Abstract
Cervical orthoses, vital for neck immobilization in medical care and sports, often struggle to provide adequate support due to individual neck shape and size variations. This study addresses this issue by developing a specific computer-aided orthosis design software tailored for creating customized 3D-printed cervical orthoses. The self-developed software embedded anatomical and rehabilitation knowledge into the orthosis design process, ensuring consistency and reducing manual modification. Finite element analysis of cervical orthoses determined that a minimum thickness of 5 mm PLA (polylactic acid) material is necessary to meet safety requirements. This study highlights the automation potential of customized computer-aided orthosis design and underscores the potential to revolutionize orthopedic care. We also applied easy-to-access 3D printing technology to fabricate well-fitting and immobilized cervical orthoses. These customized cervical orthoses offer a promising future with the advantages of being cost-effective, lightweight, immobility, comfortable, easy to wear, and minimal accessories to meet clinical needs, enhancing patient comfort and compliance and providing reassurance about the economic benefits of the technology.
1. Introduction
Cervical orthoses are commonly used by patients who have had a surgical intervention of the cervical spine to immobilize the neck. They allow for proper support and immobilizing of the neck to prevent secondary injuries [1]. Commercially available cervical orthoses are modularized in a few sizes with adjustable accessories to accommodate an individual’s neck height, width, and circumstances [2]. One’s willingness to wear the cervical orthosis may be reduced if discomfort, humidity, and stuffiness arise, especially for patients who genuinely need orthoses to support and immobilize protection during neck injury or after cervical surgery.
The additive manufacturing (AM) technology enables the production of highly customized items with minimal material usage, ideal for customized medical devices, such as cervical orthosis [3,4,5,6,7,8], wrist orthoses [9], bone plates, etc. [10]. As AM technology advances, hours of fabricating a 3D printing object decrease, enabling rapid production of customized items [11]. Utilizing 3D scanning technology, customized cervical orthoses can be additively manufactured to fit the individual better, increasing neck support, reducing pressure, and avoiding size mismatches [12].
Studies employ general computer-aided design (CAD) software to generate customized orthoses [4,7,9]. These kinds of software are fully functional for industrial components; they are not explicitly developed for customized orthoses. It provides neither anatomical guidelines nor constraints relevant to neck immobility and comfort. Without a background knowledge of anatomy and good posture, designers may be unable to perform neck rehabilitation. This results in orthoses that fail to achieve the intended use or provide safe support, not even concerning the comfort or long-term use, thus limiting the effectiveness of the orthoses.
To address these issues, the study developed specific software for customized cervical orthosis design, incorporating professional knowledge in anatomical and rehabilitation. We present a generic template to shorten orthosis design processes in automation and minimize the variation of different designers while maintaining the flexibility of details. To meet the safety requirements, we invoked the finite element method to simulate the stress distribution on orthosis, revealing the minimum thickness of the simple structure of the two-piece design.
2. Materials and Methods
Cervical orthosis is designed to immobilize and support the neck. It usually encircles the neck with fabric, resilient material, or rigid plastic. Rigid cervical orthosis is recommended for neck trauma to reduce neurological disability and provide spinal stability. Soft collars have been proposed as a good alternative because of the complications related to rigid collars. Rigid collars provided significantly higher stability than soft collars in terms of ROM (range of motion) [13]. No cervical orthoses could provide enough immobilization for neck extension or vertebra’s intersegmental motion. More rigidity means more restriction on the neck and more effective immobility. However, it may lead to discomfort and possible complications. In this situation, the willingness to wear it for a specific period decreases, which may affect the effect of rehabilitation treatment.
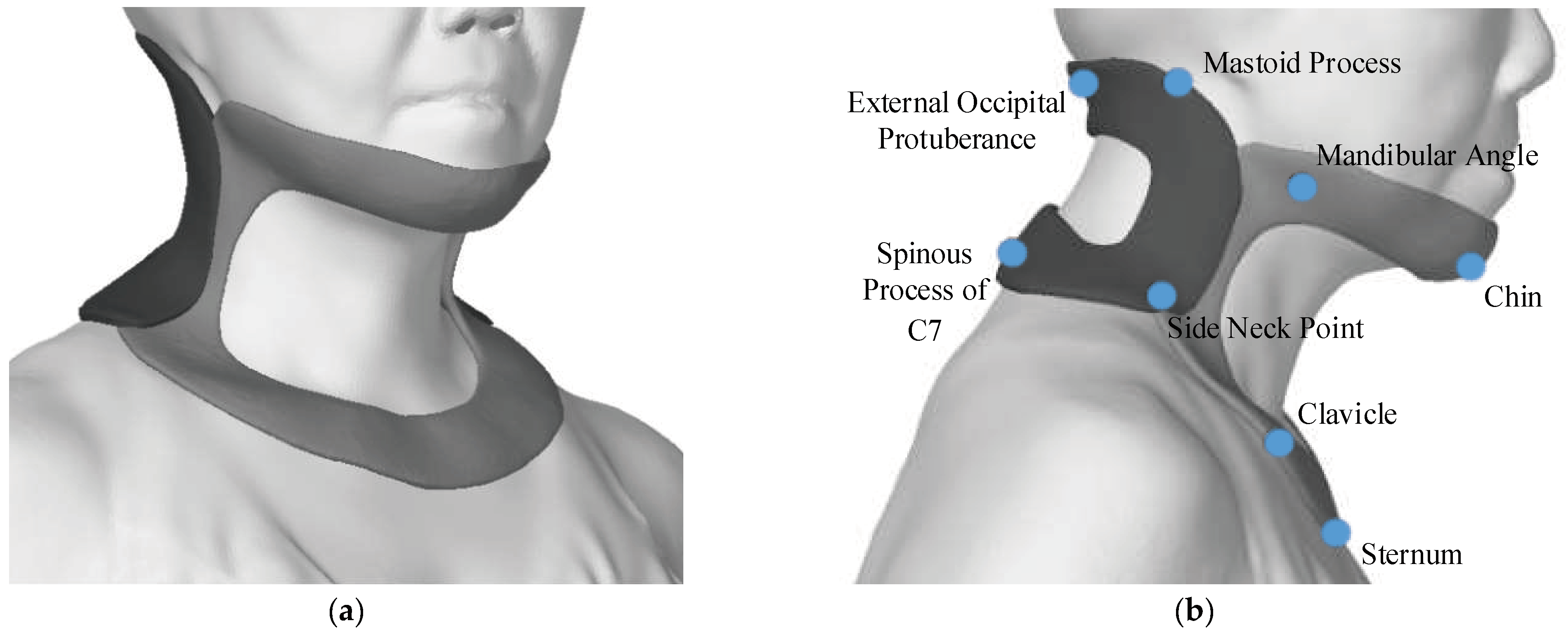
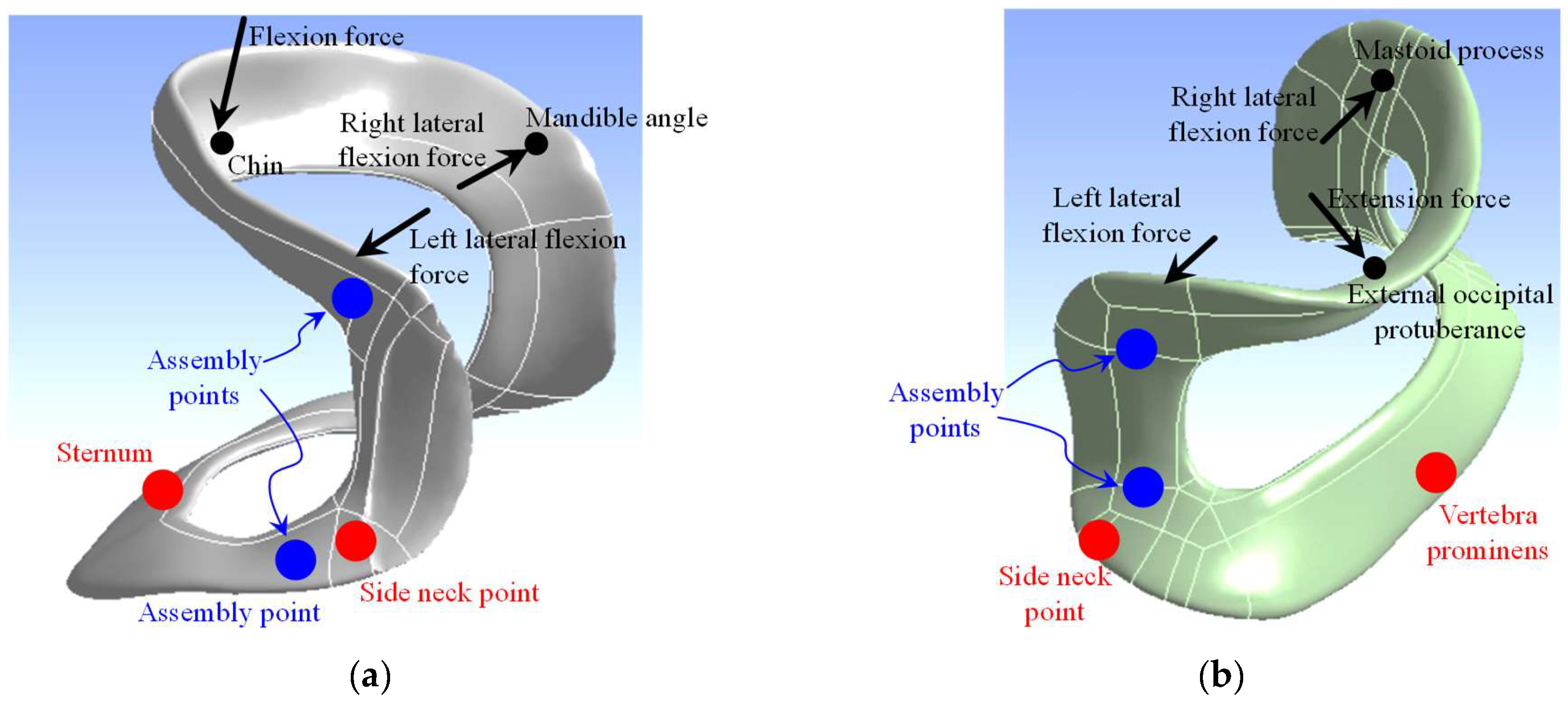
This study adopts a two-piece cervical orthosis that covers the subsurface bones surrounding the neck. As shown in Figure 1, the designed cervical orthosis accommodates 12 anatomical features. They include the chin, mandibular angles, side neck points, clavicles, sternum in the front piece, external occipital protuberance, mastoid processes, and spinous process of the seventh cervical vertebra (C7) in the back piece. All these features are located on the subsurface of the corresponding anatomical bone.
