Performance Analysis of the Maximum Likelihood Estimation of Signal Period Length and Its Application in Heart Rate Estimation with Reduced Respiratory Influence
Abstract
:Featured Application
Abstract
1. Introduction
1.1. Background
1.2. Contributions of This Paper
- (1)
- A heart rate estimation method is proposed.
- (2)
- A regularized estimation model is proposed, and the asymptotic estimation variance of the estimator was derived accordingly.
- (3)
- The proposed method was further validated by experimental data.
2. Method
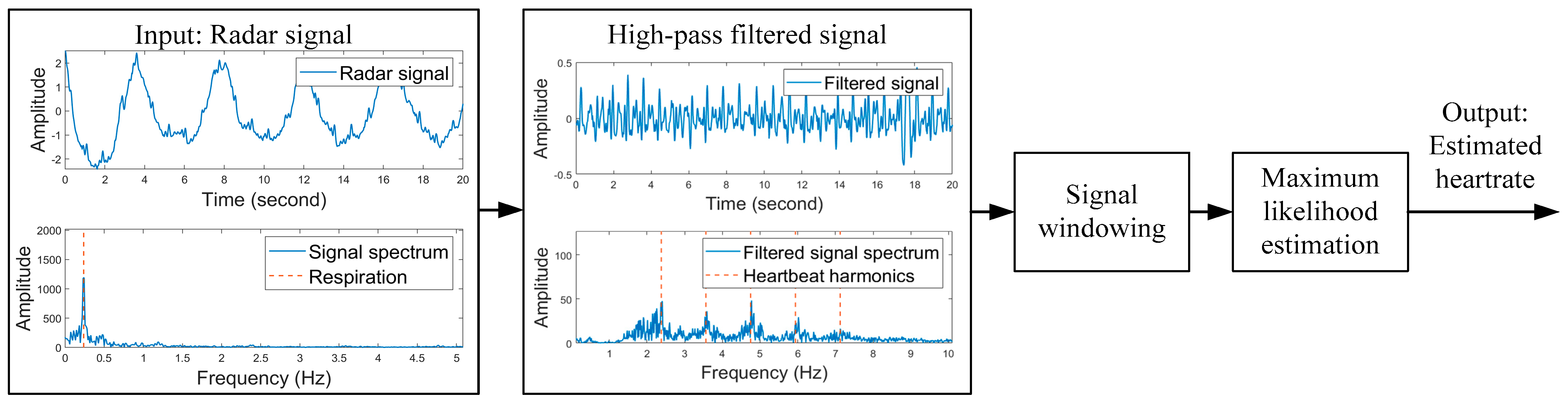
2.1. Radar-Based Heartbeat Rate Estimation
2.2. Asymptotic Performance of the Maximum Likelihood Estimation
3. Experiments
3.1. Simulation
3.2. Verification with Measured Data
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, C.; Peng, Z.; Huang, T.; Fan, T.; Wang, F.; Horng, T.; Munoz-Ferreras, J.; Gómez-García, R.; Ran, L.; Lin, J. A review on recent progress of portable short-range noncontact microwave radar systems. IEEE Trans. Microw. Theory Techal. 2017, 65, 1692–1706. [Google Scholar] [CrossRef]
- Yoo, Y.-K.; Shin, H.-C. Movement Compensated driver’s respiratory rate extraction. Appl. Sci. 2022, 12, 2695. [Google Scholar] [CrossRef]
- Yoo, Y.; Jung, C.; Shin, H.-C. Unsupervised detection of multiple sleep stages using a single FMCW radar. Appl. Sci. 2023, 13, 4468. [Google Scholar] [CrossRef]
- Mercuri, M.; Lu, Y.; Polito, S.; Wieringa, F.; Liu, Y.; Veen, A.; Hoof, C.; Torfs, T. Enabling robust radar-based localization and vital signs monitoring in multipath propagation environments. IEEE Trans. Biomed. Eng. 2021, 68, 3228–3240. [Google Scholar] [CrossRef]
- Alizadeh, M.; Shaker, G.; Almeida, J.C.M.; Morita, P.P.; Safavi-Naeini, S. Remote monitoring of human vital signs using mm-wave FMCW radar. IEEE Access 2019, 7, 54958–54968. [Google Scholar] [CrossRef]
- Cho, H.S.; Choi, B.; Park, Y.J. Monitoring heart activity using ultra-wideband radar. Electron. Lett. 2019, 55, 878–881. [Google Scholar] [CrossRef]
- Chen, J.; Zhang, D.; Wu, Z.; Zhou, F.; Sun, Q.; Chen, Y. Contactless electrocardiogram monitoring with millimeter wave radar. IEEE Trans. Mob. Comput. 2022. [Google Scholar] [CrossRef]
- Ling, L.; Zhou, W.; Ren, Y.; Wang, J.; Guo, L. Non-contact heart rate monitoring based on millimeter wave radar. IEEE Access 2022, 10, 74033–74044. [Google Scholar] [CrossRef]
- Dong, X.; Feng, Y.; Cui, C.; Lu, J. CEEMDAN-ICA-based radar monitoring of adjacent multi-target vital signs. Electronics 2023, 12, 2732. [Google Scholar] [CrossRef]
- Park, B.-K.; Boric-Lubecke, O.; Lubecke, V.M. Arctangent demodulation with DC offset compensation in quadrature doppler radar receiver systems. IEEE T. Microw. Theory 2007, 55, 1073–1079. [Google Scholar] [CrossRef]
