Machine Learning-Based Fatigue Level Prediction for Exoskeleton-Assisted Trunk Flexion Tasks Using Wearable Sensors
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
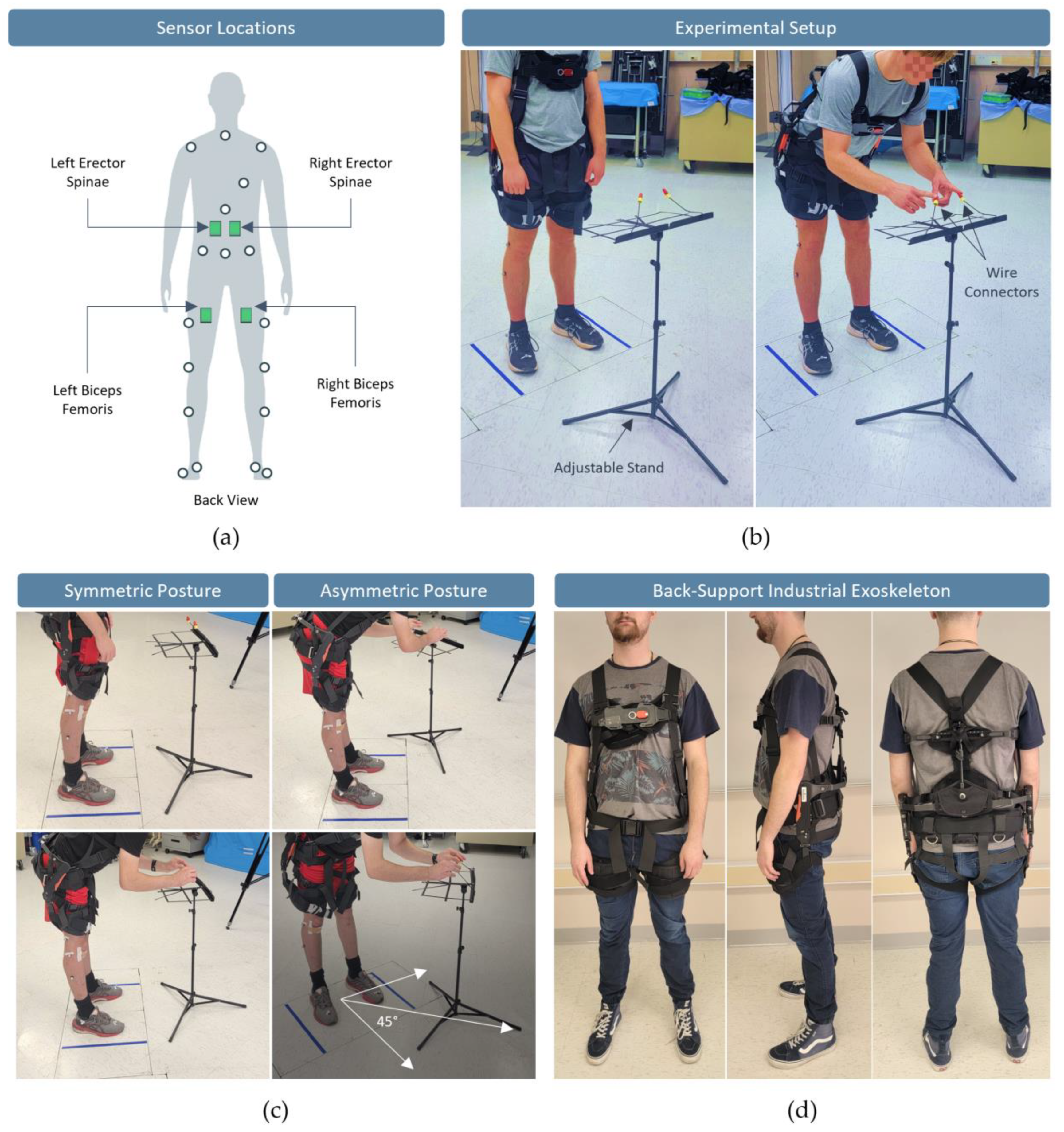
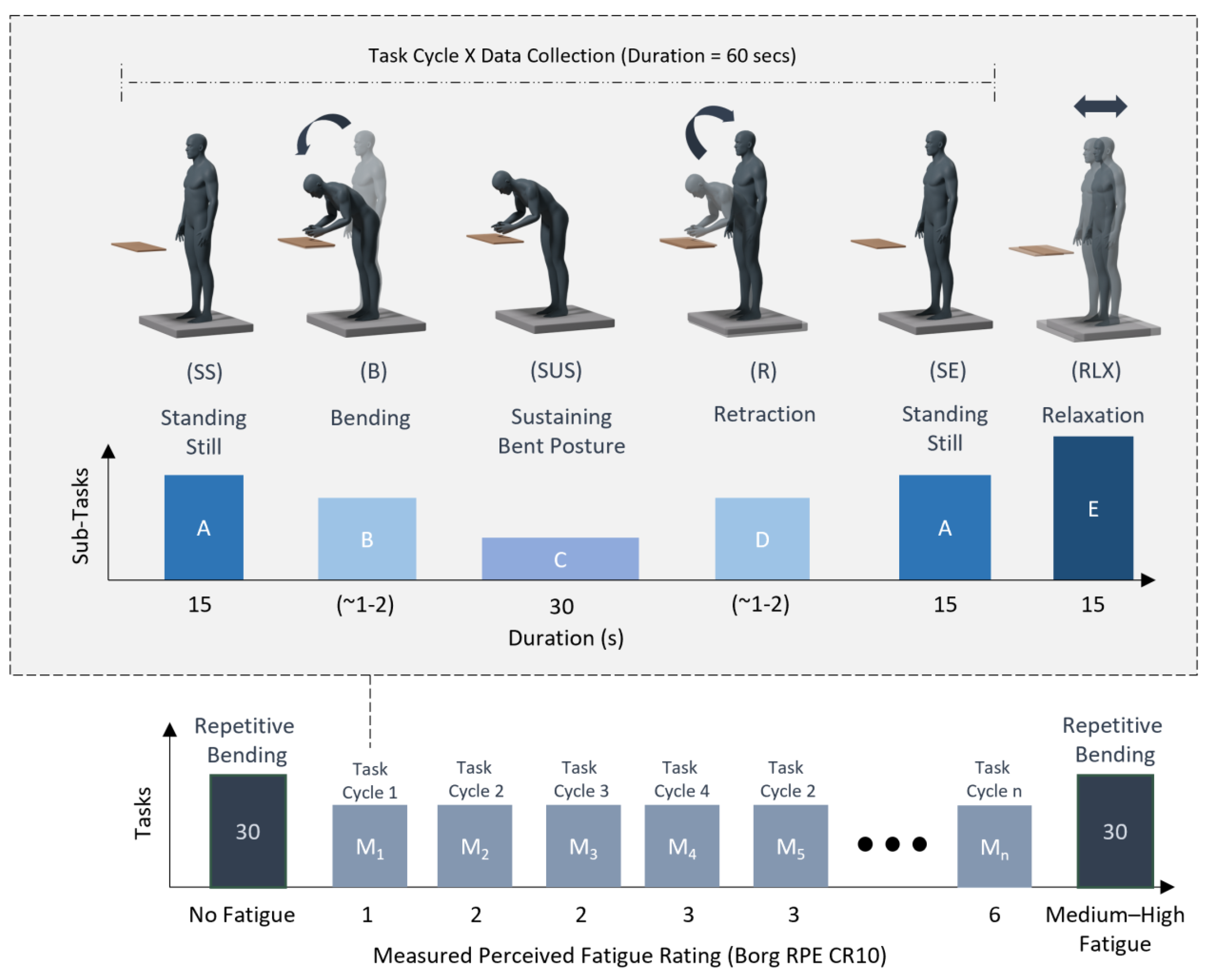
2.2. Experimental Tasks, Apparatus, and Equipment
2.3. Experimental Protocol
2.4. Feature Engineering and Model Development
2.5. Performance Evaluation and Validation
- True Positive (TP): The number of instances correctly predicted as positive.
