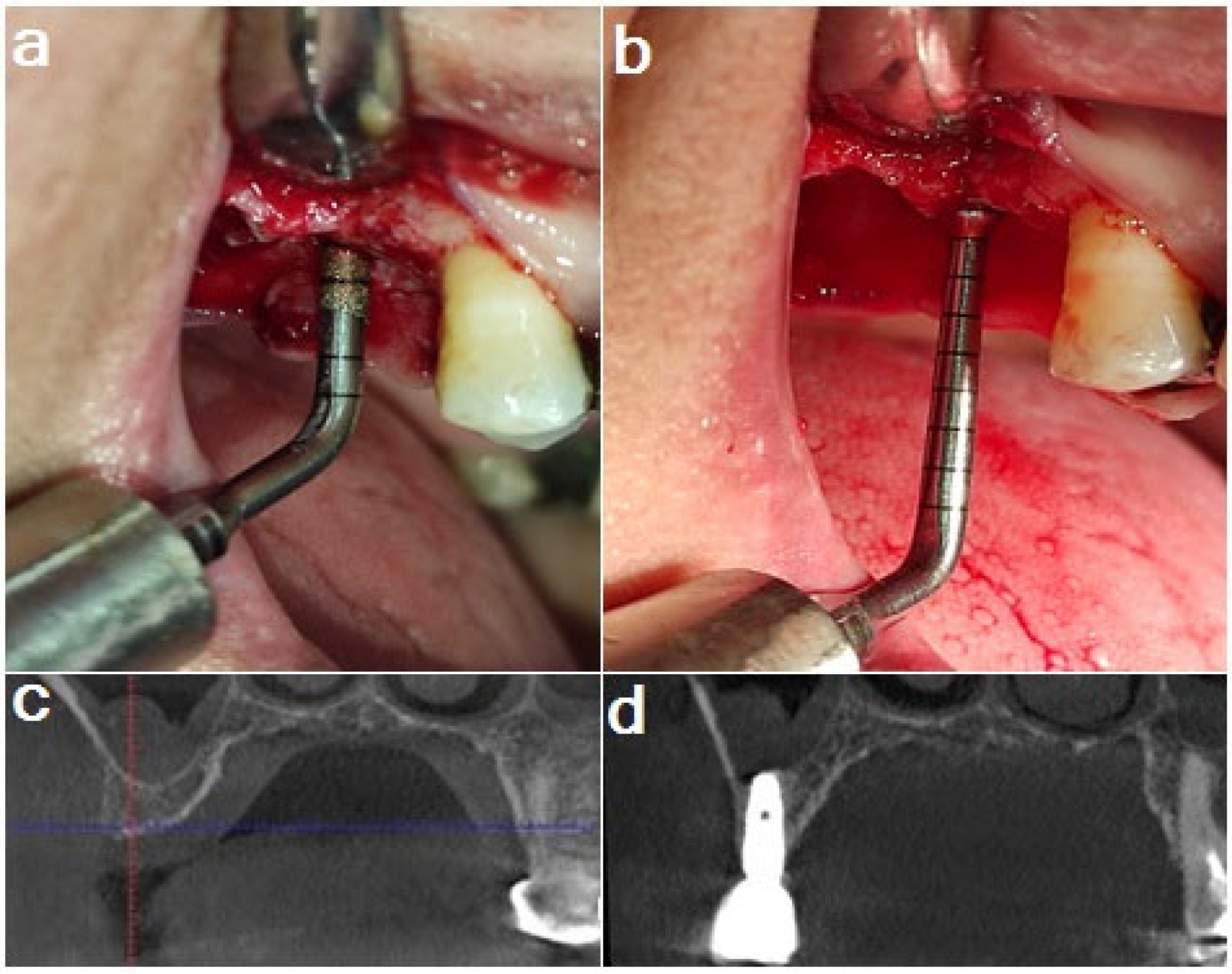
2.4. Surgical Procedures
2.5. Bone Graft and Implant Placement
2.6. Implant Stability Measurement
2.7. Postoperative Care
2.8. Follow-Up and Procedures
2.9. Radiographic Evaluation
2.9.1. Bone Height
2.9.2. Bone Density
2.9.3. Crestal Bone Loss (CBL)
2.10. Primary and Secondary Outcomes
2.11. Statistical Analysis
3. Results
3.1. Implant Stability
3.2. Bone Height (mm)
- (a)
- Comparisons of bone height measurements among the three groups
- (b)
- Vertical bone gain comparison
3.3. Bone Density (HU)
3.4. Crestal Bone Loss (mm)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sato, T.; Abe, T.; Nakamoto, N.; Tomaru, Y.; Koshikiya, N.; Nojima, J.; Kokabu, S.; Sakata, Y.; Kobayashi, A.; Yoda, T. Nicotine Induces Cell Proliferation in Association with Cyclin D1 up-Regulation and Inhibits Cell Differentiation in Association with P53 Regulation in a Murine Pre-Osteoblastic Cell Line. Biochem. Biophys. Res. Commun. 2008, 377, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Mertens, C.; Meyer-Bäumer, A.; Kappel, H.; Hoffmann, J.; Steveling, H.G. Use of 8-Mm and 9-Mm Implants in Atrophic Alveolar Ridges: 10-Year Results. Int. J. Oral Maxillofac. Implant. 2012, 27, 1501–1508. [Google Scholar]
- Sennerby, L.; Roos, J. Surgical Determinants of Clinical Success of Osseointegrated Oral Implants: A Review of the Literature. Int. J. Prosthodont. 1998, 11, 408–420. [Google Scholar]
- Kim, B.; Lee, J. The Retrospective Study of Survival Rate of Implants with Maxillary Sinus Floor Elevation. J. Korean Assoc. Oral Maxillofac. Surg. 2010, 36, 108. [Google Scholar] [CrossRef]
- Kim, Y.K.; Hwang, J.Y.; Yun, P.Y. Relationship between Prognosis of Dental Implants and Maxillary Sinusitis Associated with the Sinus Elevation Procedure. Int. J. Oral Maxillofac. Implant. 2013, 28, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Morand, M.; Irinakis, T. The Challenge of Implant Therapy in the Posterior Maxilla: Providing a Rationale for the Use of Short Implants. J. Oral Implant. 2007, 33, 257–266. [Google Scholar] [CrossRef]
- Tatum, H., Jr. Maxillary and Sinus Implant Reconstructions. Dent. Clin. N. Am. 1986, 30, 207–229. [Google Scholar] [CrossRef]
- Wallace, S.S.; Froum, S.J. Effect of Maxillary Sinus Augmentation on the Survival of Endosseous Dental Implants. A Systematic Review. Ann. Periodontol. 2003, 8, 328–343. [Google Scholar] [CrossRef]
- Wallace, S.S.; Mazor, Z.; Froum, S.J.; Cho, S.C.; Tarnow, D.P. Schneiderian Membrane Perforation Rate During Sinus Elevation Using Piezosurgery: Clinical Results of 100 Consecutive Cases. Int. J. Periodontics Restor. Dent. 2007, 27, 413–419. [Google Scholar]
- Reiser, G.M.; Rabinovitz, Z.; Bruno, J.; Damoulis, P.D.; Griffin, T.J. Evaluation of Maxillary Sinus Membrane Response Following Elevation with the Crestal Osteotome Technique in Human Cadavers. Int. J. Oral Maxillofac. Implant. 2001, 16, 833–840. [Google Scholar]
