Clinical Comparative Study for Validation of Digital Impression Reliability with the Gypsum Check: A Simple and Fast Way to Evaluate the Trueness and Accuracy of Implant-Supported Rehabilitation
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Description
- A treatment plan which includes rehabilitation with at least two adjacent implants;
- The clinical indication of implant-supported FDP;
- Good periodontal conditions;
- Stable occlusion;
- No comorbidities that contraindicated implant surgery;
- Reduced gag reflex.
- Clinical contraindications to implant treatment;
- Implants that exceeded the maximum mutual inclination allowed by manufacturers;
- Presence of parafunction or periodontal disease;
- Poor oral hygiene;
- Increased gag reflex;
- Presence of comorbidities that contraindicated implant surgery.
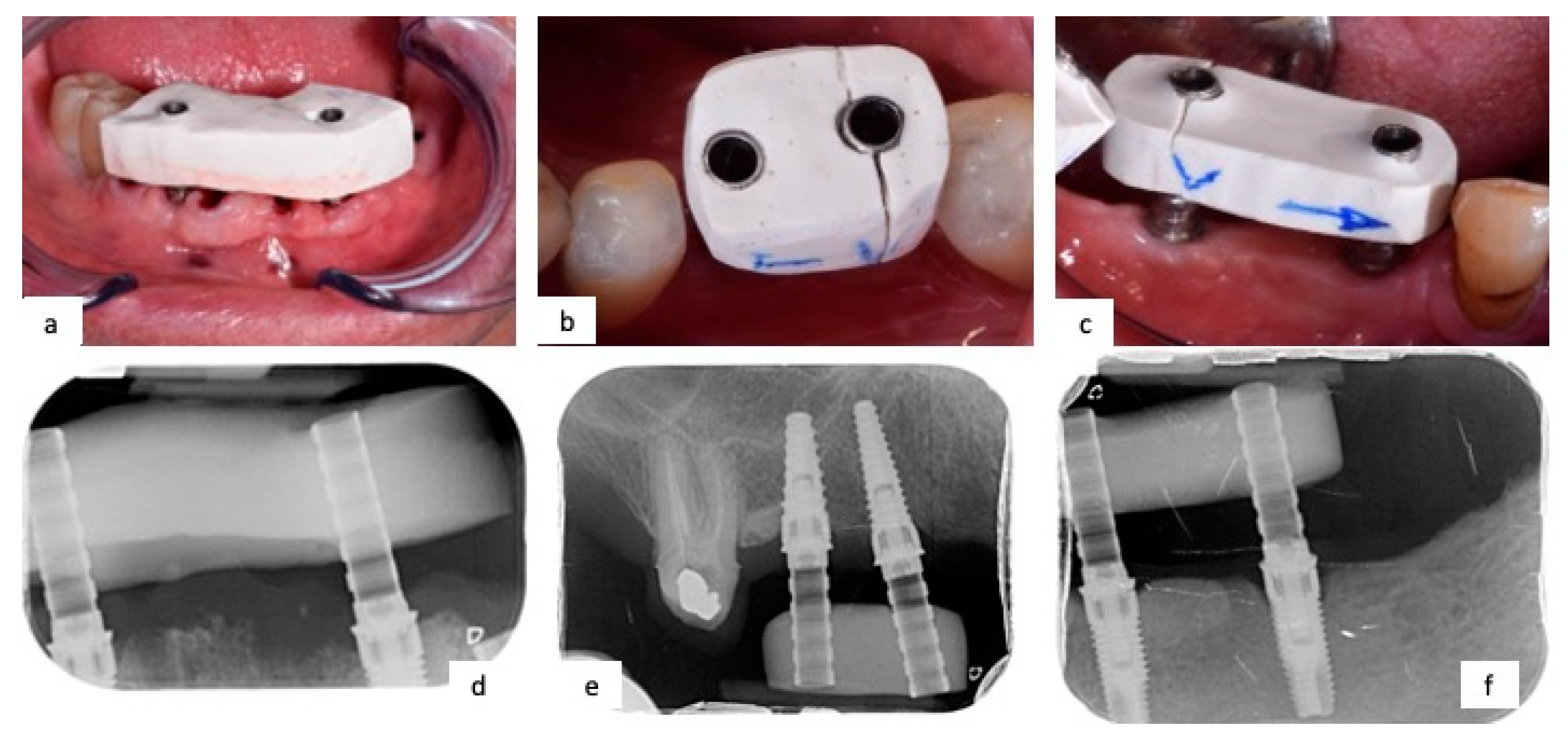
2.2. Workflow and Operating Protocol Description
- Initial evaluation: compilation of medical records with anamnesis, orthopantomography, and eventual intraoral radiograph, and, when necessary, CBCT; impression taking using irreversible hydrocolloid impression material (Alginate—Kromopan LASCOD, Sesto Fiorentino, Italy); and analysis of the study models.
