Abstract
Aging can have a negative impact on the perioral region, affecting both appearance and self-esteem. Dentists offer various treatment options to address these changes, using surgical and non-surgical techniques. One such technique is facial filling with hyaluronic acid, a minimally invasive approach to improve the perioral region’s function and aesthetics and counteract aging effects. A literature review was conducted to collect scientific evidence on the subject, utilizing the mnemonic PI(C)O to refine the research question. The search for articles was accomplished on the EBSCOhost platform, specifically targeting those published between January 2009 and April 2023 in MEDLINE Complete, CINAHL Complete, and MedicLatina databases. Sixteen articles were carefully chosen, and the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) method were followed throughout the process. The major findings reported in the selected articles suggest that using hyaluronic acid as a mechanism to mitigate the effects of face lower third aging following orofacial harmonization procedures in dentistry offers significant benefits to patients, improving the aesthetic appearance of the face, increasing patients’ self-esteem and satisfaction, and providing a better quality of life. Nevertheless, a weak evidence level was found in the selected articles due to methodological issues, highlighting the need to increase the methodological quality of future studies.
1. Introduction
Human aging refers to the natural, gradual, and irreversible physiological and psychological changes in individuals as they progress through their lifespans. It encompasses a wide range of biological processes that lead to a decline in various bodily functions and an increased vulnerability to age-related diseases and illnesses. As people age, cells, tissues, and organs undergo degenerative changes, reducing their strength, flexibility, and overall vitality. Additionally, aging is often accompanied by cognitive decline, decreased sensory perception, and increased susceptibility to chronic conditions. While aging is a universal phenomenon, the rate and expression of these changes can vary among individuals due to genetic, lifestyle, and environmental factors [1].
The face is a visible reflection of human aging. The various changes in the face resulting from the overall aging process include the development of wrinkles and folds, fine lines, age spots, poor skin tone and texture, loss of skin elasticity and firmness, and imbalanced distribution of soft tissues. The underlying structures of the face, such as the subcutaneous cellular tissue areas and facial muscles, also change, leading to a loss of volume, sagging, and changes in facial contours [2,3]. Furthermore, signs of face wear can affect interpersonal relationships in various ways, such as influencing perceived character or personality traits and contributing to erroneously projected emotions that may not reflect the individual’s true feelings [4,5].
Non-surgical and minimally invasive options are increasingly being used to promote facial rejuvenation. Topical or laser-based therapies are insufficient to allow for volumetric rejuvenation, so the use of Botox and dermal fillers have gained increased notoriety by helping reduce the appearance of wrinkles, fine lines, and sagging skin, thus providing a more refreshed and youthful appearance of the face [6,7]. The burst in popularity of Botox and dermal fillers, the increasing patient population, and the need for quick solutions and long-lasting results have led to an increase in practitioners operating in the facial rejuvenation field. For example, dermatologists and plastic surgeons are health professionals that provide many therapeutic options in this field [8,9,10].
The aging of the perioral region is also a dentist’s professional activity sector [11], and “orofacial harmonization” is one of its professional abilities already considered in Portuguese law [12], encompassing techniques, procedures, and products with therapeutic, rehabilitation, or even prevention applications, such as botulinum toxin (Botox) or hyaluronic acid (HA). Depending on their expertise and training, dentists are health professionals who can offer non-surgical facial treatments using Botox (it freezes muscle) and HA (a dermal filler that gives fullness to the muscle) to address fine lines and wrinkles around the mouth and jaw area [13,14]. Dentists can also improve facial aesthetics in conjunction with the application of dental procedures such as dental implants, orthodontic treatments, or oral rehabilitation, which contribute to a more balanced and harmonious facial appearance [15,16].
Due to its therapeutic benefits, Botox is frequently employed in managing temporomandibular joint disorder (TMJD) and facial pain within the oral maxillofacial region. Injecting Botox into specific muscles can effectively relax the affected areas, relieving muscle spasms and reducing pain associated with TMJD. Additionally, Botox has effectively alleviated chronic facial pain, such as trigeminal neuralgia and myofascial pain syndrome. Moreover, Botox finds utility in dental aesthetics, as it can enhance smile aesthetics by targeting the muscles responsible for excessive gingival display or gummy smiles. Furthermore, it can aid therapeutic dental treatments by minimizing muscle contractions during orthodontic adjustments or prosthodontic rehabilitation procedures [13,14,17].
In dentistry, fillers, such as HA, are commonly employed to address various aesthetic and functional concerns. One area where fillers find utility is in treating a gummy smile, which occurs when an excessive amount of gum tissue is exposed while smiling. By strategically injecting fillers in the upper lip or around the gum line, the appearance of a gummy smile can be minimized, creating a more balanced and harmonious smile. Fillers are also used during gingivectomy procedures, where excess gum tissue is removed to enhance the smile’s aesthetics or facilitate better oral hygiene. Moreover, fillers can aid in periodontal and implant surgeries by supporting and shaping the soft tissues around the affected area, aiding in proper healing and optimal implant placement. Additionally, fillers can enhance lip and perioral volume, allowing patients to achieve fuller and more youthful-looking lips and address fine lines and wrinkles in the surrounding areas. Overall, fillers are versatile in dentistry, contributing to functional [18] and cosmetic treatment approaches [17,19,20].
Although there is no preferred strategy in dentistry regarding the use of Botox and dermal fillers such as HA, as it depends on the specific treatment goals and the patient’s needs, the latter is one of the most popular aesthetic procedures performed in the USA, mainly aiming to mitigate wrinkles and folds around the mouth, at the jawline, and at the chin, which occur due to facial aging [21], and it is also considered an increasingly popular facial rejuvenation modality (the second most common non-surgical aesthetic procedure performed) [7]. HA has unique physicochemical properties (hygroscopicity and viscoelasticity) and distinctive biological functions [20], improving the appearance of the lips and filling wrinkles, creases, and areas that have lost volume, such as the perioral and periorbital regions, helping to restore desired facial contours [6,7,22].
The scientific literature on the application of HA by dentists to mitigate the effects of facial aging in the perioral region is relatively scarce, even though this strategy is emerging as a promising one in facial rejuvenation to be exploited by these health professionals. Thus, this research aimed to conduct an integrative literature review to bring out the scientific evidence about the benefits of the application of HA by dentists as a strategy for facial rejuvenation to compensate for the consequences of aging, more particularly of the facial lower third, improving the aesthetic appearance of the face and increasing the patient’s self-esteem. It also aims to identify possible limitations in the existing literature and future research areas to help guide clinical practice in orofacial harmonization in dentistry. By synthesizing the findings of multiple studies, the authors believe that researchers can identify practical implications, best practices, or recommendations that can inform decision-making in real-world contexts.
