Abstract
Background: Patellar instability can cause pain and disability. A finite element model of a healthy human knee was performed to analyze the role of quadriceps and medial retinaculum imbalance in patellar instability. Methods: The model was created by matching magnetic resonance and computed tomography images of a normal adult patient’s knee. Muscle force intensities were calculated by static optimization, considering the lower limb muscles, knee movement and the ground reaction during walking. Patellar instability was experimentally generated by progressively uncoupling muscular forces, (90 N versus 110 N), while at the same time, the load derived from the quadriceps was gradually reduced by 20%. Results: This loss in force symmetry of 10 N on the retinaculum may produce a displacement of approximately 7 mm, with an increase in patellar contact forces of approximately 44%. When the quadriceps force is reduced by 10% and the unbalanced medial retinaculum acts together, the displacements are in the order of 14 mm, and the patellar contact forces increase by 84%. Conclusion: A reduced quadriceps force alone is not able to cause significant patellar instability, while an imbalance of forces at the level of the retinaculum could lead to patellar instability, especially when the two effects are combined. A better understanding of joint relationships and muscle synergies can help to improve clinical approaches to patella instability
1. Introduction
The knee joint is essential for movement, standing, and walking, and is the focus of much research into therapeutic treatments and biomechanical modelling [1]. Data on the biomechanics of the knee, the response to external forces, combined with the mechanical properties of the individual tissues involved, can be used to better understand joint disease [2].
The knee joint is a highly mobile joint made up of the tibial–femoral and patellofemoral joints [3], the first consists of two geometrically incongruent bone segments, the femur, and the tibia, which are joined by the condyles of the femur and the tibial plateau, between which the menisci are located [4]. These two bony ends are covered by a strong fibrous capsule which holds them together in synergy with the action of the ligaments, which, combined with the geometry, restrict movement [5,6]. On the other hand, the patellofemoral joint is composed of the patella and the trochlear surface, which are morphologically related, i.e., the patella has an optimised surface for sliding over the femur, which in turn forms a groove that acts as a track for the patella [7].
Bone surfaces are covered by a superficial layer of cartilage that promotes gliding and contributes to cushioning [4]. The ability of the knee to move in different planes varies according to the angle of flexion–extension and the patellofemoral joint holds a prominent place in these movements [8]. In fact, the patella is a fundamental contributor to knee dynamics because it is the point where the quadriceps muscle bundles converge [9].
The connection between the patella and the femur is provided by the quadriceps muscle tendon and the patellofemoral joint is functionally dependent on the patellar tendon insertion because it improves biomechanics during knee extension [5].
The patella is stabilized by several structures, such as the patellar tendon, retinacula (lateral and medial) and quadriceps tendon distal portion [10]; the retinacular ligaments, also called the patellofemoral and patellotibial ligaments, connect the patella to the femoral condyles and the patella to the front of the tibia [11].
Thus, at maximum knee extension in the frontal plane, the patella is in a medial position between the femoral condyles, in a relaxed and slightly mobile state [12]. In this condition, it is possible to identify the direction of quadriceps traction, the Q angle, which is the angle between the quadriceps traction line and the patella centre and the line joining the patella to tibial tuberosity [13].
In addition, the patella plays an important biomechanical role during flexion–extension movement, adapting extension quadriceps force and moving the point of application to a more favourable position [10].
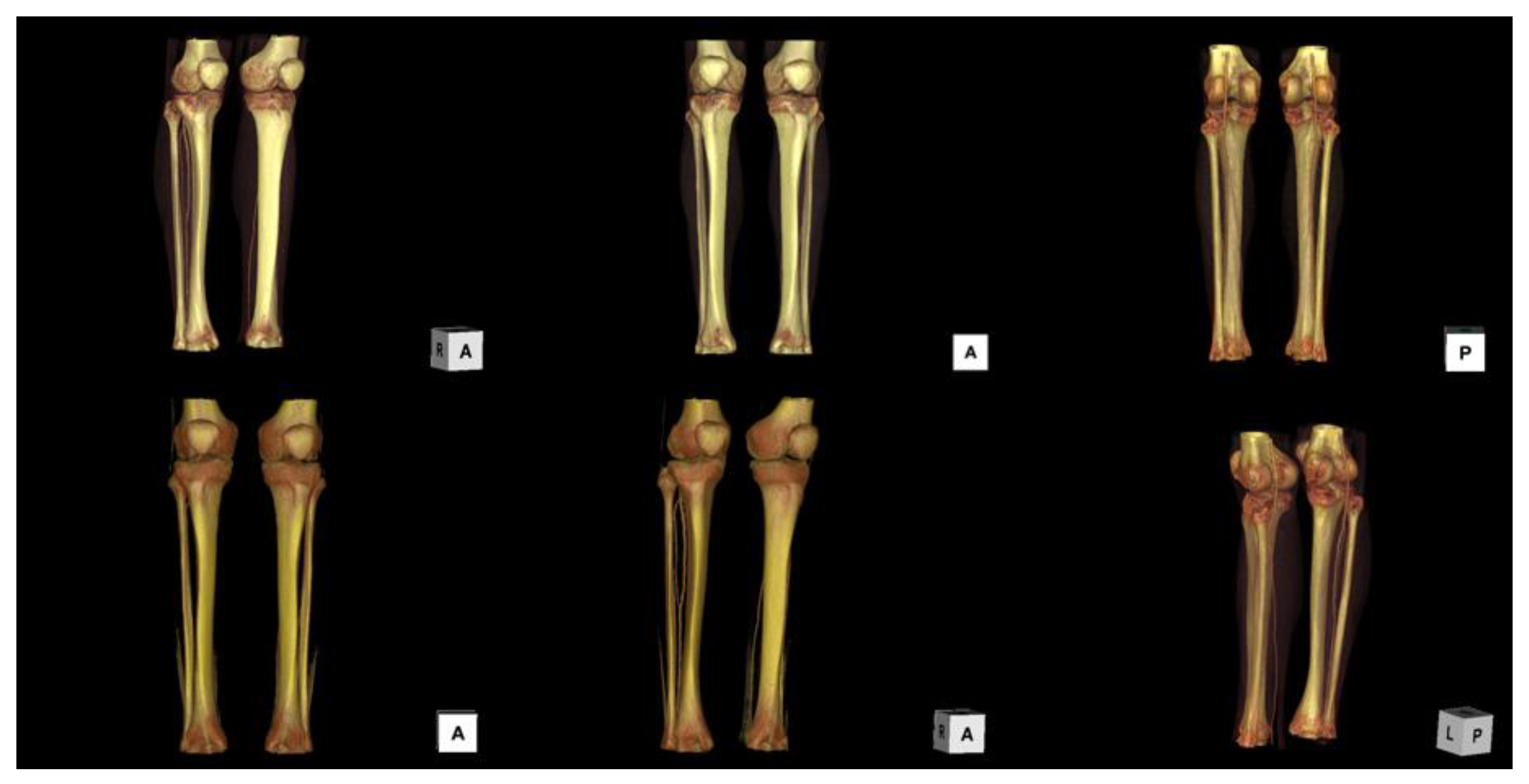
The most significant patellar movement occurs in the sagittal plane, but significant horizontal sliding is possible in the frontal plane [7]. In order to provide an anatomical description, as has been done previously by other authors [14], Figure 1 shows a 3D volume rendering of the knee from the TC images. During the flexion–extension movement, the patella is guided by the posterior action of the quadriceps muscle, which forces it to slide along the geometric coupling with the femoral groove [15].
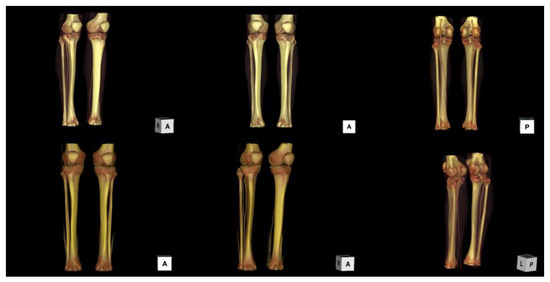
Figure 1.
Representation of the knee in different planes by 3D volume rendering of TC images.
Patellar instability occurs when the patella does not slide correctly over the femur, causing a dislocation, and accounts for 2–3% of knee accidents with 6/100,000 patients’ yearly incidence, rising to 29/100,000 in teenagers [16,17,18]. This condition can be caused by injury to the patellar ligaments, muscle imbalances, anatomical deformity, or changes in biomechanics, often leading to pain and disability [19,20,21].
The medial patellofemoral ligament (MPFL) is the main resistance ligament during lateral dislocation and has the highest frequency of accidents [16,22].
Clinical signs of patellar dislocation may include knee effusion, bone bruising and damage to the MPFL and medial retinaculum [5,23], making approximately one third of patients susceptible to repeated dislocation [24]. In addition, the main complications can be pain and functional limitations in the short term and, over time, cartilage damage and osteoarthritis, leading to a deterioration in the quality of life [25].
The risk of recurrent dislocation may be increased by anatomical problems, i.e., MPFL incompetence, trochlear anatomical changes, and tibial tubercle lateralisation [26,27,28]. Therefore, a better understanding of the anatomical stability factors of the patella is required to guide effective treatment [29,30,31].
The study of patellofemoral joint stability has been the subject of much research, focusing on the interaction of various factors, including quadriceps muscle forces, retinacular structures, tibial rotation, and articular geometry [31,32]. Some authors have extended the analysis of Q-angle [33,34], quadriceps tension imbalances [35] and retinacular releases on patellar kinematics and contact patterns [36]. Others have examined the role of tibial rotation and the correlation between patellar tracking and femoral and patellar topography [37,38,39].
Bone abnormalities associated with patellar malalignment include conditions such as high or low patella, high tibial tuberosity, trochlear dysplasia, shallow or convex intercondylar fossa, patellar dysplasia, external tibial rotation, or internal femoral rotation [40,41]. Many studies have investigated the weakened vastus medialis obliquus (VMO) muscle as a cause of patellar malalignment, as it is unable to adequately limit patellar displacement and loses its stabilising effect [42,43].
