Abstract
Background: An increasing number of people around the world suffer from Crohn’s disease (CD), one of the inflammatory bowel diseases (IBDs). Recent evidence suggests that the endogenous cannabinoid system plays an important role in IBD. The main endocannabinoids, anandamide (AEA) and 2-arachidonoylglycerol (2-AG), are ligands of the CB1 and CB2 receptors that are expressed on immune cells. These receptors as well as endocannabinoids are believed to mediate inflammatory activity and participate in the pathophysiology of CD. Objective: Very little is known about the secretion of endogenous cannabinoids throughout the course of CD. Therefore, the aim of this study was to determine and analyze the 2-AG and AEA concentrations in children who suffered from CD. Methods: We studied 34 adolescents with CD, mean age 13.5 years ± 2.0. Blood samples were collected three times in the active phase of the disease (during admission to hospital, before treatment), 2–4 weeks later, during the treatment and clinical improvement of the patients, and 3–6 months later, in the period of remission. The control group included 33 healthy teenagers of the same age who were examined once. In all patients, fasting blood samples were collected in the morning. 2AG and AEA concentrations in serum were measured using EIA kits (Abclonal, Woburn, MA, USA and ELK Biotechnology Co., Ltd. Wuhan, China, respectively). Results: The median 2-AG concentration in the study group was stable: acute phase 907.4 [379.3; 1300.5] pg/mL, during treatment 715.1 [416.7; 1302.5] pg/mL; remission 991.1 [381.1; 1652.5] pg/mL, and similar to the values observed in the control group 761.8 [504.3; 1497.0] pg/mL. No significant differences were found between the results obtained at all time points in the study group and compared to the control group (in all cases p > 0.44). In the case of AEA, in the study group before treatment, the median concentration was 2.63 [2.24; 2.79] ng/mL and similar to values obtained during treatment 2.56 [2.33; 3.06] ng/mL, and in remission, with 2.61 [2.46; 2.85] ng/mL. All these concentrations were lower compared to the values measured in the control group of 3.18 [2.57; 3.88] ng/mL (p = 0.023, p = 0.035, p = 0.056, respectively). Conclusions: While 2-AG levels remained stable throughout the disease course and were comparable to controls, AEA concentrations were consistently lower in CD patients. Therefore, therapeutic interventions aimed at increasing AEA-related signaling, such as administration of its analogues or fatty acid amide hydrolase inhibitors, may improve symptoms associated with Crohn’s disease in children.
1. Introduction
Crohn’s disease (CD) poses a significant challenge to healthcare systems in many countries. It is estimated that the incidence of CD ranges from 5 to 20.2/100,000 cases per year depending on the region of the world [1]. The highest incidence rates are recorded in highly developed countries, especially in Europe and North America [2]. Although the peak incidence occurs in the second and third decade of life, CD in children and adolescents accounts for approximately one-fourth of all cases [3]. The first symptoms of CD are often atypical and include abdominal pain and diarrhea [4]. Patients may also suffer from abdominal pain of various locations and intensity, and chronic diarrhea. The latter may result in developmental disorders in children and nutritional deficiencies [5]. All these symptoms might significantly reduce the quality of life of CD patients. Several theories exist as to the cause of the disease, but the most current theory on the pathogenesis of IBD suggests a loss of tolerance to the intestinal microbiota and abnormal bacteria–host interactions that induce an autoimmune response and promote inflammation in the gut [6,7,8].
The endocannabinoid system (ECS) consists of three main parts: receptors, endogenous agonists, and cannabinoid-degrading enzymes. There are two classical types of G protein-coupled metabotropic receptors, type 1 and 2 [9,10]. The type 1 cannabinoid receptor (CB1) is mainly present on the cells of the central nervous system (CNS) but can also be found in other parts of the body, such as the gastrointestinal tract (GI tract) and vascular endothelium [11]. Type 2 cannabinoid receptor (CB2) is expressed mostly on cells and organs of the immune system, such as macrophages, leukocytes, spleen, tonsils, and thymus. CB2 seems to be highly inducible, with its concentration in the CNS increasing many times during inflammation, although it is not clear whether this increase is due to CB2-expressing immune cell migration or to increased expression of the receptor on CNS cells [9]. Both receptors are also common in the gastrointestinal tract, especially in enteric nerves and enteroendocrine cells [12,13]. The effects of CB1 and CB2 stimulation are complex and often overlapping; primarily, CB1 stimulation increases reactive oxygen species (ROS) and tumor necrosis factor α (TNF-α) production and induces M1 macrophage (classically activated by IFN-γ or lipopolysaccharide (LPS)) polarization. CB2 enhances macrophage polarization toward the M2 form (alternatively activated by cytokines) and reduces proinflammatory cytokine secretion from T-cells [14]. Apart from said receptors, there are also several poorly understood orphan receptors, such as GPR3, GPR55, and GPR84.
Endogenous cannabinoids (eCBs) are derivatives (esters and amides) of long-chain polyunsaturated fatty acids and they act through described specific receptors. The two most important among them are 2-arachidonoylglycerol (2-AG) and anandamide (AEA). They are synthesized by enzymes: diacylglycerol lipase (DAGL) and N-acyl-phosphatidylethanolamine phospholipase (NAPE-PLD), respectively [15]. 2-AG has a high affinity toward both CB1 and CB2 receptors, while AEA binds preferably to the CB1 receptor and has a low affinity for CB2 [14]. AEA can also inhibit neutrophil recruitment and thus reduce inflammation [16].
Two main enzymes responsible for endocannabinoid degradation are monoacylglycerol lipase (MAGL) and fatty acid amide hydrolase (FAAH). 2-AG is primarily metabolized by MAGL, which hydrolyses about 85% of 2-AG in the brain, thus being the most important 2-AG-degrading enzyme in the CNS [17]. The FAAH enzyme metabolizes AEA but is also capable of breaking down 2-AG to some extent.
According to research, exposure to chronic stress impacts the homeostasis of the endocannabinoid system. The release of corticotropin-releasing hormone (CRH) by the pituitary gland changes the activity of the FAAH enzyme, resulting in a decrease in AEA levels. It has been discovered that the rise of 2-AG is linked to an increase in cortisol levels. It was also suggested that during exposition to stress, endogenous cannabinoids have the capability of modulating visceral hyperalgesia—an increase in the perception of visceral pain [15,18]. The ECS’s actions also participate in the regulation of motility and inflammation in the GI tract.
