Fracture and Deflection of Orthodontic Miniscrews—A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Data Extraction
2.4. Risk of Bias Assessment
3. Results
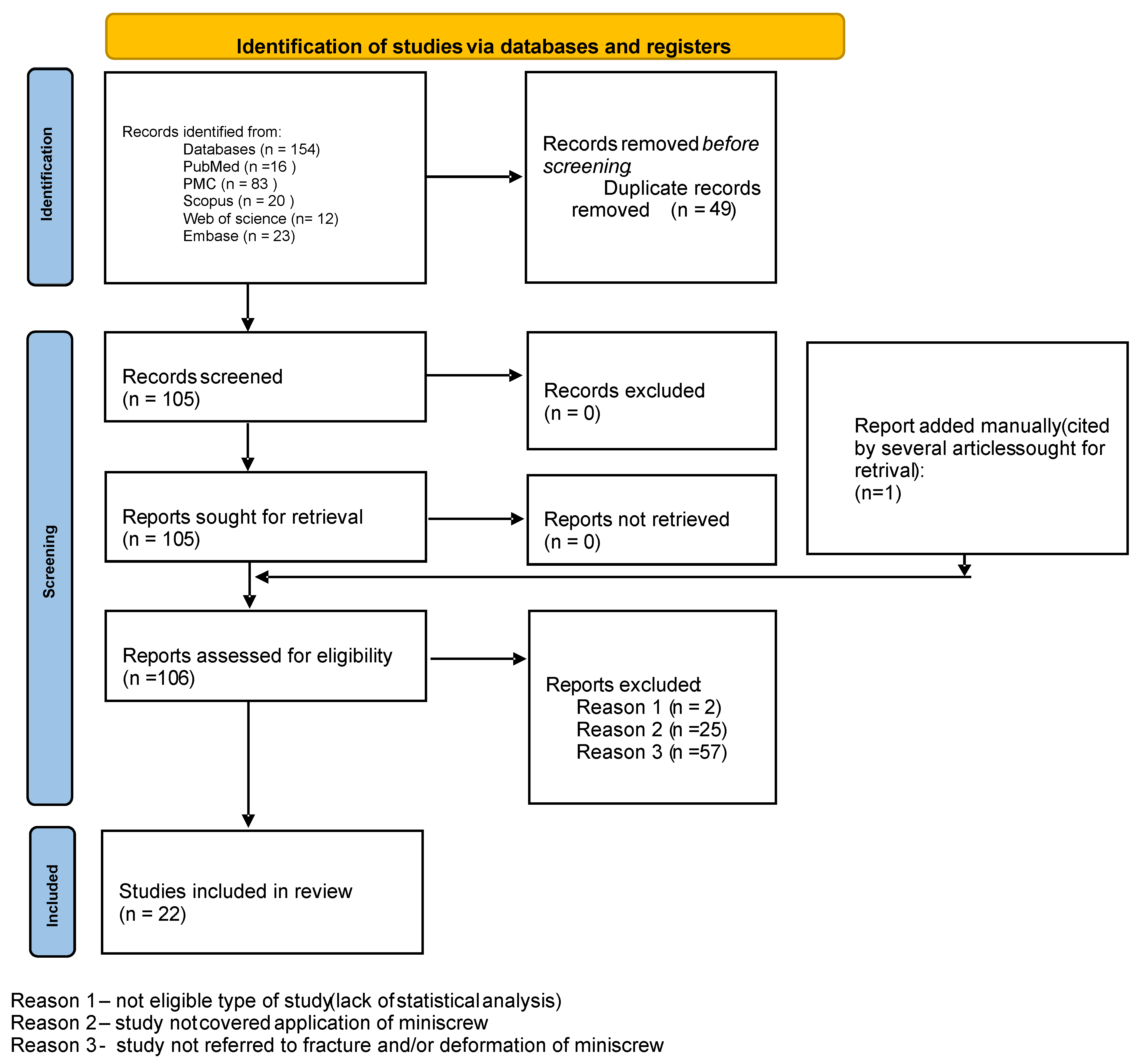
3.1. Search Results
3.2. Risk of Bias Assessment
4. Discussion
Limitations
5. Conclusions
- The most important factor influencing miniscrews’ plastic deformation and fracture was screw diameter.
