BUU-LSPINE: A Thai Open Lumbar Spine Dataset for Spondylolisthesis Detection
Abstract
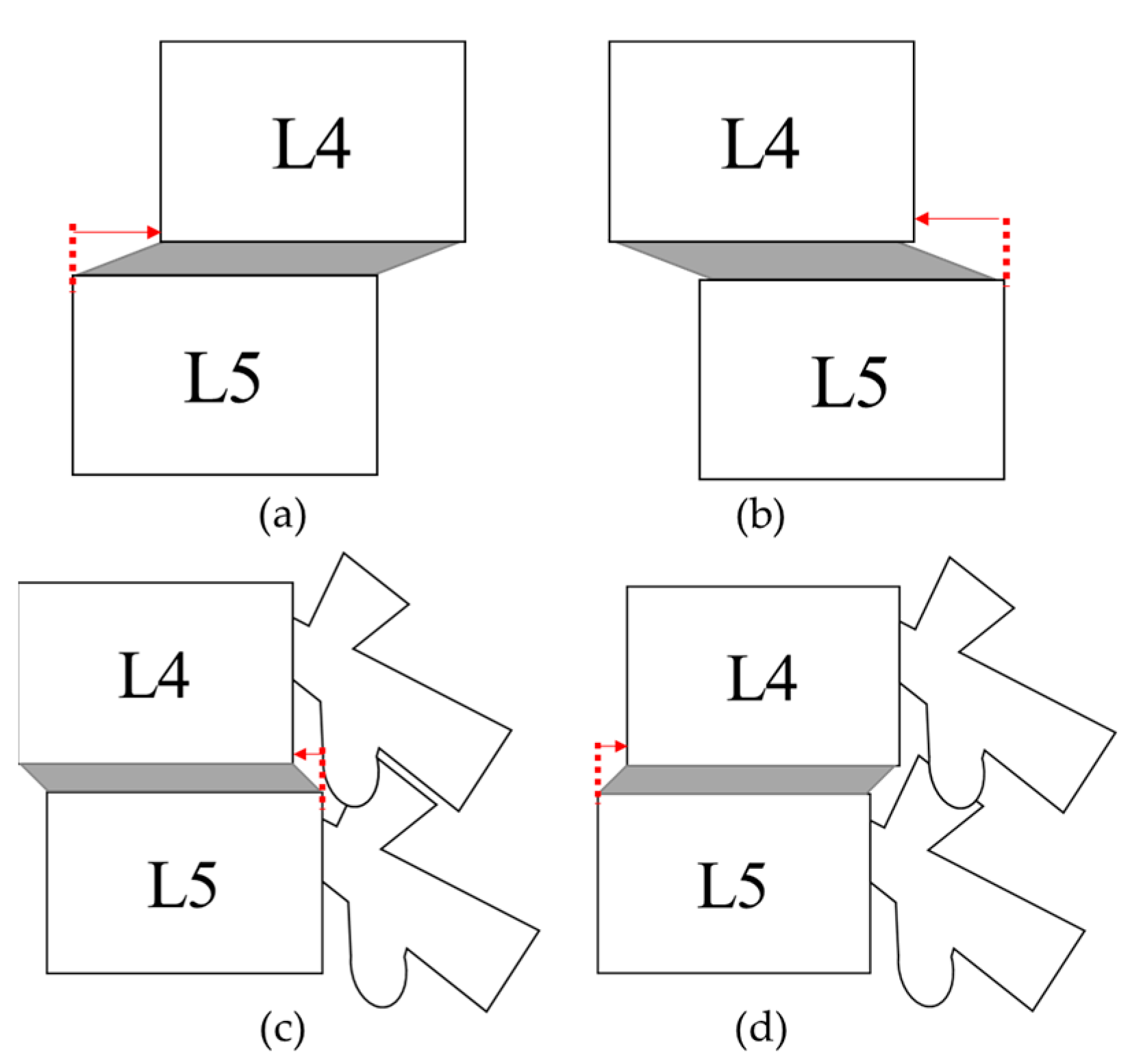
:1. Introduction
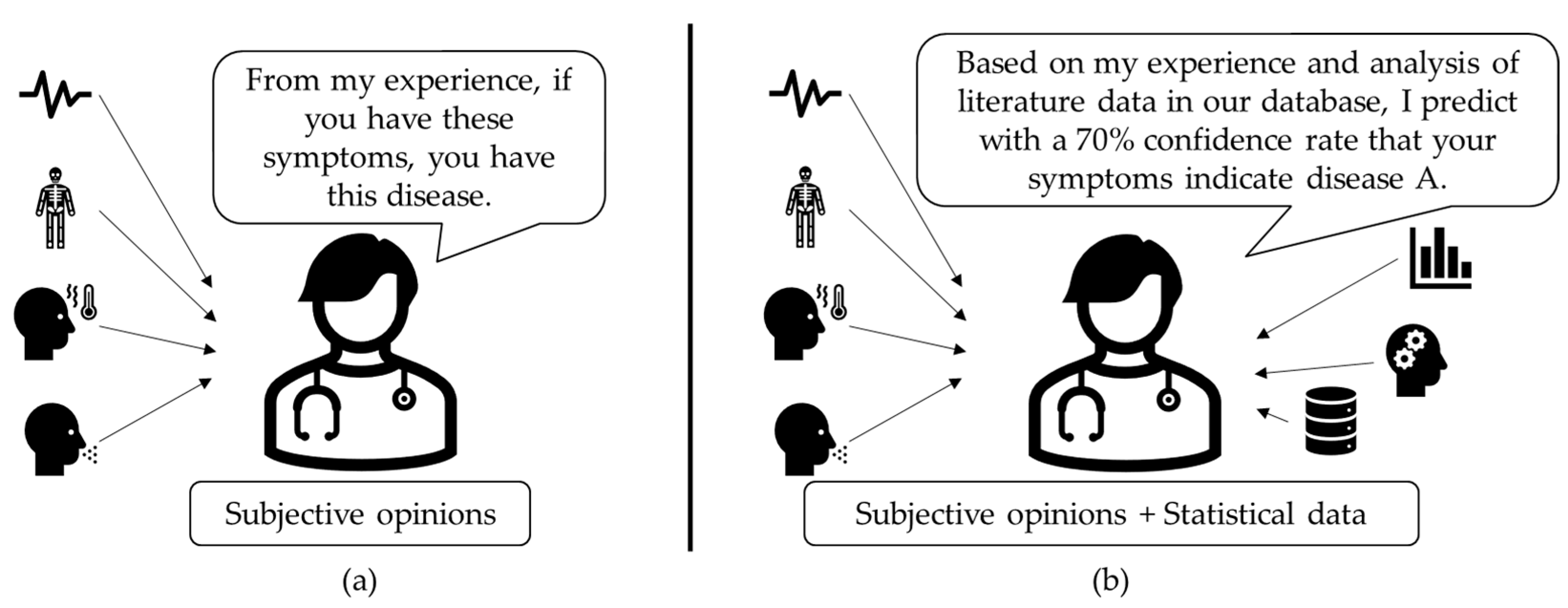
1.1. Background Knowledge
1.2. Literature Review
2. Materials and Methods
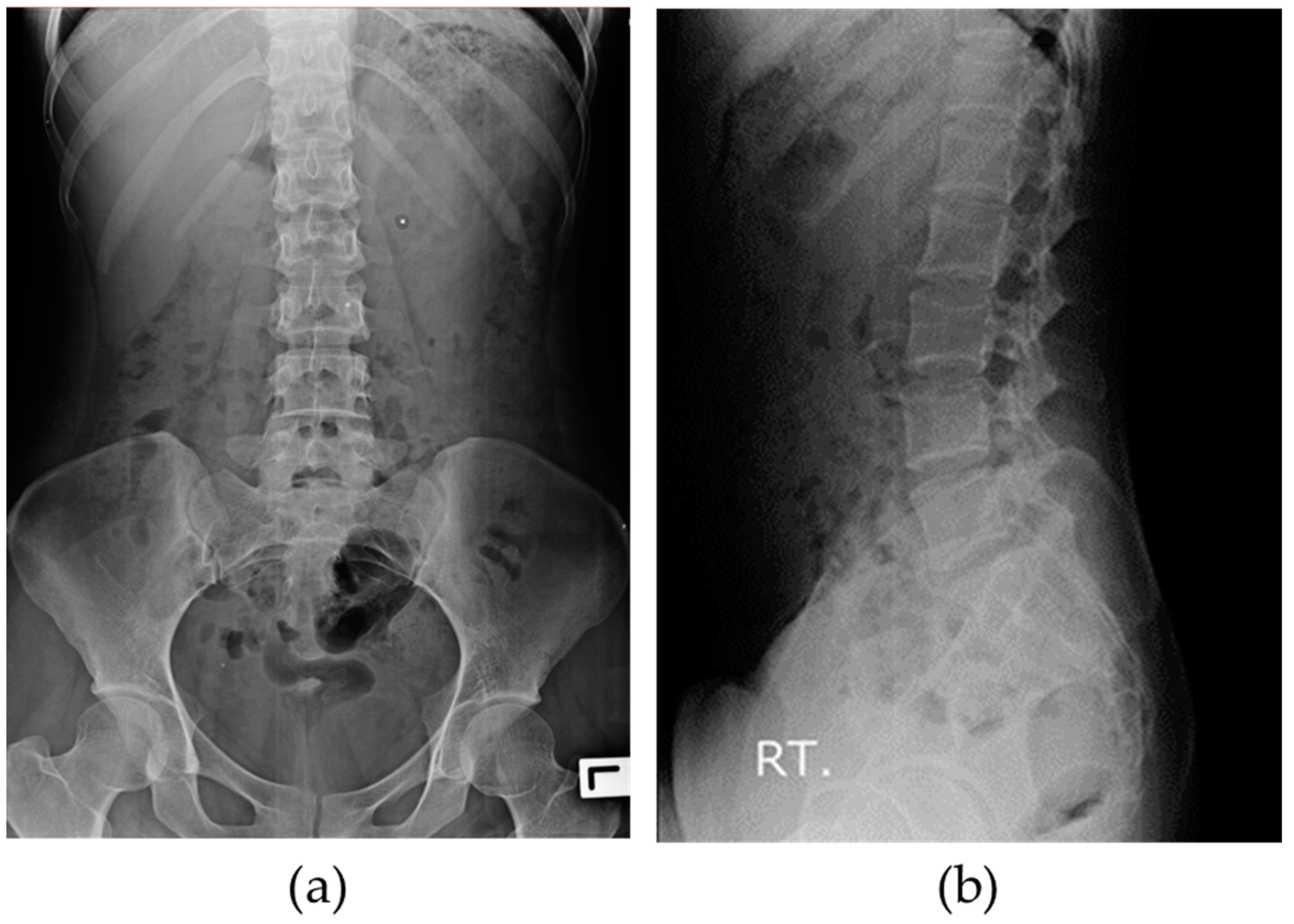