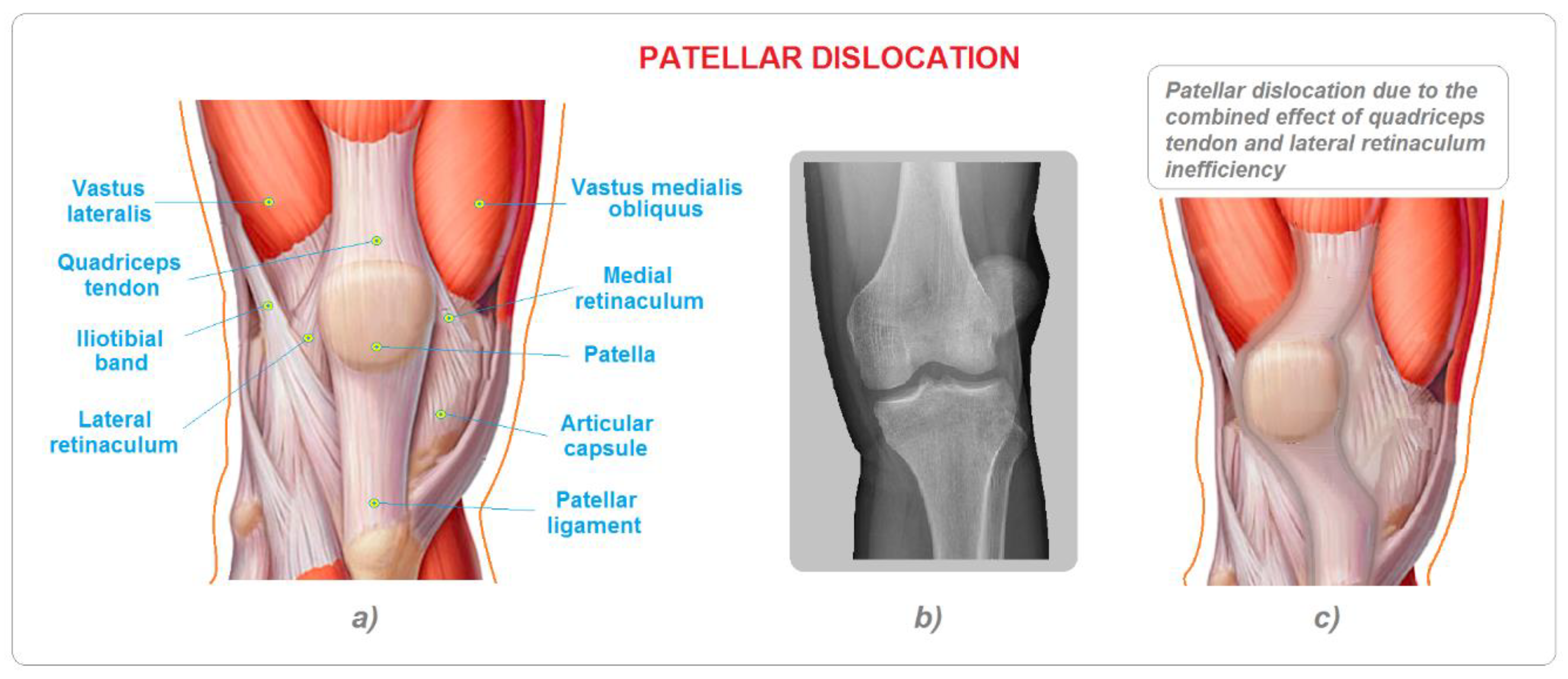
Other soft-tissue abnormalities associated with patellar malalignment include medial retinaculum damages, augmented Q-angle, lateral retinaculum resistance, hamstrings, iliotibial band, and vastus lateralis (Figure 2) [44]. Some authors support the thesis that changes in patellar alignment are due to a general malfunction in the synergies of the joints of the lower limb, particularly in imbalances of forces between the extrarotator and intrarotator hip muscles [45,46].
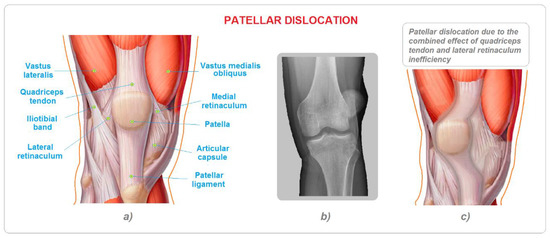
Figure 2.
(a) Anatomical representation of a normal knee; (b) radiological image in antero-posterior projection of patellar dislocation; and (c) anatomical representation of a patellar dislocation.
However, less attention has been paid to the patellar lateral ligaments; in fact, only a few studies have investigated the role of the different medial retinaculum portions [47,48]. Previous studies have analysed the patellar lateral displacement restraint-force variations during knee flexion and quadriceps loading [49]. However, although many studies have only looked at specific anatomical areas, others have attempted to take a broader view by extending the analysis to all the joints of the lower limb [50]. The main objective of this study was to provide greater knowledge of the quadriceps muscles and the role of the medial retinaculum structures in providing stability to the patellofemoral joint, using numerical finite element (FE) modelling. The model was developed to assess the specific contribution of the quadriceps tendon, by reducing its intensity by 10%, and the retinaculum structure to the imbalance of the left aging forces on the patella. This approach can provide interesting information on the forces involved in patella displacement at different knee-flexion angles and can offer possible new insights on stabilising contributions of the structures involved. A better understanding of the causes of patellar dislocation and the muscular implications can help to guide treatment strategies for patellofemoral instability disorders.
2. Material and Methods
2.1. Computational Modelling
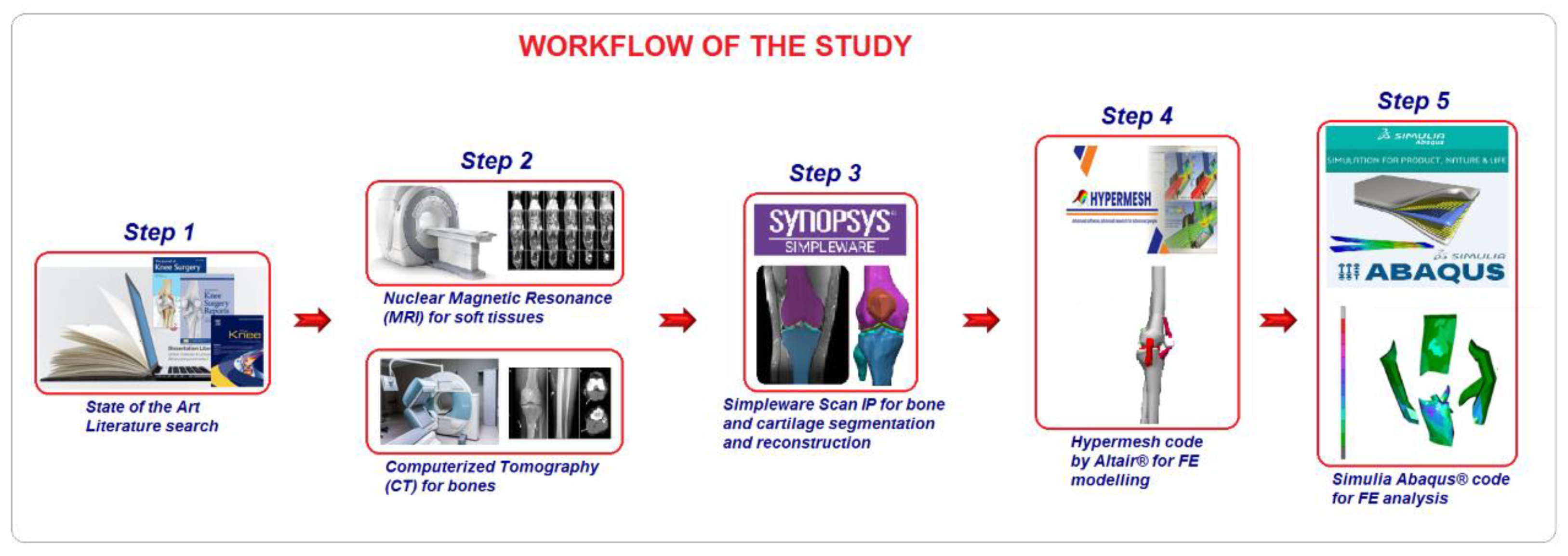
Magnetic resonance (MR) and computed tomography (CT) images of a healthy adult were combined to create a numerical model of the knee [51]. Data were imported into the commercial Hypermesh code by Altair®, where the final FE model was realized. The final FE models were developed in Abaqus® CAE ver. 6.14-2 [52]. Figure 3 provides a workflow of the study.
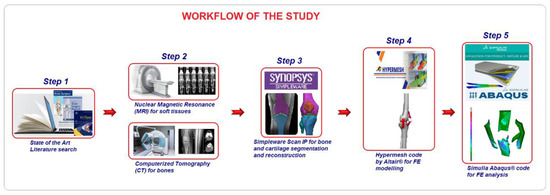
Figure 3.
Study workflow.
2.2. Material Properties
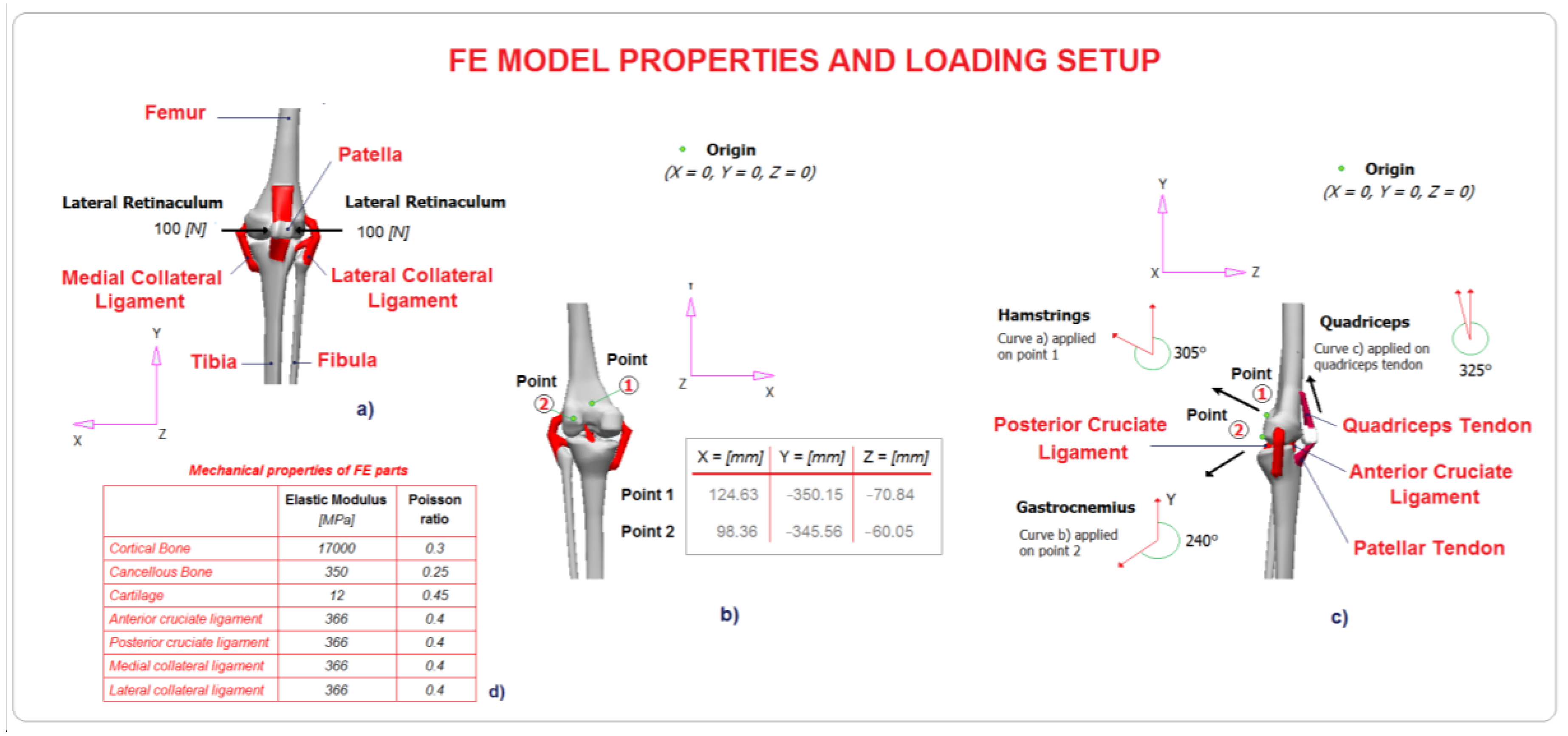
The homogeneous and linearly elastic law was chosen to characterize the material behaviour of the cortical and spongious bone and cartilage. From data in the literature, the authors chose the elastic moduli and Poisson’s ratio [51]. Solid structures were modelled for the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL), while the medial and lateral retinacula were simulated with a symmetric load of 100 N applied to the patella left and right lateral sides. A mesh convergence test was performed using an iterative process governed by the reduction of the average element length and the stress values obtained.