- True Negative (TN): The number of instances correctly predicted as negative.
- False Positive (FP): The number of instances incorrectly predicted as positive.
- False Negative (FN): The number of instances incorrectly predicted as negative.
2.6. Determining Optimal Model Parameters
3. Results
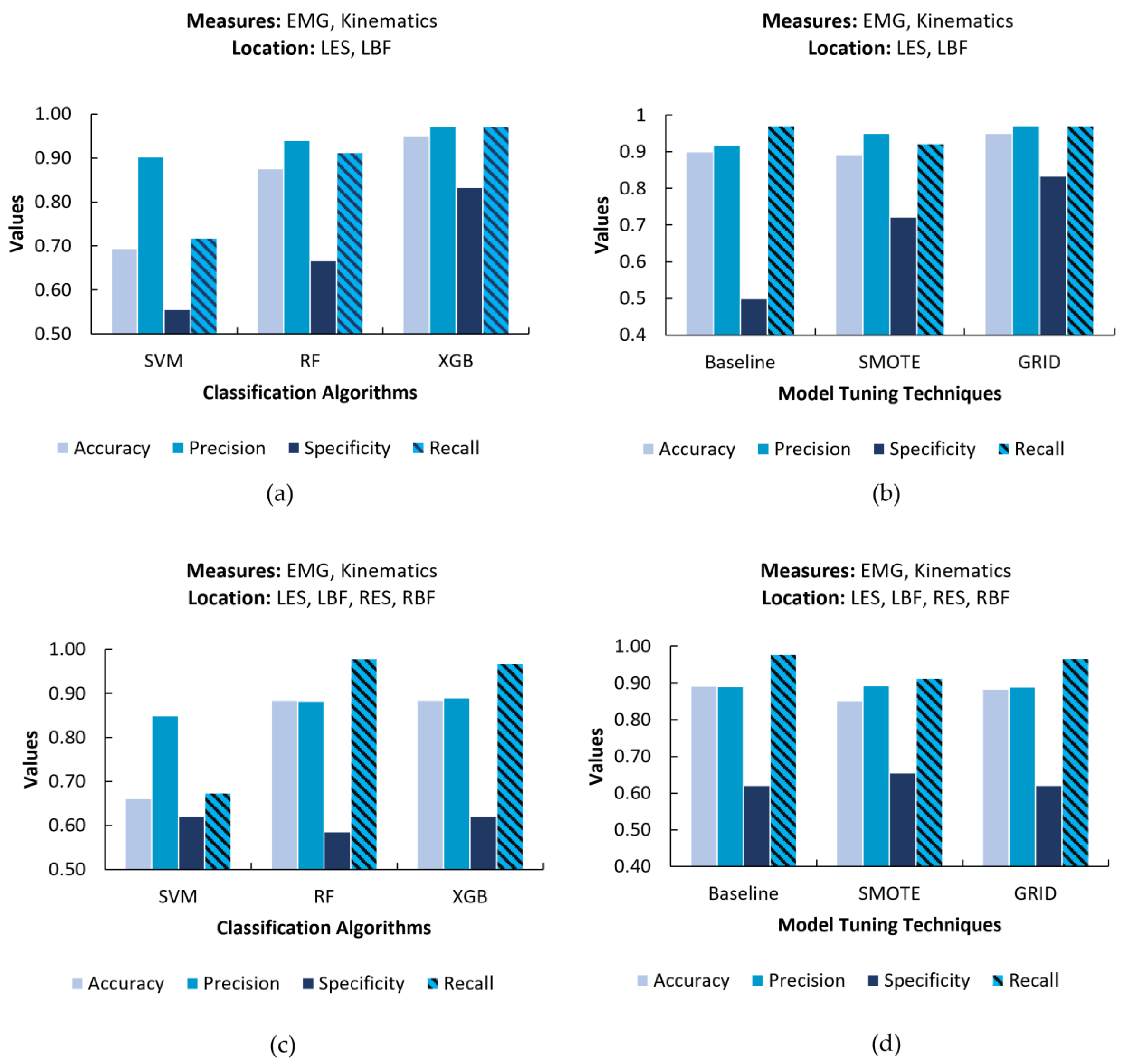
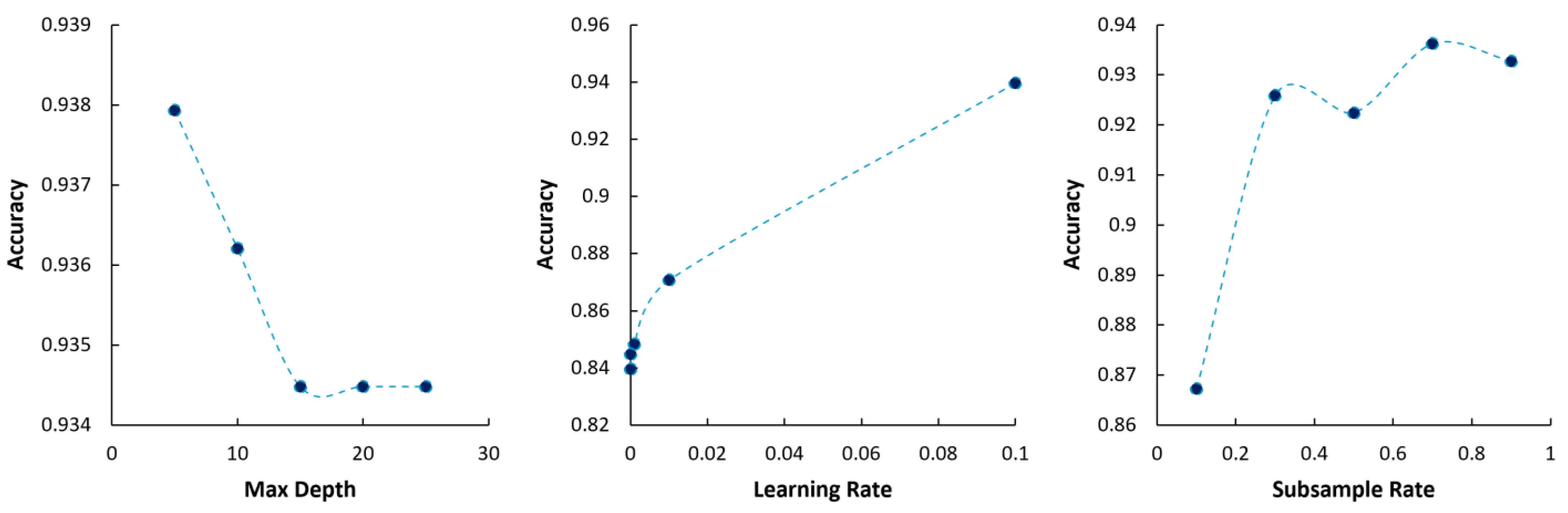
3.1. Effects of Performance with Variation in Model Factors and Parameters
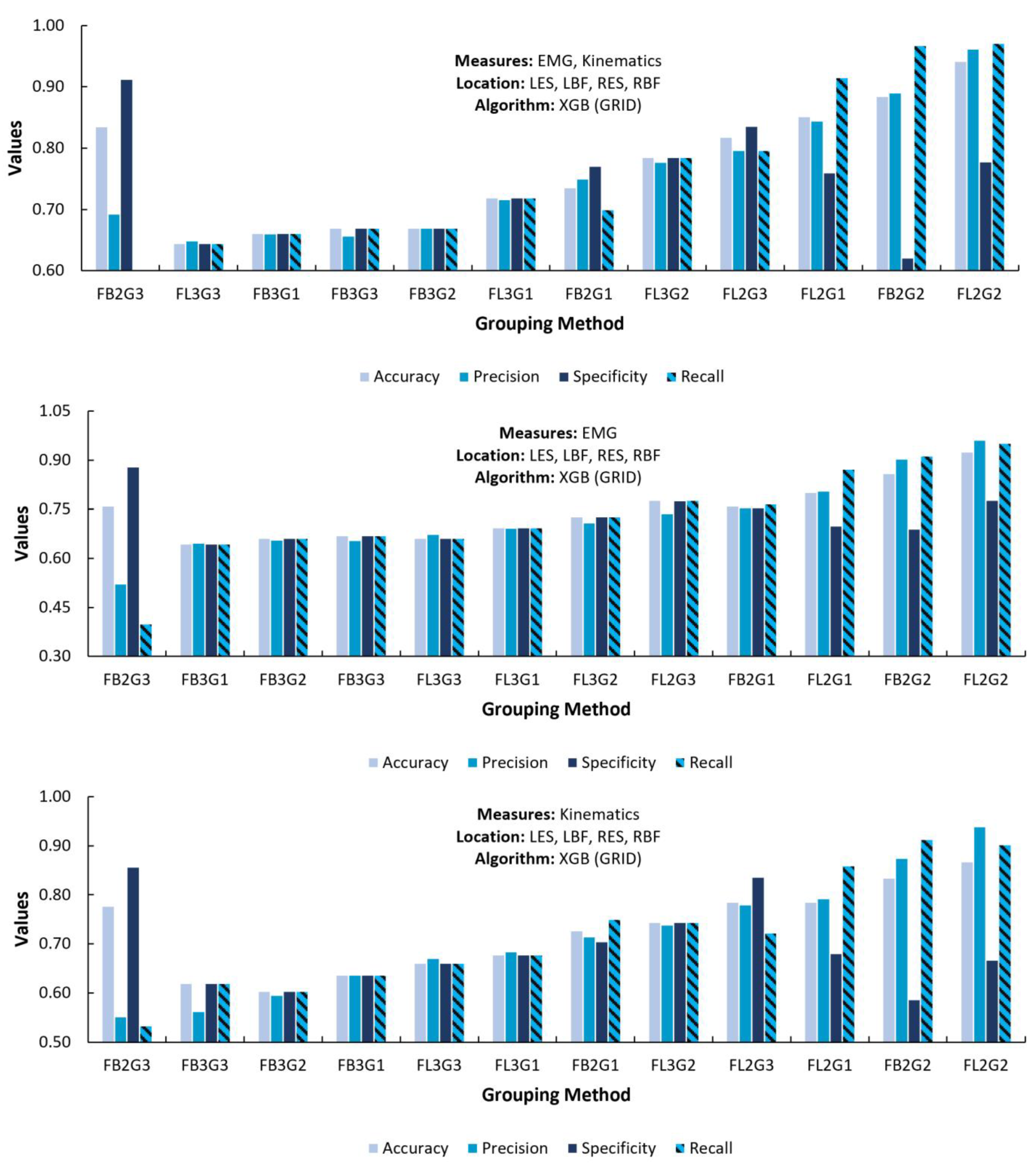
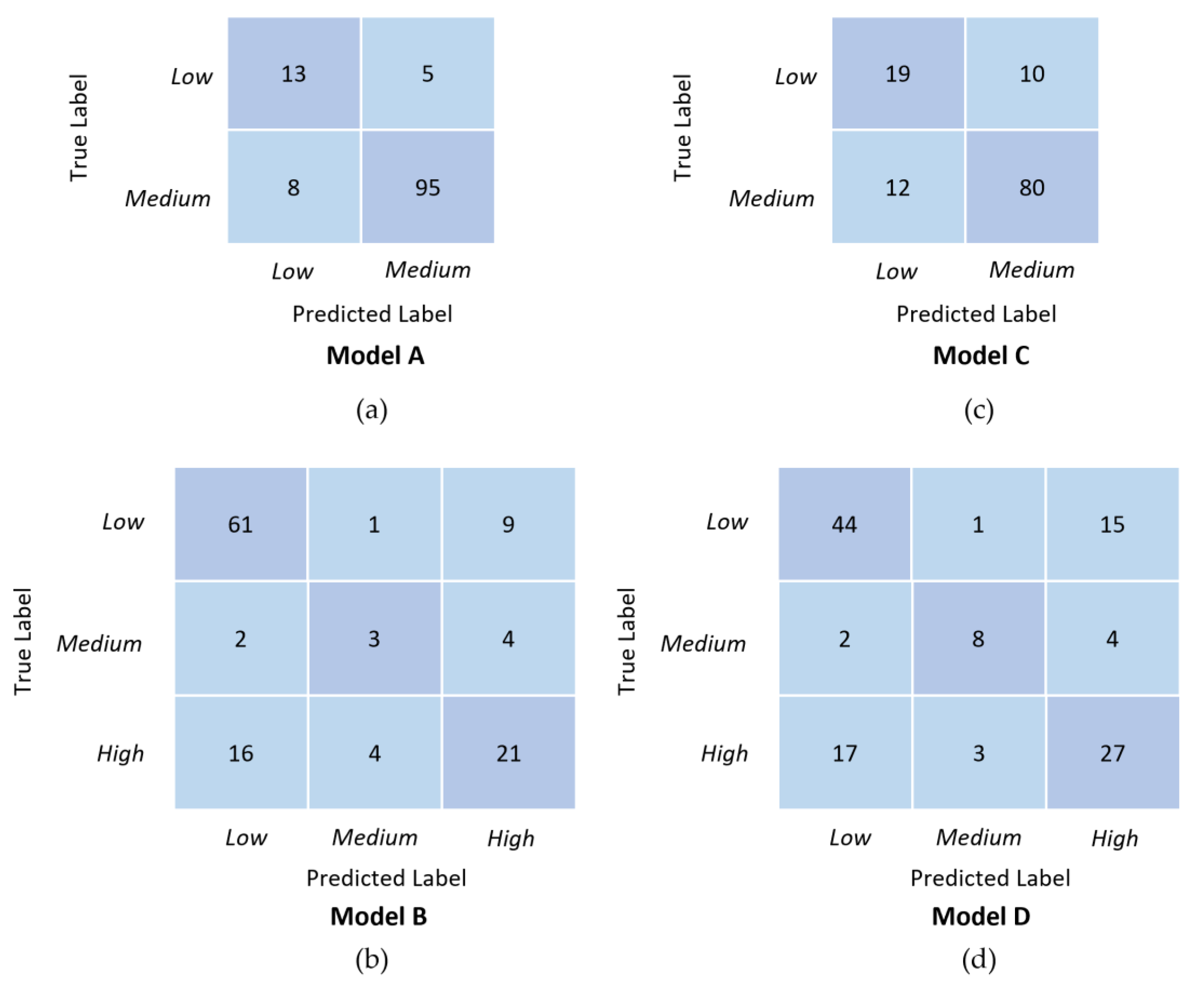
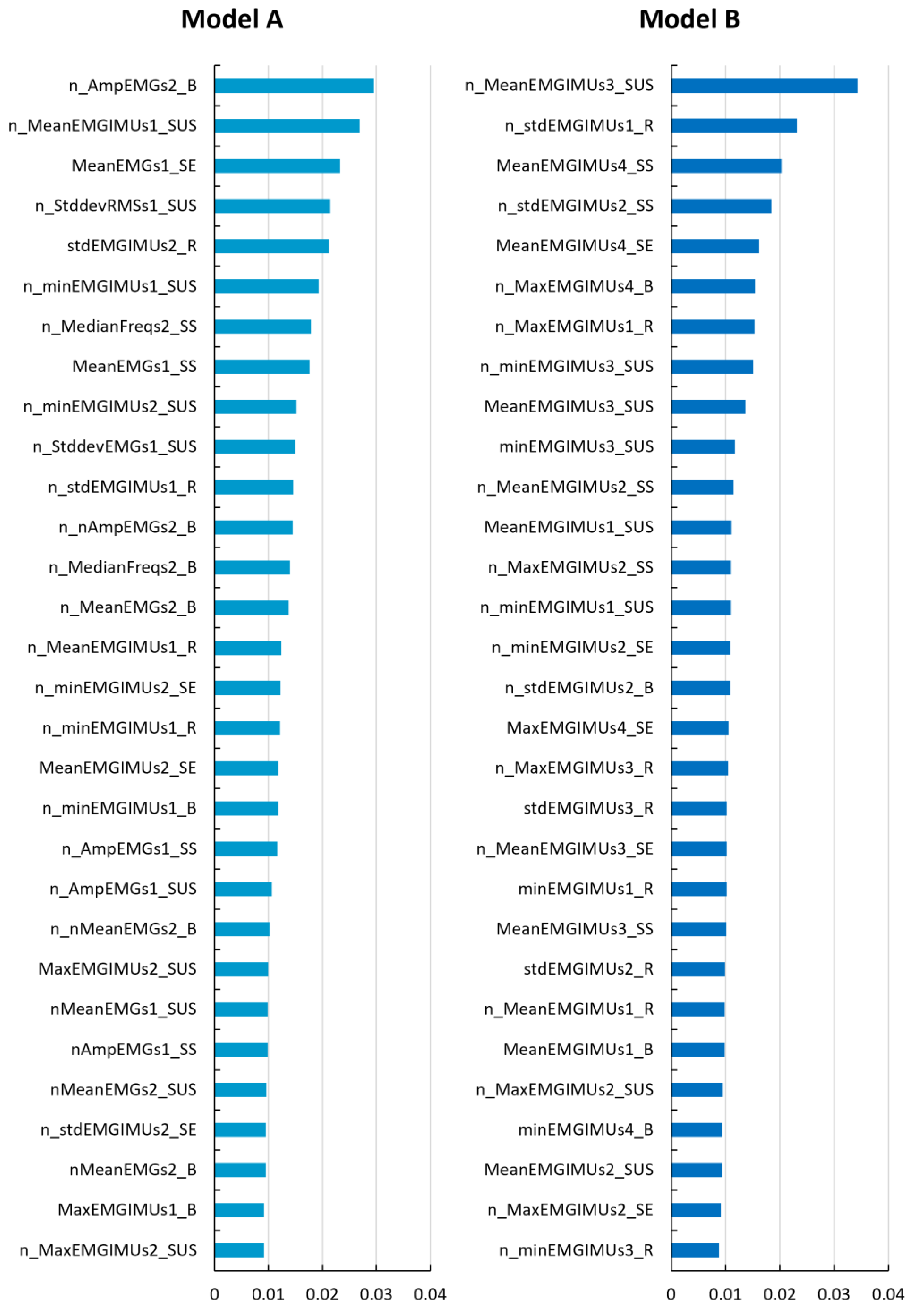
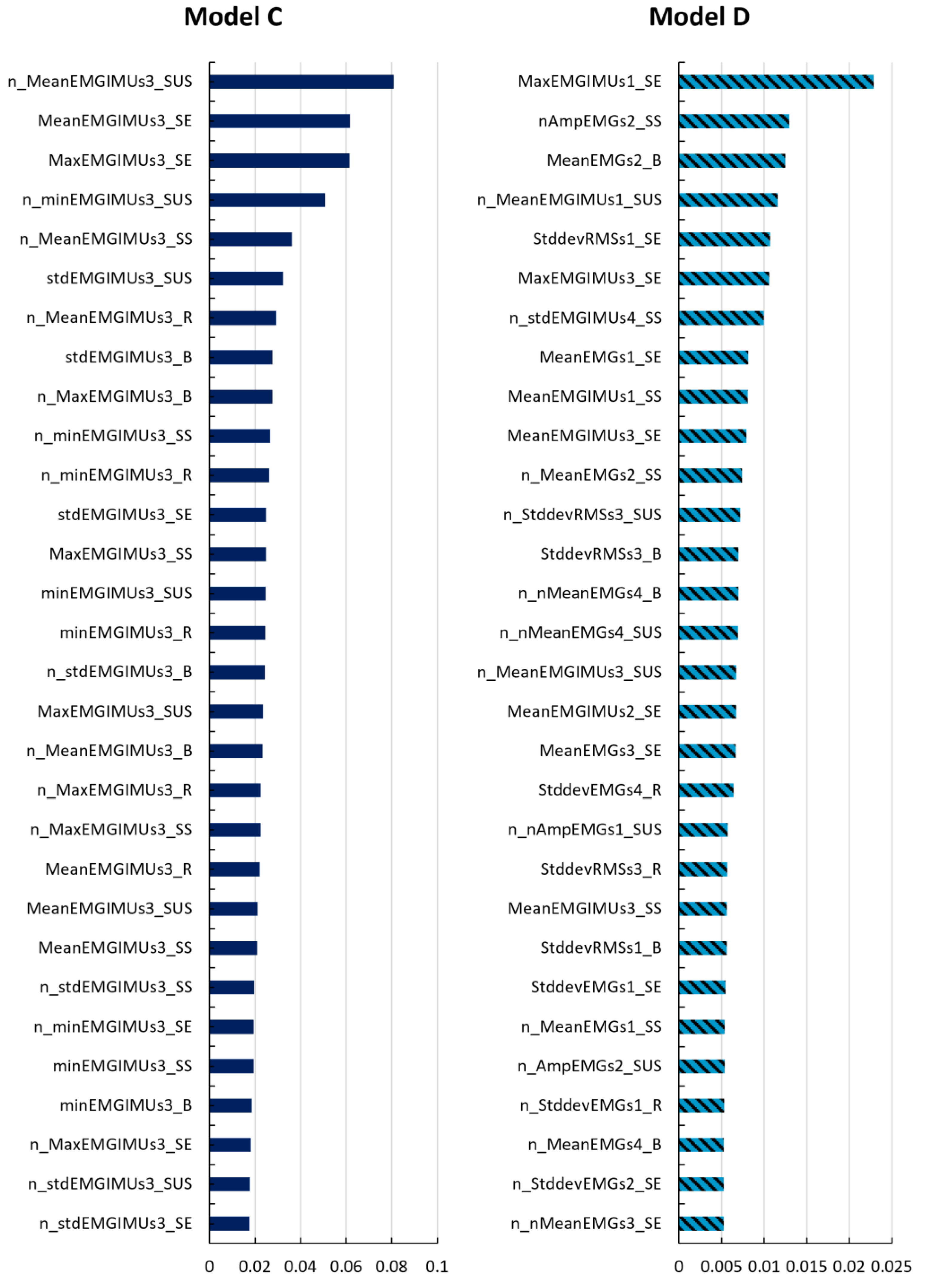
3.2. Model Selection and Feature Importances
4. Discussion
4.1. Performance Variation across Fatigue Level Grouping Methods
4.2. Performance Variation between Measures for Selected Models
4.3. Performance Variation between Levels of Fatigue Grouping Methods
5. Study Limitations and Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sadeghniiat-Haghighi, K.; Yazdi, Z. Fatigue Management in the Workplace. Ind. Psychiatry J. 2015, 24, 12. [Google Scholar] [CrossRef] [PubMed]
- Butkeviçiüte, E.; Erinš, M.; Bikulçiene, L. An Adaptable Human Fatigue Evaluation System. Procedia Comput. Sci. 2021, 192, 1274–1284. [Google Scholar] [CrossRef]
- Ricci, J.A.; Chee, E.; Lorandeau, A.L.; Berger, J. Fatigue in the U.S. Workforce: Prevalence and Implications for Lost Productive Work Time. J. Occup. Environ. Med. 2007, 49, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Williams, N. The Borg Rating of Perceived Exertion (RPE) Scale. Occup. Med. 2017, 67, 404–405. [Google Scholar] [CrossRef]
- Garcia, G.; Arauz, P.G.; Alvarez, I.; Encalada, N.; Vega, S.; Martin, B.J. Impact of a Passive Upper-Body Exoskeleton on Muscle Activity, Heart Rate and Discomfort during a Carrying Task. PLoS ONE 2023, 18, e0287588. [Google Scholar] [CrossRef]
- Duan, S.; Wang, C.; Li, Y.; Zhang, L.; Yuan, Y.; Wu, X. A Quantifiable Muscle Fatigue Method Based on SEMG during Dynamic Contractions for Lower Limb Exoskeleton. In Proceedings of the 2020 IEEE International Conference on Real-time Computing and Robotics (RCAR), Asahikawa, Japan, 28–29 September 2020; pp. 20–25. [Google Scholar]
- Zamunér, A.R.; Moreno, M.A.; Camargo, T.M.; Graetz, J.P.; Rebelo, A.C.S.; Tamburús, N.Y.; da Silva, E. Assessment of Subjective Perceived Exertion at the Anaerobic Threshold with the Borg CR-10 Scale. J. Sports Sci. Med. 2011, 10, 130–136. [Google Scholar] [PubMed]
- Aryal, A.; Ghahramani, A.; Becerik-Gerber, B. Monitoring Fatigue in Construction Workers Using Physiological Measurements. Autom. Constr. 2017, 82, 154–165. [Google Scholar] [CrossRef]
- Chai, G.; Wang, Y.; Wu, J.; Yang, H.; Tang, Z.; Zhang, L. Study on the Recognition of Exercise Intensity and Fatigue on Runners Based on Subjective and Objective Information. Healthcare 2019, 7, 150. [Google Scholar] [CrossRef]
- Völker, I.; Kirchner, C.; Bock, O.L. On the Relationship between Subjective and Objective Measures of Fatigue. Ergonomics 2016, 59, 1259–1263. [Google Scholar] [CrossRef]
- Aguirre, A.; Pinto, M.J.; Cifuentes, C.A.; Perdomo, O.; Díaz, C.A.R.; Múnera, M. Machine Learning Approach for Fatigue Estimation in Sit-to-Stand Exercise. Sensors 2021, 21, 5006. [Google Scholar] [CrossRef]
