Nuclear Medicine Radiological Hot Laboratory Simulation: A Mixed-Method Intervention Study on Immersive Virtual Reality for Sustainable Education
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Objectives
- Understand the safety requirements for entering the radiopharmaceutical preparation laboratory (hot lab) and protection from radiation hazards.
- Gain competency in the simulated preparation of 99mTc-MDP.
- Gain competency in quality control of 99mTc-MDP.
- Understand health and safety legislation requirements.
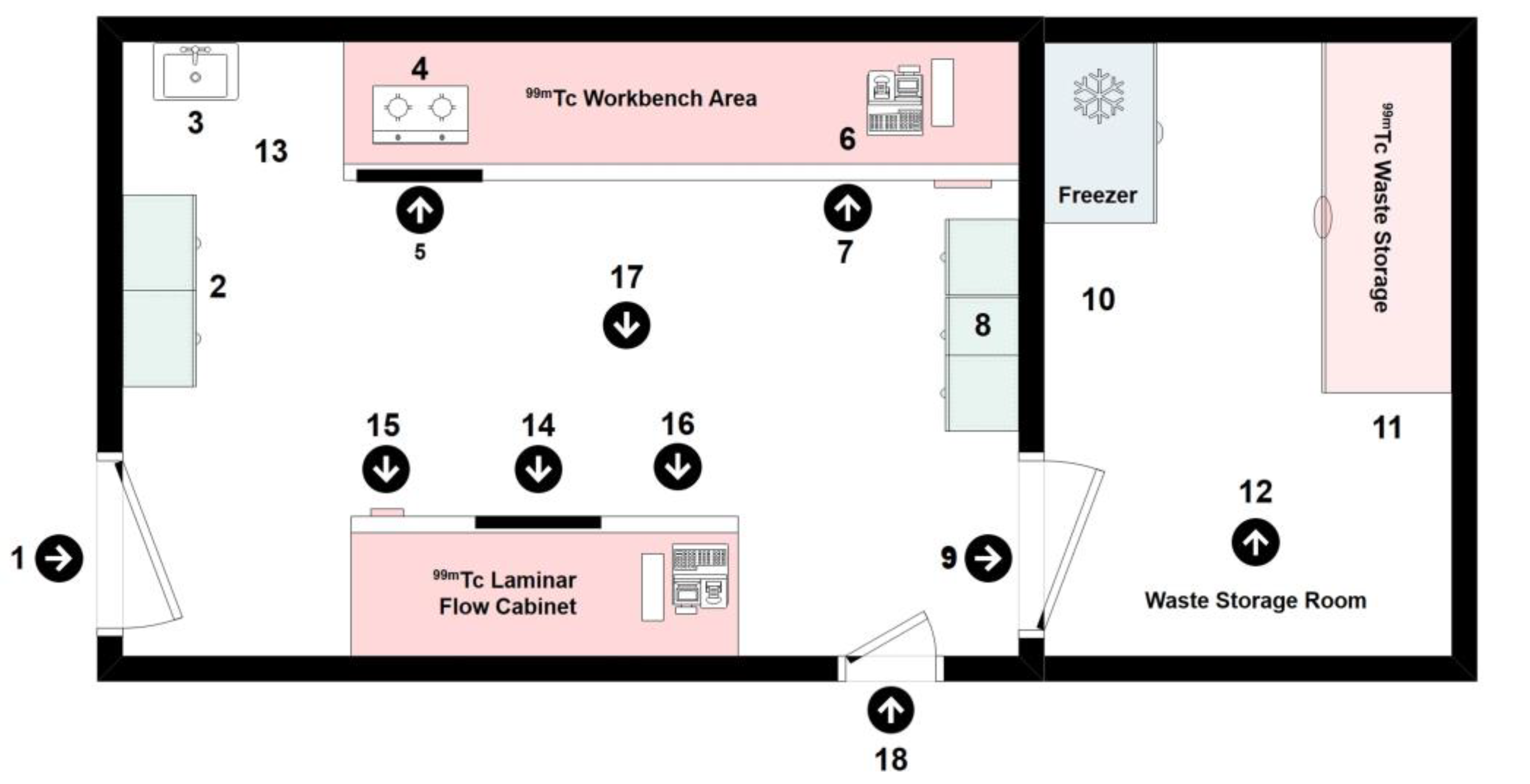
2.2. Study Location
- Radiopharmaceutical Preparation Laboratory (hot lab), Department of Radiology, Faculty of Medicine, Prince of Songkla University, Thailand.
- Laboratory 1 and 2, Radiological Technology Program, Department of Radiology, Faculty of Medicine, Prince of Songkla University, Thailand.
2.3. Quantitative Study: Study Design and Participants
2.4. Ethical Considerations
2.5. Hot Lab: Assessment of Radiation Dose in Nuclear Medicine Controlled Areas during Preparation and Handling of 99mTc-MDP Radiopharmaceutical
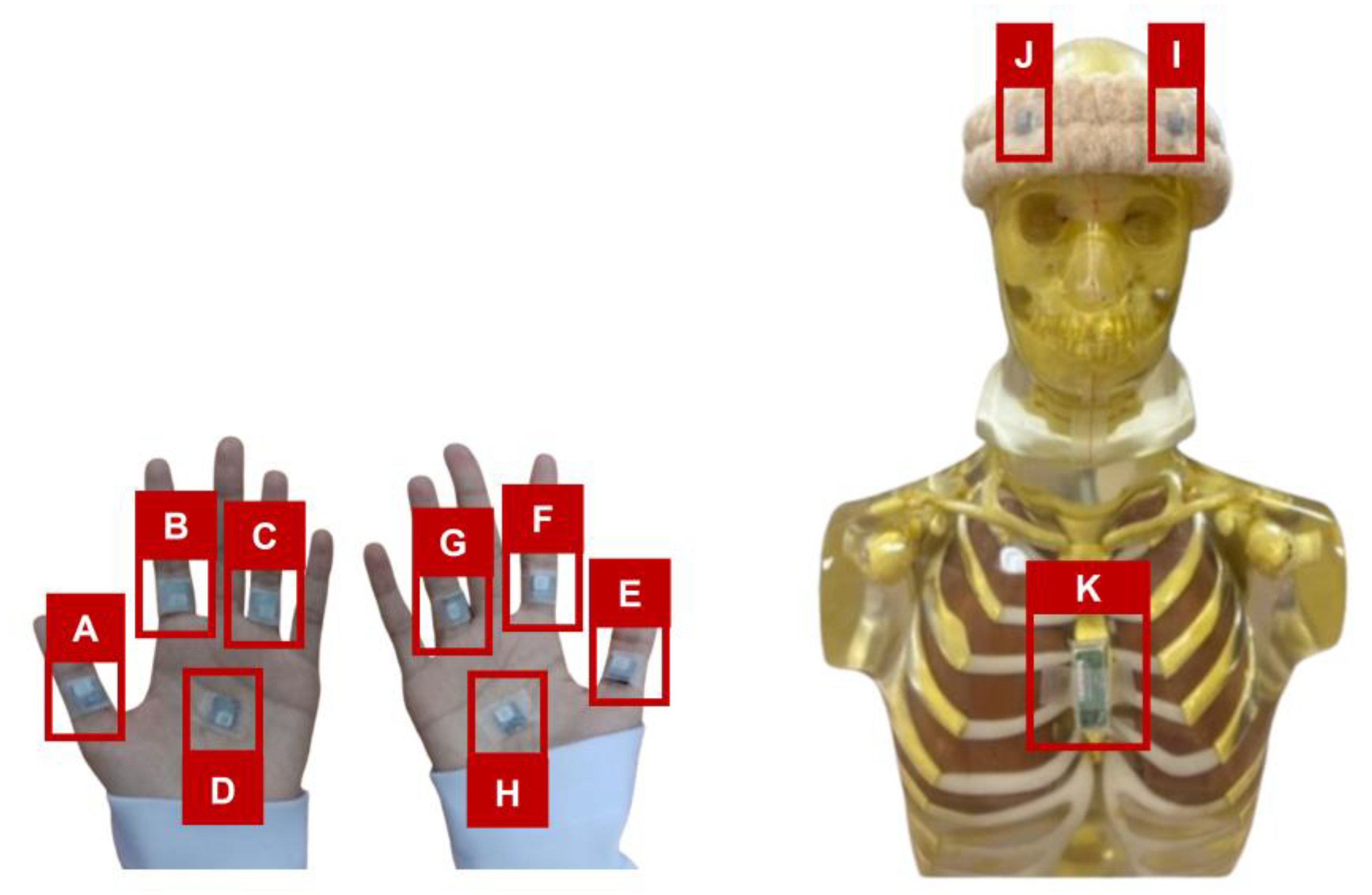
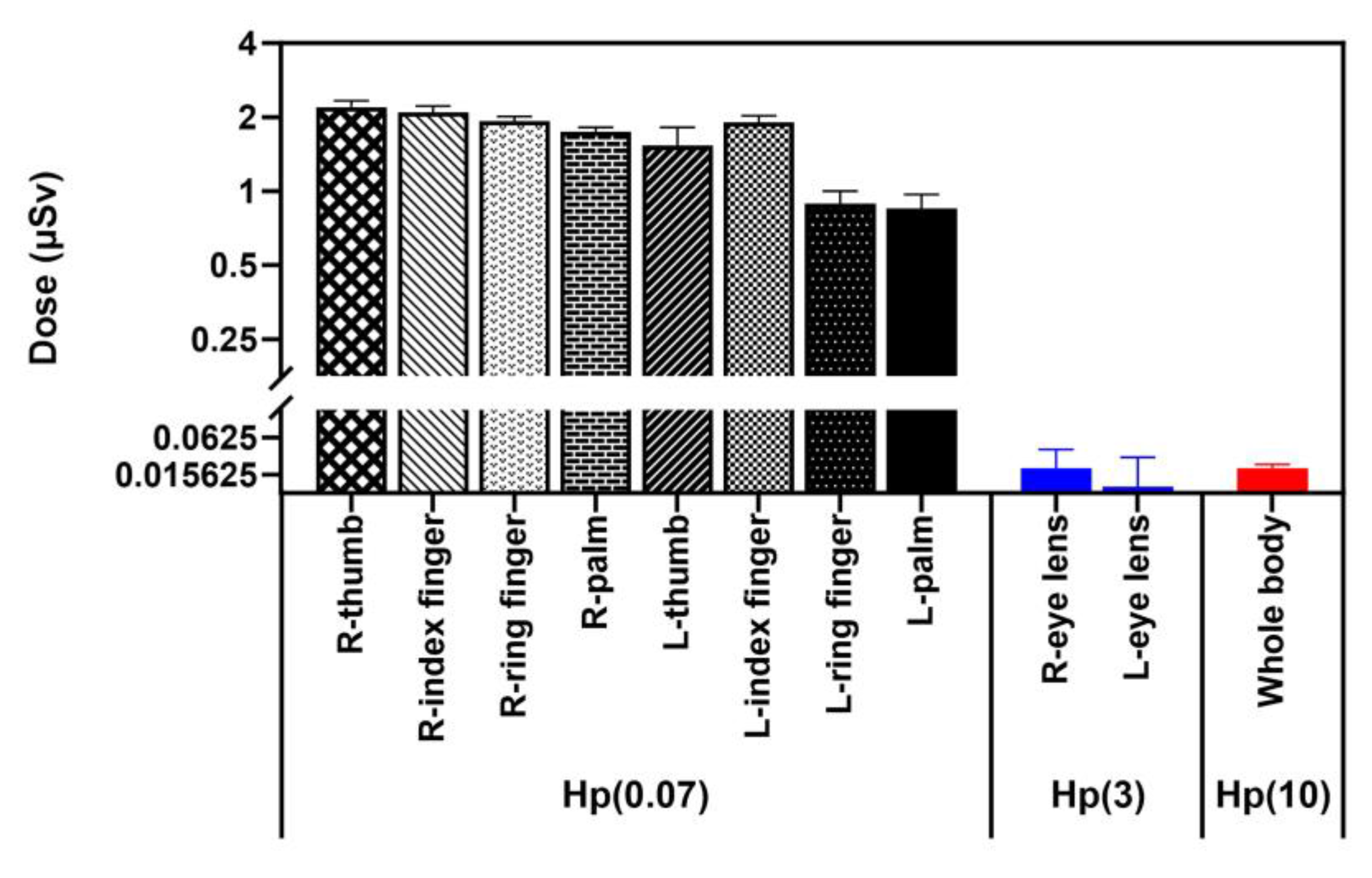
2.6. Personnel Dose Assessment from Radiation Exposure during Preparation and Handling of 99mTc-MDP Radiopharmaceutical
2.7. Evaluation of Virtual Reality as a Technological Tool
2.7.1. Technology Acceptance Model (TAM) Development of Virtual World Technology Learning Media
- Perceived usefulness refers to users’ subjective evaluation of the extent to which technology enhances performance or facilitates job processes. Individuals are more likely to embrace and utilize technologies that offer significant value.
- Perceived ease of use: the ease or difficulty of utilizing a certain technology; higher acceptance levels are characterized by ease of use.
- Behavioral intention refers to a user’s expressed willingness or intention to employ a certain technology. According to TAM, the perceived usefulness and simplicity impact this objective.
2.7.2. Content Validation: Content Validity Index (CVI)
- Define the construct clearly to measure.
- Select experts and identify a panel of experts knowledgeable in VR.
- Item generation creates questions for the measuring tool based on the construct.
- Content review by experts panel evaluation of the questions to ensure they are clear, relevant, and indicative of the VR training module goals.
- Gather expert advice on rephrasing, adding, or eliminating items to improve questionnaire validity.
- Content validity index (CVI) calculation: CVI is calculated separately for each item and then averaged across all items, using the item content validity index (I-CVI).