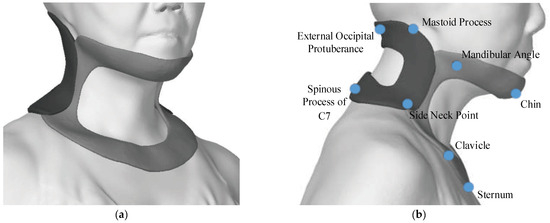
Figure 1.
(a) The designed cervical orthosis. (b) The anatomical features below the cervical orthosis.
2.1. The Design Workflow of Cervical Orthosis
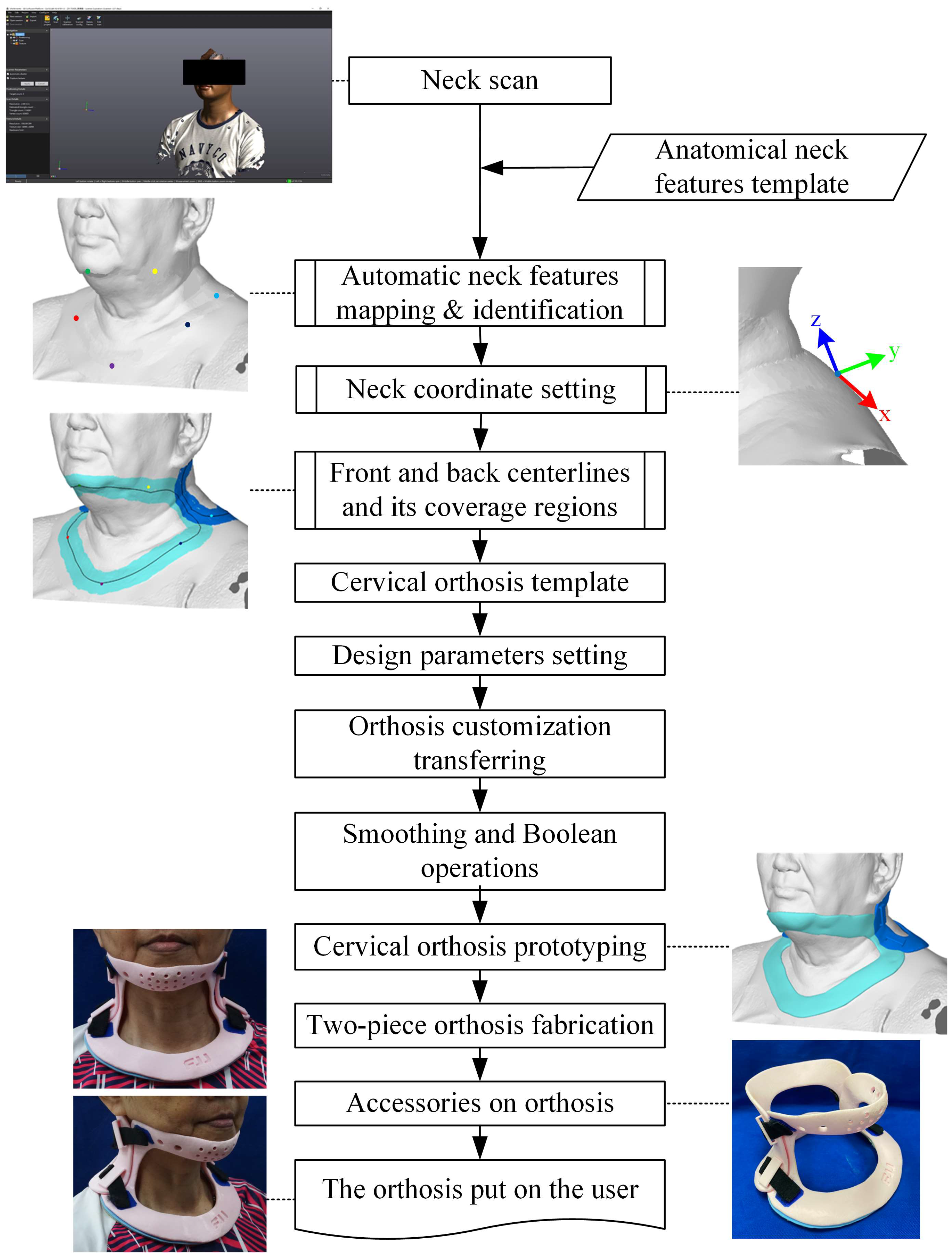
The fully automatic orthosis design software was implemented using Microsoft Visual Studio 2015 with the C++ programming language. Figure 2 shows the automatic workflow for the customized cervical orthosis. We used a 3D scanner (Go!Scan 50, Ceaform, QC, Canada) to scan the neck region of the subject. When scanning, the subject sits comfortably against the back of the chair and tucks their chin with the eyes closed, ensuring the ear canals are directly above the shoulders. The scanning area includes the upper chest and back, the entire neck, and the partial head region next to the neck. We pre-set an anatomical neck feature template for neck features matching between the template and the subject by the maximum bipartite matching algorithm [14]. A Hungarian algorithm was then applied to obtain a perfect match with minimum weight after distance normalization between every pair of features [15]. These features serve as reference points to determine the neck coordinate and circulated connection to form two centerlines of the front and back pieces of the orthosis. The orthosis prototype is formed by expanding a given width and thickness on the surface of the neck model. Boolean difference and smoothing operations are applied to the front and back pieces for refinement before 3D printing. They were fabricated using a fused deposition modeling (FDM) 3D printer with polylactic acid material. It was then padded below the front piece above the subsurface of the clavicles and the back piece behind mastoid processes to prevent pressure ulcers. Four Velcro accessories were glued tightly on the upper and lower lateral sides of the front and back pieces, allowing opening and closing when wearing and untying the orthosis.
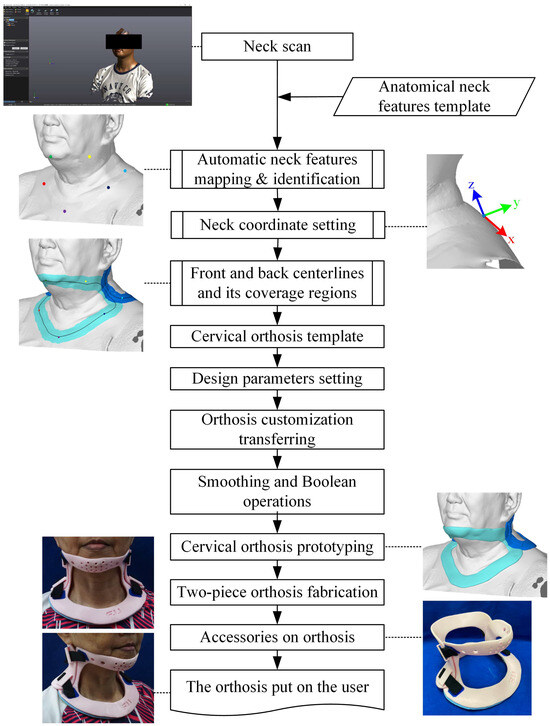
Figure 2.