2.3. Model Loading
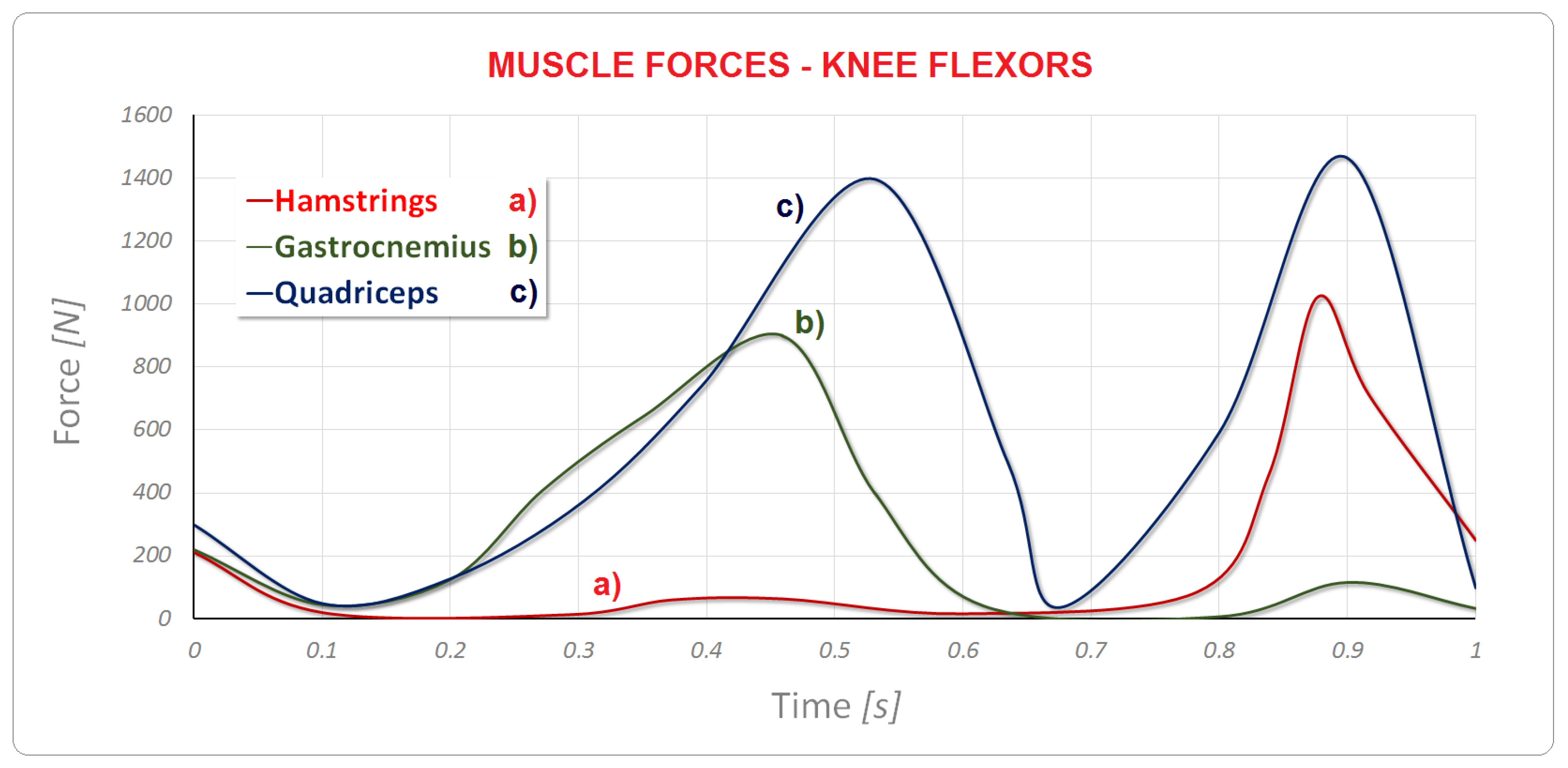
The loading setup was selected from data in the literature (Figure 4) [51]; the hamstring contribution was applied to point 1 and the gastrocnemius contribution was applied to point 2, as shown in Figure 5. Finally, the tension force given by the muscle was applied on the quadriceps tendon. The tibia was restrained at the lower extremity. In addition, to investigate the contribution of different forces to patellar instability, the quadriceps tendon force was gradually reduced by 10% and an asymmetrical load of 90 N on the left and 100 N on the right was applied to the patella, simulating a weak lateral retinaculum. The patellofemoral contact behaviour was set as frictional (coefficient of 0.2). The surface cartilage was attached to the bone using the same coefficient of friction [53].
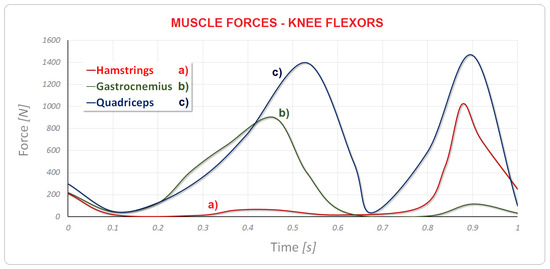
Figure 4.
Model muscle forces: (a) hamstrings; (b) gastrocnemius; and (c) quadriceps.
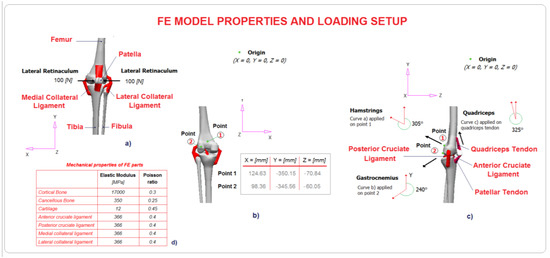
Figure 5.
Loading setup of numerical FE model: (a) X-Y planar view of the numerical model detailed with bony and soft components, with reference to a balanced retinaculum condition; (b) coordinates of points 1 and 2 where loads were applied, with reference to the origin; (c) Y-Z planar view of the numerical model detailed with bony and soft components, with muscular loads applied to points 1 and 2, with angles of application; (d) mechanical properties of the FE parts.
3. Results
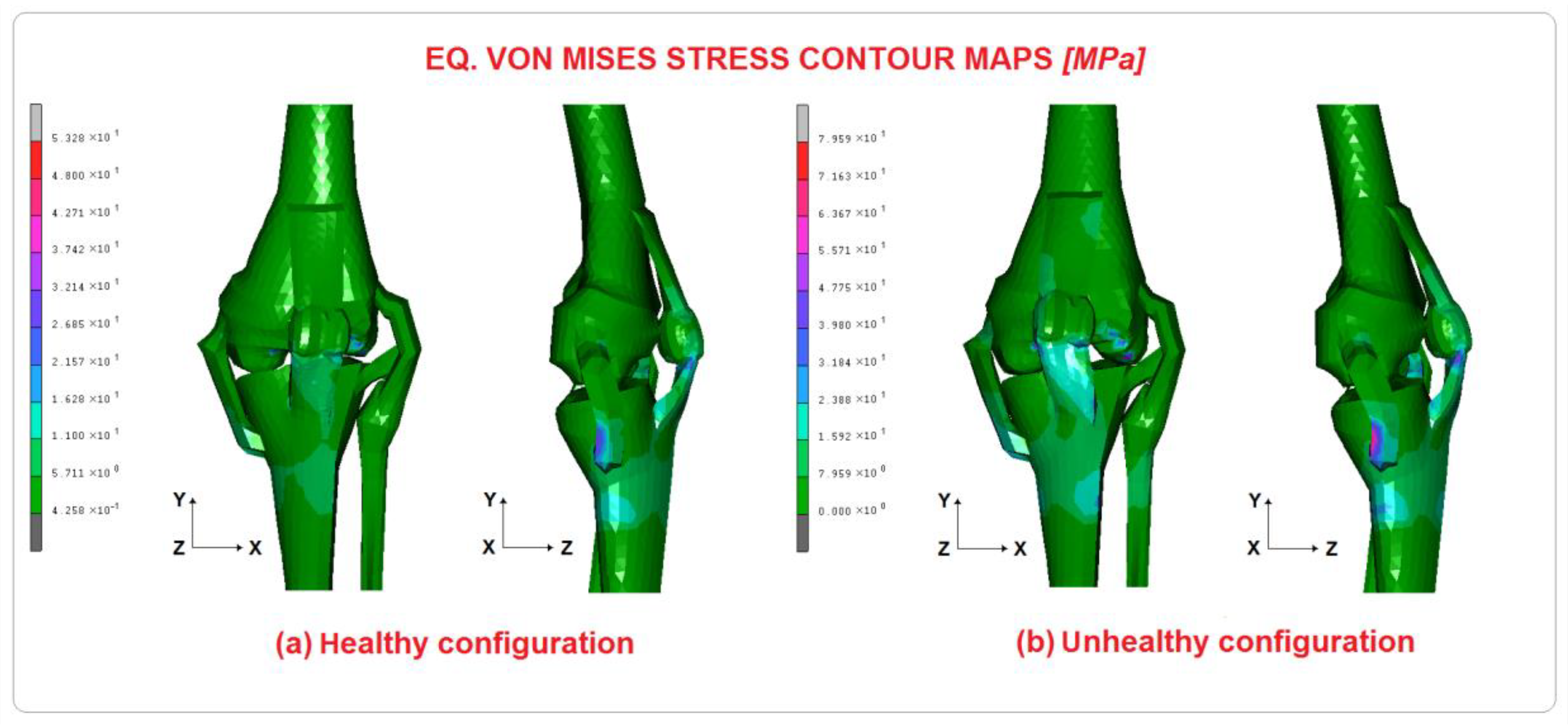
An FE model was developed, taking into account the physiological conditions resulting from the loads produced by the hamstrings, gastrocnemius, and quadriceps muscles on the knee range of movement. To investigate the quadriceps tendon and the lateral retinaculum isolated action in patellar instability, different loading cases were performed, reducing the quadriceps tendon intensity force at 90% and unbalancing the lateral retinaculum at 90 N. Figure 6 shows the stress-contour maps evaluated for a healthy knee, (a) configuration, without patellar instability induced, and an unhealthy one, (b) configuration, obtained with a force of 90 N applied to the lateral retinaculum, while the medial is loaded with 100 N, and a quadriceps tendon force reduced by 10%. As can be seen from Eq., the von Mises stress is higher in configuration (b), about 79 MPa instead of 53 MPa found in configuration (a), which is a percentage difference of 49%. Table 1 shows the maximum stress peaks on the FE models. The results confirm the obvious variances in the femur and patella with respect to the two configurations studied, with differences of 49% and 30%, respectively. It can be argued that the patellar tendon is subjected to the higher stress in (b) configurations and the percentage difference is 43%, followed by the posterior cruciate ligament with 34%.
