Abstract
Cephalometry is a crucial examination in orthodontic diagnostics and during the planning of orthognathic surgical procedures. The objective of this article was to compare cephalometric measurements conducted by different specialists and systems tailored for such measurements, as well as to evaluate the capabilities of artificial intelligence in this field. In January 2024, we conducted electronic searches in the PubMed, Scopus, and Web of Science (WoS) databases. In the Scopus database, the results were refined to titles, abstracts, and keywords, while in PubMed, they were narrowed down to titles and abstracts. In WoS, the results were refined only to abstracts. The search criteria were based on the following terms: (cephalometric) AND (analysis) AND (discrepancy) AND ((orthodontic) OR (radiologist)). A total of 263 articles were identified, of which 17 met the criteria and were incorporated into the review. The review allowed us to conclude that the accuracy of cephalometric measurements relied on the expertise of the operator—specialists with more experience exhibited greater precision compared to novices or individuals not specialized in orthodontics. Cephalometric measurement computer programs yielded outcomes that streamlined work processes, minimized human errors, and enhanced precision. A novel aspect involved the application of artificial intelligence, which also demonstrated high precision and a substantial reduction in working time, although its utilization still necessitates further enhancements. Further research was required to address these limitations and to optimize the incorporation of technology in orthodontic and orthognathic surgery practices.
1. Introduction
Nowadays, orthodontic treatment relies significantly on precise radiographic diagnostics [1]. Traditional panoramic radiographs (dental X-ray of the upper and lower jaw) and lateral cephalograms (standardized lateral view X-ray of the head and neck for the evaluation of bony and soft tissue structures) serve as fundamental tools for assessing jaw, teeth, and dento-alveolar discrepancies [1]. Additionally, modern techniques, like CBCT (cone-beam computed tomography) and 3D facial evaluation, play supplementary roles in the comprehensive assessment of both facial soft and hard tissues, and become crucial in cases of doubt about the position of cephalometric points (landmarks, defined points found in the area of the human head) or a large defect that may require surgical intervention [1,2]. While some dento-alveolar discrepancies may stem solely from dental issues, others may involve skeletal abnormalities. In such cases, thorough and improved diagnostics become imperative [1,2]. CBCT is an advanced imaging modality that offers a radiation exposure dose that is 10 times less than that of conventional CT scans during maxillofacial exposure and enables three-dimensional imaging of hard tissue structures [3].
Despite the utilization of various diagnostic and orthodontic tools, certain anatomical reference points remain pivotal in establishing basic patient characteristics and, thus, in choosing the right treatment. Classic orthodontic approaches mostly use a standard lateral cephalometric radiograph to evaluate the patient’s profile, bite, and occlusion [1,2,3]. The so-called 3D individual approach for each patient is currently regarded as the method of choice for several reasons [4,5,6,7]. Due to improvements in digital diagnostics, orthodontic treatment is greatly influenced by these advancements. The use of 3D devices and the importance of cone-beam computed tomography (CBCT) significantly impact novel orthodontic and orthognathic surgery advances in the field of diagnostics, planning, and evaluation of the craniofacial skeleton. Currently, many reports describe improvements in CBCT, 3D imaging, artificial intelligence (AI) usage, and other devices to enhance overall facial and bite diagnostics. These advancements aim to establish the most accurate and up-to-date treatment plans for each case of dental and skeletal malocclusions [4,5,6,7]. Due to the numerous papers focusing on computer-enhanced planning and evaluation, it is essential to understand not only the benefits, limitations, strengths, and weaknesses of each classic 2D versus 3D evaluation but also how new techniques can assess the cephalometric image of each patient in computer-assisted and AI-improved studies [7,8,9,10,11].
In cases of severe dento-alveolar and skeletal discrepancies, a detailed evaluation of the 3D relationship of various cephalometric landmarks is crucial for planning the extent of the surgical operation. While orthodontic evaluations typically rely on individual landmark assessments by each clinician, specialized software can offer automatic features to find these reference points according to a predefined algorithm. During manual examination and evaluation of these cephalometric points, difficulties in finding their position and the angulation of selected variables may be observed [1,2,12,13]. Each orthodontist should enhance their treatment approach and leverage the benefits of new technologies, particularly the recent advances in 3D-CBCT. Software programs, in particular, hold significant potential to greatly enhance each diagnostic step [14,15]. Despite the plethora of available software, CBCTs, and other devices used in today’s dental, surgical, and orthodontic practices, there are still many underestimated and not fully evaluated aspects. One of these is the comparison between AI-derived and computer-enhanced automatic cephalometric analysis versus the classic 2D manual approach [14,15,16,17,18]. There seems to be a growing trend towards the integration of new technologies and advancements in both medicine and dentistry. This trend holds the promise of significantly enhancing patient diagnostics, therapies, and overall outcomes, thereby improving patients’ quality of life.
Selecting the most accurate cephalometric reference point is influenced by various factors. Foremost among these factors is the experience and expertise of each clinician. Additionally, the quality and clarity of the radiographs used for anthropometric purposes greatly affect the placement of selected points [2]. At the same time the distinction between the hard structures and the soft structures in their proximity is important to establish this position correctly. One potential solution to this issue could involve enhancing clinician training in selecting the most precise anatomical point positions and leveraging artificial intelligence (AI) for the development of automatic measurement protocols to achieve more reliable and accurate anatomical reference points [1,2,12,13,19,20,21,22,23,24]. The review on the usage of AI-driven and improved cephalometric analysis prevented herein is very important for the future of dentistry and orthodontics. This might be related to more accurate, 3D diagnostics, focused on each patient individual anatomy of the facial skeleton, jaws, teeth relations and might improve the reliability and reproducibility of three-dimensional cephalometric landmarks, similar to the findings presented in a review by Lisboa et al. [25].
Currently, cone-beam computed tomography (CBCT) stands as the standard for evaluating craniofacial features, encompassing both dento-alveolar and skeletal abnormalities within the facial skeleton [1,3]. Authors of this systematic review aim to emphasize the utilization of artificial intelligence for manual computer-driven cephalometric evaluations in patients undergoing orthodontic or combined orthodontic-surgical treatments. The purpose of this review is to compare and establish the most accurate and detailed method for the placement and tracing of cephalometric reference points as well as to determine whether the existing literature provides examples of potential solutions for the accurate landmark localization of individual patient characteristics, with a particular focus on artificial intelligence-based modelling. Given the absence of a systematic review on this specific topic in the searched databases, it is deemed essential to address this gap through a systematic approach.
2. Materials and Methods
2.1. Focused Question
This systematic review followed the PICO framework [26] as follows.