- Matijevich, E.S.; Volgyesi, P.; Zelik, K.E. A Promising Wearable Solution for the Practical and Accurate Monitoring of Low Back Loading in Manual Material Handling. Sensors 2021, 21, 340. [Google Scholar] [CrossRef]
- Agrawal, D.K.; Usaha, W.; Pojprapai, S.; Wattanapan, P. Fall Risk Prediction Using Wireless Sensor Insoles With Machine Learning. IEEE Access 2023, 11, 23119–23126. [Google Scholar] [CrossRef]
- Qiu, H.; Rehman, R.Z.U.; Yu, X.; Xiong, S. Application of Wearable Inertial Sensors and A New Test Battery for Distinguishing Retrospective Fallers from Non-Fallers among Community-Dwelling Older People. Sci. Rep. 2018, 8, 16349. [Google Scholar] [CrossRef] [PubMed]
- Ramos, G.; Vaz, J.R.; Mendonça, G.V.; Pezarat-Correia, P.; Rodrigues, J.; Alfaras, M.; Gamboa, H.; Zou, L. Fatigue Evaluation through Machine Learning and a Global Fatigue Descriptor. J. Healthc. Eng. 2020, 2020, 6484129. [Google Scholar] [CrossRef]
- Serpen, G.; Khan, R.H. Real-Time Detection of Human Falls in Progress: Machine Learning Approach. Procedia Comput. Sci. 2018, 140, 238–247. [Google Scholar] [CrossRef]
- Jiang, Y.; Duan, J.; Deng, S.; Qi, Y.; Wang, P.; Wang, Z.; Zhang, T. Sitting Posture Recognition by Body Pressure Distribution and Airbag Regulation Strategy Based on Seat Comfort Evaluation. J. Eng. 2019, 2019, 8910–8914. [Google Scholar]
- Scherpereel, K.L.; Bolus, N.B.; Jeong, H.K.; Inan, O.T.; Young, A.J. Estimating Knee Joint Load Using Acoustic Emissions During Ambulation. Ann. Biomed. Eng. 2021, 49, 1000–1011. [Google Scholar] [CrossRef] [PubMed]
- Abdollahi, M.; Rashedi, E.; Jahangiri, S.; Kuber, P.M.; Azadeh-Fard, N.; Dombovy, M. Fall Risk Assessment in Stroke Survivors: A Machine Learning Model Using Detailed Motion Data from Common Clinical Tests and Motor-Cognitive Dual-Tasking. Sensors 2024, 24, 812. [Google Scholar] [CrossRef]
- Le Minh, T.; Van Tran, L.; Dao, S.V.T. A Feature Selection Approach for Fall Detection Using Various Machine Learning Classifiers. IEEE Access 2021, 9, 115895–115908. [Google Scholar] [CrossRef]
- Liu, G.; Dobbins, C.; D’Souza, M.; Phuong, N. A Machine Learning Approach for Detecting Fatigue during Repetitive Physical Tasks. Pers. Ubiquitous Comput. 2023, 27, 2103–2120. [Google Scholar] [CrossRef]
- Antwi-Afari, M.F.; Anwer, S.; Umer, W.; Mi, H.Y.; Yu, Y.; Moon, S.; Hossain, M.U. Machine Learning-Based Identification and Classification of Physical Fatigue Levels: A Novel Method Based on a Wearable Insole Device. Int. J. Ind. Ergon. 2023, 93, 103404. [Google Scholar] [CrossRef]
- Pinto-Bernal, M.J.; Cifuentes, C.A.; Perdomo, O.; Rincón-Roncancio, M.; Múnera, M. A Data-Driven Approach to Physical Fatigue Management Using Wearable Sensors to Classify Four Diagnostic Fatigue States. Sensors 2021, 21, 6401. [Google Scholar] [CrossRef] [PubMed]
- Liew, B.X.W.; Pfisterer, F.; Rügamer, D.; Zhai, X. Strategies to Optimise Machine Learning Classification Performance When Using Biomechanical Features. J. Biomech. 2024, 165, 111998. [Google Scholar] [CrossRef] [PubMed]
- Baghdadi, A.; Megahed, F.M.; Esfahani, E.T.; Cavuoto, L.A. A Machine Learning Approach to Detect Changes in Gait Parameters Following a Fatiguing Occupational Task. Ergonomics 2018, 61, 1116–1129. [Google Scholar] [CrossRef] [PubMed]
