Investigation of the Photothermal Performance of the Composite Scaffold Containing Light-Heat-Sensitive Nanomaterial SiO2@Fe3O4
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemicals
2.2. Experimental Equipment
2.3. Selection of Material Proportions for Bone Scaffolds
2.4. Synthesis of Photothermal-Sensitive Nanoparticles
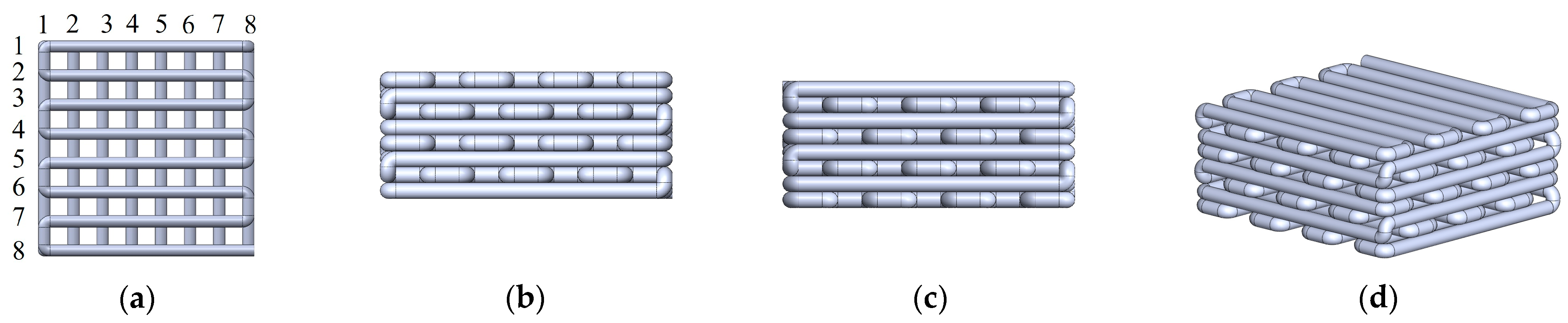
2.5. Preparation of Photothermal Composite Bone Scaffold
2.6. XRD Analysis
2.7. Microstructural Analysis
2.8. Measurement of Water Contact Angle
2.9. Mechanical Properties Testing
2.10. Photothermal Characterization
3. Results and Discussion
3.1. Orthogonal Experimental Analysis of Scaffold Materials
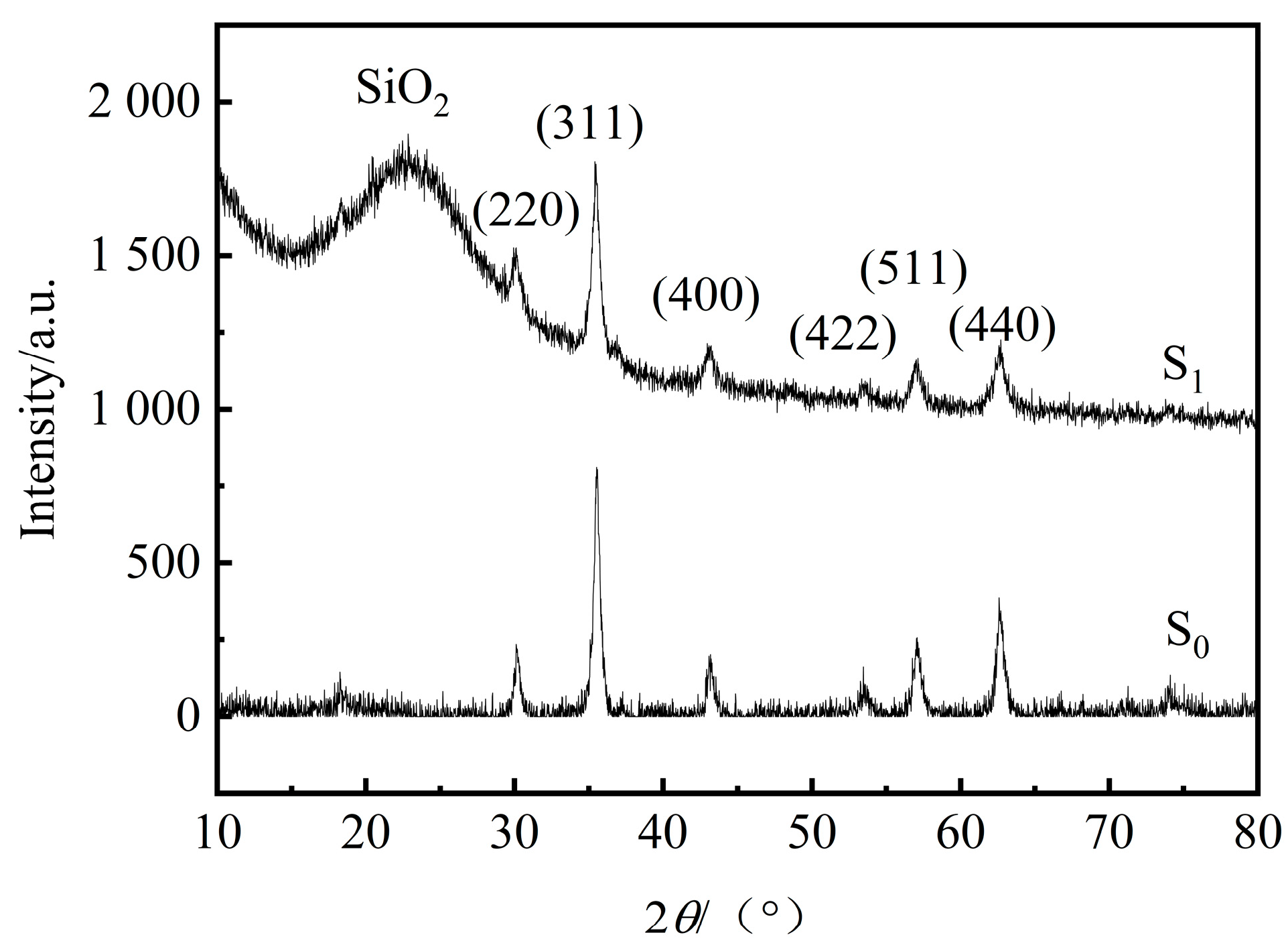
