Investigation on the Application of Artificial Intelligence in Prosthodontics
Abstract
1. Introduction
2. Methodology
- What kinds of AI methods are currently being employed in the prosthodontic field?
- How does AI enhance clinical decision-making and outcomes in prosthodontics?
- What are the current clinical uses of AI in prosthodontics, and how well does it work as a diagnostic tool during the determination of the type of prosthesis required for a particular patient?
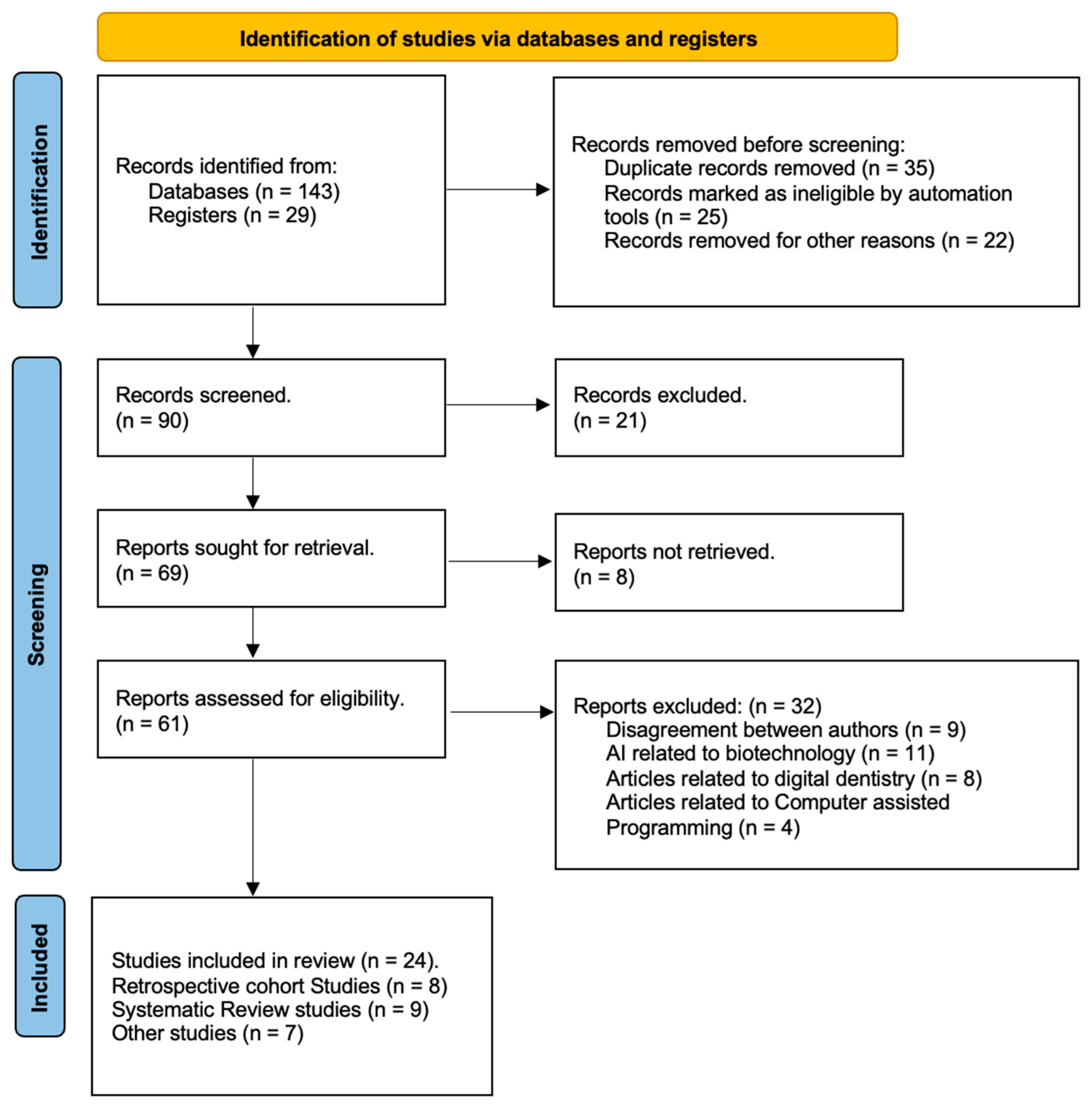
2.1. Data Collection
Data Extraction
2.2. Study Selection
2.3. Study Characteristics
Assessment of the Risk of Bias in Included Studies
2.4. Statistical Analysis
3. Result
3.1. Descriptive Analysis
3.2. Statistical Analysis by ANOVA
3.3. Diagnostic Accuracy
3.4. Error Reduction
4. Discussion
4.1. Application of AI in Prosthodontics
4.2. Use of AI in Implant Prosthodontics
4.3. CAD/CAM and AI
4.4. Maxillofacial Prostheses and AI
4.5. Limitations of AI
4.6. Ethical Considerations with AI
4.7. Future Scope
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mahdi, S.S.; Battineni, G.; Khawaja, M.; Allana, R.; Siddiqui, M.K.; Agha, D. How does artificial intelligence impact digital healthcare initiatives? A review of AI applications in dental healthcare. Int. J. Inf. Manag. Data Insights 2023, 3, 100144. [Google Scholar] [CrossRef]
- Femiano, F.; Femiano, R.; Femiano, L.; Nucci, L.; Minervini, G.; Antonelli, A.; Bennardo, F.; Barone, S.; Scotti, N.; Sorice, V.; et al. A New Combined Protocol to Treat the Dentin Hypersensitivity Associated with Non-Carious Cervical Lesions: A Randomized Controlled Trial. Appl. Sci. 2020, 11, 187. [Google Scholar] [CrossRef]
- Evangelista, K.; de Freitas Silva, B.S.; Yamamoto-Silva, F.P.; Valladares-Neto, J.; Silva, M.A.G.; Cevidanes, L.H.S.; de Luca Canto, G.; Massignan, C. Accuracy of artificial intelligence for tooth extraction decision-making in orthodontics: A systematic review and meta-analysis. Clin. Oral Investig. 2022, 26, 6893–6905. [Google Scholar] [CrossRef] [PubMed]
- Pareek, M.; Kaushik, B. Artificial intelligence in prosthodontics: A scoping review on current applications and future possibilities. Int. J. Adv. Med. 2022, 9, 367. [Google Scholar] [CrossRef]
- Cicciù, M. Prosthesis: New Technological Opportunities and Innovative Biomedical Devices. Prosthesis 2019, 1, 1–2. [Google Scholar] [CrossRef]
- Cicciù, M.; Cervino, G.; Terranova, A.; Risitano, G.; Raffaele, M.; Cucinotta, F.; Santonocito, D.; Fiorillo, L. Prosthetic and Mechanical Parameters of the Facial Bone under the Load of Different Dental Implant Shapes: A Parametric Study. Prosthesis 2019, 1, 41–53. [Google Scholar] [CrossRef]
- Alsubaiy, E.F.; Chaturvedi, S.; Qutub, O.A.; Mously, H.A.; Zarbah, M.A.; Haralur, S.B.; Bhagat, T.V. Novel CAD-CAM zirconia coping design to enhance the aesthetics and strength for anterior PLZ crowns. Technol. Health Care 2021, 29, 1161–1171. [Google Scholar] [CrossRef]
- Cicciù, M. Past, Present and Future of Prosthesis: 2020 Upgrade. Prosthesis 2021, 3, 9–10. [Google Scholar] [CrossRef]
- Chaturvedi, S.; Alqahtani, N.M.; Addas, M.K.; Alfarsi, M.A. Marginal and internal fit of provisional crowns fabricated using 3D printing technology. Technol. Health Care 2020, 28, 635–642. [Google Scholar] [CrossRef]
- Minervini, G.; Fiorillo, L.; Russo, D.; Lanza, A.; D’Amico, C.; Cervino, G.; Meto, A.; di Francesco, F. Prosthodontic Treatment in Patients with Temporomandibular Disorders and Orofacial Pain and/or Bruxism: A Review of the Literature. Prosthesis 2022, 4, 253–262. [Google Scholar] [CrossRef]
- Abella Sans, F. Minimally Invasive Alternatives to Dental Extraction and Implant Placement. In Minimally Invasive Approaches in Endodontic Practice; Springer International Publishing: Cham, Switzerland, 2021; pp. 203–231. [Google Scholar]
- Paschou, T.; Rapaccini, M.; Adrodegari, F.; Saccani, N. Digital servitization in manufacturing: A systematic literature review and research agenda. Ind. Mark. Manag. 2020, 89, 278–292. [Google Scholar] [CrossRef]
- Naddeo, P.; Laino, L.; la Noce, M.; Piattelli, A.; de Rosa, A.; Iezzi, G.; Laino, G.; Paino, F.; Papaccio, G.; Tirino, V. Surface biocompatibility of differently textured titanium implants with mesenchymal stem cells. Dent. Mater. 2015, 31, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Shah, K.C.; Lum, M.G. Treatment planning for the single-tooth implant restoration--general considerations and the pretreatment evaluation. J. Calif. Dent. Asso.c 2008, 36, 827–834. [Google Scholar]
- Jihed, M.; Dallel, I.; Tobji, S.; ben Amor, A. The Impact of Artificial Intelligence on Contemporary Orthodontic Treatment Planning-A Systematic Review and Meta-Analysis. Sch. J. Dent. Sci. 2022, 9, 70–87. [Google Scholar] [CrossRef]