The design workflow for cervical orthoses.
Along with the fundamental theory, by importing the scanned cloud points, our developed software embedded a fully automatic process for neck feature identification, coordinate systems’ transformation, the orthosis template, normalization, denormalization, and customized cervical orthosis prototyping. The developed software gives adjustable parameters for only one orthosis thickness and seven allowance settings between the user and the orthosis, including anterior, posterior, and lateral orthosis; mandibular angles, mastoid processes; clavicles; and prominent vertebra regions. The design of the new type of orthosis adopts the advantages of the currently available and popular cervical orthosis, Vista Multipost Collar (Aspen Medical Products, Irvine, CA, USA), in support and stabilization but improves lightweight, ventilation, and strength of cervical orthosis.
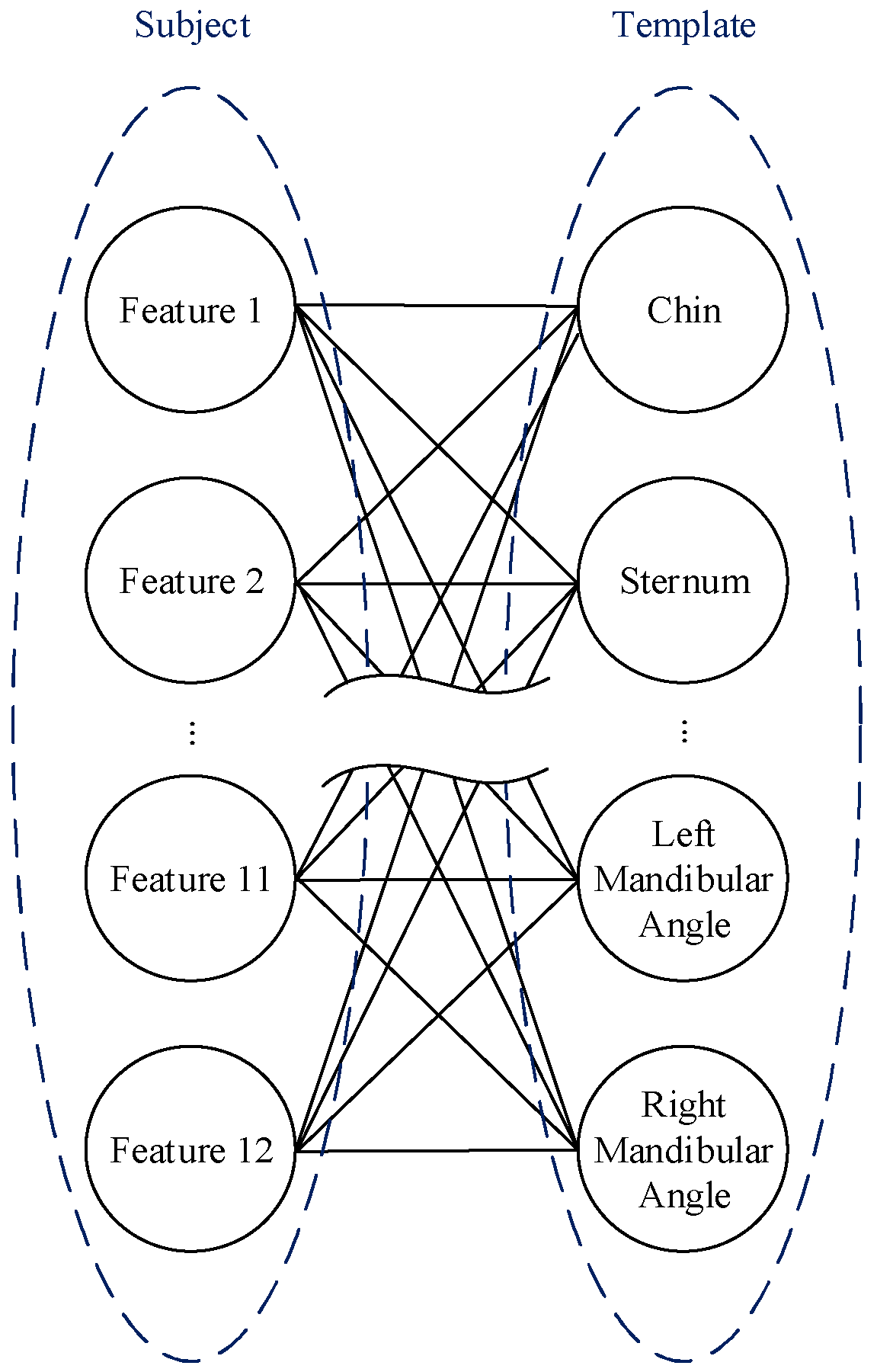
2.1.1. Features Identification
The 12 neck features were marked before scanning. We created a features template and applied the bipartite graph matching algorithm to match and identify the 12 feature points. The coordinates of each feature point are the center of color marks in the scan model. Two feature sets, S and T, each contain 12 points. Set S, referred to as the subject, consists of features from the digital scan, and set T, the template, also comprises features of the anatomical template. Figure 3 shows the bipartite graph, with an edge connected to every two features between the two sets to be potential matches.

Figure 3.
Bipartite graph of 12 features.
A set center can be represented as an average of features in a set. If the corresponding features of two sets are matched in the proper position, then the orientation of the matching features associated with the set center will be similar. Therefore, we can find the minimal distance summations between each corresponding point.
Let and be the i-th and j-th features in set S and T, respectively. The and represent the center in set S and T, respectively. Then, the squared difference between the normalizations of the two sets becomes
ensuring that the perfect match is the minimum weighting. Suppose the k-th matching matches the and in set S and T, respectively. Then, we can minimize the total weight to achieve a perfect match.
We employ the Hungarian algorithm [15] to obtain perfect matching, ensuring the 12 matchings are at the minimum weight. Then, the 12 neck features can be identified automatically.
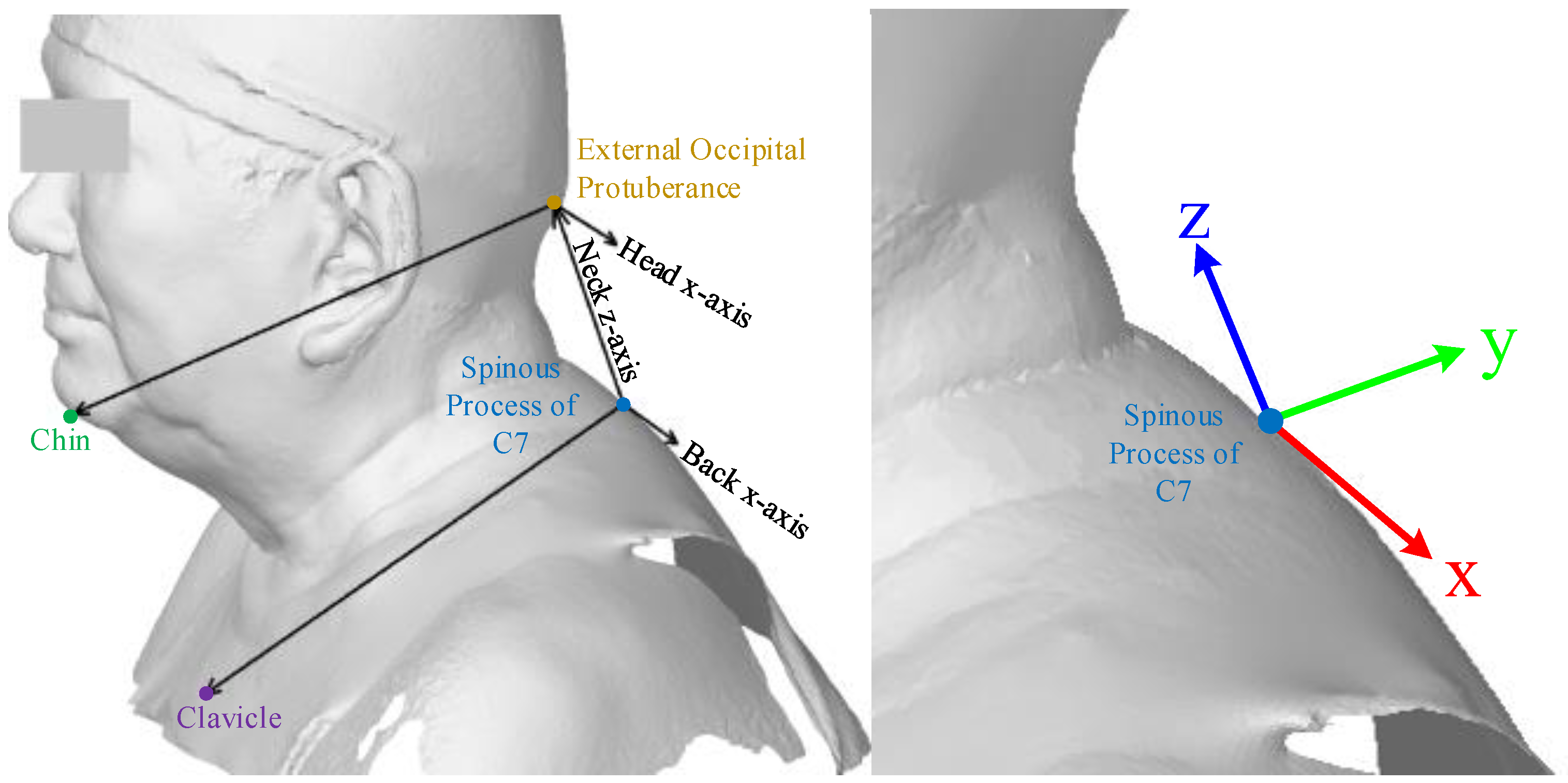
2.1.2. Neck Coordinate
Based on the anatomical features shown in Figure 4, we defined a unique neck coordinate system for further orthosis design automation. According to the 12 feature points obtained from the previous section, the origin of the neck coordinate is set to the subsurface of the spinous process of cervical 7, C7. The detailed neck coordinate setup procedures are listed below.