- The fracture and deflection resistance of MSs increased with diameter. The length did not influence MS properties significantly.
- Both length and diameter should be selected in accordance with the anatomical conditions of the clinical site.
- Partial insertion of the MS increases the fracture and deformation risk.
- The alloy used in MSs does not influence deformation or fracture significantly.
- If the cortical bone thickness of the insertion site exceeds 3 mm, pre-drilling is recommended.
- Orthodontic MSs should not be reused (tip deformation occurs and cutting ability is reduced, increasing the risk of fracture).
- High-quality clinical studies are needed for suitable scientific evidence on the subject of MS deformation.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data availability statement
Conflicts of Interest
References
- Francioli, D.; Ruggiero, G.; Giorgetti, R. Mechanical properties evaluation of an orthodontic miniscrew system for skeletal anchorage. Prog. Orthod. 2010, 11, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Tepedino, M.; Masedu, F.; Chimenti, C. Comparative evaluation of insertion torque and mechanical stability for self-tapping and self-drilling orthodontic miniscrews—An in vitro study. Head Face Med. 2017, 13, 10. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.; Hosein, Y.K.; Dunning, C.E.; Tassi, A. Fracture resistance of commonly used self-drilling orthodontic mini-implants. Angle Orthod. 2015, 85, 26–32. [Google Scholar] [CrossRef]
- Scribante, A.; Montasser, M.A.; Radwan, E.S.; Bernardinelli, L.; Alcozer, R.; Gandini, P.; Sfondrini, M.F. Reliability of Orthodontic Miniscrews: Bending and Maximum Load of Different Ti-6Al-4V Titanium and Stainless Steel Temporary Anchorage Devices (TADs). Materials 2018, 11, 1138. [Google Scholar] [CrossRef] [PubMed]
- Quraishi, E.; Sherriff, M.; Bister, D. Peak insertion torque values of five mini-implant systems under different insertion loads. J. Orthod. 2014, 41, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Reicheneder, C.; Rottner, K.; Bokan, I.; Mai, R.; Lauer, G.; Richter, G.; Gedrange, T.; Proff, P. Mechanical loading of orthodontic miniscrews—Significance and problems: An experimental study. Biomed. Tech. 2008, 53, 242–245. [Google Scholar] [CrossRef] [PubMed]
- Cho, I.S.; Kim, T.W.; Ahn, S.J.; Yang, I.H.; Baek, S.H. Effects of insertion angle and implant thread type on the fracture properties of orthodontic mini-implants during insertion. Angle Orthod. 2013, 83, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Chung, C.J.; Jung, K.Y.; Choi, Y.J.; Kim, K.H. Biomechanical characteristics and reinsertion guidelines for retrieved orthodontic miniscrews. Angle Orthod. 2014, 84, 878–884. [Google Scholar] [CrossRef] [PubMed]
- Lopes, G.B.; Pithon, M.M.; Mordente, C.M.; Nojima, L.I.; Horta, M.C.R.; Oliveira, D.D.; Soares, R.V. Mechanical properties of mini-implants used in extra-radicular anchorage. Pesqui. Bras. Odontopediatria Clín. Integr. 2023, 23, 2101–2155. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar]
- Hooijmans, C.R.; Rovers, M.M.; de Vries, R.B.M.; Leenaars, M.; Ritskes-Hoitinga, M.; Langendam, M.W. SYRCLE’s Risk of Bias Tool for Animal Studies. BMC Med. Res. Methodol. 2014, 14, 43. [Google Scholar] [CrossRef]
- Sheth, V.H.; Shah, N.P.; Jain, R.; Bhanushali, N.; Bhatnagar, V. Development and Validation of a Risk-of-Bias Tool for Assessing in Vitro Studies Conducted in Dentistry: The QUIN. J. Prosthet. Dent. 2024, 131, 1038–1042. [Google Scholar] [CrossRef] [PubMed]
- Alavi, S.; Asadi, F.; Raji, S.A.H.; Samie, S. Effect of steam and dry heat sterilization on the insertion and fracture torque of orthodontic miniscrews. Dent. Res. J. 2020, 17, 219–224. [Google Scholar]