PICO question: In the case of cephalometric X-rays (population), will performing a cephalometric analysis by a radiologist or artificial intelligence (investigated condition) lead to a change in the measurements values (outcome) compared to the analysis results obtained by the orthodontist (comparison condition)?
2.2. Protocol
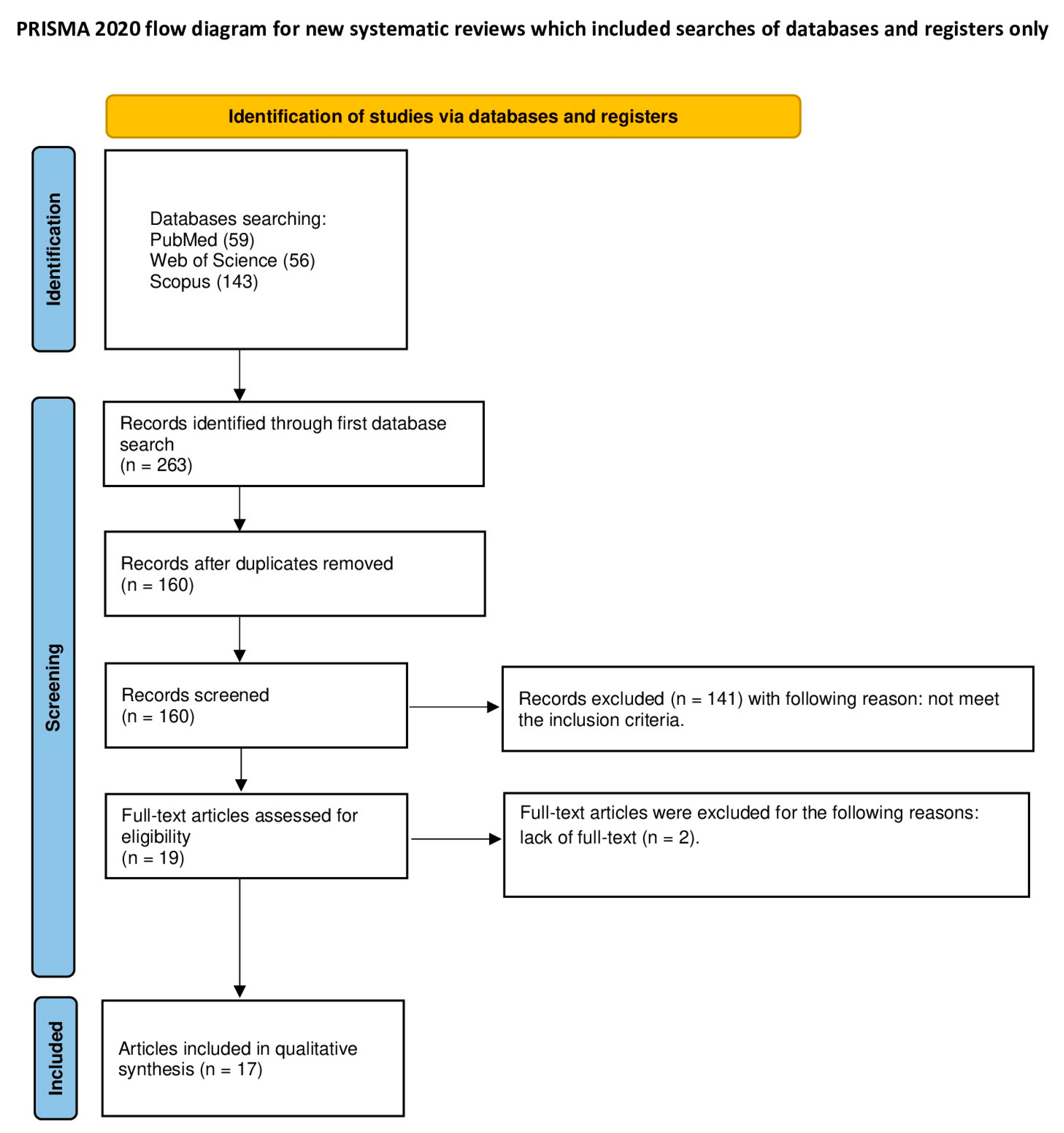
The article selection process for this systematic review was meticulously outlined according to the PRISMA flow diagram (see Figure 1). The systematic review was registered on the Open Science Framework under the following link: https://osf.io/2vyd7/ (accessed on 3 June 2024).
Figure 1.
The PRISMA 2020 flow diagram [27].
2.3. Eligibility Criteria
All studies incorporated into the systematic review were required to adhere to the following criteria: they had to investigate discrepancies in cephalometric analysis results between orthodontists and radiologists, as well as between orthodontists and artificial intelligence (AI), encompassing both manual and digital methods of analysis. Additionally, studies needed to be published in English, with no restrictions on the publication date [26,28,29,30,31,32,33,34,35,36,37,38]. The authors of this review established the following exclusion criteria: studies written in languages other than English, comparisons solely between two orthodontists, clinical reports, opinions, editorial papers, review articles, and studies lacking a full-text version [26,28,29,30,31,32,33,34,35,36,37,38].
2.4. Information Sources, Search Strategy, and Study Selection
In January 2024, we conducted electronic searches in the PubMed, Scopus and Web of Science (WoS) databases. In the Scopus database, the results were refined to titles, abstracts and keywords, while in PubMed they were narrowed down to titles and abstracts. In WoS, the results were refined only to abstracts. The search criteria were based on the following keywords: (cephalometric) AND (analysis) AND (discrepancy) AND ((orthodontic) OR (radiologist)). All searches adhered to the established eligibility criteria, and only articles with available full-text versions were considered.
2.5. Data Collection and Data Items
Six researchers (K.W., J.K., N.S., K.N., J.K. and W.D.) meticulously curated the articles that met the predefined criteria. Subsequently, the pertinent data were gathered and recorded in a standardized Microsoft Excel 2013 (Microsoft, Redmond, WA, USA).
2.6. Assessing Risk of Bias in Individual Studies
In the initial phase of the study topic selection, the authors autonomously assessed the titles and abstracts of each paper to mitigate potential bias. The degree of consensus among researchers was evaluated using Cohen’s κ test. Any disparities regarding the inclusion or exclusion of a paper were resolved through collaborative discussions among the authors.
2.7. Quality Assessment
Two independent evaluators (J.M. and M.D.) assessed the procedural quality of each study included in the article. The assessment criteria focused on key aspects related to the methods of cephalometric analysis. The criteria for evaluating study design, implementation, and analysis included a minimum group size of 10 subjects, sample size calculation, presence of at least 5 landmarks, blinding, a minimum of triple measurements, and researchers’ experience. Studies were assigned scores ranging from 0 to 6 points, with higher scores indicating better study quality. The risk of bias was categorized as follows: 0–2 points denoted a high risk, 3–4 points denoted a moderate risk, and 5–6 points indicated a low risk. Any discrepancies in scoring were resolved through discussion until a consensus was reached [26,28,29,30,31,32,33,34,35,36,37,38].