Autoregulation of the endocannabinoid system is also closely associated with the gut microbiome. Although the exact nature of this relationship is still for the most part unknown, a study conducted in 2007 by Rousseaux et al. proved the oral administration of L. acidophilus NCFM strain induced a significant increase in CNR2 (cannabinoid receptor type 2) mRNA in epithelial cells [19]. Experiments on healthy mice showed that antibiotic treatment caused a significant reduction of the CB1 receptor in the colon. Altering the gut microbiota using prebiotics also influenced the level of FAAH and MGL mRNA in obese mice [20]. This relation between gut microbiota and endocannabinoids also functions in the opposite direction; a study by Dione et al. showed that MAGL-deficient mice had different levels of certain bacterial strains (Hydrogenoanaerobacterium, Roseburia, and Ruminococcus) than wild-type mice [21,22]. Further studies are needed on the topic, especially involving humans, but evidence gathered from mouse and cell models clearly prove a correlation between intestinal endocannabinoid tone and the composition of the gut microbiota. This might have important clinical implications, as several studies demonstrated that patients with CD exhibit dysbiosis, though the causality is yet to be proved [23,24].
Therapies that target the endogenous cannabinoid system have been in use for a considerable time, particularly in the form of cannabis use. The therapeutic effects of cannabis include the reduction in inflammation, visceral pain, and diarrhea, among others. Nonetheless, the primary role of cannabinoids is to control nausea and vomiting. This function is regulated by the activation of the CB1 receptor, which results in reduced cramping and slowed GI tract motility [25]. The widespread distribution of CB1 receptors throughout the body limits the applicability of treatments aimed at these receptors.
The purpose of our research was to determine the concentration of AEA and 2-AG in the blood of adolescent patients with CD. Our goal was also to make measurements in subsequent phases of the disease and analyze changes depending on CD activity in adolescents—from the moment of diagnosis, i.e., in the acute phase of the disease, during the period of clinical improvement caused by treatment, and in the period of remission.
2. Materials and Methods
2.1. Patients
Adolescents (aged 10–18) were recruited for the study from among hospitalized patients of the Department of Pediatrics, Gastroenterology, and Nutrition of the University Children’s Hospital in Krakow, according to a previously described protocol [26]. The key condition was newly diagnosed Crohn’s disease based on the revised Porto criteria, and no previous pharmacological or nutritional treatment prior to the current hospital stay [27]. In the group of CD patients, fasting blood was collected three times: in the active phase of the disease (CD1) before prescription of pharmacological treatment, up to 24 h after admission to the ward; 2–4 weeks after admission during the period of hospital treatment and clinical improvement (CD2); and in remission, 3–6 months after the hospital stay, during follow-up visits at the clinic (CD3). Age-matched adolescents from the researchers’ families and friends were recruited into the control group (C). These adolescents did not have any pathological clinical symptoms or complaints, and no pharmacological treatment was used. In the control group, blood was collected once, in the morning, on an empty stomach. All samples were immediately transferred to the hospital laboratory.
2.2. Laboratory Measurements
In the laboratory, the tubes with blood were centrifugated after 30 min required for coagulation (2000× g, 20 min, room temperature). The aliquots of serum were banked at −80 °C. The serum samples were stored no longer than 18 months. The endogenous cannabinoid levels were determined using commercially available immunoassays. The AEA kit was obtained from ELK Biotechnology Co. Ltd. (Wuhan, China), and 2-AG from Abclonal (Woburn, MA, USA).
Just before the measurements, the samples were slowly defrosted. In the first step, samples were transferred from deep freeze (−80 °C) to the −20 °C refrigerator for a night; later, just before the laboratory determination, serum samples were slowly thawed in ice water. Ten pilot sample measurements showed that sample dilution was not necessary. Testing procedures were conducted according to the manufacturer’s instructions using a Bio-Rad plate washer and reader (Hercules, CA, USA). As stated in kit leaflets by manufacturers, the used tests had high sensitivity and specificity and showed no significant cross-reactivity between the analytes and their metabolites or known analogues, or any significant interference from typical serum content.
The Helsinki Declaration has been followed for involving human subjects in the study. The protocol of the study was approved by the Jagiellonian University Bioethical Committee (decision no. 1072.6120.238.2019). Written informed consent was obtained from patients and their parents.
2.3. Statistical Analysis
Statistical analysis and graphs were performed using IBM SPSS Statistics 29.0 (IBM Armonk, NY, USA). Normality was checked by the Shapiro–Wilk test in each group. Except for ANA, concentrations of 2-AG and ANA in the remaining groups significantly differed from a normal distribution. Therefore, endogenous cannabinoid serum concentrations were shown as median and quartiles. The differences between the studied groups and the control group were checked by the Kruskal–Wallis test. In all analyses, a p value < 0.05 was considered statistically significant.
3. Results
3.1. Studied Groups
We recruited 34 adolescents hospitalized due to newly diagnosed CD (18 boys, 14 girls, mean age 13.5 ± 2.0 years). Patients received exclusive enteral nutrition using a semi-elemental diet for 6 weeks and 5-aminosalicylate (5-ASA, sulfasalazine, mesalamine) orally at a dose of 50 mg/kg. Participants from the studied group did not receive biological therapy (like anti-TNF alpha). Also, no systemic or local steroids, probiotics, as well as opioid analgesia were prescribed to the recruited patients, during the period of study observation. In all adolescents, 2-AG was tested in all, described above, time points, and in 20 patients chosen randomly from this group (12 boys, 8 girls, mean age 13.2 ± 2.2 years), AEA was measured in all time points. The control group comprised 33 healthy adolescents (12 boys and 21 girls, mean age 14.0 ± 2.5 years). In all controls, 2-AG was measured, and in 20 randomly chosen adolescents, AEA was tested. The latter subgroup consisted of 12 girls and 8 boys, with a mean age of 14.2 ± 2.7 years.
