Exploratory Anterior Cruciate Ligament Graft Stress during Medial Knee Rotation with and without Iliotibial Band–Intermuscular Septum Lateral Extra-Articular Tenodesis for Transtibial and Anteromedial Femoral Tunnels
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Design
2.2. Geometry and Mesh Generation
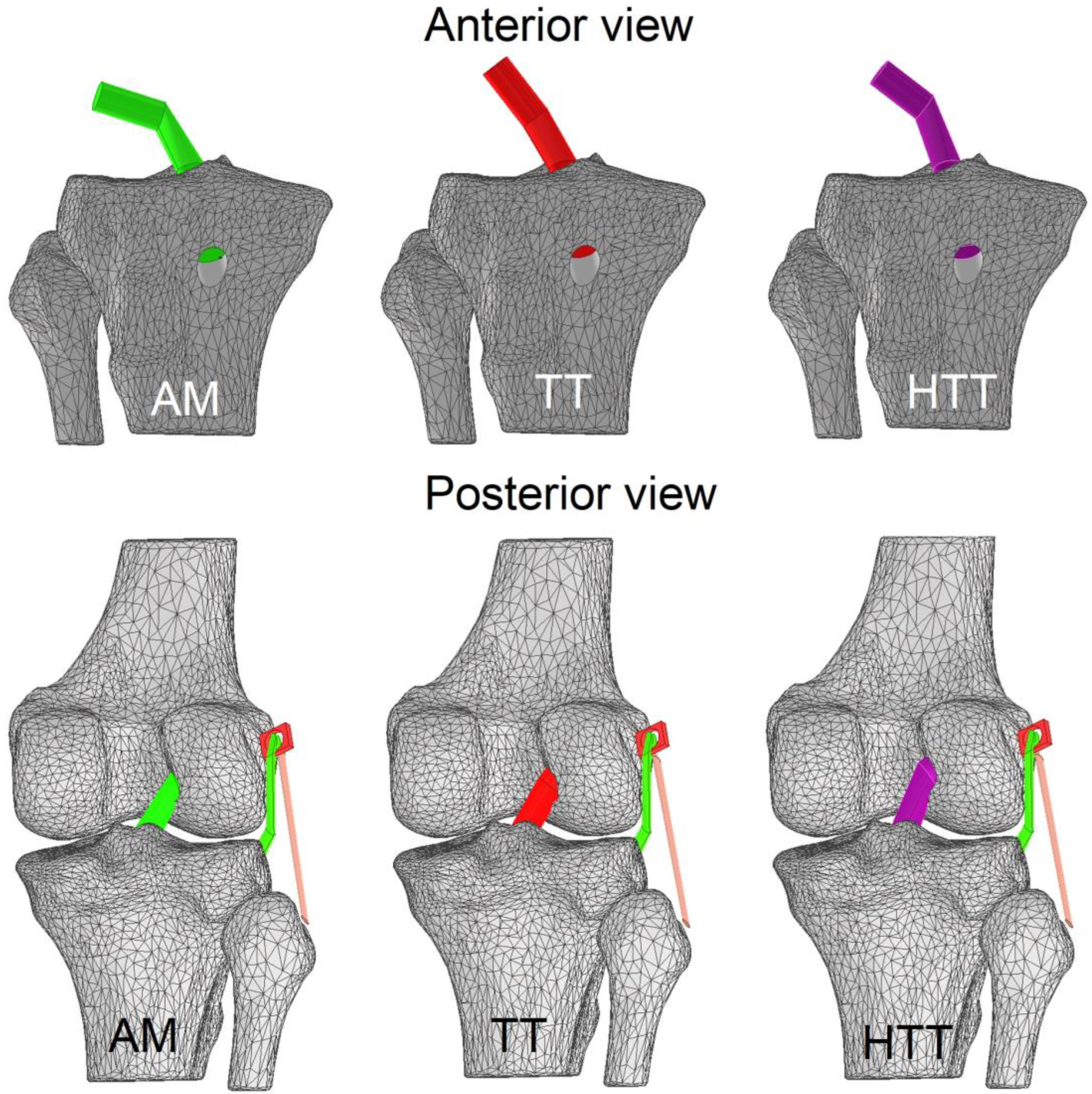
2.3. Knee Tunnels and ACLr Graft
2.4. Iliotibial Band–Intermuscular Septum LET
2.5. Materials Properties
2.6. Boundary Conditions
2.7. Validation of the FE Model
2.8. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grassi, A.; Pizza, N.; Al-Zu’bi, B.B.H.; Fabbro, G.D.; Lucidi, G.A.; Zaffagnini, S. Clinical Outcomes and Osteoarthritis at Very Long-Term Follow-up After ACL Reconstruction: A Systematic Review and Meta-Analysis. Orthop. J. Sports Med. 2022, 10, 23259671211062238. [Google Scholar] [CrossRef] [PubMed]
- Michel, E.; Jordan, E.; Canovas, F.; Bouchdoug, K.; Dagneaux, L.; Gaillard, F. Influence of Residual Anterior Laxity on Functional Outcomes after Anterior Cruciate Ligament Reconstruction. Orthop. Traumatol. Surg. Res. 2022, 108, 103264. [Google Scholar] [CrossRef] [PubMed]
- Tudisco, C.; Bisicchia, S.; Cosentino, A.; Chiozzi, F.; Piva, M. Knee Stability, Athletic Performance and Sport-Specific Tasks in Non-Professional Soccer Players after ACL Reconstruction: Comparing Trans-Tibial and Antero-Medial Portal Techniques. Muscles Ligaments Tendons J. 2015, 5, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Kulczycka, P.; Larbi, A.; Malghem, J.; Thienpont, E.; Vande Berg, B.; Lecouvet, F. Imaging ACL Reconstructions and Their Complications. Diagn. Interv. Imaging 2015, 96, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.-S.; Song, S.Y.; Oh, J.U.; Seo, Y.-J. Effects of Modified Trans-Tibial versus Trans-Portal Technique on Stress Patterns around the Femoral Tunnel in Anatomical Single-Bundle ACL Reconstruction with Different Knee Flexion Angles Using Finite Element Analysis. BMC Musculoskelet. Disord. 2022, 23, 759. [Google Scholar] [CrossRef] [PubMed]
- Na, B.-R.; Kwak, W.-K.; Seo, H.-Y.; Seon, J.-K. Clinical Outcomes of Anterolateral Ligament Reconstruction or Lateral Extra-Articular Tenodesis Combined with Primary ACL Reconstruction: A Systematic Review With Meta-Analysis. Orthop. J. Sports Med. 2021, 9, 23259671211023099. [Google Scholar] [CrossRef] [PubMed]