- Seckanovic, A.; Sehovac, M.; Spahic, L.; Ramic, I.; Mamatnazarova, N.; Pokvic, L.G.; Badnjevic, A.; Kacila, M. Review of Artificial Intelligence Application in Cardiology. In Proceedings of the 2020 9th Mediterranean Conference on Embedded Computing, MECO 2020, Budva, Montenegro, 8–11 June 2020. [Google Scholar] [CrossRef]
- Stokes, K.; Castaldo, R.; Franzese, M.; Salvatore, M.; Fico, G.; Pokvic, L.G.; Badnjevic, A.; Pecchia, L. A machine learning model for supporting symptom-based referral and diagnosis of bronchitis and pneumonia in limited resource settings. Biocybern. Biomed. Eng. 2021, 41, 1288–1302. [Google Scholar] [CrossRef]
- Granulo, E.; Bećar, L.; Gurbeta, L.; Badnjević, A. Telemetry system for diagnosis of asthma and chronical obstructive pulmonary disease (COPD). In Lecture Notes of the Institute for Computer Sciences, Social-Informatics and Telecommunications Engineering, LNICST; Springer International Publishing: Cham, Switzerland, 2016. [Google Scholar] [CrossRef]
- Shajahan, P.A.; Raghavan, R.; Joe, N. Application of artificial intelligence in prosthodontics. Int. J. Sci. Health Care Res. 2021, 6, 57–60. [Google Scholar]
- Saghiri, M.A.; Vakhnovetsky, J.; Nadershahi, N. Scoping review of artificial intelligence and immersive digital tools in dental education. J. Dent. Educ. 2022, 86, 736–750. [Google Scholar] [CrossRef] [PubMed]
- Cicciù, M.; Fiorillo, L.; D’Amico, C.; Gambino, D.; Amantia, E.M.; Laino, L.; Crimi, S.; Campagna, P.; Bianchi, A.; Herford, A.S.; et al. 3D Digital Impression Systems Compared with Traditional Techniques in Dentistry: A Recent Data Systematic Review. Materials 2020, 13, 1982. [Google Scholar] [CrossRef]
- Agrawal, P.; Nikhade, P. Artificial Intelligence in Dentistry: Past, Present, and Future. Cureus 2022, 14, e27405. [Google Scholar] [CrossRef]
- Ametrano, G.; D’Antò, V.; di Caprio, M.P.; Simeone, M.; Rengo, S.; Spagnuolo, G. Effects of sodium hypochlorite and ethylenediaminetetraacetic acid on rotary nickel-titanium instruments evaluated using atomic force microscopy. Int. Endod. J. 2011, 44, 203–209. [Google Scholar] [CrossRef]
- Krifka, S.; Petzel, C.; Bolay, C.; Hiller, K.-A.; Spagnuolo, G.; Schmalz, G.; Schweikl, H. Activation of stress-regulated transcription factors by triethylene glycol dimethacrylate monomer. Biomaterials 2011, 32, 1787–1795. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, T.; Jamal, R.F.; Battineni, G.; Teja, K.V.; Marto, C.M.; Spagnuolo, G. A review of prolonged post-COVID-19 symptoms and their implications on dental management. Int. J. Environ. Res. Public Health 2021, 18, 5131. [Google Scholar] [CrossRef] [PubMed]
- Rengo, C.; Goracci, C.; Ametrano, G.; Chieffi, N.; Spagnuolo, G.; Rengo, S.; Ferrari, M. Marginal leakage of class v composite restorations assessed using microcomputed tomography and scanning electron microscope. Oper. Dent. 2015, 40, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Spagnuolo, G.; Sorrentino, R. The Role of Digital Devices in Dentistry: Clinical Trends and Scientific Evidences. J. Clin. Med. 2020, 9, 1692. [Google Scholar] [CrossRef] [PubMed]
- Kochhar, A.S.; Sidhu, M.S.; Prabhakar, M.; Bhasin, R.; Kochhar, G.K.; Dadlani, H.; Spagnuolo, G.; Mehta, V.V. Intra- and Interobserver Reliability of Bone Volume Estimation Using OsiriX Software in Patients with Cleft Lip and Palate Using Cone Beam Computed Tomography. Dent. J. 2021, 9, 14. [Google Scholar] [CrossRef]
- Abdinian, M.; Moshkforoush, S.; Hemati, H.; Soltani, P.; Moshkforoushan, M.; Spagnuolo, G. Comparison of Cone Beam Computed Tomography and Digital Radiography in Detecting Separated Endodontic Files and Strip Perforation. Appl. Sci. 2020, 10, 8726. [Google Scholar] [CrossRef]
- Spagnuolo, G. Cone-Beam Computed Tomography and the Related Scientific Evidence. Appl. Sci. 2022, 12, 7140. [Google Scholar] [CrossRef]
- Rengo, C.; Spagnuolo, G.; Ametrano, G.; Juloski, J.; Rengo, S.; Ferrari, M. Micro-computerized tomographic analysis of premolars restored with oval and circular posts. Clin. Oral Investig. 2014, 18, 571–578. [Google Scholar] [CrossRef]
- Bernauer, S.A.; Zitzmann, N.U.; Joda, T. The Use and Performance of Artificial Intelligence in Prosthodontics: A Systematic Review. Sensors 2021, 21, 6628. [Google Scholar] [CrossRef]
- Thurzo, A.; Urbanová, W.; Novák, B.; Czako, L.; Siebert, T.; Stano, P.; Mareková, S.; Fountoulaki, G.; Kosnáčová, H.; Varga, I. Where Is the Artificial Intelligence Applied in Dentistry? Systematic Review and Literature Analysis. Healthcare 2022, 10, 1269. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Grischke, J.; Johannsmeier, L.; Eich, L.; Griga, L.; Haddadin, S. Dentronics: Towards robotics and artificial intelligence in dentistry. Dent. Mater. 2020, 36, 765–778. [Google Scholar] [CrossRef] [PubMed]
