Retromalleolar Groove Deepening in Recurrent Peroneal Tendon dislocation: Short- and Medium-Term Functional Outcomes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Demographic
2.2. Clinical Evaluation
2.3. Radiographic Measures
2.4. Clinical Scores
2.5. Retromalleolar Groove Deepening Technique
2.6. Post-Operative Care and Rehabilitation
2.7. Statistics
3. Results
3.1. Clinical Results
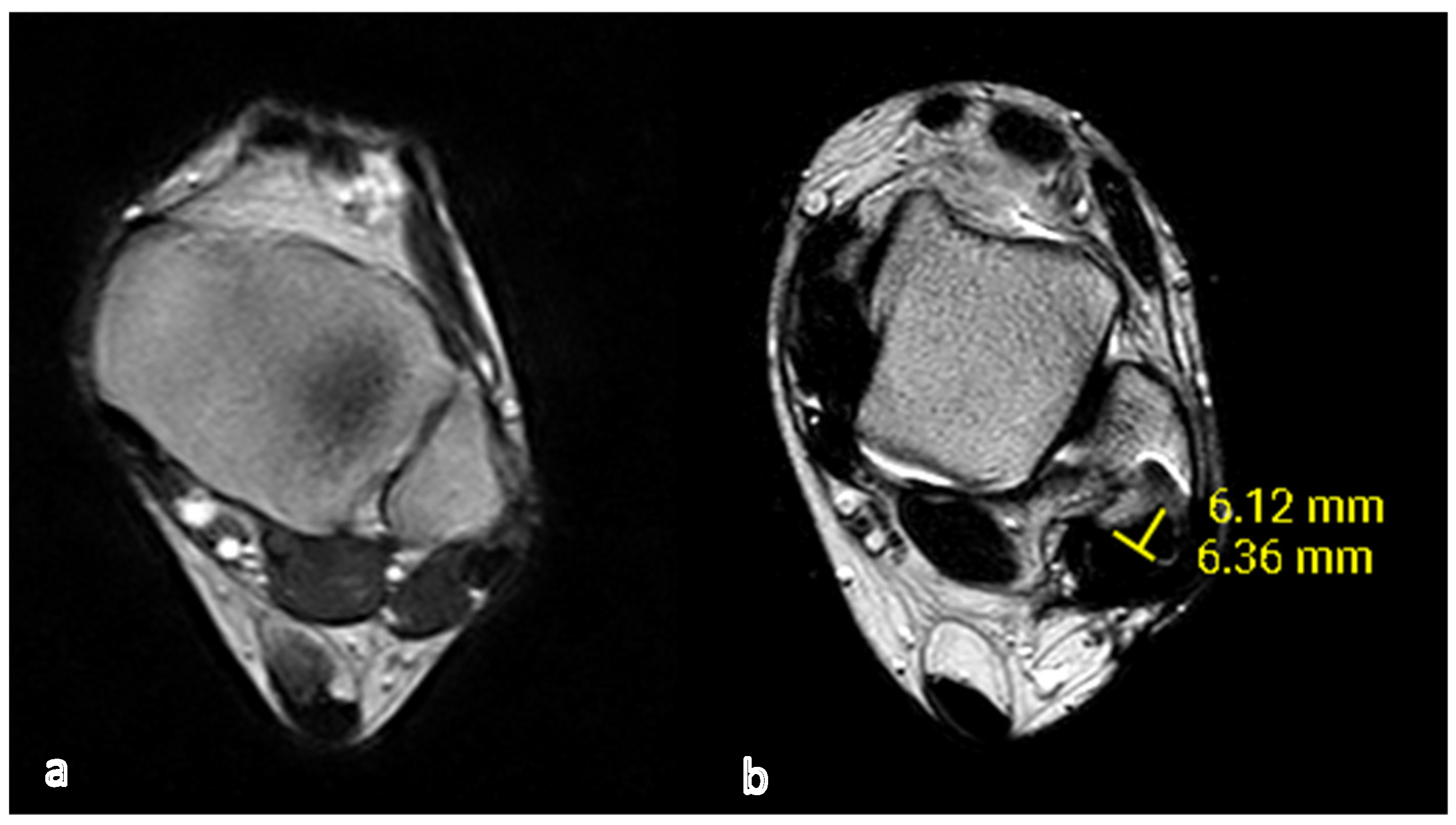
3.2. Radiologic Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dombek, M.F.; Lamm, B.M.; Saltrick, K.; Mendicino, R.W.; Catanzariti, A.R. Peroneal tendon tears: A retrospective review. J. Foot Ankle Surg. 2003, 42, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Espinosa, N.; Maurer, M.A. Peroneal tendon dislocation. Eur. J. Trauma. Emerg. Surg. 2015, 41, 631–637. [Google Scholar] [CrossRef]
- Kwaadu, K.Y.; Fleming, J.J.; Florek, D. Superior peroneal retinacular injuries in calcaneal fractures. J. Foot Ankle Surg. 2015, 54, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Mabit, C.; Salanne, P.; Boncoeur-Martel, M.P.; Fiorenza, F.; Valleix, D.; Descottes, B.; Caix, M. La gouttière rétromalléolaire latérale: Étude radio-anatomique [The lateral retromalleolar groove: A radio-anatomic study]. Bull. Assoc. Anat. 1996, 80, 17–21. [Google Scholar]
- Wang, X.T.; Rosenberg, Z.S.; Mechlin, M.B.; Schweitzer, M.E. Normal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging features. Radiographics 2005, 25, 587–602. [Google Scholar] [CrossRef]
- Klammer, G.; Benninger, E.; Espinosa, N. The varus ankle and instability. Foot Ankle Clin. 2012, 17, 57–82. [Google Scholar] [CrossRef]
- Edwards, M. The relations of the peroneal tendons to the fibula, calcaneus, and cuboideum. Am. J. Anat. 1927, 42, 213–252. [Google Scholar] [CrossRef]
- Athavale, S.A.; Swathi Vangara, S.V. Anatomy of the superior peroneal tunnel. J. Bone Joint Surg. 2011, 93, 564–571. [Google Scholar] [CrossRef]
- Lugo-Pico, J.G.; Kaiser, J.T.; Sanchez, R.A.; Aiyer, A.A. Peroneal Tendinosis and Subluxation. Clin. Sports Med. 2020, 39, 845–858. [Google Scholar] [CrossRef]
- Oden, R.R. Tendon injuries about the ankle resulting from skiing. Clin. Orthop. Relat. Res. 1987, 216, 63–69. [Google Scholar] [CrossRef]
- Philbin, T.M.; Landis, G.S.; Smith, B. Peroneal tendon injuries. J. Am. Acad. Orthop. Surg. 2009, 17, 306–317. [Google Scholar] [CrossRef] [PubMed]
- Adamson, C.; Cymet, T. Ankle sprains: Evaluation, treatment, rehabilitation. Md. Med. J. 1997, 46, 530–537. [Google Scholar] [PubMed]
- Hutchinson, B.L.; Gustafson, L.S. Chronic peroneal tendon subluxation. New surgical technique and retrospective analysis. J. Am. Podiatr. Med. Assoc. 1994, 84, 511–517. [Google Scholar] [PubMed]
