Abstract
Neck pain can induce specific motor responses and alterations in muscle strength. Therefore, this study aimed to investigate and compare the progression of cervical muscle strength within and between students with and without neck pain over the course of their first semester of clinical training. We used an online Nordic Musculoskeletal Questionnaire for group allocation, and neck strength in flexion, extension, and lateral flexion on both sides was measured using the KForce Bubble Pro hand-held dynamometer. Forty-four students were divided into neck pain (n = 21) and asymptomatic (n = 23) groups. Both groups increased neck strength by the end of the semester in flexion, extension, and left and right lateral flexion (p < 0.001). Students experiencing neck pain showed a significantly lesser degree of improvement (p = 0.036) in right lateral flexion. The agonist/antagonist ratios revealed an enhanced role of neck extensors across both groups. Dental students showed overall increased cervical strength in their first semester of clinical training. Those with neck pain exhibited a diminished rate of strength gain in right lateral flexion when compared with students without pain by the semester’s end, suggesting different neuromuscular adjustments to clinical practice in students experiencing pain, which may lead to functional impairments in later training stages.
1. Introduction
Work-related musculoskeletal disorders (WMSDs) represent a significant health concern [1], especially among dental professionals and dental students [2,3,4,5], with 95.8% of dentists reporting these issues in their lifetime [6]. Notably, the onset of these disorders is often reported during the early stages of their professional training, with a wide-ranging occurrence rate between 44 and 93% [2,7,8,9,10,11]. These disorders are frequently aggravated by the unique demands of the dental profession [6,12]. Dental professionals are particularly vulnerable due to the static and asymmetrical postures as well as repetitive movements that are inherent in their daily work [2,8,9,10,11]. In dental students, the physical strain is particularly prevalent in the neck region. A meta-analysis indicated a 12-month occurrence rate of neck pain ranging from 44 to 69% [11,13,14,15] among these students. This rate significantly exceeds the general population’s reported rate by more than tenfold [16,17] and is three times higher than that reported for the broader working population [18]. Pain, inherently a multifactorial phenomenon, is characterized by unique experiences that induce specific motor responses and alterations [19,20]. Specifically, cervical pain has been linked to alterations in muscle strength [21,22,23,24,25,26,27,28] and motor unit activity [21,22,23,26,29,30,31], and these changes are critically related to the potential development and progression of chronic postural neck pain [23,32]. Furthermore, contractions at unfavorable muscle lengths and awkward moment angles during biaxial movements have been shown to reduce muscle strength by 40–56% [33], depending on the plane of motion. This reduction in strength hinders the muscles from reaching their normal strength potential, leading to increased fatigue over extended working hours and often resulting in imbalances and pain.
A variety of methods for assessing cervical segment strength are available, each with its own set of limitations [34]. However, according to a systematic review [35], hand-held dynamometers (HHD) are a reliable and valid instrument for measuring muscle strength. This assertion was further supported by recent studies [36,37,38] that found good to excellent correlation for the isometric strength in healthy populations, particularly for proximal muscle groups. These findings validate the use of HHD as a reliable and straightforward test for evaluating maximal isometric cervical muscle strength both in healthy patients [38] and those with neck pain [39].
We hypothesize that students without neck pain will demonstrate an increase in neck strength because of their exposure to clinical training, and the presence of neck pain in other students will inhibit their ability to achieve similar strength adaptations. Therefore, we aimed to investigate and compare the progression of cervical muscle strength within and between students with and without neck pain over the course of their first semester of clinical training.
2. Materials and Methods
2.1. Study Design
This was a longitudinal study approved by the Egas Moniz School of Health & Science Ethics Committee, under the number CEEM-1122, in September 2022. All participant data were anonymized and treated confidentially, in compliance with the European Union General Data Protection Regulation, and are scheduled for deletion in December 2028. All methodologies applied within the study rigorously adhered to the ethical principles rooted in the 1975 Declaration of Helsinki, as revised in 2008. This study’s design and findings were reported following the guidelines of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [40].