Figure 4.
The neck coordinate system.
- Define the neck z-axis from C7 to the external occipital protuberance.
- Set the head x-axis to be the cross product of the neck z-axis and the vector from the external occipital protuberance to the chin.
- Set the back x-axis as the cross product of the neck z-axis and the vector from the spinous process of C7 to the sternum.
- Define the neck x-axis as the average vector of the head x-axis and the back x-axis.
- Define the neck y-axis as the cross product of the neck z-axis and the neck x-axis.
2.1.3. Orthosis Template
According to the neck coordinate, we need to generate two centerlines for the front and back pieces by connecting the front and back neck features in associated loops, as the black line loops shown in Figure 3. We expanded a given width based on the centerline to prototype the width of a two-piece orthosis. These methods can create a template for orthosis region setup in automation. In addition, we can ensure the width remains consistent in the customized cervical orthosis.
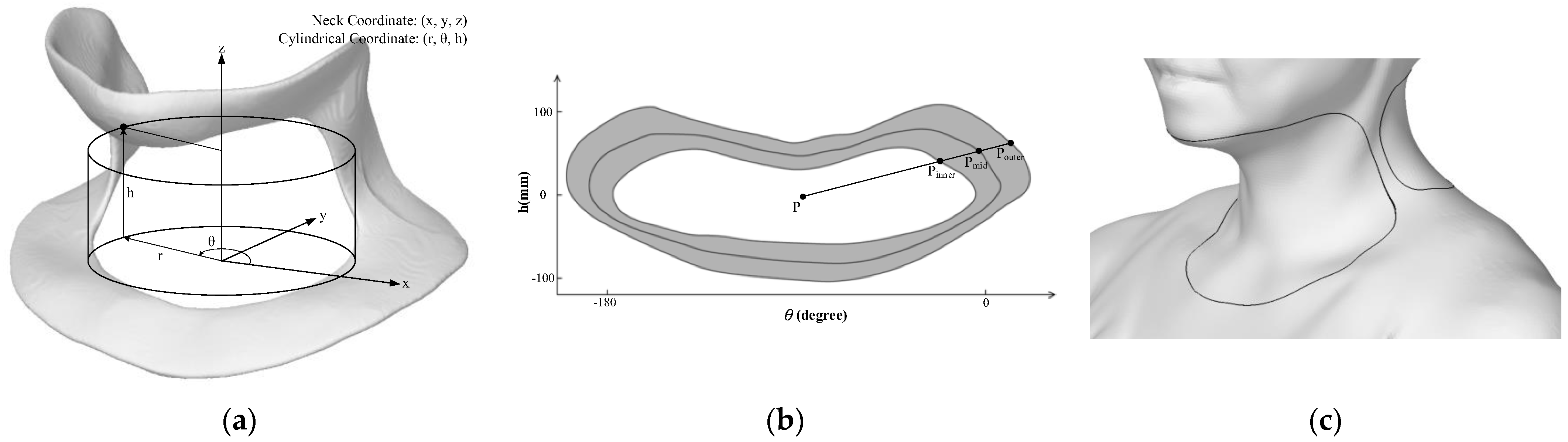
As shown in Figure 5a, we transformed the template coordinate from the neck Cartesian coordinate (x, y, z) into the cylindrical coordinate (r, θ, h) with radius r, rotation angle θ, and height h. An unfolded graph of the cervical orthosis’ front piece in cylindrical coordinates is shown in Figure 5b. The center of the bounding rectangle of the unfolded graph is set as the center point P. A ray outward extended from P to any direction intersects the orthosis graph at Pinner, Pmid, and Pouter. The midpoint Pmid is located on the centerline of the orthosis. By emitting 360-degree rays from the P in the graph, we can obtain the central line with the inner and outer edges of the front piece of the cervical orthosis. The same procedure was applied to find the central line and the inner and outer edges of the back piece cervical orthosis. Figure 5 c shows the centerlines of the two-piece cervical orthosis.

Figure 5.
(a) Relationship between neck Cartesian coordinates (x, y, z) and cylindrical coordinates (r, θ, h). (b) Unfolded graph of the front piece of the cervical orthosis. (c) Centerline of the two-piece cervical orthosis.
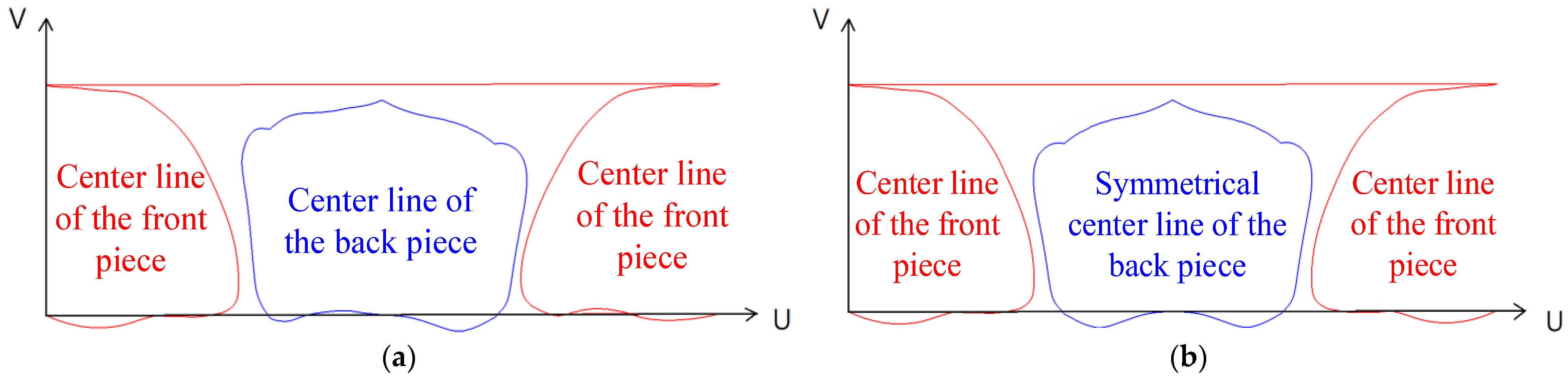
A minor skew sometimes appears on the subject’s neck in a neutral position. In such circumstances, the centerlines generated from the digital scan model are usually not symmetrical. Besides supporting and immobility orthoses, we also consider correcting the state of neck skew when wearing the orthosis. Therefore, we built a symmetrical centerline template for the front and back pieces that can remain symmetric when transferring to the other. We normalized the U and V axes in the cylindrical coordinates, as shown in Figure 6a, to mirror half of the centerline on the line across the chin and sternum to make a completely symmetrical centerline (Figure 6b). Based on the coordinate transfer from Cartesian to cylindrical, it is then transferred back to Cartesian to generate an orthosis geometry model.
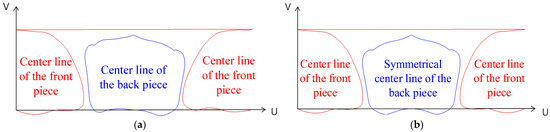
Figure 6.
The centerline template (a) before and (b) after being symmetrized.
