Factors Associated with the Proximity of the Incisive Canal to the Maxillary Central Incisor
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
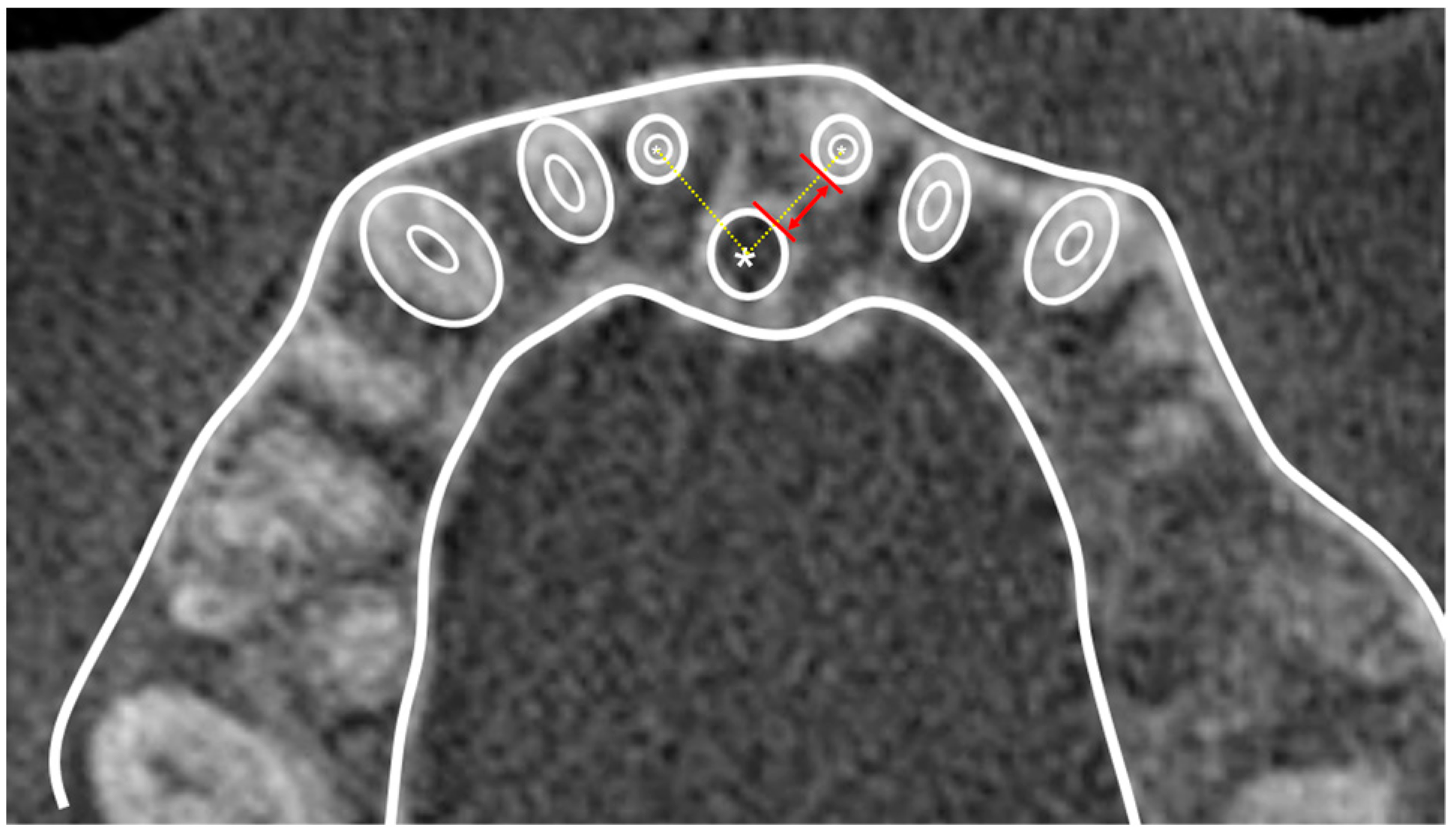
2.2. Data Acquisition and Measurements
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sarver, D.M. The importance of incisor positioning in the esthetic smile: The smile arc. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 98–111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zachrisson, B.U. Esthetic factors involved in anterior tooth display and the smile: Vertical dimension. J. Clin. Orthod. 1998, 32, 432–445. [Google Scholar]
- Riedel, R.A. Esthetics and its relation to orthodontic therapy. Angle Orthod. 1950, 20, 168–178. [Google Scholar] [CrossRef] [PubMed]
- Barteczko, K.; Jacob, M. A re-evaluation of the premaxillary bone in humans. Anat. Embryol. 2004, 207, 417–437. [Google Scholar] [CrossRef]
- Hong, S.Y.; Shin, J.W.; Hong, C.; Chan, V.; Baik, U.B.; Kim, Y.H.; Chae, H.S. Alveolar bone remodeling during maxillary incisor intrusion and retraction. Prog. Orthod. 2019, 20, 47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gull, M.A.B.; Maqbool, S.; Mushtaq, M.; Ahmad, A. Evaluation of morphologic features and proximity of incisive canal to the maxillary central incisors using cone beam computed tomography. Angle Orthod. 2018, 17, 46–50. [Google Scholar]
- Chung, C.J.; Choi, Y.J.; Kim, K.H. Approximation and contact of the maxillary central incisor roots with the incisive canal after maximum retraction with temporary anchorage devices: Report of 2 patients. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 493–502. [Google Scholar] [CrossRef] [Green Version]
- Uesugi, S.; Imamura, T.; Kokai, S.; Ono, T. Cone-beam computed tomography-based diagnosis and treatment simulation for a patient with a protrusive profile and a gummy smile. Korean J. Orthod. 2018, 48, 189–199. [Google Scholar] [CrossRef]
- Pan, Y.; Chen, S. Contact of the incisive canal and upper central incisors causing root resorption after retraction with orthodontic mini-implants: A CBCT study. Angle Orthod. 2019, 89, 200–205. [Google Scholar] [CrossRef] [Green Version]
- William, R.P.; Henry, W.F., Jr.; Brent, E.L.; David, M.S. Contemporary Orthodontics, 6th ed.; Elsevier: St. Louis, MI, USA, 2018; pp. 657–809. [Google Scholar]
- Proffit, W.R.; Ackerman, J.L. Diagnosis and treatment planning. In Current Orthodontic Concepts and Techniques; Graber, T.M., Swain, B.F., Eds.; Mosby: St. Louis, MI, USA, 1982; pp. 3–100. [Google Scholar]
- Sheng, Y.; Guo, H.M.; Bai, Y.X.; Li, S. Dehiscence and fenestration in anterior teeth: Comparison before and after orthodontic treatment. J. Orofac. Orthop. 2020, 81, 1–9. [Google Scholar] [CrossRef]
- Hoang, N.; Nelson, G.; Hatcher, D.; Oberoi, S. Evaluation of mandibular anterior alveolus in different skeletal patterns. Prog. Orthod. 2016, 17, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wainwright, W.M. Faciolingual tooth movement: Its influence on the root and cortical plate. Am. J. Orthod. 1973, 64, 278–302. [Google Scholar] [CrossRef] [PubMed]