2.2. Participants
Fourth-year dental students enrolled in the master’s degree in dentistry at Egas Moniz School of Health & Science—Portugal, volunteered to participate in the study. Participants were categorized into one of two groups based on their responses to the Nordic Musculoskeletal Questionnaire (NMQ): asymptomatic for the control group (CG) or fourth-year students with neck pain (NP). The allocation to groups was blinded to all investigators and assessors. Inclusion criteria were (i) students actively involved in clinical practice and (ii) students from the fourth year. Exclusion criteria were (i) students who had clinical practice before September 2023; (ii) studentss over 30 years of age; (iii) students with ongoing musculoskeletal disorders; (iv) the inability or unwillingness to provide informed consent; (v) communication difficulties with investigators; (vi) major neurological disorders; (vii) dysfunctions of the central or peripheral nervous system; (viii) a diagnosis of schizophrenia, bipolar disorder, or other psychotic disorders; (ix) alcohol or other substance abuse; or (x) major depression.
A sample size minimum of 28 participants was calculated with GPower software (v.3.1.9.7, Düsseldorf University, Düsseldorf, Germany) considering α = 0.05 (5% chance of type one error), a minimum 1 − β = 0.95, (% of power of the sample), and a large effect size of 0.361 [41].
2.3. Procedure
To allocate the students between groups, we employed an online method that included the informed consent and the Nordic Musculoskeletal Questionnaire (NMQ) [42]. The questionnaire was administered twice: at the start of the curricular year in September and at the semester’s end in December. Participants were required to read and provide their consent digitally before proceeding to complete the questionnaire and the subsequent strength testing.