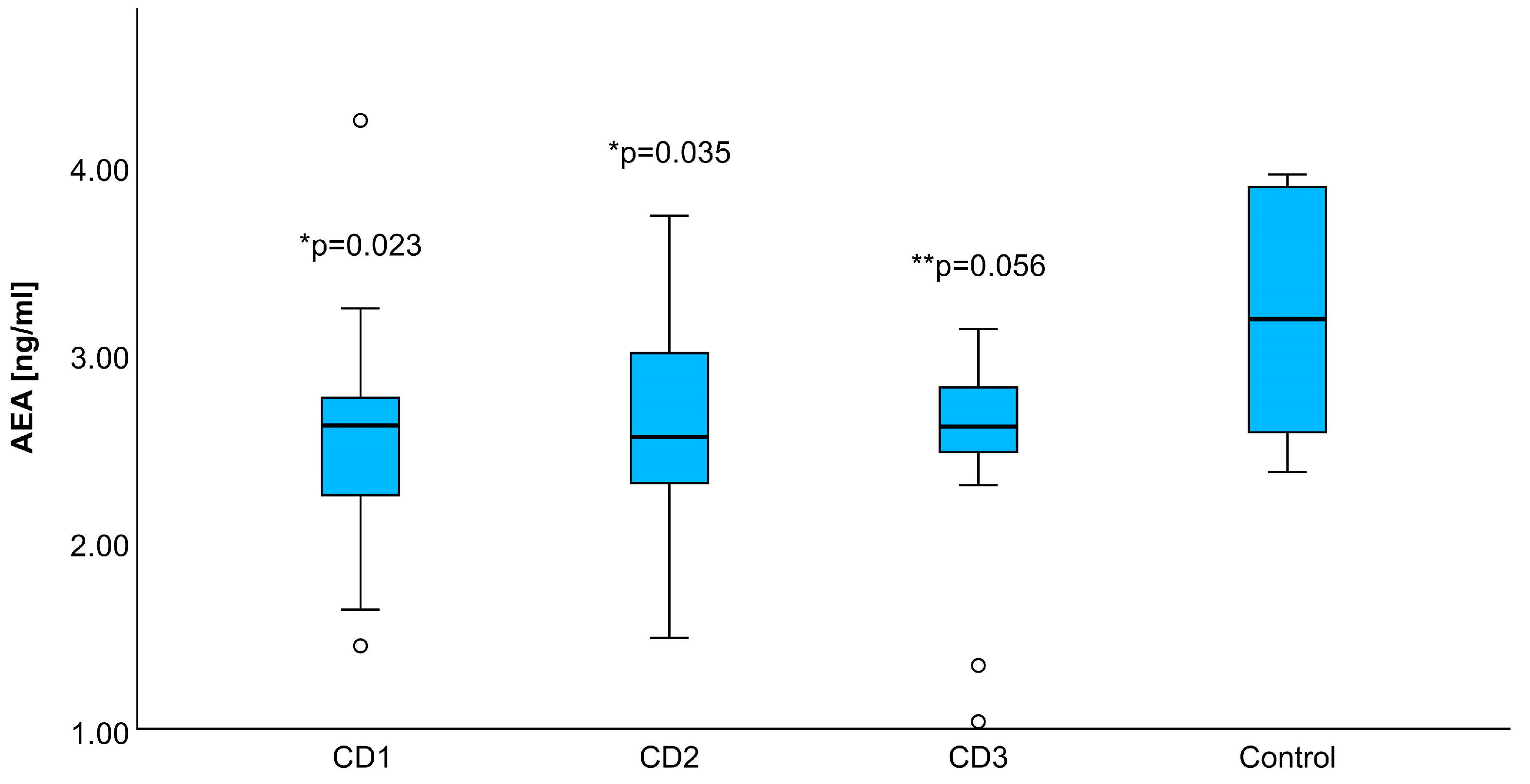
3.2. Anandamide
The serum concentration of AEA in the study group before treatment was 2.63 [2.24; 2.79] ng/mL, similar during the treatment 2.56 [2.33; 3.06] ng/mL, and in the remission-2.61 [2.46; 2.85] ng/mL. As illustrated in Figure 1, all AEA mean concentrations in the CD group were lower as compared to values observed in the control group—3.18 [2.57; 3.88] ng/mL. The results between the CD groups in every phase and the control group were statistically significant (CD1 vs. C p = 0.023, CD2 vs. C p = 0.035, CD3 vs. C p = 0.056 (at the border line of statistical significance)).
Figure 1.
Comparison of AEA levels shown as mean and quartiles across three phases of Crohn’s disease: acute phase (CD1), during the treatment (CD2), remission (CD3), and in the control group. * means the statistically significant difference between the studied group and controls. ** indicates the probability at the border line of statistical significance, ○ shows outliers.
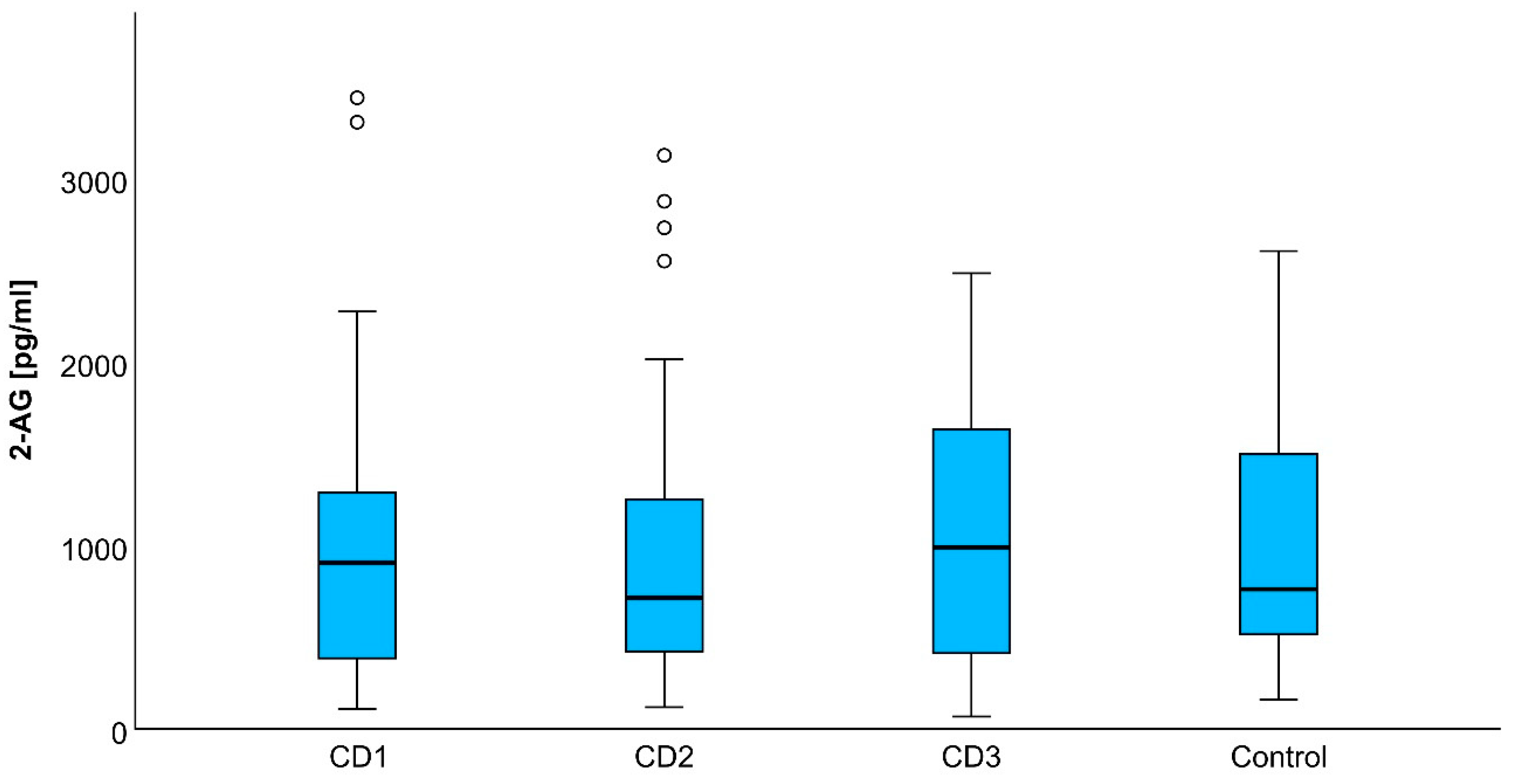
3.3. 2-Arachidonoylglycerol
The concentrations of 2-AG in the study group were stable—acute phase (CD1) 907.4 [379.3; 1300.5] pg/mL, during the treatment (CD2) 715.1 [416.7; 1302.5] pg/mL, remission (CD3) 991.1 [381.1; 1652.5] pg/mL, and similar to the values observed in the control group 761.8 [504.3; 1497.0] pg/mL (Figure 2). There were no significant differences between the results obtained at all examined time points in the study group and in comparison to the results in the control group (p > 0.44 in all cases).