- Assad-Loss, T.F.; Kitahara-Céia, F.M.F.; Silveira, G.S.; Elias, C.N.; Mucha, J.N. Fracture strength of orthodontic mini-implants. Dental Press. J. Orthod. 2017, 22, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Barros, S.E.; Vanz, V.; Chiqueto, K.; Janson, G.; Ferreira, E. Mechanical strength of stainless steel and titanium alloy mini-implants with different diameters: An experimental laboratory study. Prog. Orthod. 2021, 22, 9. [Google Scholar] [CrossRef]
- Barros, S.E.; Janson, G.; Chiqueto, K.; Garib, D.G.; Janson, M. Effect of mini-implant diameter on fracture risk and self-drilling efficacy. Am. J. Orthod. Dentofacial Orthop. 2011, 140, 181–192. [Google Scholar] [CrossRef]
- Fabi, B.A.J.; Ahmed, V.K.S.; Krishnaswamy, N.R.; Thavarajah, R. Morphologic changes in miniscrew implant after root contact and the mechanical risks of its reinsertion. AJO-DO Clin. Companion 2022, 2, 2–10. [Google Scholar] [CrossRef]
- Hosein, Y.K.; Smith, A.; Dunning, C.E.; Tassi, A. Insertion Torques of Self-Drilling Mini-Implants in Simulated Mandibular Bone: Assessment of Potential for Implant Fracture. Int. J. Oral Maxillofac. Implants 2016, 31, 57–64. [Google Scholar] [CrossRef]
- Kang, H.K.; Chu, T.M.; Dechow, P.; Stewart, K.; Kyung, H.M.; Liu, S.S. Laser-treated stainless steel mini-screw implants: 3D surface roughness, bone-implant contact, and fracture resistance analysis. Eur. J. Orthod. 2016, 38, 154–162. [Google Scholar] [CrossRef]
- Pithon, M.M.; Figueiredo, D.S.; Oliveira, D.D. Mechanical evaluation of orthodontic mini-implants of different lengths. J. Oral Maxillofac. Surg. 2013, 71, 479–486. [Google Scholar] [CrossRef]
- Reimann, S.; Ayubi, M.; McDonald, F.; Bourauel, C. Experimental investigation of the fracture torque of orthodontic anchorage screws. J. Orofac. Orthop. 2016, 77, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Santos, R.F.; Ruellas, A.C.; Fernandes, D.J.; Elias, C.N. Insertion torque versus mechanical resistance of mini-implants inserted in different cortical thickness. Dental Press J Orthod. 2014, 19, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Serra, G.; Morais, L.; Elias, C.N.; Semenova, I.P.; Valiev, R.; Salimgareeva, G.; Pithon, M.; Lacerda, R. Nanostructured severe plastic deformation processed titanium for orthodontic mini-implants. Mater. Sci. Eng. C Mater. Biol. Appl. 2013, 33, 4197–4202. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Gandini, P.; Alcozer, R.; Vallittu, P.K.; Scribante, A. Failure load and stress analysis of orthodontic miniscrews with different transmucosal collar diameter. J. Mech. Behav. Biomed. Mater. 2018, 87, 132–137. [Google Scholar] [CrossRef]
- Walter, A.; Winsauer, H.; Marcé-Nogué, J.; Mojal, S.; Puigdollers, A. Design characteristics, primary stability and risk of fracture of orthodontic mini-implants: Pilot scan electron microscope and mechanical studies. Med. Oral Patol. Oral Cir. Bucal 2013, 18, 804–810. [Google Scholar] [CrossRef] [PubMed]
- Wilmes, B.; Panayotidis, A.; Drescher, D. Fracture resistance of orthodontic mini-implants: A biomechanical in vitro study. Eur. J. Orthod. 2011, 33, 396–401. [Google Scholar] [CrossRef]
- Patil, P.; Kharbanda, O.P.; Duggal, R.; Das, T.K.; Kalyanasundaram, D. Surface deterioration and elemental composition of retrieved orthodontic miniscrews. Am. J. Orthod. Dentofacial Orthop. 2015, 147, 88–100. [Google Scholar] [CrossRef]
- Velasco-Ortega, E.; Jos, A.; Cameán, A.M.; Pato-Mourelo, J.; Segura-Egea, J.J. In vitro evaluation of cytotoxicity and genotoxicity of a commercial titanium alloy for dental implantology. Mutat. Res. 2010, 702, 17–23. [Google Scholar] [CrossRef]
| Author and Year | Type of Study | No of Subjects | Comparison Made | Measurement Unit | Results |
|---|---|---|---|---|---|