- Surgical time: after local anesthesia, a full-thickness flap was elevated, two adjacent implants were inserted according to the actual guidelines of the operating protocol, and the implant site was immediately closed with a cover screw.
- Exposure of the cover screw and substitution with the healing abutment after four months from the surgical time;
- Definitive impression;
- Positioning of provisional PMMA composed of 3 elements (one single pontic);
- Definitive impression.
- Custom tray fabrication after alginate impression, perforated to allow the unscrewing of transfers;
- Removal of the healing screw;
- Positioning of impression transfer coping at 30–35 N;
- Radiological check of correct insertion;
- Splinting of impression transfer coping with Duralay (Reliance Dental, Worth, IL, USA), an autopolymerizing polymethylmethacrylate (PMMA) resin;
- Clinicians took the conventional impression with a polyether (Impregum, 3M ESPE, Dental Products, St. Paul, MN, USA);
- After 6 min, impression transfer copings were unscrewed, and the custom impression tray was removed from the patients;
- Assessment of definitive impression taken;
- Extra-hard plaster cast was made with 4th-type gypsum (Fujirock Ep Classic, GC Corporation, Tokyo, Japan);
- Plaster cast digitalization using 3Shape D500 (Copenhagen, Denmark) laboratory scanner.
- Vivadent Optragate (Schaan, Liechtenstein) retractor was positioned;
- Healing screws were replaced by PEEK scanbodies;
- Optical impression was taken with Carestream 3600 (Rochester, New York, NY, USA);
- STL file was generated on CAD station and the digital cast was reconstructed.
2.3. Accuracy Analysis
2.4. Clinical Cases
2.5. Statistical Analysis
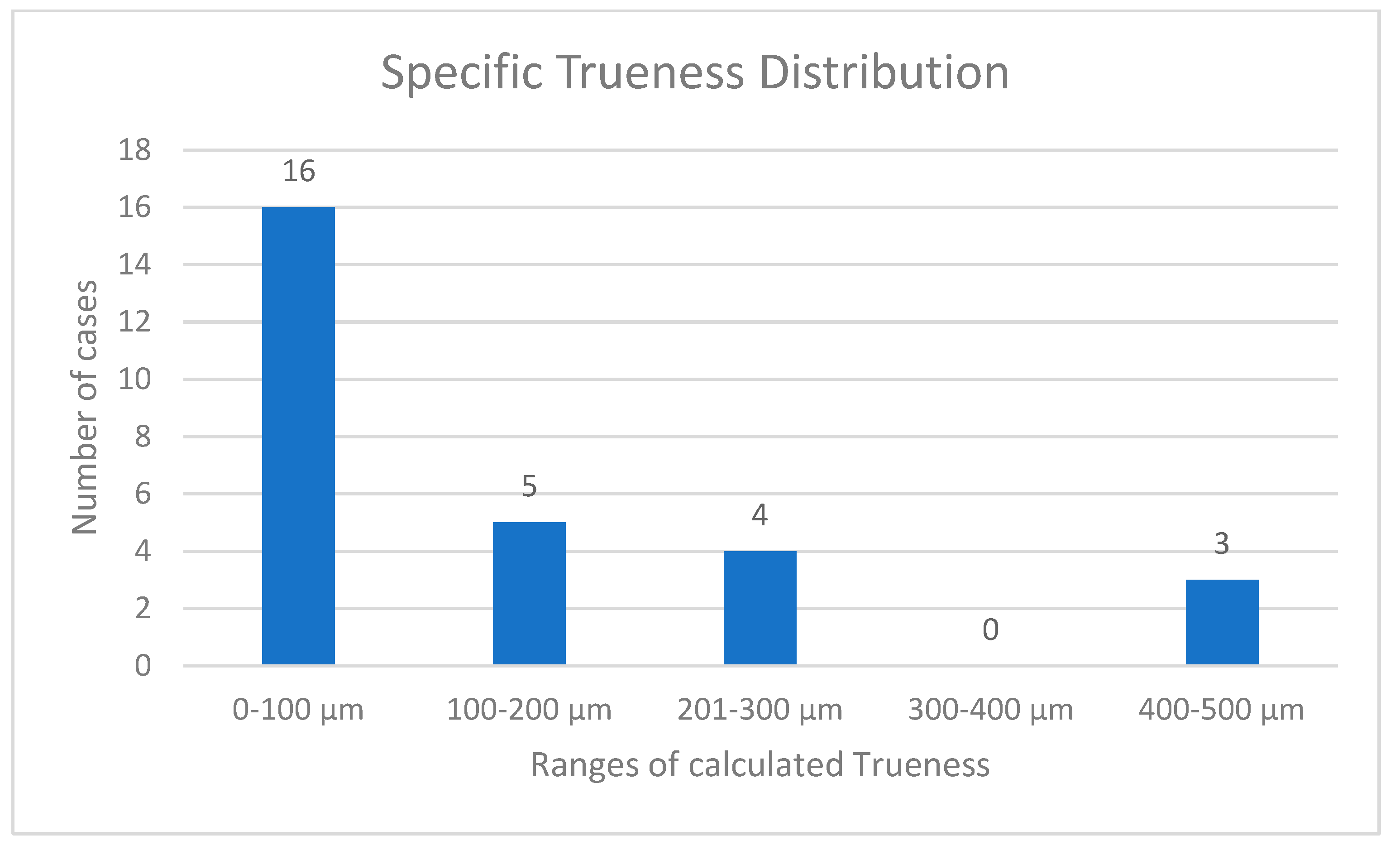
3. Results
4. Discussion
4.1. Accuracy Evaluation of Digital Impression
4.2. Comparison between Digital and Conventional Impressions
4.3. Comparison between Different Intraoral Scanners (IOS)
4.4. Limitations of Previous Studies
4.5. Clinical Considerations of Misfit
4.6. Clinical Comparative Studies Evaluation
4.7. Limitations and Recommendations for Future Research
5. Conclusions
- Despite the limitations of this pilot study, the authors suggest that the gypsum check screwed onto implant abutments is an effective method to quickly detect the Trueness and Accuracy values of digital impressions, considering, respectively, cut-off threshold values of 100 µm for Trueness and 98% for Accuracy percentage.