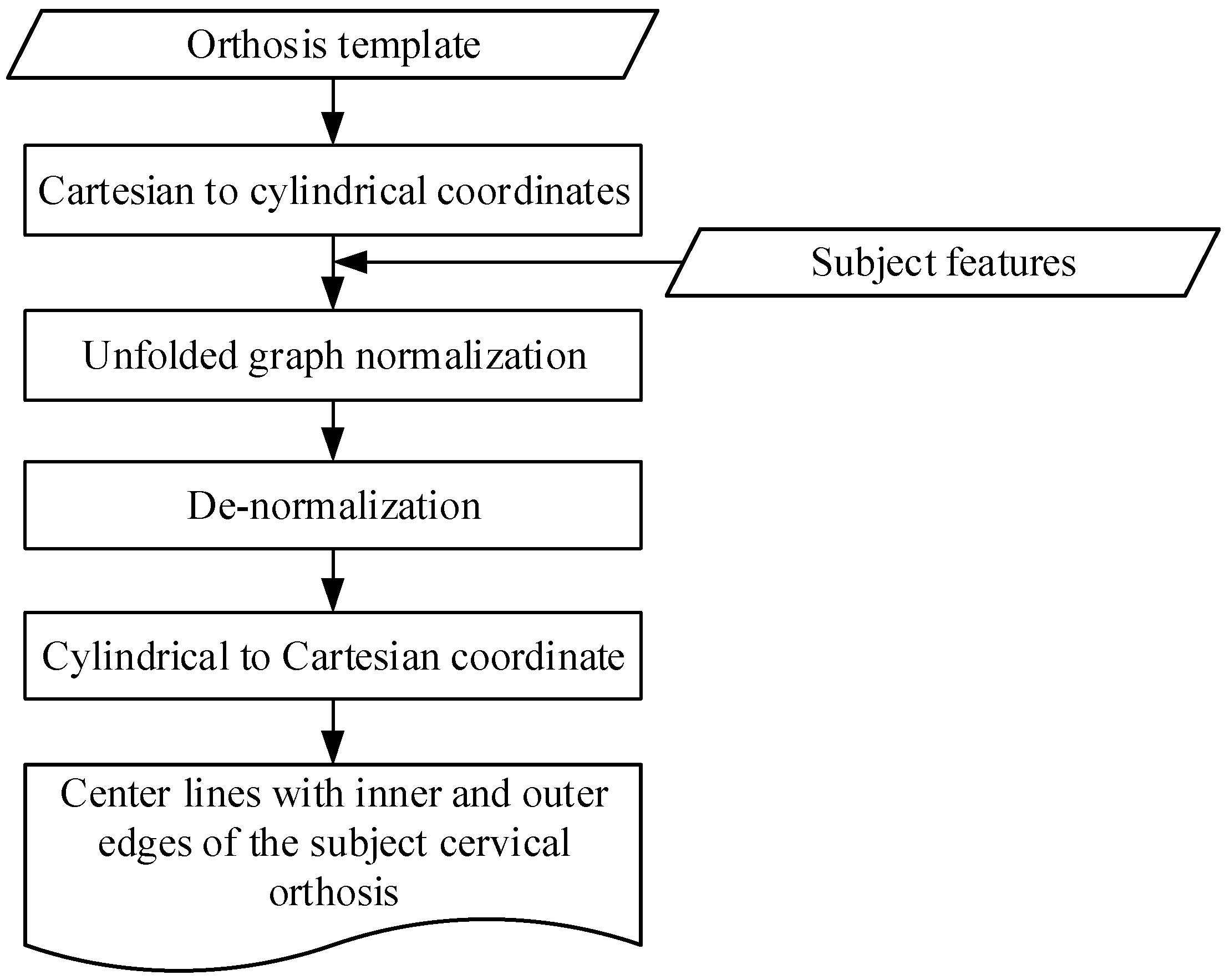
2.1.4. Transfer Orthosis Template to Customization
The orthosis template contains 12 anatomical neck features and 2 central lines with the inner and outer edges of the front and back piece orthosis. However, the neck morphology of individuals varies. Transferring an orthosis template to an individual geometry is crucial for customizing automated cervical orthoses. Therefore, we applied normalization and denormalization processes to achieve a customized automated orthosis design. Figure 7 illustrates the whole transferring procedure. The neck orthosis template was transferred from Cartesian to cylindrical coordinates to adapt the neck geometry. We normalize and then de-normalize the unfolded graphs of the template and subject. After normalizing and de-normalizing, the subject’s central lines with the inner and outer edges of the two-piece orthosis were generated. We then reversed the transferred coordinates from cylindrical to Cartesian. When the inner and outer edges of the two-piece orthosis are set, the cover region on the neck of the two-piece cervical orthosis can be determined.
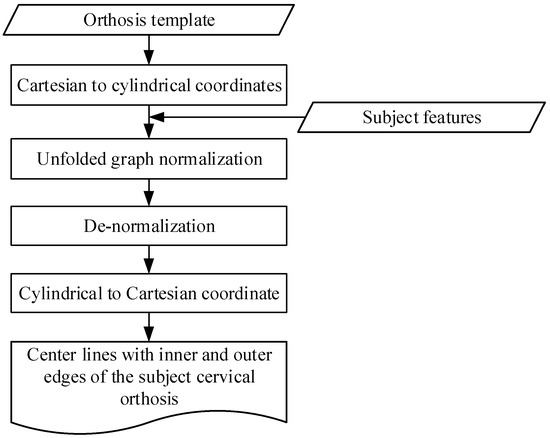
Figure 7.
The customization procedure from template to individual.
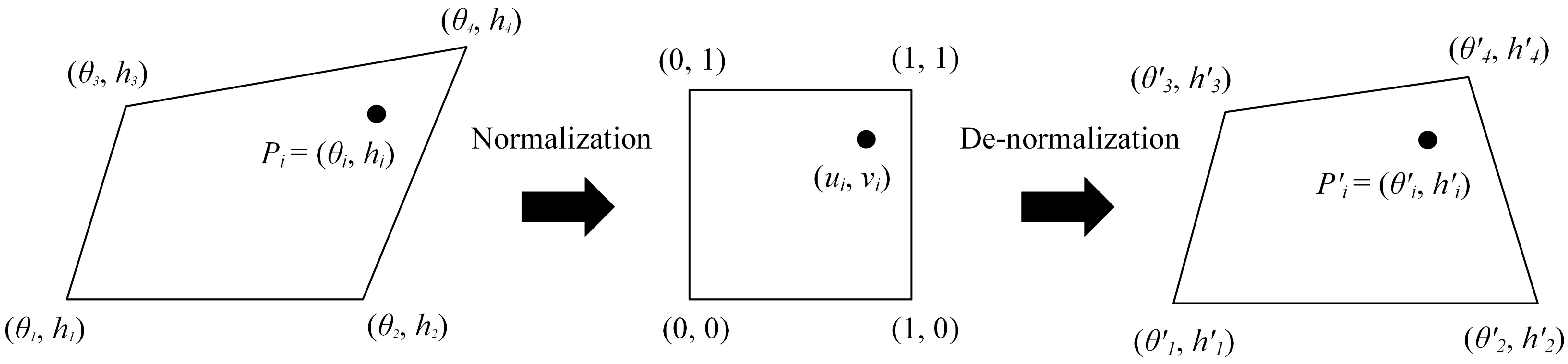
The feature vertexes represent the same anatomical feature of each subject due to the neck geometry and circumference varying in different subjects. Based on the 12 neck features, normalization and de-normalization were applied on the azimuth angle, θ, and height, h. Figure 8 is a diagram of the normalization and de-normalization processes for the ith feature, Pi, on the central line of either the front or back piece. The corner vertices of the quadrilateral represent four features near to Pi, , , , and . (θ, ) and (u, v) present the orientation, height, and centerline after normalization. We then denormalized (u, v) to to the four quadrilateral corners, , , , and , to obtain the subject’s central line on the scan model.

Figure 8.
Normalization and de-normalization processes in the central line.
Normalize transfer the coordinates of θ and h to [0,1].
And the de-normalization is
2.1.5. Orthosis Generation
We applied the geodesic algorithm [16] to constantly set the expansion width along the centerlines of front and back pieces as coverage areas. We offset the triangle meshes from scratch using multiple normal vectors of those vertexes in the coverage areas to build the meshes in the inner and outer layers of the orthosis [17]. The inner layer contacts the neck surface, whereas the outer layer is above the inner by expanding the multiple normal vectors of the inner vertexes.
We connected the edges of the inner- and outer-layer mesh by adding several layers of array meshes to form an enclosed piece object. The added vertexes were distributed by averaging the normal vector of its adjacent meshes. For instance, suppose N adjacent meshes surround a vertex, and the average vector of the ith adjacent meshes is . It can duplicate a new vertex along the mean normalization vector
Based on the added vertex position setting of the inner layer, we set several allowances on the neck features, usually less than or equal to 1.0 mm, to prevent tie contact between the inner orthosis and neck subsurface.
Since the meshes of orthosis were generated from scratch, the sharp edges of those meshes on the outer layer were not preventable. We applied the Laplacian smoothing algorithm [18] to eliminate sharp edges on the outer surface of the front and back pieces. The overlap region of the front and back pieces was a Boolean difference operation to make a groove on the front piece to interlock each other. We also applied a Boolean union operation to set up four pairs of buckle seats. The front and back pieces of personal orthosis are finally secured with elastic straps to fix around the user’s neck. This design slightly restricts the flexion, lateral flexion, and extension of the user’s neck when wearing.