- Neustadter, J.; Raikin, S.M.; Nazarian, L.N. Dynamic sonographic evaluation of peroneal tendon subluxation. AJR Am. J. Roentgenol. 2004, 183, 985–988. [Google Scholar] [CrossRef]
- Rosenberg, Z.S.; Bencardino, J.; Astion, D.; Schweitzer, M.E.; Rokito, A.; Sheskier, S. MRI features of chronic injuries of the superior peroneal retinaculum. AJR Am. J. Roentgenol. 2003, 181, 1551–1557. [Google Scholar] [CrossRef]
- Saupe, N.; Mengiardi, B.; Pfirrmann, C.W.; Vienne, P.; Seifert, B.; Zanetti, M. Anatomic variants associated with peroneal tendon disorders: MR imaging findings in volunteers with asymptomatic ankles. Radiology 2007, 242, 509–517. [Google Scholar] [CrossRef]
- Stover, C.N.; Bryan, D.R. Traumatic dislocation of the peroneal tendons. Am. J. Surg. 1962, 103, 180–186. [Google Scholar] [CrossRef]
- Escalas, F.; Figueras, J.M.; Merino, J.A. Dislocation of the peroneal tendons. Long-term results of surgical treatment. J. Bone Joint Surg. Am. 1980, 62, 451–453. [Google Scholar] [CrossRef]
- Ferran, N.A.; Oliva, F.; Maffulli, N. Recurrent subluxation of the peroneal tendons. Sports Med. 2006, 36, 839–846. [Google Scholar] [CrossRef]
- Selmani, E.; Gjata, V.; Gjika, E. Current concepts review: Peroneal tendon disorders. Foot Ankle Int. 2006, 27, 221–228. [Google Scholar] [CrossRef]
- Davda, K.; Malhotra, K.; O’Donnell, P.; Singh, D.; Cullen, N. Peroneal tendon disorders. EFORT Open Rev. 2017, 2, 281–292. [Google Scholar] [CrossRef] [PubMed]
- Coughlin, M.J.; Schon, L.C. Disorders of tendons. In Mann’s Surgery of the Foot and Ankle, 9th ed.; Coughlin, M.J., Mann, R.A., Saltzman, C.L., Eds.; Mosby Elsevier: Philadelphia, PA, USA, 2013. [Google Scholar]
- Shawen, S.B.; Anderson, R.B. Indirect Groove Deepening in the Management of Chronic Peroneal Tendon Dislocation. Tech. Foot Ankle Surg. 2004, 3, 118–125. [Google Scholar] [CrossRef]
- Safran, M.R.; O’Malley, D., Jr.; Fu, F.H. Peroneal tendon subluxation in athletes: New exam technique, case reports, and review. Med. Sci. Sports Exerc. 1999, 31 (Suppl. S7), S487–S492. [Google Scholar] [CrossRef] [PubMed]
- Matcuk, G.R. Fibular groove morphology and measurements on MRI: Correlation with fibularis tendon abnormalities. Surg. Radiol. Anat. 2019, 41, 75–85. [Google Scholar] [CrossRef]
- Leigheb, M.; Janicka, P.; Andorno, S.; Marcuzzi, A.; Magnani, C.; Grassi, F. Italian translation, cultural adaptation and validation of the “American Orthopaedic Foot and Ankle Society’s (AOFAS) ankle-hindfoot scale”. Acta Biomed. 2016, 87, 38–45. [Google Scholar]
- Richter, M.; Agren, P.H.; Besse, J.L.; Cöster, M.; Kofoed, H.; Maffulli, N.; Rosenbaum, D.; Steultjens, M.; Alvarez, F.; Boszczyk, A.; et al. EFAS Score—Multilingual development and validation of a patient-reported outcome measure (PROM) by the score committee of the European Foot and Ankle Society (EFAS). Foot Ankle Surg. 2018, 24, 185–204. [Google Scholar] [CrossRef]