- Considering that the passive fit of the framework plays a central role in prosthetic rehabilitations which involve multiple implants, the authors propose 100 µm as a maximum clinical tolerance misfit value: at values over 100 µm of misfit, the impression could not be considered reliable because it does not allow the passive fit of future prosthetic frameworks.
- Further clinical studies on larger samples with many years of follow-up may confirm these considerations or propose a more accurate method.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Papadiochos, I.; Papadiochou, S.; Emmanouil, I. The Historical Evolution of Dental Impression Materials. J. Hist. Dent. 2017, 65, 79–89. [Google Scholar] [PubMed]
- Cervino, G.; Fiorillo, L.; Herford, A.S.; Laino, L.; Troiano, G.; Amoroso, G.; Crimi, S.; Matarese, M.; D’Amico, C.; Nastro Siniscalchi, E.; et al. Alginate Materials and Dental Impression Technique: A Current State of the Art and Application to Dental Practice. Mar. Drugs 2018, 17, 18. [Google Scholar] [CrossRef] [PubMed]
- Jayaraman, S.; Singh, B.P.; Ramanathan, B.; Pazhaniappan Pillai, M.; MacDonald, L.; Kirubakaran, R. Final-Impression Techniques and Materials for Making Complete and Removable Partial Dentures. Cochrane Database Syst. Rev. 2018, 4, CD012256. [Google Scholar] [CrossRef] [PubMed]
- Duret, F.; Preston, J.D. CAD/CAM Imaging in Dentistry. Curr. Opin. Dent. 1991, 1, 150–154. [Google Scholar] [PubMed]
- Mangano, F.G.; Hauschild, U.; Veronesi, G.; Imburgia, M.; Mangano, C.; Admakin, O. Trueness and Precision of 5 Intraoral Scanners in the Impressions of Single and Multiple Implants: A Comparative in Vitro Study. BMC Oral Health 2019, 19, 101. [Google Scholar] [CrossRef]
- Schepke, U.; Meijer, H.J.A.; Kerdijk, W.; Cune, M.S. Digital versus Analog Complete-Arch Impressions for Single-Unit Premolar Implant Crowns: Operating Time and Patient Preference. J. Prosthet. Dent. 2015, 114, 403–406.e1. [Google Scholar] [CrossRef]
- Rapone, B.; Palmisano, C.; Ferrara, E.; Di Venere, D.; Albanese, G.; Corsalini, M. The Accuracy of Three Intraoral Scanners in the Oral Environment with and without Saliva: A Comparative Study. Appl. Sci. 2020, 10, 7762. [Google Scholar] [CrossRef]
- ISO 5725-1:1994; Accuracy (Trueness and Precision) of Measurement Methods and Results—Part 1: General Principles and Definitions. ISO: Geneva, Switzerland, 1994. Available online: https://www.iso.org/standard/11833.html (accessed on 12 January 2023).
