Toward Patient-Centric Healthcare Systems: Key Requirements and Framework for Personal Health Records Based on Blockchain Technology
Abstract
1. Introduction
Motivation
- Data ownership: to ensure patients own and control their data;
- Access control: to allow patients to grant, revoke, or deny access to their data to other healthcare service providers or network researchers;
- Auditability: to allow patients to rigorously know how their data are being used, giving them authority to revoke access to anyone who has been found to be in violation.
- It proposes a solution for personal health records based on blockchain to give patients the power to own and benefit from their data.
- It introduces Hyperledger Fabric to achieve access control; govern identities for peers and users; and provide user authentication, credential validation, signature generation, and verification.
- It designs and develops a working prototype based on the defined requirements.
- It engages stakeholders from the industry to understand the real needs and to identify the requirements for PHRs.
- It evaluates the functionality of the system’s performance using the Hyperledger Caliper tool.
2. Blockchain Technology Overview
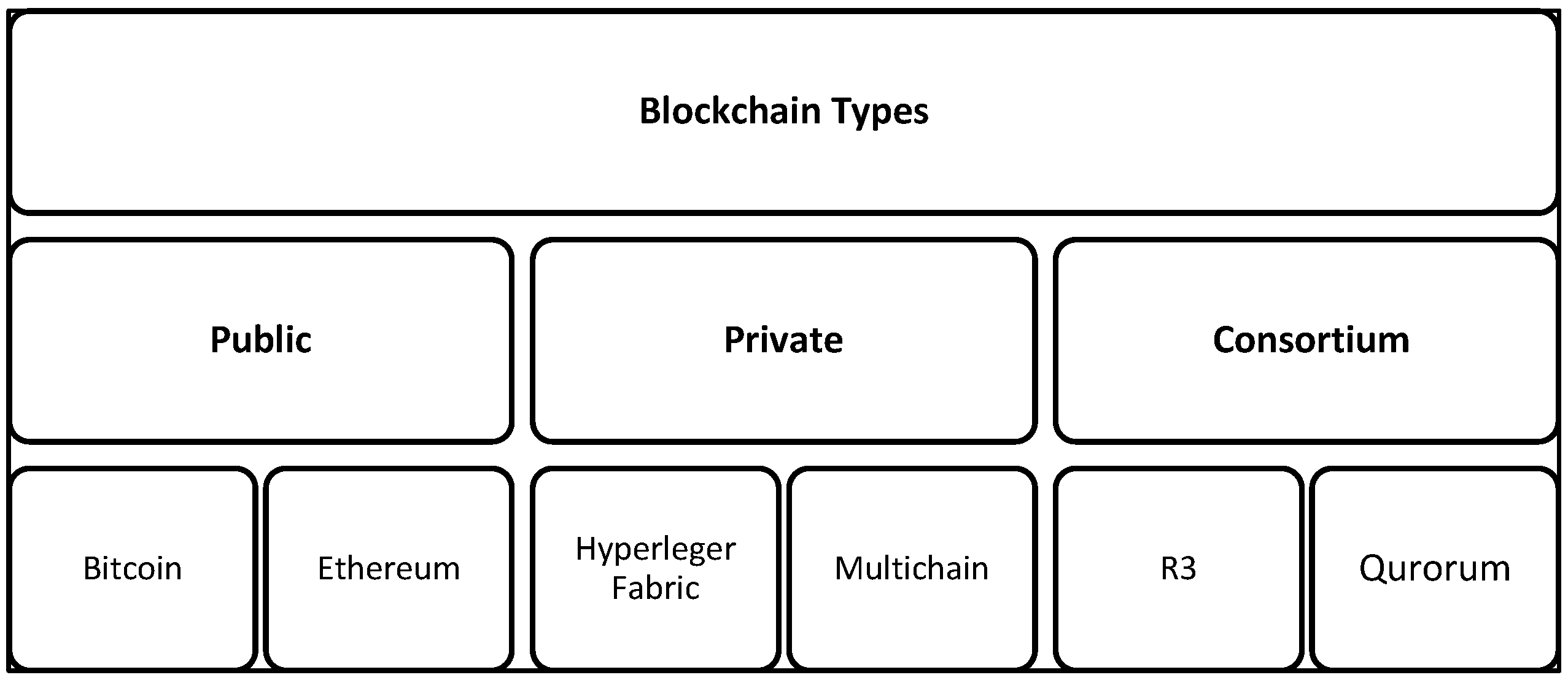
2.1. Blockchain Types
- Public blockchain
- Private blockchain
- Consortium blockchain
2.2. Hyperledger Fabric
- It is an open-source framework that permits work with open, widespread programming languages;
- It allows for the creation of private blockchains, which are crucial for supporting sensitive data;
- It does not require a mining process;
- It establishes a decentralized trust network of known participants instead of a public network of anonymous participants.
3. Related Work
3.1. Access Control and Data Ownership
3.2. Health Records and Patient Incentives
3.3. Health Records and Stakeholder Engagement
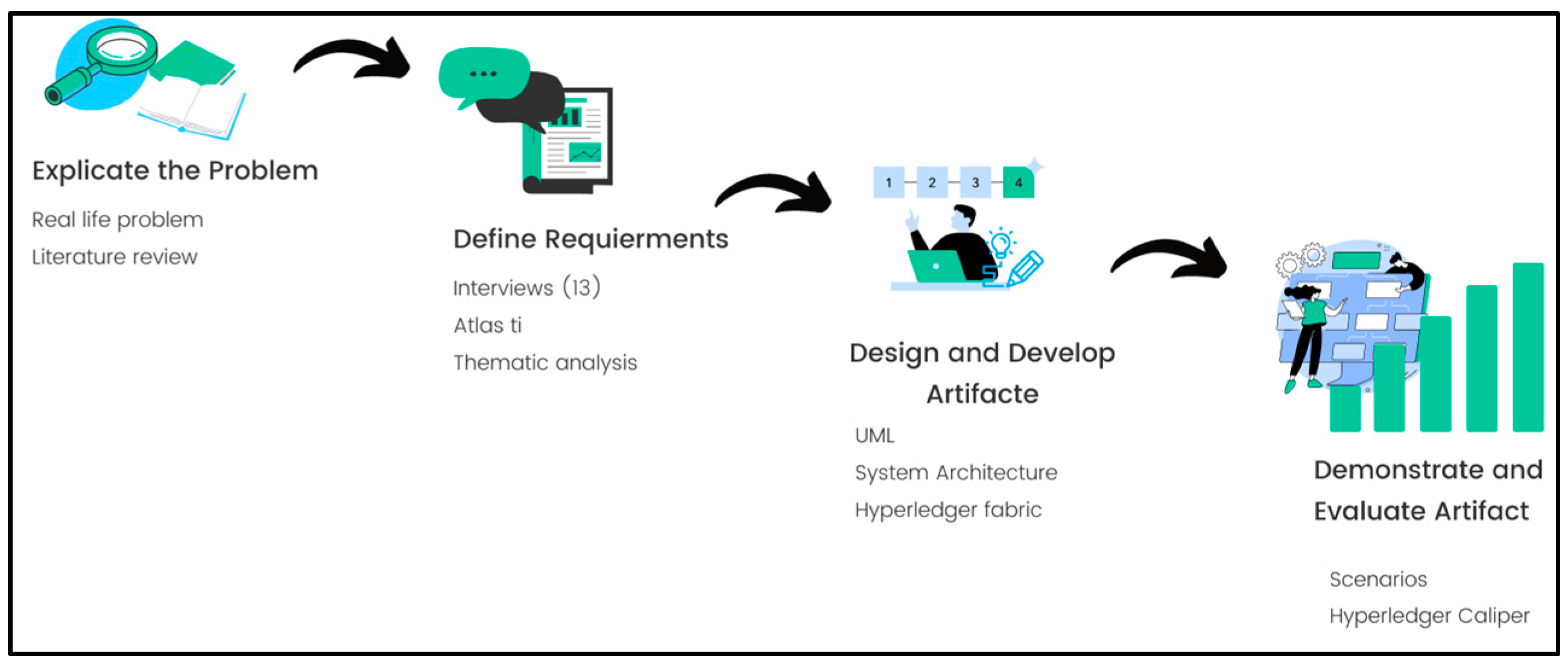
4. Methodology
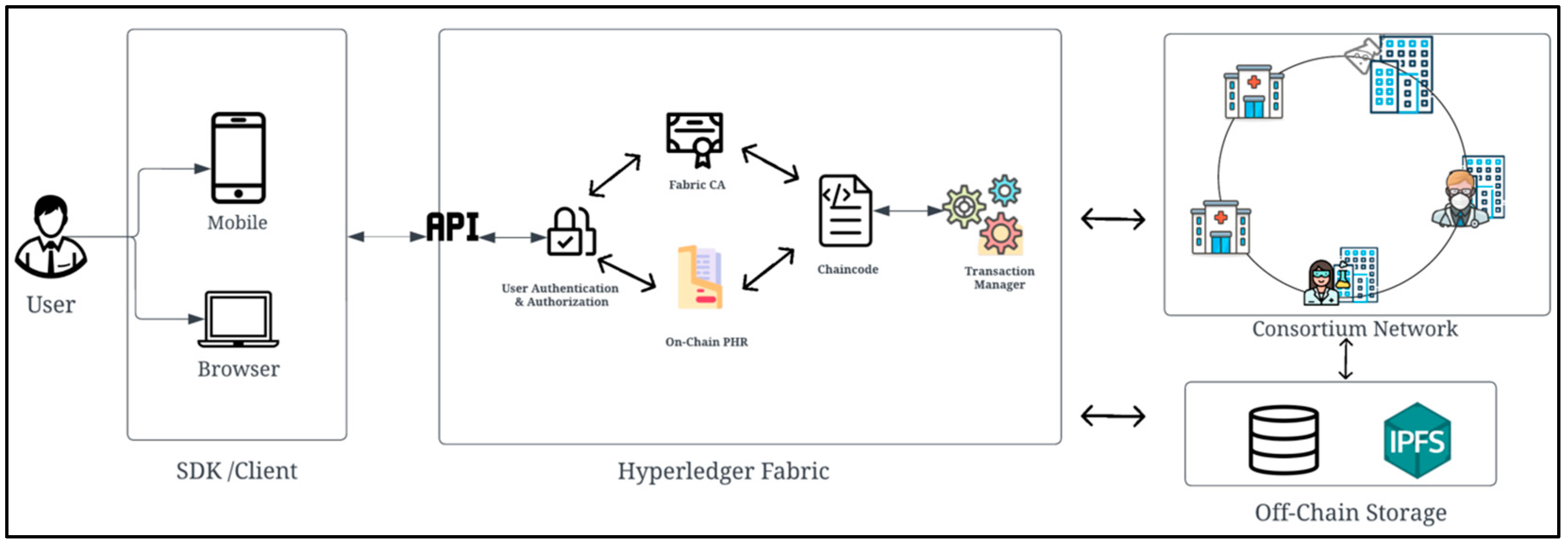
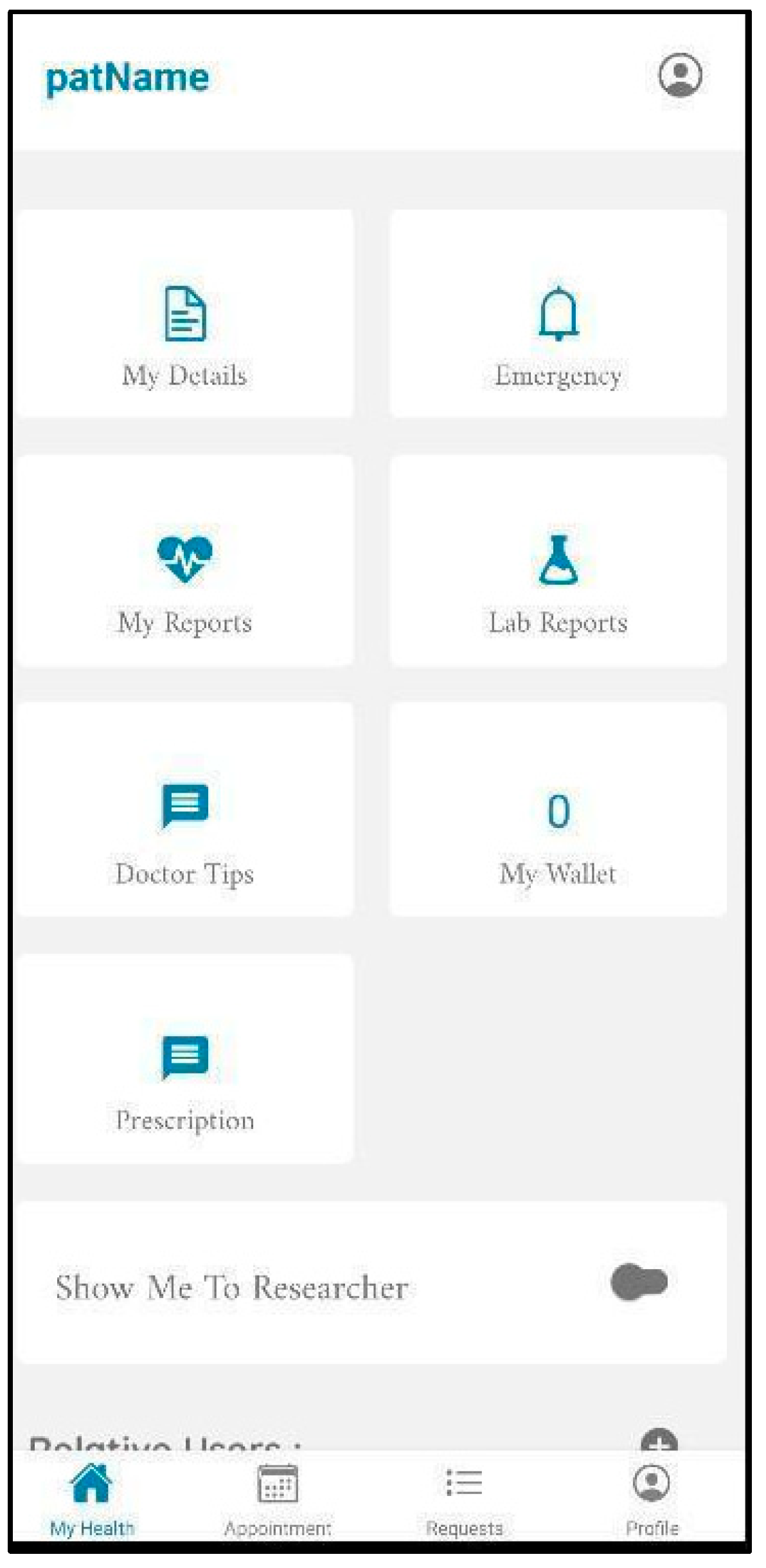
- Web and mobile applications: a frontend web application for administrators, healthcare centers, and physicians and mobile apps for patients;
- Node API server: a RESTful API (application programming interface) that uses HTTP requests to GET, PUT, POST, and DELETE data to the blockchain. It enables external components to access the blockchain;
- Hyperledger Fabric network: a blockchain backend platform;
- Interplanetary file system (IPFS): a peer-to-peer decentralized storage service that stores vast PDF files such as X-rays with the proper security access, which reduces the load on the blockchain and enhances performance [51].