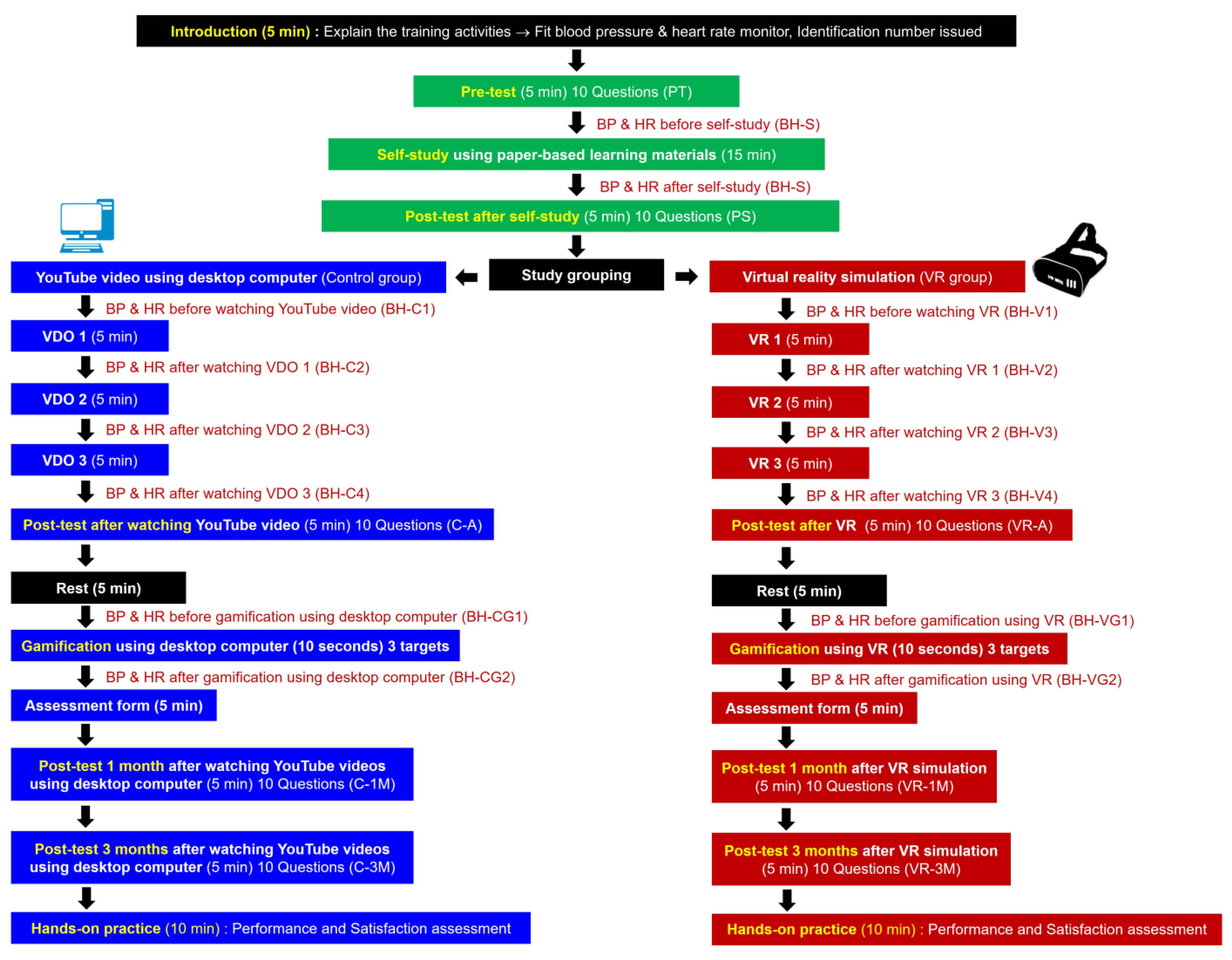
2.8. Comprehensive Evaluation of the Effectiveness of VR-Assisted Teaching in Enhancing Students’ Learning Experiences
2.9. Gamification Supporting Practical and Experimental Learning
2.10. Student Engagement: Physical Assessment Using Blood Pressure and Heart Rate
2.11. Assessment of Satisfaction in VR-Enhanced Learning Experiences: Prioritizing Educational Significance and Practicality in VR-Assisted Teaching
2.12. VR Training Module Questionnaire Analysis
2.12.1. Radiophobia and Safety Confidence
2.12.2. Assessment of Cybersickness in VR-Assisted Teaching Materials
2.13. Qualitative Study of Students’ Perspectives
2.14. Statistical Analysis
3. Results
3.1. Enhancing Virtual Reality Immersive Learning: Implementing Revised Bloom’s Taxonomy in VR Training
3.2. Hot Lab: Assessment of Radiation Dose in Nuclear Medicine Controlled Areas during Preparation and Handling of 99mTc-MDP Radiopharmaceutical
3.3. Personnel Radiation Exposure during Preparation and Handling of 99mTc-MDP Radiopharmaceutical
3.4. Evaluation of Virtual Reality as a Technological Tool: Technology Acceptance Model (TAM) and Content Validation: Content Validity Index (CVI)
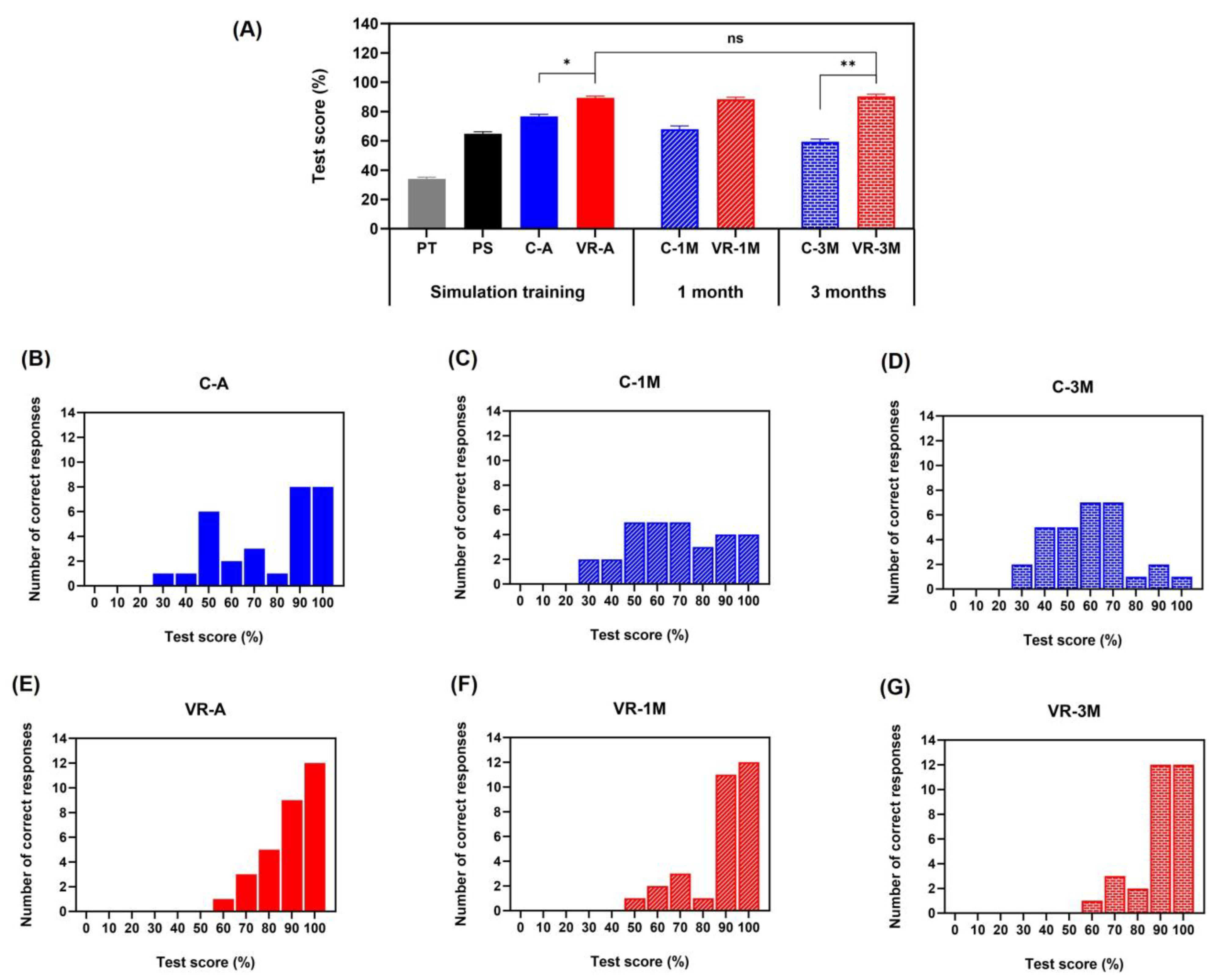
3.5. VR-Assisted Teaching Can Improve Students’ Learning Effectiveness (Pre-Test, Same Day Post-Test, after 1 Month, and after 3 Months)
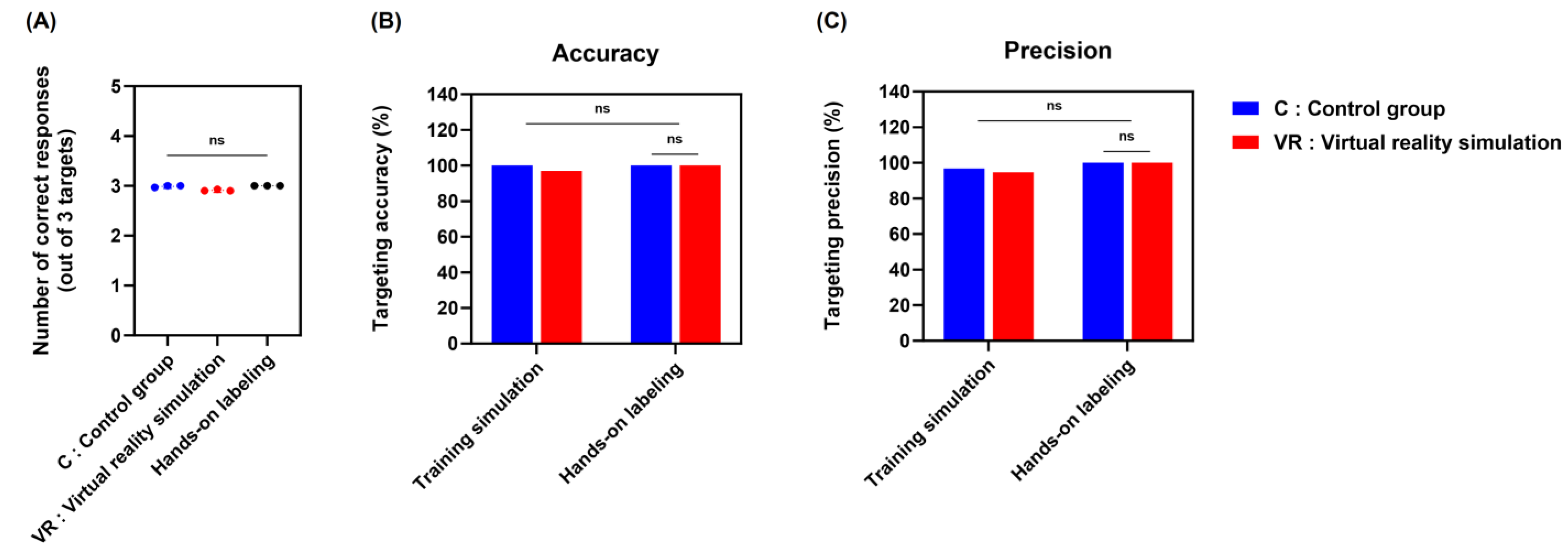
3.6. Supporting Practical and Experimental Gamification of Learning
3.7. Student Engagement: Physical Assessment of Blood Pressure and Heart Rate
3.8. Satisfaction in VR-Enhanced Learning Experience: Prioritizing Educational Significance and Practicality in VR-Assisted Teaching
3.9. VR Training Module Questionnaire Analysis
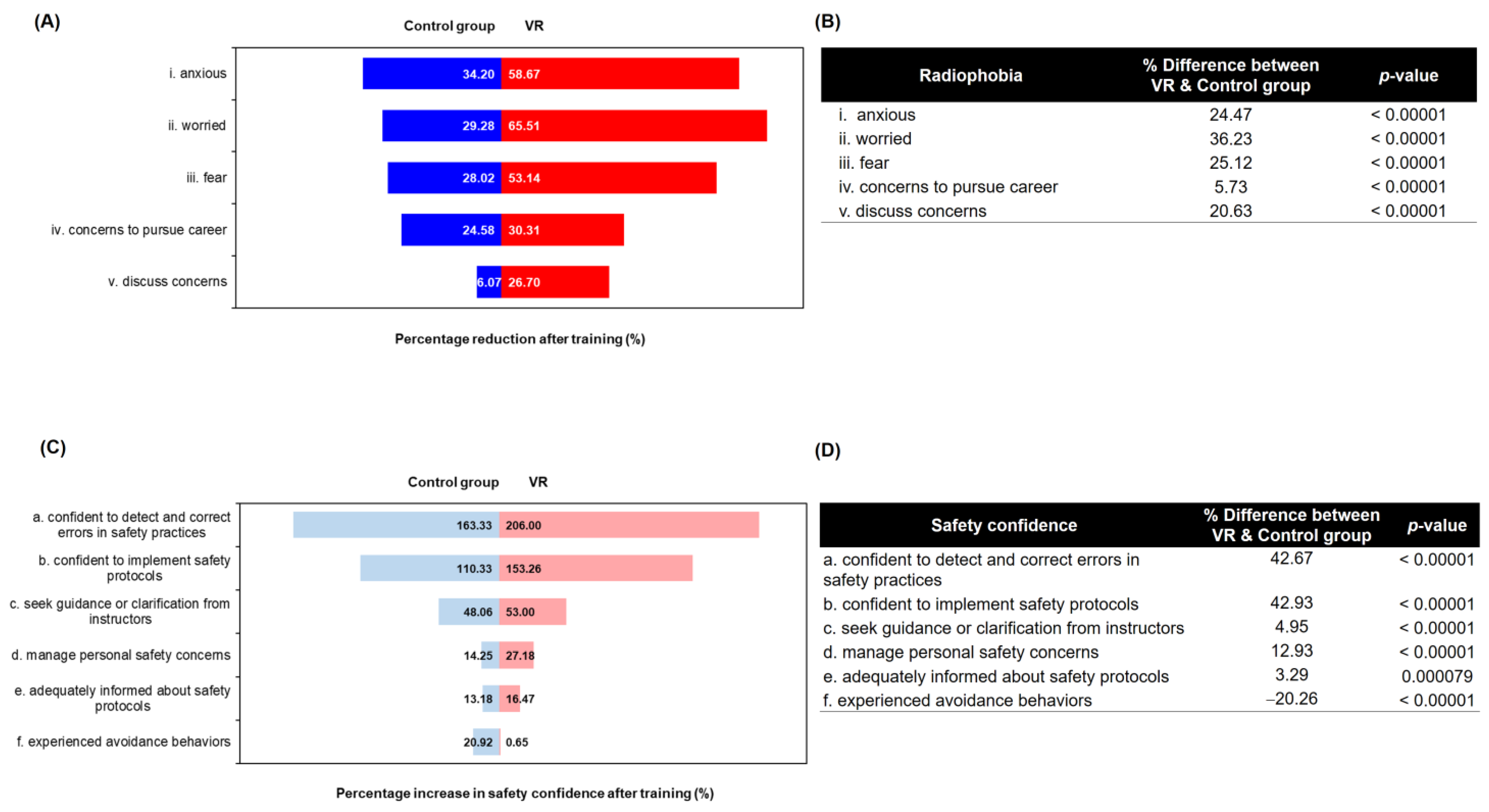
3.9.1. Radiophobia
3.9.2. Safety Confidence
3.9.3. Assessment of Cybersickness in VR-Assisted Teaching Materials
3.10. Qualitative Study of Students’ Perspectives
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hauptmann, M.; Byrnes, G.; Cardis, E.; Bernier, M.-O.; Blettner, M.; Dabin, J.; Engels, H.; Istad, T.S.; Johansen, C.; Kaijser, M. Brain Cancer after Radiation Exposure from CT Examinations of Children and Young Adults: Results from the EPI-CT Cohort Study. Lancet Oncol. 2023, 24, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.J.; Choi, Y.; Ko, S.; Cha, E.S.; Kim, J.; Kim, Y.M.; Kong, K.A.; Seo, S.; Bang, Y.J.; Ha, Y.W. Projected Lifetime Cancer Risks from Occupational Radiation Exposure among Diagnostic Medical Radiation Workers in South Korea. BMC Cancer 2018, 18, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Güngördü, N.; Kurtul, S.; Özdil, A.; Erdoğan, M.S. Does Occupational Ionizing Radiation Exposure in Healthcare Workers Affect Their Hematological Parameters? Arch. Environ. Occup. Health 2023, 78, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Li, Y.-W.; Lu, X.; Liu, Y.; Tian, X.-L.; Gao, L.; Liu, Q.-J.; Fan, L.; Tian, M. Low-Dose Ionizing Radiation: Effects on the Proliferation and Migration of Lens Epithelial Cells via Activation of the Wnt/β-Catenin Pathway. Mutat. Res./Genet. Toxicol. Environ. Mutagen. 2023, 888, 503637. [Google Scholar] [CrossRef] [PubMed]