- Ten Hoeve, A.; Mulie, R.M. The effect of antero-postero incisor repositioning on the palatal cortex as studied with laminagraphy. J. Clin. Orthod. 1976, 10, 804–822. [Google Scholar]
- Kaley, J.; Phillips, C. Factors related to root resorption in edgewise practice. Angle Orthod. 1991, 61, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Horiuchi, A.; Hotokezaka, H.; Kobayashi, K. Correlation between cortical plate proximity and apical root resorption. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Sadek, M.M.; Sabet, N.E.; Hassan, I.T. Alveolar bone mapping in subjects with different vertical facial dimensions. Eur. J. Orthod. 2015, 37, 194–201. [Google Scholar] [CrossRef]
- Alhadlaq, A.M. Association between anterior alveolar dimensions and vertical facial pattern among Saudi adults. Saudi Dent. J. 2016, 28, 70–75. [Google Scholar] [CrossRef] [Green Version]
- Cho, E.A.; Kim, S.J.; Choi, Y.J.; Kim, K.H.; Chung, C.J. Morphologic evaluation of the incisive canal and its proximity to the maxillary central incisors using computed tomography images. Angle Orthod. 2016, 86, 571–576. [Google Scholar] [CrossRef] [Green Version]
- Mraiwa, N.; Jacobs, R.; Van Cleynenbreugel, J.; Sanderink, G.; Schutyser, F.; Suetens, P.; van Steenberghe, D.; Quirynen, M. The nasopalatine canal revisited using 2D and 3D CT imaging. Dentomaxillofacial Radiol. 2004, 33, 396–402. [Google Scholar] [CrossRef]
- Liang, X.; Jacobs, R.; Martens, W.; Hu, Y.; Adriaensens, P.; Quirynen, M.; Lambrichts, I. Macro- and micro-anatomical, histological and computed tomography scan characterization of the nasopalatine canal. J. Clin. Periodontol. 2009, 36, 598–603. [Google Scholar] [CrossRef] [Green Version]
- Song, W.C.; Jo, D.I.; Lee, J.Y.; Kim, J.N.; Hur, M.S.; Hu, K.S.; Kim, H.J.; Shin, C.; Koh, K.S. Microanatomy of the incisive canal using three-dimensional reconstruction of microCT images: An ex vivo study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 108, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Thakur, A.R.; Burde, K.; Guttal, K.; Naikmasur, V.G. Anatomy and morphology of the nasopalatine canal using cone-beam computed tomography. Imaging Sci. Dent. 2013, 43, 273–281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antúnez, V.; Vicente, J. Hipótesis para un derecho alternativo desde la perspectiva latinoamericana. Opción 2016, 32, 7–10. [Google Scholar]
- Da Costa, E.D.D.; Nejaim, Y.; Martins, L.A.C.; Peyneau, P.D.; Ambrosano, G.M.B.; Oliveira, M.L. Morphological evaluation of the nasopalatine canal in patients with different facial profiles and ages. J. Oral Maxillofac. Surg. 2019, 77, 721–729. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, T.; Ishida, Y.; Kawabe, A.; Ono, T. Quantitative analysis of the relationship between maxillary incisors and the incisive canal by cone-beam computed tomography in an adult Japanese population. Prog. Orthod. 2017, 18, 24. [Google Scholar] [CrossRef] [PubMed]