- Weber, A.E.; Zuke, W.; Mayer, E.N.; Forsythe, B.; Getgood, A.; Verma, N.N.; Bach, B.R.; Bedi, A.; Cole, B.J. Lateral Augmentation Procedures in Anterior Cruciate Ligament Reconstruction: Anatomic, Biomechanical, Imaging, and Clinical Evidence. Am. J. Sports Med. 2019, 47, 740–752. [Google Scholar] [CrossRef]
- Inderhaug, E.; Stephen, J.M.; Williams, A.; Amis, A.A. Biomechanical Comparison of Anterolateral Procedures Combined With Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2017, 45, 347–354. [Google Scholar] [CrossRef]
- Devitt, B.M.; Bouguennec, N.; Barfod, K.W.; Porter, T.; Webster, K.E.; Feller, J.A. Combined Anterior Cruciate Ligament Reconstruction and Lateral Extra-Articular Tenodesis Does Not Result in an Increased Rate of Osteoarthritis: A Systematic Review and Best Evidence Synthesis. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1149–1160. [Google Scholar] [CrossRef]
- Taketomi, S. Editorial Commentary: Tunnel Widening After Anterior Cruciate Ligament Reconstruction May Increase Laxity and Complicate Revision. Arthroscopy 2021, 37, 2564–2566. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, B.; Cheng, C.-K. Stiffness and Shape of the ACL Graft Affects Tunnel Enlargement and Graft Wear. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 2184–2193. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Papannagari, R.; DeFrate, L.E.; Yoo, J.D.; Park, S.E.; Gill, T.J. Comparison of the ACL and ACL Graft Forces before and after ACL Reconstruction: An in-Vitro Robotic Investigation. Acta Orthop. 2006, 77, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Jennings, J.K.; Leas, D.P.; Fleischli, J.E.; D’Alessandro, D.F.; Peindl, R.D.; Piasecki, D.P. Transtibial Versus Anteromedial Portal ACL Reconstruction: Is a Hybrid Approach the Best? Orthop. J. Sports Med. 2017, 5, 2325967117719857. [Google Scholar] [CrossRef] [PubMed]
- Dargel, J.; Schmidt-Wiethoff, R.; Fischer, S.; Mader, K.; Koebke, J.; Schneider, T. Femoral Bone Tunnel Placement Using the Transtibial Tunnel or the Anteromedial Portal in ACL Reconstruction: A Radiographic Evaluation. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.Y.; Kim, G.-H.; Seon, J.K.; Jeon, I. Finite Element Study on the Anatomic Transtibial Technique for Single-Bundle Anterior Cruciate Ligament Reconstruction. Med. Biol. Eng. Comput. 2016, 54, 811–820. [Google Scholar] [CrossRef] [PubMed]