- Vassileva, J.; Holmberg, O. Radiation Protection Perspective to Recurrent Medical Imaging: What Is Known and What More Is Needed? Br. J. Radiol. 2021, 94, 20210477. [Google Scholar] [CrossRef] [PubMed]
- Boice, J.D., Jr.; Cohen, S.S.; Mumma, M.T.; Howard, S.C.; Yoder, R.C.; Dauer, L.T. Mortality among Medical Radiation Workers in the United States, 1965–2016. Int. J. Radiat. Biol. 2023, 99, 183–207. [Google Scholar] [CrossRef] [PubMed]
- Hamada, N. Noncancer Effects of Ionizing Radiation Exposure on the Eye, the Circulatory System and beyond: Developments Made since the 2011 ICRP Statement on Tissue Reactions. Radiat. Res. 2023, 200, 188–216. [Google Scholar] [CrossRef]
- Hayashi, S.; Takenaka, M.; Kogure, H.; Yakushijin, T.; Maruyama, H.; Hori, Y.; Yoshio, T.; Ikezawa, K.; Takagi, T.; Asai, S. A Questionnaire Survey on Radiation Protection among 282 Medical Staff from 26 Endoscopy-fluoroscopy Departments in Japan. DEN Open 2021, 1, e5. [Google Scholar] [CrossRef]
- Saha, G.B. Radiation Safety in Nuclear Medicine: A Practical, Concise Guide; Springer Nature: Berlin/Heidelberg, Germany, 2023; ISBN 3-031-24609-8. [Google Scholar]
- Frane, N.; Bitterman, A. Radiation Safety and Protection; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- O’Connor, M.; Rainford, L. The Impact of 3D Virtual Reality Radiography Practice on Student Performance in Clinical Practice. Radiography 2023, 29, 159–164. [Google Scholar] [CrossRef]
- Gunn, T.; Jones, L.; Bridge, P.; Rowntree, P.; Nissen, L. The Use of Virtual Reality Simulation to Improve Technical Skill in the Undergraduate Medical Imaging Student. Interact. Learn. Environ. 2018, 26, 613–620. [Google Scholar] [CrossRef]
- O’Connor, M.; Stowe, J.; Potocnik, J.; Giannotti, N.; Murphy, S.; Rainford, L. 3D Virtual Reality Simulation in Radiography Education: The Students’ Experience. Radiography 2021, 27, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Sapkaroski, D.; Mundy, M.; Dimmock, M. Virtual Reality versus Conventional Clinical Role-Play for Radiographic Positioning Training: A Students’ Perception Study. Radiography 2020, 26, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Karpicke, J.D.; Blunt, J.R. Retrieval Practice Produces More Learning than Elaborative Studying with Concept Mapping. Science 2011, 331, 772–775. [Google Scholar] [CrossRef] [PubMed]
- Roediger, H.L.; Butler, A.C. The Critical Role of Retrieval Practice in Long-Term Retention. Trends Cogn. Sci. 2011, 15, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Glenn, D.I. Determining Sample Size. In A Series of the Program Evaluation and Organizational Development; University of Florida: Gainesville, FL, USA, 1992. [Google Scholar]
- Vajak, D.; Livada, Č. Combining Photogrammetry, 3D Modeling and Real Time Information Gathering for Highly Immersive VR Experience. In Proceedings of the 2017 Zooming Innovation in Consumer Electronics International Conference (ZINC), Novi Sad, Serbia, 31 May–1 June 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 82–85. [Google Scholar]