- Lahoud, P.; EzEldeen, M.; Beznik, T.; Willems, H.; Leite, A.; Van Gerven, A.; Jacobs, R. Artificial Intelligence for fast and accurate 3-dimensional tooth segmentation on cone-beam computed tomography. J. Endod. 2021, 47, 827–835. [Google Scholar] [CrossRef] [PubMed]
- Farook, T.H.; Jamayet, N.B.; Abdullah, J.Y.; Alam, M.K. Machine learning and intelligent diagnostics in dental and Orofacial Pain Management: A systematic review. Pain Res. Manag. 2021, 2021, 6659133. [Google Scholar] [CrossRef] [PubMed]
- Talpur, S.; Azim, F.; Rashid, M.; Syed, S.A.; Talpur, B.A.; Khan, S.J. Use of different machine learning algorithms for diagnosis of dental caries. J. Healthc. Eng. 2022, 2022, 5032435. [Google Scholar] [CrossRef]
- Limones, A.; Celemín-Viñuela, A.; Romeo-Rubio, M.; Castillo-Oyagüe, R.; Gómez-Polo, M.; Martínez Vázquez de Parga, J.A. Outcome measurements and quality of randomized controlled clinical trials of tooth-supported fixed dental prostheses: A systematic review and qualitative analysis. J. Prosthet. Dent. 2022, S0022-3913, 00282-7. [Google Scholar] [CrossRef]
- van Riet, T.C.T.; Chin Jen Sem, K.T.H.; Ho, J.-P.T.F.; Spijker, R.; Kober, J.; de Lange, J. Robot Technology in Dentistry: Part One of a Systematic Review: Literature Characteristics. Dent. Mater. 2021, 37, 1217–1226. [Google Scholar] [CrossRef]
- Delgado, A.H.S.; Sauro, S.; Lima, A.F.; Loguercio, A.D.; Della Bona, A.; Mazzoni, A.; Collares, F.M.; Staxrud, F.; Ferracane, J.; Tsoi, J.; et al. Risk of bias tool and guideline to support reporting of pre-clinical Dental Materials Research and assessment of Systematic Reviews. J. Dent. 2022, 127, 104350. [Google Scholar] [CrossRef]
- Kirubarajan, A.; Young, D.; Khan, S.; Crasto, N.; Sobel, M.; Sussman, D. Artificial Intelligence and Surgical Education: A systematic scoping review of interventions. J. Surg. Educ. 2022, 79, 500–515. [Google Scholar] [CrossRef]
- Afrashtehfar, K.I.; Alnakeb, N.A.; Assery, M.K. Accuracy of intraoral scanners versus traditional impressions: A Rapid Umbrella Review. J. Evid. Based Dent. Pract. 2022, 22, 101719. [Google Scholar] [CrossRef]
- Albanchez-González, M.I.; Brinkmann, J.C.-B.; Peláez-Rico, J.; López-Suárez, C.; Rodríguez-Alonso, V.; Suárez-García, M.J. Accuracy of digital dental implant impression using intraoral scanners compared with conventional impression techniques: A systematic review of in vitro studies. Int. J. Environ. Res. Public Health 2022, 19, 2026. [Google Scholar] [CrossRef]
- Mai, H.Y.; Mai, H.N.; Kim, H.J.; Lee, J.; Lee, D.H. Accuracy of removable partial denture metal frameworks fabricated by computer-aided design/computer-aided manufacturing method: A systematic review and meta-analysis. J. Evid. Based Dent. Pract. 2022, 22, 101681. [Google Scholar] [CrossRef]
- Touati, R.; Sailer, I.; Marchand, L.; Ducret, M.; Strasding, M. Communication tools and patient satisfaction: A scoping review. J. Esthet. Restor. Dent. 2021, 34, 104–116. [Google Scholar] [CrossRef] [PubMed]
- Adel, S.; Zaher, A.; El Harouni, N.; Venugopal, A.; Premjani, P.; Vaid, N. Robotic applications in orthodontics: Changes in Contemporary Clinical Care. BioMed Res. Int. 2021, 2021, 9954615. [Google Scholar] [CrossRef]
- Tian, Y.; Chen, C.X.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.Y.; Lee, E.-S.; Jiang, H.B. Review of 3D printing in Dentistry: Technologies, affecting factors, and applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef]
- Nguyen, T.M.; Tonmukayakul, U.; Le, L.K.-D.; Calache, H.; Mihalopoulos, C. Economic evaluation of preventive interventions for dental caries and periodontitis: A systematic review. Appl. Health Econ. Health Policy 2022, 21, 53–70. [Google Scholar] [CrossRef]
- Costa, R.T.F.; de Oliveira Limirio, J.P.J.; do Egito Vasconcelos, B.C.; Pellizzer, E.P.; de Moraes, S.L.D. Rehabilitation with dental prostheses and its influence on brain activity: A systematic review. J. Prosthet. Dent. 2022, S0022-3913, 00090-7. [Google Scholar] [CrossRef] [PubMed]
- Sridharan, K.; Alsobaiei, M.; Sivaramakrishnan, G.; AlSulaiti, F. Detection of caries under fixed prosthodontic restorations using cone-beam CT: A meta-analysis. Int. J. Prosthodont. Restor. Dent. 2020, 10, 170–175. [Google Scholar] [CrossRef]
- Abad-Coronel, C.; Valdiviezo, O.P.; Naranjo, O.B. Intraoral scanning devices are used in fixed prosthodontics. Acta Sci. Dent. Sci. 2019, 7, 44–51. [Google Scholar]