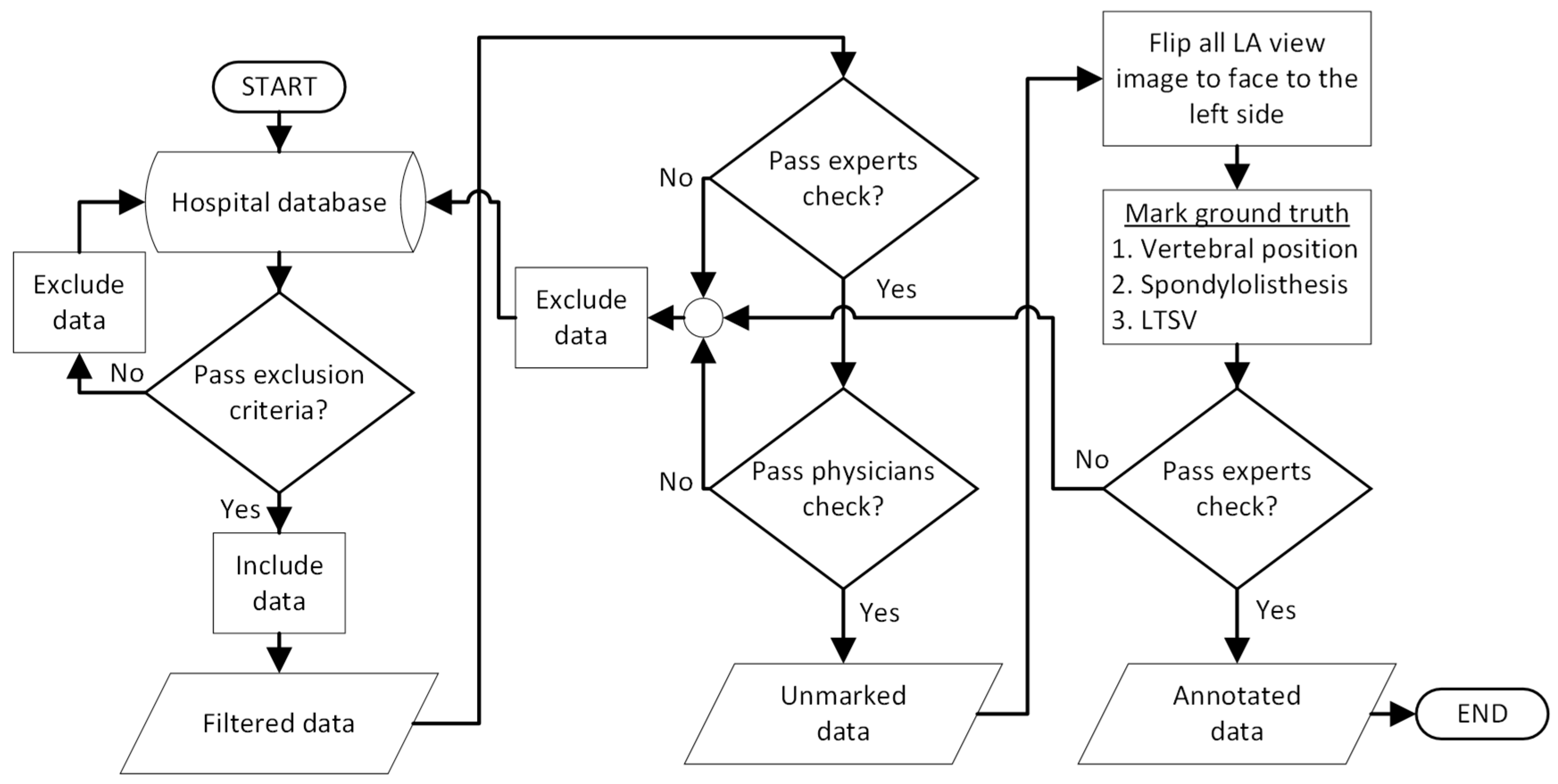
2.1. BUU-LSPINE
2.2. Ground Truth Data
- Low quality and high noise (challenging to distinguish the vertebrae);
- Embedded medical devices (cover the lumbar vertebrae area);
- Missing some of the lumbar vertebrae;
- Highly damaged vertebrae (challenging to determine the vertebral body).