- Vaudreuil, N.J.; Rothrauff, B.B.; de Sa, D.; Musahl, V. The Pivot Shift: Current Experimental Methodology and Clinical Utility for Anterior Cruciate Ligament Rupture and Associated Injury. Curr. Rev. Musculoskelet. Med. 2019, 12, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Guarino, A.; Farinelli, L.; Iacono, V.; Screpis, D.; Piovan, G.; Rizzo, M.; Mariconda, M.; Zorzi, C. Lateral Extra-Articular Tenodesis and Anterior Cruciate Ligament Reconstruction in Young Patients: Clinical Results and Return to Sport. Orthop. Rev. (Pavia) 2022, 14, 33696. [Google Scholar] [CrossRef] [PubMed]
- Wascher, D.C.; Lording, T.D.; Neyret, P. Extra-Articular Procedures for the ACL-Deficient Knee: A State of the Art Review. J. ISAKOS 2016, 1, 174–182. [Google Scholar] [CrossRef]
- Moreno Mateo, F.; Perea, S.H.; Green, D.W. Lateral-Extra Articular Tenodesis vs. Anterolateral Ligament Reconstruction in Skeletally Immature Patients Undergoing Anterior Cruciate Ligament Reconstruction. Curr. Opin. Pediatr. 2022, 34, 71–75. [Google Scholar] [CrossRef]
- Nazzal, E.M.; Keeling, L.E.; Ryan, P.M.; Herman, Z.J.; Hughes, J.D. The Role of Lateral Extra-Articular Tenodesis in Anterior Cruciate Ligament Reconstruction and Treatment of Rotatory Knee Instability: A Scoping Review. Curr. Rev. Musculoskelet. Med. 2023, 16, 235–245. [Google Scholar] [CrossRef]
- Kurzweil, P.R.; Frogameni, A.D.; Jackson, D.W. Tibial Interference Screw Removal Following Anterior Cruciate Ligament Reconstruction. Arthroscopy 1995, 11, 289–291. [Google Scholar] [CrossRef] [PubMed]
- Hirschmann, M.T.; Adler, T.; Rasch, H.; Hügli, R.W.; Friederich, N.F.; Arnold, M.P. Painful Knee Joint after ACL Reconstruction Using Biodegradable Interference Screws- SPECT/CT a Valuable Diagnostic Tool? A Case Report. BMC Sports Sci. Med. Rehabil. 2010, 2, 24. [Google Scholar] [CrossRef] [PubMed]
- Abusleme, S.; Strömbäck, L.; Caracciolo, G.; Zamorano, H.; Cheyre, J.; Vergara, F.; Yañez, R. Lateral Extra-Articular Tenodesis: A Technique With an Iliotibial Band Strand Without Implants. Arthrosc. Tech. 2021, 10, e85–e89. [Google Scholar] [CrossRef] [PubMed]
- Slette, E.L.; Mikula, J.D.; Schon, J.M.; Marchetti, D.C.; Kheir, M.M.; Turnbull, T.L.; LaPrade, R.F. Biomechanical Results of Lateral Extra-Articular Tenodesis Procedures of the Knee: A Systematic Review. Arthroscopy 2016, 32, 2592–2611. [Google Scholar] [CrossRef] [PubMed]
- Herrera, A.; Ibarz, E.; Cegoñino, J.; Lobo-Escolar, A.; Puértolas, S.; López, E.; Mateo, J.; Gracia, L. Applications of Finite Element Simulation in Orthopedic and Trauma Surgery. World J. Orthop. 2012, 3, 25–41. [Google Scholar] [CrossRef] [PubMed]