- Lee, J.H.; Jeong, S.N. Efficacy of deep convolutional neural network algorithm for the identification and classification of dental implant systems, using panoramic and periapical radiographs: A pilot study. Medicine 2020, 99, e20787. [Google Scholar] [CrossRef] [PubMed]
- Lerner, H.; Mouhyi, J.; Admakin, O.; Mangano, F. Artificial intelligence in fixed implant prosthodontics: A retrospective study of 106 implant-supported monolithic zirconia crowns inserted in the posterior jaws of 90 patients. BMC Oral Health 2020, 20, 80. [Google Scholar] [CrossRef]
- Yamaguchi, S.; Lee, C.; Karaer, O.; Ban, S.; Mine, A.; Imazato, S. Predicting the Debonding of CAD/CAM Composite Resin Crowns with AI. J. Dent. Res. 2019, 98, 1234–1238. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, D.H.; Jeong, S.N.; Choi, S.H. Detection and diagnosis of dental caries using a deep learning-based convolutional neural network algorithm. J. Dent. 2018, 77, 106–111. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, D.H.; Jeong, S.N.; Choi, S.H. Diagnosis and prediction of periodontally compromised teeth using a deep learning-based convolutional neural network algorithm. J. Periodontal Implant Sci. 2018, 48, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Raith, S.; Vogel, E.P.; Anees, N.; Keul, C.; Güth, J.F.; Edelhoff, D.; Fischer, H. Artificial Neural Networks as a powerful numerical tool to classify specific features of a tooth based on 3D scan data. Comput. Biol. Med. 2017, 80, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Peng, M.; Li, Q.; Wang, Y. Evaluation of a Novel Computer Color Matching System Based on the Improved Back- Propagation Neural Network Model. J. Prosthodont. 2018, 27, 775–783. [Google Scholar] [CrossRef]
- Ahmed, N.; Abbasi, M.S.; Zuberi, F.; Qamar, W.; Halim, M.S.B.; Maqsood, A.; Alam, M.K. Artificial Intelligence Techniques: Analysis, Application, and Outcome in Dentistry—A Systematic Review. Biomed. Res. Int. 2021, 2021, 9751564. [Google Scholar] [CrossRef] [PubMed]
- Khanagar, S.B.; Al-ehaideb, A.; Maganur, P.C.; Vishwanathaiah, S.; Patil, S.; Baeshen, H.A.; Sarode, S.C.; Bhandi, S. Developments, application, and performance of artificial intelligence in dentistry–A systematic review. J. Dent. Sci. 2021, 16, 508–522. [Google Scholar] [CrossRef] [PubMed]
- Fontenele, R.C.; Gerhardt, M.d.N.; Pinto, J.C.; van Gerven, A.; Willems, H.; Jacobs, R.; Freitas, D.Q. Influence of dental fillings and tooth type on the performance of a novel artificial intelligence-driven tool for automatic tooth segmentation on CBCT images—A validation study. J. Dent. 2022, 119, 104069. [Google Scholar] [CrossRef] [PubMed]
- Abouzeid, H.L.; Chaturvedi, S.; Abdelaziz, K.M.; Alzahrani, F.A.; AlQarni, A.A.S.; Alqahtani, N.M. Role of Robotics and Artificial Intelligence in Oral Health and Preventive Dentistry-Knowledge, Perception and Attitude of Dentists. Oral Health Prev. Dent. 2021, 19, 353–363. [Google Scholar]
- Amornvit, P.; Rokaya, D.; Sanohkan, S. Comparison of Accuracy of Current Ten Intraoral Scanners. Biomed Res. Int. 2021, 2021, 2673040. [Google Scholar] [CrossRef]
- Cabanes-Gumbau, G.; Palma, J.C.; Kois, J.C.; Revilla-León, M. Transferring the tooth preparation finish line on intraoral digital scans to dental software programs: A dental technique. J. Prosthet. Dent. 2022, S0022-3913, 00582-5. [Google Scholar] [CrossRef]
- van der Meer, W.J.; Andriessen, F.S.; Wismeijer, D.; Ren, Y. Application of intra-oral dental scanners in the digital workflow of implantology. PLoS ONE 2012, 7, e43312. [Google Scholar] [CrossRef]
- Rekow, E.D. Digital dentistry: The new state of the art—Is it disruptive or destructive? Dent. Mater. 2020, 36, 9–24. [Google Scholar] [CrossRef] [PubMed]
- Jreige, C.S.; Kimura, R.N.; Segundo, Â.R.T.C.; Coachman, C.; Sesma, N. Esthetic treatment planning with digital animation of the smile dynamics: A technique to create a 4-dimensional virtual patient. J. Prosthet. Dent. 2022, 128, 130–138. [Google Scholar] [CrossRef]
- Lahoud, P.; Jacobs, R.; Boisse, P.; EzEldeen, M.; Ducret, M.; Richert, R. Precision medicine using patient-specific modelling: State of the art and perspectives in dental practice. Clin. Oral Investig. 2022, 26, 5117–5128. [Google Scholar] [CrossRef] [PubMed]
- Shen, K.; Huang, C.; Lin, Y.; Du, J.; Chen, F.; Kabasawa, Y.; Chen, C.; Huang, H. Effects of artificial intelligence-assisted dental monitoring intervention in patients with periodontitis: A randomized controlled trial. J. Clin. Periodontol. 2022, 49, 988–998. [Google Scholar] [CrossRef]
- Javaid, M.; Haleem, A.; Pratap Singh, R.; Suman, R. Pedagogy and innovative care tenets in COVID-19 pandemic: An enhancive way through Dentistry 4.0. Sens. Int. 2021, 2, 100118. [Google Scholar] [CrossRef] [PubMed]