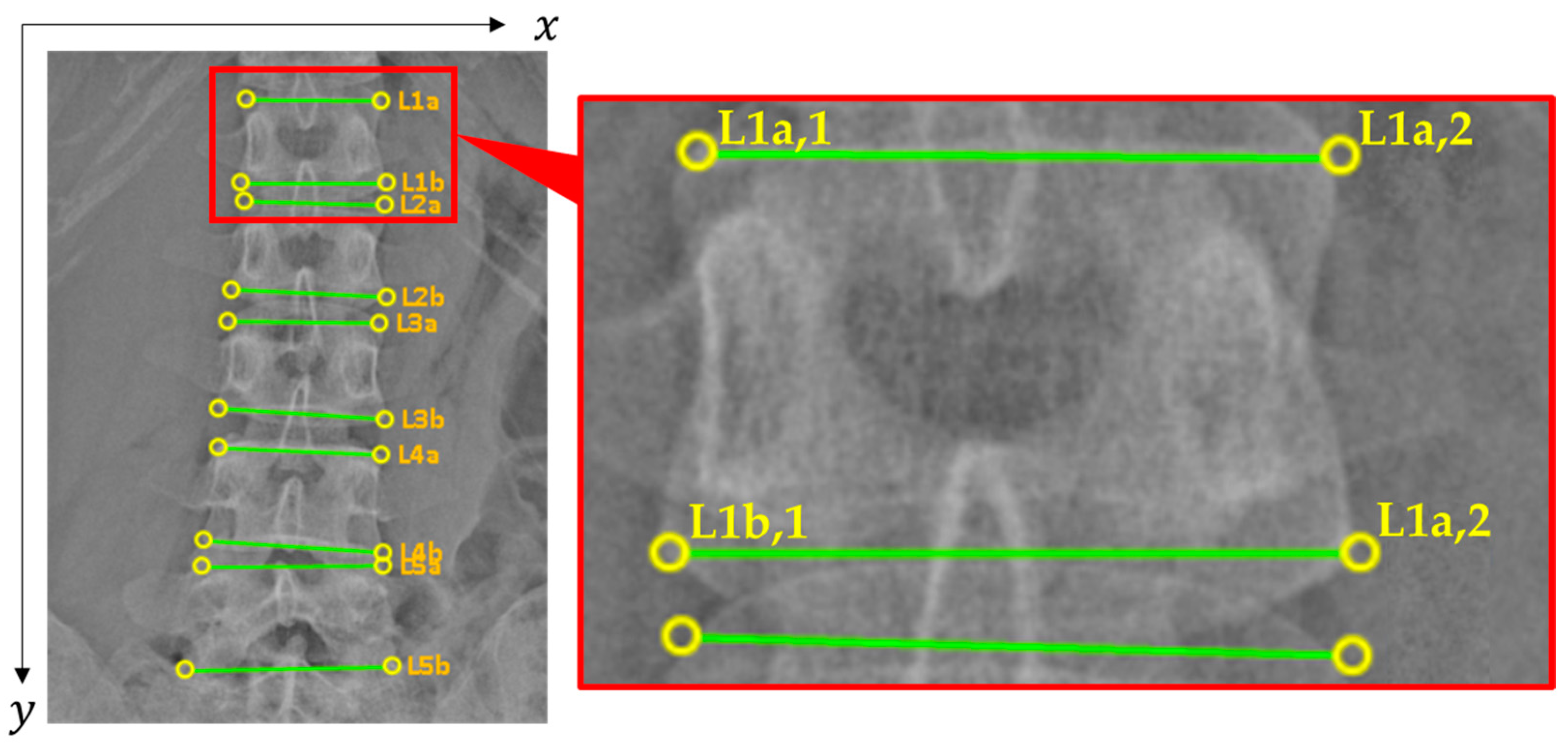
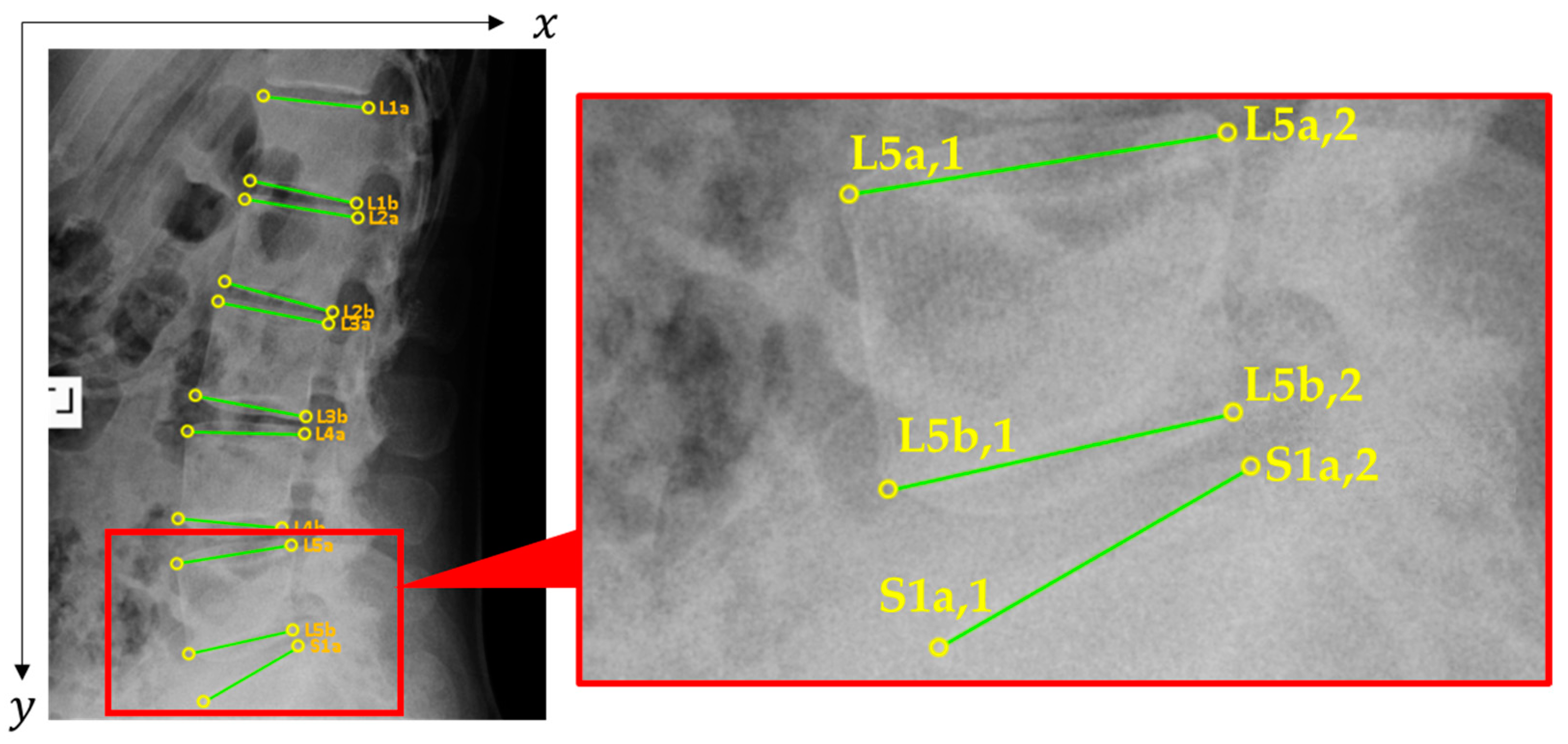
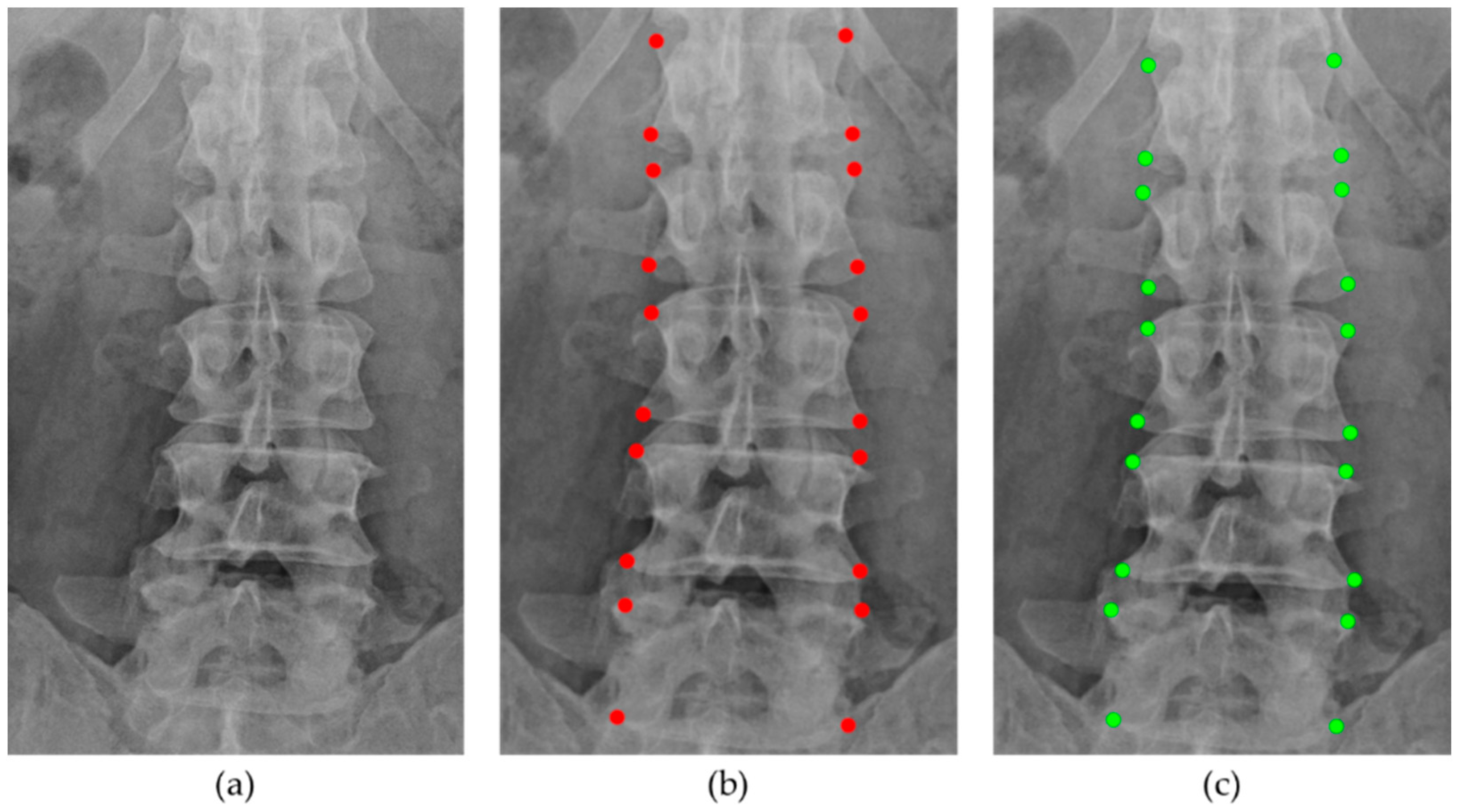
2.2.1. Vertebral Positions
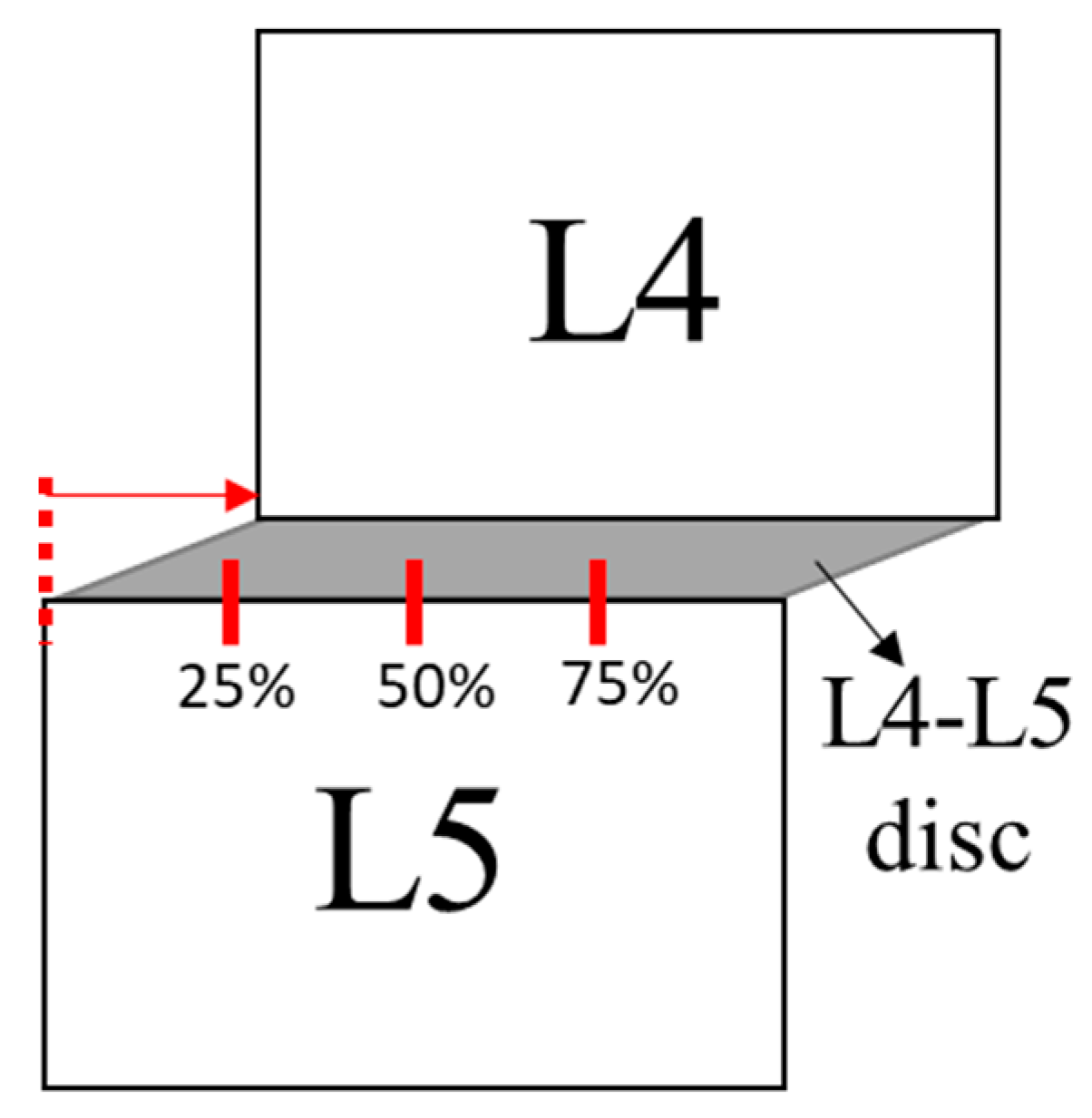
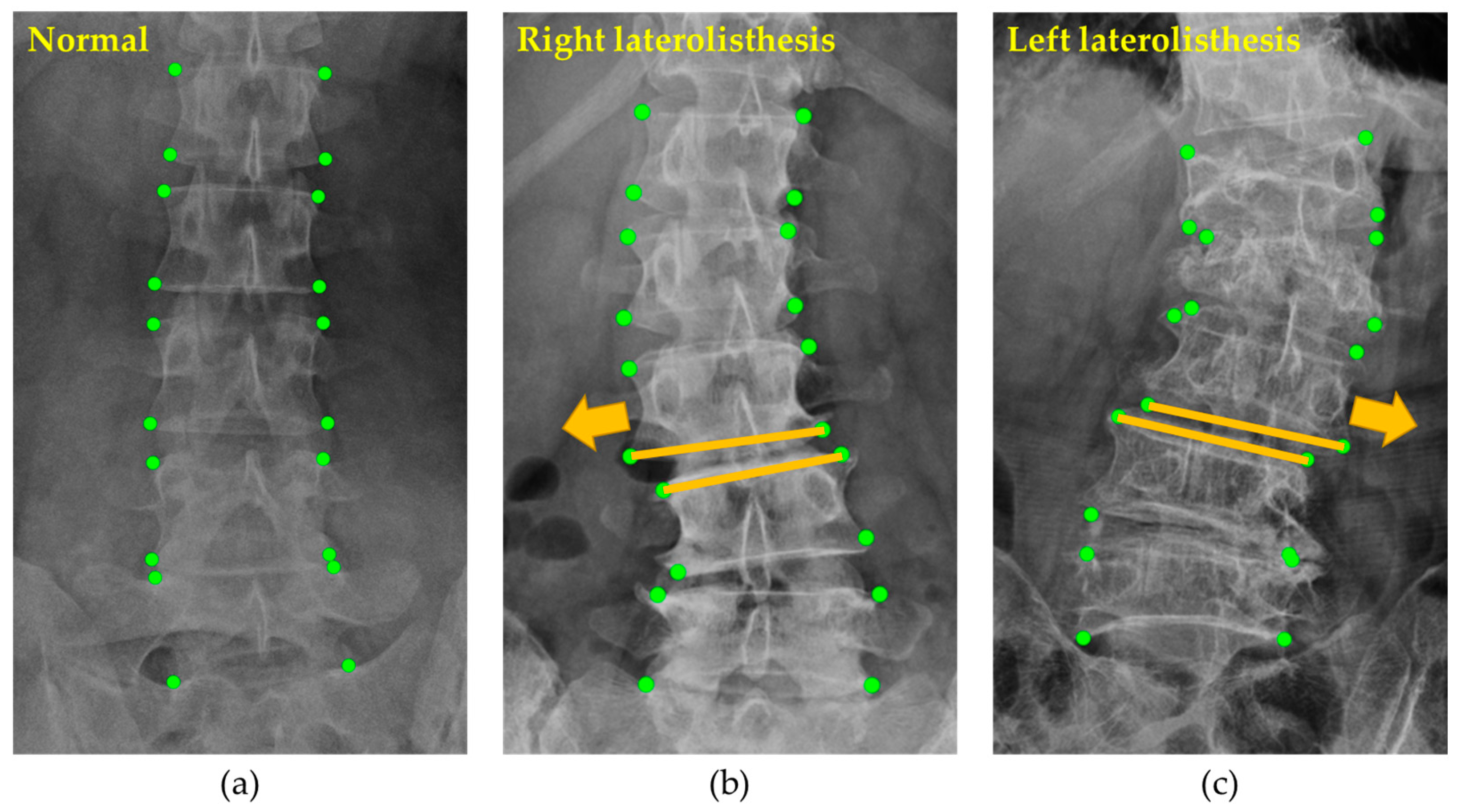
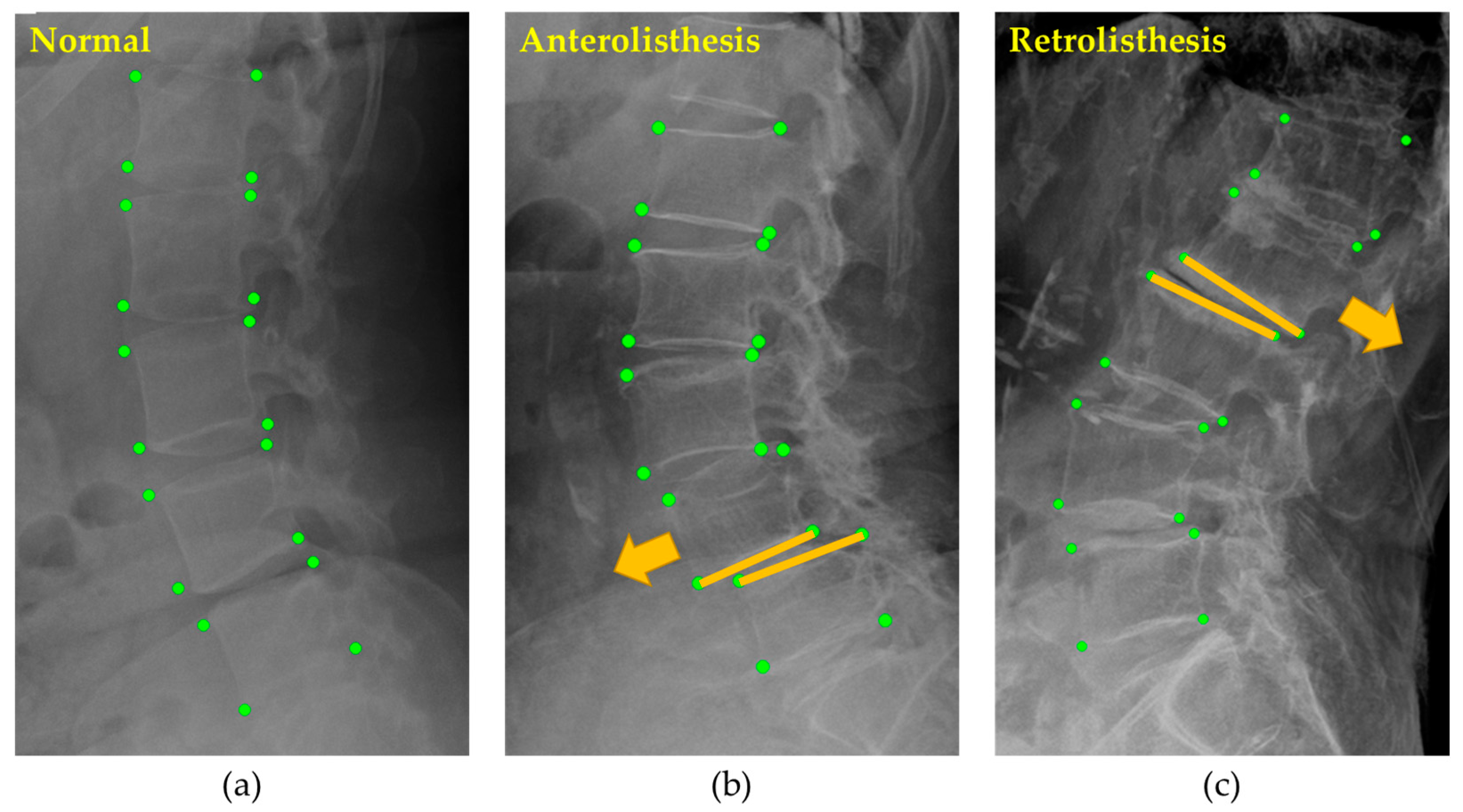
2.2.2. Spondylolisthesis
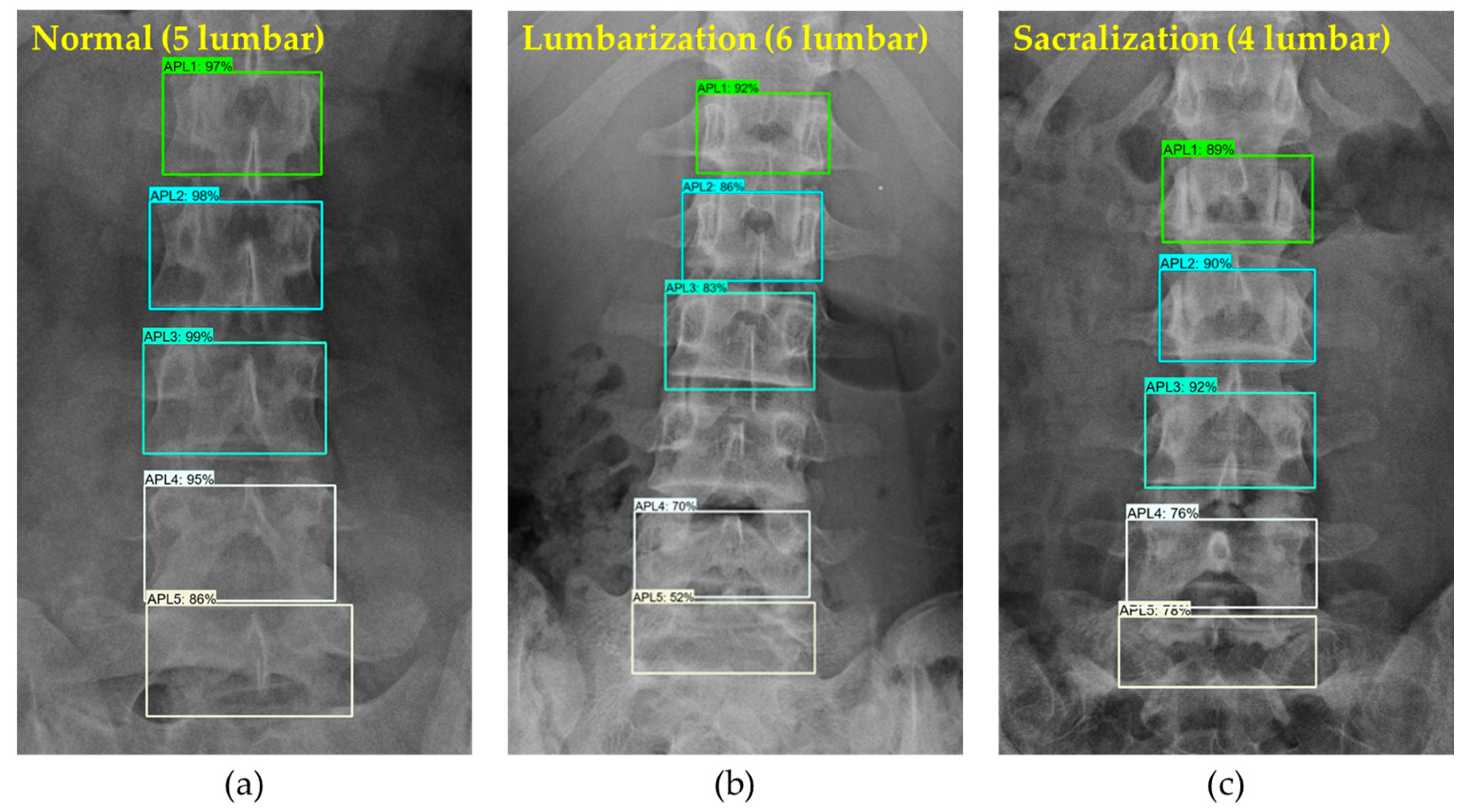
2.2.3. LSTV
2.3. Benefit of BUU-LSPINE
2.4. Experiments
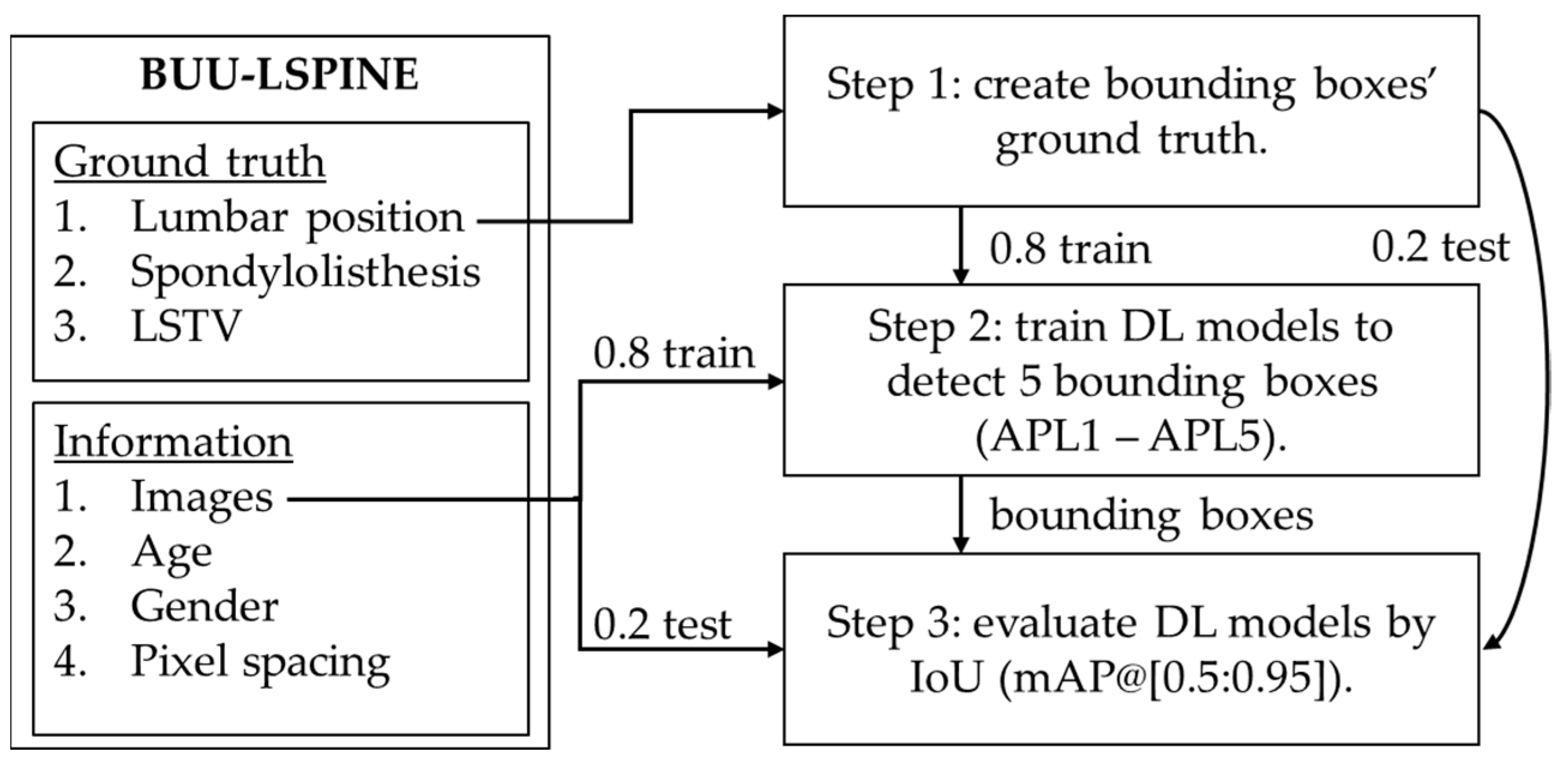
2.4.1. Lumbar Vertebrae Detection
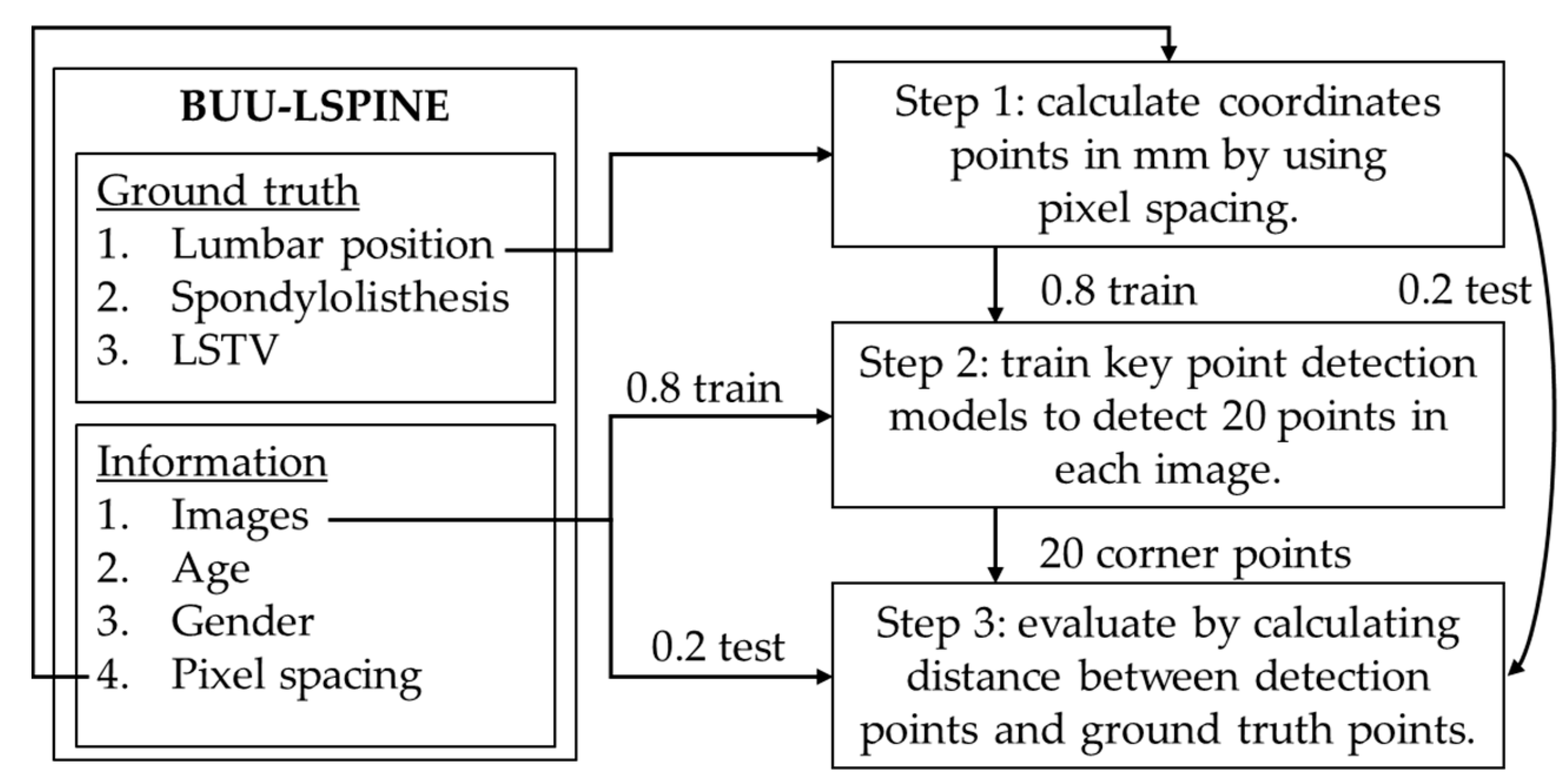
2.4.2. Vertebral Corner Points Extraction
2.4.3. Spondylolisthesis Prediction
3. Results
3.1. Lumbar Vertebrae Detection
3.2. Vertebral Corner Point Extraction
3.3. Spondylolisthesis Prediction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LSTV | Lumbosacral transitional vertebrae |
| AP | Anteroposterior |
| LA | Lateral |
| SVM | Support Vector Machine |
| CDSS | Clinical Decision Support System |
References
- Chan, A.K.; Sharma, V.; Robinson, L.C.; Mummaneni, P.V. Summary of guidelines for the treatment of lumbar spondylolisthesis. Neurosurg. Clin. 2019, 30, 353–364. [Google Scholar] [CrossRef]
- Beck, A.W.; Simpson, A.K. High-grade lumbar spondylolisthesis. Neurosurg. Clin. 2019, 30, 291–298. [Google Scholar] [CrossRef]
- Yamaguchi, K.T.; Skaggs, D.L.; Acevedo, D.C.; Myung, K.S.; Choi, P.; Andras, L. Spondylolysis is frequently missed by MRI in adolescents with back pain. J. Child. Orthop. 2012, 6, 237–240. [Google Scholar] [CrossRef] [Green Version]
- Kunze, K.N.; Lilly, D.T.; Khan, J.M.; Louie, P.K.; Ferguson, J.; Basques, B.A.; Nolte, M.T.; Dewald, C.J. High-grade spondylolisthesis in adults: Current concepts in evaluation and management. Int. J. Spine Surg. 2020, 14, 327–340. [Google Scholar] [CrossRef]
- Alqarni, A.M.; Schneiders, A.G.; Cook, C.E.; Hendrick, P.A. Clinical tests to diagnose lumbar spondylolysis and spondylolisthesis: A systematic review. Phys. Ther. Sport 2015, 16, 268–275. [Google Scholar] [CrossRef]
- Zhao, S.; Wu, X.; Chen, B.; Li, S. Automatic spondylolisthesis grading from MRIs across modalities using faster adversarial recognition network. Med. Image Anal. 2019, 58, 101533. [Google Scholar] [CrossRef]