2. Materials and Methods
This integrative literature review synthesized and analyzed research studies on the use of HA as a strategy to mitigate the effects of face lower third aging in dentistry to provide a comprehensive and cohesive understanding of the subject. The following methodological steps were taken as proposed by Mota de Sousa et al. [23]: (i) identifying the research question; (ii) defining the studies’ inclusion and exclusion criteria; (iii) defining the information to be extracted from the studies; (iv) analyzing the included articles; (v) presenting and discussing the results; and (vi) synthesizing the findings.
To start with, as the first methodological step, the following background research question was formulated: “The clinical application of hyaluronic acid plays a decisive role as a method to mitigate the aging in the soft tissues of the perioral area of the face, more, in particular, its lower third?”
This research question was then reformulated recurring to the PI(C)O methodology, which includes categories intended to be addressed in this integrative literature review, where “P” corresponds to Population, “I” to Intervention, “C” refers to Comparison/Control, and “O” to Outcomes. Based on this, the following foreground research question was formulated: “What are the gains obtained in terms of facial rejuvenation and harmonization (Outcomes) with hyaluronic acid filling of the soft tissues of the perioral region (Intervention) in people with anatomical aging of the facial lower third (Population)?”
Concerning the second methodological step, the following inclusion and exclusion criteria were established: (i) inclusion: (a) articles published between January 2009 and April 2023; (b) with full text available; (c) written in English, Portuguese, and Italian languages; (d) whose sample considered is composed only of human beings; and (e) addresses the efficacy of using hyaluronic acid to mitigate the effects of aging of the facial lower third; and (ii) exclusion: all articles that do not meet the five requirements mentioned for the inclusion criteria.
Once the PI(C)O research question had been formulated, data were collected during April 2023 through the EBSCOhost platform, with MEDLINE complete, CINAHL complete, and MedicLatina databases. The following descriptors were used: “old”, “elderly”, “aged”, “adult”, “hyaluronic acid”, “filler”, “dermal filler”, “dermal”, “dental”, “dentist”, “dentistry”, “face”, and “facial”. These descriptors were organized using the Boolean operators OR and AND as follows:
(old OR elderly OR aged OR adult) AND (hyaluronic acid OR filler OR dermal filler OR dermal) AND (dental OR dentist OR dentistry) AND (face OR facial).
For the article selection task, a first reading of their title and abstract was carried out to verify if there was consensus regarding their inclusion and/or exclusion, following the pre-defined criteria. If the title and abstract were of interest or inconclusive, the entire document was read to minimize the loss of valuable information for the study. If the article was interesting for the study, it was then included.
3. Results
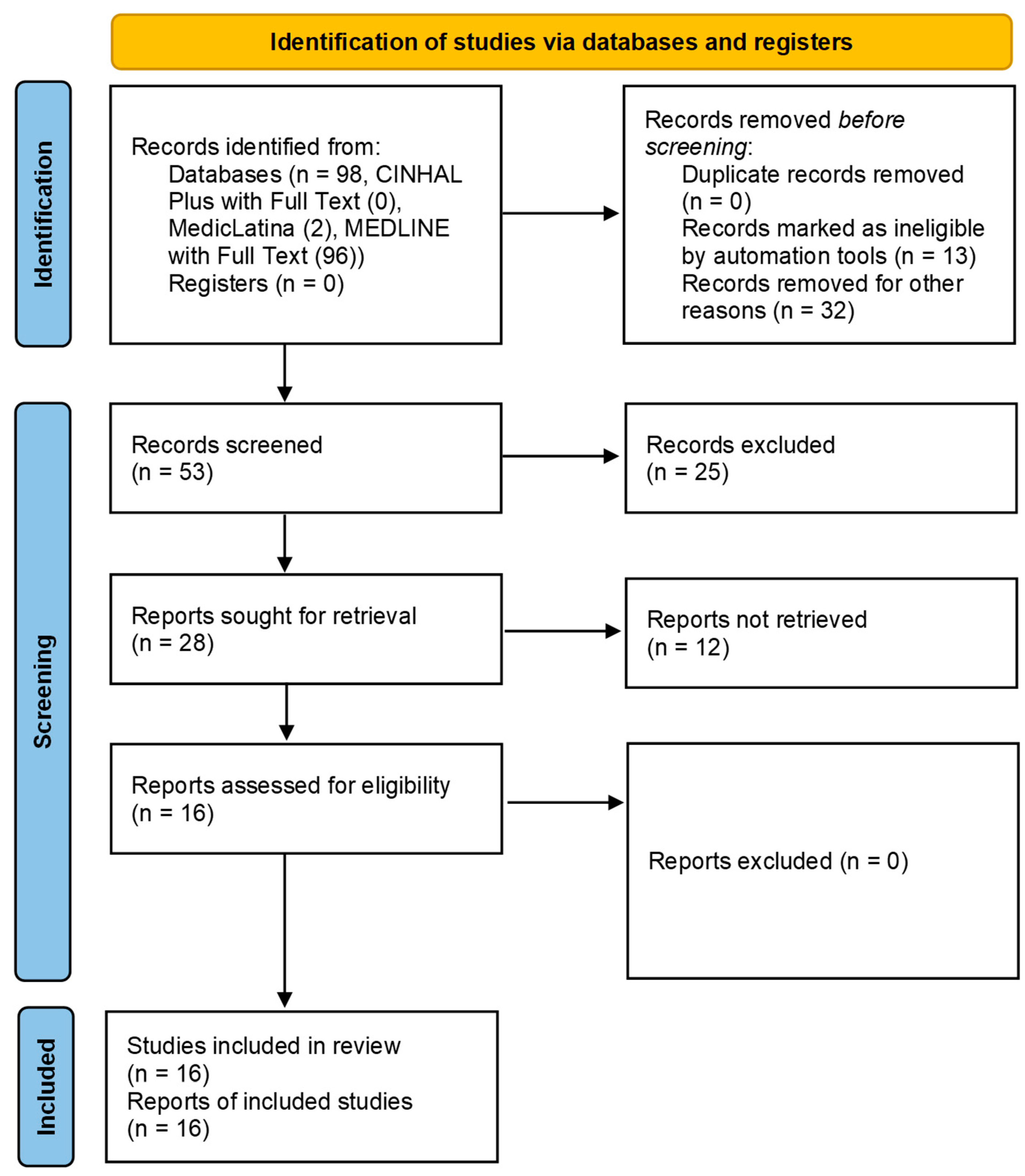
The search conducted in the databases mentioned above resulted in 98 articles. After eliminating 45 articles, of which 13 were considered duplicates and 32 did not meet the inclusion criteria, 53 articles were screened, from which the respective titles and abstracts were extracted for analysis. After reading their titles/abstracts, 25 articles were eliminated since they did not fit the study’s subject. Then, 28 articles were sought for retrieval and selected for full-text analysis, with 12 being unable to be retrieved, preventing the full reading of the text. Finally, 16 articles were included in the present integrative review. The flow chart representing the research pathway is shown in Figure 1, using the PRISMA flow diagram [24].