3.2. XRD Analysis of Photothermal Sensitive Nanoparticles
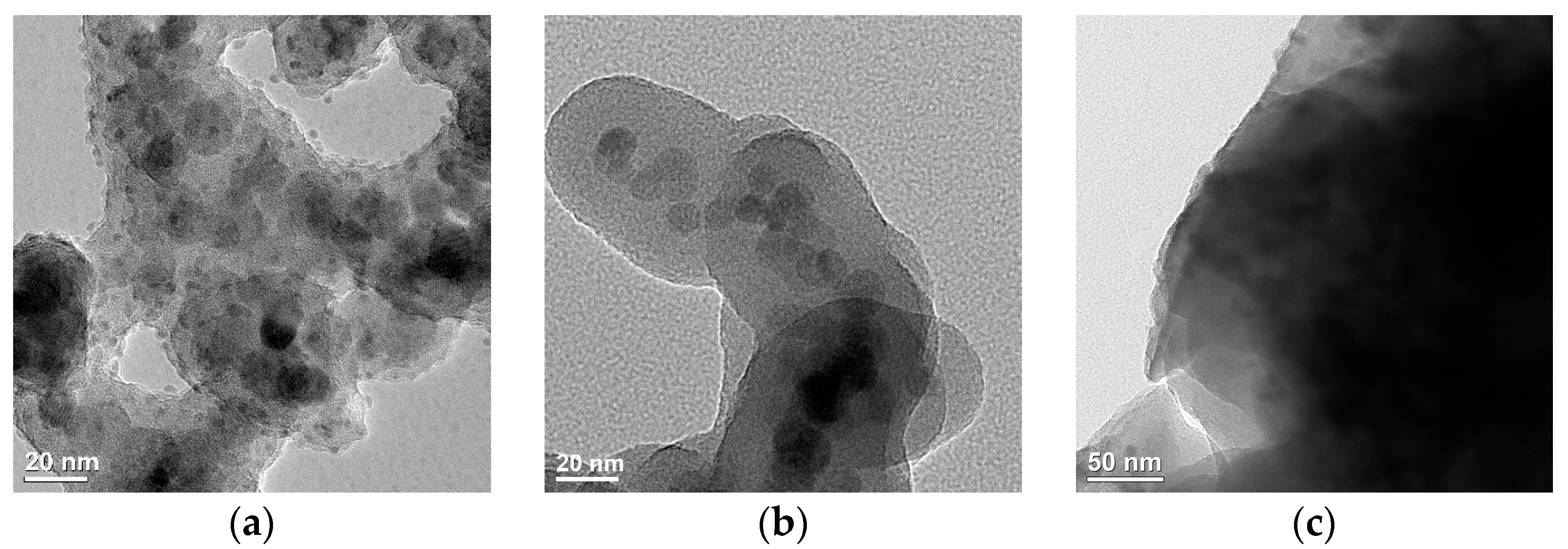
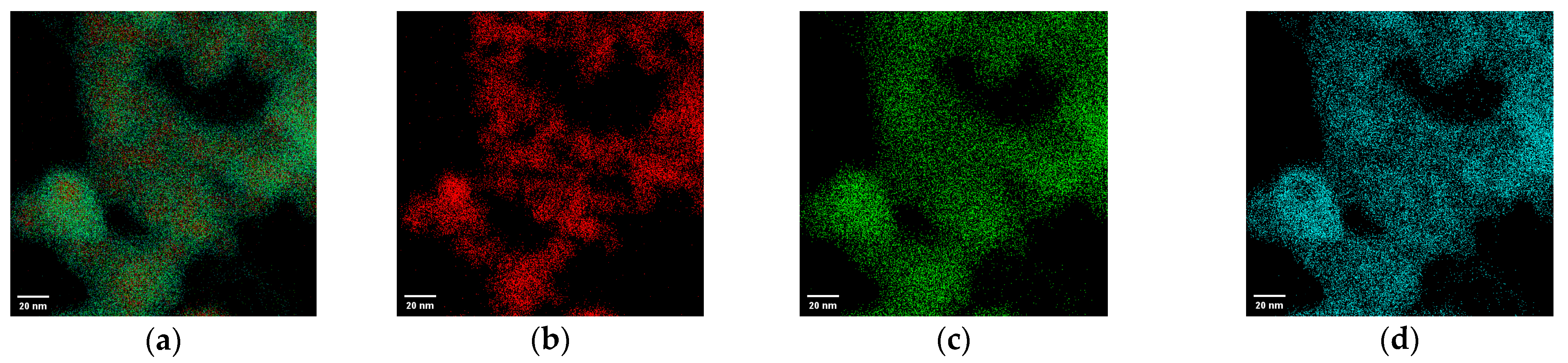
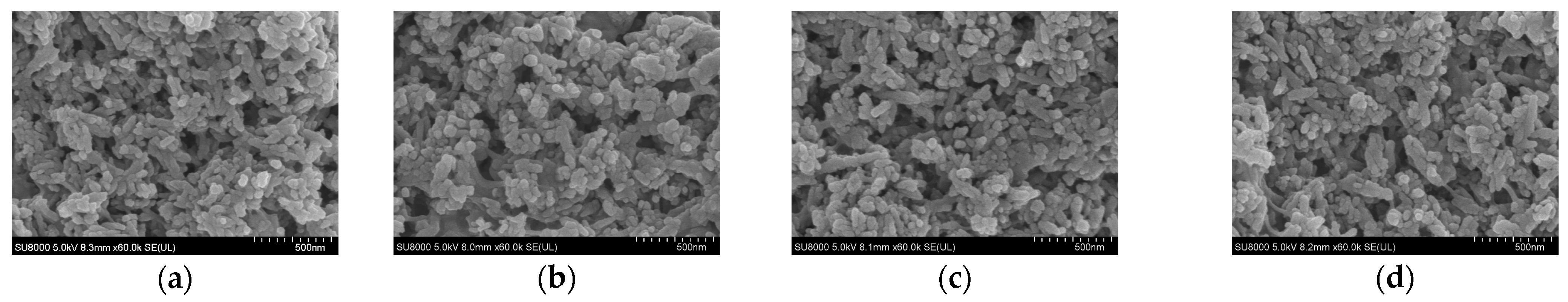
3.3. Microstructural Analysis
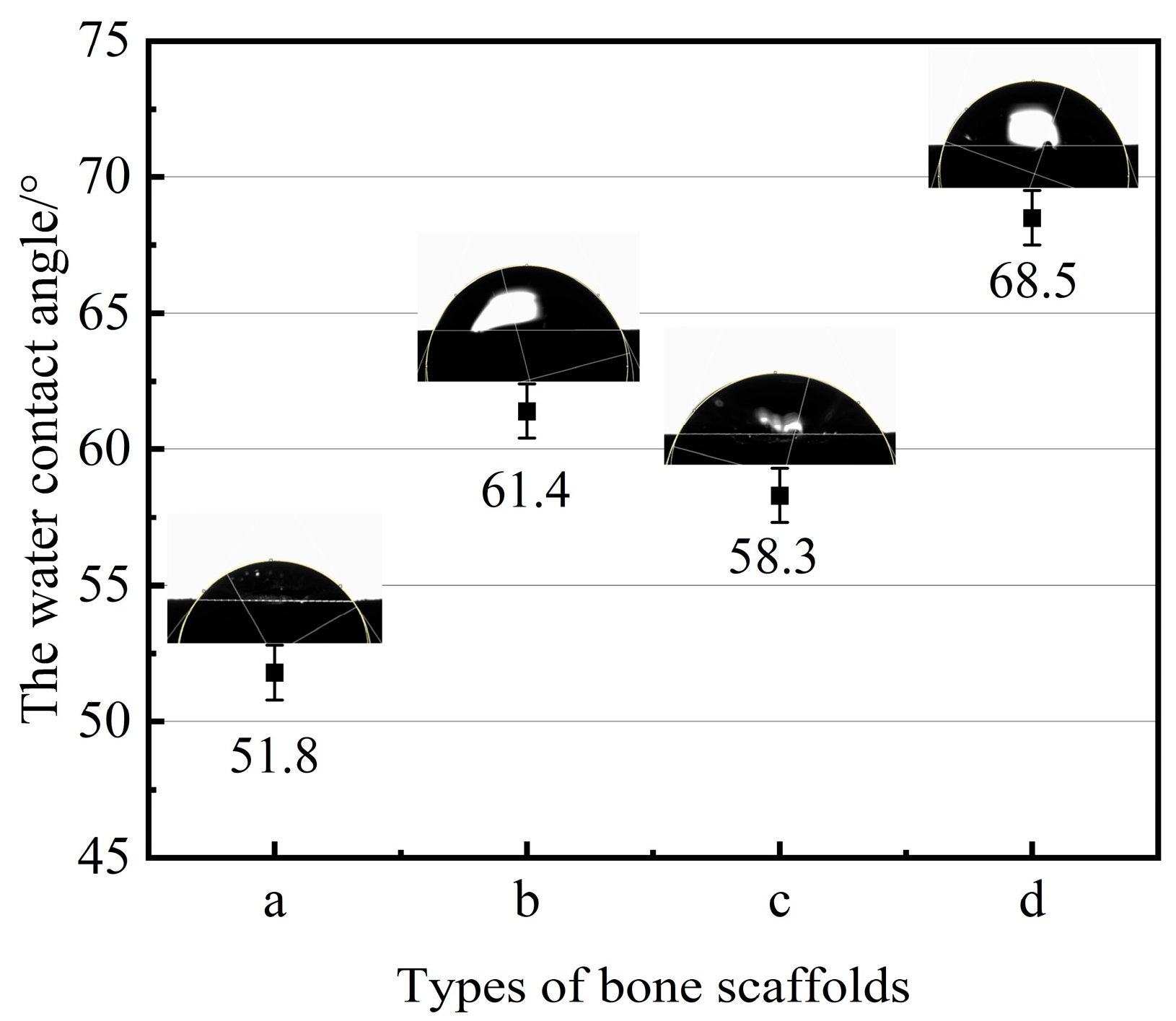
3.4. Measurement of Contact Angle and Mechanical Properties of Bone Scaffolds