- Summers, R.B. A New Concept in Maxillary Implant Surgery: The Osteotome Technique. Compendium 1994, 15, 154–156. [Google Scholar]
- Toffler, M.; Rosen, P. Complications with Transcrestal Sinus Floor Elevation: Etiology, Prevention, and Treatment. In Dental Implant Complications; Stuart, J.F., Ed.; Wiley Blackwell: Hoboken, NJ, USA, 2015. [Google Scholar]
- Vercellotti, T.; De Paoli, S.; Nevins, M. The Piezoelectric Bony Window Osteotomy and Sinus Membrane Elevation: Introduction of a New Technique for Simplification of the Sinus Augmentation Procedure. Int. J. Periodontics. Restor. Dent 2001, 21, 561–567. [Google Scholar]
- Stübinger, S.; Kuttenberger, J.; Filippi, A.; Sader, R.; Zeilhofer, H.F. Intraoral Piezosurgery: Preliminary Results of a New Technique. J. Oral Maxillofac. Surg. 2005, 63, 1283–1287. [Google Scholar] [CrossRef]
- Toscano, N.J.; Holtzclaw, D.; Rosen, P.S. The Effect of Piezoelectric Use on Open Sinus Lift Perforation: A Retrospective Evaluation of 56 Consecutively Treated Cases from Private Practices. J. Periodontol. 2010, 81, 167–171. [Google Scholar] [CrossRef]
- Li, J.; Lee, K.; Chen, H.; Ou, G. Piezoelectric Surgery in Maxillary Sinus Floor Elevation with Hydraulic Pressure for Xenograft and Simultaneous Implant Placement. J. Prosthet. Dent. 2013, 110, 344–348. [Google Scholar] [CrossRef]
- Huwais, S.; Meyer, E.G. A Novel Osseous Densification Approach in Implant Osteotomy Preparation to Increase Biomechanical Primary Stability, Bone Mineral Density, and Bone-to-Implant Contact. Int. J. Oral Maxillofac. Implant. 2017, 32, 27–36. [Google Scholar] [CrossRef]
- Sammartino, G.; Prados-Frutos, J.C.; Riccitiello, F.; Felice, P.; Cerone, V.; Gasparro, R.; Wang, H.L. The Relevance of the Use of Radiographic Planning in Order to Avoid Complications in Mandibular Implantology: A Retrospective Study. BioMed Res. Int. 2016, 2016, 8175284. [Google Scholar] [CrossRef]
- Shahidi, S.; Zamiri, B.; Abolvardi, M.; Akhlaghian, M.; Paknahad, M. Comparison of Dental Panoramic Radiography and Cbct for Measuring Vertical Bone Height in Different Horizontal Locations of Posterior Mandibular Alveolar Process. J. Dent. 2018, 19, 83–91. [Google Scholar]
- Pattijn, V.; Van Lierde, C.; Van Der Perre, G.; Naert, I.; Vander Sloten, J. The Resonance Frequencies and Mode Shapes of Dental Implants: Rigid Body Behaviour Versus Bending Behaviour. A Numerical Approach. J. Biomech. 2006, 39, 939–947. [Google Scholar] [CrossRef]
- Huang, H.; Wu, G.; Hunziker, E. The Clinical Significance of Implant Stability Quotient (Isq) Measurements: A Literature Review. J. Oral Biol. Craniofac. Res. 2020, 10, 629–638. [Google Scholar]