Figure 1.
PRISMA flow diagram representing the research pathway.
The 16 eligible articles were read in full, and their content was analyzed to meet the goals proposed in this integrative literature review. The features and main findings are summarized in Table 1, in descending chronological order of publication.

Table 1.
Article identification and main results.
4. Discussion
Overall, the articles eligible for this review provided consistent results that support the use of HA to mitigate the signs of aging of the facial lower third. They also reported benefits of its use, such as volume enhancement, wrinkle reduction, and restoration of facial harmony, which seem to improve patients’ self-esteem and quality of life [38]. In addition, the use of HA was found to be a safe and minimally invasive technique with low complication rates.
This discussion is structured in sections, defined after grouping the articles according to their context and content. It will focus on applying the different therapeutic strategies that emerged during the review in the dentistry context.
4.1. Non-Surgical Modalities and Various Applicabilities of HA in Dentistry
Li et al. [26] showed consistent positive outcomes of non-surgical approaches, such as botulinum toxin and dermal fillers, in mitigating signs of facial aging. The interventions effectively reduced wrinkles and expression lines and restored facial volume while improving skin texture and tone. The authors emphasized the significance of personalized treatment planning and careful patient selection to achieve optimal results and minimize potential adverse effects. These findings underscore the importance of non-surgical methods as valuable options for mitigating facial aging, with dentists playing a crucial role in providing these treatments to patients.
Casale et al. [19] highlighted that HA possesses anti-inflammatory, antibacterial, and tissue-regenerating properties, which are valuable in dental specialties like periodontics, endodontics, and orthodontics. The versatility of HA and its ability to promote tissue regeneration make it a valuable material for non-surgical treatments in dentistry. The positive results and properties identified in the study support the increasing demand for HA and establish it as a promising therapeutic option for dental professionals.
Shuai et al. [30] conducted a survey in China to examine the public’s preference for non-invasive facial rejuvenation methods, specifically dermal fillers with HA and neurotoxins. The reported results showed that more than half of the respondents had chosen some non-invasive facial rejuvenation, with dermal fillers being the most popular technique. These findings suggest a growing demand for non-surgical approaches like HA-based treatments as alternatives to invasive methods. It was also found that the primary motivation for individuals seeking these treatments was to enhance their appearance, highlighting the importance of facial aesthetics in decision-making. Safety played a crucial role in treatment selection, with patients favoring non-invasive options that provide effective results with minimal risk. However, the authors reported a relatively low awareness and knowledge among the public regarding non-invasive facial rejuvenation procedures that dental practitioners can perform. Most people relied on advertising to learn about these techniques, indicating the need for better education and professional outreach to raise awareness about available options. Other authors such as Chaput et al. [35], Spatafora et al. [34], Zupi [33], and Tran Cao [31] also corroborate the findings reported by Shuai et al. [30], reinforcing the growing popularity of HA and other non-surgical modalities requested of dentists by patients, which is directly related to the search for satisfactory aesthetic results, low rates of complication and significant adverse effects, and shorter recovery time, thus avoiding invasive surgical procedures.
In sum, these studies show that HA is becoming more popular in dental medicine as a non-surgical treatment option. It offers aesthetic benefits, anti-inflammatory and antibacterial properties, and tissue-regeneration capabilities. Additionally, the public prefers non-invasive treatments. Therefore, dental professionals should consider integrating HA into their practices to meet patient needs and achieve better results.
4.2. Dentists as Specialists
In the study published by Tran Cao [31], the use of botulinum toxin and dermal fillers in dentistry to enhance patient attractiveness was explored. The author examined the historical and current applications of these treatments in facial aesthetics, their administration techniques, potential implications for dentistry, and the role of dentists in providing these treatments. The study found a growing demand for botulinum toxin and dermal fillers in dentistry as more dentists incorporate them into their practices to improve patients’ perceived attractiveness, confidence, quality of life, and satisfaction. However, the need for proper training of dentists and awareness of potential risks associated with these treatments was also highlighted.
Zupi [33] focused his study on the benefits of using HA fillers in dentistry. His research highlighted how these fillers could improve the outcomes of aesthetic dental treatments, leading to greater patient satisfaction and compliance. The HA fillers effectively restore volume to facial areas lost due to aging or other factors, improving facial harmony and overall appearance. The study highlighted the dentists’ expertise in facial anatomy, pain management, and orofacial harmonization procedures. The author also highlights the importance of adequately training dentists on the latest techniques, materials, and approaches to ensure optimal results and patient satisfaction [39,40].
Spatafora et al. [34] provide, in their research, valuable information about the role of dentists in aesthetic procedures within dentistry, as do the findings published by Zupi [33] and Tran Cao [31]. The study emphasizes the increasing recognition and appreciation of dentists’ ability to provide integrated care based on scientific knowledge and advanced techniques. Dentists’ understanding of facial structure enables them to achieve aesthetic and functional harmony, restoring lost volume and improving patients’ attractiveness. However, dentists’ involvement in non-surgical aesthetic modalities raises essential legal and ethical considerations. The study highlights the importance of dentists being aware of and adhering to regulations, guidelines, legal restrictions, ethical standards, and specific professional practices related to aesthetic treatments. The need for ongoing training and education for dentists interested in incorporating aesthetic treatments into their practices is also highlighted, along with the importance of these health professionals holding a sound background covering both technical aspects and legal/ethical considerations in dental practice.
The abovementioned findings are also supported by Chaput et al. [35], who shed light on the legal regulations surrounding the use of dermal fillers, specifically HA, by dentists in France. The authors report that dentists possess the necessary knowledge and expertise to perform aesthetic treatments with dermal fillers, which suggests adequate training for these procedures. The discussion emphasizes the impact of these regulations on dentistry as they establish guidelines for dentists offering these treatments. When integrating the results stated by Chaput et al. [35] with those reported by Spatafora et al. [34], Zupi [33], and Tran Cao [31], it is evident that dentists are recognized for their expertise in orofacial harmonization. However, legal regulations underscore the importance of ethical and legal standards compliance.