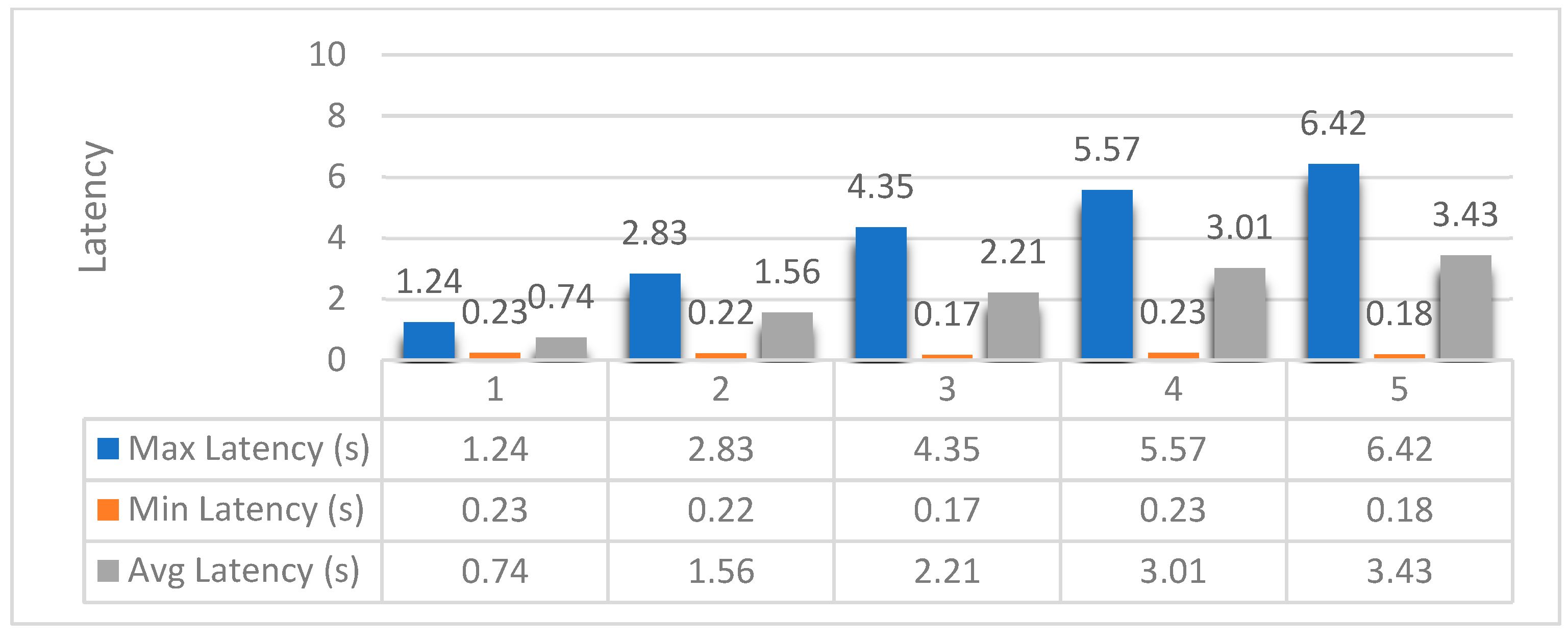
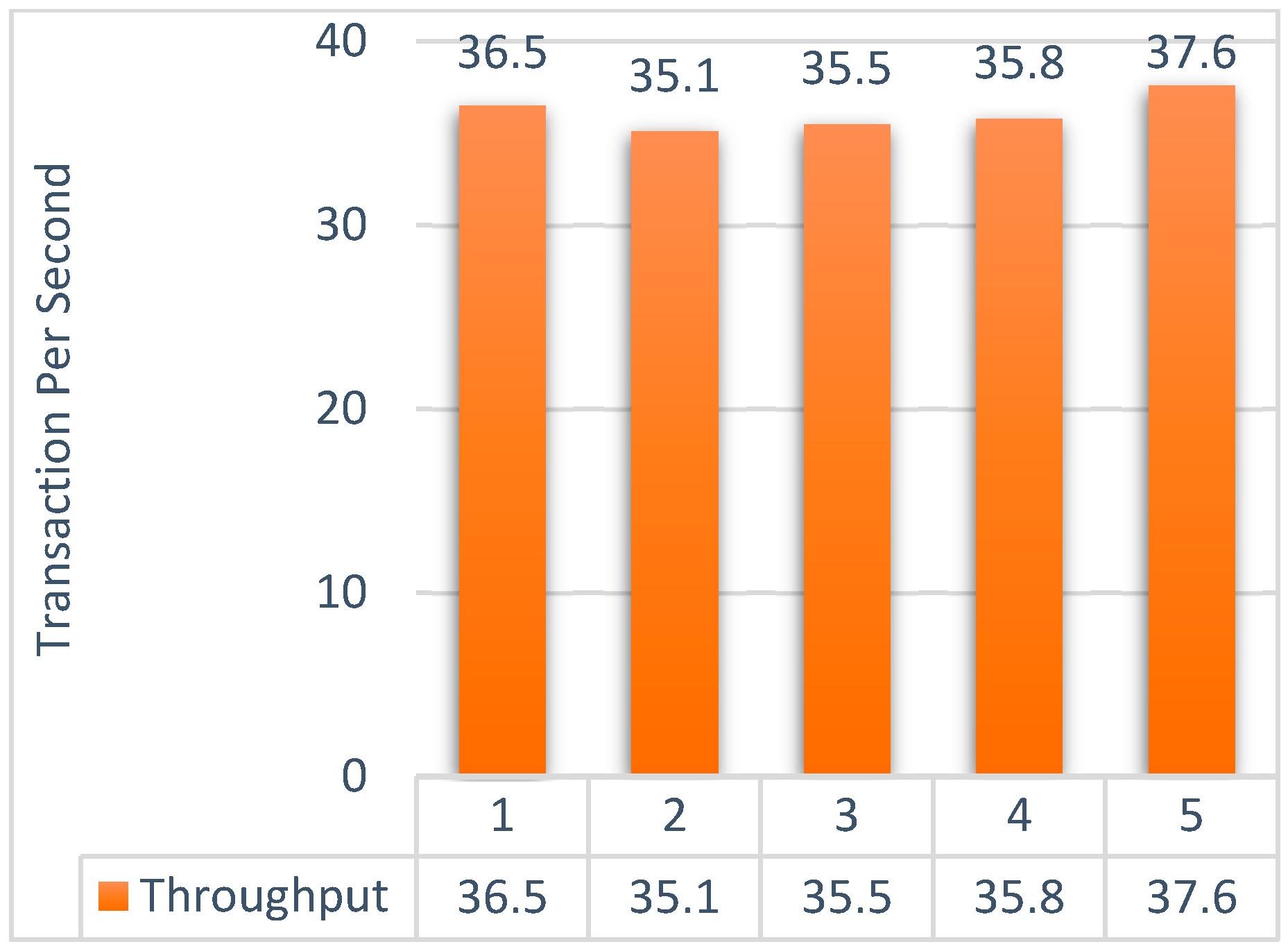
- Transaction throughput: number of successful transactions per second (TPS);
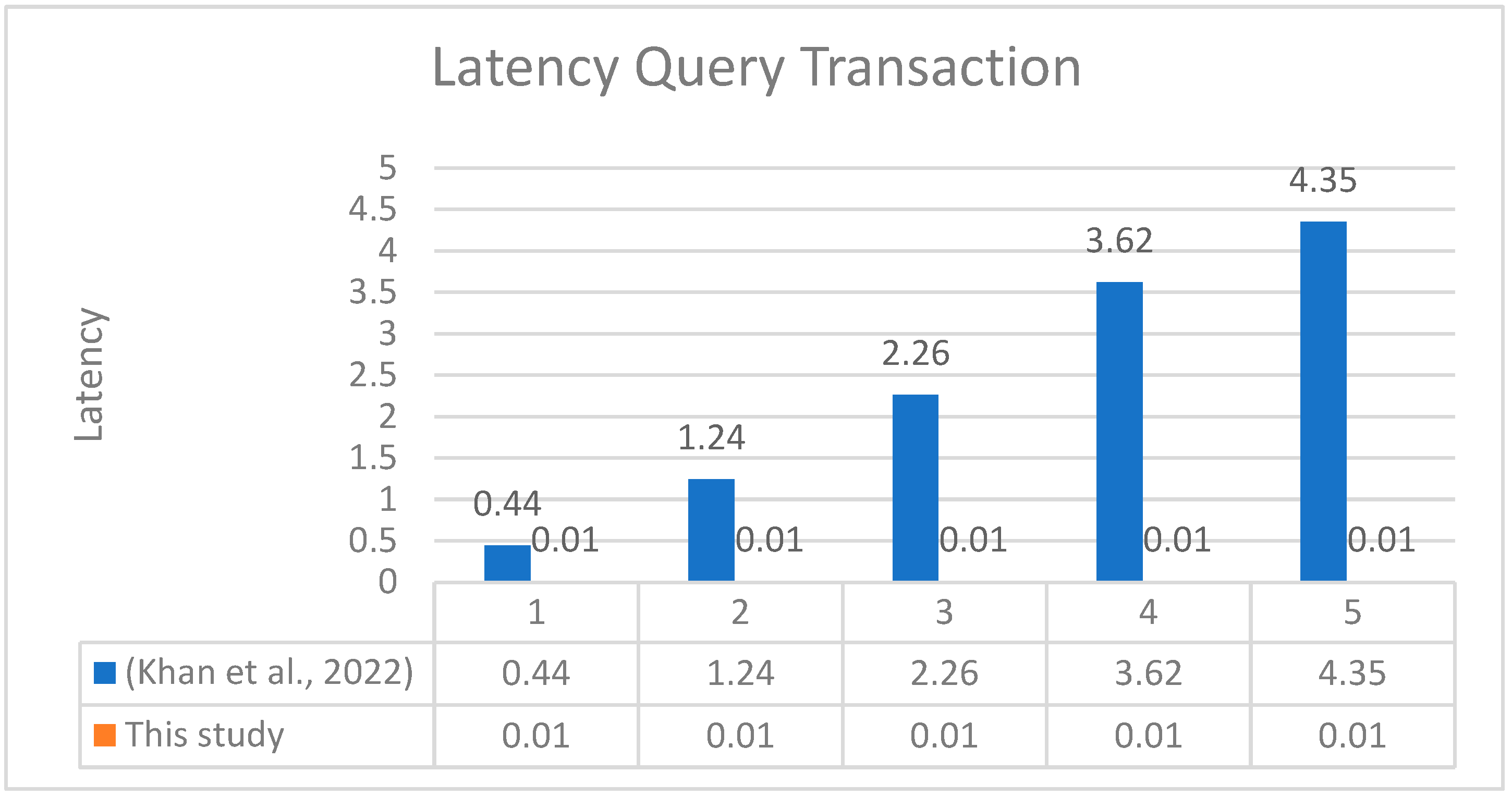
- Transaction latency: amount of time for transaction initialization and actual execution (i.e., response time);
- Success rate: number of successful transactions overall.