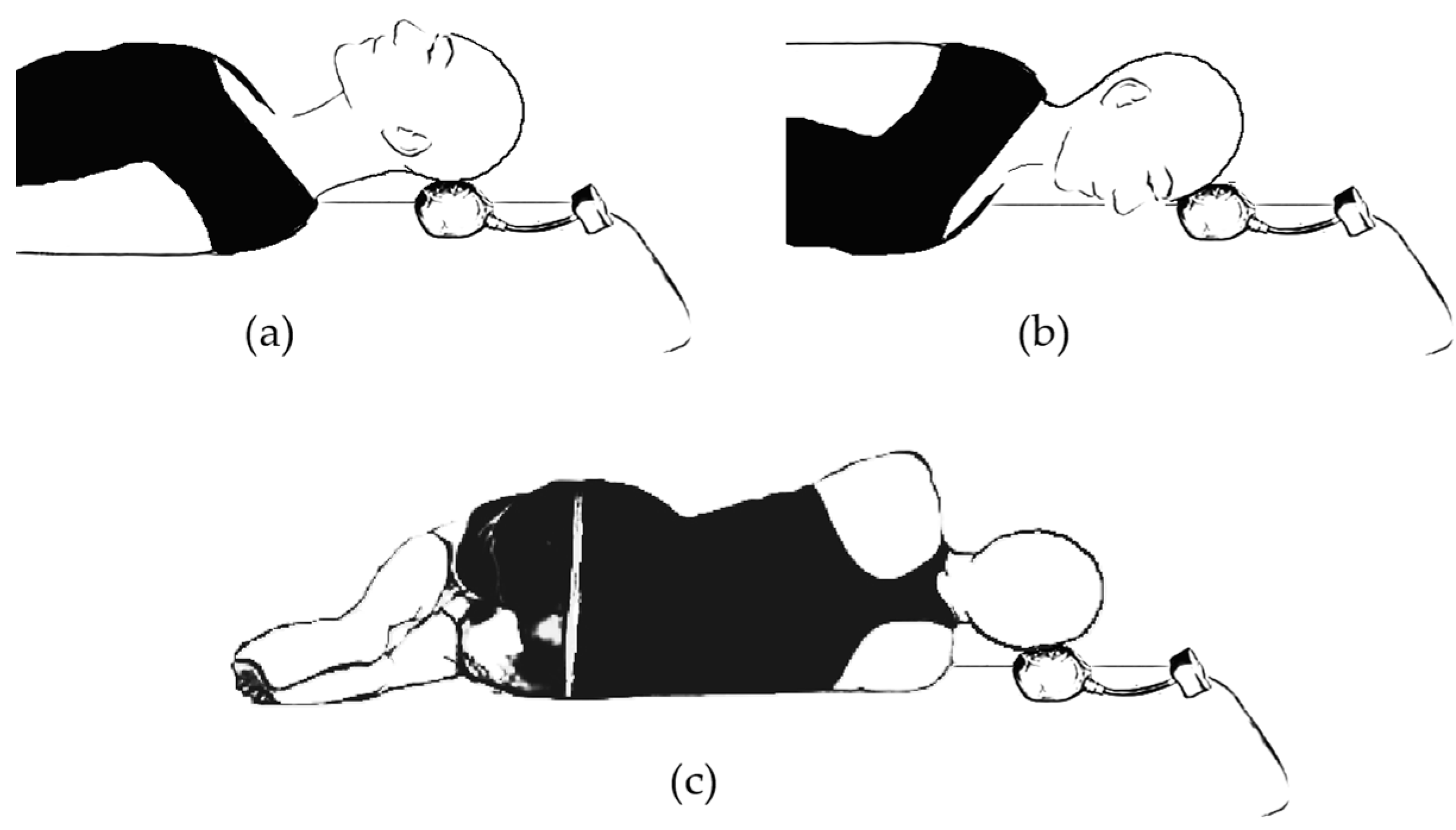
Neck strength in flexion, extension, and lateral flexion on both sides was assessed using the KForce Bubble Pro (Kinvent, Montpellier, France) hand-held dynamometer during maximum voluntary isometric contractions (MVIC), in line with the latest recommendations [43]. Prior to data collection, participants were trained and instructed on proper movement execution. The assessment utilized a “make test”, wherein participants exerted maximum force against the dynamometer anchored to the examination couch. For flexion measurements, participants were in a prone position, while extension assessments were conducted in a supine position with arms at the sides. Lateral flexion was measured in a side decubitus position with knees and hips flexed at 45 degrees and arms crossed over the chest. A diagrammatic representation of the assessment positions is provided in Figure 1. Participants were instructed to gradually increase contraction for one second to minimize positional and stabilization errors, followed by a verbal directive to exert maximum force for five seconds. Each participant performed three consecutive maximal effort actions for each movement, with 5-s durations and 30-s rest intervals to prevent fatigue, and the best repetition was used for analysis. Eventual position and stabilization errors implied the repetition of the MVIC test. The testing sequence was randomized for each participant.
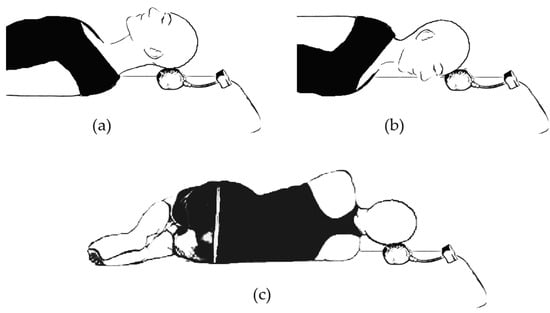
Figure 1.
Strength assessment positions: (a) supine position for neck extensors assessment; (b) prone position for neck flexors assessment; (c) side decubitus for neck lateral flexors assessment.