- Nguyen, T.P.; Chae, D.-S.; Park, S.-J.; Kang, K.-Y.; Yoon, J. Deep learning system for Meyerding classification and segmental motion measurement in diagnosis of lumbar spondylolisthesis. Biomed. Signal Process. Control 2021, 65, 102371. [Google Scholar] [CrossRef]
- Varçın, F.; Erbay, H.; Çetin, E.; Çetin, İ.; Kültür, T. End-to-end computerized diagnosis of spondylolisthesis using only lumbar X-rays. J. Digit. Imaging 2021, 34, 85–95. [Google Scholar] [CrossRef]
- Fraiwan, M.; Audat, Z.; Fraiwan, L.; Manasreh, T. Using deep transfer learning to detect scoliosis and spondylolisthesis from X-ray images. PLoS ONE 2022, 17, e0267851. [Google Scholar] [CrossRef]
- Sekharappa, V.; Amritanand, R.; Krishnan, V.; David, K.S. Lumbosacral transition vertebra: Prevalence and its significance. Asian Spine J. 2014, 8, 51. [Google Scholar] [CrossRef] [Green Version]
- Li, X.; Morgan, P.S.; Ashburner, J.; Smith, J.; Rorden, C. The first step for neuroimaging data analysis: DICOM to NIfTI conversion. J. Neurosci. Methods 2016, 264, 47–56. [Google Scholar] [CrossRef]
- Hughes, R.J.; Saifuddin, A. Imaging of lumbosacral transitional vertebrae. Clin. Radiol. 2004, 59, 984–991. [Google Scholar] [CrossRef]
- Gopalan, B.; Yerramshetty, J.S. Lumbosacral transitional vertebra-related low back pain: Resolving the controversy. Asian Spine J. 2018, 12, 407. [Google Scholar] [CrossRef]
- McGrath, K.; Schmidt, E.; Rabah, N.; Abubakr, M.; Steinmetz, M. Clinical assessment and management of Bertolotti Syndrome: A review of the literature. Spine J. 2021, 21, 1286–1296. [Google Scholar] [CrossRef]
- Landauer, F.; Trieb, K. Diagnostic Limitations and Aspects of the Lumbosacral Transitional Vertebrae (LSTV). Appl. Sci. 2022, 12, 10830. [Google Scholar] [CrossRef]
- Molina, D.; Blumenthal, S. Chapter 13—Lumbosacral Spine Plain Radiographs. In Atlas of Spinal Imaging; Louie, P.K., An, H.S., Samartzis, D., Eds.; Elsevier: Amsterdam, The Netherlands, 2022; pp. 173–181. [Google Scholar] [CrossRef]
- Konin, G.; Walz, D. Lumbosacral transitional vertebrae: Classification, imaging findings, and clinical relevance. Am. J. Neuroradiol. 2010, 31, 1778–1786. [Google Scholar] [CrossRef] [Green Version]
- Deng, Y.; Wang, C.; Hui, Y.; Li, Q.; Li, J.; Luo, S.; Sun, M.; Quan, Q.; Yang, S.; Hao, Y. Ctspine1k: A large-scale dataset for spinal vertebrae segmentation in computed tomography. arXiv 2021, arXiv:2105.14711. [Google Scholar]