In Portugal, the dentist is a health professional who is qualified to carry out all courses of action that are necessary or appropriate for the prevention, diagnosis, and treatment of anomalies and diseases of the teeth, mouth, jaws, and attached structures and tissues concerning the stomatognathic system. Orofacial harmonization is one of the dentist’s professional competencies already included in the legal regulations published in the Portuguese Official Gazette [12], encompassing techniques, procedures, and products with therapeutic, rehabilitative, or even preventive applications in dentistry, using injectable products such as botulinum toxin or HA [41]. This legal recognition reinforces the dentist’s authority and responsibility in performing these procedures and highlights the importance of their training and expertise in orofacial harmonization.
4.3. Pharmacodynamics of HA
Bukhari et al. [32] explore the pharmacodynamics and rheological characteristics of HA in skin rejuvenation and aesthetic procedures. HA can retain water, improve skin hydration, and act as a dermal filler to reduce wrinkles and enhance skin elasticity. Understanding the rheological properties of HA is crucial in predicting its effectiveness, integration into the skin, response to facial expressions, and gradual dissipation of clinical effects, as stated by Dastoor et al. [36]. Both studies emphasize how analyzing these properties helps physicians select the right product, determine injection techniques and volume, and optimize aesthetic results, safety, and patient satisfaction. When administered correctly by qualified professionals, HA has proven benefits in skin rejuvenation, wrinkle filling, hydration increase, and improved skin elasticity, findings that are also corroborated by Wang et al. [42], Gavard Molliard et al. [43], and Fagien et al. [44].
Other studies also broadly support the above findings, highlighting that the pharmacodynamics of HA in non-surgical aesthetic procedures, coupled with proper administration techniques, offer significant benefits in skin rejuvenation. This understanding reinforces the importance of HA as a viable option in dentistry and highlights the need for specialization of healthcare professionals (dentists) to ensure satisfactory aesthetic outcomes for patients [45,46,47]. Additionally, for a complete and integrated approach to facial aesthetic rehabilitation, it becomes necessary to start from the assessment of several facial parameters, namely: (i) face shape, appearance, and position of soft tissues (such as the nose, lips, and chin) and supporting structures (bones, cartilage, and teeth); (ii) muscle activity; and (iii) aging, i.e., the way these tissues have or will age [33,48,49].
4.4. Skin Aging
Rogerio et al. [28] introduce the Mimicking Intraoral Mucosal Tissues (MIMT) concept in orofacial aesthetics. This concept aims to replicate the characteristics and properties of oral mucosal tissues in dental procedures and restoration. By using materials and techniques that mimic the natural tissues of the mouth, dental professionals can achieve more natural aesthetic results, where restoration and prosthetics blend seamlessly with the surrounding tissues. Mimicking the characteristics of intraoral tissues, such as texture, color, and elasticity, the materials used in dental procedures can provide greater comfort and adaptation for patients. In addition, the authors suggest that incorporating dermal HA fillers, such as those in the Restylane® product line, along with the MIMT concept, can provide natural and long-lasting results in orofacial rejuvenation, as they consider the unique qualities of intraoral mucosal tissues.
Hong [25], meanwhile, proposes different aesthetic techniques that use botulinum toxin and/or dermal fillers in the oral and maxillofacial area. The author analyzes the relevant anatomy and physiology of the muscles and skin of the region and discusses the various aesthetic approaches in which botulinum toxin and dermal fillers can be used. The study highlights that botulinum toxin and HA are safe and effective options for treating the oral and maxillofacial area and can produce optimal aesthetic results for patients.
Silva et al. [29] discuss the suggestions for using HA in different areas of the perioral region, lips, and jaw and describe injection techniques to achieve a more youthful and balanced facial appearance. In addition, the article highlights the possible side effects of HA, such as edema, hematomas, infection, and vascular complications, so recommendations are provided to minimize these risks and ensure safe and effective application, as reported in other research studies [50,51,52,53,54]. The authors also highlight that facial filler with HA has been established as an effective and safe intervention because it is a biocompatible substance that occurs naturally in the body, which minimizes the risk of adverse reactions and increases patient acceptance of the treatment, as reported by other researchers [53,55,56,57].
According to Raschke et al. [11], changes in the perioral region that occur with aging are evaluated using anthropometric measurements. The sample consisted of seventy individuals of different ages and gender, and age-related changes in perioral morphology were identified. These changes included decreased lip height and thickness, increased philtrum depth, decreased chin projection, and increased vertical distance between the lower lip and chin. The study aimed to provide a better understanding of how the perioral region changes with age and its clinical implications for aesthetic and reconstructive procedures in this area. The authors also discussed their findings’ clinical implications, suggesting that dermal fillers, fat grafting, or surgical procedures could restore a youthful appearance in the perioral region.
The research studies by Kapoor et al. [58], Rauso et al. [59], Hernandez et al. [60], and Islam et al. [61] also address different aspects of skin aging and the aesthetic approaches used for facial rejuvenation, adding evidence that HA and botulinum toxin are safe and effective options in dentistry for facial rejuvenation, thus supporting the abovementioned findings. These fillers can fill wrinkles, increase skin hydration, improve elasticity, and provide a more youthful and balanced appearance. The studies report the importance of recognizing the anatomy and physiology of the oral and maxillofacial region and the appropriate application techniques to achieve optimal aesthetic results. Moreover, it is emphasized that using these fillers in combination with other procedures can potentiate the effects and achieve satisfactory patient results.
4.5. Skin and Lip Rejuvenation
Dantas et al. [27] aimed to assess the safety and effectiveness of using hyaluronic acid (HA) for enhancing the lips’ appearance. The researchers discussed the process of injecting HA into the lips, explored various HA formulations available, and examined the potential benefits and risks associated with this treatment. Furthermore, the study compared the attractiveness of lips with different thicknesses after undergoing hyaluronic acid fillers, as perceived by dental surgeons, facial harmonization specialists, and laypersons. The results demonstrated that HA injections were a safe and effective method for rejuvenating the lips. The treatment significantly improved lip volume, contour, and overall appearance, with a low risk of adverse effects. Heidekrueger et al. [62], Pascali et al. [63], and Kau et al. [64] also corroborated the findings reported by Dantas et al. [27], suggesting that HA injections can be a valuable tool to improve smile attractiveness that is affected by the lips, gums, and teeth and increase patient satisfaction with their facial aesthetics with the result that lip augmentation has become increasingly popular in recent years as a reflection of cultural trends that emphasize youth and beauty. However, it is poorly understood whether lip thickness before filling may favor greater attractiveness after the procedure, so the authors studied this phenomenon of interest.