- Benos, L.; Stanev, D.; Spyrou, L.; Moustakas, K.; Tsaopoulos, D.E. A Review on Finite Element Modeling and Simulation of the Anterior Cruciate Ligament Reconstruction. Front. Bioeng. Biotechnol. 2020, 8, 967. [Google Scholar] [CrossRef] [PubMed]
- Fedorov, A.; Beichel, R.; Kalpathy-Cramer, J.; Finet, J.; Fillion-Robin, J.-C.; Pujol, S.; Bauer, C.; Jennings, D.; Fennessy, F.; Sonka, M.; et al. 3D Slicer as an Image Computing Platform for the Quantitative Imaging Network. Magn. Reson. Imaging 2012, 30, 1323–1341. [Google Scholar] [CrossRef]
- Trofa, D.P.; Saltzman, B.M.; Corpus, K.T.; Connor, P.M.; Fleischli, J.E.; Piasecki, D.P. A Hybrid Transtibial Technique Combines the Advantages of Anteromedial Portal and Transtibial Approaches: A Prospective Randomized Controlled Trial. Am. J. Sports Med. 2020, 48, 3200–3207. [Google Scholar] [CrossRef]
- Zamorano, H.; Yáñez-Diaz, R.; Vergara, F.; Caracciolo, G.; Valdés, S.; Yáñez-Rojo, R.; De la Fuente, C. Achilles Tendon Allograft Preparation Technique for Anterior Cruciate Ligament Reconstruction: A Technical Note. Arthrosc. Tech. 2021, 10, e2143–e2150. [Google Scholar] [CrossRef]
- Hayashi, A.; Maruyama, Y. Lateral Intermuscular Septum of the Thigh and Short Head of the Biceps Femoris Muscle: An Anatomic Investigation with New Clinical Applications. Plast. Reconstr. Surg. 2001, 108, 1646–1654. [Google Scholar] [CrossRef]
- Cheng, R.; Wang, H.; Jiang, Z.; Dimitriou, D.; Cheng, C.-K.; Tsai, T.-Y. The Femoral Tunnel Drilling Angle at 45° Coronal and 45° Sagittal Provided the Lowest Peak Stress and Strain on the Bone Tunnels and Anterior Cruciate Ligament Graft. Front. Bioeng. Biotechnol. 2021, 9, 797389. [Google Scholar] [CrossRef] [PubMed]
- Guenther, D.; Irarrázaval, S.; Bell, K.M.; Rahnemai-Azar, A.A.; Fu, F.H.; Debski, R.E.; Musahl, V. The Role of Extra-Articular Tenodesis in Combined ACL and Anterolateral Capsular Injury. J. Bone Jt. Surg. Am. 2017, 99, 1654–1660. [Google Scholar] [CrossRef] [PubMed]
- Risvas, K.; Stanev, D.; Moustakas, K. Can Lateral Tenodesis Improve the Rotational Stability of the ACL Reconstruction? A Finite Element Analysis. PLoS ONE 2024, 19, e0293161. [Google Scholar] [CrossRef] [PubMed]
- Neira, A.; Silvestre, R.; Debandi, A.; Darras, D.; Cristi-Sánchez, I.; Barra, I.; Peñailillo, L.; De La Fuente, C. Is the Rotatory Knee Stability Immediately Decreased Following a Competitive Soccer Match? Front. Bioeng. Biotechnol. 2022, 10, 903131. [Google Scholar] [CrossRef] [PubMed]