- Karthick, P.A.; Ghosh, D.M.; Ramakrishnan, S. Surface Electromyography Based Muscle Fatigue Detection Using High-Resolution Time-Frequency Methods and Machine Learning Algorithms. Comput. Methods Programs Biomed. 2018, 154, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Onose, G.; Cârdei, V.; Craciunoiu, S.T.; Avramescu, V.; Opris, I.; Lebedev, M.A.; Constantinescu, M.V. Mechatronic Wearable Exoskeletons for Bionic Bipedal Standing and Walking: A New Synthetic Approach. Front. Neurosci. 2016, 10, 343. [Google Scholar] [CrossRef] [PubMed]
- De Bock, S.; Ghillebert, J.; Govaerts, R.; Tassignon, B.; Rodriguez-Guerrero, C.; Crea, S.; Veneman, J.; Geeroms, J.; Meeusen, R.; De Pauw, K. Benchmarking Occupational Exoskeletons: An Evidence Mapping Systematic Review. Appl. Ergon. 2022, 98, 103582. [Google Scholar] [CrossRef] [PubMed]
- de Looze, M.P.; Bosch, T.; Krause, F.; Stadler, K.S.; O’Sullivan, L.W. Exoskeletons for Industrial Application and Their Potential Effects on Physical Work Load. Ergonomics 2016, 59, 671–681. [Google Scholar] [CrossRef] [PubMed]
- Kuber, P.M.; Rashedi, E. Product Ergonomics in Industrial Exoskeletons: Potential Enhancements for Workforce Safety and Efficiency. TheoreTical Issues Ergon. Sci. 2020, 22, 729–752. [Google Scholar] [CrossRef]
- Crowell, H.P.; Park, J.-H.; Haynes, C.A.; Neugebauer, J.M.; Boynton, A.C. Design, Evaluation, and Research Challenges Relevant to Exoskeletons and Exosuits: A 26-Year Perspective From the U.S. Army Research Laboratory. IISE Trans. Occup. Ergon. Hum. Factors 2019, 7, 199–212. [Google Scholar] [CrossRef]
- Romanato, M.; Spolaor, F.; Beretta, C.; Fichera, F.; Bertoldo, A.; Volpe, D.; Sawacha, Z. Quantitative Assessment of Training Effects Using EksoGT® Exoskeleton in Parkinson’s Disease Patients: A Randomized Single Blind Clinical Trial. Contemp. Clin. Trials Commun. 2022, 28, 100926. [Google Scholar] [CrossRef] [PubMed]
- Morone, G.; Paolucci, S.; Cherubini, A.; De Angelis, D.; Venturiero, V.; Coiro, P.; Iosa, M. Robot-Assisted Gait Training for Stroke Patients: Current State of the Art and Perspectives of Robotics. Neuropsychiatr. Dis. Treat. 2017, 13, 1303–1311. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, N.; Prokop, G.; Weidner, R. Methodologies for Evaluating Exoskeletons with Industrial Applications. Ergonomics 2022, 65, 276–295. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.K.; Kim, K.; Ma, S.; Ueda, J. A Robotic Wearable Exoskeleton for Construction Worker’s Safety and Health. In Proceedings of the Construction Research Congress 2018: Safety and Disaster Management, New Orleans, LA, USA, 2–4 April 2018. [Google Scholar] [CrossRef]
- Bureau of Labor Statistics. 2016 Survey of Occupational Injuries & Illnesses. 2016. Available online: https://www.bls.gov/iif/nonfatal-injuries-and-illnesses-tables/soii-summary-historical/soii-charts-2016.pdf (accessed on 20 April 2024).
- Jia, B.; Kim, S.; Nussbaum, M.A. An EMG-Based Model to Estimate Lumbar Muscle Forces and Spinal Loads during Complex, High-Effort Tasks: Development and Application to Residential Construction Using Prefabricated Walls. Int. J. Ind. Ergon. 2011, 41, 437–446. [Google Scholar] [CrossRef]