- Van Dijk, P.A.; Miller, D.; Calder, J.; DiGiovanni, C.W.; Kennedy, J.G.; Kerkhoffs, G.M.; Kynsburtg, A.; Havercamp, D.; Guillo, S.; Oliva, X.M.; et al. The ESSKA-AFAS international consensus statement on peroneal tendon pathologies. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3096–3107. [Google Scholar] [CrossRef]
- Heckman, D.S.; Reddy, S.; Pedowitz, D.; Wapner, K.L.; Parekh, S.G. Operative treatment for peroneal tendon disorders. J. Bone Joint Surg. Am. 2008, 90, 404–418. [Google Scholar] [CrossRef]
- Van Dijk, P.A.; Gianakos, A.L.; Kerkhoffs, G.M.; Kennedy, J.G. Return to sports and clinical outcomes in patients treated for peroneal tendon dislocation: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 1155–1164. [Google Scholar] [CrossRef]
- Park, S.H.; Choi, Y.R.; Lee, J.; Seo, J.; Lee, H.S. Treatment of Recurrent Peroneal Tendon Dislocation by Peroneal Retinaculum Reattachment Without Fibular Groove Deepening. J. Foot Ankle Surg. 2021, 60, 994–997. [Google Scholar] [CrossRef]
- Adachi, N.; Fukuhara, K.; Tanaka, H.; Nakasa, T.; Ochi, M. Superior retinaculoplasty for recurrent dislocation of peroneal tendons. Foot Ankle Int. 2006, 27, 1074–1078. [Google Scholar] [CrossRef]
- Raikin, S.M.; Elias, I.; Nazarian, L.N. Intrasheath subluxation of the peroneal tendons. J. Bone Joint Surg. Am. 2008, 90, 992–999. [Google Scholar] [CrossRef] [PubMed]
- Mabit, C.; Salanne, P.H.; Blanchard, F. The retromalleolar groove of the fibula: A radio-anatomical study. Foot Ankle Surg. 1999, 5, 179–186. [Google Scholar] [CrossRef]
- Hwang, I.M.; Del Sol, S.R.; Jenkins, S.M.; Bryant, S.A.; Gardner, B.B.; McGahan, P.; Chen, J. Open Peroneal Tendon Stabilization With Fibular Groove Deepening. Arthrosc. Tech. 2022, 11, e347–e352. [Google Scholar] [CrossRef]
- Van Dijk, P.A.D.; Vopat, B.G.; Guss, D.; Younger, A.; DiGiovanni, C.W. Retromalleolar Groove Deepening in Recurrent Peroneal Tendon Dislocation: Technique Tip. Orthop. J. Sports Med. 2017, 5, 2325967117706673. [Google Scholar] [CrossRef] [PubMed]
- Lootsma, J.; Wuite, S.; Hoekstra, H.; Matricali, G.A. Surgical treatment options for chronic instability of the peroneal tendons: A systematic review and proportional meta-analysis. Arch. Orthop. Trauma Surg. 2023, 143, 1903–1913. [Google Scholar] [CrossRef] [PubMed]
- Kumai, T.; Benjamin, M. The histological structure of the malleolar groove of the fibula in man: Its direct bearing on the displacement of peroneal tendons and their surgical repair. J. Anat. 2003, 203, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Martens, M.A.; Noyez, J.F.; Mulier, J.C. Recurrent dislocation of the peroneal tendons. Results of rerouting the tendons under the calcaneofibular ligament. Am. J. Sport. Med. 1986, 14, 148–150. [Google Scholar] [CrossRef]