- El-Destawy, M.T.; Khedr, M.F.; Hosny, M.M.; Bilal, A.M.; Elshamy, A.M.; El Sayed, I.S.; Borhamy, A.E.; Aboamo, A.A.; Gamal, A.Y. A Novel Approach of Periodontal Osseous Wall Piezosplitting and Sequential Bone Expansion in Management of Localized Intra-Bony Defects with Wide Angulation—A Randomized Controlled Trial. Healthcare 2023, 6, 791. [Google Scholar] [CrossRef]
- Sculean, A.; Stavropoulos, A.; Windisch, P.; Keglevich, T.; Karring, T.; Gera, I. Healing of Human Intrabony Defects Following Regenerative Periodontal Therapy with a Bovine-Derived Xenograft and Guided Tissue Regeneration. Clin. Oral Investig. 2004, 8, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Baldi, D.; Menini, M.; Pera, F.; Ravera, G.; Pera, P. Sinus Floor Elevation Using Osteotomes or Piezoelectric Surgery. Int. J. Oral Maxillofac. Surg. 2011, 40, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Simunek, A.; Cierny, M.; Kopecka, D.; Kohout, A.; Bukac, J.; Vahalova, D. The Sinus Lift with Phycogenic Bone Substitute. A Histomorphometric Study. Clin. Oral Implant. Res. 2005, 16, 342–348. [Google Scholar] [CrossRef]
- Hieu, P.D.; Chung, J.H.; Yim, S.B.; Hong, K.S. A Radiographical Study on the Changes in Height of Grafting Materials after Sinus Lift: A Comparison between Two Types of Xenogenic Materials. J. Periodontal Implant Sci. 2010, 40, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Sorní, M.; Guarinos, J.; Penarrocha, M. Implants in Anatomical Buttresses of the Upper Jaw. Med. Oral Patol. Oral Cir. Bucal 2005, 10, 163–168. [Google Scholar]
- Mittal, Y.; Jindal, G.; Garg, S. Bone Manipulation Procedures in Dental Implants. Indian J. Dent. 2016, 7, 86–94. [Google Scholar] [CrossRef]
- Huwais, S.; Mazor, Z.; Ioannou, A.L.; Gluckman, H.; Neiva, R. A Multicenter Retrospective Clinical Study with up-to-5-Year Follow-up Utilizing a Method That Enhances Bone Density and Allows for Transcrestal Sinus Augmentation through Compaction Grafting. Int. J. Oral Maxillofac. Implant. 2018, 33, 1305–1311. [Google Scholar] [CrossRef]
- Baron, T.K.; Venkatraman, N. Minimally Invasive Crestal Approach Sinus Floor Elevation Using Densah Burs, and Hydraulic Lift Utilising Putty Graft in Cartridge Delivery. Clin. Oral Implant. Res. 2017, 28, 203. [Google Scholar]
- El-Ghobashy, M.T.; Shaaban, A.M.; Melek, L.N. Osseodensification by Densah Burs Versus Osteotome for Transcrestal Maxillary Sinus Lifting with Simultaneous Implant Placement. Alex. Dent. J. 2023, 48, 51–58. [Google Scholar] [CrossRef]
- Hamdi, D.; Hemd, D. Comparison between Osseo Densification Burs and Osteotome Technique for Closed Sinus Lift in Partially Edentulous Maxilla (Clinical and Radiological Study). J. Univ. Shanghai Sci. Technol. 2021, 23, 392–411. [Google Scholar] [CrossRef]
- Amira, K.A. Assessment of Dental Implants Placed in Posterior Maxillary Ridge Using Densah Burs Versus Standard Drills. Master’s Thesis, Cairo University, Cairo, Egypt, 2018. [Google Scholar]