- Shojaei, I.; Salt, E.G.; Hooker, Q.; Van Dillen, L.R.; Bazrgari, B. Comparison of Lumbo-Pelvic Kinematics during Trunk Forward Bending and Backward Return between Patients with Acute Low Back Pain and Asymptomatic Controls. Clin. Biomech. 2017, 41, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Bosch, T.; van Eck, J.; Knitel, K.; de Looze, M. The Effects of a Passive Exoskeleton on Muscle Activity, Discomfort and Endurance Time in Forward Bending Work. Appl. Ergon. 2016, 54, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Graham, R.B.; Agnew, M.J.; Stevenson, J.M. Effectiveness of an On-Body Lifting Aid at Reducing Low Back Physical Demands during an Automotive Assembly Task: Assessment of EMG Response and User Acceptability. Appl. Ergon. 2009, 40, 936–942. [Google Scholar] [CrossRef] [PubMed]
- Yap, H.K.; Ng, H.Y.; Yeow, C.-H. High-Force Soft Printable Pneumatics for Soft Robotic Applications. Soft Robot. 2016, 3, 144–158. [Google Scholar] [CrossRef]
- Ali, A.; Fontanari, V.; Schmoelz, W.; Agrawal, S.K. Systematic Review of Back-Support Exoskeletons and Soft Robotic Suits. Front. Bioeng. Biotechnol. 2021, 9, 765257. [Google Scholar] [CrossRef]
- Kermavnar, T.; de Vries, A.W.; de Looze, M.P.; O’Sullivan, L.W. Effects of Industrial Back-Support Exoskeletons on Body Loading and User Experience: An Updated Systematic Review. Ergonomics 2021, 64, 685–711. [Google Scholar] [CrossRef]
- Toxiri, S.; Näf, M.B.; Lazzaroni, M.; Fernández, J.; Sposito, M.; Poliero, T.; Monica, L.; Anastasi, S.; Caldwell, D.G.; Ortiz, J. Back-Support Exoskeletons for Occupational Use: An Overview of Technological Advances and Trends. IISE Trans. Occup. Ergon. Hum. Factors 2019, 7, 237–249. [Google Scholar] [CrossRef]
- Stirling, L.; Kelty-Stephen, D.; Fineman, R.; Jones, M.L.H.; Daniel Park, B.K.; Reed, M.P.; Parham, J.; Choi, H.J. Static, Dynamic, and Cognitive Fit of Exosystems for the Human Operator. Hum. Factors 2020, 62, 424–440. [Google Scholar] [CrossRef] [PubMed]
- Garrec, P. Design of an Anthropomorphic Upper Limb Exoskeleton Actuated by Ball-Screws and Cables. Bull. Acad. Sci. Ussr-Phys. Ser. 2010, 72, 23–34. [Google Scholar]
- Langlois, K.; Rodriguez-Cianca, D.; Serrien, B.; De Winter, J.; Verstraten, T.; Rodriguez-Guerrero, C.; Vanderborght, B.; Lefeber, D. Investigating the Effects of Strapping Pressure on Human-Robot Interface Dynamics Using a Soft Robotic Cuff. IEEE Trans. Med. Robot. Bionics 2021, 3, 146–155. [Google Scholar] [CrossRef]
- Kang, S.H.; Mirka, G.A. Effect of Trunk Flexion Angle and Time on Lumbar and Abdominal Muscle Activity While Wearing a Passive Back-Support Exosuit Device during Simple Posture-Maintenance Tasks. Ergonomics 2023, 66, 2182–2192. [Google Scholar] [CrossRef]
- Kazerooni, H.; Tung, W.; Pillai, M. Evaluation of Trunk-Supporting Exoskeleton. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2019, 63, 1080–1083. [Google Scholar] [CrossRef]
- Poliero, T.; Sposito, M.; Toxiri, S.; Di Natali, C.; Iurato, M.; Sanguineti, V.; Caldwell, D.G.; Ortiz, J. Versatile and Non-Versatile Occupational Back-Support Exoskeletons: A Comparison in Laboratory and Field Studies. Wearable Technol. 2021, 2, e12. [Google Scholar] [CrossRef]
- Baltrusch, S.J.; van Dieën, J.H.; Bruijn, S.M.; Koopman, A.S.; van Bennekom, C.A.M.; Houdijk, H. The Effect of a Passive Trunk Exoskeleton on Metabolic Costs during Lifting and Walking. Ergonomics 2019, 62, 903–916. [Google Scholar] [CrossRef]