- Hegde, S.; Ajila, V.; Zhu, W.; Zeng, C. Artificial intelligence in early diagnosis and prevention of oral cancer. Asia-Pac. J. Oncol. Nurs. 2022, 9, 100133. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, K.; Iversen, L.; Titlestad, T.L.; Winther, O. Systematic review of machine learning for diagnosis and prognosis in dermatology. J. Dermatol. Treat. 2020, 31, 496–510. [Google Scholar] [CrossRef] [PubMed]
- Monill-González, A.; Rovira-Calatayud, L.; d’Oliveira, N.G.; Ustrell-Torrent, J.M. Artificial intelligence in orthodontics: Where are we now? A scoping review. Orthod. Craniofac. Res. 2021, 24, 6–15. [Google Scholar] [CrossRef]
- Mureșanu, S.; Almășan, O.; Hedeșiu, M.; Dioșan, L.; Dinu, C.; Jacobs, R. Artificial intelligence models for clinical usage in dentistry with a focus on dentomaxillofacial CBCT: A systematic review. Oral Radiol. 2023, 39, 18–40. [Google Scholar] [CrossRef] [PubMed]
- Crompton, H.; Jones, M.V.; Burke, D. Affordances and challenges of artificial intelligence in K-12 education: A systematic review. J. Res. Technol. Educ. 2022, 1–21. [Google Scholar] [CrossRef]
- Mohammad-Rahimi, H.; Nadimi, M.; Rohban, M.H.; Shamsoddin, E.; Lee, V.Y.; Motamedian, S.R. Machine learning and orthodontics, current trends and the future opportunities: A scoping review. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 170–192.e4. [Google Scholar] [CrossRef]
- Khanagar, S.B.; Vishwanathaiah, S.; Naik, S.; Al-Kheraif, A.A.; Devang Divakar, D.; Sarode, S.C.; Bhandi, S.; Patil, S. Application and performance of artificial intelligence technology in forensic odontology-A systematic review. Leg. Med. 2021, 48, 101826. [Google Scholar] [CrossRef]
- Khanagar, S.B.; Al-Ehaideb, A.; Vishwanathaiah, S.; Maganur, P.C.; Patil, S.; Naik, S.; Baeshen, H.A.; Sarode, S.S. Scope and performance of artificial intelligence technology in orthodontic diagnosis, treatment planning, and clinical decision-making—A systematic review. J. Dent. Sci. 2021, 16, 482–492. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Gómez-Polo, M.; Barmak, A.B.; Inam, W.; Kan, J.Y.K.; Kois, J.C.; Akal, O. Artificial intelligence models for diagnosing gingivitis and periodontal disease: A systematic review. J. Prosthet. Dent. 2022, S0022-3913, 00075-0. [Google Scholar] [CrossRef]
- Besse, P.; del Barrio, E.; Gordaliza, P.; Loubes, J.-M.; Risser, L. A Survey of Bias in Machine Learning Through the Prism of Statistical Parity. Am. Stat. 2022, 76, 188–198. [Google Scholar] [CrossRef]
- Rajput, G.; Ahmed, S.; Chaturvedi, S.; Addas, M.K.; Bhagat, T.V.; Gurumurthy, V.; Alqahtani, S.M.; Alobaid, M.A.; Alsubaiy, E.F.; Gupta, K.; et al. Comparison of Microleakage in Nanocomposite and Amalgam as a Crown Foundation Material Luted with Different Luting Cements under CAD-CAM Milled Metal Crowns: An In Vitro Microscopic Study. Polymers 2022, 14, 2609. [Google Scholar]
- Nair, U.P.; Shivamurthy, R.; Nagate, R.R.; Chaturvedi, S.; Al-Qahtani, S.M.; al Magbol, M.; Gokhale, S.T.; Tikare, S.; Chaturvedi, M. Effect of Injectable Platelet-Rich Fibrin with a Nano-Hydroxyapatite Bone Graft on the Treatment of a Grade II Furcation Defect. Bioengineering 2022, 9, 602. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.; Chaturvedi, S.; Ali, M.; Pandey, K.K.; Alqahtani, N.M.; Alfarsi, M.A.; Addas, M.K.; Vaddamanu, S.K.; Ahmari, N.M.; Alqahtani, S.M.; et al. Dimensional Stability of Light-Activated Urethane Dimethacrylate Denture Base Resins. Polymers 2023, 15, 744. [Google Scholar] [CrossRef]
- Rai, J.J.; Chaturvedi, S.; Gokhale, S.T.; Nagate, R.R.; Al-Qahtani, S.M.; Magbol, A.M.; Bavabeedu, S.S.; Elagib, M.F.A.; Venkataram, V.; Chaturvedi, M. Effectiveness of a Single Chair Side Application of NovaMin® [Calcium Sodium Phosphosilicate] in the Treatment of Dentine Hypersensitivity following Ultrasonic Scaling—A Randomized Controlled Trial. Materials 2023, 16, 1329. [Google Scholar] [CrossRef] [PubMed]
- Mittal, P.; Gokhale, S.T.; Manjunath, S.; Al-Qahtani, S.M.; Magbol, A.M.; Nagate, R.R.; Tikare, S.; Chaturvedi, S.; Agarwal, A.; Venkataram, V. Comparative Evaluation of Locally Administered 2% Gel Fabricated from Lemongrass Polymer and 10% Doxycycline Hyclate Gel as an Adjunct to Scaling and Root Planing in the Treatment of Chronic Periodontitis—A Randomized Controlled Trial. Polymers 2022, 14, 2766. [Google Scholar] [CrossRef]
- Chen, Y.-W.; Stanley, K.; Att, W. Artificial intelligence in dentistry: Current applications and future perspectives. Quintessence Int. 2020, 51, 248–257. [Google Scholar] [PubMed]