Perenack [37] examines the impact of aging on lip structure and its implications for oral aesthetics. The article discusses various treatment options to enhance the appearance of aging lips, including injectable lip augmentation fillers, lip lift surgeries, and maxillofacial surgery. Injectable fillers are highlighted as a minimally invasive technique that can effectively improve the look of the lips and perioral region. The study also mentions using fillers to address concerns like nasolabial folds and marionette lines, which are common aesthetic issues for patients. Furthermore, it refers to several recent studies that explore different techniques and therapeutic approaches to rejuvenate the lips and perioral region [26,65,66].
The study by Aubry et al. [10] explored the effectiveness of HA in treating facial aging in fully edentulous patients. The research involved 45 randomly assigned participants to receive either HA injections in the facial region (intervention group) or placebo injections (control group). The findings demonstrated that HA injections successfully enhanced facial wrinkles, skin hydration, and overall appearance in fully edentulous patients. The intervention group experienced significant improvements in the severity of facial wrinkles and skin hydration level compared to the control group. Other studies, including those published by Hegde [67], Cervino et al. [68], van Loghem et al. [69], and Hakobyan et al. [70], also supported the use of HA injections in edentulous patients, emphasizing its safety and tolerability without any serious adverse events reported. The authors of these studies suggested that HA injections could serve as a safe and effective alternative or complementary treatment to traditional dental prostheses for enhancing oral and facial health in fully edentulous patients. Furthermore, dentistry has begun exploring the use of HA as an adjuvant in the healing processes following titanium implant insertion, utilizing its advantageous chemical properties such as hygroscopicity, viscoelasticity, space-filling ability, bacteriostatic effect, anti-edema effect, antioxidant effect, biocompatibility, and non-immunogenicity.
4.6. Further Considerations
In addition to the topics included in the discussion, a visual guide to facial aesthetic enhancement and dermal filler injection techniques can be found in the book written by Braz and Sakuma [71], where the authors provide a wide range of injection techniques for facial aesthetics, including wrinkle reduction and contouring, discussing crucial subjects like facial assessment, hyaluronic acid science, facial aging, and pain management with regional nerve blocks and also providing meticulous anatomical descriptions and images, helping clinicians understand the connections between superficial and deeper structures, such as blood vessels, to prevent serious complications during procedures.
Finally, although investigating the complications of using hyaluronic acid to mitigate aging in the facial lower third was outside the scope of the proposal, while hyaluronic-acid-based dermal fillers generally exhibit a low occurrence of long-term side effects, there have been instances of occasional adverse outcomes recorded, which encompass chronic lymphoplasmacytic inflammatory reactions and classic foreign-body-type granulomatous reactions, as stated by Edwards and Fantasia [72]. Abduljabbar and Basendwh [73] report that using hyaluronic acid fillers is generally associated with mild and reversible complications. However, there are rare but serious risks, such as cutaneous necrosis and blindness due to vascular occlusion, which can occur if the filler compresses or is injected directly into a blood vessel. The most common side effects are related to the injection and are usually temporary. Vascular occlusion is the most severe complication, but a comprehensive understanding of facial vascular anatomy can help minimize the risk. Detecting vascular occlusion early and intervening without delay can significantly reduce the chances of long-term consequences. In their published paper, the authors suggest some guidelines to avoid, identify, and manage the different complications of hyaluronic acid fillers. Some case reports also describe complications from a hyaluronic acid dermal filler, like the one reported by Alli et al. [74], in which a 66-year-old female experienced a late-onset complication from a hyaluronic acid dermal filler, leading to firm perioral swellings that resembled a salivary gland neoplasm. Therefore, research on this topic is crucial and will be one of the authors’ goals in future research.
The limitations of this review are essentially related to the fact that the selection of articles included only Portuguese, English, and Italian, which may have limited the scope of the results obtained and, consequently, led to a loss of important information from other international investigations written in other languages but which are potentially significant. It is essential to emphasize that this review allowed obtaining an overview of the studies already conducted on a given topic but does not guarantee the total comprehensiveness of all available information. Therefore, it is necessary to continue researching and updating knowledge on the topic to ensure a complete and up-to-date approach.
5. Conclusions
This review highlights that using hyaluronic acid as a mechanism to mitigate the effects of face lower third aging following orofacial harmonization procedures in dentistry offers significant benefits to patients, improving the aesthetic appearance of the face, increasing patients’ self-esteem and satisfaction, and providing a better quality of life. Nonetheless, a note is made regarding the frail methodological evidence level in the selected articles due to limitations such as small sample sizes, absence of control groups, inadequate randomization, and insufficient statistical analyses, emphasizing the need for more methodologically rigorous studies to be published.
Author Contributions
Conceptualization, H.M.; methodology, H.M., I.C., P.M., M.G. and H.O.; software, H.O.; validation, H.M., I.C., P.M., M.G. and H.O.; formal analysis, H.M., M.G. and H.O.; investigation, H.M.; resources, M.G. and H.M.; data curation, H.M., M.G. and H.O.; writing—original draft preparation, H.M.; writing—review and editing, I.C., P.M., M.G. and H.O.; visualization, H.M., M.G. and H.O.; supervision, I.C., P.M., M.G. and H.O.; project administration, H.O.; funding acquisition, H.O. All authors have read and agreed to the published version of the manuscript.