3. Results
3.1. Study Selection
The initial database search across PubMed, Scopus, and WoS yielded 263 articles potentially relevant for the review. Following the removal of duplicates, 160 articles underwent screening. The initial screening of titles and abstracts resulted in the exclusion of 141 articles that did not involve a comparison of analysis between different specialists or AI/software. Subsequently, 19 articles underwent further full-text analysis, during which 2 articles were excluded for not meeting the inclusion criteria. Ultimately, a total of 17 articles were included in the qualitative synthesis of this review. The considerable heterogeneity among the included studies prevents the possibility of conducting a meta-analysis.
3.2. General Characteristics of the Included Studies
Selected studies compared the quality of cephalometric analysis performed by different specialists with varying levels of experience. The study conducted by Chen et al. [39] compared landmark detection and cephalometric analysis performed by an experienced specialist and a novice specialist. Similarly, Kuyl et al. [40] conducted a study comparing orthodontists, senior assistants, junior assistants, and non-orthodontist dentists. The results of both studies indicated that specialists with more experience demonstrated greater proficiency in performing cephalometric analysis. Furthermore, the accuracy of the analysis was found to be influenced by specialization, with orthodontists performing the analysis more thoroughly than non-orthodontist dentists. However, the level of orthodontists’ training did not impact the consistency of the measurements [39].
An alternative to the conventional method of cephalometric analysis involves the utilization of specialized software designed for this purpose. Among the included studies, eleven focused on comparing the accuracy of cephalometric analysis between clinicians and various software programs. The software programs used in these studies include CADCAS [41], CASS [42], PANN [43], PACS [44], Screenceph [45], Ceph X [46], Onyx Ceph (version 2.5.6.) [47], CephNinja (version 4.20) [48], and NemoCeph NX 2009 [49]. In a study conducted by Kumar M et al. [49], the last two software programs were compared with each other in terms of their accuracy. The majority of studies indicated that analysis performed by software was superior to traditional manually conducted analysis methods [39,42,43,45,46,50].
According to the authors of the included studies, the main benefits of using specialized software for cephalometric analysis are increased accuracy, reduced time, and minimized human error [39,43,46,50]. In their opinion, the use of cephalometric analysis systems makes it possible to reproduce intricate details and parameters that are essential for accurate diagnosis. For instance, the CASS software conducted an analysis on computed tomography, facilitating the recreation of Spee and Wilson curves [42]. However, certain studies did not identify significant differences between analysis conducted by software and that performed by a specialist [39,44,47,51]. Nonetheless, it is important to note that the selected software may not always serve as a flawless replacement. Errors can still occur despite a relatively well-conducted analysis. For instance, Zamrik et al. [52] demonstrated such a scenario in their study, where the measurement of the U1-A point was inaccurately performed. In terms of the efficacy of individual programs, a study by Kumar et al. [49] suggests that orthodontic analysis programs exhibit similar effectiveness.
The results of studies comparing artificial intelligence (AI) and traditional cephalometric analysis vary. Some authors highlight numerous advantages of AI, such as increased convenience, shorter analysis time, and high accuracy [48,53]. For instance, a study by Wang et al. [54] suggests that AI analysis demonstrates high precision, with deviations of up to 2 mm, and a detection rate of up to 80%. However, research conducted by Gupta et al. [55] did not find significant differences between traditional and AI-based analysis methods. This could be attributed to the fact that AI is still a relatively new tool in orthodontics and requires further refinement [53]. A general characteristic of the included studies has been demonstrated in Table 1.

Table 1.
General characteristics of studies.
3.3. Main Study Outcomes
Studies selected in this systematic review varied in their comparison of cephalometric analysis conducted through different methodologies. Among them, one study distinguished itself by comparing analyses between three specialists with varying levels of experience [40]. Additionally, eleven studies focused on comparing analyses performed by clinicians and software programs [39,41,42,43,44,45,46,47,50,51,52]. Another study compared two different software analysis methods [49], while four studies examined the comparison between analyses conducted by clinicians and artificial intelligence [53,54,55]. Furthermore, one study investigated a comparison between clinicians, software, and artificial intelligence [48]. The studies were not homogeneous in terms of the type of the analysis. Some of the studies focused only on landmarks identification [45,53,54] while the others investigated linear and angular analysis as well [39,40,41,42,43,44,46,47,48,49,50,51,52,55]. The detailed characteristics of the included studies are shown in Table 2.

Table 2.
Detailed characteristics of studies.
3.4. Quality Assessment
Among the articles included in the review, one [49] was rated as high-quality, achieving a score of 5/6 points. Seven studies [41,42,44,45,47,51,52] were categorized as low-quality. Furthermore, nine studies [39,40,43,46,48,50,53,54,55] were identified as having a moderate risk of bias, scoring between 3 points (see Table 3).

Table 3.
Quality assessment table.
4. Discussion
This review looks at studies relevant to comparing human cephalometric assessments with assessments enhanced by artificial intelligence-enhanced software [23]. Although traditional methods of cephalometric assessment have prevailed for years, the advent of modern tools has made it possible to automatically refine such records based on computation or artificial intelligence [24]. Nevertheless, the number of articles on the subject is small or their availability remains limited, which makes it necessary to postulate that further similar studies should be carried out as widely as possible. AI-enhanced software is already reported in some papers from general dentistry, focusing on its role on dental feelings, occlusion, prosthodontics and general conservative dentistry [56,57,58,59,60]. Each orthodontic treatment focuses on achieving a good, balanced and functioning occlusion to improve patients bite, chewing and overall quality of life. It seems that AI and 3D-CBCT can improve orthodontics and lead to better and more accurate patient outcomes from orthodontic treatments.
Currently, a comprehensive evaluation of the facial skeleton in conjunction with soft tissue proportions, skeletal features, teeth, and occlusion holds paramount importance in contemporary orthodontic treatment and orthognathic surgery protocols. Numerous advancements in orthodontic and orthognathic studies have been reported, as noted by Prasad et al. [61] and Starch-Jensen et al. [1]. The main findings suggest that new technologies in cephalometric assessment are the future, but significant efforts are needed to fully optimize their performance.