- Lake, S.; Iwanaga, J.; Kikuta, S.; Oskouian, R.J.; Loukas, M.; Tubbs, R.S. The incisive canal: A comprehensive review. Cureus 2018, 10, e3069. [Google Scholar] [CrossRef] [Green Version]
- Khurana, S.; Parasher, P.; Mukherjee, P.; Mupparapu, M.; Lotlikar, P.P.; Creanga, A.G. Cone beam computed tomographic–based retrospective study on Newark population for the assessment of distance between incisive canal and maxillary central incisors: Clinical implications. Indian J. Dent. Res. 2020, 31, 175–179. [Google Scholar] [CrossRef]
- Yu, J.H.; Nguyen, T.; Kim, Y.I.; Hwang, S.; Kim, K.H.; Chung, C.J. Morphologic changes of the incisive canal and its proximity to maxillary incisor roots after anterior tooth movement. Am. J. Orthod. Dentofac. Orthop. 2022, 161, 396–403.e1. [Google Scholar] [CrossRef]
- Chung, C.J.; Nguyen, T.; Lee, J.H.; Kim, K.H. Incisive canal remodelling following maximum anterior retraction reduces apical root resorption. Orthod. Craniofac. Res. 2021, 24 (Suppl. S1), 59–65. [Google Scholar] [CrossRef]
- Nakada, T.; Motoyoshi, M.; Horinuki, E.; Shimizu, N. Cone-beam computed tomography evaluation of the association of cortical plate proximity and apical root resorption after orthodontic treatment. J. Oral Sci. 2016, 58, 231–236. [Google Scholar] [CrossRef] [Green Version]
- Imamura, T.; Uesugi, S.; Ono, T. Unilateral maxillary central incisor root resorption after orthodontic treatment for Angle Class II, division 1 malocclusion with significant maxillary midline deviation: A possible correlation with root proximity to the incisive canal. Korean J. Orthod. 2020, 50, 216–226. [Google Scholar] [CrossRef] [PubMed]
- Ono, T. Should the “envelope of discrepancy” be revised in the era of three-dimensional imaging? J. World Fed. Orthod. 2020, 9, S59–S66. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, R.; Lambrichts, I.; Liang, X.; Martens, W.; Mraiwa, N.; Adriaensens, P.; Gelan, J. Neurovascularization of the anterior jaw bones revisited using high-resolution magnetic resonance imaging. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2007, 103, 683–693. [Google Scholar] [CrossRef] [PubMed]
- Langrodi, S.S.R.; Goudarzi, F.; Stanbouly, D. Etiology of Tinnitus on CT and CBCT: A Narrative Review. Int. Tinnitus J. 2022, 26, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Raber, A.; Kula, K.; Ghoneima, A. Three-dimensional evaluation of labial alveolar bone overlying the maxillary and mandibular incisors in different skeletal classifications of malocclusion. Int. Orthod. 2019, 17, 287–295. [Google Scholar] [CrossRef]
- Pepicelli, A.; Woods, M.; Briggs, C. The mandibular muscles and their importance in orthodontics: A contemporary review. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 774–780. [Google Scholar] [CrossRef]