Figure 2.
2-AG concentrations in studied groups shown as median and quartiles in the acute phase (CD1), during the treatment (CD2), remission (CD3), and in the control group. ○ shows outliers.
4. Discussion
In recent years, the endocannabinoid system (ECS) has been receiving increased interest from researchers due to its potentially beneficial effects on the physiological processes underlying chronic pain, psychiatric disorders, epilepsy, autoimmune diseases, and cancer. Recent studies have shown that altering the endocannabinoid system influences inflammation and immune responses within the gut, similar to the disturbances in the endoopioid system. Therefore, the endocannabinoid system is a potential therapeutic target in patients suffering from inflammatory bowel diseases (IBDs) [28].
Studies on endogenous cannabinoids in inflammatory bowel diseases have been rare, and results and conclusions are sometimes conflicting. Some studies have focused on patients with IBDs and summarized data from CD and ulcerative colitis (UC) [29,30]. Discrepancies may also result from the different types of samples, methods, and kits used for analysis, as well as the age of studied persons. Some researchers examined biopsies of inflamed intestinal tissue [29,31], while others have measured endocannabinoid concentrations in the serum or plasma [30].
The observed decrease in serum AEA levels which appeared in our study was also reported by Di Sabatino et al.; however, another study by Grill et al. reported increased levels of AEA in patients with CD [28,29]. There are different theories and proofs for the observed changes in endocannabinoid blood levels. Di Sabatino et al. examined the mucosal activity of the enzymes responsible for AEA synthesis and degradation, NAPE-PLD and FAAH. These researchers concluded that the cause of lowered AEA levels was decreased activity of NAPE-PLD and increased activity of FAAH. Grill et al. found an increase in both AEA and 2-AG levels in adults with CD by testing the eCB plasma levels [29]. The authors concluded that the decreased CB1 gene expression, which is the primary receptor for AEA, is the reason. The disparity in the results between studies should be an indication of the need for further research into the characteristics of AEA.
The lack of changes in the concentration of 2-AG, a representative of endocannabinoids in the course of CD, is puzzling. Similar observations were noted by Di Sabatino et al., with no statistically significant differences found between the control group and the group of patients with CD and UC in the concentration of 2-AG in the intestinal mucosa obtained during a biopsy or surgery in adults [28]. The researchers suggest that the real expression of 2-AG could be increased in IBD patients but is masked by an increased level of the enzymes responsible for the degradation of endocannabinoids, FAAH and MAGL. The other explanation is the decreased activity of NAPE-PLD.
In 2004, Massa et al. showed that CB1-deficient mice had more intensive inflammation during induced colitis than normal mice; the same results were observed when the CB1 receptor was pharmacologically blocked. Moreover, administration of cannabinoid receptor agonist resulted in protection against induced colitis in FAAH-deficient and wild mice [31]. It was noted that the administered cannabinoid receptor agonist also targeted other metabolic pathways, resulting in an anti-inflammatory mechanism. Nevertheless, the CB1 receptor plays a major role in the prevention of intestinal inflammation, based on observations in CB1-deficient mice. As AEA is a potent CB1 agonist, it is possible that the decrease in its serum concentration results in reduced anti-inflammatory activity on GI mucosa, thus resulting in more pronounced CD symptoms, and in patients in remission, facilitating recurrence of the disease. Sabatino et al. found the AEA concentration to be lower in IBD inflamed mucosa in comparison to IBD uninflamed mucosa, which implies some kind of self-reinforcing dysregulation inflammatory processes related to the EC system. Interestingly, the same study also found the CB1 receptor expression to be higher in the inflamed mucosa, which might be some kind of compensation for a lower concentration of AEA [28].
On the other hand, cannabinoids have also the ability to regulate intestinal motility by reducing smooth muscle contractility [32] and the rate of gastric emptying. This slowing of motility may be one of the factors behind some reports on the effectiveness of cannabis in reducing diarrhea, though such reports mostly rely on patient-reported outcomes. The positive effect of cannabinoids (exo- and endogenous) in the course of CD also includes the stimulating effect on the appetite center, which is especially important in the period of remission [32,33]. It is estimated that 65 to 75% of CD patients suffer from malnutrition. Depending on the severity of the course of CD and the duration of the disease, secondary symptoms associated with the malabsorption syndrome may appear, such as electrolyte disturbances, anemia, avitaminosis, especially B12, and hypoproteinemia. In pediatric patients, malnutrition is the main cause of growth retardation [34,35]. Additionally, a decrease in bone mineral density is often noticed in CD patients, which may be related to the frequent vitamin D3 deficiency [36]. According to a study by Storr et al., patients with IBD who used cannabis reported significant improvement in various self-assessed symptoms, such abdominal pain, abdominal cramping, diarrhea, and joint pain. Interestingly, the same study also found a correlation between long-term cannabis use and the necessity for surgery in patients with CD, but as the authors noted, it may be because people who used cannabis for their symptoms had greater disease severity [37,38]. The diminished long-term concentration of AEA deteriorates all these above-mentioned symptoms and deficiencies, worsening the course of the disease and prolonging the duration of the disease.