In the past, the process of measuring angles and distances on X-ray film, as well as transferring reference points on tracing paper, was a time-consuming one [3]. The time required to manually draw points and create lines on tracing paper, take measurements with a ruler and protractor, and finally record cephalometric measurements was approximately 30 min. The digitization of X-rays and the ability to trace reference points with a computer mouse on the monitor screen represented a significant advance. The capacity to magnify individual structures on the monitor screen while marking successive reference points, coupled with the ongoing enhancement of digital cephalograms, has markedly enhanced the precision of measurements. Concurrently, the time required for the analysis using computer programs, which automatically count the individual parameters of the cephalometric analyses and place the results in tables and graphs after the doctor has entered the points, has decreased to approximately one to two minutes. It is crucial to recognize the benefits of new technologies and software that can enhance the work of dentists, particularly orthodontists. Over the past decade, advancements in virtual reality techniques, computer-enhanced technologies, cone-beam computed tomography (CBCT), and many others have significantly improved overall dental treatment. Today, 3D cephalometric measurements, 3D virtual treatment planning for skeletal, facial, jaw/bone, and teeth measurements, along with detailed 3D studies of superficial, skeletal, and skin anatomy, appear to greatly enhance success rates and reduce the occurrence of troublesome complications or limitations in treatment algorithms [62,63,64,65,66]. Despite the advancements and improvements in new techniques, it is always important to consider the potential for human and computer errors. Therefore, after each evaluation, it is crucial to double-check the results and ensure that the proposed treatment or diagnostic algorithm is sufficient and adequate for each patient’s case.
Some computer programs employ artificial intelligence to perform tasks previously reserved for medical professionals, such as identifying and marking reference points [67]. Nevertheless, the creators of these programs consistently advise medical professionals to verify that the program has correctly identified the relevant points. This is due to the fact that some bone and skin structures that overlap in an X-ray image may be misinterpreted by the computer program. Furthermore, the difficulty of computer programs in reading visual material is a common feature used to detect malicious bots employing CAPTCHA techniques.
The most illustrative example of this type of difficulty in orthodontic practice is the determination of Downs’ A-point [68]. In such instances, the bony structure may be erroneously identified as the shadow of the buccal fat pad. An erroneous determination of this point will result in a significant error in the diagnosis of the sagittal position of the maxilla in relation to the mandible, as evidenced by incorrect ANB and WITS parameters. It can be concluded that the reduction in time for the application of reference points achieved by the automatic procedure is a minor advantage, since at most two minutes of analysis time are saved. However, this does not guarantee the correctness of the diagnosis, especially in difficult cases. It is crucial to emphasize that orthodontic diagnosis is not solely dependent on the speed of the process.
In turn, other factors, such as patient positioning, maintaining a good NHP, and ensuring appropriate resting positions of the jaw, teeth, facial features, skull, and body posture during examination, are areas that still warrant attention [1,61]. The most critical aspect of evaluating facial photographs, CBCT scans, and 3D assessments lies in achieving a natural, physiologically balanced head position and patient silhouette. Many authors seem to align with this perspective [12,69]. Consequently, the utilization of craniometric studies in anatomical and radiological tracings can be more dependable. When the patient’s head position is secured in the most reliable manner, further cephalometric analysis can be conducted [68]. In the past, such patient positioning for evaluations was pivotal in ensuring the most accurate and precise placement of craniometric and anthropometric points within the assessed data. In today’s context, this scenario still holds significant importance. Even though automatic tracing software can identify precise anatomical landmarks, the accuracy of proportions, angles, and correlations between points may be compromised due to head positioning in the NHP (natural head position). Whether utilizing manual or automatic/computer-enhanced tracing methods, as well as AI software, the NHP and patient posture during the examination are crucial factors. Both the experience and expertise of clinicians, as well as the proficiency and knowledge of younger clinicians, can greatly influence cephalometric tracings and their accuracy [13]. While manual tracings rely on the clinician’s experience and knowledge to utilize craniometric reference points, automatic or AI-driven software evaluates images based on algorithms or other automated tools. It seems, however, that the issue of correct patient positioning remains outside the area that can be optimized with computer programs.
Regardless of the method used, the most crucial factor is to establish the most accurate, comprehensive, and sufficient analysis for each patient’s case. The precise placement of anatomical cephalometric landmarks to enhance the linear, angular, and planar comparison of selected landmarks is pivotal for planning both orthodontic and orthognathic surgery procedures [20]. Numerous authors, such as Chen et al. [23], Kuyl et al. [40] and others, have studied the skill of placing anatomical and cephalometric points and concluded that a skilled specialist with more years of active clinical practice demonstrates greater proficiency in accurately placing the necessary reference points for conducting a precise cephalometric analysis [19]. Furthermore, it is important to note that clinicians, dentists, surgeons, and orthodontists who perform such analyses routinely possess more experience compared to those who perform them sporadically or infrequently.
With the advancements in 3D software and the computer-enhanced evaluation of radiographs, CBCT studies, and facial photographs, new techniques used in both orthodontics and orthognathic surgery are being widely embraced for their rapid and precise analysis. Similar studies conducted by Chen et al. [39], Baker et al. [42], Mario et al. [43], Turner et al. [45], Mosley et al. [46], and Tsorovas et al. [50], among others, tend to corroborate these findings. Today’s software aims not only for precise and accurate measurements but also to mitigate any potential human errors or inaccuracies in craniometric evaluation [1,61]. From the author’s perspective, this situation is quite evident, but when patients’ head positioning in NHP during radiographs, facial photographs, and CBCT evaluation is misaligned, even with numerous new devices and software, the results may not be accurate. This situation holds particular importance in planning surgical interventions, such as in orthognathic surgery, where establishing the full scope of the soft and hard tissue contour and balance is imperative without any disruptions. When this criterion is not met, numerous disturbances in measurements are observed, irrespective of the computed-enhanced/AI or classic manual evaluation methods utilized in various studies. This aspect is considered one of the most crucial parts of each cephalometric evaluation and has been well-documented [19,20,70]. From the author’s perspective, regardless of the anthropometric reference points and techniques used, some cases of severe skeletal malocclusion surpass the capabilities of standard planning methods, necessitating a combined manual-approach and 3D/AI-driven software.
The discussion regarding the comparison between manual classic cephalometric evaluation and those conducted by AI-computed assisted software is steadily gaining traction in the existing literature. Both methods possess their respective advantages and disadvantages, and it is particularly noteworthy that some very complex and challenging cases still require traditional manual hand-made evaluation, cephalometric measurements, and estimation. Presently, the rapidly expanding integration of AI and computed CBCT evaluation holds promise for the future of next-generation orthodontic and orthognathic surgery treatments. However, there is still much work to be carried out, primarily because further improvements are necessary [6]. The most significant clinical observation is that contemporary orthognathic surgery relies heavily on 3D-CBCT patient evaluation, complemented by facial, bite, and occlusal photographs, which are integrated and amalgamated to estimate, measure, and predict the most effective treatment plan for each patient case. Without the aid of new technologies, such as CBCT and AI-automatic software tracings, achieving this level of precision would not be feasible. However, it is important to note that a few exceptionally complex cases of severe skeletal malocclusion may still necessitate manual-based evaluations, particularly those associated with significant skeletal jawbone disproportions and similar factors [71,72]. While the key conclusions drawn by the authors align partially with those of other relevant papers, it is crucial to acknowledge the variability in results across different studies, attributable to the diverse capabilities and resources of each tool and software program for cephalometric tracings.