- Riddle, W.R.; Pickens, D.R. Extracting data from a DICOM file. Med. Phys. 2005, 32 Pt 1, 1537–1541. [Google Scholar] [CrossRef]
- Cai, Y.; Leung, S.; Warrington, J.; Pandey, S.; Shmuilovich, O.; Li, S. Direct spondylolisthesis identification and measurement in mr/ct using detectors trained by articulated parameterized spine model. In Proceedings of the Medical Imaging 2017: Image Processing, Orlando, FL, USA, 11–16 February 2017; pp. 362–369. [Google Scholar]
- Saravagi, D.; Agrawal, S.; Saravagi, M.; Rahman, M.H. Diagnosis of Lumbar Spondylolisthesis Using a Pruned CNN Model. Comput. Math. Methods Med. 2022, 2022, 2722315. [Google Scholar] [CrossRef]
- Liao, S.; Zhan, Y.; Dong, Z.; Yan, R.; Gong, L.; Zhou, X.S.; Salganicoff, M.; Fei, J. Automatic lumbar spondylolisthesis measurement in CT images. IEEE Trans. Med. Imaging 2016, 35, 1658–1669. [Google Scholar] [CrossRef]
- Trinh, G.M.; Shao, H.-C.; Hsieh, K.L.-C.; Lee, C.-Y.; Liu, H.-W.; Lai, C.-W.; Chou, S.-Y.; Tsai, P.-I.; Chen, K.-J.; Chang, F.-C. Detection of Lumbar Spondylolisthesis from X-ray Images Using Deep Learning Network. J. Clin. Med. 2022, 11, 5450. [Google Scholar] [CrossRef]
- Chu, C.; Belavy, D.L.; Armbrecht, G.; Bansmann, M.; Felsenberg, D.; Zheng, G. Annotated T2-Weighted Mr Images of the Lower Spine. Zenodo 2015. [Google Scholar] [CrossRef]
- Sekuboyina, A.; Husseini, M.E.; Bayat, A.; Löffler, M.; Liebl, H.; Li, H.; Tetteh, G.; Kukačka, J.; Payer, C.; Štern, D. VerSe: A vertebrae labelling and segmentation benchmark for multi-detector CT images. Med. Image Anal. 2021, 73, 102166. [Google Scholar] [CrossRef]
- Masood, R.F.; Hassan, T.; Raja, H.; Hassan, B.; Dias, J.; Werghi, N. A Composite Dataset of Lumbar Spine Images with Mid-Sagittal View Annotations and Clinically Significant Spinal Measurements. In Proceedings of the 2022 2nd International Conference on Digital Futures and Transformative Technologies (ICoDT2), Rawalpindi, Pakistan, 24–26 May 2022; pp. 1–5. [Google Scholar]
- Koslosky, E.; Gendelberg, D. Classification in brief: The Meyerding classification system of spondylolisthesis. Clin. Orthop. Relat. Res. 2020, 478, 1125. [Google Scholar] [CrossRef]