- Zaffagnini, S.; Lucidi, G.A.; Macchiarola, L.; Agostinone, P.; Neri, M.P.; Marcacci, M.; Grassi, A. The 25-Year Experience of over-the-Top ACL Reconstruction plus Extra-Articular Lateral Tenodesis with Hamstring Tendon Grafts: The Story so Far. J. Exp. Orthop. 2023, 10, 36. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Liu, Y.; Ma, S.; Ding, C.; Kong, Z.; Li, H.; Huang, F.; Chen, H.; Zhong, H. Stress and Strain Changes of the Anterior Cruciate Ligament at Different Knee Flexion Angles: A Three-Dimensional Finite Element Study. J. Orthop. Sci. 2023; in press. [Google Scholar] [CrossRef]
- Yao, S.; Yung, P.S.H.; Lui, P.P.Y. Tackling the Challenges of Graft Healing After Anterior Cruciate Ligament Reconstruction-Thinking From the Endpoint. Front. Bioeng. Biotechnol. 2021, 9, 756930. [Google Scholar] [CrossRef]



| Knee Element | Material | Parameters |
|---|---|---|
| Bones | Rigid | Young modulus = 0.4 GPa Poisson coefficient = 0.33 |
| ACLr graft | Isotropic hyperelastic (no linear) | Veronda–Westmann coefficients of α = 0.3 MPa β = 12.20 |
| Lateral collateral ligament | Hyperelastic isotropic | Mooney–Rivlin with c1 = 30.1 MPa c2 = −27.1 MPa |
| Iliotibial band LET | Hyperelastic isotropic | Mooney–Rivlin with c1 = 30.1 MPa c2 = −27.1 MPa |
| Septum | Rigid | Young modulus = 0.4 GPa Poisson coefficient = 0.33 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yañez, R.; Silvestre, R.; Roby, M.; Neira, A.; Madera, S.; De la Fuente, C. Exploratory Anterior Cruciate Ligament Graft Stress during Medial Knee Rotation with and without Iliotibial Band–Intermuscular Septum Lateral Extra-Articular Tenodesis for Transtibial and Anteromedial Femoral Tunnels. Appl. Sci. 2024, 14, 5160. https://doi.org/10.3390/app14125160
Yañez R, Silvestre R, Roby M, Neira A, Madera S, De la Fuente C. Exploratory Anterior Cruciate Ligament Graft Stress during Medial Knee Rotation with and without Iliotibial Band–Intermuscular Septum Lateral Extra-Articular Tenodesis for Transtibial and Anteromedial Femoral Tunnels. Applied Sciences. 2024; 14(12):5160. https://doi.org/10.3390/app14125160
Chicago/Turabian StyleYañez, Roberto, Rony Silvestre, Matias Roby, Alejandro Neira, Samuel Madera, and Carlos De la Fuente. 2024. "Exploratory Anterior Cruciate Ligament Graft Stress during Medial Knee Rotation with and without Iliotibial Band–Intermuscular Septum Lateral Extra-Articular Tenodesis for Transtibial and Anteromedial Femoral Tunnels" Applied Sciences 14, no. 12: 5160. https://doi.org/10.3390/app14125160