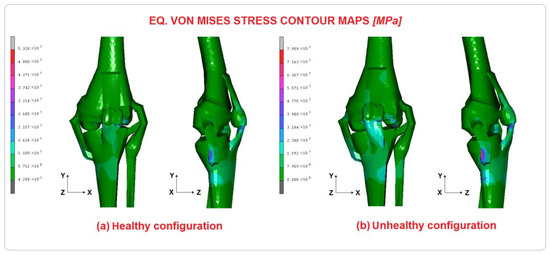
Figure 6.
Eq. von Mises contour maps for healthy and unhealthy configuration.

Table 1.
Stress values calculated on the bony parts and percentage difference.
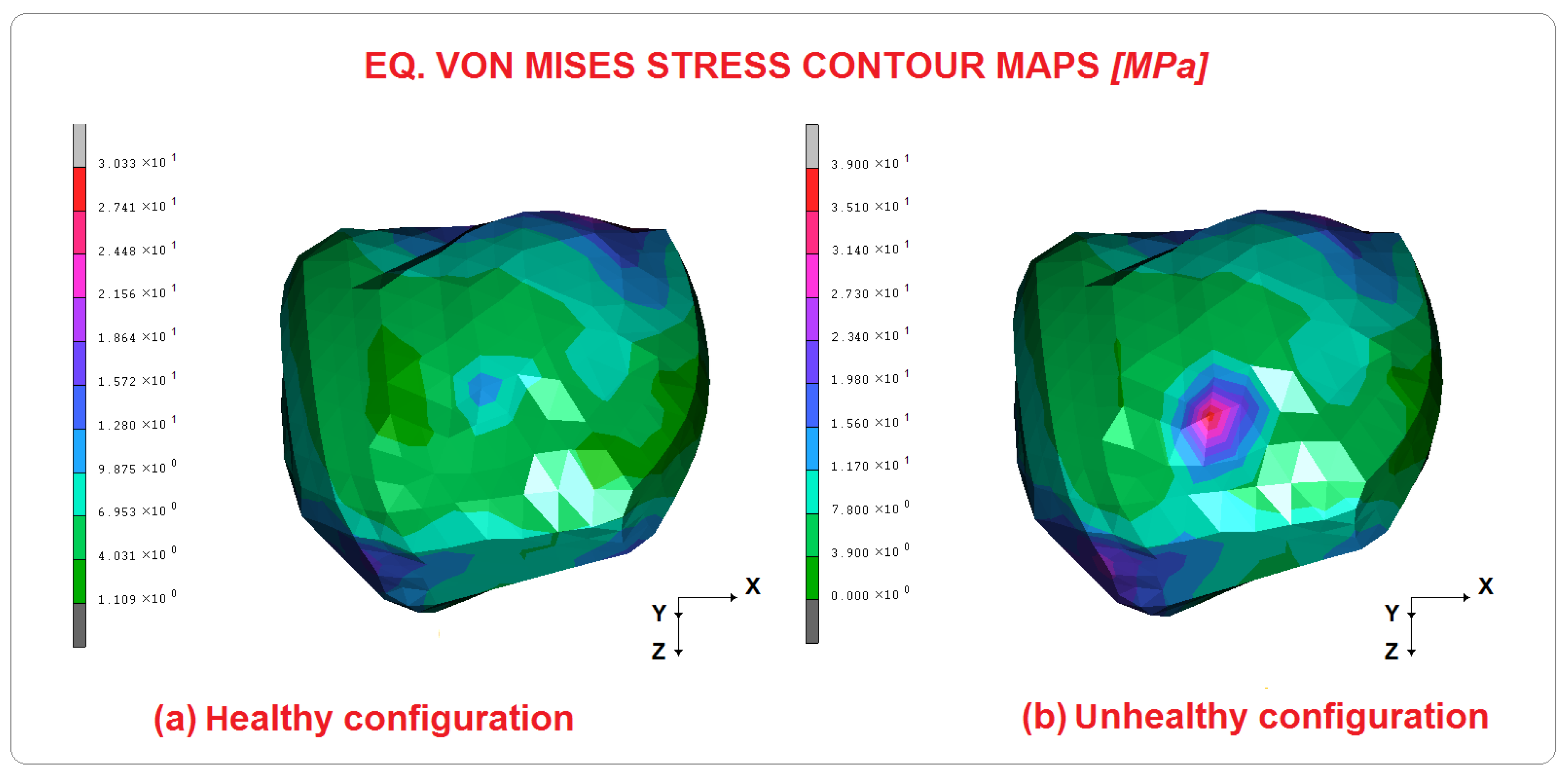
Different considerations must be made for the displacements, which show significant differences only for the patella translations. In configuration (a), its displacement is approximately 5 mm, while in configuration (b) it is 14 mm. Figure 7 shows a detailed comparative Eq. von Mises contour map of the patella. As has already been said, important differences were obtained in terms of stress, evidenced by the significant contact area shown by the unhealthy configuration. The patella right upper part is the contact area, which cannot structurally withstand this type of stress, such as the femur. The displacements obtained are 5 mm in (a) and 14 mm in (b). In addition, a reaction force of 60 N was evaluated in patella for (a) configuration at 45° of knee flexion, and 130 N for (b).
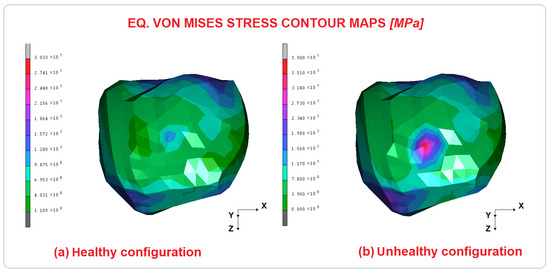
Figure 7.
Eq. von Mises contour maps for healthy and unhealthy configuration of the patella.
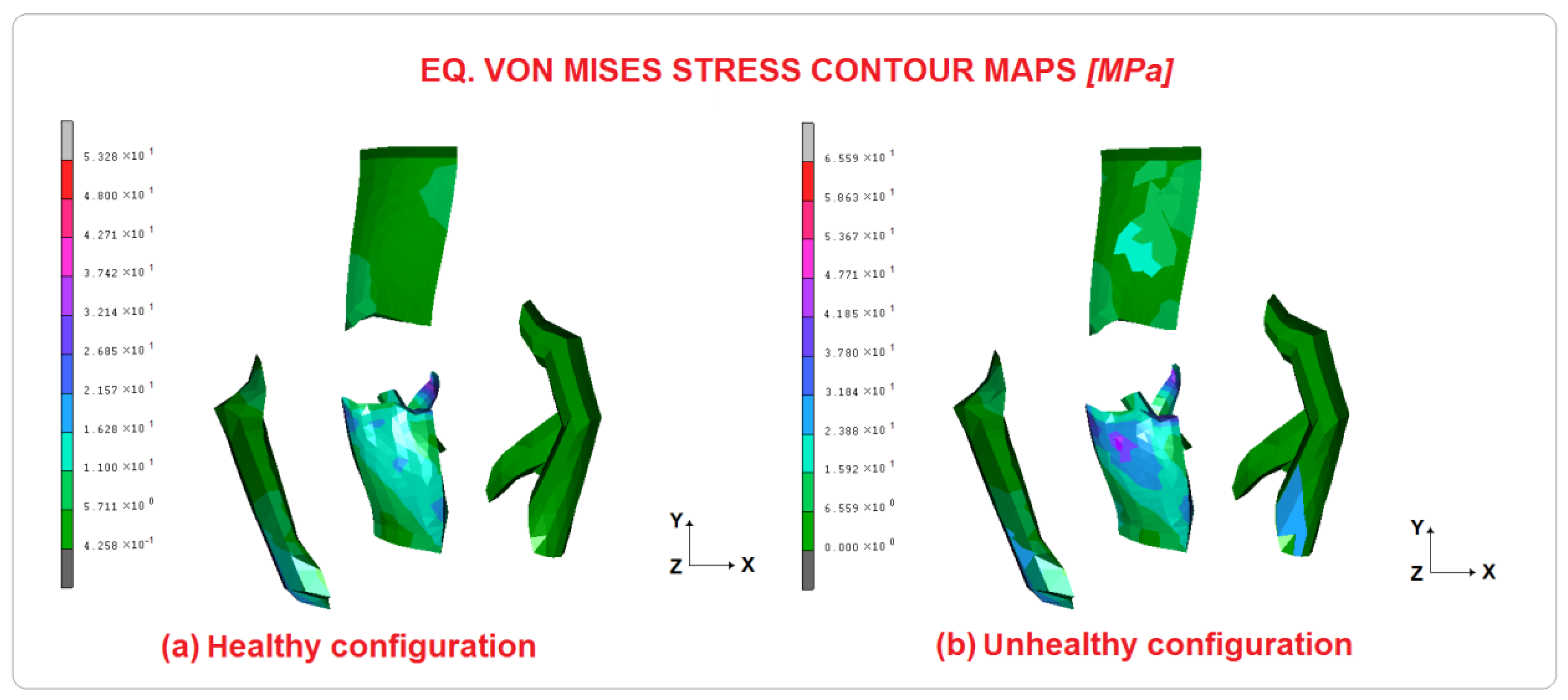
The ageing stresses in the elastic components of the model (i.e., ligaments and cartilage) are represented in Figure 7 and Figure 8 and Table 2. Soft tissues are fundamental for the absorption of the incremental stress caused by the patella’s non-physiological position, specifically the patellar tendon is subjected to a higher stress of 43%, while in the PCL, the difference is approximately 34%. This, of course, depends on the forces at work: the patella translates laterally while the tendons try to correct its position. Similarly, both the lateral and medial collateral ligaments undergo an increased load of 19% and 23% respectively. On the other hand, the femoral and tibial cartilages are subjected to 25% and 21% more stress, respectively.
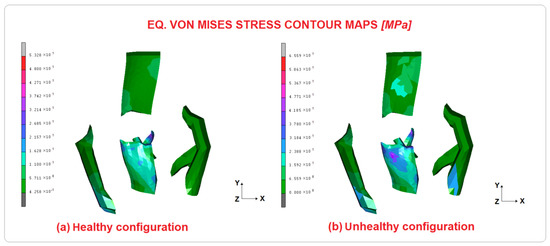
Figure 8.
Eq. von Mises contour maps for healthy and unhealthy configuration of soft tissues.

Table 2.
Stress values calculated on soft tissues and percentage difference.