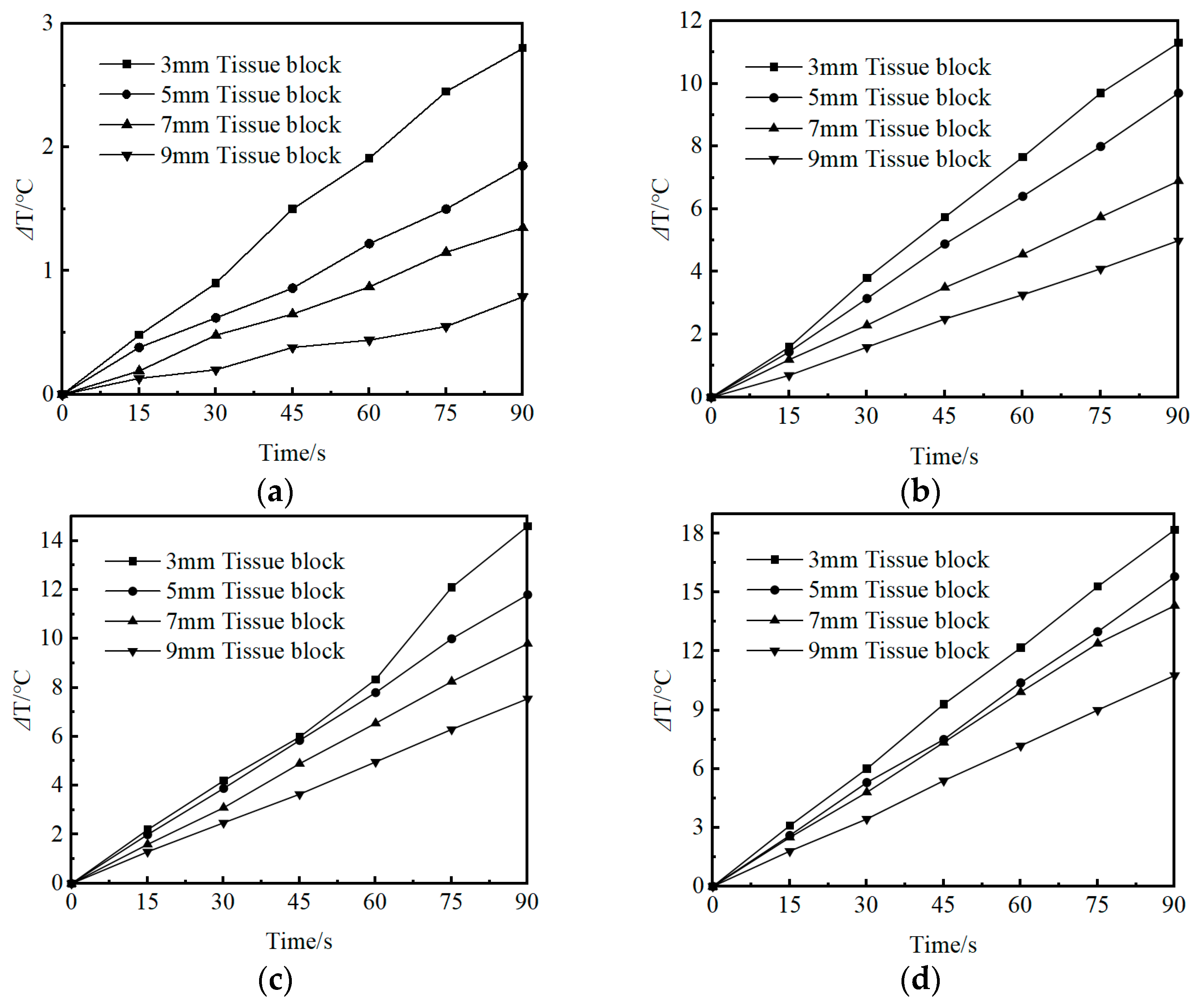
3.5. Evaluation of the Photothermal Properties of Bone Scaffolds
4. Conclusions
- (1)
- The photothermal-sensitive nanoparticles SiO2@Fe3O4, synthesized via hydrolysis and condensation using 5 mL TEOS, exhibited approximately 18 nm SiO2 coatings. These coatings were uniformly distributed, effectively preventing the aggregation of the photothermal-sensitive nanoparticles Fe3O4. Additionally, the micro-pore structure of the fabricated photothermal composite bone scaffold showed uniform distribution, devoid of localized aggregation phenomena. This ensured the avoidance of adverse effects on the properties and applications of the scaffold material.