According to the widely accepted assumption of “geometric similarity” (i.e., all human bodies have the same shape, so they only differ in size), muscle force should be proportional to either body height squared or body mass raised to the power of two-thirds (m2/3) [44]. Therefore, to ensure the comparability of muscle strength test outcomes among different participants and studies, we utilized the allometric scaling method [44] based on the equation Sn = S/mb, where Sn (normalized strength) is found, dividing muscle strength (S), recorded as muscle force, by body mass (m) raised to the allometric exponent (b), which is set at 0.67 for dynamometer-recorded muscle force, to facilitate the assessment of body-size-independent muscle strength indices [44].
2.4. Statistical Analysis
We used Jamovi (v 2.4.8) [45,46,47,48] for the statistical analysis. Following the verification of normality (Shapiro–Wilk) and homogeneity of variances (Levene’s), a repeated-measures analysis of variance (ANOVA) was employed to analyze differences within and between the groups, including a Tukey’s post hoc adjustment. The alpha significance level was set at 0.05.
3. Results
Sixty students were approached to participate in our study. Of these, three declined to participate. The remaining 57 students agreed to participate and proceeded to data collection. During the study, 13 (22.8%) participants dropped out after failing the second assessment, culminating in a final sample of 44 participants. The participants were 68.2% women (n = 30) and 31.8% men (n = 14) with the average age of 22.34 ± 2.06 years and an average body mass index (BMI) of 21.76 ± 3.07 kg/m2. Analysis of the NMQ data allowed the allocation of the participants between the two groups. The control group (n = 23) comprised students without neck pain, while the neck pain group (n = 21) was composed of 4th-year students with neck pain. Comprehensive sociodemographic information on the participants is detailed in Table 1.

Table 1.
Sociodemographic characteristics of the participants.
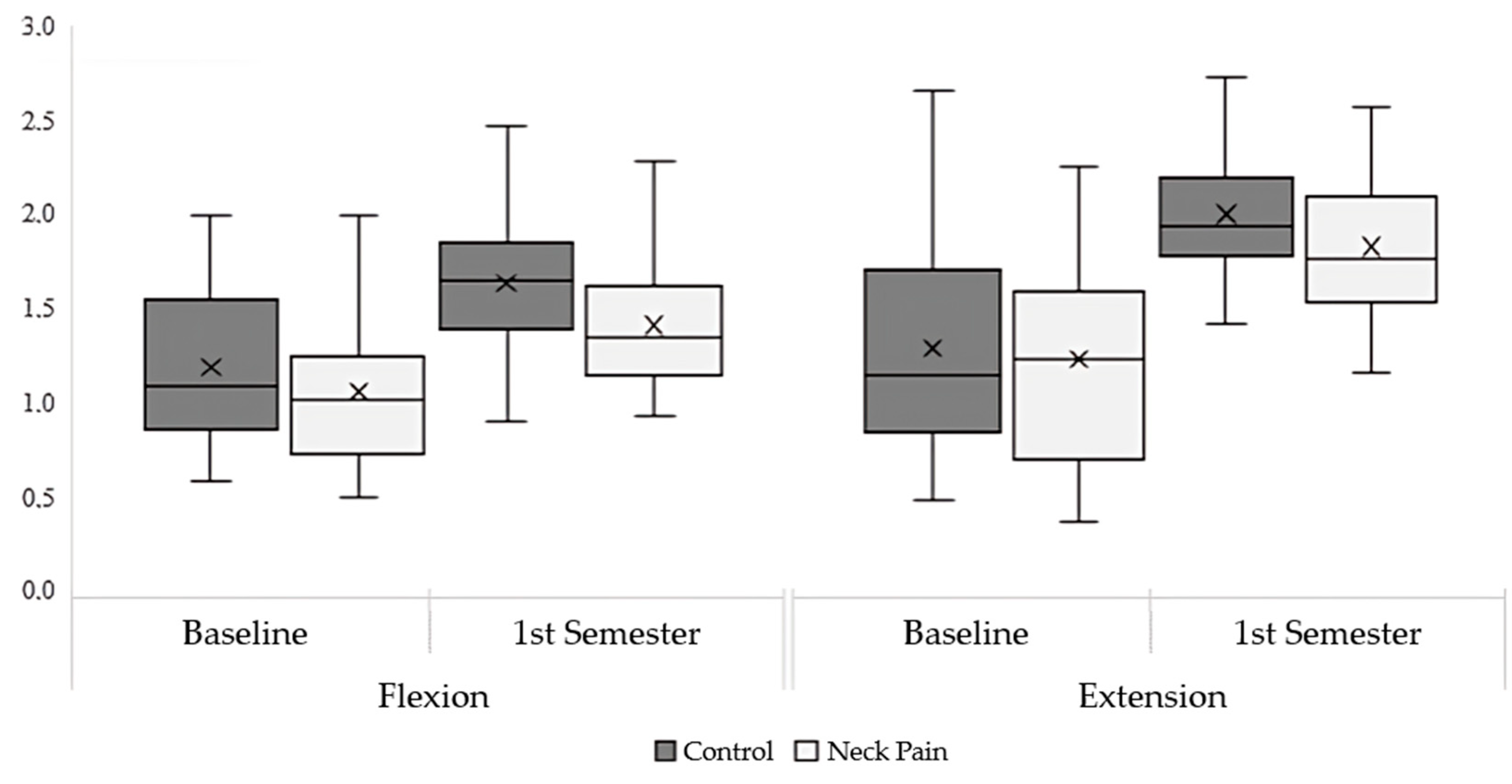
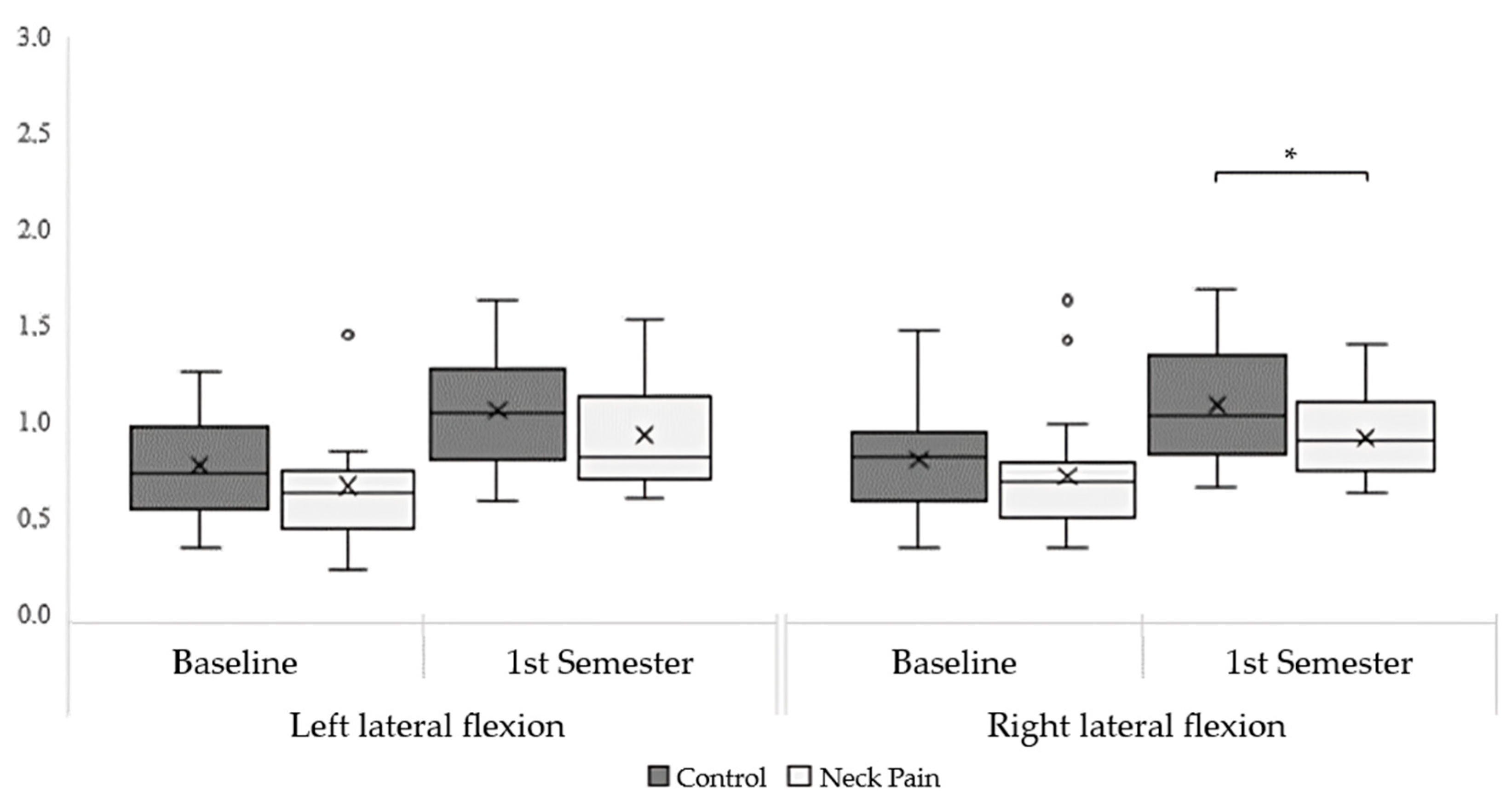
Both groups had similar neck strength at the baseline. At the end of the first semester, the neck pain group had less right lateral flexion strength than the asymptomatic group [t(42) = 2.83; p = 0.034]. The cervical strength in flexion [t(42) = 2.11; p = 0.165], extension [t(42) = 1.77; p = 0.302], and left lateral flexion [t(42) = 2.36; p = 0.101] remained similar between groups. In a within analysis, both groups increased their strength levels throughout the semester for all movements. Neck flexion [F(1, 42) = 39.1; p < 0.001; η2p = 0.482] increased in the CG [mean difference (MD) = 0.417; standard error (SE) = 0.093; t(42) = 4.48; p < 0.001] and NP groups [MD = 0.388; SE = 0.089; t(42) = 4.37; p < 0.001]. Extension [F(1, 42) = 69.0; p < 0.001; η2p = 0.622] increased in the CG [MD = 0.670; SE = 0.113; t(42) = 5.91; p < 0.001] and NP groups [MD = 0.633; SE = 0.108; t(42) = 5.84; p < 0.001]. Right lateral flexion [F(1, 42) = 31.1; p < 0.001; η2p = 0.432] increased in the CG [MD = 0.310; SE = 0.069; t(42) = 4.52; p < 0.001] and NP groups [MD = 0.225; SE = 0.067; t(42) = 3.36; p = 0.009]. Left lateral flexion [F(1, 42) = 31.9; p < 0.001; η2p = 0.438] increased in the CG [MD = 0.296; SE = 0.075; t(42) = 3.97; p < 0.002] and NP groups [MD = 0.292; SE = 0.073; t(42) = 4.02; p = 0.001]. Figure 2 and Figure 3 graphically depict these results, illustrating the comparative strength changes in each group for all movements.
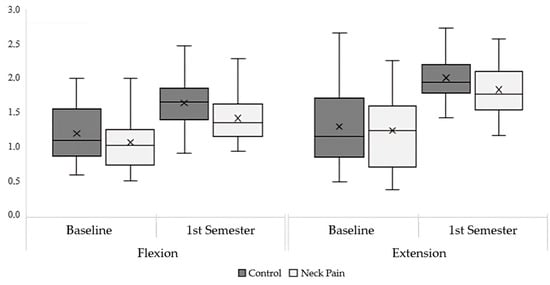
Figure 2.
Neck flexion and extension strength normalized by body weight.