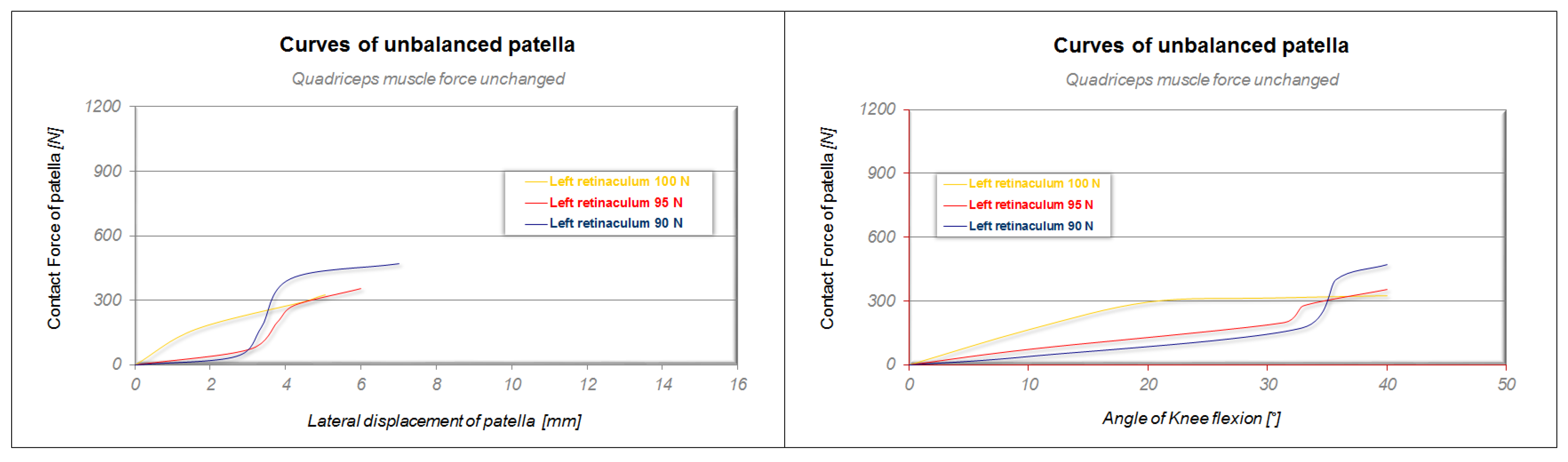
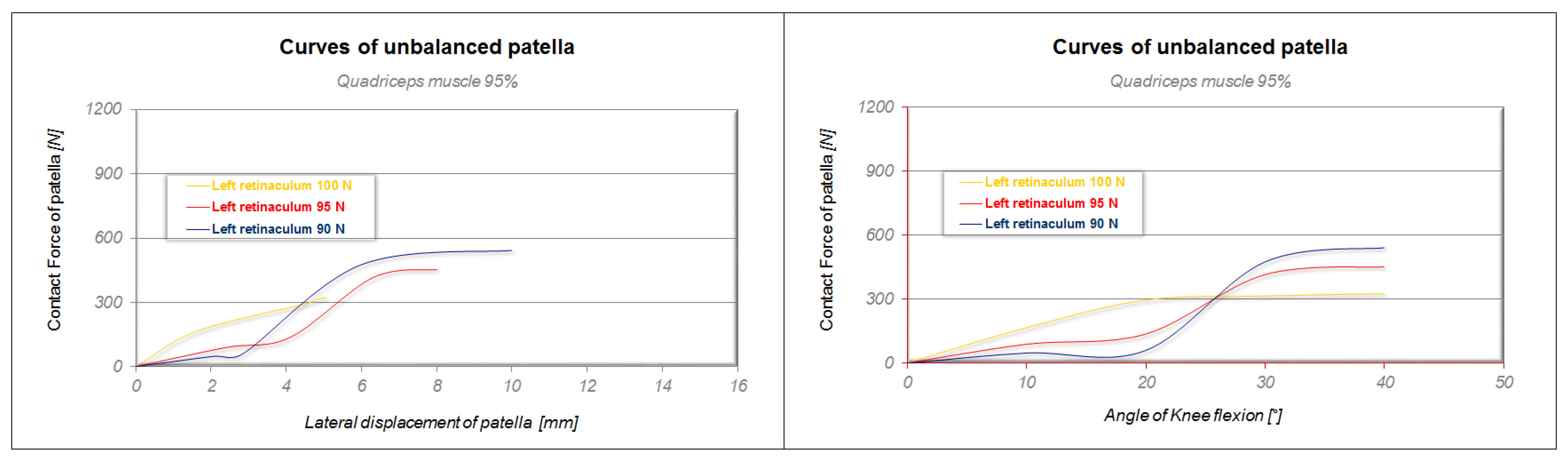
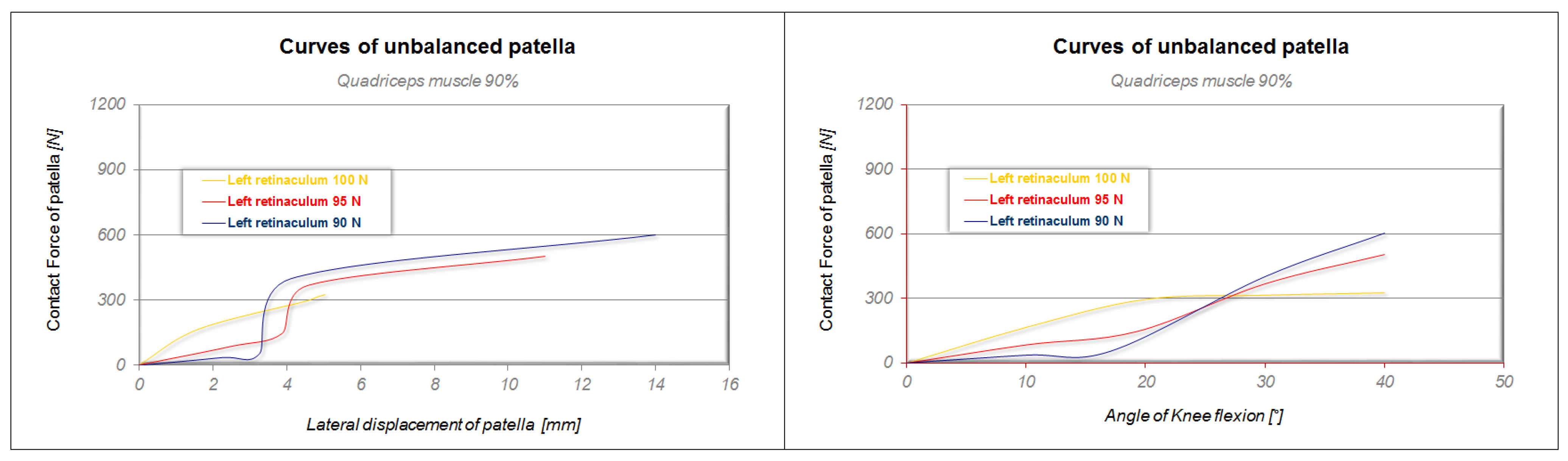
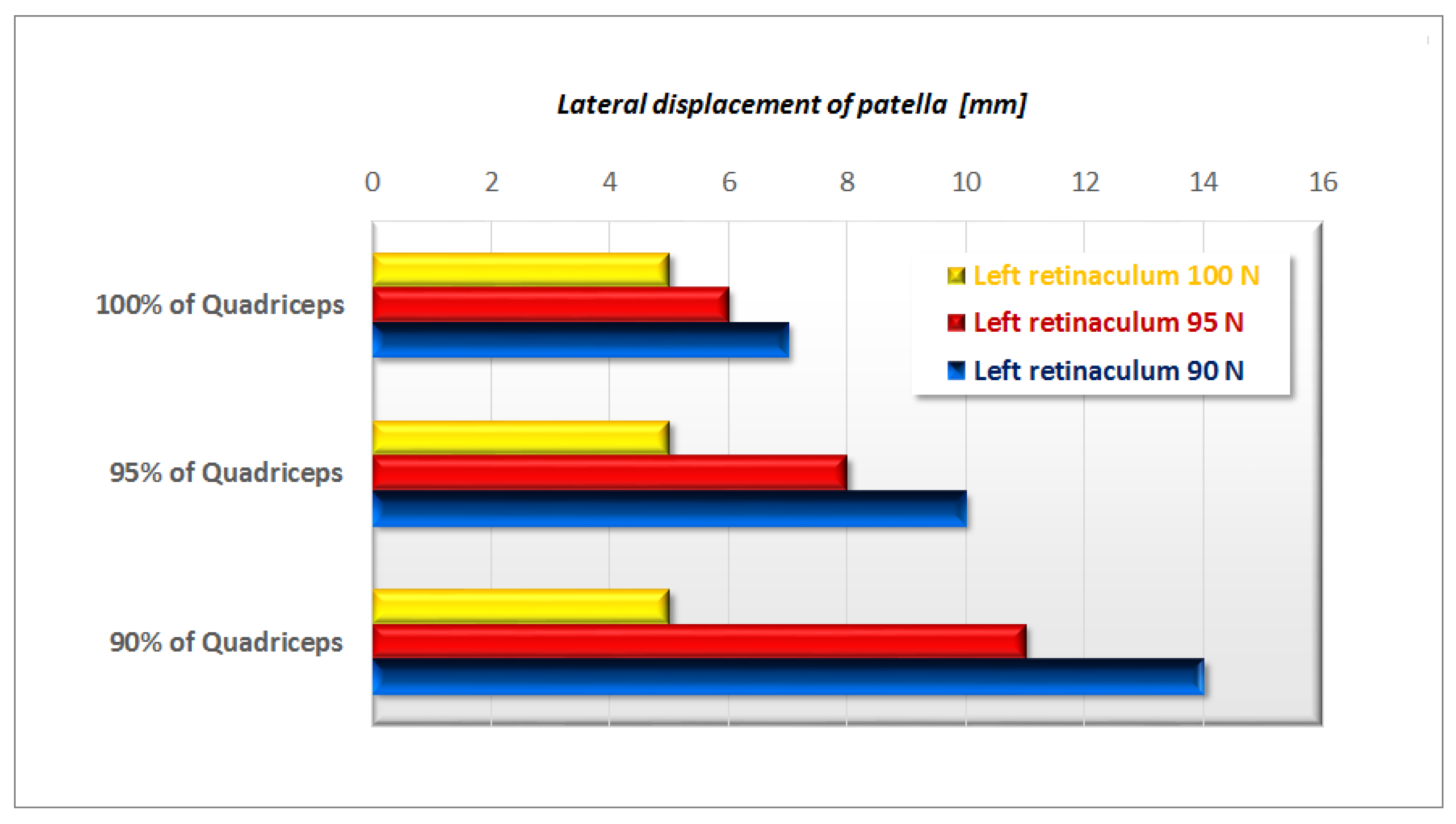
Figure 9, Figure 10 and Figure 11 report the contact forces of the calculated patella curves versus its lateral displacement and knee-flexion angle, plotting the results extracted by numerical simulations as a function of decreasing quadriceps’ muscle force (from 100% to 90%) and unbalanced medial retinaculum force (from 100 N to 90 N). The yellow curve in Figure 9 represents the healthy knee configuration (quadriceps force 100%, retinaculum balanced) with an increasing trend, and no slope changes. The displacement maximum is approximately 5 mm, and this behaviour is the same for Figure 10 and Figure 11 (contact force about 320 N). The simulations were performed up to 40° knee flexion. The red and blue curves refer to an imbalance of the left retinaculum of 95 N and 90 N, respectively, with respect to the right retinaculum, which is always equal to 100 N. The final displacements are 6 and 7 mm, respectively, and the slope of both curves is less accentuated than the yellow one during contact. This is due to the low resistance offered by the unbalanced retinaculum. Between 3 mm, for the blue curve, and 4 mm, for the red curve, of displacement, the trend suddenly has an increase in its trend due to the malalignment of the patella. This is confirmed by the other graph, where this phenomenon occurs at around 35° of knee flexion. The contact forces are 354 N in the case of the left retinaculum, equal to 95 N and 470 N in the other. The other two series of numerical simulations were performed, reducing the quadriceps muscle intensity to 95% and finally to 90%, as shown in Figure 10 and Figure 11. The behaviour of all the red and blue curves is quite complicated because of the different ways in which the dislocated patella slips and slides between it and the femur. The first phase of patellar dislocation always occurs at 3 mm for the blue curve and at 4 mm for the red one, while after this the displacements start to increase until 8 mm in the case of the left retinaculum equal to 95 N and 10 mm in the other, with respect to 95% of the quadriceps force. There are also contact forces of 450 N and 540 N. The knee-flexion angle curves show the difference of the tendency at 20°. Finally, the displacements reach 11 mm on the red curve and 14 mm on the blue curve with a quadriceps force of 90%. In this case, the flexion point on the knee-angle curves is reached by the curves at 15° and the contact forces are 500 N for the red curve and 600 N for the other. Figure 12 shows a meaningful histogram representing the correlation between reduced quadriceps strength with increased left medial retinaculum imbalance.