- (2)
- The photothermal composite scaffold with a mass fraction of 5% for photothermal-sensitive nanoparticles exhibited a compressive strength of 5.722 MPa and a contact angle of 58.3°, demonstrating favorable mechanical support and hydrophilicity. This scaffold provides a stable environment for the adhesion and growth of bone tissue cells. Upon exposure to near-infrared light for 40–45 s, the 5% photothermal composite scaffold induced a temperature increase of 3–6 °C in different tissue depths, achieving controlled internal temperature variations through mild thermal stimulation. This approach aims to promote osteogenic differentiation and facilitate the repair of bone defects.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Konda, S.R.; Littlefield, C.P.; Carlock, K.D.; Ganta, A.; Leucht, P.; Egol, K.A. Autogenous iliac crest bone grafting for tibial nonunions revisited: Does approach matter? Arch. Orthop. Trauma Surg. 2021, 142, 961–968. [Google Scholar] [CrossRef] [PubMed]
- Xie, H.Y.; Ruan, S.J.; Zhao, M.L.; Long, J.; Ma, X.; Guo, J.; Lin, X. Preparation and characterization of 3D hydroxyapatite/collagen scaffolds and its application in bone regeneration with bone morphogenetic protein-2. RSC Adv. 2023, 13, 23010–23020. [Google Scholar] [CrossRef] [PubMed]
- Motamedian, S.R.; Khojaste, M.; Khojasteh, A. Success rate of implants placed in autogenous bone blocks versus allogenic bone blocks: A systematic literature review. Ann. Maxillofac. Surg. 2016, 6, 78–90. [Google Scholar] [PubMed]
- Sharmin, F.; O’Sullivan, M.; Malinowski, S.; Lieberman, J.R.; Khan, Y. Large scale segmental bone defect healing through the combined delivery of VEGF and BMP-2 from biofunctionalized cortical allografts. J. Biomed. Mater. Res. Part B Appl. Biomater. 2019, 107, 1002–1010. [Google Scholar] [CrossRef] [PubMed]
- Das, G.; Shin, H.S.; Campos, E.V.R.; Fraceto, L.F.; del Pilar Rodriguez-Torres, M.; Mariano, K.C.F.; de Araujo, D.R.; Fernández-Luqueño, F.; Grillo, R.; Patra, J.K. Sericin based nanoformulations: A comprehensive review on molecular mechanisms of interaction with organisms to biological applications. J. Nanobiotechnol. 2021, 19, 30. [Google Scholar] [CrossRef] [PubMed]
- Sangeetha, K.; Ashok, M.; Girija, E.K. Development of multifunctional cobalt ferrite/hydroxyapatite nanocomposites by microwave assisted wet precipitation method: A promising platform for synergistic chemo-hyperthermia therapy. Ceram. Int. 2019, 45, 12860–12869. [Google Scholar] [CrossRef]
- Menazea, A.A.; Mostafa, M.S.; Awwad, N.S.; Ali, H.E.; Moustapha, M.E.; Bajaber, M.A. Improvement of medical applicability of hydroxyapatite/antimonous oxide/graphene oxide mixed systems for biomedical application. J. Inorg. Organomet. Polym. Mater. 2022, 32, 3220–3234. [Google Scholar] [CrossRef]
- Kurtuldu, F.; Mutlu, N.; Boccaccini, A.R.; Galusek, D. Gallium containing bioactive materials: A review of anticancer, antibacterial, and osteogenic properties. Bioact. Mater. 2022, 17, 125–146. [Google Scholar] [CrossRef] [PubMed]