3. Finite Element Analysis
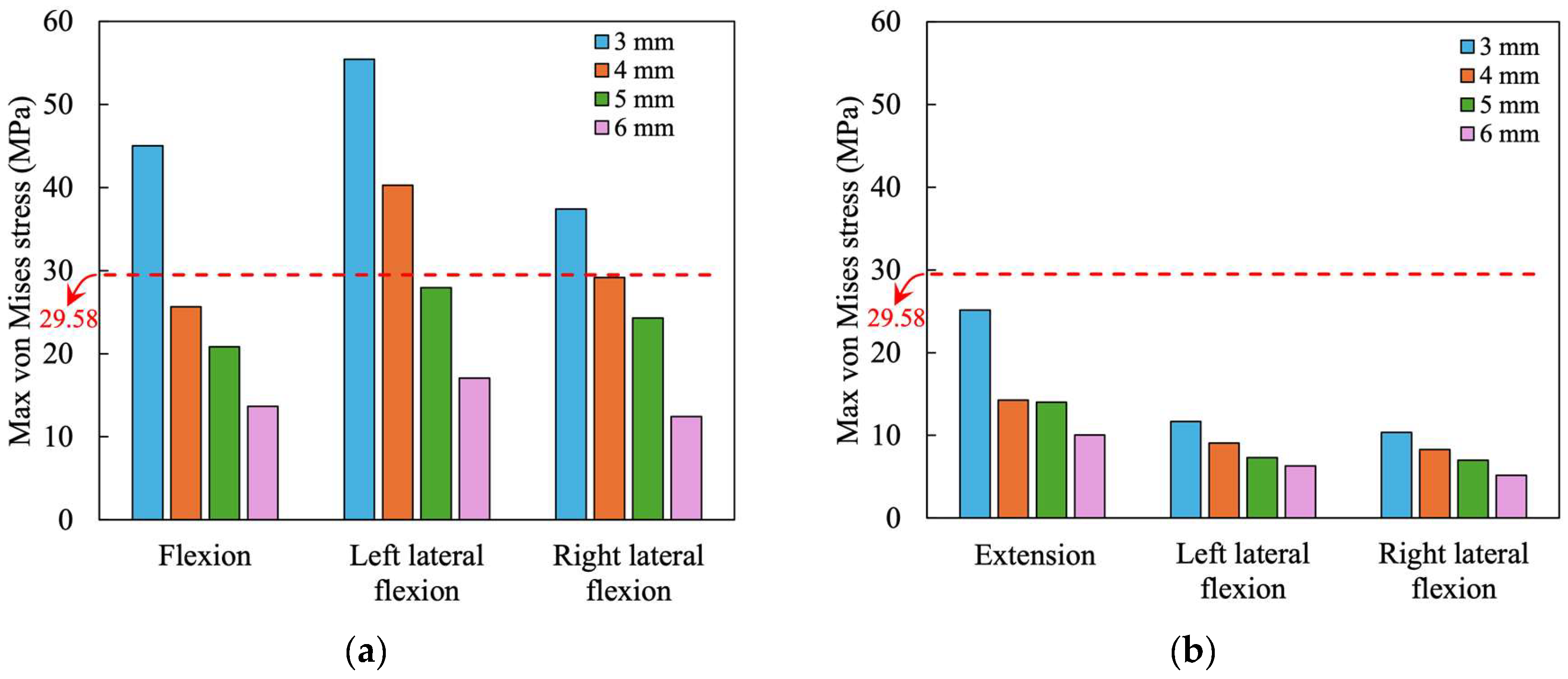
To ensure the strength of loading support of the 3D printing orthosis, a finite element analysis with ANSYS (version 19.2) was conducted to simulate the stress distribution in the orthosis under various loadings of postures. The coverage area on the lateral side of the orthosis includes the ribs, which provide necessary support for the orthosis. The parameters for the front and back pieces of the orthosis were 30 mm wide, with four different thicknesses of 3 mm, 4 mm, 5 mm, and 6 mm for finite element analysis. The orthosis was fabricated using an FDM 3D printer with PLA at 20% infill. The elastic modulus for 3D-printed PLA with 25%, 50%, and 75% infills are 0.866, 0.985, and 1.223 GPa, respectively, while the elastic modulus for these three infills is 31.4 MPa, 34.96 MPa, and 42.67 MPa, respectively [19]. In the finite element model, the mechanical properties for PLA with 20% infill, listed in Table 1, can be obtained by extrapolating the above measurement data reported in [19]. The boundary conditions in the finite element analysis are shown in Figure 9. For all postures, the sternum and side neck points are fixed in the front piece model, while the seventh cervical vertebra and side neck points are fixed in the back piece model. For the front piece with flexion posture, an extra fixation at the assembly points shown in Figure 9 is added due to the constraint from the back piece. Similarly, the back piece assembly points are also fixed for extension posture. The assembly points are not fixed for left and right lateral flexions. According to the moments at the seventh cervical vertebra for various postures obtained from [20,21], the equivalent forces applied on the front and back pieces of orthosis in each posture are listed in Table 2 and Table 3.

Table 1.
Material properties of PLA with 20% infill [19].
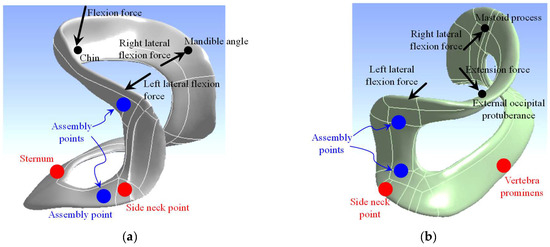
Figure 9.
Fixed points and loading points for the finite element analysis: (a) the front piece, (b) the back piece.

Table 2.
Loads on the front piece of orthosis in each posture.

Table 3.
Loads on the back piece of orthosis in each posture.
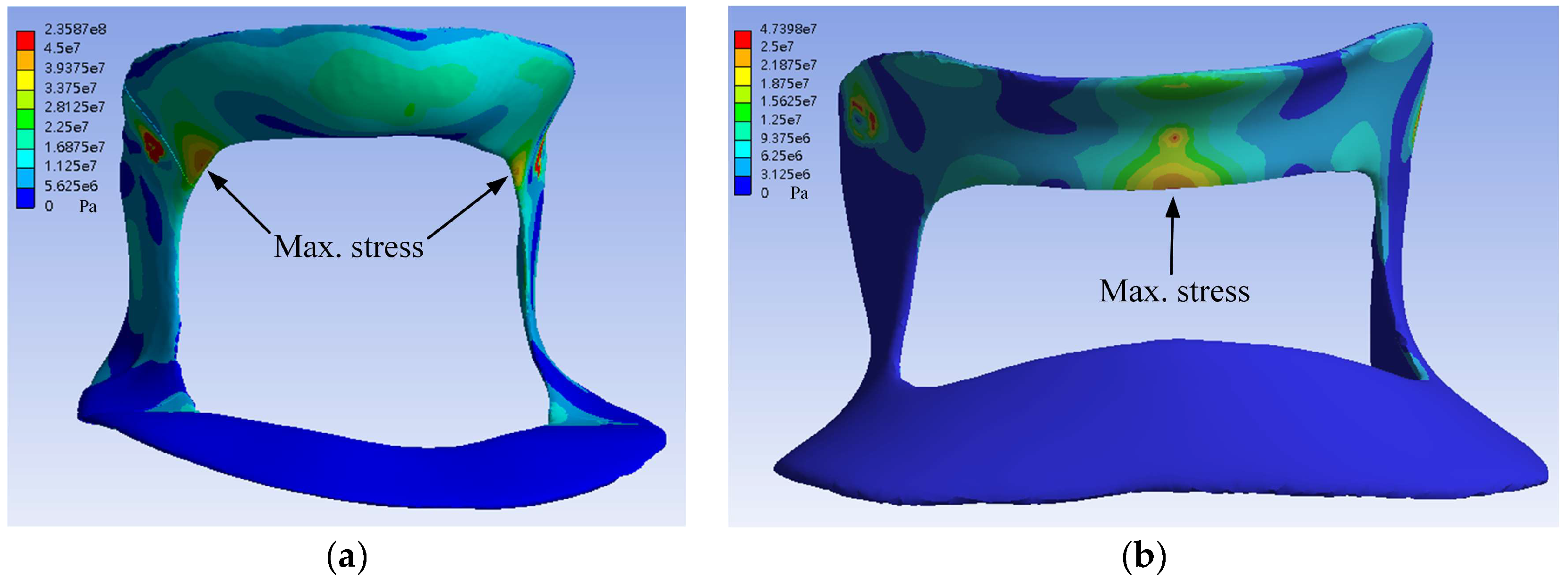
Table 4 and Table 5 show the maximum von Mises stress of the respective front and back pieces of orthosis for various postures from finite element analysis. Figure 10 shows the stress simulation outcomes for the front and back pieces. The horizontal dashed line indicates the tensile strength, 29.58 MPa. The stress contours for cervical orthosis with a thickness of 3 mm are shown in Figure 11. The results indicate that the maximum stress decreases as the thickness increases, regardless of the neck postures. In the front piece, the maximum stress exceeds the tensile strength, 29.58 MPa, at 3 mm thickness for flexion, left lateral flexion, and right lateral flexion and 4 mm thickness for left lateral flexion. The back piece found no maximum stress exceeding the yield strength. According to the finite element analysis results, the front piece should be at least 5 mm thick, and the back piece should be at least 3 mm thick to ensure the maximum stress remains below the PLA tensile strength of 29.58 MPa. For safety reasons, it is recommended to utilize a minimum thickness of 5 mm for customized orthosis fabricated with 20% infill PLA material.