5. Results and Discussion
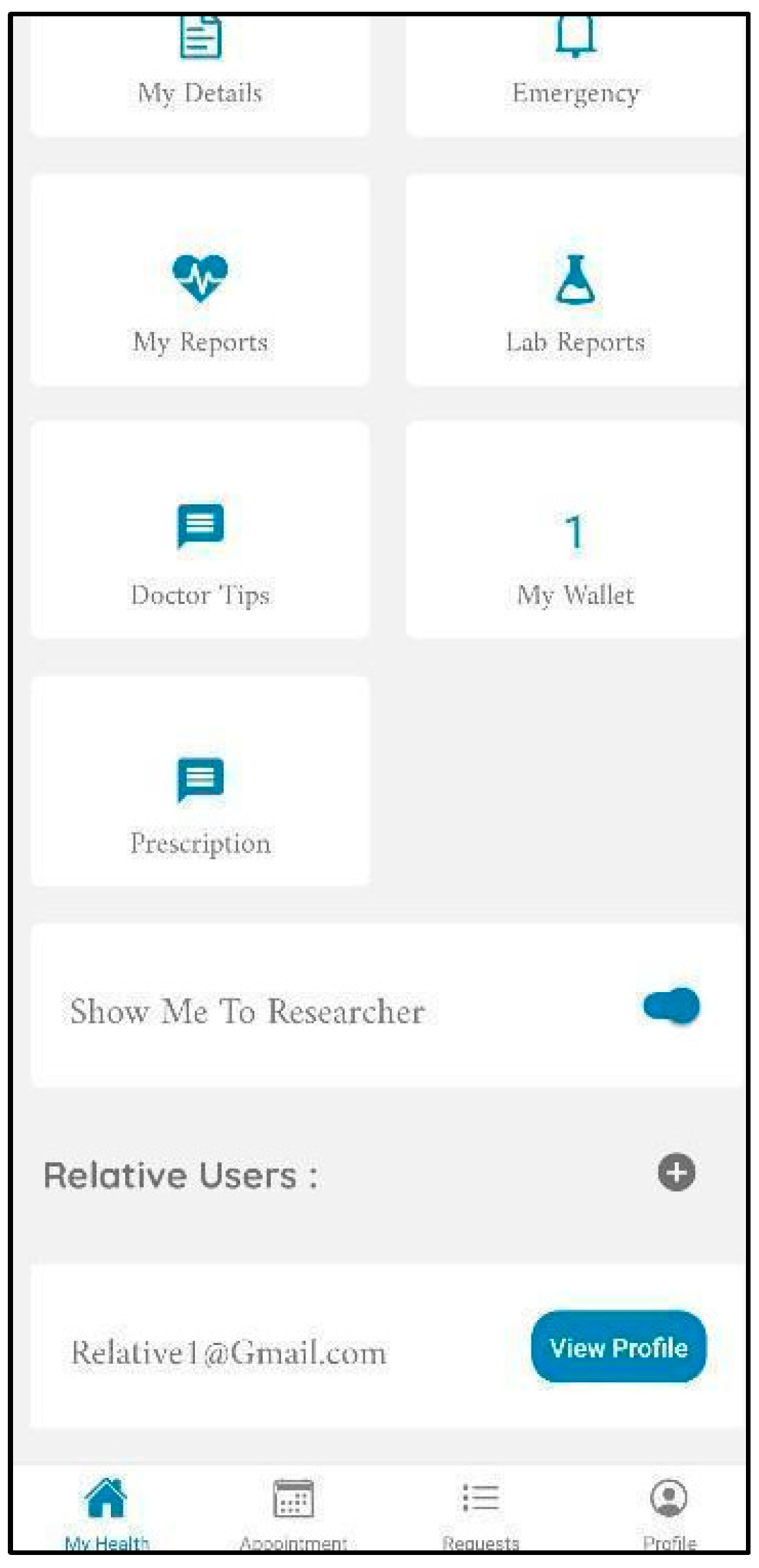
- Primary stakeholders: patients are the pivotal actors and primary beneficiaries of their records as the owners and data controllers at the first level;
- At the same level, primary stakeholders are also physicians, therapists, and those who provide advice and treatment to the patient in addition to that of pharmacies and laboratories, and who add the results of tests and other processes to a health record;
- Next, secondary stakeholders include insurance organizations who are responsible for medical approvals, relatives authorized by the patient on behalf of their health record, and employees responsible for administrative matters;
- Finally, tertiary stakeholders include government or private agencies, researchers, and medical institutions.
5.1. Functional Requirements
5.1.1. Identity Management and Data Ownership
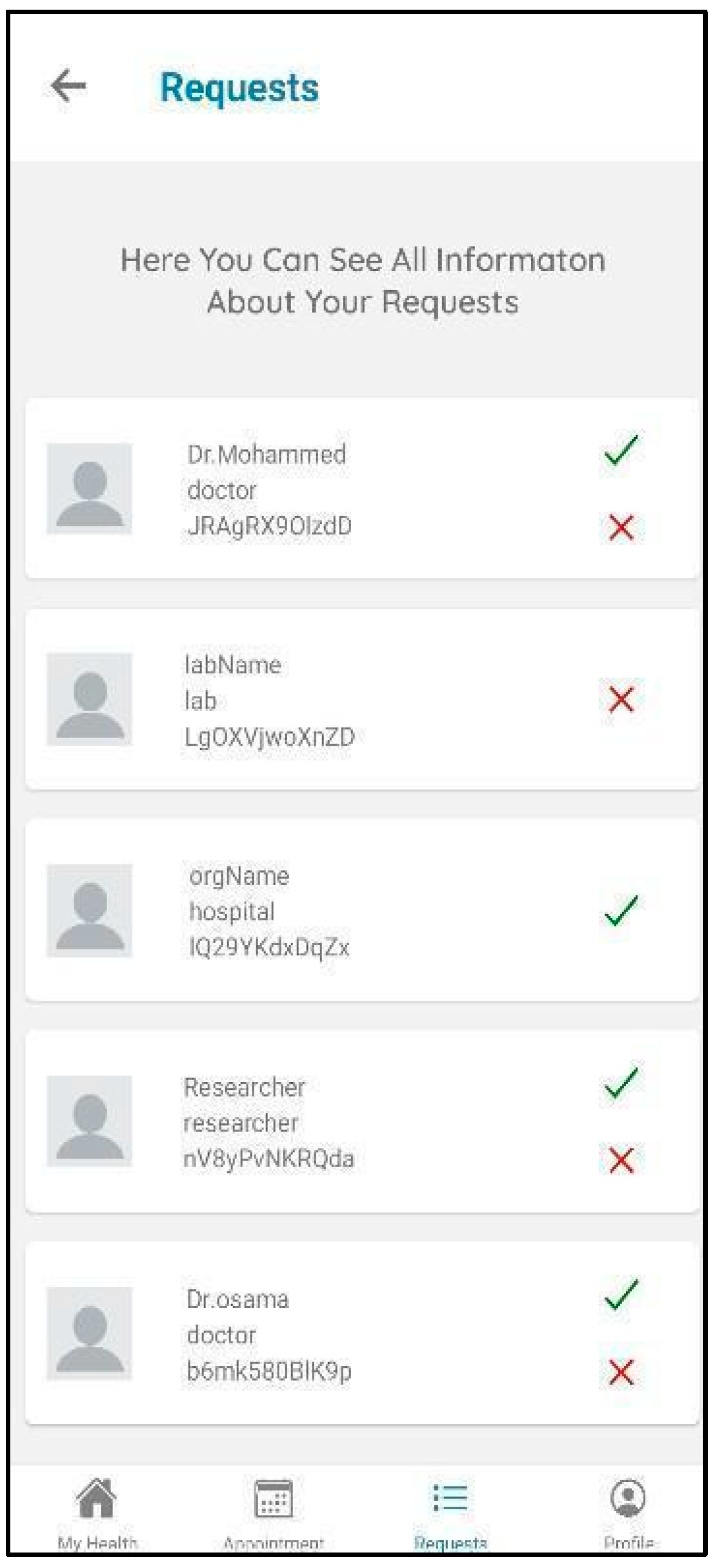
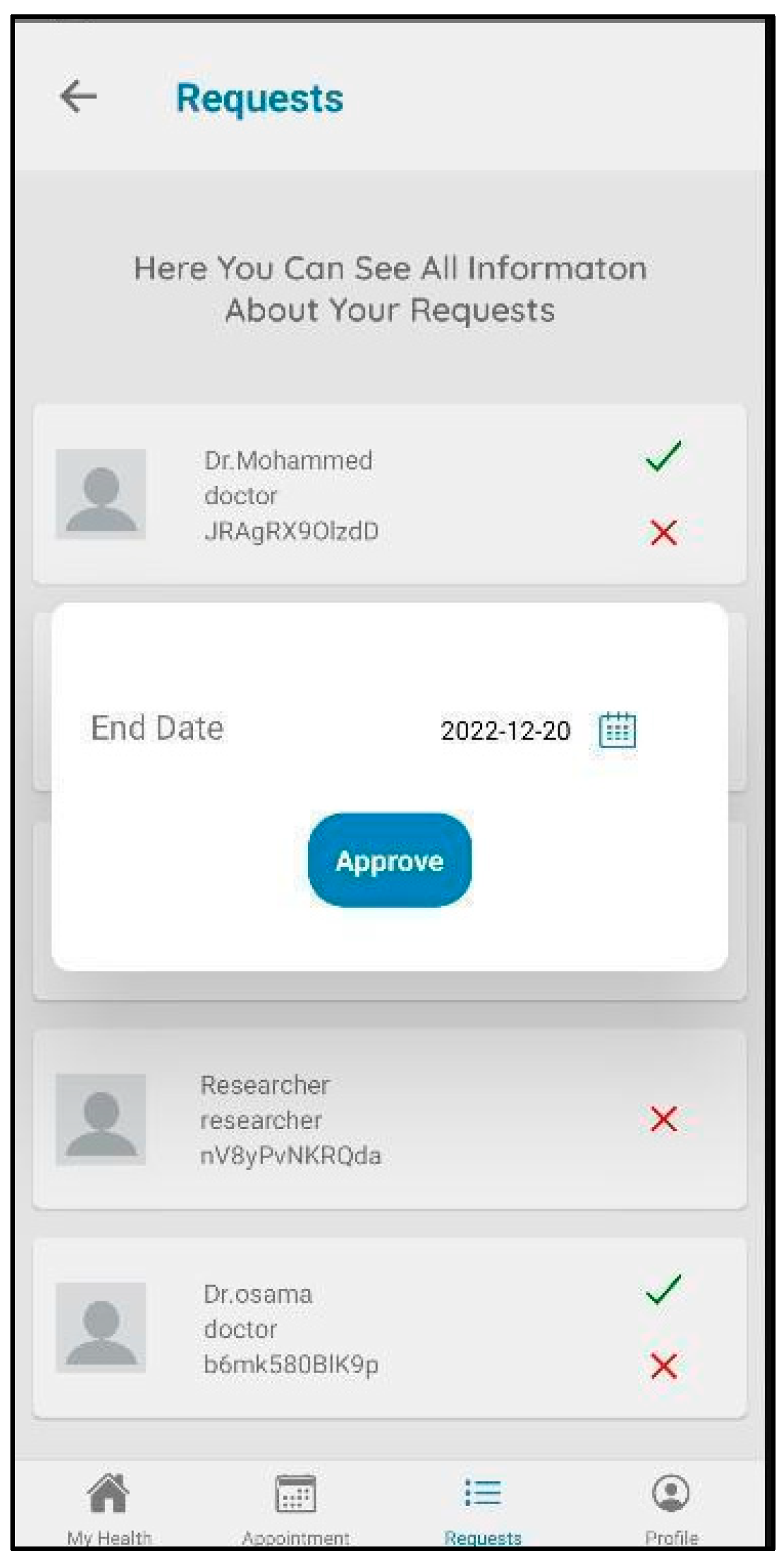
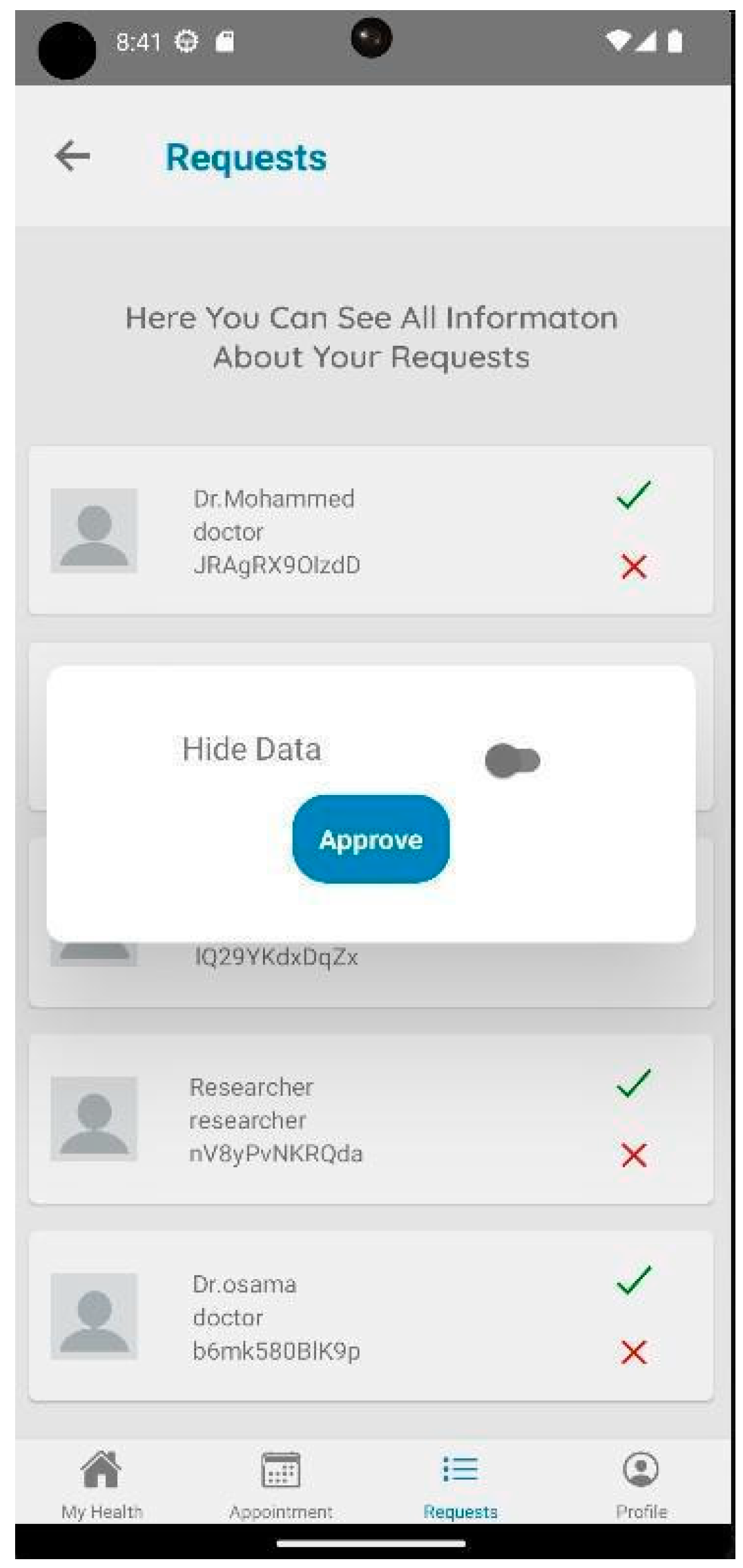
- Provide access control
- Share data with researchers and receive incentives
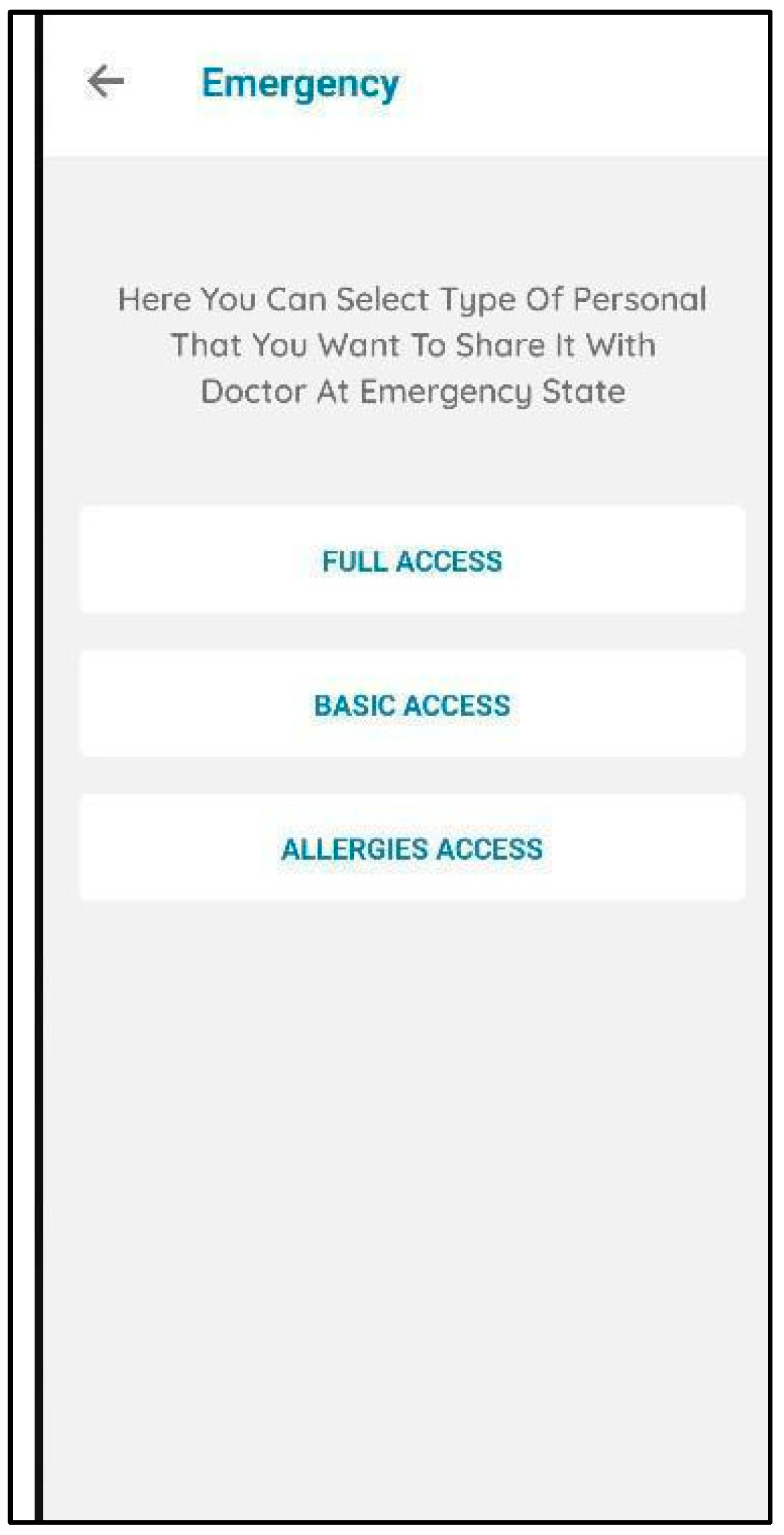
- Emergency and relatives’ access
5.1.2. PHR Content
- Medical support and appointment reservation
- Have all patient details, family history, allergies, and complete medical history
5.1.3. PHR and Stakeholders
- Unified medical standards and regulations
5.1.4. Healthcare Provider Administration Issues and PHRs
- Keep PHR for patient use and have another for healthcare center administrative use
- The section for physician documentation is not visible to a patient without a release option
5.2. System Design Requirements
- Location features for health recommendation and notification services
- Accessibility features and the right to be forgotten
- Two sections for inpatient and outpatient details
5.3. Nonfunctional Requirements
- Mobility and decentralized storage