| No | Study | Source | Spondylolisthesis Diagnosis | Vertebra Position | LSTV Info | Number of Patients | View(s) |
|---|---|---|---|---|---|---|---|
| 1. | Zhao et al. [6] | Private | ✓ | ✓ | ✕ | 150 | LA |
| 2. | Saravagi et al. [21] | Private | ✓ | ✕ | ✕ | 337 | AP, LA |
| 3. | Liao et al. [22] | Private | ✓ | ✓ | ✕ | 558 | LA |
| 4. | Varçın et al. [8] | Private | ✓ | ✓ | ✕ | 600 | LA |
| 5. | Trinh et al. [23] | Private | ✓ | ✓ | ✕ | 706 | LA |
| 6. | Nguyen et al. [7] | Private | ✓ | ✓ | ✕ | 1000 | LA |
| 7. | Cai et al. [20] | Public | ✓ (synthesized) | ✕ | ✕ | 47 | LA |
| 8. | Fraiwan et al. [9] | Public | ✓ | ✕ | ✕ | 338 | AP |
| 9. | Chu et al. [24] | Public | ✕ | ✓ | ✕ | 23 | 3D |
| 10. | Sekuboyina et al. [25] | Public | ✕ | ✓ | ✕ | 355 | 3D |
| 11. | Masood et al. [26] | Public | ✕ | ✓ | ✕ | 514 | LA |
| 12. | Deng et al. [18] | Public | ✕ | ✓ | ✕ | 1005 | 3D |
| 13. | Our proposed dataset | Public | ✓ | ✓ | ✓ | 3600 | AP, LA |
| No | Field Name | Description | |
|---|---|---|---|
| 1. | Image Type | X-ray (PF) | |
| 2. | Image View | AP and LA | |
| 3. | Body Part | Lumbar spine (LSPINE) | |
| 4. | Total number of patients | 3600 patients | |
| 5. | Total number of images | 7200 images | |
| 6. | Total number of spondylolisthesis patients | 621 patients | |
| 7. | Total number of spondylolisthesis instances | 788 instances (Some patients include multiple instances) | |
| 8. | Datasets storage size | 18.5 GB | |
| 9. | Ground truth | Vertebral position, | |
| Spondylolisthesis diagnosis, | |||
| LSTV | |||
| 10. | Lumbar vertebral position targets | The coordinate corner points of L1 to L5 | |
| 11. | Spondylolisthesis diagnosis targets | Left laterolisthesis, | |
| Right laterolisthesis | |||
| Anterolisthesis | |||
| Retrolisthesis | |||
| 12. | LSTV targets | Sacralization, | |
| Lumbarization | |||
| 13. | File types | Images: .jpg | |
| Ground truth: .csv | |||
| 14. | Locations | Burapha University Hospital, Thailand | |
| 15. | Year period | 2000–2021 | |
| 16. | Age range | 6–97 years old | |
| 17. | Image dimensions | Height: 1434–3408 pixels, Width: 860–3040 pixels, Pixel Spacing: 0.125–0.175 mm | |
| 18. | X-ray imaging parameters | AP | kV: 70–75 kV mAs: 32–40 mAs |