There are various approaches that can enhance endocannabinoid-related signaling: increasing eCB production and secretion, administration of exogenic eCB analogs, and inhibiting the enzymes responsible for the degradation of eCBs. So far, the most extensively examined was the third approach. To date, there are a few studies on humans describing the effects of FAAH inhibitors on various diseases, but none regarding their use in treating IBD. Animal studies revealed the mechanism of action of FAAH and/or MAGL inhibitors. Sudeshna Ghosh et al. have shown that total FAAH inhibition combined with partial inhibition of MAGL (using PF-3845 combined with JZL184) in mice has a strong antinociceptive effect without significant cannabimimetic side effects; additionally, the measured brain AEA levels increased more than 10 times, while 2-AG levels increased 2–3 times [39]. A similar study, using only MAGL inhibitor JZL184, also by Sudeshna Ghosh et al., showed a reduction of mechanical allodynia and paw edema in the carrageenan test in mice [40]. In a study by Sałaga et al., FAAH inhibitor PF-3845 administered to two mouse models of colitis (TNBS-induced and DSS-induced) provided an anti-inflammatory effect measured by both microscopic and biochemical findings in the TNBS-induced colitis model, but it had no positive effect on DSS-induced colitis [41]. As previously stated, reduced activity of the FAAH enzyme, which is responsible for breaking down AEA, is responsible for the increased concentration of AEA which has anti-inflammatory properties. Nonetheless, the use of inhibitors of FAAH, increasing the AEA levels, and thus creating a positive impact on the course of Crohn’s disease seems to be promising but requires more pre-clinical and clinical studies.
The clinical trials with exogenous cannabinoid treatments in IBD patients are quite intensively being carried out. Attempts are being made to treat pain and diarrhea in CD with cannabinoids such as Δ9-tetrahydrocannabinol (THC) or cannabidiol (CBD) [42,43]. It was expected that cannabinoids, through endocannabinoid receptors, would help regulate the functioning of the brain (central regulation) and the immune system (peripheral effects) [44,45,46]. Naftali et al. performed a double-blind trial with cannabinoids in CD patients [47]. Health improvement was noted in 90% of patients. Another study found that cannabinoids reduced abdominal pain (83.9%), abdominal cramps (76.8%), joint pain (48.2%), and diarrhea (28.6%) [37]. However, studies conducted on patients do not clearly prove whether the alleviation of CD symptoms such as pain, diarrhea, or lack of appetite [48] is related to healing and diminishing inflammation and/or associated with the psychotropic effects of cannabinoids such as analgesia and euphoria and the proportion of these actions [49]. The analysis of the effect of exocannabinoids on the endocannabinoid system was taken once by Matalon et al. According to their study, specifically cannabis consumption had a positive effect on AEA and 2-AG concentrations in patients suffering from UC but did not have any effect on examined endocannabinoids in the CD group [30]. However, as the authors concluded, the observed disparity in results between the groups may be due to different treatment delivery method (inhalation of cigarettes vs. oral administration of oil) and/or differences in delta-9-tetrahydrocannabinol (THC) content, with levels of 23% in the UC group compared to 5% in the other. These data showed a limited usefulness of exocannabinoids in CD in terms of anti-inflammatory action via AEA, or even compensation of diminished concentration of AEA.
What is more, there are some justified worries about the usage of exogenous cannabinoids for therapeutic medical treatment and their legal recreational use allowance in several countries. The usage of exogenous cannabinoids frequently elicits various emotions related to their belonging to drugs (narcotics). Moreover, these medicaments should not be used in minors, the pregnant, those allergic to exocannabinoids, or those predisposed to psychotic disturbances [50,51]. There are also common opinions about the negative effects of cannabinoid use in some vulnerable groups, especially drivers. Additionally, some studies showed that the use of cannabinoids in CD may be harmful because their use is associated with a higher risk of complications leading to surgery [37] and temporary side effects such as weakness or dizziness [52]. Furthermore, the medical usage of cannabinoids sometimes is a double-edged sword, for example when it comes to the antiemetic qualities of those substances. There have been reports of a hyperemesis syndrome following chronic cannabis use, though there are some controversies regarding diagnosis, stemming from the difficulty to specify the exact number of vomiting episodes, amount of cannabis use, etc. [53]. It is nevertheless a significant problem, because Crohn’s disease is a chronic illness and therefore patients are at risk of prolonged cannabinoid usage. Another issue worth considering is that the usage of some cannabis derivates, especially acquired from unregulated sources, can lead to a toxidrome closely resembling serotonin syndrome, which is a potentially life-threatening condition [54].
In our discussion, we also have to consider anandamide metabolism and its implications on the conclusions. Classic theory, although recently questioned, is that anandamide is produced on demand from cell membrane phospholipid precursors and then is taken up by cells [55]. It is possible that lower plasma concentrations of AEA in CD patients observed by us are simply a result of increased uptake by inflamed cells of the GI tract and not a result of diminished production in the body as a whole. Lower AEA concentrations can also be the result of a complex genetical predisposition; as stated above, this substance has a profound effect on many processes and systems in the human body (including regulation of inflammation) and our findings may indicate the cause of CD in our patients, more than just being merely a sign of a disease. Both of these hypothetical mechanisms of diminishing AEA levels did not influence the final effect of low concentration of AEA on inflammation in CD. The shortage of AEA in CD due to any case is unfavorable.
Hypothetical long-term supplementation with exogenous AEA needs to consider the possible side effects. Administering large amounts of this substance with a high degree of probability would induce side effects stemming from AEA uptake by the central nervous system such as impaired memory [56]. Because of that, we rather consider the stimulation of endogenous AEA production or therapeutic monitoring of this agonist; further studies are needed to establish therapeutic ranges in that case. Therefore, it is advisable to develop therapeutic methods to enhance the concentration of endogenous cannabinoids. This type of treatment should be free from numerous side effects associated with exogenous cannabinoid medication, especially addiction, and therefore accepted by doctors and patients. An approach potentially worth considering is the pharmacological lowering of FAAH activity. The effect of such a therapy targeted on endocannabinoids should be beneficial and multidirectional—ranging from their anti-inflammatory, analgesic, anti-diarrheal, and improving mood effects to enhancing appetite and nutritional status.
5. Limitation of the Study
This is a preliminary study. The study group is relatively small, but patients were chosen from very specific and criterion-determined population of minors. However, a small number of patients in the test group and the control group might affect the results with potential bias. Also, biological variability in small groups might cause such a dispersion of results that lacks statistical significance in some comparisons.
6. Conclusions
Our results confirm that endocannabinoids are involved in the pathogenesis of Crohn’s disease. The severe course of CD caused reduced concentration of anandamide. Lower anandamide concentrations, even in remission, facilitate the recurrence of the disease and suggest some kind of genetic susceptibility to CD. Future research directions should focus on enhancing anandamide concentrations rather than exogenous cannabinoid administration. Also, therapy equalizing anandamide levels should be long-lasting.