- Performance, scalability, and availability
- Security and privacy
- Interoperability
- User friendliness and efficiency
5.4. Design of the Proposed System
5.4.1. The High-Level Architecture of the Proposed System
- The Logical Structure of Hyperledger Fabric
- Presentation layer: the patient can access their PHR from a mobile app or web browser and interact with a Fabric blockchain network through a system development kit (SDK).
- Data access layer: the SDK provides a simple application programming interface (API) that encapsulates all access to the ledger by allowing an application to interact with Fabric. The system provides a security layer so that the system’s members can access their related documents and information based on their role.
- Logic layer: this layer represents the functions of the chaincode for different members, which are healthcare centers, patients, physicians, etc. In addition, CouchDB and the ledger store the healthcare center’s information and the transaction history on the Hyperledger Fabric blockchain to maintain immutability and security. Each member can request access to the PHR, but they cannot view the record unless the patient grants them access.
- Data storage layer: the system solution contains data that are off-chain and data that are on-chain to maintain security and efficiency simultaneously; these are:
- Off-chain: this stores a user’s basic information through the health provider, including their mobile numbers, email addresses, and hashed passwords, in a regular secure database to provide them with the ability to delete and remove their accounts from the system at any time;
- Interplanetary file system (IPFS): a peer-to-peer decentralized storage service that stores vast PDF files such as X-rays with the proper security access, which will reduce the load on the blockchain and enhance performance [51].