- Pokhrel, S. Hydroxyapatite: Preparation, properties and its biomedical applications. Adv. Chem. Eng. Sci. 2018, 8, 225. [Google Scholar] [CrossRef]
- Suhardi, J.V.; Morgan, D.F.A.; Muratoglu, O.K.; Oral, E. Radioprotection and cross-linking of allograft bone in the presence of vitamin E. J. Biomed. Mater. Res. Part B Appl. Biomater. 2020, 108, 2354–2367. [Google Scholar] [CrossRef]
- Park, H.; Choi, J.W.; Jeong, W.S. Clinical application of three-dimensional printing of polycaprolactone/beta-tricalcium phosphate implants for cranial reconstruction. J. Craniofacial Surg. 2022, 33, 1394–1399. [Google Scholar] [CrossRef] [PubMed]
- Peroglio, M.; Gremillard, L.; Gauthier, C.; Chazeau, L.; Verrier, S.; Alini, M.; Chevalier, J. Mechanical properties and cytocompatibility of poly (ε-caprolactone)-infiltrated biphasic calcium phosphate scaffolds with bimodal pore distribution. Acta Biomater. 2010, 6, 4369–4379. [Google Scholar] [CrossRef] [PubMed]
- Hang, K.; Ye, C.Y.; Chen, E.M.; Zhang, W.; Xue, D.; Pan, Z. Role of the heat shock protein family in bone metabolism. Cell Stress Chaperones 2018, 23, 1153–1164. [Google Scholar] [CrossRef] [PubMed]
- Han, L.; Guo, Y.; Jia, L.; Zhang, Q.; Sun, L.; Yang, Z.; Dai, Y.; Lou, Z.; Xia, Y. 3D magnetic nanocomposite scaffolds enhanced the osteogenic capacities of rat bone mesenchymal stem cells in vitro and in a rat calvarial bone defect model by promoting cell adhesion. J. Biomed. Mater. Res. Part A 2021, 109, 1670–1680. [Google Scholar] [CrossRef] [PubMed]
- Yun, H.M.; Ahn, S.J.; Park, K.R.; Kim, M.J.; Kim, J.J.; Jin, G.Z.; Kim, H.W.; Kim, E.C. Magnetic nanocomposite scaffolds combined with static magnetic field in the stimulation of osteoblastic differentiation and bone formation. Biomaterials 2016, 85, 88–98. [Google Scholar] [CrossRef] [PubMed]
- Beitollahi, H.; Ebadinejad, F.; Shojaie, F.; Torkzadeh-Mahani, M. A magnetic core–shell Fe3O4@SiO2/MWCNT nanocomposite modified carbon paste electrode for amplified electrochemical sensing of amlodipine and hydrochlorothiazide. Anal. Methods 2016, 8, 6185–6193. [Google Scholar] [CrossRef]
- Singh, R.K.; Kim, T.H.; Patel, K.D.; Knowles, J.C.; Kim, H.W. Biocompatible magnetite nanoparticles with varying silica-coating layer for use in biomedicine: Physicochemical and magnetic properties, and cellular compatibility. J. Biomed. Mater. Res. Part A 2012, 100, 1734–1742. [Google Scholar] [CrossRef] [PubMed]
- Duta, L.; Dorcioman, G.; Grumezescu, V. A review on biphasic calcium phosphate materials derived from fish discards. Nanomaterials 2021, 11, 2856. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Hu, B.; Li, H.; Feng, G.; Pan, S.; Chen, Z.; Li, B.; Song, J. Biomimetic mineralized hydroxyapatite nanofiber-incorporated methacrylated gelatin hydrogel with improved mechanical and osteoinductive performances for bone regeneration. Int. J. Nanomed. 2022, 17, 1511–1529. [Google Scholar] [CrossRef]