| LA | kV: 80–90 kV mAs: 50–60 mAs | ||
| Line | x1 | y1 | x2 | y2 | Class |
|---|---|---|---|---|---|
| L1a | 876 | 167 | 1111 | 169 | ✕ 1 |
| L1b | 866 | 314 | 1120 | 314 | 0 |
| L2a | 871 | 344 | 1117 | 351 | ✕ 1 |
| L2b | 848 | 498 | 1120 | 511 | 0 |
| L3a | 842 | 553 | 1109 | 557 | ✕ 1 |
| L3b | 825 | 706 | 1118 | 725 | 0 |
| L4a | 826 | 775 | 1112 | 787 | ✕ 1 |
| L4b | 801 | 937 | 1114 | 958 | 0 |
| L5a | 798 | 983 | 1115 | 980 | ✕ 1 |
| L5b | 767 | 1164 | 1129 | 1158 | 0 |
| Line | x1 | y1 | x2 | y2 | Class |
|---|---|---|---|---|---|
| L1a | 609 | 353 | 827 | 377 | ✕ 1 |
| L1b | 581 | 529 | 802 | 577 | 0 |
| L2a | 570 | 568 | 805 | 607 | ✕ 1 |
| L2b | 527 | 743 | 752 | 805 | 0 |
| L3a | 513 | 785 | 744 | 830 | ✕ 1 |
| L3b | 467 | 982 | 696 | 1025 | 0 |
| L4a | 450 | 1057 | 693 | 1063 | ✕ 1 |
| L4b | 430 | 1239 | 648 | 1259 | 0 |
| L5a | 427 | 1334 | 667 | 1295 | ✕ 1 |
| L5b | 452 | 1523 | 670 | 1474 | 0 |
| S1a | 483 | 1624 | 682 | 1508 | 0 2 |
| Class | Diagnosis | Female | Male | Total | View |
|---|---|---|---|---|---|
| 0 | Normal | 22,276 | 12,936 | 35,212 | AP, LA |
| 1 | Left laterolisthesis | 44 | 17 | 61 | AP |
| 2 | Right laterolisthesis | 43 | 26 | 69 | AP |
| 3 | Anterolisthesis | 343 | 121 | 464 | LA |
| 4 | Retrolisthesis | 94 | 100 | 194 | LA |
| Class | Diagnosis | Female | Male | Total |
|---|---|---|---|---|
| 0 | Normal | 2181 | 1275 | 3456 |
| 20 | Lumbarization | 6 | 9 | 15 |
| 21 | Sacralization | 93 | 36 | 129 |
| Meyerding Classification | Percentage of Slip |
|---|---|
| Grade I | 0–25% |
| Grade II | 25–50% |
| Grade III | 50–75% |
| Grade IV | 75–100% |
| Grade V | >100% |
| Model | View | Mean Average Precision (%) | Recall | ||
|---|---|---|---|---|---|
| @IoU [0.5] | @IoU [0.75] | @IoU [0.5, 0.95] | |||
| YOLOv5 | AP | 96.68 | 95.86 | 81.93 | 95.82 |
| LA | 95.83 | 95.50 | 83.45 | 95.72 | |
| MobileNetV1 | AP | 90.70 | 88.57 | 75.77 | 80.81 |
| LA | 89.48 | 88.72 | 76.02 | 81.91 | |
| MobileNetV2 | AP | 93.26 | 89.95 | 77.63 | 82.19 |
| LA | 91.79 | 90.51 | 78.38 | 83.58 | |
| ResNet50V1 | AP | 92.22 | 90.08 | 77.70 | 81.43 |
| LA | 91.03 | 89.95 | 77.73 | 81.97 | |
| ResNet101V1 | AP | 89.26 | 86.42 | 71.80 | 76.68 |
| LA | 91.43 | 90.37 | 78.45 | 83.20 | |
| ReseNet152V1 | AP | 93.07 | 90.25 | 77.32 | 81.31 |