- System Implementation Details
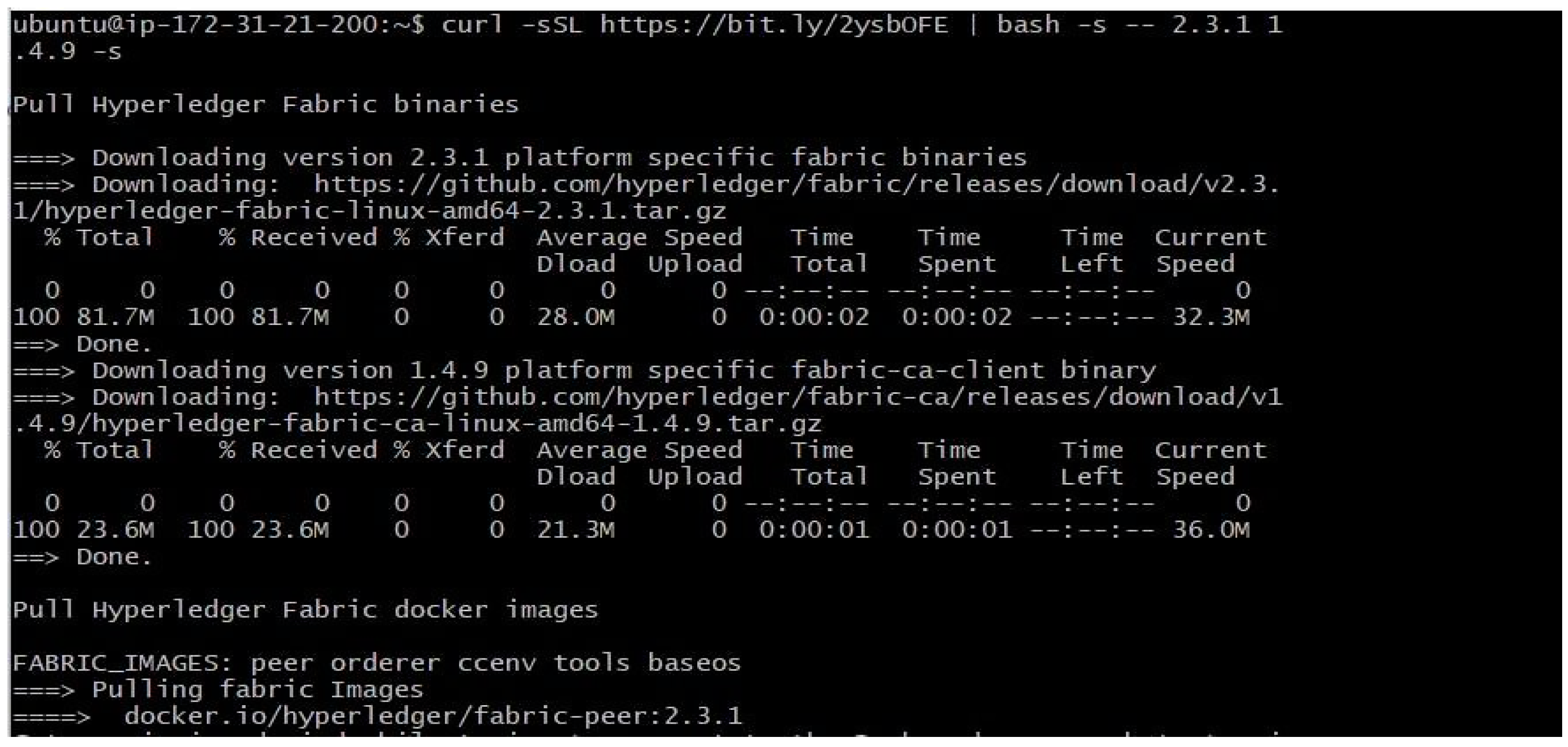
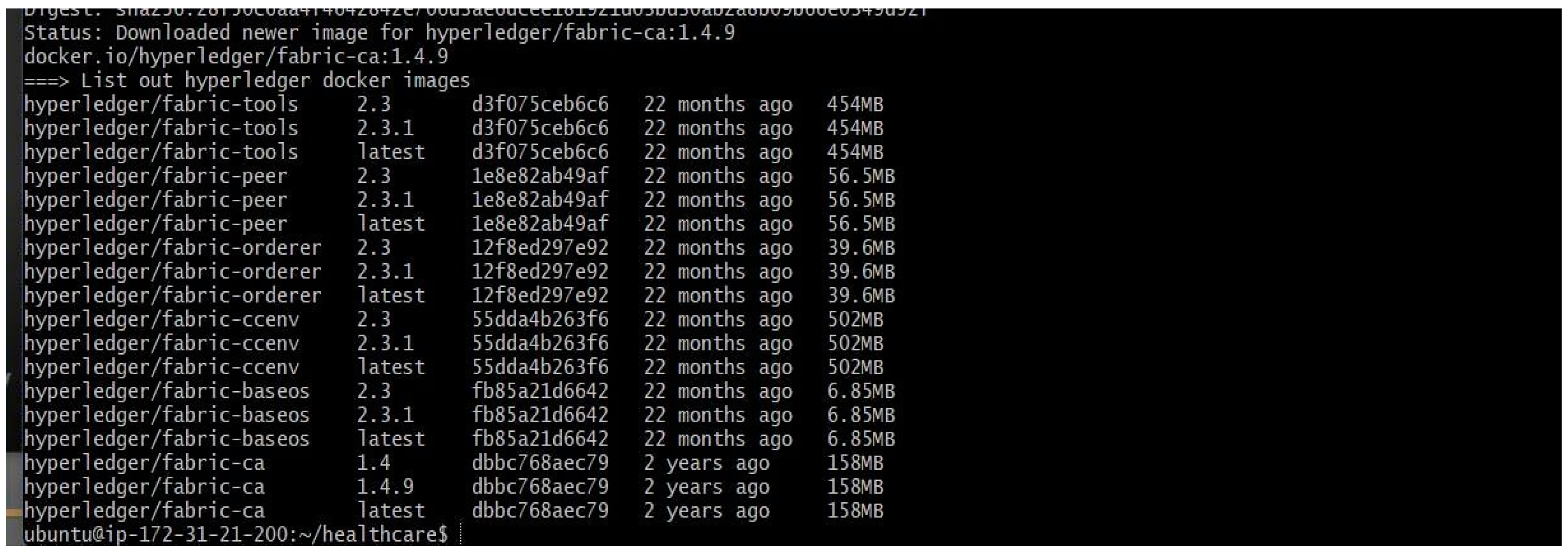
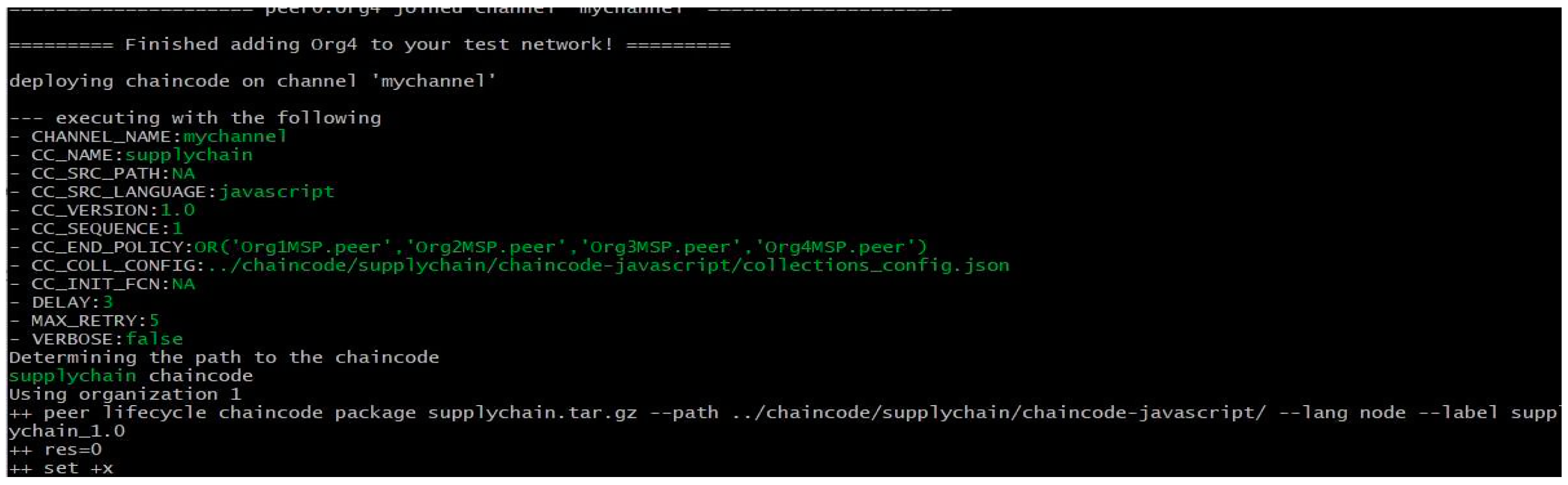
5.4.2. Implementation and Configuration
- Environment Setup
- One orderer;
- Four organizations with one peer per organization;
- One CouchDB instance per peer;
- CA server for the peers and orderer;
- One chaincode per organization.
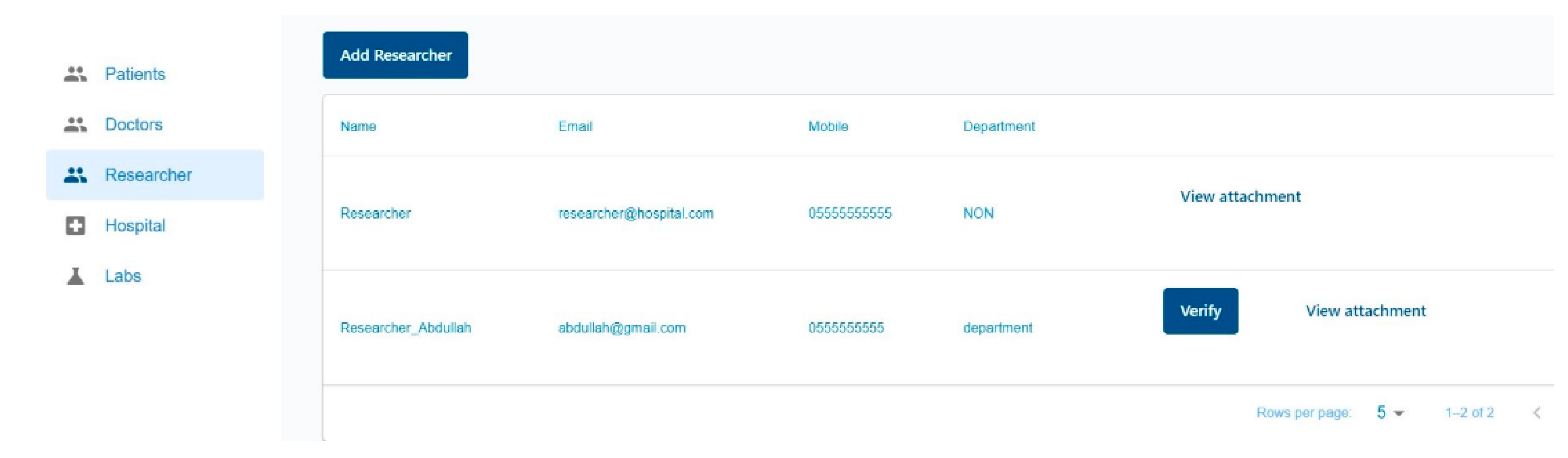
- Implementation Overview
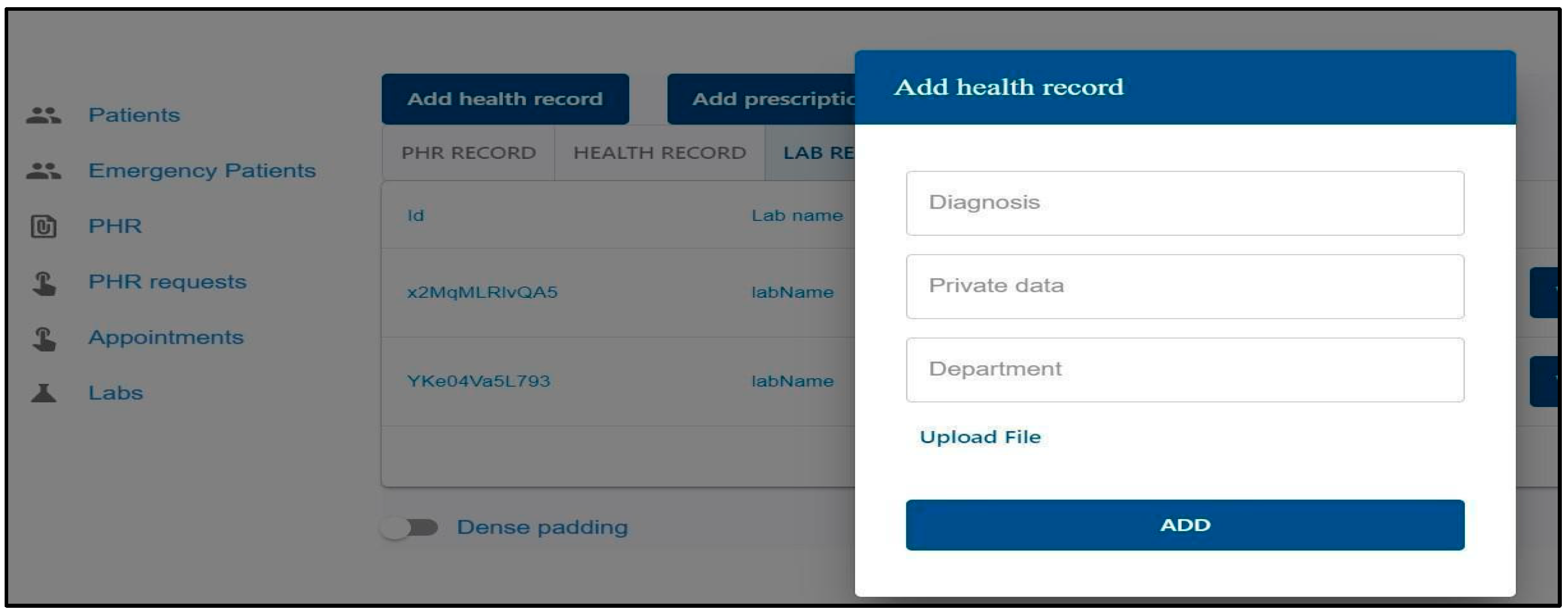
- PHR
- Researchers
- Physician
6. System Evaluation
6.1. Comparison with an Empirical Study
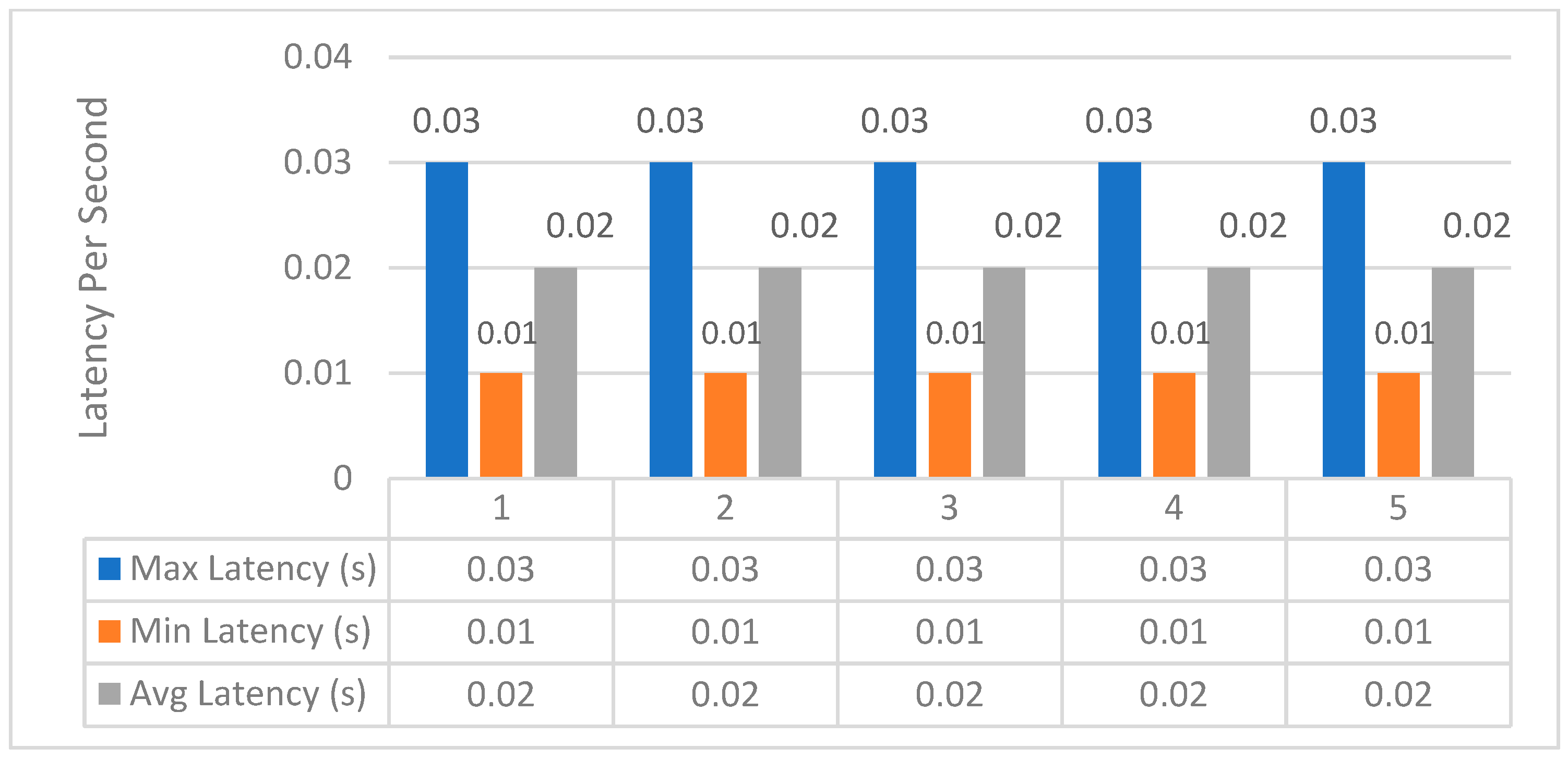
6.2. Latency
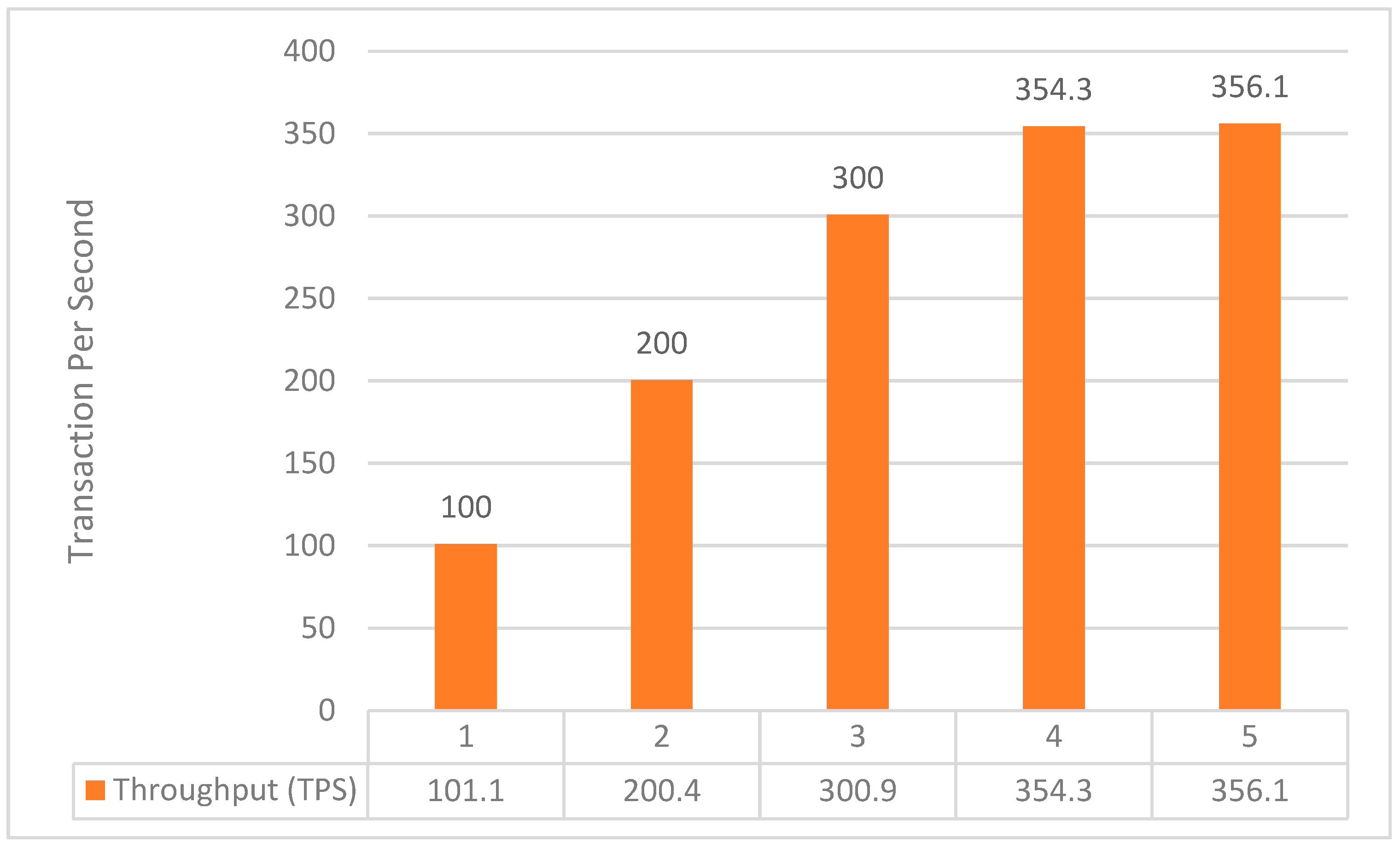
6.3. Throughput
6.4. Limitations
- Management of invoices and payments;
- Unified medical data standards and regulations;
- Sharing data with another health provider;
- Keeping PHRs for patient use and having another copy for healthcare centers’ administrative use.
- Accessibility features;
- Location features for health recommendations;
- Two sections for inpatient and outpatient details.
7. Conclusions
7.1. Major Contributions
- Proposed a solution for personal health records based on blockchain to give patients the power to own and benefit from their data;
- Introduced Hyperledger Fabric to achieve access control and govern identity for peers and users, user authentication, credential validation, signature generation, and verification;
- Designed and developed a working prototype based on the defined requirements;