Funding
This work is funded by FCT/MCTES through national funds and when applicable co-funded by EU funds under the project UIDB/50008/2020.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data and materials in this article can be obtained by contacting the corresponding author, Henrique Oliveira (hjmo@lx.it.pt).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Candore, G.; Caruso, C. Human Aging; Academic Press: Cambridge, MA, USA, 2021. [Google Scholar] [CrossRef]
- Farkas, J.P.; Pessa, J.E.; Hubbard, B.; Rohrich, R.J. The Science and Theory behind Facial Aging. Plast. Reconstr. Surg. Glob. Open 2013, 1, e8–e15. [Google Scholar] [CrossRef]
- Swift, A.; Liew, S.; Weinkle, S.; Garcia, J.K.; Silberberg, M.B. The Facial Aging Process From the “Inside Out”. Aesthetic Surg. J. 2021, 41, 1107–1119. [Google Scholar] [CrossRef] [PubMed]
- Fölster, M.; Hess, U.; Werheid, K. Facial age affects emotional expression decoding. Front. Psychol. 2014, 5, 30. [Google Scholar] [CrossRef] [PubMed]
- Pearlstein, S.L.; Taylor, C.T.; Stein, M.B. Facial Affect and Interpersonal Affiliation: Displays of Emotion During Relationship Formation in Social Anxiety Disorder. Clin. Psychol. Sci. 2019, 7, 826–839. [Google Scholar] [CrossRef] [PubMed]
- Goodman, G.J.; Liew, S.; Callan, P.; Hart, S. Facial aesthetic injections in clinical practice: Pretreatment and posttreatment consensus recommendations to minimise adverse outcomes. Australas. J. Dermatol. 2020, 61, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Akinbiyi, T.; Othman, S.; Familusi, O.; Calvert, C.; Card, E.B.; Percec, I. Better Results in Facial Rejuvenation with Fillers. Plast. Reconstr. Surg.-Glob. Open 2020, 8, e2763. [Google Scholar] [CrossRef] [PubMed]
- Chuang, J.; Barnes, C.; Wong, B. Overview of Facial Plastic Surgery and Current Developments. Surg. J. 2016, 02, e17–e28. [Google Scholar] [CrossRef]
- Chng, W.Q.; Samuel, M.; Naidoo, K.; Jaffar, H.; Khor, I.W.; Yiong Huak, C.; Watson, R.E.B.; De Mozzi, P.; Tam, W.W.S.; Camargo, C.P.; et al. Topical treatments and skin-resurfacing techniques for skin ageing. Cochrane Database Syst. Rev. 2021, 2021, CD014391. [Google Scholar] [CrossRef]
- Aubry, S.; Collart-Dutilleul, P.-Y.; Renaud, M.; Batifol, D.; Montal, S.; Pourreyron, L.; Carayon, D. Benefit of Hyaluronic Acid to Treat Facial Aging in Completely Edentulous Patients. J. Clin. Med. 2022, 11, 5874. [Google Scholar] [CrossRef]
- Raschke, G.F.; Rieger, U.M.; Bader, R.-D.; Schaefer, O.; Guentsch, A.; Gomez Dammeier, M.; Schultze-Mosgau, S. Perioral aging—An anthropometric appraisal. J. Cranio-Maxillofac. Surg. 2014, 42, e312–e317. [Google Scholar] [CrossRef]
- Diário da Repúbica. Diário da República, Regulamento n.º 1007/2021; Ordem dos Médicos Dentistas: Lisboa, Portugal, 2021. [Google Scholar]
- Nayyar, P. BOTOX: Broadening the Horizon of Dentistry. J. Clin. Diagn. Res. 2014, 8, ZE25. [Google Scholar] [CrossRef] [PubMed]
- Sheen, D.; Clarkson, E. Botox and Dermal Fillers. Dent. Clin. N. Am. 2020, 64, 325–339. [Google Scholar] [CrossRef] [PubMed]
- Malcmacher, L. Facial aesthetics in dentistry. Dent. Today 2009, 28, 116–117. [Google Scholar]
- Roberts, W. Incorporating facial rejuvenation procedures in the dental practice. Todays FDA 2013, 25, 50–53. [Google Scholar] [PubMed]
- Sonone, T.; Soni, V.; Gupta, S.; Shekatkar, Y.; Thorat, A.; Pol, T. Botox and dermal fillers in orthodontics—A review. J. Pharm. Bioallied Sci. 2022, 14, S60. [Google Scholar] [CrossRef]
- Goes, M.; Lopes, M.; Oliveira, H.; Marôco, J.; Fonseca, C.; Santos, M.; Caeiro, J. Psychometric Qualities of a Core Set to Ascertain the Functional Profile of Portuguese Elderly Citizens. In International Workshop on Gerontechnology; Communications in Computer and Information Science; Springer: Cham, Switzerland, 2020; pp. 314–329. [Google Scholar]
- Casale, M.; Moffa, A.; Vella, P.; Sabatino, L.; Capuano, F.; Salvinelli, B.; Lopez, M.A.; Carinci, F.; Salvinelli, F. Hyaluronic acid: Perspectives in dentistry. A systematic review. Int. J. Immunopathol. Pharmacol. 2016, 29, 572–582. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Aranda, M.; Iborra-Badia, I.; Alpiste-Illueca, F.; López-Roldán, A. Hyaluronic acid for periodontal tissue regeneration in intrabony defects. A systematic review. Dent. Rev. 2022, 2, 100057. [Google Scholar] [CrossRef]
- Hausauer, A.K.; Jones, D.H. Soft Tissue Augmentation (Temporary Injectable Fillers) of the Lower Face and Neck (Lips, Perioral, Nose, Neck). In Evidence-Based Procedural Dermatology; Springer: Cham, Switzerland, 2019; pp. 659–678. [Google Scholar]
- Beasley, K.; Weiss, M.; Weiss, R. Hyaluronic Acid Fillers: A Comprehensive Review. Facial Plast. Surg. 2009, 25, 086–094. [Google Scholar] [CrossRef] [PubMed]
- Mota de Sousa, L.M.; Furtado Firmino, C.; Alves Marques-Vieira, C.M.; Silva Pedro Severino, S.; Castelão Figueira Carlos Pestana, H. Revisões da literatura científica: Tipos, métodos e aplicações em enfermagem. Rev. Port. Enferm. Reabil. 2018, 1, 45–55. [Google Scholar] [CrossRef]
- PRISMA. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). Available online: http://www.prisma-statement.org/PRISMAStatement/FlowDiagram (accessed on 18 May 2023).