| Alavi S. et al., 2020 [14] | Experimental study (in vitro) | 36 | - Change in insertion and fracture torques after steam and dry heat sterilization. | N.cm | - Steam sterilization had no effect on fracture torque and insertion torque values. - Dry heat sterilization lowered fracture torque value - Steam sterilization had no detrimental effects on torque values of miniscrews; dry heat sterilization affected their mechanical properties. |
| Assad-Loss T.F. et al., 2017 [15] | Experimental research (in vitro) | 50 | Five brands of titanium alloy MS: - Design and dimensions; - Torsional fracture strength in the neck and the tip; - Insertion torque values. | N.cm µm | - Fracture torque of the neck: 23.45 N.cm 34.82 N.cm, of the tip: 9.35 N.cm (CON) to 24.36 N.cm (NEO). - Insertion torque values ranged from 6.6 N.cm (RMO) to 10.2 N.cm (NEO). - Fracture torque resistance is determined by: outside diameter, internal diameter, ratio of inner and outer diameter, and milling in the apical region. - The fracture torques of both the tip and neck were higher than the torque required to insert MSs. |
| Barros S.E. et al., 2021 [16] | Experimental research (in vitro) | 252 (SS-MS) 252 (TiA-MS) | - Two MS alloys: stainless steel (SS-MS) and titanium alloy (TiA-MS); - Correlation of MS diameter (1.2–1.8 mm) with torsional fracture and deflection resistance; - Thread resistance to morphological damage after insertion. | N.cm (fracture torque) N (flexural force) | - SS-MSs were 13.2% and 20.2% more resistant to torsional fracture and deflection. - MS diameter explained 90.3% of the total variation in fracture torque, 2.2% was explained by the metallic alloy. - Flexural strength of SS and TiA-MSs at 1 mm and 2 mm deflection was 18.21 N and 17.55 N. - No noticeable morphological damage to the threads of SS-MSs and TiA-MSs. - The use of SS-MSs can reduce the fracture risk without increasing the MS diameter. |
| Barros S.E, Janson G, et al., 2011 [17] | Experimental research (in vitro) | 405 | - Correlation of MS diameter (1.2–2 mm) with placement torque value, axial placement load, fracture torque value, and self-drilling efficacy. | N.cm | - Increases in MS diameter increased the placement torque and fracture torque, which reduced the fracture risk. - The self-drilling efficacy was not strongly influenced by diameter. |
| Cho I-S. et al., 2013 [7] | Experimental study (in vitro) | 100 | Different insertion angles and MS thread types (single, dual). - Insertion torque, total insertion energy, and peak time. | N.cm, J, s | - Increase in insertion angle increased insertion torque values in both thread groups. - Dual-thread MS: more fracturing than deformation compared to single-thread MSs. |
| Chung CJ et al., 2014 [8] | Experimental study (in vitro) | 84 | - Unused and retrieved MSs: deformation of the tip, changes in insertion torque, insertion time, and insertion load; - Surface composition analysis of retrieved MSs. | N µm | - Tip deformation was found in 84.5% of retrieved MSs. - Insertion site or duration of insertion not associated with tip deformation. - Insertion load increased with tip deformation. - Changes in insertion torque similar to unused MSs. - Debris of carbon, calcium, and phosphorus on the MSs. - MSs retrieved exhibited decreased cutting ability due to deformation of the tip structure and surface contamination. |
| Fabi B.A.J, 2022 [18] | Experimental research (in vitro) | 150 | - Insertion torque of 3 types of TiA-MS vs. the insertion torque of the retrieved MS after root contact; - Structural and dimensional changes in as-received MSs and retrieved MSs after root contact (SEM). | N.cm µm | Deformation of MS upon root contact: dimensional changes (blunting) in the MS tip and threads, decreased cutting ability on reinsertion, increase in maximum torque insertion value - Excessive insertion force may hinder soft tissue healing, cause MS fracture, and induce microcracks and bone damage. |