- Arafat, S.W.; A Elbaz, M. Clinical and Radiographic Evaluation of Osseodensification Versus Osteotome for Sinus Floor Elevation in Partially Atrophic Maxilla: A Prospective Long Term Study. Egypt. Dent. J. 2019, 65, 189–195. [Google Scholar] [CrossRef]
- Ahmed Mohamed, B.; Mohamed Mohamed, B.; Akram Abbass, A.-A.; Mahmoud Taha, E.-D.; Mostafa Mohamed, H. Clinical and Radiographic Evaluation of Crestal Ridge Splitting Versus Osseodensification Techniques for Dental Implant Placement into the Narrow Alveolar Ridge. J. Int. Dent. Med. Res. 2022, 15, 205–211. [Google Scholar]
- Lahens, B.; Neiva, R.; Tovar, N.; Alifarag, A.M.; Jimbo, R.; Bonfante, E.A.; Bowers, M.M.; Cuppini, M.; Freitas, H.; Witek, L.; et al. Biomechanical and Histologic Basis of Osseodensification Drilling for Endosteal Implant Placement in Low Density Bone. An Experimental Study in Sheep. J. Mech. Behav. Biomed. Mater. 2016, 63, 56–65. [Google Scholar] [CrossRef]
- Beziat, J.L.; Vercellotti, T.; Gleizal, A. What Is Piezosurgery? Two-Years Experience in Craniomaxillofacial Surgery. Rev. Stomatol. Chir. Maxillofac 2007, 108, 101–107. [Google Scholar] [CrossRef]
- Slete, F.B.; Olin, P.; Prasad, H. Histomorphometric Comparison of 3 Osteotomy Techniques. Implant. Dent. 2018, 27, 424–428. [Google Scholar] [CrossRef]
- Schlee, M.; Steigmann, M.; Bratu, E.; Garg, A.K. Piezosurgery: Basics and Possibilities. Implant. Dent. 2006, 15, 334–340. [Google Scholar] [CrossRef]
- Vercellotti, T. Technological Characteristics and Clinical Indications of Piezoelectric Bone Surgery. Minerva Stomatol. 2004, 53, 207–214. [Google Scholar]
- Albrektsson, T.; Isidor, F. Proceedings of the First European Workshop on Periodontology; Quintessence Publishing: London, UK, 1994. [Google Scholar]
- Cordioli, G.; Mazzocco, C.; Schepers, E.; Brugnolo, E.; Majzoub, Z. Maxillary Sinus Floor Augmentation Using Bioactive Glass Granules and Autogenous Bone with Simultaneous Implant Placement. Clinical and Histological Findings. Clin. Oral Implant. Res. 2001, 12, 270–278. [Google Scholar] [CrossRef]
- Moy, P.K.; Lundgren, S.; Holmes, R.E. Maxillary Sinus Augmentation: Histomorphometric Analysis of Graft Materials for Maxillary Sinus Floor Augmentation. J. Oral Maxillofac. Surg. 1993, 51, 857–862. [Google Scholar] [CrossRef]
- Boëck-Neto, R.J.; Gabrielli, M.; Lia, R.; Marcantonio, E.; Shibli, J.A.; Marcantonio, E., Jr. Histomorphometrical Analysis of Bone Formed after Maxillary Sinus Floor Augmentation by Grafting with a Combination of Autogenous Bone and Demineralized Freeze-Dried Bone Allograft or Hydroxyapatite. J. Periodontol. 2002, 73, 266–270. [Google Scholar] [CrossRef] [PubMed]
- Maiorana, C.; Redemagni, M.; Rabagliati, M.; Salina, S. Treatment of Maxillary Ridge Resorption by Sinus Augmentation with Iliac Cancellous Bone, Anorganic Bovine Bone, and Endosseous Implants: A Clinical and Histologic Report. Int. J. Oral Maxillofac. Implant. 2000, 15, 873–878. [Google Scholar]