- Engaged stakeholders from the industry to understand the real needs and to identify the requirements for PHRs;
- Evaluated the functionality of the system’s performance using the Hyperledger Caliper tool.
7.2. Minor Contributions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hau, Y.S.; Lee, J.M.; Park, J.; Chang, M.C. Attitudes toward blockchain technology in managing medical information: Survey study. J. Med. Internet Res. 2019, 21, e15870. [Google Scholar] [CrossRef]
- Chen, Y.; Ding, S.; Xu, Z.; Zheng, H.; Yang, S. Blockchain-Based Medical Records Secure Storage and Medical Service Framework. J. Med. Syst. 2018, 43, 5. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Dong, M.; Li, J.; Xu, G.; Chen, X.; Ota, K. Healthchain: Secure EMRs Management and Trading in Distributed Healthcare Service System. IEEE Internet Things J. 2020, 8, 7192–7202. [Google Scholar] [CrossRef]
- Yaqoob, I.; Salah, K.; Jayaraman, R.; Al-Hammadi, Y. Blockchain for healthcare data management: Opportunities, challenges, and future recommendations. Neural Comput. Appl. 2021, 34, 11475–11490. [Google Scholar] [CrossRef]
- Arndt, R.Z. How Third Parties Harvest Health Data from Providers, Payers and Pharmacies. Modern Healthcare. 2018. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=129027739&site=ehost-live&scope=site (accessed on 1 October 2020).
- Office of the Federal Register. Health Insurance Portability and Accountability Act of 1996. Public Law 104-191. 110; U.S. Government Printing Office: Washington, DC, USA, 1996; pp. 1936–2103.