| Francioli D., 2010 [1] | Experimental study (in vitro) | 10 (ø1.5 mm) 10 (ø2 mm) | SS-MS: - Torsional resistance; - Flexural strength. | N.cm N | Torsional resistance: Ø1.5 mm: 26.5 N.cm, ø2 mm: 48.3 N.cm. Flexural strength: ø1.5 mm: 105,4 N, ø2 mm: 216.7 N. Higher fracture and deformation resistance for higher diameter. |
| Hosein Y.K., 2016 [19] | Experimental study (in vitro) | 60 | Six MS systems (Aarhus, Dual-top, OrthoEasy, Thomas-pin, Unitek, VectorTAS). - Torque ratio as fracture potential (insertion torque as % of fracture torque) in 3 mm cortical bone. | N.cm % | Highest ratio: Aarhus MS. Lowest ratio: Unitek. - Safe use of Unitek, VectorTAS, OrthoEasy, Dual-top in 3 mm bone without pre-drilling |
| Kang H-K, 2016 [20] | Research animal study (experimental in vitro) | 48 | SS-MS: - Machined vs. Nd-YAG laser surface-treated. - Surface roughness, texture, fracture resistance, bone–implant contact (BIC). | N.cm µm | - Higher surface roughness of laser-treated MSs. - No significant differences in fracture resistance and BIC between the two groups. - Laser treatment increased surface roughness without compromising fracture resistance. Despite increasing surface roughness, laser treatment did not improve bone–implant contact. |
| Lopes G.B., 2023 [9] | Experimental study (in vitro) | 72 (24 per group) | Two MS alloys: stainless steel (SS-MS) ø1.5 mm and ø2 mm and titanium alloy (TiA-MS) ø1.5 mm. - Insertion torque, fracture torque, pull-out, degree of mobility on percussion, MS fracture pattern. | N/cm² | - Insertion torque and fracture torque similar for ø1.5 mm MI, higher for ø2 mm MI. - Pull-out and percussion tests presented similar values. - Fracture point was predominantly on 4th thread for SS-MS and on the 7th thread for TiA-MSs. |
| Pithon M.M., 2013 [21] | Experimental study (in vitro) | 405 | MSs of different lengths: 6, 8, 10 mm: - Cortical bone thicknesses (1–6 mm); - Insertion torque, fracture torque, deformation. | N/cm² | - Insertion torque increased with screw length and cortical bone thickness. - Length of MSs did not influence fracture strength on insertion, flexural strength, fracture strength on flexion - Increase in screw length does not increase the mechanical strength of the implant. |
| Quraishi E., 2014 [5] | Experimental study (in vitro) | 40 | Five MI systems: - Max insertion torque under 1 and 3 kg load (fracture risk). | N.cm | MSs of cylindrical and mixed designs fractured at higher torque values compared to tapered designs for both loads of 1 and 3 kg. - Pressure of 3 kg increased risk of bending tapered MS before fracture. |
| Reicheneder C., 2008 [6] | Experimental study (in vitro) | 50 | Five MS systems: - Plastic deformation under insertion and flexural loading. - Material composition of MSs. | mm | - All systems: deformations of approximately 0.15–0.25 mm, depending on the insertion depth. - Comparable elemental composition. - Differences in mechanical properties are attributed to screw design; partial insertion increases fracture risk upon flexural loading. |
| Reimann S., 2016 [22] | Experimental study (in vitro) | 17 | Eight MS systems: - Fracture torque; - Deformation torque. | N.cm | - Fracture torque increased with the increase in MS diameter. - Plastic deformation often occurred below the industrial standard torque values (20 N.cm). |