- Emmerich, D.; Att, W.; Stappert, C. Sinus Floor Elevation Using Osteotomes: A Systematic Review and Meta-Analysis. J. Periodontol. 2005, 76, 1237–1251. [Google Scholar] [CrossRef] [PubMed]
- Rodoni, L.R.; Glauser, R.; Feloutzis, A.; Hämmerle, C.H. Implants in the Posterior Maxilla: A Comparative Clinical and Radiologic Study. Int. J. Oral Maxillofac. Implant. 2005, 20, 231–237. [Google Scholar]







| Time | Densah (n = 7) | Piezo (n = 7) | Osteotome (n = 7) | p Value | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Baseline | 74.2 A | 3.9 | 62.8 C | 4.7 | 68.5 B | 2.2 | <0.001 * |
| At 6-month follow-up | 87.1 A | 3.3 | 71.8 B | 4.8 | 80.2 B | 1.6 | <0.001 * |
| Time | Densah (n = 7) | Piezo (n = 7) | Osteotome (n = 7) | p Value | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Baseline | 4.66 | 0.37 | 4.7 | 0.45 | 4.68 | 0.26 | 0.982 |
| At 6-month follow-up | 10.47 B | 0.59 | 10.41 B | 0.49 | 11.61 A | 0.53 | 0.001 * |
| Densah (n = 7) | Piezo (n = 7) | Osteotome (n = 7) | p Value | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| 5.81 B | 0.51 | 5.72 B | 0.44 | 6.93 A | 0.45 | <0.001 * |
| Time | Densah (n = 7) | Piezo (n = 7) | Osteotome (n = 7) | p Value * | |||
|---|---|---|---|---|---|---|---|
| Median | Range | Median | Range | Median | Range | ||
| Baseline | 266.4 | 106.6–464.4 | 224.8 | 124.9–412.1 | 248.8 | 166.2–523.9 | 0.754 |
| At 6-month follow-up | 660.3 | 350.9–740.2 | 560.4 | 388.1–701 | 530.4 | 444.8–890.7 | 0.580 |
| Side | Densah (n = 7) | Piezo (n = 7) | Osteotome (n = 7) | p Value * | |||
|---|---|---|---|---|---|---|---|
| Median | Range | Median | Range | Median | Range | ||
| Buccal | 0.24 | 0–0.96 | 0.7 | 0.45–1.2 | 0.6 | 0–1.14 | 0.193 |
| Palatal | 0.08 | 0–0.64 | 0.66 | 0.3–0.9 | 0.4 | 0–0.82 | 0.071 |
| Overall | 0.2 | 0–0.73 | 0.66 | 0.4–1.05 | 0.43 | 0–0.97 | 0.073 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hashem, A.H.; Khedr, M.F.; Hosny, M.M.; El-Destawy, M.T.; Hashem, M.I. Effect of Different Crestal Sinus Lift Techniques for Implant Placement in the Posterior Maxilla of Deficient Height: A Randomized Clinical Trial. Appl. Sci. 2023, 13, 6668. https://doi.org/10.3390/app13116668
Hashem AH, Khedr MF, Hosny MM, El-Destawy MT, Hashem MI. Effect of Different Crestal Sinus Lift Techniques for Implant Placement in the Posterior Maxilla of Deficient Height: A Randomized Clinical Trial. Applied Sciences. 2023; 13(11):6668. https://doi.org/10.3390/app13116668
Chicago/Turabian StyleHashem, Ahmed Halim, Mohamed Fekry Khedr, Mostafa Mohamed Hosny, Mahmoud Taha El-Destawy, and Mohamed Ibrahim Hashem. 2023. "Effect of Different Crestal Sinus Lift Techniques for Implant Placement in the Posterior Maxilla of Deficient Height: A Randomized Clinical Trial" Applied Sciences 13, no. 11: 6668. https://doi.org/10.3390/app13116668