- Luhmann, T.; Robson, S.; Kyle, S.; Boehm, J. Close-Range Photogrammetry and 3D Imaging; Walter de Gruyter GmbH & Co KG: Berlin, Germany, 2023; ISBN 3-11-102967-0. [Google Scholar]
- Likert, R. A Technique for the Measurement of Attitudes. Arch. Psychol. 1932, 22, 55. [Google Scholar]
- Nemoto, T.; Beglar, D. Likert-Scale Questionnaires 2014. In Proceedings of the JALT 2013 Conference Proceedings, Kobe, Japan, 25–28 October 2013; pp. 1–8. [Google Scholar]
- Harpe, S.E. How to Analyze Likert and Other Rating Scale Data. Curr. Pharm. Teach. Learn. 2015, 7, 836–850. [Google Scholar] [CrossRef]
- Brewer-Deluce, D.; Bak, A.B.; Simms, A.J.; Sinha, S.; Mitchell, J.P.; Shin, D.; Saraco, A.N.; Wainman, B.C. Virtual Reality Bell-ringer: The Development and Testing of a Stereoscopic Application for Human Gross Anatomy. Anat. Sci. Educ. 2021, 14, 330–341. [Google Scholar] [CrossRef] [PubMed]
- Lateef, F. Maximizing Learning and Creativity: Understanding Psychological Safety in Simulation-Based Learning. J. Emergencies Trauma Shock 2020, 13, 5. [Google Scholar] [CrossRef] [PubMed]
- Vogt, J.; Oeh, U.; Maringer, F.J. Development of the Occupational Exposure during the Production and Application of Radiopharmaceuticals in Germany. J. Radiol. Prot. 2024, 44, 011508. [Google Scholar] [CrossRef]
- Marshall, S.K.; Prom-On, P.; Sangkue, S.; Thiangsook, W. Assessment of Radiation Exposure in a Nuclear Medicine Department during 99mTc-MDP Bone Scintigraphy. Toxics 2023, 11, 814. [Google Scholar] [CrossRef]
- International Atomic Energy Agency. Quality Management Audits in Nuclear Medicine Practices: Non-Serial Publications; International Atomic Energy Agency: Vienna, Austria, 2009; ISBN 1-282-87844-1. [Google Scholar]
- Furuta, H.; Tsujimura, N.; Nishide, A.; Kudo, S.; Saigusa, S. Conversion Factor from Dosemeter Reading to Air Kerma for Nuclear Worker Using Anthropomorphic Phantom for Further Conversion from Air Kerma to Organ-Absorbed Dose. Radiat. Prot. Dosim. 2020, 189, 371–383. [Google Scholar] [CrossRef] [PubMed]
- International Commission on Radiological Protection. General Principles for the Radiation Protection of Workers: Adopted by the Commission in January 1997; Pergamon Press: Oxford, UK, 1997; ISBN 0-08-042741-3. [Google Scholar]
- International Atomic Energy Agency. Occupational Radiation Protection: General Safety Guide; IAEA: Vienna, Austria, 2018; ISBN 92-0-102917-9. [Google Scholar]
- Solanki, K. Operational Guidance on Hospital Radiopharmacy: A Safe and Effective Approach; International Atomic Energy Agency: Vienna, Austria, 2008. [Google Scholar]
- International Commission on Radiation Units. Quantities and Units in Radiation Protection Dosimetry; International Commission on Radiation: Stockholm, Sweden, 1993; ISBN 0-913394-50-5. [Google Scholar]
- Protection, R. ICRP Publication 103. Ann. ICRP 2007, 37, 2. [Google Scholar]
- Perks, C.A.; Yahnke, C.; Million, M. Medical Dosimetry Using Optically Stimulated Luminescence Dots and microStar Readers. Available online: https://api.semanticscholar.org/CorpusID:7217500 (accessed on 14 February 2024).