| Santos R., 2014 [23] | Experimental study (in vitro) | 10 | - Insertion torque of MSs in different cortical thicknesses; - Resistance to fracture of MS tip and neck; - MS surface morphology before and after mechanical test. | N.cm | - Insertion torque for 1 mm (7.60 N.cm) and 2 mm (13.27 N.cm) cortical thicknesses. - Mechanical resistance to fracture (tip 22.14 N.cm and neck 54.95 N.cm): higher than insertion torque. - No changes in MS surface morphology before and after tests. - Safe placement of MS in 1 and 2 mm cortical thickness; in 3 mm and dense bones, authors recommend pre-drilling before insertion. |
| Scribante A., 2018 [4] | Experimental study (in vitro) | 70 | Two MS alloys: stainless steel (SS-MS) and titanium alloy (TiA-MS) ø1.5 mm and ø2 mm. - Deflection and maximum load. | N | - MSs of ø2 mm showed higher bending and fracture resistance than ø1.5 mm diameter MSs. - No significant differences between TiA-MSs and SS-MSs with the same diameter. |
| Serra G., 2013 [24] | Experimental study (material research) | 15 | Three MS materials: commercially pure titanium (cpTi), Ti-6Al-4V alloy, nanostructured titanium (nTi). - Maximum torque resistance, surface morphology, fracture surface characteristics. | N.mm | - Maximum torque resistance of nTi higher than cpTi, similar to Ti-6Al-4V. - Similar surface finishing and fracture processes among the 3 types of MSs. |
| Sfondrini M.F., 2018 [25] | Experimental study (in vitro) | 70 | Seven diameters of Ti-6Al-4V miniscrews: forces to bend at 0.1 mm, 0.2 mm magnitude of deflections and at maximum load. | N | - At 0.1 mm or 0.2 mm deflections and at maximum load, highest forces were reported with 1.7, 1.8, 1.9, and 2.0 mm TADs. - The lowest values were reported with 1.6, 1.5, and 1.3 mm MSs. - No significant differences between 1.6 mm and 1.7 mm screws. |
| Smith A., 2015 [3] | Experimental study (in vitro) | 90 | Six brands of titanium MS (ø1.4–1.8 mm): fracture torques during insertion. | N.cm | Unitek (72 N.cm) > Tomas-pin (36 N.cm) > Dual-Top (32 N.cm) ≈ VectorTAS (31 N.cm) > OrthoEasy (28 N.cm) > Aarhus (25 N.cm). Weak correlation between mini-implant diameter and fracture resistance. |
| Walter A., 2013 [26] | Experimental study (in vitro) | 12 | Twelve designs of MS: - Design (shape); - Pullout strength, insertion torques and, torsional fracture. | Mm N.cm | - Cylindrical MSs: higher pull-out strength, lower insertion torque values. - Outer and inner MS diameters correlated with pull-out strength, insertion torque, and torsional fracture values. - Greater thread depth was related to greater pull-out strength values. - Torsional fracture depended on the MS inner and outer diameters. - Thread-depth-to-outer-diameter ratio increased torsional fracture risk by 40%. - MS outer and inner diameters are the most important factors for primary stability. |
| Wilmes B.,Panayotidis A., 2011 [27] | Experimental study (in vitro) | 41 | Different designs and diameters of MSs: - Insertion and fracture torque (with pre-drilling). | N.mm | - Fracture torque varied depending on MS design. - Increasing fracture torque value with increased MS diameter. |
| Criteria No. | Criteria | Alavi S., 2020 [14] | Assad-Loss T.F, 2017 [15] | Barros S.E, 2021 [16] | Barros S.E, Janson G, 2011 [17] | Cho I-S., 2013 [7] | Chung CJ, 2014 [8] | Fabi B.A.J, 2022 [18] | Francioli D., 2010 [1] | Hosein Y.K., 2016 [19] | Kang H-K, 2016 [20] |
| 1 | Clearly stated aims/objectives | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 2 | Detailed explanation of sample size calculation | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 3 | Detailed explanation of sampling technique | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 1 | 2 | 2 |
| 4 | Details of comparison group | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 5 | Detailed explanation of methodology | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 1 | 2 | 2 |
| 6 | Operator details | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 2 | 2 |