- Hong, S.O. Cosmetic Treatment Using Botulinum Toxin in the Oral and Maxillofacial Area: A Narrative Review of Esthetic Techniques. Toxins 2023, 15, 82. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Meng, F.; Li, Y.; Tian, Y.; Chen, H.; Jia, Q.; Cai, H.; Jiang, H.; Isola, G. Application of Nonsurgical Modalities in Improving Facial Aging. Int. J. Dent. 2022, 2022, 8332631. [Google Scholar] [CrossRef] [PubMed]
- Dantas, A.; Bezerra, R.; Nojima, C.; Lira, K.; Silva, G.; Oliveira, J.; Moreira, A. Lip Rejuvenation with Hyaluronic Acid. Health Soc. 2022, 2, 164–174. [Google Scholar] [CrossRef]
- Rogerio, V.; Vieira, M.; Rabelo, V.; Carbone, A.; Filho, D.M.; Silva, A.; Canales, G. Features to consider for mimicring tissues in orofacial aesthetics with optimal balance technology and non-animal stabilized hyaluronic acid (Restylane®): The MIMT concept. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, 440–447. [Google Scholar] [CrossRef]
- Silva, L.; Barros, P.; Barioni, E.; Constantino, E.; Hanai-Yoshida, V.; Oliveira, R. Complicações com o uso do ácido hialurônico na harmonização facial. Res. Soc. Dev. 2022, 11, e23111528052. [Google Scholar] [CrossRef]
- Shuai, L.; Sultan, M.; Hui, L. Noninvasive Facial Rejuvenation with Dermal Fillers and Neurotoxins, Public’s Preference: A Survey Report. N. Am. Acad. Res. NAAR 2021, 4, 257–274. [Google Scholar] [CrossRef]
- Tran Cao, P. The Use of Botulinum Toxin and Dermal Fillers to Enhance Patients’ Perceived Attractiveness. Dent. Clin. N. Am. 2020, 64, 659–668. [Google Scholar] [CrossRef]
- Bukhari, S.; Roswandi, N.; Waqas, M.; Habib, H.; Hussain, F.; Khan, S.; Sohail, M.; Ramli, N.; Thu, H.; Hussain, Z. Hyaluronic acid, a promising skin rejuvenating biomedicine: A review of recent updates and pre-clinical and clinical investigations on cosmetic and nutricosmetic effects. Int. J. Biol. Macromol. 2018, 120, 1682–1695. [Google Scholar] [CrossRef]
- Zupi, A. Who is the facial specialist? Hyaluronic acid fillers: Optimisation of aesthetic dentistry and patient loyalty. Stomatol. Edu J. 2016, 3, 168–177. [Google Scholar] [CrossRef]
- Spatafora, F.; Argo, A.; Campisi, G. Il ruolo dell’odontoiatra nella medicina estetica: Norme e indicazioni. Dent. Cadmos 2012, 80, 301–318. [Google Scholar] [CrossRef]
- Chaput, B.; Boutault, F.; Garrido, I.; Lopez, R. La lutte des chirurgiens-dentistes français pour conserver le droit aux injections de produits de comblement sur la face. Ann. Chir. Plast. Esthet. 2012, 57, 192–193. [Google Scholar] [CrossRef]
- Dastoor, S.F.; Misch, C.E.; Wang, H.-L. Dermal Fillers for Facial Soft Tissue Augmentation. J. Oral Implantol. 2007, 33, 191–204. [Google Scholar] [CrossRef]
- Perenack, J. Treatment Options to Optimize Display of Anterior Dental Esthetics in the Patient With the Aged Lip. J. Oral Maxillofac. Surg. 2005, 63, 1634–1641. [Google Scholar] [CrossRef]
- Torre, E.; Vetrano, S.; Vertué, S.; Zazzaron, M.; Russo, R. Satisfaction outcomes for patients and physicians following use of a new hyaluronic acid fillers. J. Cosmet. Dermatol. 2023, 22, 1–8. [Google Scholar] [CrossRef]
- Goes, M.; Oliveira, H.; Lopes, M.; Fonseca, C.; Pinho, L. Satisfaction: A Concept Based on Functionality and Quality of Life to Be Integrated in a Nursing Care Performance System. In International Workshop on Gerontechnology; Springer: Cham, Switzerland, 2022; pp. 84–93. [Google Scholar]
- Goes, M.; Oliveira, H.; Lopes, M.; Fonseca, C.; Pinho, L.; Marques, M. A nursing care-sensitive patient satisfaction measure in older patients. Sci. Rep. 2023, 13, 7607. [Google Scholar] [CrossRef]
- Ordem dos Médicos Dentistas. Harmonização Orofacial, Direito de Resposta ao Jornal Expresso. Available online: https://www.omd.pt/2022/04/harmonizao-orofacial-resposta/ (accessed on 6 June 2023).
- Wang, F.; Garza, L.A.; Kang, S.; Varani, J.; Orringer, J.S.; Fisher, G.J.; Voorhees, J.J. In Vivo Stimulation of De Novo Collagen Production Caused by Cross-linked Hyaluronic Acid Dermal Filler Injections in Photodamaged Human Skin. Arch. Dermatol. 2007, 143, 155–163. [Google Scholar] [CrossRef]
- Gavard Molliard, S.; Bon Bétemps, J.; Hadjab, B.; Topchian, D.; Micheels, P.; Salomon, D. Key rheological properties of hyaluronic acid fillers: From tissue integration to product degradation. Plast. Aesthetic Res. 2018, 5, 17. [Google Scholar] [CrossRef]
- Fagien, S.; Bertucci, V.; von Grote, E.; Mashburn, J.H. Rheologic and Physicochemical Properties Used to Differentiate Injectable Hyaluronic Acid Filler Products. Plast. Reconstr. Surg. 2019, 143, 707e–720e. [Google Scholar] [CrossRef]
- Vandana, K.L.; Singh, S.; Anil, L. Histologic evaluation of 5% Hyaluronic acid injection in oral tissue: A pilot study. Int. J. Mol. Biol. 2019, 4, 206–208. [Google Scholar] [CrossRef]
- Leong, X.Y.; Gopinath, D.; Syeed, S.M.; Veettil, S.K.; Shetty, N.Y.; Menon, R.K. Comparative Efficacy and Safety of Interventions for the Treatment of Oral Lichen Planus: A Systematic Review and Network Meta-Analysis. J. Clin. Med. 2023, 12, 2763. [Google Scholar] [CrossRef]
- Mandel, I.; Farkasdi, S.; Varga, G.; Károly Nagy, Á. Comparative Evaluation of Two Hyaluronic Acid Gel Products for the Treatment of Interdental Papillary Defects. Acta Stomatol. Croat. 2020, 54, 227–237. [Google Scholar] [CrossRef] [PubMed]
- Costa, E. Estetica dei Tessuti Orali e Periorali in Odontoiatria; Acta Medica Edizioni: Figino Serenza, Italy, 2014. [Google Scholar]
- Goes, M.; Lopes, M.; Oliveira, H.; Marôco, J.; Fonseca, C.; Santos, M.; Caeiro, J. A Nursing Care Intervention Model for Elderly People Adopting Self-care as a Central Concept. In International Workshop on Gerontechnology; Springer: Cham, Switzerland, 2020; pp. 359–372. [Google Scholar]
- Chen, Q.; Liu, Y.; Fan, D. Serious Vascular Complications after Nonsurgical Rhinoplasty. Plast. Reconstr. Surg.-Glob. Open 2016, 4, e683. [Google Scholar] [CrossRef]