The following limitations were encountered during the study: an insufficient number of papers comparing natural head position (NHP) and the usage of AI-driven software, leading to gaps in understanding; significant variability in the software and computer-enhanced programs utilized, along with their 3D/measurement capabilities, complicating comparisons and standardization; a limited number of studies on patients discussing and describing the preparation, positioning, and evaluation process before and during the study, which hinders reproducibility and generalizability; diverse cephalometric measurements utilized across various orthodontic protocols, making it challenging to establish consensus and comparability; limitations in the size, resolution, and accuracy of CBCT scans, traditional radiographs, scanners, and software utilized, affecting the quality and reliability of the data; and a plethora of radiographic software, programs, and companies involved in the dental market, contributing to heterogeneity and potential inconsistencies in methodologies and results. Significant heterogeneity among the included studies does not allow for performing a meta-analysis. However, further research should be conducted to enable proceeding with a meta-analysis.
5. Conclusions
The studies examined comparisons between specialists of varying experience levels, clinicians, software programs, and artificial intelligence (AI). In general, specialists with more experience demonstrated greater proficiency in cephalometric analysis. However, the accuracy of the analysis was influenced by specialization. The utilization of specialized software for cephalometric analysis demonstrated numerous advantages, including enhanced precision, reduced time requirements, and the minimization of human errors. Such errors may be caused by intra- and interobserver variations, or by operator fatigue. While some studies have indicated that software-based analysis is superior to traditional methods, others have not identified any significant differences. The efficacy of AI-based analysis was found to vary across studies. Some studies highlighted the advantages of AI-based analysis in terms of convenience, shorter analysis time, and high accuracy. However, other studies found no significant differences between AI-based analysis and traditional methods. It is, however, important to note that AI in orthodontics is still in a state of evolution and requires further refinement. There are still challenges that need to be addressed, including variations in software and methodologies, limitations in patient positioning protocols, and diverse cephalometric measurement standards across studies. This may indicate that optimization using new software and artificial intelligence is not feasible in all areas. Conversely, the benefits of automated referencing, such as reduced analysis time, are in fact minimal, as the advantage of automated referencing over human referencing is less than two minutes. While AI-driven enhancements offer potential for the future, manual evaluations remain necessary for complex cases. Further research is required to address these limitations and to optimize the incorporation of technology in orthodontic and orthognathic surgery practices.
Author Contributions
Conceptualization, P.S., J.M. and M.D.; methodology, P.S. and J.M.; software, P.S.; validation, P.S. and J.M.; formal analysis, P.S.; investigation, K.N., J.K. (Jan Kiryk), J.K. (Julia Kensy), N.S., K.W., S.K. and W.D.; resources, J.M., P.S. and J.K. (Jan Kiryk); data curation, J.M. and M.D.; writing—original draft preparation, P.S., K.N., J.K. (Jan Kiryk), J.K. (Julia Kensy), N.S., K.W., S.K. and W.D. writing—review and editing, M.D. and J.M.; visualization, J.K. (Jan Kiryk); supervision, P.S., M.D. and J.M.; project administration, J.M. and M.D.; funding acquisition, J.M. and M.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by a subsidy from Wroclaw Medical University, number SUBZ.B180.24.058.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Starch-Jensen, T.; Hernández-Alfaro, F.; Kesmez, Ö.; Gorgis, R.; Valls-Ontañón, A. Accuracy of Orthognathic Surgical Planning Using Three-Dimensional Virtual Techniques Compared with Conventional Two-Dimensional Techniques: A Systematic Review. J. Oral Maxillofac. Res. 2023, 14, 14101. [Google Scholar] [CrossRef] [PubMed]
- Alkhayer, A.; Piffkó, J.; Lippold, C.; Segatto, E. Accuracy of Virtual Planning in Orthognathic Surgery: A Systematic Review. Head Face Med. 2020, 16, 34. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Shanavas, M.; Sidappa, A.; Kiran, M. Cone Beam Computed Tomography—Know Its Secrets. J. Int. Oral Health 2015, 7, 64. [Google Scholar] [PubMed]
- Chien, P.C.; Parks, E.T.; Eraso, F.; Hartsfield, J.K.; Roberts, W.E.; Ofner, S. Comparison of Reliability in Anatomical Landmark Identification Using Two-Dimensional Digital Cephalometrics and Three-Dimensional Cone Beam Computed Tomography in Vivo. Dentomaxillofacial Radiol. 2014, 38, 262–273. [Google Scholar] [CrossRef] [PubMed]
- Hariharan, A.; Diwakar, N.R.; Jayanthi, K.; Hema, H.M.; Deepukrishna, S.; Ghaste, S.R. The Reliability of Cephalometric Measurements in Oral and Maxillofacial Imaging: Cone Beam Computed Tomography versus Two-Dimensional Digital Cephalograms. Indian J. Dent. Res. 2016, 27, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Teixeira, H.; Tanna, N.; Zheng, Z.; Chen, S.H.Y.; Zou, M.; Chung, C.H. The Reliability of Two- and Three-Dimensional Cephalometric Measurements: A CBCT Study. Diagnostics 2021, 11, 2292. [Google Scholar] [CrossRef] [PubMed]