- Al-Senan, R.M.; Hatab, M.R. Characteristics of an OSLD in the Diagnostic Energy Range. Med. Phys. 2011, 38, 4396–4405. [Google Scholar] [CrossRef] [PubMed]
- Giansante, L.; Santos, J.C.; Umisedo, N.K.; Terini, R.A.; Costa, P.R. Characterization of OSL Dosimeters for Use in Dose Assessment in Computed Tomography Procedures. Phys. Medica 2018, 47, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Davis, F.D. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Pastor, A.; Bourdin-Kreitz, P. Comparing Episodic Memory Outcomes from Walking Augmented Reality and Stationary Virtual Reality Encoding Experiences. Sci. Rep. 2024, 14, 1–23. [Google Scholar]
- Cimadevilla, J.M.; Nori, R.; Piccardi, L. Application of Virtual Reality in Spatial Memory. Brain Sci. 2023, 13, 1621. [Google Scholar] [CrossRef] [PubMed]
- Boller, B.; Ouellet, É.; Belleville, S. Using Virtual Reality to Assess and Promote Transfer of Memory Training in Older Adults with Memory Complaints: A Randomized Controlled Trial. Front. Psychol. 2021, 12, 627242. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Shen, S.; Lu, Q.; Zhong, S.; Lv, S.; Lai, S.; Luo, Y.; Ran, H.; Duan, M.; Song, K. Virtual Reality Working Memory Training Improves Cognitive Performance of Acute and Remitted Patients with Major Depressive Disorder. J. Affect. Disord. 2024, 344, 267–276. [Google Scholar] [CrossRef]
- Gentry, S.V.; Gauthier, A.; Ehrstrom, B.L.; Wortley, D.; Lilienthal, A.; Car, L.T.; Dauwels-Okutsu, S.; Nikolaou, C.K.; Zary, N.; Campbell, J. Serious Gaming and Gamification Education in Health Professions: Systematic Review. J. Med. Internet Res. 2019, 21, e12994. [Google Scholar] [CrossRef]
- Choi, D.; Seo, S.; Park, H.; Hong, T.; Koo, C. Forecasting Personal Learning Performance in Virtual Reality-Based Construction Safety Training Using Biometric Responses. Autom. Constr. 2023, 156, 105115. [Google Scholar] [CrossRef]
- Darnell, D.K.; Krieg, P.A. Student Engagement, Assessed Using Heart Rate, Shows No Reset Following Active Learning Sessions in Lectures. PLoS ONE 2019, 14, e0225709. [Google Scholar] [CrossRef] [PubMed]
- Bustos-López, M.; Cruz-Ramírez, N.; Guerra-Hernández, A.; Sánchez-Morales, L.N.; Cruz-Ramos, N.A.; Alor-Hernández, G. Wearables for Engagement Detection in Learning Environments: A Review. Biosensors 2022, 12, 509. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, C.M.; Gomes, R.D.A.; Monteiro, C.B.D.M.; Dias, R.M.; Simcsik, A.O.; de Araújo, L.V.; Maia, L.C.P.; de Oliveira, A.P.; de Freitas, B.L.; Dawes, H. Heart Rate Variability during Virtual Reality Activity in Individuals after Hospitalization for COVID-19: A Cross-Sectional Control Study. Electronics 2023, 12, 1925. [Google Scholar] [CrossRef]
- Weibel, R.P.; Grübel, J.; Zhao, H.; Thrash, T.; Meloni, D.; Hölscher, C.; Schinazi, V.R. Virtual Reality Experiments with Physiological Measures. JoVE (J. Vis. Exp.) 2018, 138, e58318. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Harrell, M.C.; Bradley, M. Data Collection Methods: Semi-Structured Interviews and Focus Groups; RAND Corporation: Santa Monica, CA, USA, 2009. [Google Scholar]
- Gill, P.; Baillie, J. Interviews and Focus Groups in Qualitative Research: An Update for the Digital Age. Br. Dent. J. 2018, 225, 668–672. [Google Scholar] [CrossRef] [PubMed]
- Longhurst, R. Semi-Structured Interviews and Focus Groups. Key Methods Geogr. 2003, 3, 143–156. [Google Scholar]
- Whitman, L.; Malzahn, D.; Madhavan, V.; Weheba, G.; Krishnan, K. Virtual Reality Case Study throughout the Curriculum to Address Competency Gaps. Int. J. Eng. Educ. 2004, 20, 690–702. [Google Scholar]
- Meyer, O.; Imhof, M.; Coyle, D.; Banerjee, M. Positive Learning and Pluriliteracies: Growth in Higher Education and Implications for Course Design, Assessment and Research. In Positive Learning in the Age of Information: A Blessing or a Curse? Springer: Berlin/Heidelberg, Germany, 2018; pp. 235–265. [Google Scholar]
- Catai, A.M.; Pastre, C.M.; de Godoy, M.F.; da Silva, E.; de Medeiros Takahashi, A.C.; Vanderlei, L.C.M. Heart Rate Variability: Are You Using It Properly? Standardisation Checklist of Procedures. Braz. J. Phys. Ther. 2020, 24, 91–102. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Training, R. TRAININGCOURSESERIES 39. Available online: https://www-pub.iaea.org/MTCD/Publications/PDF/TCS-39_web.pdf (accessed on 25 February 2024).