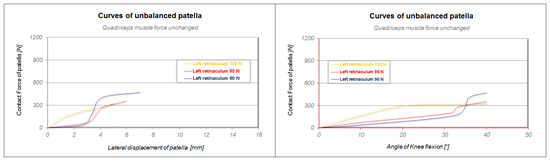
Figure 9.
Contact-force curves versus lateral displacements and knee-flexion angle for a quadriceps force unchanged.
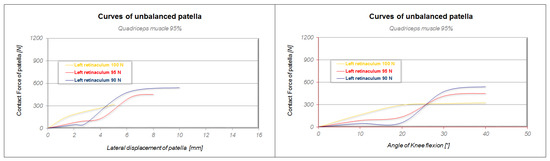
Figure 10.
Contact-force curves versus lateral displacements and knee-flexion angle for a quadriceps force equal to 95%.
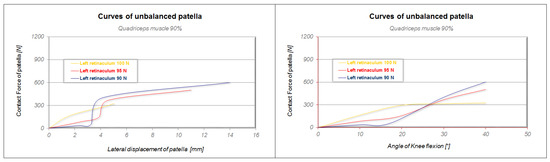
Figure 11.
Contact-force curves versus lateral displacements and knee-flexion angle for a quadriceps force equal to 90%.
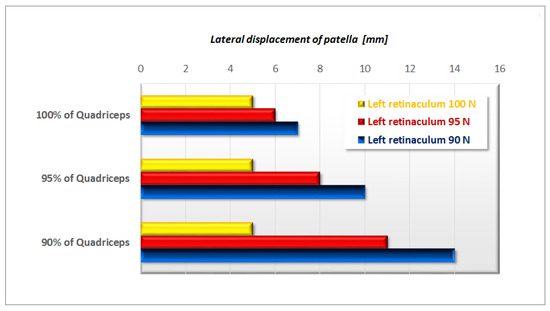
Figure 12.
Histogram showing correlation between the effects of quadriceps decreased force in addition with an increased unbalancing of the left medial retinaculum.
4. Discussion
The simulations considered the effects of the hamstrings, gastrocnemius, quadriceps, and medial retinaculum during knee flexion and how an imbalance of these structures could cause patellar instability and displacement, leading to pain, reduced function, and potentially osteoarthritis. Clinical studies have shown that restoring normal knee function in cases of patellar instability is difficult and that a multidisciplinary approach is required to better understand knee biomechanics to determine the most appropriate strategy treatment [15,35,54]. FE analysis, supported by clinical studies, can lead to a better disease-management approach in terms of time, results, and improved healthcare costs [55]. Effective treatment options are important to improve patient outcomes and prevent further deterioration; thus, conservative treatment through gradual muscle-strengthening and improvement of joint proprioception plays a fundamental role in the management of the pathology [7]. Prevention is also essential in patients with anatomical and biomechanical predispositions, and in those with a history of dislocation [25]; however, the best treatment for patellar instability remains controversial, with differing opinions regarding surgical versus non-surgical approaches and the most effective surgical techniques [27].
The results showed that the combined effect of quadriceps intensity and lateral retinaculum weakness produced a patellar displacement of 14 mm and increased stress in the contact area from a knee-flexion angle of 25–30°. These are in line with other studies. Ahmed et al. and Goh et al. simulated muscular forces using wires to induce patellar instability [56,57,58].
The stresses acting in the FE model were analysed in terms of the equivalent von Mises stress and the results confirm maximum values of approximately 80 MPa. According to Ammarullah et al., the von Mises stress criterion is a very useful instrument to predict material failure, based on the consideration that when the material reaches the yield stress during numerical simulation, it loses its elastic properties and cannot return to its original shape, causing complications related to dislocation initiation or interactions with the contact interface, among others [59].
Furthermore, Farahmand et al. developed a patellofemoral loading system to study the effects of the quadriceps and medial retinaculum by studying it in vitro and obtained a patellar-restraint force of approximately 50 N, which correlates with a 5 mm lateral displacement of the patella in a healthy knee [60].
Quadriceps forces had important clinical implications for patellar stability, so that when the distribution of quadriceps forces changed, so did the holding force [33]. The study highlights the important role of both active (quadriceps muscles) and passive (medial retinaculum) restraints in the assessment and treatment of patellar instability. Clinical findings and the literature report similar results, including that the vastus medialis contributes to patellar subluxation and dislocation [40,42,61]. At maximum knee extensions, the soft tissues, muscles and retinacula perform a restraining effect on the patella lateral displacement [11] and during knee flexion, the femur and patella are engaged, resulting in an increased joint compression force vector [47]. This results in an almost constant holding force from 0 to 60° flexion, despite the diminishing effect of the retinacular structures [29]. The patella makes contact with the femur at approximately 10° of flexion, while the role of the retinaculum decreases with flexion, becoming almost zero at 35–45° of flexion [32]. The reduction in restraint by the retinacular structures during knee flexion is counteracted by the increase in joint compressive force due to the relationship of the quadriceps—patellar tendon, resulting in almost constant restraint [62].
Overall, the results suggest that at around 25° of knee flexion, patella alignment is maintained by bony anatomy. A second adjustment phase is due to the elasticity of the ligaments and tendons. When quadriceps strength is at 90% with an unbalanced lateral load (90 N), the phenomenon becomes more pronounced and can occur at around 15–20° of knee flexion. In cases of ‘high patella’, the patella is unable to follow the anatomy of the bone, which can lead to dislocation [63]. The study suggests that a knee-flexion angle of 25° may be the most dangerous for possible patellar instability. Many studies have investigated the role of the quadriceps in patellar stabilisation and dislocation, suggesting that a balance between the forces of the individual muscle components is necessary for patellar stability. In particular, the vastus obliquus medialis fascia plays a crucial role during flexion–extension movements, assisted by the medial and lateral retinaculum [64,65,66].
These muscle synergies are also supported by numerous studies showing the negative effect of imbalanced forces after vastus lateralis tendon release surgery alone [67], or medial plication [68], demonstrating that a whole-joint procedure is the best solution [69,70]. As a result, these data support both preventive and post-operative rehabilitation for patellar instability using both clinical assessment and radiological parameters [66].
Over the years, several FE models have been developed to determine bone stress shielding under paraphysiological conditions or after replacement surgery, confirming that the model appears to be an effective tool for investigating knee biomechanics [71,72,73]. In addition, other authors emphasise the forces due to body weight, with different effects depending on the body-mass index, which also affect both the body joint and prosthesis [74,75].
Recently, other studies have investigated various clinical conditions using FE to study knee pathologies such as osteoarthritis, high patella, anatomical changes, and surgical reconstructions [76,77,78,79].
Our results are in line with other studies, such as the cadaver study by Nomura et al. that showed that when a lateral displacement force (10 N) occurs, patella displacement is about 6 and 13 mm, respectively, with a normal medial patellofemoral ligament [80]. Other authors have demonstrated how lateral imbalance could reduce the force required to dislocate the patella by 10 mm at different angles, by approximately 20% [81].
The present study has several limitations. First, the FE model analysis results are highly dependent on the data input and setup of the experimental model to approximate a real joint with loads that also depend on in vivo tissue characteristics. The simulation also remains an artificial version of reality with all its limitations, including the absence of important anatomical elements in the dynamics of the joint (i.e., menisci) capable of effectively transmitting loads through the joint and absorbing shocks. In addition, as with other FE models, tissue properties were approximated and therefore the data obtained may be moderately different. The proposed finite element model was fully customised in terms of the loading conditions imposed during the simulation and was based on a single subject.
5. Conclusions
The authors aimed to prove that reduced quadriceps strength alone is not capable of producing significant patellar instability, otherwise unbalanced retinaculum forces can produce a real difference in displacement on contact patellar forces. Very interesting results can be obtained by analysing the combined effect of the two factors, when a weak quadriceps muscle and the unbalanced medial retinaculum act simultaneously, highlighting the importance of considering the forces generated by the quadriceps muscle and the asymmetric forces on the medial retinaculum when assessing patellar instability. Future research could implement the accuracy of the materials to make the FE as similar to the human body as possible, using images from multiple subjects to make the model applicable to the general population. A further future development may be to simulate specific defects in the articular cartilage and bone components to understand how features such as size, position, and possible structural abnormalities may influence the stresses on the patella and promote instability.