- Bindushree, V.; Sameen, R.J.; Vasudevan, V.; Shrihari, T.G.; Devaraju, D.; Mathew, N.S. Artificial Intelligence: In Modern Dentistry. J. Dent. Res. Rev. 2020, 7, 27. [Google Scholar]
- Revilla-León, M.; Gómez-Polo, M.; Vyas, S.; Barmak, A.B.; Gallucci, G.O.; Att, W.; Özcan, M.; Krishnamurthy, V.R. Artificial intelligence models for tooth-supported fixed and removable prosthodontics: A systematic review. J. Prosthet. Dent. 2021, 129, 276–292. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Singh, T.; Lee, J.-H.; Gaudin, R.; Chaurasia, A.; Wiegand, T.; Uribe, S.; Krois, J. Artificial intelligence in dental research: Checklist for authors, reviewers, readers. J. Dent. 2021, 107, 103610. [Google Scholar] [CrossRef] [PubMed]
- Jose, A.A.; Sawhney, H.; Jose, C.M.; Center, G.D. Artificial intelligence: The immeasurable limits in pediatric dentistry. Int. J. Early Child. 2020, 16, 300–309. [Google Scholar] [CrossRef]
- Takahashi, T.; Nozaki, K.; Gonda, T.; Ikebe, K. A system for designing removable partial dentures using artificial intelligence. Part 1. Classification of partially edentulous arches using a convolutional neural network. J. Prosthodont. Res. 2021, 65, 115–118. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Gómez-Polo, M.; Vyas, S.; Barmak, B.A.; Galluci, G.O.; Att, W.; Krishnamurthy, V.R. Artificial intelligence applications in implant dentistry: A systematic review. J. Prosthet. Dent. 2021, 129, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Asiri, A.F.; Altuwalah, A.S. The role of neural artificial intelligence for diagnosis and treatment planning in endodontics: A qualitative review. Saudi Dent. J. 2022, 34, 270–281. [Google Scholar] [CrossRef] [PubMed]
- Mohaideen, K.; Negi, A.; Verma, D.K.; Kumar, N.; Sennimalai, K.; Negi, A. Applications of artificial intelligence and machine learning in orthognathic surgery: A scoping review. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, e962–e972. [Google Scholar] [CrossRef] [PubMed]
- Holzinger, A.; Langs, G.; Denk, H.; Zatloukal, K.; Müller, H. Causability and explainability of artificial intelligence in medicine. Wiley Interdiscip. Rev. Data Min. Knowl. Discov. 2019, 9, e1312. [Google Scholar] [CrossRef] [PubMed]
| Study Title, Author Name and Publishing Year [Citation] | Country | Study Design | Journal | Aim of the Study |
|---|---|---|---|---|
| Artificial intelligence for fast and accurate 3-dimensional tooth segmentation on cone-beam computed tomography (EzEldeen et al. [36]) | Belgium | CBCT | Journal of Endodontic | The purpose of this research was to create and verify an AI-driven instrument for automatic teeth segmentation using cone beam computed tomography (CBCT). |
| Machine learning and intelligent diagnostics in dental and orofacial pain management (Farook et al. [37]) | Malaysia Saudi Arabia | Systematic review | Pain Research and Management | Machine learning was investigated to determine its clinical impact, efficacy, limitations, and results when compared to human diagnostics for identifying the root causes of dental and orofacial pain, and (6) bone and temporomandibular joint. |
| Uses of Different Machine Learning Algorithms for Diagnosis of Dental Caries (Talpur et al. [38]) | Pakistan | DDC | Journal of Healthcare Engineering | The primary goal of this research was to systematically examine existing literature on the topic of how machine learning can affect dental caries. The PICO criteria will be used as a framework for this study’s design. |
| Outcome measurements and quality of randomized controlled clinical trials of tooth-supported fixed dental prostheses (Limones et al. [39]) | Spain | Systematic review | The Journal of Prosthetic Dentistry | This systematic review aimed to identify all primary and secondary outcome metrics in tooth-supported FDP RCTs. Secondary aims were to assess methodological quality using the Cochrane Collaboration’s risk of bias instrument (RoB, v2.0) and reporting quality using a 16-item CONSORT evaluation tool through published reports. |
| Robot technology in dentistry (Van Riet et al. [40]) | Netherlands | Systematic review | Dental Materials | The goal of this evidence-based review was to give dentists and researchers a bird’s-seeing view of the features of the literature surrounding dental robotics projects. |
| A risk of bias tool and guideline to support reporting of pre-clinical dental materials research and assessment of systematic reviews (Delgado et al. [41]) | Spain, Brazil, etc. | Systematic review | Journal of Dentistry | The purpose of this study was to aid in the reporting of future investigations and to enhance the assessment in systematic reviews. |