- Costa, E.D.; de Oliveira Reis, L.; Gaêta-Araujo, H.; Martins, L.A.C.; Oliveira-Santos, C.; Freitas, D.Q. Comparison of distance of upper central incisor root and incisive canal in different sagittal and vertical skeletal patterns and sex: A retrospective CBCT study. Int. Orthod. 2021, 19, 462–470. [Google Scholar] [CrossRef]
- Springate, S.D. The effect of sample size and bias on the reliability of estimates of error: A comparative study of Dahlberg’s formula. Eur. J. Orthod. 2012, 34, 158–163. [Google Scholar] [CrossRef] [Green Version]
- Ongprakobkul, N.; Ishida, Y.; Petdachai, S.; Ishizaki, A.; Shimizu, C.; Techalertpaisarn, P.; Ono, T. Morphometric and volumetric analysis of the proximity between the incisive canal and maxillary central incisors during anterior retraction: A retrospective cone-beam computed tomography study. Angle Orthod. 2022, 93, 159–167. [Google Scholar] [CrossRef]
- Chatriyanuyoke, P.; Lu, C.I.; Suzuki, Y.; Lozada, J.L.; Rungcharassaeng, K.; Kan, J.Y.; Goodacre, C.J. Nasopalatine canal position relative to the maxillary central incisors: A cone beam computed tomography assessment. J. Oral Implantol. 2012, 38, 713–717. [Google Scholar] [CrossRef]
- Kamburoglu, K.; Murat, S.; Kolsuz, E.; Kurt, H.; Yüksel, S.; Paksoy, C. Comparative assessment of subjective image quality of cross-sectional cone-beam computed tomography scans. J. Oral Sci. 2011, 53, 501–508. [Google Scholar] [CrossRef] [Green Version]
- Sang, Y.H.; Hu, H.C.; Lu, S.H.; Wu, Y.W.; Li, W.R.; Tang, Z.H. Accuracy Assessment of Three-dimensional Surface Reconstructions of In vivo Teeth from Cone-beam Computed Tomography. Chin. Med. J. 2016, 29, 1464–1470. [Google Scholar] [CrossRef] [PubMed]
- Liedke, G.S.; da Silveira, H.E.D.; da Silveira, H.E.D.; Dutra, V.; de Figueiredo, J.A.P. Influence of voxel size in the diagnostic ability of cone beam tomography to evaluate simulated external root resorption. J. Endod. 2009, 35, 233–235. [Google Scholar] [CrossRef] [PubMed]
- Kan, J.Y.; Rungcharassaeng, K.; Roe, P.; Mesquida, J.; Chatriyamuyoke, P.; Caruso, J.M. Maxillary central incisor-incisive canal relationship: A cone beam computed tomography study. Am. J. Esthet. Dent. 2012, 2, 180–187. [Google Scholar]
- Ponraj, R.R.; Korath, V.A.; Nagachandran, V.D.; Vijayalakshmi, D.; Parameswaran, R.; Raman, P.; Sunitha, C.; Khan, N. Relationship of anterior alveolar dimensions with mandibular divergence in class I malocclusion—A cephalometric study. J. Clin. Diagn. Res. 2016, 10, ZC29–ZC33. [Google Scholar] [CrossRef]
- Gracco, A.; Lombardo, L.; Mancuso, G.; Gravina, V.; Siciliani, G. Upper incisor position and bony support in untreated patients as seen on CBCT. Angle Orthod. 2009, 79, 692–702. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hwang, S.; Jeong, S.; Choi, Y.J.; Chung, C.J.; Lee, H.S.; Kim, K.H. Three-dimensional evaluation of dentofacial transverse widths of adults with various vertical facial patterns. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 692–700. [Google Scholar] [CrossRef]