Author Contributions
Conceptualization, Writing—original draft, Methodology, Supervision, A.A.; Investigation, Data curation, Software Validation, Conceptualization, Writing, V.F.; Review, Editing supervision, Methodology, D.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Erdemir, A. Open Knee: Open Source Modeling and Simulation in Knee Biomechanics. J. Knee Surg. 2016, 29, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Shao, B.; Xing, J.; Zhao, B.; Wang, T.; Mu, W. Role of the proximal tibiofibular joint on the biomechanics of the knee joint: A three-dimensional finite element analysis. Injury 2022, 53, 2446–2453. [Google Scholar] [CrossRef] [PubMed]
- Biko, D.M.; Miller, A.L.; Ho-Fung, V.; Jaramillo, D. MRI of congenital and developmental abnormalities of the knee. Clin. Radiol. 2012, 67, 1198–1206. [Google Scholar] [CrossRef] [PubMed]
- Thompson, P.; Metcalfe, A.J. Current concepts in the surgical management of patellar instability. Knee 2019, 26, 1171–1181. [Google Scholar] [CrossRef]
- Bowd, J.; Van Rossom, S.; Williams, D.; Elson, D.; Wilson, C.; Whatling, G.; Holt, C.; Jonkers, I. Using musculoskeletal modelling to estimate knee joint loading pre and post high tibial osteotomy. Clin. Biomech. 2023, 101, 105855. [Google Scholar] [CrossRef]
- Zibis, A.H.; Vassalou, E.E.; Raoulis, V.A.; Lampridis, V.; Klontzas, M.E.; Fyllos, A.; Stavlas, P.; Karantanas, A.H. Knee Capsule Anatomy: An MR Imaging and Cadaveric Study. Diagnostics 2021, 11, 1965. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Maffulli, N.; Vaishya, R. Patellofemoral instability: Current status and future perspectives. J. Orthop. 2023, 36, 49–50. [Google Scholar] [CrossRef]
- Sato, A.; Takagi, H.; Koya, T.; Espinoza Orias, A.A.; Kanzaki, K.; Inoue, N. Clinical three-dimensional anatomy of the femur considering navigation-aided surgery of total knee arthroplasty in Japanese patients. Knee 2023, 41, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Patterson, B.E.; Girdwood, M.A.; West, T.J.; Bruder, A.M.; Oiestad, B.E.; Juhl, C.; Culvenor, A.G. Muscle strength and osteoarthritis of the knee: A systematic review and meta-analysis of longitudinal studies. Skeletal. Radiol. 2022. [Google Scholar] [CrossRef] [PubMed]
- Loudon, J.K. Biomechanics and Pathomechanics of the Patellofemoral Joint. Int. J. Sport. Phys. Ther. 2016, 11, 820–830. [Google Scholar]
- Lack, S.; Anthony, L.; Noake, J.; Brennan, K.; Zhang, B.; Morrissey, D. Medial and Lateral Patellofemoral Joint Retinaculum Thickness in People with Patellofemoral Pain: A Case-Control Study. J. Ultrasound Med. 2019, 38, 1483–1490. [Google Scholar] [CrossRef] [PubMed]
- Teichtahl, A.J.; Wluka, A.E.; Cicuttini, F.M. Frontal plane knee alignment is associated with a longitudinal reduction in patella cartilage volume in people with knee osteoarthritis. Osteoarthr. Cartil. 2008, 16, 851–854. [Google Scholar] [CrossRef] [PubMed]
- Seyyed Hossein, H.; Sara, A.; Hasan, D.; Navid, K. The effect of three types of exercises programs on the patella location in athletes with patellofemoral pain. Knee 2023, 41, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Cascio, F.; Cacciola, A.; Portaro, S.; Basile, G.A.; Rizzo, G.; Felippu, A.W.D.; Felippu, A.W.D.; Bruschetta, A.; Anfuso, C.; Cascio, F.; et al. In Vivo Computed Tomography Direct Volume Rendering of the Anterior Ethmoidal Artery: A Descriptive Anatomical Study. Int. Arch. Otorhinolaryngol. 2020, 24, e38–e46. [Google Scholar] [CrossRef] [PubMed]
- Schache, A.G.; Sritharan, P.; Culvenor, A.G.; Patterson, B.E.; Perraton, L.G.; Bryant, A.L.; Guermazi, A.; Morris, H.G.; Whitehead, T.S.; Crossley, K.M. Patellofemoral joint loading and early osteoarthritis after ACL reconstruction. J. Orthop. Res. 2023. [Google Scholar] [CrossRef] [PubMed]
- Krebs, C.; Tranovich, M.; Andrews, K.; Ebraheim, N. The medial patellofemoral ligament: Review of the literature. J. Orthop. 2018, 15, 596–599. [Google Scholar] [CrossRef]
- Tisano, A.; Alito, A.; Milardi, D.; Fazio, R.; Virelli, L.; Zanella, C.; Ruggeri, C.; Filardi, V.; Bruschetta, D. Statistical investigation about spinal clinical asymmetry in a school population. J. Orthop. 2020, 22, 336–340. [Google Scholar] [CrossRef] [PubMed]
- Simonaityte, R.; Rutkauskas, S.; Cekanauskas, E.; Labanauskas, L.; Barauskas, V. First-Time Acute Lateral Patellar Dislocation in Children and Adolescents: What about Unaffected Knee Patellofemoral Joint Anatomic Abnormalities? Medicina 2021, 57, 206. [Google Scholar] [CrossRef]
- Sinikumpu, J.; Nicolaou, N. Current concepts in the treatment of first-time patella dislocation in children and adolescents. J. Child. Orthop. 2023, 17, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Palco, M.; Rizzo, P.; Basile, G.C.; Alito, A.; Bruschetta, D.; Accorinti, M.; Restuccia, R.; Leonetti, D. Short- and Midterm Comparison of Platelet-Rich Plasma with Hyaluronic Acid versus Leucocyte and Platelet-Rich Plasma on Pain and Function to Treat Hip Osteoarthritis. A Retrospective Study. Gels 2021, 7, 222. [Google Scholar] [CrossRef]
- Trisolino, G.; Depaoli, A.; Gallone, G.; Ramella, M.; Olivotto, E.; Zarantonello, P.; Stallone, S.; Persiani, V.; Casadei, G.; Rocca, G. A 20-Year Retrospective Study of Children and Adolescents Treated by the Three-in-One Procedure for Patellar Realignment. J. Clin. Med. 2023, 12, 702. [Google Scholar] [CrossRef]
- Palco, M.; Rizzo, P.; Sanzarello, I.; Nanni, M.; Leonetti, D. Congenital and Bilateral Dislocation of the Knee: Case Report and Review of Literature. Orthop. Rev. 2022, 14, 33926. [Google Scholar] [CrossRef] [PubMed]
- Schubert, I.; Morris, P.; Dickschas, J.; Strohm, P.C. The Impact of Anatomical Predisposition and Mechanism of Trauma on Dislocation of the Patella: A Retrospective Analysis of 104 Cases. J. Pers. Med. 2022, 13, 84. [Google Scholar] [CrossRef]
- Chen, J.; Li, Q.; Liu, S.; Fan, L.; Yin, B.; Yang, X.; Wang, L.; Xu, Z.; Zhang, J.; Quan, Z.; et al. Prediction of Subsequent Contralateral Patellar Dislocation after First-Time Dislocation Based on Patellofemoral Morphologies. J. Clin. Med. 2022, 12, 180. [Google Scholar] [CrossRef] [PubMed]
- Kuwabara, A.; Cinque, M.; Ray, T.; Sherman, S.L. Treatment Options for Patellofemoral Arthritis. Curr. Rev. Musculoskelet. Med. 2022, 15, 90–106. [Google Scholar] [CrossRef] [PubMed]
- Jain, N.P.; Khan, N.; Fithian, D.C. A treatment algorithm for primary patellar dislocations. Sport. Health 2011, 3, 170–174. [Google Scholar] [CrossRef]
- Atkin, D.M.; Fithian, D.C.; Marangi, K.S.; Stone, M.L.; Dobson, B.E.; Mendelsohn, C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am. J. Sport. Med. 2000, 28, 472–479. [Google Scholar] [CrossRef]
- Pratelli, E.; Alito, A.; Zanella, C.; Busi, L.; Mangone, G.; Scarselli, M.; Pasquetti, P. Lower limbs heterometry correction in patients with osteoporosis and increased risk of falls. Clin. Cases Min. Bone Metab. 2017, 14, 294–297. [Google Scholar] [CrossRef] [PubMed]
- Biyani, R.; Elias, J.J.; Saranathan, A.; Feng, H.; Guseila, L.M.; Morscher, M.A.; Jones, K.C. Anatomical factors influencing patellar tracking in the unstable patellofemoral joint. Knee Surg. Sport. Traumatol. Arthrosc. 2014, 22, 2334–2341. [Google Scholar] [CrossRef] [PubMed]
- Sakai, N.; Luo, Z.P.; Rand, J.A.; An, K.N. The influence of weakness in the vastus medialis oblique muscle on the patellofemoral joint: An in vitro biomechanical study. Clin. Biomech. 2000, 15, 335–339. [Google Scholar] [CrossRef] [PubMed]
- Stephen, J.; Alva, A.; Lumpaopong, P.; Williams, A.; Amis, A.A. A cadaveric model to evaluate the effect of unloading the medial quadriceps on patellar tracking and patellofemoral joint pressure and stability. J. Exp. Orthop. 2018, 5, 34. [Google Scholar] [CrossRef] [PubMed]
- Siljander, B.; Tompkins, M.; Martinez-Cano, J.P. A Review of the Lateral Patellofemoral Joint: Anatomy, Biomechanics, and Surgical Procedures. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2022, 6, e21.00255. [Google Scholar] [CrossRef]
- Yoo, Y.H.; Lee, S.J.; Jeong, S.W. Effects of quadriceps angle on patellofemoral contact pressure. J. Vet. Sci. 2020, 21, e69. [Google Scholar] [CrossRef]
- Choi, W.; Lee, S.J.; Oh, J.; Baek, H.; Yang, J.; Shin, J.; Jung, B.; Lee, S. Magnetic Resonance Imaging of Patellofemoral Morphometry Reveals Age and Gender Variations in the Knees of Children and Adolescents. Diagnostics 2021, 11, 1985. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, S.; Varacallo, M.; Thomas, J.D.; Carroll, J.J.; Kahwaji, C.I. Patellar Instability; StatPearls: Treasure Island, FL, USA, 2022. [Google Scholar]
- Huddleston, H.P.; Shewman, E.F.; Knapik, D.; Yanke, A.B. Lateral Patellofemoral Ligament Reconstruction: A Biomechanical Comparison of 2 Techniques. Am. J. Sport. Med. 2023, 51, 446–452. [Google Scholar] [CrossRef] [PubMed]
- Zarins, B. Tibial External Rotation Test for Patellar Instability. J. Bone Jt. Surg. Am. 2022, 104, e16. [Google Scholar] [CrossRef]
- White, A.E.; Otlans, P.T.; Horan, D.P.; Calem, D.B.; Emper, W.D.; Freedman, K.B.; Tjoumakaris, F.P. Radiologic Measurements in the Assessment of Patellar Instability: A Systematic Review and Meta-analysis. Orthop. J. Sport. Med. 2021, 9, 2325967121993179. [Google Scholar] [CrossRef]
- Alito, A.; Filardi, V.; Fama, F.; Bruschetta, D.; Ruggeri, C.; Basile, G.; Stancanelli, L.; D’Amico, C.; Bianconi, S.; Tisano, A. Traumatic and non-traumatic spinal cord injury: Demographic characteristics, neurological and functional outcomes. A 7-year single centre experience. J. Orthop. 2021, 28, 62–66. [Google Scholar] [CrossRef]
- Jibri, Z.; Jamieson, P.; Rakhra, K.S.; Sampaio, M.L.; Dervin, G. Patellar maltracking: An update on the diagnosis and treatment strategies. Insights Imaging 2019, 10, 65. [Google Scholar] [CrossRef]