- Amin, S.; Weber, H.P.; Finkelman, M.; El Rafie, K.; Kudara, Y.; Papaspyridakos, P. Digital vs. Conventional Full-Arch Implant Impressions: A Comparative Study. Clin. Oral Impl. Res. 2017, 28, 1360–1367. [Google Scholar] [CrossRef]
- Alsharbaty, M.H.M.; Alikhasi, M.; Zarrati, S.; Shamshiri, A.R. A Clinical Comparative Study of 3-Dimensional Accuracy between Digital and Conventional Implant Impression Techniques. J. Prosthodont. 2019, 28, e902–e908. [Google Scholar] [CrossRef]
- Katsoulis, J.; Takeichi, T.; Sol Gaviria, A.; Peter, L.; Katsoulis, K. Misfit of Implant Prostheses and Its Impact on Clinical Outcomes. Definition, Assessment and a Systematic Review of the Literature. Eur. J. Oral Implantol. 2017, 10 (Suppl. S1), 121–138. [Google Scholar]
- Manzella, C.; Bignardi, C.; Burello, V.; Carossa, S.; Schierano, G. Method to Improve Passive Fit of Frameworks on Implant-Supported Prostheses: An in Vitro Study. J. Prosthet. Dent. 2016, 116, 52–58. [Google Scholar] [CrossRef]
- Wulfman, C.; Naveau, A.; Rignon-Bret, C. Digital Scanning for Complete-Arch Implant-Supported Restorations: A Systematic Review. J. Prosthet. Dent. 2020, 124, 161–167. [Google Scholar] [CrossRef]
- Gedrimiene, A.; Adaskevicius, R.; Rutkunas, V. Accuracy of Digital and Conventional Dental Implant Impressions for Fixed Partial Dentures: A Comparative Clinical Study. J. Adv. Prosthodont. 2019, 11, 271. [Google Scholar] [CrossRef]
- Ender, A.; Mehl, A. Accuracy of Complete-Arch Dental Impressions: A New Method of Measuring Trueness and Precision. J. Prosthet. Dent. 2013, 109, 121–128. [Google Scholar] [CrossRef]
- Ender, A.; Mehl, A. In-Vitro Evaluation of the Accuracy of Conventional and Digital Methods of Obtaining Full-Arch Dental Impressions. Quintessence Int. 2015, 46, 9–17. [Google Scholar] [CrossRef]
- Menini, M.; Setti, P.; Pera, F.; Pera, P.; Pesce, P. Accuracy of Multi-Unit Implant Impression: Traditional Techniques versus a Digital Procedure. Clin. Oral Investig. 2018, 22, 1253–1262. [Google Scholar] [CrossRef]
- Hayama, H.; Fueki, K.; Wadachi, J.; Wakabayashi, N. Trueness and Precision of Digital Impressions Obtained Using an Intraoral Scanner with Different Head Size in the Partially Edentulous Mandible. J. Prosthodont. Res. 2018, 62, 347–352. [Google Scholar] [CrossRef]
- Nedelcu, R.; Olsson, P.; Nyström, I.; Rydén, J.; Thor, A. Accuracy and Precision of 3 Intraoral Scanners and Accuracy of Conventional Impressions: A Novel in Vivo Analysis Method. J. Dent. 2018, 69, 110–118. [Google Scholar] [CrossRef]
- Schmidt, A.; Billig, J.-W.; Schlenz, M.A.; Wöstmann, B. Do Different Methods of Digital Data Analysis Lead to Different Results? Int. J. Comput. Dent. 2021, 24, 157–164. [Google Scholar]