- Schmalz, T.; Colienne, A.; Bywater, E.; Fritzsche, L.; Gärtner, C.; Bellmann, M.; Reimer, S.; Ernst, M. A Passive Back-Support Exoskeleton for Manual Materials Handling: Reduction of Low Back Loading and Metabolic Effort during Repetitive Lifting. IISE Trans. Occup. Ergon. Hum. Factors 2022, 10, 7–20. [Google Scholar] [CrossRef]
- Koopman, A.S.; Toxiri, S.; Power, V.; Kingma, I.; van Dieën, J.H.; Ortiz, J.; de Looze, M.P. The Effect of Control Strategies for an Active Back-Support Exoskeleton on Spine Loading and Kinematics during Lifting. J. Biomech. 2019, 91, 14–22. [Google Scholar] [CrossRef]
- Abdoli-E, M.; Stevenson, J.M. The Effect of On-Body Lift Assistive Device on the Lumbar 3D Dynamic Moments and EMG during Asymmetric Freestyle Lifting. Clin. Biomech. 2008, 23, 372–380. [Google Scholar] [CrossRef] [PubMed]
- Kuber, P.M.; Abdollahi, M.; Alemi, M.M.; Rashedi, E. A Systematic Review on Evaluation Strategies for Field Assessment of Upper-Body Industrial Exoskeletons: Current Practices and Future Trends. Ann. Biomed. Eng. 2022, 50, 1203–1231. [Google Scholar] [CrossRef] [PubMed]
- Kuber, P.M.; Godbole, H.; Rashedi, E. Detecting Fatigue during Exoskeleton-Assisted Trunk Flexion Tasks: A Machine Learning Approach. Appl. Sci. 2024, 14, 3563. [Google Scholar] [CrossRef]
- Poon, N.; van Engelhoven, L.; Kazerooni, H.; Harris, C. Evaluation of a Trunk Supporting Exoskeleton for Reducing Muscle Fatigue. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2019, 63, 980–983. [Google Scholar] [CrossRef]
- Rashedi, E.; Kim, S.; Nussbaum, M.A.; Agnew, M.J. Ergonomic Evaluation of a Wearable Assistive Device for Overhead Work. Ergonomics 2014, 57, 1864–1874. [Google Scholar] [CrossRef] [PubMed]
- Hefferle, M.; Snell, M.; Kluth, K. Influence of Two Industrial Overhead Exoskeletons on Perceived Strain—A Field Study in the Automotive Industry; Springer International Publishing: Berlin/Heidelberg, Germany, 2021; Volume 1210, ISBN 9783030517571. [Google Scholar]
- Chowdhury, R.H.; Reaz, M.B.I.; Bin Mohd Ali, M.A.; Bakar, A.A.A.; Chellappan, K.; Chang, T.G. Surface Electromyography Signal Processing and Classification Techniques. Sensors 2013, 13, 12431–12466. [Google Scholar] [CrossRef] [PubMed]
- Zheng, W.; Jin, M. The Effects of Class Imbalance and Training Data Size on Classifier Learning: An Empirical Study. SN Comput. Sci. 2020, 1, 71. [Google Scholar] [CrossRef]
- Madinei, S.; Alemi, M.M.; Kim, S.; Srinivasan, D.; Nussbaum, M.A. Biomechanical Evaluation of Passive Back-Support Exoskeletons in a Precision Manual Assembly Task: “Expected” Effects on Trunk Muscle Activity, Perceived Exertion, and Task Performance. Hum. Factors 2020, 62, 441–457. [Google Scholar] [CrossRef] [PubMed]
- Kuber, P.M.; Rashedi, E. Towards Reducing Risk of Injury in Nursing: Design and Analysis of a New Passive Exoskeleton for Torso Twist Assist. Proc. Int. Symp. Hum. Factors Ergon. Health Care 2021, 10, 217–222. [Google Scholar]
- Bär, M.; Luger, T.; Seibt, R.; Rieger, M.A.; Steinhilber, B. Using a Passive Back Exoskeleton During a Simulated Sorting Task: Influence on Muscle Activity, Posture, and Heart Rate. Hum. Factors 2024, 66, 40–55. [Google Scholar] [CrossRef] [PubMed]