- Sanchis-Alfonso, V.; Teitge, R.A. Torsional Abnormality: The Forgotten Issue in the Diagnosis and Treatment of the Anterior Knee Pain Patient. J. Clin. Med. 2022, 11, 3530. [Google Scholar] [CrossRef]
- Colvin, A.C.; West, R.V. Patellar instability. J. Bone Jt. Surg. 2008, 90, 2751–2762. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.F.; Lin, J.J.; Jan, M.H.; Wei, T.C.; Shih, H.Y.; Cheng, C.K. Role of the vastus medialis obliquus in repositioning the patella: A dynamic computed tomography study. Am. J. Sport. Med. 2008, 36, 741–746. [Google Scholar] [CrossRef]
- Siegel, M.; Maier, P.; Taghizadeh, E.; Fuchs, A.; Yilmaz, T.; Meine, H.; Schmal, H.; Lange, T.; Izadpanah, K. Change in Descriptive Kinematic Parameters of Patients with Patellofemoral Instability When Compared to Individuals with Healthy Knees—A 3D MRI In Vivo Analysis. J. Clin. Med. 2023, 12, 1917. [Google Scholar] [CrossRef]
- Mascal, C.L.; Landel, R.; Powers, C. Management of patellofemoral pain targeting hip, pelvis, and trunk muscle function: 2 case reports. J. Orthop. Sports Phys. Ther. 2003, 33, 647–660. [Google Scholar] [CrossRef]
- Ng, G.Y.; Cheng, J.M. The effects of patellar taping on pain and neuromuscular performance in subjects with patellofemoral pain syndrome. Clin. Rehabil. 2002, 16, 821–827. [Google Scholar] [CrossRef]
- Cancienne, J.M.; Christian, D.R.; Redondo, M.L.; Huddleston, H.P.; Shewman, E.F.; Farr, J.; Cole, B.J.; Yanke, A.B. The Biomechanical Effects of Limited Lateral Retinacular and Capsular Release on Lateral Patellar Translation at Various Flexion Angles in Cadaveric Specimens. Arthrosc. Sport. Med. Rehabil. 2019, 1, e137–e144. [Google Scholar] [CrossRef]
- Filardi, V.; Milardi, D. Experimental strain analysis on the entire bony leg compared with FE analysis. J. Orthop. 2017, 14, 115–122. [Google Scholar] [CrossRef]
- Filardi, V. FE analysis of stress and displacements occurring in the bony chain of leg. J. Orthop. 2014, 11, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Filardi, V. Stress shielding in the bony chain of leg in presence of varus or valgus knee. J. Orthop. 2015, 12, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Filardi, V.; Risitano, G.; Vaishya, R. Numerical investigation of patellar instability during knee flexion due to an unbalanced medial retinaculum loading effect. J. Orthop. 2023, 36, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Filardi, V. Hallux valgus (HV): A multi-approach investigation analysis. J. Orthop. 2020, 18, 166–170. [Google Scholar] [CrossRef] [PubMed]
- Filardi, V. Flatfoot and normal foot a comparative analysis of the stress shielding. J. Orthop. 2018, 15, 820–825. [Google Scholar] [CrossRef]
- Petri, M.; Ettinger, M.; Stuebig, T.; Brand, S.; Krettek, C.; Jagodzinski, M.; Omar, M. Current Concepts for Patellar Dislocation. Arch. Trauma Res. 2015, 4, e29301. [Google Scholar] [CrossRef] [PubMed]
- Jamari, J.; Ammarullah, M.I.; Santoso, G.; Sugiharto, S.; Supriyono, T.; Permana, M.S.; Winarni, T.I.; van der Heide, E. Adopted walking condition for computational simulation approach on bearing of hip joint prosthesis: Review over the past 30 years. Heliyon 2022, 8, e12050. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.M.; Duncan, N.A. Correlation of patellar tracking pattern with trochlear and retropatellar surface topographies. J. Biomech. Eng. 2000, 122, 652–660. [Google Scholar] [CrossRef]
- Goh, J.C.; Lee, P.Y.; Bose, K. A cadaver study of the function of the oblique part of vastus medialis. J. Bone Jt. Surg. Br. 1995, 77, 225–231. [Google Scholar] [CrossRef]
- Ruffilli, A.; Traina, F.; Pilla, F.; Fenga, D.; Faldini, C. Marchetti Vicenzi elastic retrograde nail in the treatment of humeral shaft fractures: Review of the current literature. Musculoskelet. Surg. 2015, 99, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Ammarullah, M.I.; Hartono, R.; Supriyono, T.; Santoso, G.; Sugiharto, S.; Permana, M.S. Polycrystalline Diamond as a Potential Material for the Hard-on-Hard Bearing of Total Hip Prosthesis: Von Mises Stress Analysis. Biomedicines 2023, 11, 951. [Google Scholar] [CrossRef]
- Farahmand, F.; Naghi Tahmasbi, M.; Amis, A. The contribution of the medial retinaculum and quadriceps muscles to patellar lateral stability—An in-vitro study. Knee 2004, 11, 89–94. [Google Scholar] [CrossRef]
- Carson, W.G., Jr.; James, S.L.; Larson, R.L.; Singer, K.M.; Winternitz, W.W. Patellofemoral disorders: Physical and radiographic evaluation. Part II: Radiographic examination. Clin. Orthop. Relat. Res. 1984, 185, 178–186. [Google Scholar] [CrossRef]
- Zimmermann, F.; Privalov, M.; Franke, J.; Grutzner, P.A.; Balcarek, P.; Vetter, S.Y. Reconstruction of the medial patellofemoral ligament with nonresorbable suture tape normalizes patellar maltracking independent of patella-side fixation technique. Knee Surg. Sport. Traumatol. Arthrosc. 2022. [Google Scholar] [CrossRef]
- Koh, J.L.; Stewart, C. Patellar instability. Orthop. Clin. N. Am. 2015, 46, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Abelleyra Lastoria, D.A.; Benny, C.K.; Hing, C.B. The effect of quadriceps anatomical factors on patellar stability: A systematic review. Knee 2023, 41, 29–37. [Google Scholar] [CrossRef]
- Maine, S.T.; O’Gorman, P.; Barzan, M.; Stockton, C.A.; Lloyd, D.; Carty, C.P. Rotational Malalignment of the Knee Extensor Mechanism: Defining Rotation of the Quadriceps and Its Role in the Spectrum of Patellofemoral Joint Instability. JBJS Open Access 2019, 4, e0020. [Google Scholar] [CrossRef]
- Saad, A.; Iqbal, A.; Ehiogu, U.; James, S.; Botchu, R. Do the quadriceps and hamstring muscles have an effect on patella stability in trochlear dysplasia? Pol. J. Radiol. 2021, 86, e232–e238. [Google Scholar] [CrossRef]
- Woods, G.W.; Elkousy, H.A.; O’Connor, D.P. Arthroscopic release of the vastus lateralis tendon for recurrent patellar dislocation. Am. J. Sport. Med. 2006, 34, 824–831. [Google Scholar] [CrossRef]
- Miller, J.R.; Adamson, G.J.; Pink, M.M.; Fraipont, M.J.; Durand, P., Jr. Arthroscopically assisted medial reefing without routine lateral release for patellar instability. Am. J. Sport. Med. 2007, 35, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Ricchetti, E.T.; Mehta, S.; Sennett, B.J.; Huffman, G.R. Comparison of lateral release versus lateral release with medial soft-tissue realignment for the treatment of recurrent patellar instability: A systematic review. Arthroscopy 2007, 23, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Drez, D., Jr.; Edwards, T.B.; Williams, C.S. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy 2001, 17, 298–306. [Google Scholar] [CrossRef]
- Filardi, V.; Simona, P.; Cacciola, G.; Bertino, S.; Soliera, L.; Barbanera, A.; Pisani, A.; Milardi, D.; Alessia, B. Finite element analysis of sagittal balance in different morphotype: Forces and resulting strain in pelvis and spine. J. Orthop. 2017, 14, 268–275. [Google Scholar] [CrossRef]
- Filardi, V. The healing stages of an intramedullary implanted tibia: A stress strain comparative analysis of the calcification process. J. Orthop. 2015, 12, S51–S61. [Google Scholar] [CrossRef]
- Sanchis-Alfonso, V.; Ginovart, G.; Alastruey-Lopez, D.; Montesinos-Berry, E.; Monllau, J.C.; Alberich-Bayarri, A.; Perez, M.A. Evaluation of Patellar Contact Pressure Changes after Static versus Dynamic Medial Patellofemoral Ligament Reconstructions Using a Finite Element Model. J. Clin. Med. 2019, 8, 2093. [Google Scholar] [CrossRef] [PubMed]
- Sayed-Noor, A.S.; Mukka, S.; Mohaddes, M.; Karrholm, J.; Rolfson, O. Body mass index is associated with risk of reoperation and revision after primary total hip arthroplasty: A study of the Swedish Hip Arthroplasty Register including 83,146 patients. Acta Orthop. 2019, 90, 220–225. [Google Scholar] [CrossRef]
- Ammarullah, M.I.; Santoso, G.; Sugiharto, S.; Supriyono, T.; Tauviqirrahman, M.; Winarni, T.I.; Jamari, J. Tresca stress study of CoCrMo-on-CoCrMo bearings based on body mass index using 2D computational model. J. Tribol. 2022, 33, 31–38. [Google Scholar]
- Kaiser, D.; Trummler, L.; Gotschi, T.; Waibel, F.W.A.; Snedeker, J.G.; Fucentese, S.F. The quantitative influence of current treatment options on patellofemoral stability in patients with trochlear dysplasia and symptomatic patellofemoral instability—A finite element simulation. Clin. Biomech. 2021, 84, 105340. [Google Scholar] [CrossRef] [PubMed]
- Sanchis-Alfonso, V.; Alastruey-Lopez, D.; Ginovart, G.; Montesinos-Berry, E.; Garcia-Castro, F.; Ramirez-Fuentes, C.; Monllau, J.C.; Alberich-Bayarri, A.; Perez, M.A. Parametric finite element model of medial patellofemoral ligament reconstruction model development and clinical validation. J. Exp. Orthop. 2019, 6, 32. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, K.; Mutsuzaki, H.; Fukaya, T.; Aoyama, T.; Nakajima, S.; Sekine, N.; Mori, K. Simulating Knee-Stress Distribution Using a Computed Tomography-Based Finite Element Model: A Case Study. J. Funct. Morphol. Kinesiol. 2023, 8, 15. [Google Scholar] [CrossRef]
- Watson, N.A.; Duchman, K.R.; Grosland, N.M.; Bollier, M.J. Finite Element Analysis of Patella Alta: A Patellofemoral Instability Model. Iowa Orthop. J. 2017, 37, 101–108. [Google Scholar] [PubMed]
- Nomura, E.; Horiuchi, Y.; Kihara, M. Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee 2000, 7, 121–127. [Google Scholar] [CrossRef]
- Abdelrahman, T.; Moatshe, G.; Arendt, E.; Feller, J.; Getgood, A. Combined Medial Patellofemoral Ligament and Medial Patellotibial Ligament Reconstruction for Recurrent Lateral Patellar Dislocation in Flexion. Arthrosc. Tech. 2021, 10, e385–e395. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).