- Revilla-León, M.; Jiang, P.; Sadeghpour, M.; Piedra-Cascón, W.; Zandinejad, A.; Özcan, M.; Krishnamurthy, V.R. Intraoral Digital Scans—Part 1: Influence of Ambient Scanning Light Conditions on the Accuracy (Trueness and Precision) of Different Intraoral Scanners. J. Prosthet. Dent. 2020, 124, 372–378. [Google Scholar] [CrossRef]
- Son, K.; Jin, M.-U.; Lee, K.-B. Feasibility of Using an Intraoral Scanner for a Complete-Arch Digital Scan, Part 2: A Comparison of Scan Strategies. J. Prosthet. Dent. 2021, 129, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Mennito, A.S.; Evans, Z.P.; Lauer, A.W.; Patel, R.B.; Ludlow, M.E.; Renne, W.G. Evaluation of the Effect Scan Pattern Has on the Trueness and Precision of Six Intraoral Digital Impression Systems. J. Esthet. Restor. Dent. 2018, 30, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Rotar, R.N.; Faur, A.B.; Pop, D.; Jivanescu, A. Scanning Distance Influence on the Intraoral Scanning Accuracy—An In Vitro Study. Materials 2022, 15, 3061. [Google Scholar] [CrossRef] [PubMed]
- Imburgia, M.; Logozzo, S.; Hauschild, U.; Veronesi, G.; Mangano, C.; Mangano, F.G. Accuracy of Four Intraoral Scanners in Oral Implantology: A Comparative in Vitro Study. BMC Oral Health 2017, 17, 92. [Google Scholar] [CrossRef] [PubMed]
- Nulty, A.B. A Comparison of Full Arch Trueness and Precision of Nine Intra-Oral Digital Scanners and Four Lab Digital Scanners. Dent. J. 2021, 9, 75. [Google Scholar] [CrossRef]
- Di Fiore, A.; Meneghello, R.; Graiff, L.; Savio, G.; Vigolo, P.; Monaco, C.; Stellini, E. Full Arch Digital Scanning Systems Performances for Implant-Supported Fixed Dental Prostheses: A Comparative Study of 8 Intraoral Scanners. J. Prosthodont. Res. 2019, 63, 396–403. [Google Scholar] [CrossRef]
- Chochlidakis, K.M.; Papaspyridakos, P.; Geminiani, A.; Chen, C.-J.; Feng, I.J.; Ercoli, C. Digital versus Conventional Impressions for Fixed Prosthodontics: A Systematic Review and Meta-Analysis. J. Prosthet. Dent. 2016, 116, 184–190.e12. [Google Scholar] [CrossRef]
- Lee, J.-H.; Bae, J.-H.; Lee, S.Y. Trueness of Digital Implant Impressions Based on Implant Angulation and Scan Body Materials. Sci. Rep. 2021, 11, 21892. [Google Scholar] [CrossRef]
- Miyoshi, K.; Tanaka, S.; Yokoyama, S.; Sanda, M.; Baba, K. Effects of Different Types of Intraoral Scanners and Scanning Ranges on the Precision of Digital Implant Impressions in Edentulous Maxilla: An in Vitro Study. Clin. Oral Implants Res. 2020, 31, 74–83. [Google Scholar] [CrossRef]
- Roig, E.; Garza, L.C.; Álvarez-Maldonado, N.; Maia, P.; Costa, S.; Roig, M.; Espona, J. In Vitro Comparison of the Accuracy of Four Intraoral Scanners and Three Conventional Impression Methods for Two Neighboring Implants. PLoS ONE 2020, 15, e0228266. [Google Scholar] [CrossRef]
- Huang, R.; Liu, Y.; Huang, B.; Zhang, C.; Chen, Z.; Li, Z. Improved Scanning Accuracy with Newly Designed Scan Bodies: An in Vitro Study Comparing Digital versus Conventional Impression Techniques for Complete-arch Implant Rehabilitation. Clin. Oral Implants Res. 2020, 31, 625–633. [Google Scholar] [CrossRef]