- Masumoto, T.; Hayashi, I.; Kawamura, A.; Tanaka, K.; Kasai, K. Relationships among facial type, buccolingual molar inclination, and cortical bone thickness of the mandible. Eur. J. Orthod. 2001, 23, 15–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horner, K.A.; Behrents, R.G.; Kim, K.B.; Buschang, P.H. Cortical bone and ridge thickness of hyperdivergent and hypodivergent adults. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Ozdemir, F.; Tozlu, M.; Germec-Cakan, D. Cortical bone thickness of the alveolar process measured with cone-beam computed tomography in patients with different facial types. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 190–196. [Google Scholar] [CrossRef]
- Güncü, G.N.; Yıldırım, Y.D.; Yılmaz, H.G.; Galindo-Moreno, P.; Velasco-Torres, M.; Al-Hezaimi, K.; Al-Shawaf, R.; Karabulut, E.; Wang, H.L.; Tözüm, T.F. Is there a gender difference in anatomic features of incisive canal and maxillary environmental bone? Clin. Oral Implant. Res. 2013, 24, 1023–1026. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jain, N.V.; Gharatkar, A.A.; Parekh, B.A.; Musani, S.I.; Shah, U.D. Three-dimensional analysis of the anatomical characteristics and dimensions of the nasopalatine canal using cone beam computed tomography. J. Maxillofac. Oral Surg. 2017, 16, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Al-Rokhami, R.K.; Sakran, K.A.; Alhammadi, M.S.; Al-Tayar, B.; Al-Gumaei, W.S.; Al-Yafrusee, E.S.; Al-Shoaibi, L.H.; Cao, B. Tridimensional analysis of incisive canal and upper central incisor approximation. Int. Dent. J. 2022, 73, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Linjawi, A.I.; Marghalani, H.Y.A. Relationship between maxillary central incisors and incisive canal: A cone-beam computed tomography study. Folia Morphol. 2022, 81, 458–463. [Google Scholar] [CrossRef]
- Ackerman, J.L.; Proffit, W.R. Soft tissue limitations in orthodontics: Treatment planning guidelines. Angle Orthod. 1997, 67, 327–336. [Google Scholar] [CrossRef]
- Thongudomporn, U.; Charoemratrote, C.; Jearapongpakorn, S. Changes of anterior maxillary alveolar bone thickness following incisor proclination and extrusion. Angle Orthod. 2015, 85, 549–554. [Google Scholar] [CrossRef] [PubMed]
- Ahn, H.W.; Moon, S.C.; Baek, S.H. Morphometric evaluation of changes in the alveolar bone and roots of the maxillary anterior teeth before and after en masse retraction using cone-beam computed tomography. Angle Orthod. 2013, 83, 212–221. [Google Scholar] [CrossRef] [Green Version]
- Arnaut, A.; Milanovic, P.; Vasiljevic, M.; Jovicic, N.; Vojinovic, R.; Selakovic, D.; Rosic, G. The Shape of Nasopalatine Canal as a Determining Factor in Therapeutic Approach for Orthodontic Teeth Movement-A CBCT Study. Diagnostics 2021, 11, 2345. [Google Scholar] [CrossRef]