- Goršič, M.; Song, Y.; Dai, B.; Novak, V.D. Short-Term Effects of the Auxivo LiftSuit during Lifting and Static Leaning. Appl. Ergon. 2022, 102, 103765. [Google Scholar] [CrossRef]

| Type of Measure from Sensor | Number of Features | List of Features |
|---|---|---|
| Low Back and Leg Movement (Inertial Sensors) | 160 | Mean (MeanEMGIMU), maximum (maxEMGIMU), minimum (minEMGIMU), standard deviation (stdEMGIMU), and variance (varEMGIMU) of the norm of acceleration, change in mean (n_meanEMGIMU), maximum (n_maxEMGIMU), minimum (n_minEMGIMU), standard deviation (n_stdEMGIMU), and variance (n_varEMGIMU) of the norm of acceleration. (for each activity within task cycle from all four sensors) |
| Muscle Activity (Electromyography) | 280 | Peak amplitude (AmpEMG), mean amplitude (MeanEMG), median frequency (MedianFrequency), standard deviation (stddevRMS), change in peak amplitude (n_AmpEMG), change in mean amplitude (n_AmpEMG), change in median frequency (n_MedianFrequency), change in standard deviation (n_stddevRMS). (for each activity within task cycle from all four sensors) |
| Factor | Level | Description | |
|---|---|---|---|
| Sensors | s1 | Sensor on Left Erector Spinae (LES) | |
| s2 | Sensor on Left Biceps Spinae (LBF) | ||
| s3 | Sensor on Right Erector Spinae (RES) | ||
| s4 | Sensor on Right Biceps Femoris (RBF) | ||
| Measures | Muscle Activity | Surface Electromyography | |
| Kinematics | Acceleration | ||
| Muscle Activity and Kinematics | Combination of Surface Electromyography and Acceleration | ||
| Fatigue Region | FB | Fatigue in Back | |
| FL | Fatigue in Legs | ||
| Grouping Method (X = B/L) | Binary (FX) | FX2G1 | IF(Fatigue Level ≤ 3,”L”,”M”) |
| FX2G2 | IF(Fatigue Level ≤ 2,”L”,”M”) | ||
| FX2G3 | IF(Fatigue Level ≤ 4,”L”,”M”) | ||
| Tertiary (FX) | FX3G1 | IF(Fatigue Level ≤ 2,”L”,(IF(Fatigue Level ≤4,”M”,”H”))) | |
| FX3G2 | IF(Fatigue Level≤1,”L”,(IF(Fatigue Level ≤ 3,”M”,”H”))) | ||
| FX3G3 | IF(Fatigue Level ≤ 3,”L”,(IF(Fatigue Level ≤ 5,”M”,”H”))) | ||
| Classification Algorithms | SVM | Support Vector Machine | |
| RF | Random Forest | ||
| XGB | XGBoost | ||
| Model-Tuning Techniques | Baseline | - | |
| SMOTE | Synthetic Minority Over-sampling Technique (SMOTE) | ||
| GRID | Finding best hyperparameters with cross validation using grid search along with SMOTE | ||
| Fatigue Region | Grouping Method | Measure | Sensors | Location | C | A | P | S | R | F1 | GI |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Leg (Binary) | FL2G2 | EMG, Kinematics | 2 | LES, LBF | XGB | 0.95 | 0.97 | 0.83 | 0.97 | 0.97 | 0.04 |
| FL2G2 | EMG, Kinematics | 4 | LES, LBF, RES, RBF | XGB | 0.94 | 0.96 | 0.78 | 0.97 | 0.97 | 0.05 | |
| FL2G2 | EMG | 4 | LES, LBF, RES, RBF | RF | 0.93 | 0.95 | 0.72 | 0.96 | 0.96 | 0.06 | |
| FL2G2 | EMG, Kinematics | 2 | LBF, RBF | RF | 0.93 | 0.95 | 0.72 | 0.96 | 0.96 | 0.06 | |
| FL2G2 | EMG, Kinematics | 1 | RES | RF | 0.93 | 0.96 | 0.78 | 0.95 | 0.96 | 0.06 | |
| FL2G2 | Kinematics | 1 | LBF | RF | 0.88 | 0.94 | 0.67 | 0.91 | 0.93 | 0.11 | |
| Leg (Tertiary) | FL3G2 | EMG, Kinematics | 4 | LES, LBF, RES, RBF | XGB | 0.79 | 0.78 | 0.79 | 0.79 | 0.78 | 0.31 |
| FL3G2 | EMG | 4 | LES, LBF, RES, RBF | RF | 0.77 | 0.76 | 0.77 | 0.77 | 0.76 | 0.33 | |
| FL3G2 | Kinematics | 4 | LES, LBF, RES, RBF | XGB | 0.74 | 0.74 | 0.74 | 0.74 | 0.74 | 0.37 | |