- Ansari, Z.A.; Choi, C.J.; Rong, A.J.; Erickson, B.P.; Tse, D.T. Ocular and cerebral infarction from periocular filler injection. Orbit 2018, 38, 322–324. [Google Scholar] [CrossRef] [PubMed]
- Bae, I.H.; Kim, M.S.; Choi, H.; Na, C.H.; Shin, B.S. Ischemic oculomotor nerve palsy due to hyaluronic acid filler injection. J. Cosmet. Dermatol. 2018, 17, 1016–1018. [Google Scholar] [CrossRef]
- Fang, M.; Rahman, E.; Kapoor, K.M. Managing Complications of Submental Artery Involvement after Hyaluronic Acid Filler Injection in Chin Region. Plast. Reconstr. Surg.-Glob. Open 2018, 6, e1789. [Google Scholar] [CrossRef] [PubMed]
- Eldweik, L. Orbital infarction syndrome following hyaluronic acid filler rhinoplasty. Am. J. Ophthalmol. Case Rep. 2021, 22, 101063. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.L.; Biesman, B.S.; Dayan, S.H.; DeLorenzi, C.; Lambros, V.S.; Nestor, M.S.; Sadick, N.; Sykes, J. Treatment of Hyaluronic Acid Filler–Induced Impending Necrosis With Hyaluronidase: Consensus Recommendations. Aesthetic Surg. J. 2015, 35, 844–849. [Google Scholar] [CrossRef]
- Tucunduva, M.J.; Tucunduva-Neto, R.; Saieg, M.; Costa, A.L.; de Freitas, C. Vascular mapping of the face: B-mode and doppler ultrasonography study. Med. Oral Patol. Oral Cir. Bucal 2016, 21, e135–e141. [Google Scholar] [CrossRef] [PubMed]
- Sykes, J.M. Commentary on: New High Dose Pulsed Hyaluronidase Protocol for Hyaluronic Acid Filler Vascular Adverse Events. Aesthetic Surg. J. 2017, 37, 826–827. [Google Scholar] [CrossRef]
- Kapoor, K.M.; Saputra, D.I.; Porter, C.E.; Colucci, L.; Stone, C.; Brenninkmeijer, E.E.A.; Sloane, J.; Sayed, K.; Winaya, K.K.; Bertossi, D. Treating Aging Changes of Facial Anatomical Layers with Hyaluronic Acid Fillers. Clin. Cosmet. Investig. Dermatol. 2021, 14, 1105–1118. [Google Scholar] [CrossRef] [PubMed]
- Rauso, R.; Rugge, L.; Chirico, F.; Nicoletti, G.F.; Fragola, R.; Bove, P.; Zerbinati, N.; Lo Giudice, G. Nonsurgical Reshaping of the Lower Jaw With Hyaluronic Acid Fillers: A Retrospective Case Series. Dermatol. Pract. Concept. 2022, 12, e2022095. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, P.; Cotrin, P.; Valarelli, F.; Oliveira, R.; Bispo, C.; Freitas, K.; Oliveira, R.; Cotrin, P. Evaluation of the attractiveness of lips with different volumes after filling with hyaluronic acid. Sci. Rep. 2023, 13, 4589. [Google Scholar] [CrossRef] [PubMed]
- Islam, H.; Poly, T.S.; Tisha, Z.T.; Rahman, S.; Naveed, A.I.J.; Ahmed, A.; Ahmed, S.N.; Hassan, J.; Uddin, M.J.; Das, D.B. 3D Printed Hollow Microneedles for Treating Skin Wrinkles Using Different Anti-Wrinkle Agents: A Possible Futuristic Approach. Cosmetics 2023, 10, 41. [Google Scholar] [CrossRef]
- Heidekrueger, P.I.; Szpalski, C.; Weichman, K.; Juran, S.; Ng, R.; Claussen, C.; Ninkovic, M.; Broer, P.N. Lip Attractiveness: A Cross-Cultural Analysis. Aesthetic Surg. J. 2016, 37, 828–836. [Google Scholar] [CrossRef] [PubMed]
- Pascali, M.; Quarato, D.; Carinci, F. Filling Procedures for Lip and Perioral Rejuvenation: A Systematic Review. Rejucenat. Res. 2018, 21, 553–559. [Google Scholar] [CrossRef]
- Kau, C.H.; Christou, T.; Xie, R.B.; Abou-Saleh, T. Rating of smile attractiveness of patients finished to the American Board of Orthodontics standards. J. Orofac. Orthop./Fortschritte Der Kieferorthopädie 2020, 81, 239–248. [Google Scholar] [CrossRef]
- Bertucci, V.; Nikolis, A.; Solish, N.; Lane, V.; Hicks, J. Efficacy and Safety of Flexible Hyaluronic Acid Fillers in Lip and Perioral Enhancement. J. Drugs Dermatol. 2021, 20, 402–408. [Google Scholar] [CrossRef]
- Rho, N.-K.; Goo, B.; Youn, S.-J.; Won, C.-H.; Han, K.-H. Lip Lifting Efficacy of Hyaluronic Acid Filler Injections: A Quantitative Assessment Using 3-Dimensional Photography. J. Clin. Med. 2022, 11, 4554. [Google Scholar] [CrossRef] [PubMed]
- Hegde, V. Significance of the Frankfort mandibular plane angle in prosthetic management of partially or completely edentulous patients with Class II malocclusions. J. Indian Prosthodont. Soc. 2005, 5, 175–179. [Google Scholar] [CrossRef]
- Cervino, G.; Meto, A.; Fiorillo, L.; Odorici, A.; Meto, A.; D’Amico, C.; Oteri, G.; Cicciù, M. Surface Treatment of the Dental Implant with Hyaluronic Acid: An Overview of Recent Data. Int. J. Environ. Res. Public Health 2021, 18, 4670. [Google Scholar] [CrossRef]
- van Loghem, J.; Sattler, S.; Casabona, G.; Cotofana, S.; Fabi, S.G.; Goldie, K.; Gout, U.; Kerscher, M.; Lim, T.S.; de Sanctis Pecora, C.; et al. Consensus on the Use of Hyaluronic Acid Fillers from the Cohesive Polydensified Matrix Range: Best Practice in Specific Facial Indications. Clin. Cosmet. Investig. Dermatol. 2021, 14, 1175–1199. [Google Scholar] [CrossRef]
- Gagik, G.; Khachik, K.; Azaryan, H.; Irina, K.; Armen, H.; Veronika, R.; Leon, K.; Manushak, M. An Multidisciplinary Approach to Treatment of Edentulous Patients with Perioral Wrinkles of the Skin. Int. J. Dermatol. Ski. Care 2021, 3, 11–21. [Google Scholar] [CrossRef]
- Braz, A.; Sakuma, T. Dermal Fillers: Facial Anatomy and Injection Techniques, 1st ed.; Thieme Publishing Group: New York, NY, USA, 2020. [Google Scholar]
- Edwards, P.; Fantasia, J. Review of long-term adverse effects associated with the use of chemically-modified animal and nonanimal source hyaluronic acid dermal fillers. Clin. Interv. Aging 2008, 2, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Abduljabbar, M.H.; Basendwh, M.A. Complications of hyaluronic acid fillers and their managements. J. Dermatol. Dermatol. Surg. 2016, 20, 100–106. [Google Scholar] [CrossRef]
- Alli, N.; Murdoch, M.; Meer, S. Delayed adverse reaction to a natural dermal filler mimicking salivary gland neoplasia. Bull. Natl. Res. Cent. 2022, 46, 97. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).