- Gkantidis, N.; Opacic, J.; Kanavakis, G.; Katsaros, C.; Halazonetis, D. Facial Asymmetry and Midsagittal Plane Definition in 3D: A Bias-Free, Automated Method. PLoS ONE 2023, 18, e0294528. [Google Scholar] [CrossRef]
- Dobai, A.; Markella, Z.; Vízkelety, T.; Fouquet, C.; Rosta, A.; Barabás, J. Landmark-Based Midsagittal Plane Analysis in Patients with Facial Symmetry and Asymmetry Based on Cbct Analysis Tomography. J. Orofac. Orthop. 2018, 79, 371. [Google Scholar] [CrossRef] [PubMed]
- Damstra, J.; Fourie, Z.; De Wit, M.; Ren, Y. A Three-Dimensional Comparison of a Morphometric and Conventional Cephalometric Midsagittal Planes for Craniofacial Asymmetry. Clin. Oral Investig. 2012, 16, 285–294. [Google Scholar] [CrossRef]
- Wang, Y.; Wu, W.; Christelle, M.; Sun, M.; Wen, Z.; Lin, Y.; Zhang, H.; Xu, J. Automated Localization of Mandibular Landmarks in the Construction of Mandibular Median Sagittal Plane. Eur. J. Med. Res. 2024, 29, 84. [Google Scholar] [CrossRef]
- Lin, Y.H.; Yao, C.F.; Chen, Y.A.; Liao, Y.F.; Chen, Y.R. Three-Dimensional Positioning of the Maxilla Using Novel Intermediate Splints in Maxilla-First Orthognathic Surgery for Correction of Skeletal Class III Deformity. Clin. Oral Investig. 2024, 28, 141. [Google Scholar] [CrossRef]
- Lin, L.O.; Kalmar, C.L.; Vu, G.H.; Zimmerman, C.E.; Humphries, L.S.; Swanson, J.W.; Bartlett, S.P.; Taylor, J.A. Value-Based Analysis of Virtual Versus Traditional Surgical Planning for Orthognathic Surgery. J. Craniofacial Surg. 2020, 31, 1238–1242. [Google Scholar] [CrossRef] [PubMed]
- Antonini, F.; Borba, A.M.; Pagnoncelli, R.M.; Han, M.; Markiewicz, M.R.; Miloro, M. Does a Learning Curve Exist for Accuracy in Three-Dimensional Planning for Maxillary Positioning in Bimaxillary Orthognathic Surgery? Int. J. Oral Maxillofac. Surg. 2020, 49, 787–793. [Google Scholar] [CrossRef] [PubMed]
- Frongia, G.; Piancino, M.G.; Bracco, A.A.; Crincoli, V.; Debernardi, C.L.; Bracco, P. Assessment of the Reliability and Repeatability of Landmarks Using 3-D Cephalometric Software. Cranio® 2012, 30, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Sam, A.; Currie, K.; Oh, H.; Flores-Mir, C.; Lagravére-Vich, M. Reliability of Different Three-Dimensional Cephalometric Landmarks in Cone-Beam Computed Tomography: A Systematic Review. Angle Orthod. 2019, 89, 317–332. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.K.; Alftaikhah, S.A.A.; Issrani, R.; Ronsivalle, V.; Lo Giudice, A.; Cicciù, M.; Minervini, G. Applications of Artificial Intelligence in the Utilisation of Imaging Modalities in Dentistry: A Systematic Review and Meta-Analysis of in-Vitro Studies. Heliyon 2024, 10, e24221. [Google Scholar] [CrossRef] [PubMed]
- Miryala, A.G.; Miryala, G.; Khan, Y.; Ramalingam, N.T.; Sevugaperumal, B.; Soman, M.; Padmanabhan, A. Revolutionizing Dental Imaging: A Comprehensive Study on the Integration of Artificial Intelligence in Dental and Maxillofacial Radiology. Cureus 2023, 15, e50292. [Google Scholar] [CrossRef] [PubMed]
- Tabatabaian, F.; Vora, S.R.; Mirabbasi, S. Applications, Functions, and Accuracy of Artificial Intelligence in Restorative Dentistry: A Literature Review. J. Esthet. Restor. Dent. 2023, 35, 842–859. [Google Scholar] [CrossRef] [PubMed]
- Akhare, P.J.; Dagab, A.M.; Alle, R.S.; Shenoyd, U.; Garla, V. Comparison of Landmark Identification and Linear and Angular Measurements in Conventional and Digital Cephalometry. Int. J. Comput. Dent. 2013, 16, 241–254. [Google Scholar]
- Giannopoulou, M.A.; Kondylidou-Sidira, A.C.; Papadopoulos, M.A.; Athanasiou, A.E. Are Orthodontic Landmarks and Variables in Digital Cephalometric Radiography Taken in Fixed and Natural Head Positions Reliable? Int. Orthod. 2020, 18, 54–68. [Google Scholar] [CrossRef]
- Wilkat, M.; Liu, S.; Schwerter, M.; Schrader, F.; Saigo, L.; Karnatz, N.; Kübler, N.R.; Rana, M. A New Approach to Virtual Occlusion in Orthognathic Surgery Planning Using Mixed Reality—A Technical Note and Review of the Literature. J. Pers. Med. 2023, 13, 1709. [Google Scholar] [CrossRef] [PubMed]
- Zammit, D.; Ettinger, R.E.; Sanati-Mehrizy, P.; Susarla, S.M. Current Trends in Orthognathic Surgery. Medicina 2023, 59, 2100. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Mo, S.; Fan, X.; You, Y.; Ye, G.; Zhou, N. A Meta-Analysis and Systematic Review Comparing the Effectiveness of Traditional and Virtual Surgical Planning for Orthognathic Surgery: Based on Randomized Clinical Trials. J. Oral Maxillofac. Surg. 2021, 79, 471.e1–471.e19. [Google Scholar] [CrossRef] [PubMed]
- Bansal, N.; Singla, J.; Gera, G.; Gupta, M.; Kaur, G. Reliability of Natural Head Position in Orthodontic Diagnosis: A Cephalometric Study. Contemp. Clin. Dent. 2012, 3, 180–183. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira Lisboa, C.; Masterson, D.; da Motta, A.F.J.; Motta, A.T. Reliability and Reproducibility of Three-Dimensional Cephalometric Landmarks Using CBCT: A Systematic Review. J. Appl. Oral Sci. 2015, 23, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Lin, J.; Demner-Fushman, D. Evaluation of PICO as a Knowledge Representation for Clinical Questions. AMIA Annu. Symp. Proc. 2006, 2006, 359. [Google Scholar] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Homa, K.; Zakrzewski, W.; Dobrzyński, W.; Piszko, P.J.; Piszko, A.; Matys, J.; Wiglusz, R.J.; Dobrzyński, M. Surface Functionalization of Titanium-Based Implants with a Nanohydroxyapatite Layer and Its Impact on Osteoblasts: A Systematic Review. J. Funct. Biomater. 2024, 15, 45. [Google Scholar] [CrossRef]