- Edanami, K.; Sun, G. Medical radar signal dataset for non-contact respiration and heart rate measurement. Data Brief 2022, 40, 107724. [Google Scholar] [CrossRef] [PubMed]
- Aardal, Ø.; Paichard, Y.; Brovoll, S.; Berger, T.; Lande, T.S.; Hamran, S.-E. Physical working principles of medical radar. IEEE Trans. Biomed. Eng. 2013, 60, 1142–1149. [Google Scholar] [CrossRef] [PubMed]
- Islam, S.M.M.; Motoyama, N.; Pacheco, S.; Lubecke, V.M. Non-contact vital signs monitoring for multiple subjects using a millimeter wave FMCW automotive radar. In Proceedings of the 2020 IEEE/MTT-S International Microwave Symposium (IMS), Los Angeles, CA, USA, 4–6 August 2020. [Google Scholar] [CrossRef]
- Petrovic, V.L.; Jankovic, M.M.; Lupsic, A.V.; Mihajlovic, V.R.; Popović-Božović, J.S. High-accuracy real-time monitoring of heart rate variability using 24 GHz continuous-wave doppler radar. IEEE Access 2019, 7, 74721–74733. [Google Scholar] [CrossRef]
- Singh, A.; Rehman, S.U.; Yongchareon, S.; Chong, P.H.J. Multi-resident non-contact vital sign monitoring using radar: A review. IEEE Sens. J. 2021, 21, 4061–4084. [Google Scholar] [CrossRef]
- Zheng, P.; Zheng, C.; Li, X.; Chen, H.; Wang, A.; Luo, Y. Second harmonic weighted reconstruction for non-contact monitoring heart rate. IEEE Sens. J. 2022, 22, 5815–5823. [Google Scholar] [CrossRef]
- Rong, Y.; Bliss, D.W. Smart homes: See multiple-heartbeats through wall using wire-less signals. In Proceedings of the 2019 IEEE Radar Conference (RadarConf), Boston, MA, USA, 22–26 April 2019. [Google Scholar] [CrossRef]
- Rong, Y.; Bliss, D.W. Remote sensing for vital information based on spectral-domain harmonic signatures. IEEE Trans. Aerosp. Electron. Syst. 2019, 55, 3454–3465. [Google Scholar] [CrossRef]
- Wise, J.D.; Caprio, J.R.; Parks, T.W. Maximum likelihood pitch estimation. IEEE Acoust. Speech Signal Process. 1976, 24, 418–423. [Google Scholar] [CrossRef]
- Conte, E.; Filippi, A.; Tomasin, S. ML period estimation with application to vital sign monitoring. IEEE Signal Process. Lett. 2010, 17, 905–908. [Google Scholar] [CrossRef]
- Zhang, C.; Wei, S.; Dong, G.; Zeng, Y. Periodic average magnitude difference function for remote heart rate monitoring. Electron. Lett. 2023, 59, e12838. [Google Scholar] [CrossRef]
- Mercuri, M.; Torfs, T.; Rykunov, M.; Laureti, S.; Ricci, M.; Crupi, F. Analysis of signal processing methods to reject the DC offset contribution of static reflectors in FMCW radar-based vital signs monitoring. Sensors 2022, 22, 9697. [Google Scholar] [CrossRef]
- Kay, S.M. Cramer-Rao lower bound. In Fundamentals of Statistical Signal Processing; PTR Prentice Hall: London, UK, 1993; Volume 1, pp. 39–42. [Google Scholar]