- Andriessen, F.S.; Rijkens, D.R.; van der Meer, W.J.; Wismeijer, D.W. Applicability and Accuracy of an Intraoral Scanner for Scanning Multiple Implants in Edentulous Mandibles: A Pilot Study. J. Prosthet. Dent. 2014, 111, 186–194. [Google Scholar] [CrossRef]
- Orejas-Perez, J.; Gimenez-Gonzalez, B.; Ortiz-Collado, I.; Thuissard, I.J.; Santamaria-Laorden, A. In Vivo Complete-Arch Implant Digital Impressions: Comparison of the Precision of Three Optical Impression Systems. Int. J. Environ. Res. Public Health 2022, 19, 4300. [Google Scholar] [CrossRef]
- De Sousa, S.A.; De Arruda Nobilo, M.A.; Henriques, G.E.P.; Mesquita, M.F. Passive Fit of Frameworks in Titanium and Palladium-Silver Alloy Submitted the Laser Welding: PASSIVE FIT OF IMPLANT FRAMEWORKS. J. Oral Rehabil. 2008, 35, 123–127. [Google Scholar] [CrossRef]
- Alhashim, A.; Flinton, R.J. Dental Gypsum Verification Jig to Verify Implant Positions: A Clinical Report. J. Oral Implantol. 2014, 40, 495–499. [Google Scholar] [CrossRef]
- Plachý, T.; Tesárek, P.; Padevět, P.; Polak, M. Determination of Young’ s Modulus of Gypsum Blocks Using Two Different Experimental Methods. In Recent Advances in Applied and Theoretical Mechanics, Proceedings of 5th WSEAS International Conference on Applied and Theoretical Mechanics, Puerto De La Cruz, Spain, 14–16 December 2009; Bulucea, C., Ed.; WSEAS Press: Athens, Greece, 2009. [Google Scholar]
- Najeeb, S.; Zafar, M.S.; Khurshid, Z.; Siddiqui, F. Applications of Polyetheretherketone (PEEK) in Oral Implantology and Prosthodontics. J. Prosthodont. Res. 2016, 60, 12–19. [Google Scholar] [CrossRef]
- Liczmanski, K.; Stamm, T.; Sauerland, C.; Blanck-Lubarsch, M. Accuracy of Intraoral Scans in the Mixed Dentition: A Prospective Non-Randomized Comparative Clinical Trial. Head Face Med. 2020, 16, 11. [Google Scholar] [CrossRef]
- Gan, N.; Xiong, Y.; Jiao, T. Accuracy of Intraoral Digital Impressions for Whole Upper Jaws, Including Full Dentitions and Palatal Soft Tissues. PLoS ONE 2016, 11, e0158800. [Google Scholar] [CrossRef]
- Rhee, Y.-K.; Huh, Y.-H.; Cho, L.-R.; Park, C.-J. Comparison of Intraoral Scanning and Conventional Impression Techniques Using 3-Dimensional Superimposition. J. Adv. Prosthodont. 2015, 7, 460–467. [Google Scholar] [CrossRef]
- Giachetti, L.; Sarti, C.; Cinelli, F.; Russo, D.S. Accuracy of Digital Impressions in Fixed Prosthodontics: A Systematic Review of Clinical Studies. Int. J. Prosthodont. 2020, 33, 192–201. [Google Scholar] [CrossRef]
- Schlenz, M.A.; Schubert, V.; Schmidt, A.; Wöstmann, B.; Ruf, S.; Klaus, K. Digital versus Conventional Impression Taking Focusing on Interdental Areas: A Clinical Trial. Int. J. Environ. Res. Public Health 2020, 17, 4725. [Google Scholar] [CrossRef] [PubMed]