- Vassileva, J.; Applegate, K.; Paulo, G.; Vano, E.; Holmberg, O. Strengthening Radiation Protection Education and Training of Health Professionals: Conclusions from an IAEA Meeting. J. Radiol. Prot. 2022, 42, 011504. [Google Scholar] [CrossRef] [PubMed]
- Santos, J.; Foley, S.; Andersson, J.; Figueiredo, J.P.; Hoeschen, C.; Damilakis, J.; Frija, G.; Alves, F.; Riklund, K.; Rainford, L. Education and Training in Radiation Protection in Europe: Results from the EURAMED Rocc-n-Roll Project Survey. Insights Into. Imaging 2023, 14, 55. [Google Scholar] [CrossRef] [PubMed]
- Newhauser, W.D.; Williams, J.P.; Noska, M.A.; Bluth, E.I.; Townsend, L.W.; Tolmachev, S.Y.; Dewji, S.A. In Support of ICRP’s Call to Action to Strengthen Expertise in Radiological Protection Worldwide. Radiat. Environ. Biophys. 2023, 62, 287–288. [Google Scholar] [CrossRef] [PubMed]
- Rühm, W.; Cho, K.; Larsson, C.-M.; Wojcik, A.; Clement, C.; Applegate, K.; Bochud, F.; Bouffler, S.; Cool, D.; Hirth, G. Vancouver Call for Action to Strengthen Expertise in Radiological Protection Worldwide. Radiat. Environ. Biophys. 2023, 62, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Giammarile, F.; Orellana, P.; Paez, D. IAEA Strategy for Enhancing the Sustainability of Nuclear Medicine in Low-and Middle-Income Countries. In Beyond Becquerel and Biology to Precision Radiomolecular Oncology: Festschrift in Honor of Richard P. Baum; Springer International Publishing: Cham, Switzerland, 2024; pp. 101–107. [Google Scholar]
- Wilmoth, J.; Menozzi, C.; Bassarsky, L. Global Population Growth and Sustainable Development; United Nations: New York, NY, USA, 2021. [Google Scholar]
- Kim, H.-Y.; Kim, E.-Y. Effects of Medical Education Program Using Virtual Reality: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 3895. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.C.; Roediger, H.L., III; McDaniel, M.A. Make It Stick: The Science of Successful Learning; Harvard University Press: Cambridge, UK, 2014; ISBN 0-674-72901-3. [Google Scholar]
- Rainford, L.; Tcacenco, A.; Potocnik, J.; Brophy, C.; Lunney, A.; Kearney, D.; O’Connor, M. Student Perceptions of the Use of Three-Dimensional (3-D) Virtual Reality (VR) Simulation in the Delivery of Radiation Protection Training for Radiography and Medical Students. Radiography 2023, 29, 777–785. [Google Scholar] [CrossRef] [PubMed]
- Miguel-Alonso, I.; Checa, D.; Guillen-Sanz, H.; Bustillo, A. Evaluation of the Novelty Effect in Immersive Virtual Reality Learning Experiences. Virtual Real. 2024, 28, 27. [Google Scholar] [CrossRef]
- Makransky, G.; Lilleholt, L. A Structural Equation Modeling Investigation of the Emotional Value of Immersive Virtual Reality in Education. Educ. Technol. Res. Dev. 2018, 66, 1141–1164. [Google Scholar] [CrossRef]
- Chávez, O.L.; Rodríguez, L.-F.; Gutierrez-Garcia, J.O. A Comparative Case Study of 2D, 3D and Immersive-Virtual-Reality Applications for Healthcare Education. Int. J. Med. Inform. 2020, 141, 104226. [Google Scholar] [CrossRef]
- Liu, J.Y.W.; Yin, Y.-H.; Kor, P.P.K.; Cheung, D.S.K.; Zhao, I.Y.; Wang, S.; Su, J.J.; Christensen, M.; Tyrovolas, S.; Leung, A.Y. The Effects of Immersive Virtual Reality Applications on Enhancing the Learning Outcomes of Undergraduate Health Care Students: Systematic Review With Meta-Synthesis. J. Med. Internet Res. 2023, 25, e39989. [Google Scholar] [CrossRef] [PubMed]
- Bjork, E.L.; Bjork, R.A. Making Things Hard on Yourself, but in a Good Way: Creating Desirable Difficulties to Enhance Learning. In Psychology and the Real World: Essays Illustrating Fundamental Contributions to Society; Worth Publishing: New York, NY, USA, 2011; Volume 2. [Google Scholar]
- Agarwal, P.K.; Bain, P.M.; Chamberlain, R.W. The Value of Applied Research: Retrieval Practice Improves Classroom Learning and Recommendations from a Teacher, a Principal, and a Scientist. Educ. Psychol. Rev. 2012, 24, 437–448. [Google Scholar] [CrossRef]
- Aljabari, S.; Kadhim, Z. Common Barriers to Reporting Medical Errors. Sci. World J. 2021, 2021, 6494889. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.H.; Chang, H.J.; Kim, S.S.; Park, J.E.; Chung, W.Y.; Lee, S.K.; Kim, M.; Lee, J.H.; Jung, Y.J. Effects of High-Fidelity Simulation Education on Medical Students’ Anxiety and Confidence. PLoS ONE 2021, 16, e0251078. [Google Scholar] [CrossRef] [PubMed]
- Zinchenko, Y.; Khoroshikh, P.; Sergievich, A.; Smirnov, A.; Tumyalis, A.; Kovalev, A.; Gutnikov, S.; Golokhvast, K. Virtual Reality Is More Efficient in Learning Human Heart Anatomy Especially for Subjects with Low Baseline Knowledge. New Ideas Psychol. 2020, 59, 100786. [Google Scholar] [CrossRef]
- Chung, L.-Y. Incorporating 3D-Virtual Reality into Language Learning. Int. J. Digit. Content Technol. Its Appl. 2012, 6, 249–255. [Google Scholar]
- Redondo-Rodríguez, C.; Becerra-Mejías, J.A.; Gil-Fernández, G.; Rodríguez-Velasco, F.J. Influence of Gamification and Cooperative Work in Peer, Mixed and Interdisciplinary Teams on Emotional Intelligence, Learning Strategies and Life Goals That Motivate University Students to Study. Int. J. Environ. Res. Public Health 2022, 20, 547. [Google Scholar] [CrossRef]
- Gan, W.; Mok, T.-N.; Chen, J.; She, G.; Zha, Z.; Wang, H.; Li, H.; Li, J.; Zheng, X. Researching the Application of Virtual Reality in Medical Education: One-Year Follow-Up of a Randomized Trial. BMC Med. Educ. 2023, 23, 3. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.; Uz-Bilgin, C.; Tutwiler, M.S.; Anteneh, M.; Meija, J.C.; Wang, A.; Tan, P.; Eberhardt, R.; Roy, D.; Perry, J. Immersion Positively Affects Learning in Virtual Reality Games Compared to Equally Interactive 2D Games. Inf. Learn. Sci. 2021, 122, 442–463. [Google Scholar] [CrossRef]
- Essoe, J.K.-Y.; Reggente, N.; Ohno, A.A.; Baek, Y.H.; Dell’Italia, J.; Rissman, J. Enhancing Learning and Retention with Distinctive Virtual Reality Environments and Mental Context Reinstatement. NPJ Sci. Learn. 2022, 7, 31. [Google Scholar] [CrossRef]
- Ariansyah, D.; Pardamean, B.; Barbaro, E.; Erkoyuncu, J.A. Augmented Reality Training for Improved Learnability. CIRP J. Manuf. Sci. Technol. 2024, 48, 19–27. [Google Scholar] [CrossRef]
- Radianti, J.; Majchrzak, T.A.; Fromm, J.; Wohlgenannt, I. A Systematic Review of Immersive Virtual Reality Applications for Higher Education: Design Elements, Lessons Learned, and Research Agenda. Comput. Educ. 2020, 147, 103778. [Google Scholar] [CrossRef]