- Carter, G.C. Coherence and time delay estimation. Proc. IEEE 1987, 75, 236–255. [Google Scholar] [CrossRef]
- Jacovitti, G.; Scarano, G. Discrete Time Techniques for Time Delay Estimation. IEEE Trans. Signal Process. 1993, 41, 525–533. [Google Scholar] [CrossRef]
- Schellenberger, S.; Shi, K.; Steigleder, T.; Malessa, A.; Michler, F.; Hameyer, L.; Neumann, N.; Lurz, F.; Weigel, R.; Ostgathe, C.; et al. A dataset of clinically recorded radar vital signs with synchronised reference sensor signals. Sci. Data 2020, 7, 291. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Nian, Y.; Liu, B. Noncontact heart beat signal extraction based on wavelet transform. In Proceedings of the 2015 8th International Conference on Biomedical Engineering and Informatics (BMEI), Shenyang, China, 14–16 October 2015. [Google Scholar] [CrossRef]
- Zhu, Z.; Yang, D.; Zhao, R.; Liang, B. Vital Sign Signal Extraction Method Based on Permutation Entropy and EMD Algorithm for Ultra-Wideband Radar. In Proceedings of the 2019 3rd International Conference on Electronic Information Technology and Computer Engineering (EITCE), Xiamen, China, 18–20 October 2019. [Google Scholar] [CrossRef]

| Dataset 1 [11], 10 Ghz | Dataset 1 [11], 24 Ghz | Dataset 2 [26], 24 Ghz | |
|---|---|---|---|
| Proposed | 3.88 1 | 4.47 | 6.30 |
| Park [10] | 13.47 | 16.48 | 8.18 |
| Edanami [11] | 13.22 | 15.29 | 9.46 |
| Rong [18] | 8.35 | 8.94 | 12.70 |
| Conte [20] | 10.64 | 13.00 | 8.40 |
| He [27] | 9.97 | 7.85 | 9.12 |
| Zhu [28] | 6.27 | 8.74 | 8.78 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, C.; Jin, M.; Dong, G.; Wei, S. Performance Analysis of the Maximum Likelihood Estimation of Signal Period Length and Its Application in Heart Rate Estimation with Reduced Respiratory Influence. Appl. Sci. 2023, 13, 10402. https://doi.org/10.3390/app131810402
Zhang C, Jin M, Dong G, Wei S. Performance Analysis of the Maximum Likelihood Estimation of Signal Period Length and Its Application in Heart Rate Estimation with Reduced Respiratory Influence. Applied Sciences. 2023; 13(18):10402. https://doi.org/10.3390/app131810402
Chicago/Turabian StyleZhang, Chi, Mingming Jin, Ge Dong, and Shaoming Wei. 2023. "Performance Analysis of the Maximum Likelihood Estimation of Signal Period Length and Its Application in Heart Rate Estimation with Reduced Respiratory Influence" Applied Sciences 13, no. 18: 10402. https://doi.org/10.3390/app131810402
APA StyleZhang, C., Jin, M., Dong, G., & Wei, S. (2023). Performance Analysis of the Maximum Likelihood Estimation of Signal Period Length and Its Application in Heart Rate Estimation with Reduced Respiratory Influence. Applied Sciences, 13(18), 10402. https://doi.org/10.3390/app131810402