| Landmark | Definition | |
|---|---|---|
| N | Nasion | Most anterior point of the nasofrontal suture |
| S | Sella | Center of the sella turcica |
| Or | Orbitale | Most inferior point of the lower margin of the orbit |
| Po | Porion | Most superior point of the external auditory meatus |
| Me | Menton | Most inferior point on the symphysis |
| Pog | pogonion | Most anterior point on the symphysis |
| A | point A | Point of the deepest concavity anteriorly on the maxillary alveolus |
| B | point B | Point of the deepest concavity anteriorly on the mandibular symphysis |
| ANS | anterior nasal spine | Most anterior point of the anterior nasal spine |
| PNS | posterior nasal spine | Most posterior point of anterior nasal spine |
| Ptm | pterygomaxillary fissure | Lowest point of the pterygopalatine fossa |
| U1 | upper incisor | Maxillary central incisal edge |
| SNA (°) | Angle between lines SN and NA planes |
| ANB (°) | Angle between NA and NB planes |
| U1 to FH plane (°) | Angle between Frankfort horizontal (FH) plane and line through the maxillary central incisal edge and root apex (U1 line) |
| U1 to NP plane (mm) | Vertical distance from the maxillary central incisal edge to the facial plane |
| Mandibular plane (°) | Angle between the mandibular and FH planes |
| Palatal plane (°) | Angle between the palatal and FH planes |
| A’-Ptm’ (mm) | Distance between point A and the pterygomaxillary fissure projected on the palatal plane |
| Parameters | Mean | Sex | Site | ||
|---|---|---|---|---|---|
| MCI-IC (mm) | 3.36 ± 1.33 | Male | 3.37 ± 1.30 | right | 3.43 ± 1.38 |
| Female | 3.35 ± 1.34 | left | 3.28 ± 1.37 | ||
| p | p = 0.92 | <0.05 | |||
| MCI-IC Distance | Age (y) | SNA | ANB | U1 to FH | U1 to NP | Mandibular Plane | A’-Ptm’ | |
|---|---|---|---|---|---|---|---|---|
| correlation coefficient | 1 | 0.03 | 0.16 | −0.04 | −0.24 | −0.04 | −0.19 | 0.23 |
| p | 0.70 | 0.04 | 0.66 | 0.00 | 0.63 | 0.02 | 0.00 |
| Model | B | Sth. Error | Beta | t | Sig. |
|---|---|---|---|---|---|
| (constant) | 6.857 | 2.182 | 3.143 | 0.002 | |
| A’-Ptm’ | 0.066 | 0.026 | 0.208 | 2.508 | 0.013 |
| U1 to FH | −0.049 | 0.014 | −0.298 | −3.550 | <0.001 |
| mandibular plane | −0.034 | 0.016 | −0.188 | −2.171 | 0.032 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ishii, T.; Koizumi, S.; Yamaguchi, T. Factors Associated with the Proximity of the Incisive Canal to the Maxillary Central Incisor. Appl. Sci. 2023, 13, 6899. https://doi.org/10.3390/app13126899
Ishii T, Koizumi S, Yamaguchi T. Factors Associated with the Proximity of the Incisive Canal to the Maxillary Central Incisor. Applied Sciences. 2023; 13(12):6899. https://doi.org/10.3390/app13126899
Chicago/Turabian StyleIshii, Toshiyuki, So Koizumi, and Tetsutaro Yamaguchi. 2023. "Factors Associated with the Proximity of the Incisive Canal to the Maxillary Central Incisor" Applied Sciences 13, no. 12: 6899. https://doi.org/10.3390/app13126899