- Piszko, P.J.; Piszko, A.; Kiryk, J.; Lubojański, A.; Dobrzyński, W.; Wiglusz, R.J.; Matys, J.; Dobrzyński, M. The Influence of Fluoride Gels on the Physicochemical Properties of Tooth Tissues and Dental Materials—A Systematic Review. Gels 2024, 10, 98. [Google Scholar] [CrossRef]
- Murias, I.; Grzech-Leśniak, K.; Murias, A.; Walicka-Cupryś, K.; Dominiak, M.; Deeb, J.G.; Matys, J. Efficacy of Various Laser Wavelengths in the Surgical Treatment of Ankyloglossia: A Systematic Review. Life 2022, 12, 558. [Google Scholar] [CrossRef]
- Kowalski, J.; Rygas, J.; Homa, K.; Dobrzyński, W.; Wiglusz, R.J.; Matys, J.; Dobrzyński, M. Antibacterial Activity of Endodontic Gutta-Percha—A Systematic Review. Appl. Sci. 2023, 14, 388. [Google Scholar] [CrossRef]
- Struzik, N.; Wiśniewska, K.; Piszko, P.J.; Piszko, A.; Kiryk, J.; Matys, J.; Dobrzyński, M. SEM Studies Assessing the Efficacy of Laser Treatment for Primary Teeth: A Systematic Review. Appl. Sci. 2024, 14, 1107. [Google Scholar] [CrossRef]
- Matys, J.; Kensy, J.; Gedrange, T.; Zawiślak, I.; Grzech-Leśniak, K.; Dobrzyński, M. A Molecular Approach for Detecting Bacteria and Fungi in Healthcare Environment Aerosols: A Systematic Review. Int. J. Mol. Sci. 2024, 25, 4154. [Google Scholar] [CrossRef] [PubMed]
- Kensy, J.; Dobrzyński, M.; Wiench, R.; Grzech-Leśniak, K.; Matys, J. Fibroblasts Adhesion to Laser-Modified Titanium Surfaces—A Systematic Review. Materials 2021, 14, 7305. [Google Scholar] [CrossRef] [PubMed]
- Rajewska, J.; Kowalski, J.; Matys, J.; Dobrzyński, M.; Wiglusz, R.J. The Use of Lactide Polymers in Bone Tissue Regeneration in Dentistry—A Systematic Review. J. Funct. Biomater. 2023, 14, 83. [Google Scholar] [CrossRef] [PubMed]
- Rygas, J.; Matys, J.; Wawrzyńska, M.; Szymonowicz, M.; Dobrzyński, M. The Use of Graphene Oxide in Orthodontics—A Systematic Review. J. Funct. Biomater. 2023, 14, 500. [Google Scholar] [CrossRef]
- Wiench, R.; Skaba, D.; Matys, J.; Grzech-Leśniak, K. Efficacy of Toluidine Blue—Mediated Antimicrobial Photodynamic Therapy on Candida Spp. A Systematic Review. Antibiotics 2021, 10, 349. [Google Scholar] [CrossRef]
- Woźniak, A.; Matys, J.; Grzech-Leśniak, K. Effectiveness of Lasers and APDT in Elimination of Intraoral Halitosis: A Systematic Review Based on Clinical Trials. Lasers Med. Sci. 2022, 37, 3403–3411. [Google Scholar] [CrossRef]
- Chen, S.-K.; Chen, Y.-J.; Yao, C.-C.J.; Chang, H.-F. Enhanced Speed and Precision of Measurement in a Computer-Assisted Digital Cephalometric Analysis System. Angle Orthod. 2004, 74, 501–507. [Google Scholar]
- Kuyl, M.H.; Verbeeck, R.M.H.; Dermaut, L.R. The Integumental Profile: A Reflection of the Underlying Skeletal Configuration? Am. J. Orthod. Dentofac. Orthop. 1994, 106, 597–604. [Google Scholar] [CrossRef]
- Chen, Y.-J.; Chen, S.-K.; Yao, C.-C.J.; Chang, H.-F. The Effects of Differences in Landmark Identification on the Cephalometric Measurements in Traditional Versus Digitized Cephalometry. Angle Orthod. 2004, 74, 155–161. [Google Scholar] [PubMed]
- Baker, S.B.; Goldstein, J.A.; Seruya, M. Outcomes in Computer-Assisted Surgical Simulation for Orthognathic Surgery. J. Craniofacial Surg. 2012, 23, 509–513. [Google Scholar] [CrossRef] [PubMed]
- Mario, M.C.; Abe, J.M.; Ortega, N.R.S.; Del Santo, M. Paraconsistent Artificial Neural Network as Auxiliary in Cephalometric Diagnosis. Artif. Organs 2010, 34, E215–E221. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Davies, T.I. A Comparison of Cephalometric Measurements: A Picture Archiving and Communication System versus the Hand-Tracing Method-a Preliminary Study. Eur. J. Orthod. 2011, 33, 350–353. [Google Scholar] [CrossRef] [PubMed]
- Turner, P.J.; Weerakone, S. An Evaluation of the Reproducibility of Landmark Identification Using Scanned Cephalometric Images. J. Orthod. 2001, 28, 221–230. [Google Scholar] [CrossRef]
- Mosleh, M.A.A.; Baba, M.S.; Malek, S.; Almaktari, R.A. Ceph-X: Development and Evaluation of 2D Cephalometric System. BMC Bioinform. 2016, 17, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Swennen, G.R.J.; Grimaldi, H.; Berten, J.-L.; Kramer, F.-J.; Dempf, R.; Schwestka-Polly, R.; Hausamen, J.-E. Reliability and Validity of a Modified Lateral Cephalometric Analysis for Evaluation of Craniofacial Morphology and Growth in Patients with Clefts. J. Craniofacial Surg. 2004, 15, 399–412. [Google Scholar] [CrossRef] [PubMed]
- Kılınç, D.D.; Kırcelli, B.H.; Sadry, S.; Karaman, A. Evaluation and Comparison of Smartphone Application Tracing, Web Based Artificial Intelligence Tracing and Conventional Hand Tracing Methods. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, e906–e915. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Kumari, S.; Chandna, A.; Konark; Singh, A.; Kumar, H.; Punita. Comparative Evaluation of CephNinja for Android and NemoCeph for Computer for Cephalometric Analysis: A Study to Evaluate the Diagnostic Performance of CephNinja for Cephalometric Analysis. J. Int. Soc. Prev. Community Dent. 2020, 10, 286–291. [Google Scholar] [CrossRef]
- Tsorovas, G.; Linder-Aronson Karsten, A. A Comparison of Hand-Tracing and Cephalometric Analysis Computer Programs with and without Advanced Features—Accuracy and Time Demands. Eur. J. Orthod. 2010, 32, 721–728. [Google Scholar] [CrossRef]