Author Contributions
Contributions, conceptualization, P.J.T. and A.W.; methodology, M.S.B., J.T.T., A.W. and P.J.T.; patient recruitment and sample collection, A.W.; laboratory analysis, M.S.B., J.T.T. and P.J.T.; validation, P.J.T. and A.W.; writing—original draft preparation, J.T.T. and M.S.B.; writing—review and editing, A.W., P.J.T., J.T.T. and M.S.B.; supervision, P.J.T.; project administration, P.J.T.; funding acquisition, P.J.T. All authors have read and agreed to the published version of the manuscript.
Funding
Research funded by Collegium Medicum of Jagiellonian University grant (N41/DBS/000058).
Institutional Review Board Statement
The protocol of the study was approved by the Jagiellonian University Bioethical Committee (approval no. 1072.6120.238.2019, dated 24 October 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
2-AG—2-arachidonoylglycerol, AEA—anandamide, CB1—cannabinoid receptor type 1, CB2—cannabinoid receptor type 2, CBD—cannabidiol, CD—Crohn’s disease, CRH—corticotropin-releasing hormone, CNS—central nervous system, DAGL—diacylglycerol lipase, ECS—endocannabinoid system, ELISA—enzyme-linked immunosorbent assay, FAAH—fatty acid amide hydrolase, GI tract—gastrointestinal tract, IBD—inflammatory bowel disease, MAGL—monoacylglycerol lipase, NAPE-PLD—N-acyl-phosphatidylethanolamine phospholipase, ROS—reactive oxygen species, THC—tetrahydrocannabinol, TNBS-induced and DSS-induced—2,4,6-trinitrobenzenesulfonic acid and dextran sulfate sodium-induced (models for studying colitis), TNF-α—tumor necrosis factor α, UC—ulcerative colitis, eCB(s)—endocannabinoid(s), C—control group, CD1—study group: acute phase, CD2—study group: during the treatment, CD3—study group: in remission.
References
- Molodecky, N.A.; Soon, I.S.; Rabi, D.M.; Ghali, W.A.; Ferris, M.; Chernoff, G.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Barkema, H.W.; et al. Increasing Incidence and Prevalence of the Inflammatory Bowel Diseases With Time, Based on Systematic Review. Gastroenterology 2012, 142, 46–54.e42. [Google Scholar] [CrossRef]
- Ng, S.C.; Shi, H.Y.; Hamidi, N.; Underwood, F.E.; Tang, W.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Wu, J.C.Y.; Chan, F.K.L.; et al. Worldwide Incidence and Prevalence of Inflammatory Bowel Disease in the 21st Century: A Systematic Review of Population-Based Studies. Lancet 2017, 390, 2769–2778. [Google Scholar] [CrossRef]
- Day, A.S.; Ledder, O.; Leach, S.T.; Lemberg, D.A. Crohn’s and Colitis in Children and Adolescents. World J. Gastroenterol. 2012, 18, 5862–5869. [Google Scholar] [CrossRef]
- Torres, J.; Mehandru, S.; Colombel, J.-F.; Peyrin-Biroulet, L. Crohn’s Disease. Lancet 2017, 389, 1741–1755. [Google Scholar] [CrossRef] [PubMed]
- Frigstad, S.O.; Høivik, M.L.; Jahnsen, J.; Cvancarova, M.; Grimstad, T.; Berset, I.P.; Huppertz-Hauss, G.; Hovde, Ø.; Bernklev, T.; Moum, B.; et al. Pain Severity and Vitamin D Deficiency in IBD Patients. Nutrients 2019, 12, 26. [Google Scholar] [CrossRef]
- Swidsinski, A.; Ladhoff, A.; Pernthaler, A.; Swidsinski, S.; Loening-Baucke, V.; Ortner, M.; Weber, J.; Hoffmann, U.; Schreiber, S.; Dietel, M.; et al. Mucosal Flora in Inflammatory Bowel Disease. Gastroenterology 2002, 122, 44–54. [Google Scholar] [CrossRef] [PubMed]
- Nishida, A.; Inoue, R.; Inatomi, O.; Bamba, S.; Naito, Y.; Andoh, A. Gut Microbiota in the Pathogenesis of Inflammatory Bowel Disease. Clin. J. Gastroenterol. 2018, 11, 1–10. [Google Scholar] [CrossRef]
- Kowalska-Duplaga, K.; Gosiewski, T.; Kapusta, P.; Sroka-Oleksiak, A.; Wędrychowicz, A.; Pieczarkowski, S.; Ludwig-Słomczyńska, A.H.; Wołkow, P.P.; Fyderek, K. Differences in the Intestinal Microbiome of Healthy Children and Patients with Newly Diagnosed Crohn’s Disease. Sci. Rep. 2019, 9, 18880. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.-C.; Mackie, K. An Introduction to the Endogenous Cannabinoid System. Biol. Psychiatry 2016, 79, 516–525. [Google Scholar] [CrossRef]
- Pertwee, R.G. The Diverse CB1 and CB2 Receptor Pharmacology of Three Plant Cannabinoids: Delta9-Tetrahydrocannabinol, Cannabidiol and Delta9-Tetrahydrocannabivarin. Br. J. Pharmacol. 2008, 153, 199–215. [Google Scholar] [CrossRef]
- Howlett, A.C.; Abood, M.E. CB1 and CB2 Receptor Pharmacology. Adv. Pharmacol. 2017, 80, 169–206. [Google Scholar] [CrossRef] [PubMed]
- Galligan, J.J. Cannabinoid Signalling in the Enteric Nervous System. Neurogastroenterol. Motil. 2009, 21, 899–902. [Google Scholar] [CrossRef] [PubMed]
- Stanzani, A.; Galiazzo, G.; Giancola, F.; Tagliavia, C.; De Silva, M.; Pietra, M.; Fracassi, F.; Chiocchetti, R. Localization of Cannabinoid and Cannabinoid Related Receptors in the Cat Gastrointestinal Tract. Histochem. Cell Biol. 2020, 153, 339–356. [Google Scholar] [CrossRef] [PubMed]
- Hryhorowicz, S.; Kaczmarek-Ryś, M.; Zielińska, A.; Scott, R.J.; Słomski, R.; Pławski, A. Endocannabinoid System as a Promising Therapeutic Target in Inflammatory Bowel Disease—A Systematic Review. Front. Immunol. 2021, 12, 790803. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, K.A.; Wiley, J.W. The Role of the Endocannabinoid System in the Brain-Gut Axis. Gastroenterology 2016, 151, 252–266. [Google Scholar] [CrossRef] [PubMed]