- Atieh, M.A.; Ritter, A.V.; Ko, C.-C.; Duqum, I. Accuracy Evaluation of Intraoral Optical Impressions: A Clinical Study Using a Reference Appliance. J. Prosthet. Dent. 2017, 118, 400–405. [Google Scholar] [CrossRef] [PubMed]

| Patient N. | Sex | Age | Localization (Sextant) |
|---|---|---|---|
| 1 | M | 72 | V |
| 2 | M | 69 | VI |
| 3 | M | 74 | IV |
| 4 | M | 69 | III |
| 5 | M | 62 | III |
| 6 | F | 81 | III |
| 7 | M | 71 | VI |
| 8 | M | 72 | IV |
| 9 | M | 69 | VI |
| 10 | F | 75 | I |
| 11 | F | 73 | III |
| 12 | F | 80 | III |
| 13 | M | 58 | III |
| 14 | F | 73 | II |
| Patient | DI1 (mm) | DI2 (mm) | RV (mm) | ST1 (µm) | ST 2 (µm) | Precision (µm) |
|---|---|---|---|---|---|---|
| 1 | 19.517 | 19.560 | 19.520 | 3.33 | 40.00 | 21.67 |
| 2 | 5.770 | 5.747 | 5.730 | 40.00 | 16.67 | 11.67 |
| 3 | 6.840 | 6.793 | 6.890 | 50.00 | 96.67 | 23.33 |
| 4 | 13.950 | 13.900 | 13.990 | 40.00 | 90.00 | 25.00 |
| 5 | 13.300 | 13.020 | 13.017 | 283.33 | 3.33 | 140.00 |
| 6 | 18.323 | 18.323 | 18.770 | 446.67 | 446.67 | 0.00 |
| 7 | 6.607 | 6.660 | 6.847 | 240.00 | 186.67 | 26.67 |
| 8 | 14.127 | 13.970 | 13.837 | 290.00 | 133.33 | 78.33 |
| 9 | 7.567 | 7.630 | 7.767 | 200.00 | 136.67 | 31.67 |
| 10 | 9.673 | 9.683 | 9.607 | 66.67 | 76.67 | 5.00 |
| 11 | 20.927 | 21.130 | 20.637 | 290.00 | 493.33 | 101.67 |
| 12 | 9.313 | 9.427 | 9.437 | 123.33 | 10.00 | 56.67 |
| 13 | 13.110 | 13.120 | 13.117 | 6.67 | 3.33 | 5.00 |
| 14 | 11.510 | 11.570 | 11.547 | 36.67 | 23.33 | 30.00 |
| Mean | 151.19 ± 37.23 µm | 125.47 ± 41.90 µm | 39.76 ± 10.89 µm |
| Patient | Accuracy 1 (µm) | Accuracy 2 (µm) | Dimensional Error | Accuracy % |
|---|---|---|---|---|
| 1 | 3.33 ± 21.67 | 40.00 ± 21.67 | 0.02 | 99.98 |
| 2 | 40.00 ± 11.67 | 16.67 ± 11.67 | 0.70 | 99.30 |
| 3 | 50.00 ± 23.33 | 96.67 ± 23.33 | 0.73 | 99.27 |
| 4 | 40.00 ± 25.00 | 90.00 ± 25.00 | 0.29 | 99.71 |
| 5 | 283.33 ± 140.00 | 3.33 ± 140.00 | 2.18 | 97.82 |
| 6 | 446.67 ± 0 | 446.67 ± 0 | 2.38 | 97.62 |
| 7 | 240.00 ± 26.67 | 186.67 ± 26.67 | 3.50 | 96.50 |
| 8 | 290.00 ± 78.33 | 133.33 ± 78.33 | 2.10 | 97.90 |
| 9 | 200.00 ± 31.67 | 136.67 | 2.58 | 97.42 |
| 10 | 66.67 ± 5.00 | 76.67 ± 5.00 | 0.70 | 99.30 |
| 11 | 290.00 ± 101.67 | 493.33 ± 101.67 | 1.41 | 98.59 |
| 12 | 123.33 ± 56.67 | 10.00 ± 56.67 | 1.31 | 98.69 |
| 13 | 6.67 ± 5.00 | 3.33 ± 5.00 | 0.05 | 99.95 |
| 14 | 36.67 ± 30.00 | 23.33 ± 30.00 | 0.32 | 99.68 |
| Mean | 151.19 ± 39.76 | 125.48 ± 39.76 | 1.3 | 98.70 |
| Patient N. | First Digital Impression | Second Digital Impression | Conventional Impression |
|---|---|---|---|
| 1 | Intact | Intact | Intact |
| 2 | Intact | Intact | Intact |
| 3 | Intact | Intact | Intact |
| 4 | Intact | Intact | Intact |
| 5 | Fractured | Intact | Intact |
| 6 | Fractured | Fractured | Intact |
| 7 | Fractured | Fractured | Intact |
| 8 | Fractured | Intact | Intact |
| 9 | Fractured | Fractured | Intact |
| 10 | Intact | Intact | Intact |