- Viorescu, R. 2018 Reform of Eu Data Protection Rules. Eur. J. Law Public Adm. 2017, 4, 27–39. [Google Scholar] [CrossRef]
- Argaw, S.T.; Bempong, N.E.; Eshaya-Chauvin, B.; Flahault, A. The state of research on cyberattacks against hospitals and available best practice recommendations: A scoping review. BMC Med. Inform. Decis. Mak. 2019, 19, 10. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Lim, K.; Jung, S.Y.; Ji, H.; Hong, K.; Hwang, H.; Lee, H.-Y. Perspectives of patients, health care professionals, and developers toward blockchain-based health information exchange: Qualitative study. J. Med. Internet Res. 2020, 22, e18582. [Google Scholar] [CrossRef]
- Chukwu, E.; Garg, L. A systematic review of blockchain in healthcare: Frameworks, prototypes, and implementations. IEEE Access 2020, 8, 21196–21214. [Google Scholar] [CrossRef]
- Meier, P.; Beinke, J.H.; Fitte, C.; Brinke, J.S.T.; Teuteberg, F. Generating design knowledge for blockchain-based access control to personal health records. Inf. Syst. E-Bus. Manag. 2021, 19, 13–41. [Google Scholar] [CrossRef]
- Gimenez-Aguilar, M.; de Fuentes, J.M.; Gonzalez-Manzano, L.; Arroyo, D. Achieving cybersecurity in blockchain-based systems: A survey. Future Gener. Comput. Syst. 2021, 124, 91–118. [Google Scholar] [CrossRef]
- Aldamaeen, O.; Rashideh, W.; Alalawi, S.; Obidallah, W. Personal health records: Blockchain-based identity management and data ownership. In Proceedings of the 5th International Conference on Future Networks & Distributed Systems, Dubai, United Arab Emirates, 15–16 December 2021; pp. 87–92. [Google Scholar] [CrossRef]
- Zhu, Q.; Loke, S.W.; Trujillo-rasua, R.; Jiang, F.; Xiang, Y.; Trujillo-Rasua, R. 20 Applications of Distributed Ledger Technologies to the Internet of Things: A Survey. ACM Comput. Surv. 2019, 52, 1–34. [Google Scholar] [CrossRef]
- Nakamoto, S. Bitcoin: A Peer-to-Peer Electronic Cash System. 2008. Available online: www.bitcoin.org (accessed on 29 January 2022).
- Despotou, G.; Evans, J.; Nash, W.; Eavis, A.; Robbins, T.; Arvanitis, T.N. Evaluation of patient perception towards dynamic health data sharing using blockchain based digital consent with the Dovetail digital consent application: A cross sectional exploratory study. Digit. Health 2020, 6, 2055207620924949. [Google Scholar] [CrossRef] [PubMed]
- Thwin, T.T.; Vasupongayya, S. Blockchain-Based Access Control Model to Preserve Privacy for Personal Health Record Systems. Secur. Commun. Netw. 2019, 2019, 8315614. [Google Scholar] [CrossRef]
- Christidis, K.; Devetsikiotis, M. Blockchains and Smart Contracts for the Internet of Things. IEEE Access 2016, 4, 2292–2303. [Google Scholar] [CrossRef]
- Daraghmi, E.Y.; Daraghmi, Y.A.; Yuan, S.M. MedChain: A design of blockchain-based system for medical records access and permissions management. IEEE Access 2019, 7, 164595–164613. [Google Scholar] [CrossRef]
- Kuo, T.T.; Rojas, H.Z.; Ohno-Machado, L. Comparison of blockchain platforms: A systematic review and healthcare examples. J. Am. Med. Inform. Assoc. 2019, 26, 462–478. [Google Scholar] [CrossRef]
- Lim, S.Y.; Fotsing, P.T.; Almasri, A.; Musa, O.; Kiah, M.L.M.; Ang, T.F.; Ismail, R. Blockchain technology the identity management and authentication service disruptor: A survey. Int. J. Adv. Sci. Eng. Inf. Technol. 2018, 8, 1735–1745. [Google Scholar] [CrossRef]
- Androulaki, E.; Barger, A.; Bortnikov, V.; Cachin, C.; Christidis, K.; De Caro, A.; Enyeart, D.; Ferris, C.; Laventman, G.; Manevich, Y.; et al. Hyperledger Fabric: A Distributed Operating System for Permissioned Blockchains. In Proceedings of the 13th EuroSys Conference, Porto, Portugal, 23–26 April 2018; Volume 2018. [Google Scholar] [CrossRef]
- IBM. What is Hyperledger Fabric? IBM. 2021. Available online: https://www.ibm.com/topics/hyperledger (accessed on 30 September 2022).
- Zhuang, Y.; Sheets, L.R.; Chen, Y.W.; Shae, Z.Y.; Tsai, J.J.P.; Shyu, C.R. A patient-centric health information exchange framework using blockchain technology. IEEE J. Biomed. Health Inform. 2020, 24, 2169–2176. [Google Scholar] [CrossRef]
- Zaabar, B.; Cheikhrouhou, O.; Jamil, F.; Ammi, M.; Abid, M. HealthBlock: A secure blockchain-based healthcare data management system. Comput. Netw. 2021, 200, 108500. [Google Scholar] [CrossRef]
- Pawar, P.; Parolia, N.; Shinde, S.; Edoh, T.O.; Singh, M. eHealthChain—A blockchain-based personal health information management system. Ann. Telecommun. Telecommun. 2021, 77, 33–45. [Google Scholar] [CrossRef]
- Balistri, E.; Casellato, F.; Giannelli, C.; Stefanelli, C. BlockHealth: Blockchain-based secure and peer-to-peer health information sharing with data protection and right to be forgotten. ICT Express 2021, 7, 308–315. [Google Scholar] [CrossRef]
- Tang, X.; Guo, C.; Choo, K.-K.R.; Liu, Y.; Li, L. A secure and trustworthy medical record sharing scheme based on searchable encryption and blockchain. Comput. Netw. 2021, 200, 108540. [Google Scholar] [CrossRef]
- Uddin, M.; Memon, M.S.; Memon, I.; Ali, I.; Memon, J.; Abdelhaq, M.; Alsaqour, R. Hyperledger fabric blockchain: Secure and efficient solution for electronic health records. Comput. Mater. Contin. 2021, 68, 2377–2397. [Google Scholar] [CrossRef]
- Antwi, M.; Adnane, A.; Ahmad, F.; Hussain, R.; Rehman, M.H.U.; Kerrache, C.A. The case of HyperLedger Fabric as a blockchain solution for healthcare applications. Blockchain Res. Appl. 2021, 2, 100012. [Google Scholar] [CrossRef]
- Dubovitskaya, A.; Baig, F.; Xu, Z.; Shukla, R.; Zambani, P.S.; Swaminathan, A.; Jahangir, M.; Chowdhry, K.; Lachhani, R.; Idnani, N.; et al. ACTION-EHR: Patient-Centric Blockchain-Based Electronic Health Record Data Management for Cancer Care. J. Med. Internet Res. 2020, 22, e13598. [Google Scholar] [CrossRef] [PubMed]
- Albahli, S.; Khan, R.U.; Qamar, A.M. A blockchain-based architecture for smart healthcare system: A case study of Saudi Arabia. Adv. Sci. Technol. Eng. Syst. 2020, 5, 40–47. [Google Scholar] [CrossRef]
- Toshniwal, B.; Podili; Reddy, R.J.; Kataoka, K. PACEX: PAtient-Centric EMR eXchange in Healthcare Systems using Blockchain. In Proceedings of the 2019 IEEE 10th Annual Information Technology, Electronics and Mobile Communication Conference (IEMCON), Vancouver, BC, Canada, 17–19 October 2019; Volume 2019, pp. 954–960. [Google Scholar] [CrossRef]
- Leeming, G.; Cunningham, J.; Ainsworth, J. A Ledger of Me: Personalizing Healthcare Using Blockchain Technology. Front. Med. 2019, 6, 171. [Google Scholar] [CrossRef]
- Rajput, A.R.; Li, Q.; Ahvanooey, M.T. A blockchain-based secret-data sharing framework for personal health records in emergency condition. Healthcare 2021, 9, 206. [Google Scholar] [CrossRef]
- Shuaib, K.; Abdella, J.; Sallabi, F.; Serhani, M.A. Secure decentralized electronic health records sharing system based on blockchains. J. King Saud Univ.-Comput. Inf. Sci. 2021, 34, 5045–5058. [Google Scholar] [CrossRef]
- Stafford, T.F.; Treiblmaier, H. Characteristics of a Blockchain Ecosystem for Secure and Sharable Electronic Medical Records. IEEE Trans. Eng. Manag. 2020, 67, 1340–1362. [Google Scholar] [CrossRef]
- Gan, C.; Saini, A.; Zhu, Q.; Xiang, Y.; Zhang, Z. Blockchain-based access control scheme with incentive mechanism for eHealth systems: Patient as supervisor. Multimed. Tools Appl. 2021, 80, 30605–30621. [Google Scholar] [CrossRef]
- Yakubu, A.M.; Chen, Y.P.P. A blockchain-based application for genomic access and variant discovery using smart contracts and homomorphic encryption. Futur. Gener. Comput. Syst. 2022, 137, 234–247. [Google Scholar] [CrossRef]
- Faber, B.; Michelet, G.C.; Weidmann, N.; Mukkamala, R.R.; Vatrapu, R. BPDIMS: A Blockchain-based Personal Data and Identity Management System. In Proceedings of the 52nd Hawaii International Conference on System Sciences, Maui, HI, USA, 8–11 January 2019; Volume 6, pp. 6855–6864. [Google Scholar] [CrossRef]
- Beinke, J.H.; Fitte, C.; Teuteberg, F. Towards a stakeholder-oriented blockchain-based architecture for electronic health records: Design science research study. J. Med. Internet Res. 2019, 21, e13585. [Google Scholar] [CrossRef]
- Johannesson, P.; Perjons, E. An Introduction to Design Science; Springer: Cham, Switzerland, 2014; pp. 1–197. [Google Scholar] [CrossRef]
- Hevner, A.; Chatterjee, S. Design Research in Information Systems; Springer: Boston, MA, USA, 2010; Volume 22. [Google Scholar]
- Venable, J.R.; Pries-Heje, J.; Baskerville, R.L.; Venable, J.R.; Pries-Heje, J.; Baskerville, R. Choosing a Design Science Research Methodology. ACIS 2017 Proc. 2017, 2, 112. Available online: https://aisel.aisnet.org/acis2017/112 (accessed on 31 August 2022).
- Peffers, K.; Tuunanen, T.; Rothenberger, M.A.; Chatterjee, S. A design science research methodology for information systems research. J. Manag. Inf. Syst. 2014, 24, 45–77. [Google Scholar] [CrossRef]
- Barbour, R.S. Checklists for improving rigour in qualitative research: A case of the tail wagging the dog? BMJ 2001, 322, 1115–1117. [Google Scholar] [CrossRef]
- Palinkas, L.A.; Horwitz, S.M.; Green, C.A.; Wisdom, J.P.; Duan, N.; Hoagwood, K. Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm. Policy Ment. Health Ment. Health Serv. Res. 2013, 42, 533–544. [Google Scholar] [CrossRef]
- Wiltfang, G.L.; Berg, B.L. Qualitative Research Methods for the Social Sciences. Teach. Sociol. 1990, 18, 563. [Google Scholar] [CrossRef]
- Bauer, J. Význam průkazu RAS mutací pro anti-EGFR protilátky v léčbě 1. linie metastazujícího kolorektálního karcinomu. Onkology 2013, 7, 260–261. [Google Scholar]
- ATLAS.ti|The Qualitative Data Analysis & Research Software—ATLAS.ti. Available online: https://atlasti.com/ (accessed on 20 August 2022).
- Benet, J. IPFS—Content Addressed, Versioned, P2P File System. arXiv 2014, arXiv:1407.3561. [Google Scholar]
- Hevner, A.; Chatterjee, S. Design Science Research Frameworks. In Design Research in Information Systems; Springer: Berlin/Heidelberg, Germany, 2010; pp. 23–31. [Google Scholar] [CrossRef]
- Hevner, A.R.; March, S.T.; Park, J.; Ram, S. Design science in information systems research. MIS Q. Manag. Inf. Syst. 2004, 28, 75–105. [Google Scholar] [CrossRef]
- Fan, C.; Ghaemi, S.; Khazaei, H.; Musilek, P. Performance Evaluation of Blockchain Systems: A Systematic Survey. IEEE Access 2020, 8, 126927–126950. [Google Scholar] [CrossRef]
- Hyperledger Caliper. Caliper. Hyprtledger. 2018. Available online: https://www.hyperledger.org/blog/2018/03/19/measuring-blockchain-performance-with-hyperledger-caliper (accessed on 12 June 2021).