- Cencioni, M.T.; Chiurchiù, V.; Catanzaro, G.; Borsellino, G.; Bernardi, G.; Battistini, L.; Maccarrone, M. Anandamide Suppresses Proliferation and Cytokine Release from Primary Human T-Lymphocytes Mainly via CB2 Receptors. PLoS ONE 2010, 5, e8688. [Google Scholar] [CrossRef] [PubMed]
- Blankman, J.L.; Simon, G.M.; Cravatt, B.F. A Comprehensive Profile of Brain Enzymes That Hydrolyze the Endocannabinoid 2-Arachidonoylglycerol. Chem. Biol. 2007, 14, 1347–1356. [Google Scholar] [CrossRef] [PubMed]
- Morena, M.; Patel, S.; Bains, J.S.; Hill, M.N. Neurobiological Interactions Between Stress and the Endocannabinoid System. Neuropsychopharmacology 2016, 41, 80–102. [Google Scholar] [CrossRef]
- Rousseaux, C.; Thuru, X.; Gelot, A.; Barnich, N.; Neut, C.; Dubuquoy, L.; Dubuquoy, C.; Merour, E.; Geboes, K.; Chamaillard, M.; et al. Lactobacillus Acidophilus Modulates Intestinal Pain and Induces Opioid and Cannabinoid Receptors. Nat. Med. 2007, 13, 35–37. [Google Scholar] [CrossRef]
- Muccioli, G.G.; Naslain, D.; Bäckhed, F.; Reigstad, C.S.; Lambert, D.M.; Delzenne, N.M.; Cani, P.D. The Endocannabinoid System Links Gut Microbiota to Adipogenesis. Mol. Syst. Biol. 2010, 6, 392. [Google Scholar] [CrossRef]
- Dione, N.; Lacroix, S.; Taschler, U.; Deschênes, T.; Abolghasemi, A.; Leblanc, N.; Di Marzo, V.; Silvestri, C. Mgll Knockout Mouse Resistance to Diet-Induced Dysmetabolism Is Associated with Altered Gut Microbiota. Cells 2020, 9, 2705. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, R.K.; Lutz, B.; Ruiz de Azua, I. The Microbiome and Gut Endocannabinoid System in the Regulation of Stress Responses and Metabolism. Front. Cell. Neurosci. 2022, 16, 867267. [Google Scholar] [CrossRef] [PubMed]
- Joossens, M.; Huys, G.; Cnockaert, M.; De Preter, V.; Verbeke, K.; Rutgeerts, P.; Vandamme, P.; Vermeire, S. Dysbiosis of the Faecal Microbiota in Patients with Crohn’s Disease and Their Unaffected Relatives. Gut 2011, 60, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Carding, S.; Verbeke, K.; Vipond, D.T.; Corfe, B.M.; Owen, L.J. Dysbiosis of the Gut Microbiota in Disease. Microb. Ecol. Health Dis. 2015, 26. [Google Scholar] [CrossRef] [PubMed]
- Parker, L.A.; Rock, E.M.; Limebeer, C.L. Regulation of Nausea and Vomiting by Cannabinoids. Br. J. Pharmacol. 2011, 163, 1411–1422. [Google Scholar] [CrossRef] [PubMed]
- Martyniak, A.; Wędrychowicz, A.; Tomasik, P.J. Endogenous Opioids in Crohn’s Disease. Biomedicines 2023, 11, 2037. [Google Scholar] [CrossRef] [PubMed]
- Levine, A.; Koletzko, S.; Turner, D.; Escher, J.C.; Cucchiara, S.; de Ridder, L.; Kolho, K.-L.; Veres, G.; Russell, R.K.; Paerregaard, A.; et al. ESPGHAN Revised Porto Criteria for the Diagnosis of Inflammatory Bowel Disease in Children and Adolescents. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 795–806. [Google Scholar] [CrossRef] [PubMed]
- Di Sabatino, A.; Battista, N.; Biancheri, P.; Rapino, C.; Rovedatti, L.; Astarita, G.; Vanoli, A.; Dainese, E.; Guerci, M.; Piomelli, D.; et al. The Endogenous Cannabinoid System in the Gut of Patients with Inflammatory Bowel Disease. Mucosal Immunol. 2011, 4, 574–583. [Google Scholar] [CrossRef] [PubMed]
- Grill, M.; Högenauer, C.; Blesl, A.; Haybaeck, J.; Golob-Schwarzl, N.; Ferreirós, N.; Thomas, D.; Gurke, R.; Trötzmüller, M.; Köfeler, H.C.; et al. Members of the Endocannabinoid System Are Distinctly Regulated in Inflammatory Bowel Disease and Colorectal Cancer. Sci. Rep. 2019, 9, 2358. [Google Scholar] [CrossRef]
- Tartakover Matalon, S.; Azar, S.; Meiri, D.; Hadar, R.; Nemirovski, A.; Abu Jabal, N.; Konikoff, F.M.; Drucker, L.; Tam, J.; Naftali, T. Endocannabinoid Levels in Ulcerative Colitis Patients Correlate With Clinical Parameters and Are Affected by Cannabis Consumption. Front. Endocrinol. 2021, 12, 685289. [Google Scholar] [CrossRef]
- Massa, F.; Marsicano, G.; Hermann, H.; Cannich, A.; Monory, K.; Cravatt, B.F.; Ferri, G.-L.; Sibaev, A.; Storr, M.; Lutz, B. The Endogenous Cannabinoid System Protects against Colonic Inflammation. J. Clin. Investig. 2004, 113, 1202–1209. [Google Scholar] [CrossRef]
- Goyal, H.; Singla, U.; Gupta, U.; May, E. Role of Cannabis in Digestive Disorders. Eur. J. Gastroenterol. Hepatol. 2017, 29, 135–143. [Google Scholar] [CrossRef]
- Balestrieri, P.; Ribolsi, M.; Guarino, M.P.L.; Emerenziani, S.; Altomare, A.; Cicala, M. Nutritional Aspects in Inflammatory Bowel Diseases. Nutrients 2020, 12, 372. [Google Scholar] [CrossRef]
- Scaldaferri, F.; Pizzoferrato, M.; Lopetuso, L.R.; Musca, T.; Ingravalle, F.; Sicignano, L.L.; Mentella, M.; Miggiano, G.; Mele, M.C.; Gaetani, E.; et al. Nutrition and IBD: Malnutrition and/or Sarcopenia? A Practical Guide. Gastroenterol. Res. Pr. 2017, 2017, 8646495. [Google Scholar] [CrossRef] [PubMed]