| 11 | Fractured | Fractured | Intact |
| 12 | Intact | Intact | Intact |
| 13 | Intact | Intact | Intact |
| 14 | Intact | Intact | Intact |
| Patient N. | Specific Trueness 1 | First Digital Impression | Specific Trueness 2 | Second Digital Impression | Accuracy % |
|---|---|---|---|---|---|
| 1 | 3.33 | Intact | 40.00 | Intact | 99.98 |
| 2 | 40.00 | Intact | 16.67 | Intact | 99.30 |
| 3 | 50.00 | Intact | 96.67 | Intact | 99.27 |
| 4 | 40.00 | Intact | 90.00 | Intact | 99.71 |
| 5 | 283.33 | Fractured | 3.33 | Intact | 97.82 |
| 6 | 446.67 | Fractured | 446.67 | Fractured | 97.62 |
| 7 | 240.00 | Fractured | 186.67 | Fractured | 96.50 |
| 8 | 290.00 | Fractured | 133.33 | Intact | 97.90 |
| 9 | 200.00 | Fractured | 136.67 | Fractured | 97.42 |
| 10 | 66.67 | Intact | 76.67 | Intact | 99.30 |
| 11 | 290.00 | Fractured | 493.33 | Fractured | 98.59 |
| 12 | 123.33 | Intact | 10.00 | Intact | 98.69 |
| 13 | 6.67 | Intact | 3.33 | Intact | 99.95 |
| 14 | 36.67 | Intact | 23.33 | Intact | 99.68 |
| Independent Variable | Gypsum Intact | Gypsum Fractured | p < 0.05 |
|---|---|---|---|
| Specific Trueness of first Digital Impression | p = 0.001 | ||
| <100 µm | 7 | 0 | |
| >100 µm | 1 | 6 | |
| Specific Trueness of second Digital Impression | p = 0.001 | ||
| <100 µm | 9 | 0 | |
| >100 µm | 1 | 4 | |
| Accuracy | p = 0.001 | ||
| <98% | 0 | 5 | |
| >98% | 8 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barile, G.; de Rosa, G.; Papadia, P.; Muci, G.; Capodiferro, S.; Corsalini, M. Clinical Comparative Study for Validation of Digital Impression Reliability with the Gypsum Check: A Simple and Fast Way to Evaluate the Trueness and Accuracy of Implant-Supported Rehabilitation. Appl. Sci. 2023, 13, 7358. https://doi.org/10.3390/app13137358
Barile G, de Rosa G, Papadia P, Muci G, Capodiferro S, Corsalini M. Clinical Comparative Study for Validation of Digital Impression Reliability with the Gypsum Check: A Simple and Fast Way to Evaluate the Trueness and Accuracy of Implant-Supported Rehabilitation. Applied Sciences. 2023; 13(13):7358. https://doi.org/10.3390/app13137358
Chicago/Turabian StyleBarile, Giuseppe, Giovanni de Rosa, Paride Papadia, Giovannino Muci, Saverio Capodiferro, and Massimo Corsalini. 2023. "Clinical Comparative Study for Validation of Digital Impression Reliability with the Gypsum Check: A Simple and Fast Way to Evaluate the Trueness and Accuracy of Implant-Supported Rehabilitation" Applied Sciences 13, no. 13: 7358. https://doi.org/10.3390/app13137358
APA StyleBarile, G., de Rosa, G., Papadia, P., Muci, G., Capodiferro, S., & Corsalini, M. (2023). Clinical Comparative Study for Validation of Digital Impression Reliability with the Gypsum Check: A Simple and Fast Way to Evaluate the Trueness and Accuracy of Implant-Supported Rehabilitation. Applied Sciences, 13(13), 7358. https://doi.org/10.3390/app13137358