| LA | 92.76 | 91.55 | 78.53 | 82.80 | |
| EfficientDet D0 | AP | 93.69 | 90.46 | 75.86 | 79.90 |
| LA | 92.39 | 89.76 | 72.60 | 77.25 | |
| EfficientDet D1 | AP | 93.00 | 87.38 | 70.88 | 75.63 |
| LA | 92.79 | 91.11 | 76.08 | 79.92 | |
| Models | Average Error (Millimeter) | Average Error (% of Vertebra Width) | ||
|---|---|---|---|---|
| AP | LA | AP | LA | |
| MobileNetV1 | 5.10 | 5.56 | 9.72%ก | 13.71% |
| MobileNetV2 | 6.78 | 7.29 | 12.92% | 17.98% |
| ResNet50V1 | 5.59 | 6.37 | 10.65% | 15.71% |
| ResNet101V1 | 9.81 | 8.51 | 18.70% | 20.99% |
| ResNet152V1 | 5.85 | 5.86 | 11.15% | 14.45% |
| ResNet50V2 | 5.27 | 5.83 | 10.05% | 14.38% |
| ResNet101V2 | 5.48 | 6.15 | 10.45% | 15.17% |
| ResNet152V2 | 4.63 | 5.41 | 8.83% | 13.34% |
| DenseNet201 | 4.77 | 4.91 | 9.09% | 12.11% |
| EfficientNetB0 | 143.80 | 240.38 | 274.17% | 592.94% |
| EfficientNetB1 | 26.67 | 71.82 | 50.85% | 177.16% |
| Classifier | View | Accuracy (%) | |
|---|---|---|---|
| Training Set | Testing Set | ||
| Decision Tree | AP | 100.00% | 92.77% |
| LA | 100.00% | 77.38% | |
| XGBoost | AP | 100.00% | 94.87% |
| LA | 100.00% | 86.41% | |
| SVM | AP | 99.95% | 95.14% |
| LA | 96.48% | 92.26% | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klinwichit, P.; Yookwan, W.; Limchareon, S.; Chinnasarn, K.; Jang, J.-S.; Onuean, A. BUU-LSPINE: A Thai Open Lumbar Spine Dataset for Spondylolisthesis Detection. Appl. Sci. 2023, 13, 8646. https://doi.org/10.3390/app13158646
Klinwichit P, Yookwan W, Limchareon S, Chinnasarn K, Jang J-S, Onuean A. BUU-LSPINE: A Thai Open Lumbar Spine Dataset for Spondylolisthesis Detection. Applied Sciences. 2023; 13(15):8646. https://doi.org/10.3390/app13158646
Chicago/Turabian StyleKlinwichit, Podchara, Watcharaphong Yookwan, Sornsupha Limchareon, Krisana Chinnasarn, Jun-Su Jang, and Athita Onuean. 2023. "BUU-LSPINE: A Thai Open Lumbar Spine Dataset for Spondylolisthesis Detection" Applied Sciences 13, no. 15: 8646. https://doi.org/10.3390/app13158646
APA StyleKlinwichit, P., Yookwan, W., Limchareon, S., Chinnasarn, K., Jang, J.-S., & Onuean, A. (2023). BUU-LSPINE: A Thai Open Lumbar Spine Dataset for Spondylolisthesis Detection. Applied Sciences, 13(15), 8646. https://doi.org/10.3390/app13158646