| Artificial Intelligence and Surgical Education: A Systematic Scoping Review of Interventions (Kirubarajan et al. [42]) | Canada | Systematic review | Journal of Surgical Education | The purpose of this literature review was to consolidate the available research on the application of AI to surgical education. |
| Accuracy of intraoral scanners versus traditional impressions: A rapid umbrella review (Afrashtehfar et al. [43]) | Switzerland | RU review | Journal of Evidence-Based Dental Practice | The primary purpose of this research was to (1) evaluate the reporting quality of titles and abstracts of the collected literature and (2) assess the truthfulness and precision of intraoral scanning (IOS) in dentistry based on recent secondary sources. |
| Accuracy of Digital Dental Implants Impression Taking with Intraoral Scanners Compared with Conventional Impression Techniques: A Systematic Review of In Vitro Studies (Albanchez-González [44]) | Spain | Systematic Review | International Journal of Environmental Research and Public Health | This systematic study aimed to assess the in vitro accuracy of dental implant impressions produced with an intraoral scanner to those taken with more traditional methods. |
| Accuracy of removable partial denture metal frameworks fabricated by computer-aided design/computer-aided manufacturing method: A systematic review and meta-analysis (MAI et al. [45]) | Republic of Korea | Systematic Review | Journal of Evidence Based Dental Practice | The purpose of this systematic review and meta-analysis was to evaluate the precision of removable partial denture (RPD) frameworks made with CAD/CAM systems to those made with traditional casting techniques. |
| Communication tools and patient satisfaction: A scoping review (Touati et al. [46]) | Switzerland | Scoping review | Journal of Esthetic and Restorative Dentistry | This exploratory research evaluated aesthetic dentistry communication. Various communication tools can incorporate patients in SDM. Few know how dental communication technology improves patient satisfaction. Medline, Embase, Cochrane, and World Science were searched for patient satisfaction research. |
| Robotic applications in orthodontics: Changing the face of contemporary clinical care (Adel et al. [47]) | Egypt and India | CFCC | BioMed research international | This review covered eight orthodontic domains: (1) robotic dental assistants; (2) robotics in orthodontic diagnosis and simulation; (3) robotics in patient education, teaching, and training; (4) wire bending and customized appliance robotics; (5) nanorobots/microrobots for tooth movement acceleration and remote monitoring; (6) robotics in maxillofacial surgeries and implant placement; (7) automated aligner production robotics; and (8) TMD rehabilitative robotics. |
| A review of 3D printing in dentistry: Technologies, affecting factors, and applications (Tian et al. [48]) | China and Republic of Korea | Technological application | Scanning | Three-dimensional printing has uses in dentistry, including prosthodontics, oral and maxillofacial surgery, and oral implantology. The 3D printing review is practical and scientific. |
| Economic Evaluations of Preventive Interventions for Dental Caries and Periodontitis: A Systematic Review (Nguyen et al. [49] | Australia | Systematic Review | Applied Health Economics and Health Policy | For the purpose of providing a critical analysis of the techniques employed in comprehensive economic assessments of preventative therapies for dental caries and periodontitis. |
| Rehabilitation with dental prostheses and its influence on brain activity: A systematic review (Costa et al. [50]) | Brazil | Systematic Review | The Journal of Prosthetic Dentistry | The aim was to determine whether or not oral prosthesis rehabilitation was associated with an increase in regional brain activity. |
| Detection of Caries under Fixed Prosthodontic Restorations Using Cone-beam CT: A Meta-analysis (Sivaramakrishnan et al. [51]) | Bahrain | Meta-analysis | International Journal of Prosthodontics and Restorative Dentistry | This literature review sought to synthesize the data on cone-beam computed tomography’s (CBCT) ability to identify caries under fixed restorations. |
| Intraoral scanning devices applied in fixed prosthodontics (Abad-Coronel et al. [52]) | Cuenca | Dentistry | Acta Sci Dent Sci | Intraoral scanning devices applied in fixed prosthodontics (Abad-Coronel et al. [52]). |
| Efficacy of deep convolutional neural network algorithm for the identification and classification of dental implant systems, using panoramic and periapical radiographs: A pilot study (Lee, 2020 [53]) | Republic of Korea | Retrospective Cohort Study | Medicine | The aim of the current study was to evaluate the efficacy of deep CNN algorithm for the identification and classification of dental implant systems. |