Table 4.
Maximum von Mises stress (MPa) of front piece orthosis at different thicknesses and postures.

Table 5.
Maximum von Mises stress (MPa) of back piece orthosis at different thicknesses and postures.
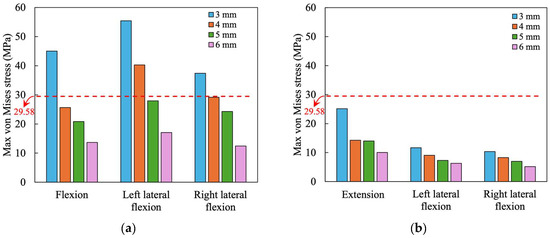
Figure 10.
Stress analysis of different thicknesses of orthosis (a) the front piece, (b) the back piece.
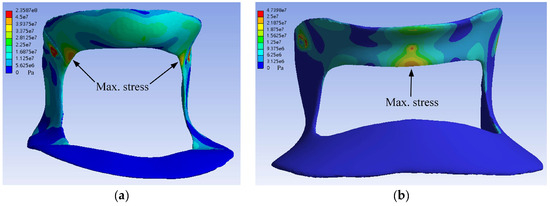
Figure 11.
Stress contours for cervical orthosis with thickness of 3 mm (a) the front piece under flexion, (b) the back piece under extension.
In the finite element analysis, the magnitudes of the loads listed in Table 2 and Table 3 are based on the strength of the neck muscles [20,21]. These test data were measured from healthy persons. This means that the loads applied to the orthosis in the finite element analysis were the maximum forces a healthy person could apply. For the orthosis with long-term wearing, the loadings listed in Table 2 and Table 3 and the stresses listed in Table 4 and Table 5 cannot be used to evaluate the fatigue issues. According to the S–N curves from the fatigue testing data of PLA specimens reported by Ezeh and Susmel [22], the fatigue strength is approximately one-sixth of the tensile strength for the fatigue limit ( cycles). Using a tensile strength of 29.58 MPa, as seen in Table 1, the fatigue strength would be 29.58/6 = 4.93 MPa. Under flexion, the 5 mm thickness front piece orthosis has a stress of 20.85 MPa, as shown in Table 4. Thus, the maximum flexion force applied on the front piece to reach the fatigue limit is 135.06/(20.85/4.93) = 31.94 N. Table 6 and Table 7 lists the loadings on the front and back pieces orthosis in which all stress values are lower than fatigue strength. It was seen that as the orthosis thickness increases, the allowable loading on the orthosis increases.

Table 6.
Maximum load (N) of front piece orthosis for fatigue strength.

Table 7.
Maximum load (N) of back piece orthosis for fatigue strength.
4. Discussion
One can adopt commercial computer-aided design software that can also be used to design a cervical orthosis from body scan data. However, this software is usually used for parameterized parts’ design purposes, making setting a symmetrical centerline path and its coverage regions with consistent widths challenging. In our previous study, the front piece’s coverage regions supported setup manually, encountering complex and demanding work that required operators to make long-hour adjustments [3]. In contrast, our design software generates the coverage area by expanding from the central line of the orthosis, ensuring a consistent width. The central line template is pre-symmetrized, allowing for the creation of a more symmetrical orthosis even if the human body is not perfectly symmetrical. Therefore, the customized symmetrical orthosis can correct a neutral minor skew head posture. Moreover, several issues arise from human factors in design variability using general CAD software. Our design is based on the crucial anatomical infrastructure, which may cause inconsistency when manually setting the infrastructure, such as anatomical neck features and feature lines. A suitable allowance can prevent pressure ulcers and maintain uniform contact forces between the user and the orthosis when worn over a long period. On the other hand, general CAD software cannot generate allowances from an irregular, complex, and concave surface. Assuming a head weight of 6 kg, we embedded the strength requirement in the software: the thickness of both the front and back pieces should be at least 5 mm from FEA results. If the head weight exceeds 6 kg, increasing the thickness is necessary to ensure safety and adequate support.
Beavis included four types of orthoses—a soft collar, rigid collar, Plastazote collar, and handmade custom-fit collar—to investigate the restriction of cervical spine motion [23]. The soft-material collar had the least effective immobilization due to its lack of a rigid support structure. In contrast, the custom-fit collar and rigid collar provided better immobilization. Given the poor immobilization capability of the soft collar, this study focuses on designing orthoses using rigid materials.
The cervical orthosis designed in this study focuses on strength, aesthetics, and ease of wear. It strategically uses key anatomical landmarks on the neck as support areas, aiming for a compact yet practical design. Specifically, it supports the head’s weight through the chin, mandibular angles, and the lower edge of the occipital bone while anchoring the orthosis to the sternum, clavicles, side neck points, and C7 (Figure 1b). This orthosis avoids contact with the throat, esophagus, aorta, and airways, ensuring the wearer usually breathes and swallows. The design considerations ensure that the orthosis provides necessary support without compromising comfort, avoiding areas that could lead to discomfort or hinder essential functions.
Due to usability considerations, rigid orthoses are generally designed as two-piece structures because their rigidity prevents deformation, necessitating division into two pieces to be effectively worn on the neck. This study developed a customized two-piece orthosis consisting of a rigid front and back support structure made of PLA. The soft material, thermoplastic polyurethane (TPU), can also be used in 3D printers. Compared to TPU material, the PLA is less elastic but has more support and immobility and is strong enough to bear the load. It was also considered that TPU can easily cause allergies, which makes it unsuitable to have contact with the skin for hours. The orthosis was fabricated by an affordable 3D printing machine (D-force V2, 3DPW, Taiwan). We set the printing parameters with an infill of 20%, a printing layer of 0.2 mm, a printing speed of 200 mm per second, and an external thickness of 0.8 mm. The contact surfaces are lined with a layer of soft material to distribute loads evenly. Typically, 3D-printed orthoses were fixed using elastic nylon straps [24]. Since these straps were single use, they were better suited for orthoses that do not require frequent removal. This study uses elastic straps with Velcro to secure the front and back pieces of the cervical orthosis. This operation was convenient and easy to put on and remove the orthosis.
Studies provide various input sources, designs, and materials for customized cervical orthoses [4,5,6,7,8]. The input sources for the neck surface in these articles were computed tomography [5,7], 3D scanners [4,6], and specific layouts of commercial sensors [8]. We used a handheld 3D scanner with a resolution of 0.5 mm to obtain body geometric models. These studies used FDM 3D printers for manufacturing, as this study did, but with different materials. The materials used include Hemp Bio-Plastic®, Boulder, CO, USA, composed of PLA and hemp shives [5,8], acrylic styrene acrylonitrile [4], acrylonitrile butadiene styrene [7], and thermoplastic elastomer flex material [6]. This study used PLA to fabricate the designed cervical orthosis.
When designing cervical orthoses, ensuring comfort and adequate ventilation is crucial. Sabyrov et al. used elliptical holes in their flexible neck orthosis design, significantly improving air circulation and reducing heat buildup [6]. Similarly, Ambu et al. found that an elliptical pattern reduces stress concentrations, making the orthosis lighter and more breathable [5]. Their subsequent study refined their approach with a Voronoi pattern, achieving better ventilation and thermal comfort [8]. Hale et al. optimized material distribution using a reaction–diffusion algorithm for improved ventilation [4]. Xu et al. used topology optimization to create specific holes for ventilation, ensuring adequate airflow and enhancing overall comfort [7]. Except for the designs mentioned above, as shown in Figure 1, our orthosis only covers regions that pass through vital anatomical features, providing maximum ventilation while maintaining necessary support.
The material utilized in this study is assumed to be isotropic for finite element analysis, although the material properties of a 3D-printed material are generally considered anisotropic. The isotropic assumption is based on the testing data obtained by Chen et al. [25], who conducted tensile testing on PLA and concluded that the variation in elastic modulus on different orientations is insignificant. The measurement data reported by Derise and Zulkharnain [19] also agree with this conclusion. Thus, the isotropic assumption in the finite element model can be accepted.