- Arif, Z.U.; Khalid, M.Y.; Noroozi, R.; Sadeghianmaryan, A.; Jalalvand, M.; Hossain, M. Recent advances in 3D-printed polylactide and polycaprolactone-based biomaterials for tissue engineering applications. Int. J. Biol. Macromol. 2022, 218, 930–968. [Google Scholar] [CrossRef]
- Entezari, A.; Roohani, I.; Li, G.; Dunstan, C.R.; Rognon, P.; Li, Q.; Jiang, X.; Zreiqat, H. Architectural design of 3D printed scaffolds controls the volume and functionality of newly formed bone. Adv. Healthc. Mater. 2019, 8, 1801353. [Google Scholar] [CrossRef] [PubMed]
- Sola, A.; Bellucci, D.; Cannillo, V. Functionally graded materials for orthopedic applications–an update on design and manufacturing. Biotechnol. Adv. 2016, 34, 504–531. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.J.; Xu, S.Q.; Zhou, S.W.; Xu, W.; Leary, M.; Choong, P.; Qian, M.; Brandt, M.; Xie, Y.M. Topological design and additive manufacturing of porous metals for bone scaffolds and orthopaedic implants: A review. Biomaterials 2016, 83, 127–141. [Google Scholar] [CrossRef] [PubMed]
- Li, W.H.; Li, S.T.; Zhang, J.W.; Zhong, H.; Liang, J.; Huang, S.; Liao, G.; Zhang, B.; Liu, C. Fabrication and evaluation of bone morphogenetic protein-2 microspheres coated black phosphorus nanosheets@ polylactic-glycolic acid copolymers scaffold: A multifunctional antibacterial photothermal scaffold for bone regeneration. Int. J. Biol. Macromol. 2022, 210, 350–364. [Google Scholar] [CrossRef]

| Levels | Factors | |||
|---|---|---|---|---|
| PVA Conc. (%) | HA: β-TCP (g:g) | HA: PCL (g:g) | Blank Column | |
| 1 | 8 | 9:1 | 4:1 | 1 |
| 2 | 10.5 | 4:1 | 7:3 | 2 |
| 3 | 13 | 7:3 | 3:2 | 3 |
| Number | PVA Conc. (%) | HA: β-TCP (g:g) | HA: PCL (g:g) | Blank Column | Compressive Strength (MPa) |
|---|---|---|---|---|---|
| 1 | 8 | 9:1 | 4:1 | 1 | 10.823 |
| 2 | 8 | 4:1 | 7:3 | 2 | 7.661 |
| 3 | 8 | 7:3 | 3:2 | 3 | 7.881 |
| 4 | 10.5 | 9:1 | 7:3 | 3 | 16.713 |
| 5 | 10.5 | 4:1 | 3:2 | 1 | 16.239 |
| 6 | 10.5 | 7:3 | 4:1 | 2 | 15.557 |
| 7 | 13 | 9:1 | 3:2 | 2 | 28.546 |
| 8 | 13 | 4:1 | 4:1 | 3 | 31.173 |
| 9 | 13 | 7:3 | 7:3 | 1 | 23.365 |
| k1 | 8.788 | 18.694 | 19.184 | 16.809 | |
| k2 | 16.170 | 18.358 | 15.913 | 17.255 | |
| k3 | 27.695 | 15.601 | 17.555 | 18.589 | |
| R | 18.907 | 3.093 | 3.271 | 1.78 | |
| Order | 1 | 3 | 2 | 4 | |
| Optimal level | A3 | B1 | C1 | ||
| Optimal combination | A3B1C1 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shan, C.; Xu, Y.; Li, S. Investigation of the Photothermal Performance of the Composite Scaffold Containing Light-Heat-Sensitive Nanomaterial SiO2@Fe3O4. Appl. Sci. 2024, 14, 4911. https://doi.org/10.3390/app14114911
Shan C, Xu Y, Li S. Investigation of the Photothermal Performance of the Composite Scaffold Containing Light-Heat-Sensitive Nanomaterial SiO2@Fe3O4. Applied Sciences. 2024; 14(11):4911. https://doi.org/10.3390/app14114911
Chicago/Turabian StyleShan, Changpeng, Yan Xu, and Shengkai Li. 2024. "Investigation of the Photothermal Performance of the Composite Scaffold Containing Light-Heat-Sensitive Nanomaterial SiO2@Fe3O4" Applied Sciences 14, no. 11: 4911. https://doi.org/10.3390/app14114911