- Thomas, J.L.; Sheridan, L.; Graviet, S. A modification of the Ellis Jones procedure for chronic peroneal subluxation. J. Foot Surg. 1992, 31, 454–458. [Google Scholar]




| Patients’ Data | Mean (Range) |
|---|---|
| Sex | |
| Male | 6 |
| Female | 3 |
| Age, years | 31.2 (14–51) |
| Side of injury | |
| Left | 8 |
| Right | 2 |
| Activity during injury | |
| Soccer | 3 |
| Dance | 1 |
| Climbing ski | 2 |
| Other (domestic accident) | 3 |
| Time from injury to surgery (months) | 11.7 ± 8.6 (7–16.5) |
| Score | Mean ± SD (N = 10) | p-Value |
|---|---|---|
| Follow-up (years) | 4.2 years | |
| (min 6 months–max 6 years) | ||
| AOFAS score | <0.005 | |
| pre-op | 74.4 (sd 17.17) | |
| post-op | 86.9 (sd 21.23) | |
| EFAS score | <0.005 | |
| pre-op | 19.7 (sd 7.50) | |
| post-op | 31 (sd 14.82) |
| Case N. | AOFAS Pre-op | AOFAS Post-op | EFAS Pre-op | EFAS Post-op |
|---|---|---|---|---|
| 1 | 82 pt | 87 pt | 16 pt | 31 pt |
| 2 | 48 pt | 38 pt | 17 pt | 3 pt |
| 3 | 74 pt | 96 pt | 25 pt | 38 pt |
| 4 | 85 pt | 100 pt | 27 pt | 40 pt |
| 5 | 92 pt | 100 pt | 26 pt | 40 pt |
| 6 | 75 pt | 100 pt | 20 pt | 40 pt |
| 7 | 81 pt | 100 pt | 12 pt | 40 pt |
| 8 | 48 pt | 88 pt | 12 pt | 34 pt |
| 9 | 61 pt | 60 pt | 10 pt | 4 pt |
| 10 | 98 pt | 100 pt | 32 pt | 40 pt |
| Mean | 74.4 pt | 86.9 pt | 19.7 pt | 31 pt |
| StDev | 17.17 | 21.23 | 7.50 | 14.82 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Samaila, E.M.; Auregli, L.; Maluta, T.; Leigheb, M.; Mazzotti, A.; Magnan, B. Retromalleolar Groove Deepening in Recurrent Peroneal Tendon dislocation: Short- and Medium-Term Functional Outcomes. Appl. Sci. 2023, 13, 11468. https://doi.org/10.3390/app132011468
Samaila EM, Auregli L, Maluta T, Leigheb M, Mazzotti A, Magnan B. Retromalleolar Groove Deepening in Recurrent Peroneal Tendon dislocation: Short- and Medium-Term Functional Outcomes. Applied Sciences. 2023; 13(20):11468. https://doi.org/10.3390/app132011468
Chicago/Turabian StyleSamaila, Elena Manuela, Ludovica Auregli, Tommaso Maluta, Massimiliano Leigheb, Antonio Mazzotti, and Bruno Magnan. 2023. "Retromalleolar Groove Deepening in Recurrent Peroneal Tendon dislocation: Short- and Medium-Term Functional Outcomes" Applied Sciences 13, no. 20: 11468. https://doi.org/10.3390/app132011468
APA StyleSamaila, E. M., Auregli, L., Maluta, T., Leigheb, M., Mazzotti, A., & Magnan, B. (2023). Retromalleolar Groove Deepening in Recurrent Peroneal Tendon dislocation: Short- and Medium-Term Functional Outcomes. Applied Sciences, 13(20), 11468. https://doi.org/10.3390/app132011468