This study has certain limitations. First, the finite analysis simulations were conducted using a model of only one subject with different thicknesses, which may not fully capture the variability in human anatomy. Second, the duration of custom orthosis manufacturing was time-consuming, requiring approximately one working day for a low-cost 3D printer to complete. However, future advancements in 3D printing technology are expected to address these limitations by increasing printing speeds and offering a more comprehensive selection of materials with vibrant colors. Third, we did not compare comfort and effectiveness with a commercial neck collar to convince the user that a better design was achieved. In future work, a clinical trial is needed to evaluate the design criteria, including comfort, immobility, and contact forces between the patient and the orthosis. Fourth, we only consider static strength in four postures with the isotropic model on the 3D-printed plastic orthosis. Further anisotropic strength analysis is needed to get closer to realistic situations.
5. Conclusions
This study combines rehabilitation and anatomical knowledge to develop design software for automated personal cervical orthosis design. We applied easy-to-access 3D printing technology to fabricate well-fitting and immobilized cervical orthoses. Finite element analysis determined that a minimum orthosis thickness of 5 mm PLA material is necessary to meet strength and safety support requirements. Considering consistency with embedded anatomical settings in automation, the design of customized cervical orthoses offers a promising future with the advantages of being cost-effective, lightweight, immobility, comfortable, and easy to wear with minimal accessories to meet clinical needs.
Author Contributions
Conceptualization, J.-J.F.; methodology, Y.-H.W.; software, Y.-H.W.; validation, J.-J.F. and C.-D.C.; formal analysis, C.-D.C., data curation, Y.-H.W. and C.-D.C.; writing—original draft preparation, Y.-C.H.; writing—review and editing, J.-J.F.; visualization, Y.-C.H., C.-D.C. and Y.-H.W.; funding acquisition, J.-J.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Ministry of Science and Technology, Taiwan, grant number MOST 104-2218-E-006-011, and the APC was supported by the Ministry of Science and Technology, Taiwan.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
No new data were created in this study.
Acknowledgments
We acknowledge the medical and rehabilitation insights and support from Ruey-Mo Lin and Cheng-Li Lin from the Department of Orthopedics, China Medical University Hospital, and National Cheng Kung University Hospital, respectively. We also appreciate Yi-Cheng Shi from the Department of Mechanical Engineering, National Cheng Kung University, for his help with the finite element analysis.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Agabegi, S.S.; Asghar, F.A.; Herkowitz, H.N. Spinal orthoses. J. Am. Acad. Orthop. Surg. 2010, 18, 657–667. [Google Scholar] [CrossRef] [PubMed]
- Gao, F. Effectiveness of adjustable cervical orthoses and modular cervical thoracic orthoses in restricting neck motion: A comparative in vivo biomechanical study. Spine 2015, 40, E1046–E1051. [Google Scholar] [CrossRef] [PubMed]
- Kuo, Y.-R.; Fang, J.-J.; Wu, C.-T.; Lin, R.-M.; Su, P.-F.; Lin, C.-L. Analysis of a customized cervical collar to improve neck posture during smartphone usage: A comparative study in healthy subjects. Eur. Spine J. 2019, 28, 1793–1803. [Google Scholar] [CrossRef]
- Hale, L.; Linley, E.; Kalaskar, D.M. A digital workflow for design and fabrication of bespoke orthoses using 3D scanning and 3D printing, a patient-based case study. Sci. Rep. 2020, 10, 7028. [Google Scholar] [CrossRef] [PubMed]
- Ambu, R.; Motta, A.; Calì, M. Design of a customized neck orthosis for FDM manufacturing with a new sustainable bio-composite. In Proceedings of the International Conference on Design Tools and Methods in Industrial Engineering, ADM 2019, Modena, Italy, 20 September 2020; pp. 707–718. [Google Scholar]
- Sabyrov, N.; Sotsial, Z.; Abilgaziyev, A.; Adair, D.; Ali, M.H. Design of a flexible neck orthosis on fused deposition modeling printer for rehabilitation on regular usage. Procedia Comput. Sci. 2021, 179, 63–71. [Google Scholar] [CrossRef]
- Xu, Y.; Li, X.; Chang, Y.; Wang, Y.; Che, L.; Shi, G.; Niu, X.; Wang, H.; Li, X.; He, Y. Design of personalized cervical fixation orthosis based on 3D printing technology. Appl. Bionics Biomech. 2022, 2022, 8243128. [Google Scholar] [CrossRef]
- Ambu, R.; Oliveri, S.M.; Calì, M. Neck orthosis design for 3D printing with user enhanced comfort features. Int. J. Interact. Des. Manuf. 2023, 1–14. [Google Scholar] [CrossRef]
- Li, J.; Tanaka, H. Feasibility study applying a parametric model as the design generator for 3D–printed orthosis for fracture immobilization. 3D Print. Med. 2018, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.E.; Dupont, K.M.; Safranski, D.L.; Blair, J.; Buratti, D.; Zeetser, V.; Callahan, R.; Lin, J.; Gall, K. Use of 3D printed bone plate in novel technique to surgically correct hallux valgus deformities. Tech. Orthop. 2016, 31, 181–189. [Google Scholar] [CrossRef]
- Baronio, G.; Harran, S.; Signoroni, A. A critical analysis of a hand orthosis reverse engineering and 3D printing process. Appl. Bionics Biomech. 2016, 2016, 8347478. [Google Scholar] [CrossRef]
- Choo, Y.J.; Boudier-Revéret, M.; Chang, M.C. 3D printing technology applied to orthosis manufacturing: Narrative review. Ann. Palliat. Med. 2020, 9, 4262–4270. [Google Scholar] [CrossRef]
- Bäcker, H.C.; Elias, P.; Braun, K.F.; Johnson, M.A.; Turner, P.; Cunningham, J. Cervical immobilization in trauma patients: Soft collars better than rigid collars? A systematic review and meta-analysis. Eur. Spine J. 2022, 31, 3378–3391. [Google Scholar] [CrossRef] [PubMed]
- Serratosa, F. Fast computation of bipartite graph matching. Pattern Recognit. Lett. 2014, 45, 244–250. [Google Scholar] [CrossRef]
- Jonker, R.; Volgenant, T. Improving the Hungarian assignment algorithm. Oper. Res. Lett. 1986, 5, 171–175. [Google Scholar] [CrossRef]
- Kimmel, R.; Sethian, J.A. Computing geodesic paths on manifolds. Proc. Natl. Acad. Sci. USA 1998, 95, 8431–8435. [Google Scholar] [CrossRef]
- Kim, S.-J.; Lee, D.-Y.; Yang, M.-Y. Offset triangular mesh using the multiple normal vectors of a vertex. Comput. Aided Des. Appl. 2004, 1, 285–291. [Google Scholar] [CrossRef]
- Field, D.A. Laplacian smoothing and Delaunay triangulations. Commun. Appl. Numer. Methods 1988, 4, 709–712. [Google Scholar] [CrossRef]
- Derise, M.R.; Zulkharnain, A. Effect of infill pattern and density on tensile properties of 3d printed polylactic acid parts via fused deposition modeling (FDM). Int. J. Mech. Mechatron. Eng. 2020, 20, 54–63. [Google Scholar] [CrossRef]
- Vasavada, A.N.; Li, S.; Delp, S.L. Three-dimensional isometric strength of neck muscles in humans. Spine 2001, 26, 1904–1909. [Google Scholar] [CrossRef]
- Harms-Ringdahl, K.; Ekholm, J.; Schüldt, K.; Németh, G.; Arborelius, U.P. Load moments and myoelectric activity when the cervical spine is held in full flexion and extension. Ergonomics 1986, 29, 1539–1552. [Google Scholar] [CrossRef] [PubMed]
- Ezeh, O.; Susmel, L. Fatigue strength of additively manufactured polylactide (PLA): Effect of raster angle and non-zero mean stresses. Int. J. Fatigue 2019, 126, 319–326. [Google Scholar] [CrossRef]
- Beavis, A. Cervical orthoses. Prosthet. Orthot. Int. 1989, 13, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Buonamici, F.; Furferi, R.; Governi, L.; Lazzeri, S.; McGreevy, K.S.; Servi, M.; Talanti, E.; Uccheddu, F.; Volpe, Y. A practical methodology for computer-aided design of custom 3D printable casts for wrist fractures. Vis. Comput. 2020, 36, 375–390. [Google Scholar] [CrossRef]
- Chen, C.-D.; Chen, C.-H.; Lin, C.-L.; Lin, C.-K.; Wang, C.-T.; Lin, R.-M.; Fang, J.-J. Developments, mechanical property measurements and strength evaluations of the wrist braces for the wrist fracture patients. J. Mech. Med. Biol. 2019, 19, 1940021. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).