| FL3G2 | EMG, Kinematics | 4 | LES, LBF, RES, RBF | RF | 0.74 | 0.73 | 0.74 | 0.74 | 0.73 | 0.37 | |
| FL3G1 | EMG, Kinematics | 4 | LES, LBF, RES, RBF | RF | 0.74 | 0.73 | 0.74 | 0.74 | 0.73 | 0.38 | |
| FL3G1 | EMG | 4 | LES, LBF, RES, RBF | RF | 0.72 | 0.72 | 0.72 | 0.72 | 0.71 | 0.40 | |
| Back (Binary) | FB2G2 | EMG, Kinematics | 4 | LES, LBF, RES, RBF | XGB | 0.88 | 0.89 | 0.62 | 0.97 | 0.93 | 0.11 |
| FB2G2 | EMG | 4 | LES, LBF, RES, RBF | XGB | 0.86 | 0.90 | 0.69 | 0.91 | 0.91 | 0.13 | |
| FB2G2 | Kinematics | 4 | LES, LBF, RES, RBF | RF | 0.86 | 0.89 | 0.62 | 0.93 | 0.91 | 0.13 | |
| FB2G2 | EMG, Kinematics | 1 | RES | XGB | 0.85 | 0.89 | 0.66 | 0.91 | 0.90 | 0.14 | |
| FB2G2 | Kinematics | 1 | RES | XGB | 0.82 | 0.89 | 0.66 | 0.87 | 0.88 | 0.17 | |
| FB2G2 | Kinematics | 1 | LES | XGB | 0.82 | 0.89 | 0.66 | 0.87 | 0.88 | 0.17 | |
| Back (Tertiary) | FB3G2 | EMG, Kinematics | 4 | LES, LBF, RES, RBF | XGB | 0.67 | 0.67 | 0.67 | 0.67 | 0.67 | 0.47 |
| FB3G3 | EMG, Kinematics | 4 | LES, LBF, RES, RBF | XGB | 0.67 | 0.66 | 0.67 | 0.67 | 0.65 | 0.48 | |
| FB3G3 | EMG | 4 | LES, LBF, RES, RBF | XGB | 0.67 | 0.65 | 0.67 | 0.67 | 0.66 | 0.48 |
| Sensors | Location | A | P | S | R | F1 | GI |
|---|---|---|---|---|---|---|---|
| 2 | LES, RES | 0.95 | 0.97 | 0.83 | 0.97 | 0.97 | 0.04 |
| 4 | LES, LBF, RES, RBF | 0.94 | 0.96 | 0.78 | 0.97 | 0.97 | 0.05 |
| 1 | RBF | 0.92 | 0.97 | 0.83 | 0.93 | 0.95 | 0.07 |
| 2 | LBF, RES | 0.92 | 0.97 | 0.83 | 0.93 | 0.95 | 0.07 |
| 2 | LBF, RBF | 0.91 | 0.96 | 0.78 | 0.93 | 0.95 | 0.08 |
| 1 | RES | 0.91 | 0.97 | 0.83 | 0.92 | 0.95 | 0.08 |
| 2 | LES, RBF | 0.90 | 0.97 | 0.83 | 0.91 | 0.94 | 0.09 |
| 1 | LBF | 0.88 | 0.94 | 0.67 | 0.92 | 0.93 | 0.10 |
| 1 | LES | 0.85 | 0.92 | 0.56 | 0.90 | 0.91 | 0.13 |
| Model | Grouping Method | Measure | Sensors | Location | A | P | S | R | F1 | GI |
|---|---|---|---|---|---|---|---|---|---|---|
| A | FL2G2 | EMG, Kinematics | 2 | LES, LBF | 0.95 | 0.97 | 0.83 | 0.97 | 0.97 | 0.04 |
| B | FL3G2 | Kinematics | 4 | LES, LBF, RES, RBF | 0.74 | 0.74 | 0.74 | 0.74 | 0.74 | 0.37 |
| C | FB2G2 | Kinematics | 1 | RES | 0.82 | 0.89 | 0.66 | 0.87 | 0.88 | 0.17 |
| D | FB3G2 | EMG, Kinematics | 4 | LES, LBF, RES, RBF | 0.67 | 0.67 | 0.67 | 0.67 | 0.67 | 0.47 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuber, P.M.; Kulkarni, A.R.; Rashedi, E. Machine Learning-Based Fatigue Level Prediction for Exoskeleton-Assisted Trunk Flexion Tasks Using Wearable Sensors. Appl. Sci. 2024, 14, 4563. https://doi.org/10.3390/app14114563
Kuber PM, Kulkarni AR, Rashedi E. Machine Learning-Based Fatigue Level Prediction for Exoskeleton-Assisted Trunk Flexion Tasks Using Wearable Sensors. Applied Sciences. 2024; 14(11):4563. https://doi.org/10.3390/app14114563
Chicago/Turabian StyleKuber, Pranav Madhav, Abhineet Rajendra Kulkarni, and Ehsan Rashedi. 2024. "Machine Learning-Based Fatigue Level Prediction for Exoskeleton-Assisted Trunk Flexion Tasks Using Wearable Sensors" Applied Sciences 14, no. 11: 4563. https://doi.org/10.3390/app14114563
APA StyleKuber, P. M., Kulkarni, A. R., & Rashedi, E. (2024). Machine Learning-Based Fatigue Level Prediction for Exoskeleton-Assisted Trunk Flexion Tasks Using Wearable Sensors. Applied Sciences, 14(11), 4563. https://doi.org/10.3390/app14114563