- Moser, S.; Zumbach, J.; Deibl, I. The Effect of Metacognitive Training and Prompting on Learning Success in Simulation-based Physics Learning. Sci. Educ. 2017, 101, 944–967. [Google Scholar] [CrossRef]
- Pellas, N. The Influence of Computer Self-Efficacy, Metacognitive Self-Regulation and Self-Esteem on Student Engagement in Online Learning Programs: Evidence from the Virtual World of Second Life. Comput. Hum. Behav. 2014, 35, 157–170. [Google Scholar] [CrossRef]
- Lindberg, J.C.; Archer, D. Radiophobia: Useful Concept, or Ostracising Term? Prog. Nucl. Energy 2022, 149, 104280. [Google Scholar] [CrossRef]
- Lindberg, J.C. ‘J’Accuse.!’: The Continuous Failure to Address Radiophobia and Placing Radiation in Perspective. J. Radiol. Prot. 2021, 41, 459. [Google Scholar] [CrossRef] [PubMed]
- Dauer, L.T.; Thornton, R.H.; Hay, J.L.; Balter, R.; Williamson, M.J.; St. Germain, J. Fears, Feelings, and Facts: Interactively Communicating Benefits and Risks of Medical Radiation with Patients. Am. J. Roentgenol. 2011, 196, 756–761. [Google Scholar] [CrossRef] [PubMed]
- Bader, I.; Bader, I.; Lopes Alves, I.; Vállez García, D.; Vellas, B.; Dubois, B.; Boada, M.; Marquié, M.; Altomare, D.; Scheltens, P. Recruitment of Pre-Dementia Participants: Main Enrollment Barriers in a Longitudinal Amyloid-PET Study. Alzheimer’s Res. Ther. 2023, 15, 189. [Google Scholar] [CrossRef]
- Kirkpatrick, J.D.; Kirkpatrick, W.K. Kirkpatrick’s Four Levels of Training Evaluation; Association for Talent Development: Alexandria, VA, USA, 2016; ISBN 1-60728-102-3. [Google Scholar]
- Anderson, C. Presenting and Evaluating Qualitative Research. Am. J. Pharm. Educ. 2010, 74, 141. [Google Scholar] [CrossRef]



| Theme | Code | Examples | Frequency | |
|---|---|---|---|---|
| n | % | |||
| Useful learning tool | Engage | “VR improves my focus and engagement, ensuring that I remain completely focused without breaks in concentration.” | 6 | 60 |
| Easy to understand | “Easier to learn and understand the radiopharmaceutical preparation process and quality control steps.” “Opportunity to see all the process and steps before lab practice and easy-to-follow protocols.” | 9 | 90 | |
| Memory | “It (VR) helps me remember information by doing and interacting rather than reading/hearing.” | 8 | 80 | |
| Safety confidence | “You may fail, make mistakes, and learn from them.” “VR…It’s building my confidence through providing a secure environment conducive to experimentation and trial and error.” “I am not so scared of working in the hot lab.” | 7 | 70 | |
| Learning experiences | “I really liked the recorded voice. That makes the experience even better for me, because I actually interacted with that voice and interactions, and, sure, it is pleasant, I feel to myself [smiles].” “It’s memorable because it’s more interactive, enjoyable, and personal.” | 7 | 70 | |
| Implement in curriculum | “VR might be used in every lesson; could you incorporate it into the curriculum.” | 8 | 80 | |
| Getting ready for the clinical practice | “There are only a few opportunities for me to practice the skills during hot lab practical, and while I am in clinical practice, I do not have the chance to practice them as frequently as I would want. VR training would enable me to practice as much as possible before clinical practice. It would be fantastic if there were booster classes that utilized virtual reality training before clinical practice.” “VR before hot lab practice and clinical practice would be beneficial.” “If I’m in clinical practice, I think I’ll feel nervous, especially when attempting something for the first time. This is where VR could be incredibly useful. It would allow me to practice hands-on procedures in a simulated environment and gain experience and confidence without the pressure of being in an actual clinical setting.” | 10 | 100 | |
| Challenges and threats | Resources incurred by the technology | “Due to costs, it is not feasible to train many students at the same time.” “It could be that insufficient VR devices could lead to students lagging behind, as some might not be able to complete the learning materials until a week after others have finished. As a result, the initial group would have a seven-day learning advantage, while the latter group would be left waiting without actively participating.” | 7 | 70 |
| Simulation sickness | “I have experienced discomfort or motion sickness when using VR systems, which can limit the duration and effectiveness of training sessions.” | 2 | 20 | |
| Interactivity limitations | “While VR can provide engaging experiences, the amount of involvement may be restricted compared to real-world interactions, reducing the depth of learning and skill development.” | 3 | 30 | |
| Lack of personalization | “I think VR simulations may not always match individual learning methods or preferences, limiting their efficacy for all interested students.” | 2 | 20 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marshall, S.K.; Sirieak, N.; Karnkorn, P.; Keawtong, V.; Hayeeabdunromae, A.; Noomad, N.; Durawee, W.; Cheewakul, J. Nuclear Medicine Radiological Hot Laboratory Simulation: A Mixed-Method Intervention Study on Immersive Virtual Reality for Sustainable Education. Appl. Sci. 2024, 14, 5041. https://doi.org/10.3390/app14125041
Marshall SK, Sirieak N, Karnkorn P, Keawtong V, Hayeeabdunromae A, Noomad N, Durawee W, Cheewakul J. Nuclear Medicine Radiological Hot Laboratory Simulation: A Mixed-Method Intervention Study on Immersive Virtual Reality for Sustainable Education. Applied Sciences. 2024; 14(12):5041. https://doi.org/10.3390/app14125041
Chicago/Turabian StyleMarshall, Suphalak Khamruang, Nantakorn Sirieak, Pornchanok Karnkorn, Virunyupa Keawtong, Awatif Hayeeabdunromae, Nadia Noomad, Wanita Durawee, and Jongwat Cheewakul. 2024. "Nuclear Medicine Radiological Hot Laboratory Simulation: A Mixed-Method Intervention Study on Immersive Virtual Reality for Sustainable Education" Applied Sciences 14, no. 12: 5041. https://doi.org/10.3390/app14125041
APA StyleMarshall, S. K., Sirieak, N., Karnkorn, P., Keawtong, V., Hayeeabdunromae, A., Noomad, N., Durawee, W., & Cheewakul, J. (2024). Nuclear Medicine Radiological Hot Laboratory Simulation: A Mixed-Method Intervention Study on Immersive Virtual Reality for Sustainable Education. Applied Sciences, 14(12), 5041. https://doi.org/10.3390/app14125041