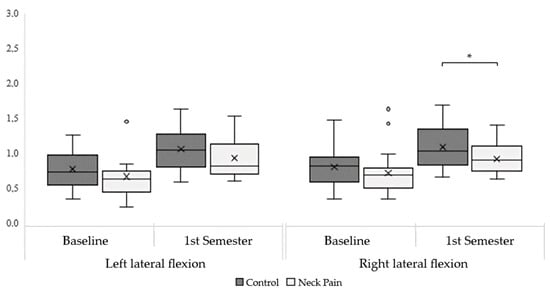
Figure 3.
Neck left and right lateral flexion strength normalized by body weight. * = p-value < 0.05.
Table 2 presents the neck strength ratios of agonists to antagonists for the two study groups at baseline and at the end of the first semester, compared with established normative values for male and female individuals aged 18 to 35 years. Both groups presented ratios closer to the reference values after the first fifteen weeks of clinical practice.

Table 2.
Neck strength ratios.
4. Discussion
Neck pain is increasingly acknowledged as a significant cause of disability globally, affecting 4.82% of the population and ranking as the fourth leading cause of disability worldwide [16,17], increasing the importance of its study. This condition is also becoming a more prevalent health concern in workplace settings [1], where it annually impacts 11% to 14.1% of workers worldwide [18]. The prevalence of neck pain among dental professionals is alarmingly high, with studies showing that 44 to 69% of dental students experience neck pain from the initial stages of their training [11,13,14,15]. This issue is further emphasized by multiple studies identifying neck pain as the primary anatomical region affected by work-related musculoskeletal disorders in this group [2,6,8,9,10,12,50], turning it into a significant concern for this professional class and its stakeholders. The heightened incidence of neck pain in dental students is largely attributed to the strenuous nature of their educational journey, encompassing intensive theoretical and practical training, ex-aminations, and the challenges posed by their relative inexperience compared to more seasoned dental practitioners [2,8,9,10,11,51]. Although pain has a multifactorial aspect, where each individual experience may trigger unique motor responses and alterations [19,20], cervical pain has been associated with changes in muscle strength [21,22,23,24,25,26,27,28] and motor unit activity [21,22,23,26,29,30,31]. These alterations are related to the possible development and progression of chronic musculoskeletal neck pain [23,32]. To improve our knowledge on this issue, we investigated and compared the progression of cervical muscle strength within and between students with and without neck pain over the course of their first semester of clinical training.
The students’ pain conditions remained consistent throughout the 15-week study, with only minor variations in pain intensity. At baseline, we observed slightly inferior but non-significant levels of neck strength in the students with neck pain for all movements. At the end of the first semester, both groups increased their neck strength levels for all muscle groups assessed, with a significant lesser degree of improvement in the neck right flexion of the group with neck pain, while the other three muscular groups remained similar. This finding opposed our hypothesis since we expected to observe an increase in neck strength in the students without pain due to their exposure to a new task with their clinical training but not in the students with neck pain, where we expected the strength to remain without differences or with a tendency to decrease as the physical strain and accumulated hours of training built up. Our rational thinking was based on the belief that the decline in neck strength originates from persistent neck pain related to the mechanical overload encountered during clinical practice among students. This overload associated with existing pain could trigger muscle inhibition [26,29,30,31,52] and avoidance patterns [27,53], ultimately resulting in aggravated cervical muscle weakness [26,27,28,41]. However, our findings showed a different dynamic in the neck strength, with both groups increasing their strength levels from the start to the end of the semester. It is known that a rapid rise in strength within the first two weeks of exposure is primarily due to neuromuscular adaptations [54,55]. Therefore, a possible explanation for this is that the exposure to the clinical practice overcame the negative neuromuscular adaptations associated with neck pain, allowing a similar muscular response to clinical training exposure. Despite our knowledge that higher loads promote greater changes in muscle architecture and function [56], several studies have reported that exposure to high levels of localized and sustained muscle activation produced from repeated contractions can provide sufficient stimulation of skeletal muscle to induce muscle changes both in size and function [57,58]. Hence, the engagement in a new activity seems to have promoted muscular adaptations independent of the previously reported neck pain, confirming that robust muscle changes can occur independent of an external load provided [57]. A possible interpretation for our findings could be the pain’s multidimensionality, which includes physical, psychological, and social aspects [19,20] such as anxiety, stress, quality of life, or kinesiophobia. Pain’s inherent complexity might explain the observed improvements in neck strength among both groups, contrary to our initial hypothesis. The subjective nature of pain, shaped by emotional and cognitive influences, allows for individual variations in pain experience and responses to management strategies. Therefore, individuals experiencing neck pain could still manifest gains in strength, potentially due to shifts in pain perception, enhanced coping mechanisms, and a greater tolerance for pain. Our results seem to underscore the necessity for a comprehensive approach to pain management, recognizing that interventions may need to address more than the physical symptoms.