- Britto, S.L.; Krishna, M.; Kellermayer, R. Weight Loss Is a Sufficient and Economical Single Outcome Measure of Murine Dextran Sulfate Sodium Colitis. FASEB BioAdvances 2019, 1, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Rocha, R.; Santana, G.O.; Almeida, N.; Lyra, A.C. Analysis of Fat and Muscle Mass in Patients with Inflammatory Bowel Disease during Remission and Active Phase. Br. J. Nutr. 2009, 101, 676–679. [Google Scholar] [CrossRef]
- Storr, M.; Devlin, S.; Kaplan, G.G.; Panaccione, R.; Andrews, C.N. Cannabis Use Provides Symptom Relief in Patients with Inflammatory Bowel Disease but Is Associated with Worse Disease Prognosis in Patients with Crohn’s Disease. Inflamm. Bowel Dis. 2014, 20, 472–480. [Google Scholar] [CrossRef]
- Alshaarawy, O.; Balasubramanian, G.; Venkatesan, T. Cannabis Use in the United States and Its Impact on Gastrointestinal Health. Nutr. Clin. Pr. 2024, 39, 281–292. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Kinsey, S.G.; Liu, Q.-S.; Hruba, L.; McMahon, L.R.; Grim, T.W.; Merritt, C.R.; Wise, L.E.; Abdullah, R.A.; Selley, D.E.; et al. Full Fatty Acid Amide Hydrolase Inhibition Combined with Partial Monoacylglycerol Lipase Inhibition: Augmented and Sustained Antinociceptive Effects with Reduced Cannabimimetic Side Effects in Mice. J. Pharmacol. Exp. Ther. 2015, 354, 111–120. [Google Scholar] [CrossRef]
- Ghosh, S.; Wise, L.E.; Chen, Y.; Gujjar, R.; Mahadevan, A.; Cravatt, B.F.; Lichtman, A.H. The Monoacylglycerol Lipase Inhibitor JZL184 Suppresses Inflammatory Pain in the Mouse Carrageenan Model. Life Sci. 2013, 92, 498–505. [Google Scholar] [CrossRef]
- Sałaga, M.; Mokrowiecka, A.; Zakrzewski, P.K.; Cygankiewicz, A.; Leishman, E.; Sobczak, M.; Zatorski, H.; Małecka-Panas, E.; Kordek, R.; Storr, M.; et al. Experimental Colitis in Mice Is Attenuated by Changes in the Levels of Endocannabinoid Metabolites Induced by Selective Inhibition of Fatty Acid Amide Hydrolase (FAAH). J. Crohns Colitis 2014, 8, 998–1009. [Google Scholar] [CrossRef] [PubMed]
- Naftali, T. An Overview of Cannabis Based Treatment in Crohn’s Disease. Expert Rev. Gastroenterol. Hepatol. 2020, 14, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Kafil, T.S.; Nguyen, T.M.; MacDonald, J.K.; Chande, N. Cannabis for the Treatment of Crohn’s Disease. Cochrane Database Syst. Rev. 2018, 11, CD012853. [Google Scholar] [CrossRef] [PubMed]
- Klein, T.W.; Cabral, G.A. Cannabinoid-Induced Immune Suppression and Modulation of Antigen-Presenting Cells. J. Neuroimmune Pharmacol. 2006, 1, 50–64. [Google Scholar] [CrossRef] [PubMed]
- Tibiriça, E. The Multiple Functions of the Endocannabinoid System: A Focus on the Regulation of Food Intake. Diabetol. Metab. Syndr. 2010, 2, 5. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, A.C.A.D.; Souza, G.A.D.; Marqui, S.V.D.; Guiguer, É.L.; Araújo, A.C.; Rubira, C.J.; Goulart, R.D.A.; Flato, U.A.P.; Bueno, P.C.D.S.; Buchaim, R.L.; et al. Cannabis and Canabidinoids on the Inflammatory Bowel Diseases: Going Beyond Misuse. Int. J. Mol. Sci. 2020, 21, 2940. [Google Scholar] [CrossRef]
- Naftali, T.; Bar-Lev Schleider, L.; Dotan, I.; Lansky, E.P.; Sklerovsky Benjaminov, F.; Konikoff, F.M. Cannabis Induces a Clinical Response in Patients with Crohn’s Disease: A Prospective Placebo-Controlled Study. Clin. Gastroenterol. Hepatol. 2013, 11, 1276–1280.e1. [Google Scholar] [CrossRef]
- Lal, S.; Prasad, N.; Ryan, M.; Tangri, S.; Silverberg, M.S.; Gordon, A.; Steinhart, H. Cannabis Use amongst Patients with Inflammatory Bowel Disease. Eur. J. Gastroenterol. Hepatol. 2011, 23, 891–896. [Google Scholar] [CrossRef]
- Hasenoehrl, C.; Taschler, U.; Storr, M.; Schicho, R. The Gastrointestinal Tract—A Central Organ of Cannabinoid Signaling in Health and Disease. Neurogastroenterol. Motil. 2016, 28, 1765–1780. [Google Scholar] [CrossRef]
- Dong, C.; Chen, J.; Harrington, A.; Vinod, K.Y.; Hegde, M.L.; Hegde, V.L. Cannabinoid Exposure during Pregnancy and Its Impact on Immune Function. Cell. Mol. Life Sci. 2019, 76, 729–743. [Google Scholar] [CrossRef]
- Lisdahl, K.M.; Wright, N.E.; Kirchner-Medina, C.; Maple, K.E.; Shollenbarger, S. Considering Cannabis: The Effects of Regular Cannabis Use on Neurocognition in Adolescents and Young Adults. Curr. Addict. Rep. 2014, 1, 144–156. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.F.; Wolff, R.F.; Deshpande, S.; Di Nisio, M.; Duffy, S.; Hernandez, A.V.; Keurentjes, J.C.; Lang, S.; Misso, K.; Ryder, S.; et al. Cannabinoids for Medical Use: A Systematic Review and Meta-Analysis. JAMA 2015, 313, 2456–2473. [Google Scholar] [CrossRef] [PubMed]
- Chu, F.; Cascella, M. Cannabinoid Hyperemesis Syndrome. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Baltz, J.W.; Le, L.T. Serotonin Syndrome versus Cannabis Toxicity in the Emergency Department. Clin. Pr. Cases Emerg. Med. 2020, 4, 171–173. [Google Scholar] [CrossRef] [PubMed]
- Alger, B.E.; Kim, J. Supply and Demand for Endocannabinoids. Trends Neurosci. 2011, 34, 304–315. [Google Scholar] [CrossRef]
- Mallet, P.E.; Beninger, R.J. The Endogenous Cannabinoid Receptor Agonist Anandamide Impairs Memory in Rats. Behav. Pharmacol. 1996, 7, 276–284. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).