- Fatokun, T.; Nag, A.; Sharma, S. Towards a blockchain assisted patient owned system for electronic health records. Electronics 2021, 10, 580. [Google Scholar] [CrossRef]
- Rajput, A.R.; Li, Q.; Ahvanooey, M.T.; Masood, I. EACMS: Emergency Access Control Management System for Personal Health Record Based on Blockchain. IEEE Access 2019, 7, 84304–84317. [Google Scholar] [CrossRef]
- Hongwei, L.; Xinhui, W.; Sanyang, L. A Case Study for Blockchain in Healthcare: ‘MedRec’ prototype for electronic health records and medical research data. Optim. Methods Softw. 2016, 19, 125–136. [Google Scholar]
- Sinha, S.R.; Park, Y. Dealing with Security, Privacy, Access Control, and Compliance. In Building an Effective IoT Ecosystem for Your Business; Springer: Berlin/Heidelberg, Germany, 2017; pp. 155–176. [Google Scholar] [CrossRef]
- McGhin, T.; Choo, K.K.R.; Liu, C.Z.; He, D. Blockchain in healthcare applications: Research challenges and opportunities. J. Netw. Comput. Appl. 2019, 135, 62–75. [Google Scholar] [CrossRef]
- Azaria, A.; Ekblaw, A.; Vieira, T.; Lippman, A. MedRec: Using blockchain for medical data access and permission management. In Proceedings of the 2016 2nd International Conference on Open and Big Data (OBD), Vienna, Austria, 22–24 August 2016; pp. 25–30. [Google Scholar] [CrossRef]
- Thwin, T.T.; Vasupongayya, S. Performance analysis of blockchain-based access control model for personal health record system with architectural modelling and simulation. Int. J. Netw. Distrib. Comput. 2020, 8, 139–151. [Google Scholar] [CrossRef]
- Dodevski, Z.; Filiposka, S.; Mishev, A.; Trajkovik, V. Real time availability and consistency of health-related information across multiple stakeholders: A blockchain based approach. Comput. Sci. Inf. Syst. 2021, 18, 927–955. [Google Scholar] [CrossRef]
- Dwivedi, A.D.; Srivastava, G.; Dhar, S.; Singh, R. A decentralized privacy-preserving healthcare blockchain for IoT. Sensors 2019, 19, 326. [Google Scholar] [CrossRef]
- Zhang, A.; Lin, X. Towards Secure and Privacy-Preserving Data Sharing in e-Health Systems via Consortium Blockchain. J. Med. Syst. 2018, 42, 140. [Google Scholar] [CrossRef]
- Rahurkar, S.; Vest, J.R.; Menachemi, N. Despite The Spread of Health Information Exchange, There Is Little Evidence of Its Impact on Cost, Use, and Quality of Care. Health Aff. 2015, 34, 477–483. [Google Scholar] [CrossRef]
- Gordon, W.J.; Catalini, C. Blockchain Technology for Healthcare: Facilitating the Transition to Patient-Driven Interoperability. Comput. Struct. Biotechnol. J. 2018, 16, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Dagher, G.G.; Mohler, J.; Milojkovic, M.; Marella, P.B. Ancile: Privacy-preserving framework for access control and interoperability of electronic health records using blockchain technology. Sustain. Cities Soc. 2018, 39, 283–297. [Google Scholar] [CrossRef]
- George, M.; Chacko, A.M. MediTrans—Patient-centric interoperability through blockchain. Int. J. Netw. Manag. 2021, 32, e2187. [Google Scholar] [CrossRef]
- Tandon, A.; Dhir, A.; Islam, N.; Mäntymäki, M. Blockchain in healthcare: A systematic literature review, synthesizing framework and future research agenda. Comput. Ind. 2020, 122, 103290. [Google Scholar] [CrossRef]
- Zghaibeh, M.; Farooq, U.; Hasan, N.U.; Baig, I. SHealth: A Blockchain-Based Health System with Smart Contracts Capabilities. IEEE Access 2020, 8, 70030–70043. [Google Scholar] [CrossRef]
- Kuzlu, M.; Pipattanasomporn, M.; Gurses, L.; Rahman, S. Performance analysis of a hyperledger fabric blockchain framework: Throughput, latency and scalability. In Proceedings of the 2019 IEEE International Conference on Blockchain (Blockchain), Atlanta, GA, USA, 14–17 July 2019; pp. 536–540. [Google Scholar] [CrossRef]
- Khan, D.; Jung, L.T.; Hashmani, M.A.; Cheong, M.K. Empirical Performance Analysis of Hyperledger LTS for Small and Medium Enterprises. Sensors 2022, 22, 915. [Google Scholar] [CrossRef]
- Pajooh, H.H.; Rashid, M.A.; Alam, F.; Demidenko, S. Experimental Performance Analysis of a Scalable Distributed Hyperledger Fabric for a Large-Scale IoT Testbed. Sensors 2022, 22, 4868. [Google Scholar] [CrossRef] [PubMed]
- Nasir, Q.; Qasse, I.A.; Talib, M.A.; Nassif, A.B. Performance analysis of hyperledger fabric platforms. Secur. Commun. Netw. 2018, 2018. [Google Scholar] [CrossRef]








| Interviewees’ Information | |||
|---|---|---|---|
| No. | Position | Experience | Healthcare Provider Sector |
| 1. | IT manager | 15 | Private |
| 2. | Medical records manager | 6 | Private |
| 3. | Information and medical records director | 21 | Government |
| 4. | Medical director and implementer of KFMC’s electronic health record system | 14 | Government |
| 5. | Physician and patient safety and quality manager | 20 | Private |
| 6. | Physician and medical director | 12 | Private |
| 7. | Clinical application specialist (ERM, ESM, HIM, charge services, and reporting) and executive manager | 28 | Government |
| 8. | HIS and EMR manager | 14 | Government |
| 9. | IT director | 13 | Private |
| 10. | IT and HIS manager | 21 | Private |
| 11. | Medical records manager | 10 | Government |
| 12. | Deputy medical director (acts as the medical manager) | 18 | Government |
| 13. | Medical records system administrator | 7 | Private |
| No. | Requirement | Reference | E1 | E2 | E3 | E4 | E5 | E6 | E7 | E8 | E9 | E10 | E11 | E12 | E13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Functional Requirements | |||||||||||||||
| A | Identity Management and Data Ownership | ||||||||||||||
| 1. | The system must allow the patient to manage their identity and be the owner of their data. | [1,2,3,16,24] | |||||||||||||
| 2. | The system should provide access control (accept/reject/deny) for patients regarding their PHR. | [1,2,16,24] | * | ||||||||||||
| 3. | The system should allow patients to approve/deny access to their data for clinical research purposes. | [11] | |||||||||||||
| 4. | The system should allow patients to hide identity and sensitive data. | [11,57] | * | ||||||||||||
| 5. | The system should allow patients to receive incentives if they agree to share data with other parties. | [37,41,56] | * | ||||||||||||
| 6. | The system should provide emergency access to PHRs based on patient preferences. | [11,35] | * | ||||||||||||
| 7. | The system should provide relatives with access. | [41] | * | * | * | ||||||||||
| B | PHRs and Stakeholders | ||||||||||||||
| 8. | The system should allow a physician to transfer a patient to another physician or healthcare center. | - | * | * | |||||||||||
| 9. | The system should have a unified record number across all healthcare centers. | * | * | * | * | ||||||||||
| 10. | The system should be able to share data with another provider. | - | * | * | * | ||||||||||
| 11. | The system must not allow a patient to edit or delete reports. | - | * | ||||||||||||
| C | PHR Content | ||||||||||||||
| 12. | The system should have a survey of family diseases. | - | * | * | |||||||||||
| 13. | The system should have all patient details and medical histories. | [41] | * | * | * | * | * | * | * | * | * | * | |||
| 14. | The system should allow patients to view all reports and to have the ability to copy them. | - | * | * | * | ||||||||||
| 15. | The system should have medical support for chatting and tips or contact information for physicians. | _ | * | * | * | * | * | * | |||||||
| 16. | The system should have a reservation system for appointments. | - | * | * | |||||||||||
| D | Healthcare Provider Administration Issues and PHRs | ||||||||||||||
| 17. | The system should have a release option for physicians for sensitive reports. | - | * | * | |||||||||||
| 18. | The system must allow a healthcare center to modify false information in PHR reports. | - | * | * | * | * | * | ||||||||
| 19. | The system should have sections for physician documentation that are not visible to the patient. | - | * | * | * | * | * | ||||||||
| 20. | The system should keep PHRs for patient use and have another copy for a healthcare center for administrative use. | - | * | ||||||||||||
| Nonfunctional Requirements | |||||||||||||||
| 1. | The system should support controlling the access of channel information based on the user’s identity (data privacy, protection, and confidentiality). | [11,19,27,61,67] | * | * | |||||||||||
| 2. | The system should be interoperable and scalable among stakeholders. | [60,61,62,63,64,66] | |||||||||||||
| 3. | The system should be usable, allowing users to complete their tasks efficiently. | [54] | * | * | |||||||||||
| 4. | The system should have the availability of infrastructure services that are core to the blockchain system’s operations. | [65] | |||||||||||||
| 5. | The system should provide security and transaction traceability. | [19,52,58] | |||||||||||||
| 6. | The system should have smart contract capabilities to validate transactions, i.e., the execution of decentralized applications. | [19,52,58,59] | |||||||||||||
| 7. | The system should provide two-factor authentication or fingerprint authorization. | - | * | * | * | * | |||||||||
| 8. | The system should support mobility and decentralized data storage. | [51,52,54,58] | |||||||||||||
| System Design Requirements | |||||||||||||||
| 1. | The system should provide notification services. | [58] | |||||||||||||
| 2. | The system should provide a right-to-be-forgotten feature. | [27] | |||||||||||||
| 3. | The graphical interface of the system should be user friendly. | [71] | |||||||||||||
| 4. | The system should have a location feature for health recommendations. | - | |||||||||||||
| 5. | The system should have two sections for inpatient and outpatient details. | - | |||||||||||||
| Performance Environment and Specifications | ||
|---|---|---|
| No. | This Study | Khan et al. (2022) [73] |
| Configuration | AWS EC2 (2.2 × large) with an 8 core CPU, 32 GB RAM, and running Ubuntu 22.04 LTS | Intel Xeon®, 2.6 GHz with a 12 core CPU, 16 GB RAM, 500 GB disk space, and running Ubuntu 18.04 LTS |
| Algorithm | RAFT | RAFT |
| Originations | 4 Organizations | 2 Organizations |
| Peers | 1 Peer each | 1 Peer each |
| Author | Fabric Version | Latency | Throughput | Test Environment | ||
|---|---|---|---|---|---|---|
| Query | Open | Query | Open | |||
| Nasir et al. (2018) [75] | Fabric 0.6 | 5.18 | 5.18 | 19.26 | 155 | HPC server in Hertz, Xeon® CPU E5-2690, 2.60 GHz, 24 core CPU, 64 GB RAM, and running Ubuntu 16.04 LTS |
| Fabric 1.0 | 1.37 | 5.18 | 461 | 185 | ||
| Khan et al. (2022) [73] | Fabric 2.2 | 6.74 | 19.66 | 45.4 | 31.7 | Intel® Xeon®, 2.6 GHz with 12 core CPU, 16 GB RAM, 500 GB disk space, and running Ubuntu 18.04 LTS |
| This study | Fabric 2.2 | 0.01 | 7.86 | 377.5 | 34.5 | AWS EC2 (2.2 × large), 8 core CPU, 32 GB RAM, and running Ubuntu 22.04 LTS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aldamaeen, O.; Rashideh, W.; Obidallah, W.J. Toward Patient-Centric Healthcare Systems: Key Requirements and Framework for Personal Health Records Based on Blockchain Technology. Appl. Sci. 2023, 13, 7697. https://doi.org/10.3390/app13137697
Aldamaeen O, Rashideh W, Obidallah WJ. Toward Patient-Centric Healthcare Systems: Key Requirements and Framework for Personal Health Records Based on Blockchain Technology. Applied Sciences. 2023; 13(13):7697. https://doi.org/10.3390/app13137697
Chicago/Turabian StyleAldamaeen, Ohud, Waleed Rashideh, and Waeal J. Obidallah. 2023. "Toward Patient-Centric Healthcare Systems: Key Requirements and Framework for Personal Health Records Based on Blockchain Technology" Applied Sciences 13, no. 13: 7697. https://doi.org/10.3390/app13137697
APA StyleAldamaeen, O., Rashideh, W., & Obidallah, W. J. (2023). Toward Patient-Centric Healthcare Systems: Key Requirements and Framework for Personal Health Records Based on Blockchain Technology. Applied Sciences, 13(13), 7697. https://doi.org/10.3390/app13137697