| Artificial intelligence in fixed implant prosthodontics: A retrospective study of 106 implant-supported monolithic zirconia crowns inserted in the posterior jaws of 90 patients (Lerner et al., 2020 [54]) | Germany | Retrospective Cohort Study | BMC Oral Health | Purpose of this retrospective clinical study is to present a protocol for the use of AI to fabricate implant-supported monolithic zirconia crowns cemented on customized hybrid abutments, via a full digital workflow. |
| Predicting the debonding of CAD/CAM composite resin crowns with AI (Yamaguchi et al., 2019 [55]) | Japan | Retrospective Cohort Study | J. Dent. Res. | The aim of this study was to assess the validity of deep learning with a CNN method to predict the debonding probability of CAD/CAM composite resins restorations from 2D images captured from 3D STL models of a die scanned by a 3D oral scanner. |
| Detection and diagnosis of dental caries using a deep learning-based convolutional neural network algorithm (Lee et al., 2018 [56]) | Republic of Korea | Retrospective Cohort Study | J. Dent. Res. | The aim of the study was to evaluate the efficacy of deep CNN algorithms for detection and diagnosis of dental caries on periapical radiographs. |
| Diagnosis and prediction of periodontally compromised teeth using a deep learning-based convolutional neural network algorithm (Lee et al., 2018 [57]) | Republic of Korea | Retrospective Cohort Study | Journal of Periodontal Implant | The aim of the current study was to develop a computer-assisted detection system based on a deep CNN algorithm and to evaluate the potential usefulness and accuracy of this system for the diagnosis and prediction of periodontally compromised teeth. |
| Artificial Neural Networks as a powerful numerical tool to classify specific features of a tooth based on 3D scan data (Raith et al., 2017 [58]) | Germany | Retrospective Cohort Study | Comput. Bio. Med. | The hypothesis was that tooth classification algorithms based on ANNs are capable of classifying teeth with sufficient accuracy for potential use in clinical practice in order to improve digital workflow in dental prosthetics. |
| Evaluation of a Novel Computer Color Matching System Based on the Improved BackPropagation Neural Network Model. J. P (Wei et al., 2018 [59]) | China | Retrospective Cohort Study | J. Prosthodont. | [The aim of this study was] to explore the feasibility of a novel computer color-matching system based on the improved back-propagation neural network model by comparing it with the traditional method. |
| Features | p-Value |
|---|---|
| Diagnostic accuracy | 0.022 |
| Error reduction | 0.027 |
| Stars | Lerner, H.; Mouhyi, J.; Admakin, O.; Mangano, F. [54] | Lee, J.-H.; Jeong, S.-N. [53] | Lee, J.-H.; Kim, D.-H.; Jeong, S.-N.; Choi, S.-H. [56] | Yamaguchi, S.; Lee, C.; Karaer, O.; Ban, S.; Mine, A.; Imazato, S. [55] | Raith, S.; Vogel, E.P.; Anees, N.; Keul, C.; Güth, J.-F.; Edelhoff, D.; Fischer, H. [58] | Lee, J.-H.; Kim, D.-h.; Jeong, S.-N.; Choi, S.-H. [57] | Wei, J.; Peng, M.; Li, Q.; Wang, Y. [59] |
|---|---|---|---|---|---|---|---|
| Determination (Max. 4 Stars) | *** | ** | ** | *** | ** | ** | * |
| Comparison (Max. 2 Stars) | - | - | - | * | - | - | - |
| Outcome (Max. 4 Stars) | * | * | * | * | * | * | * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alshadidi, A.A.F.; Alshahrani, A.A.; Aldosari, L.I.N.; Chaturvedi, S.; Saini, R.S.; Hassan, S.A.B.; Cicciù, M.; Minervini, G. Investigation on the Application of Artificial Intelligence in Prosthodontics. Appl. Sci. 2023, 13, 5004. https://doi.org/10.3390/app13085004
Alshadidi AAF, Alshahrani AA, Aldosari LIN, Chaturvedi S, Saini RS, Hassan SAB, Cicciù M, Minervini G. Investigation on the Application of Artificial Intelligence in Prosthodontics. Applied Sciences. 2023; 13(8):5004. https://doi.org/10.3390/app13085004
Chicago/Turabian StyleAlshadidi, Abdulkhaliq Ali F., Ahid Amer Alshahrani, Lujain Ibrahim N. Aldosari, Saurabh Chaturvedi, Ravinder S. Saini, Saeed Awod Bin Hassan, Marco Cicciù, and Giuseppe Minervini. 2023. "Investigation on the Application of Artificial Intelligence in Prosthodontics" Applied Sciences 13, no. 8: 5004. https://doi.org/10.3390/app13085004
APA StyleAlshadidi, A. A. F., Alshahrani, A. A., Aldosari, L. I. N., Chaturvedi, S., Saini, R. S., Hassan, S. A. B., Cicciù, M., & Minervini, G. (2023). Investigation on the Application of Artificial Intelligence in Prosthodontics. Applied Sciences, 13(8), 5004. https://doi.org/10.3390/app13085004