- Bruntz, L.Q.; Palomo, J.M.; Baden, S.; Hans, M.G. A Comparison of Scanned Lateral Cephalograms with Corresponding Original Radiographs. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 340–348. [Google Scholar] [CrossRef]
- Zamrik, O.M.; Iseri, H. The Reliability and Reproducibility of an Android Cephalometric Smartphone Application in Comparison with the Conventional Method. Angle Orthod. 2021, 91, 236–242. [Google Scholar] [CrossRef]
- Dot, G.; Schouman, T.; Chang, S.; Rafflenbeul, F.; Kerbrat, A.; Rouch, P.; Gajny, L. Automatic Three-Dimensional Cephalometric Landmarking via Deep Learning. J. Dent. Res. 2022, 101, 1380–1387. [Google Scholar] [CrossRef]
- Wang, C.W.; Huang, C.T.; Hsieh, M.C.; Li, C.H.; Chang, S.W.; Li, W.C.; Vandaele, R.; Marée, R.; Jodogne, S.; Geurts, P.; et al. Evaluation and Comparison of Anatomical Landmark Detection Methods for Cephalometric X-ray Images: A Grand Challenge. IEEE Trans. Med. Imaging 2015, 34, 1890–1900. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Kharbanda, O.P.; Sardana, V.; Balachandran, R.; Sardana, H.K. Accuracy of 3D Cephalometric Measurements Based on an Automatic Knowledge-Based Landmark Detection Algorithm. Int. J. Comput. Assist. Radiol. Surg. 2016, 11, 1297–1309. [Google Scholar] [CrossRef]
- Mörch, C.M.; Atsu, S.; Cai, W.; Li, X.; Madathil, S.A.; Liu, X.; Mai, V.; Tamimi, F.; Dilhac, M.A.; Ducret, M. Artificial Intelligence and Ethics in Dentistry: A Scoping Review. J. Dent. Res. 2021, 100, 1452–1460. [Google Scholar] [CrossRef]
- Revilla-León, M.; Gómez-Polo, M.; Vyas, S.; Barmak, A.B.; Özcan, M.; Att, W.; Krishnamurthy, V.R. Artificial Intelligence Applications in Restorative Dentistry: A Systematic Review. J. Prosthet. Dent. 2022, 128, 867–875. [Google Scholar] [CrossRef]
- Shetty, S.; Gali, S.; Augustine, D.; Sowmya, S.V. Artificial Intelligence Systems in Dental Shade-Matching: A Systematic Review. J. Prosthodont. 2023, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Gómez-Polo, M.; Vyas, S.; Barmak, A.B.; Gallucci, G.O.; Att, W.; Özcan, M.; Krishnamurthy, V.R. Artificial Intelligence Models for Tooth-Supported Fixed and Removable Prosthodontics: A Systematic Review. J. Prosthet. Dent. 2023, 129, 276–292. [Google Scholar] [CrossRef]
- Ahmed, N.; Abbasi, M.S.; Zuberi, F.; Qamar, W.; Halim, M.S.B.; Maqsood, A.; Alam, M.K. Artificial Intelligence Techniques: Analysis, Application, and Outcome in Dentistry—A Systematic Review. Biomed. Res. Int. 2021, 2021, 9751564. [Google Scholar] [CrossRef]
- Prasad, S.; Arunachalam, S.; Boillat, T.; Ghoneima, A.; Gandedkar, N.; Diar-Bakirly, S. Wearable Orofacial Technology and Orthodontics. Dent. J. 2023, 11, 24. [Google Scholar] [CrossRef] [PubMed]
- Perrotti, G.; Baccaglione, G.; Clauser, T.; Testarelli, L.; Fabbro, M.D.; Testori, T. Total Face Approach (TFA): A Novel 3D Approach to Describe the Main Cephalometric Craniomaxillofacial Parameters. Methods Protoc. 2021, 4, 15. [Google Scholar] [CrossRef] [PubMed]
- Gateno, J.; Xia, J.J.; Teichgraeber, J.F. New 3-Dimensional Cephalometric Analysis for Orthognathic Surgery. J. Oral Maxillofac. Surg. 2011, 69, 606–622. [Google Scholar] [CrossRef] [PubMed]
- Thawri, S.R.; Paul, P.; Reche, A.; Rathi, H.P. 3D Technology Used for Precision in Orthodontics. Cureus 2023, 15, e47170. [Google Scholar] [CrossRef] [PubMed]
- Castillo, J.C.; Gianneschi, G.; Azer, D.; Manosudprasit, A.; Haghi, A.; Bansal, N.; Allareddy, V.; Masoud, M.I. The Relationship between 3D Dentofacial Photogrammetry Measurements and Traditional Cephalometric Measurements. Angle Orthod. 2019, 89, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Serafin, M.; Baldini, B.; Cabitza, F.; Carrafiello, G.; Baselli, G.; Del Fabbro, M.; Sforza, C.; Caprioglio, A.; Tartaglia, G.M. Accuracy of Automated 3D Cephalometric Landmarks by Deep Learning Algorithms: Systematic Review and Meta-Analysis. Radiol. Medica 2023, 128, 544–555. [Google Scholar] [CrossRef]
- Winkler-Schwartz, A.; Bissonnette, V.; Mirchi, N.; Ponnudurai, N.; Yilmaz, R.; Ledwos, N.; Siyar, S.; Azarnoush, H.; Karlik, B.; Del Maestro, R.F. Artificial Intelligence in Medical Education: Best Practices Using Machine Learning to Assess Surgical Expertise in Virtual Reality Simulation. J. Surg. Educ. 2019, 76, 1681–1690. [Google Scholar] [CrossRef] [PubMed]
- Malkoc, S.; Sari, Z.; Usumez, S.; Koyuturk, A.E. The Effect of Head Rotation on Cephalometric Radiographs. Eur. J. Orthod. 2005, 27, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Alkaabi, S.; Maningky, M.; Helder, M.N.; Alsabri, G. Virtual and Traditional Surgical Planning in Orthognathic Surgery—Systematic Review and Meta-Analysis. Br. J. Oral Maxillofac. Surg. 2022, 60, 1184–1191. [Google Scholar] [CrossRef]
- Weingart, J.V.; Schlager, S.; Metzger, M.C.; Brandenburg, L.S.; Hein, A.; Schmelzeisen, R.; Bamberg, F.; Kim, S.; Kellner, E.; Reisert, M.; et al. Automated Detection of Cephalometric Landmarks Using Deep Neural Patchworks. Dentomaxillofacial Radiol. 2023, 52, 7280319. [Google Scholar] [CrossRef]
- Pittayapat, P.; Bornstein, M.M.; Imada, T.S.N.; Coucke, W.; Lambrichts, I.; Jacobs, R. Accuracy of Linear Measurements Using Three Imaging Modalities: Two Lateral Cephalograms and One 3D Model from CBCT Data. Eur. J. Orthod. 2015, 37, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Pittayapat, P.; Limchaichana-Bolstad, N.; Willems, G.; Jacobs, R. Three-Dimensional Cephalometric Analysis in Orthodontics: A Systematic Review. Orthod. Craniofacial Res. 2014, 17, 69–91. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).