| 7 | Randomization | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| 8 | Method of measurement of outcome | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 9 | Outcome assessor details | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 |
| 10 | Blinding | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 11 | Statistical analysis | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 12 | Presentation of results | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 13 | Overall | high | low | medium | medium | high | medium | medium | high | medium | low |
| Criteria No. | Criteria | Lopes G.B., 2023 [9] | Pithon M.M., 2013 [21] | Quraishi E., 2014 [5] | Reicheneder C., 2008 [6] | Reimann S., 2016 [22] | Santos R., 2014 [23] | Scribante A., 2018 [4] | Serra G., 2013 [24] | Sfondrini M.F., 2018 [25] | Smith A., 2015 [3] |
| 1 | Clearly stated aims/objectives | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 2 | Detailed explanation of sample size calculation | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 |
| 3 | Detailed explanation of sampling technique | 1 | 2 | 2 | 1 | 2 | 2 | 1 | 1 | 1 | 2 |
| 4 | Details of comparison group | 2 | 2 | - | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 5 | Detailed explanation of methodology | 1 | 2 | 2 | 1 | 2 | 1 | 1 | 1 | 1 | 2 |
| 6 | Operator details | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 7 | Randomization | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 8 | Method of measurement of outcome | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 9 | Outcome assessor details | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 10 | Blinding | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 11 | Statistical analysis | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 12 | Presentation of results | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 13 | Overall | high | medium | medium | high | medium | medium | medium | high | medium | medium |
| Criteria No. | Criteria | Walter A., 2013 [26] | Wilmes B., Panayotidis A., 2011 [27] | ||||||||
| 1 | Clearly stated aims/objectives | 2 | 2 | ||||||||
| 2 | Detailed explanation of sample size calculation | 2 | 0 | ||||||||
| 3 | Detailed explanation of sampling technique | 2 | 2 | ||||||||
| 4 | Details of comparison group | 2 | 2 | ||||||||
| 5 | Detailed explanation of methodology | 2 | 2 | ||||||||
| 6 | Operator details | 0 | 0 | ||||||||
| 7 | Randomization | 0 | 0 | ||||||||
| 8 | Method of measurement of outcome | 2 | 2 | ||||||||
| 9 | Outcome assessor details | 0 | 0 | ||||||||
| 10 | Blinding | 0 | 0 | ||||||||
| 11 | Statistical analysis | 2 | 0 | ||||||||
| 12 | Presentation of results | 2 | 2 | ||||||||
| 13 | Overall | medium | high | ||||||||
| Author and Year | Kang H-K, 2016 [20] |
|---|---|
| Selection bias | Not present. |
| Performance bias | Not present. |
| Detection bias | There was no sample size calculation or blinding. |
| Attrition bias | There was no description of who performed the measurements and whether they were repeated. |
| Reporting bias | Not present. |
| Other biases | Not present. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stefaniak, K.; Jedliński, M.; Mazur, M.; Janiszewska-Olszowska, J. Fracture and Deflection of Orthodontic Miniscrews—A Systematic Review. Appl. Sci. 2024, 14, 5577. https://doi.org/10.3390/app14135577
Stefaniak K, Jedliński M, Mazur M, Janiszewska-Olszowska J. Fracture and Deflection of Orthodontic Miniscrews—A Systematic Review. Applied Sciences. 2024; 14(13):5577. https://doi.org/10.3390/app14135577
Chicago/Turabian StyleStefaniak, Katarzyna, Maciej Jedliński, Marta Mazur, and Joanna Janiszewska-Olszowska. 2024. "Fracture and Deflection of Orthodontic Miniscrews—A Systematic Review" Applied Sciences 14, no. 13: 5577. https://doi.org/10.3390/app14135577