Although the changes within groups evolved differently from our hypothesis, the comparison between groups shown that despite their increasing levels of strength, the students with neck pain had a reduced rate of strength gain since the mean difference be-tween groups increased for all movements and became significative for the neck right lateral flexion movement. This finding is in line with our hypothesis that the strength differences between groups would increase over time as the increasing physical strain and accumulated clinical practice hours could aggravate the neck pain, inducing the known changes [19,20,21,22,23,24,25,26,27,28,29,30,31]. Our study comprised a 15-week period, and knowing that isometric force reaches a plateau between 12 to 16 weeks of exposure to training [54], we could speculate that once the initial muscle adaptation and the associated neuromuscular function is made and stabilized, a shift in the dynamics of neck strength, function, and pain could occur, increasing the influence of the pain, associated neuromuscular changes, and avoidance behaviors, with the difference in neck strength between these students further increasing. The belief that these differences could increase over time is based on the previously re-ported mechanism showing that working at static load levels as low as 2–5% of maximum muscle strength has been shown to cause objectively verifiable (in microscopic muscle samples and with electromyography) pathological changes, particularly in the trapezius muscle, which stabilizes the shoulder blade and entire arm. The changes can be demonstrated in everyone with pain but occasionally also occurs in those who are pain-free. Characteristic of the low load levels causing this type of muscle injury is that they occur constantly during the entire working day, such as in dentistry clinical work, since few opportunities are given for complete muscle relaxation [59]. Knowing that pain is not only influenced by organic pathology but also by induced pain-related fears, students may react with avoidance behaviors, and its persistence beyond the expected tissue healing time will prolong and exaggerate the pain and fear, causing detrimental effects to patients [53]. Pain, characterized by its multidimensional aspects and complex origins, serves as a balance between promoting and protective factors. The manifestation of pain emerges from the complex interplay of these variables [19,20], which are subject to change over the lifespan and during shorter periods, such as the two-year clinical practice undertaken by these students, which reinforces the needs for observing the evolving dynamics between these variables throughout their training.
Knowing that the disrupted balance between agonists and antagonists of the different cervical movements can lead to cervical insufficiency, which has been identified as a causing or contributing factor in the pathogenesis of head and neck pain [41,54,60], the analysis of the evolving dynamics of these ratios is essential. In our study, dental students without pain exhibited an increased flexion/extension ratio at baseline (0.92) and a similar ratio of left and right lateral flexors (0.97) compared to the established normative values for their respective age group [49], which indicated an increased influence of neck flexors in this agonist/antagonist ratio. Compared with these students, the group with neck pain had marginal lower flexion/extension ratios at baseline and a sign of imbalance in left and right lateral flexors (0.93), which should have an equivalent strength represented by a ratio closer to 1. After 15 weeks, at the end of the semester, the flexion/extension ratio of both groups decreased, which could be related to their initial exposure to clinical practice and consequent solicitation of neck extensors, enhancing their role in the agonist–antagonist relationship between neck flexors and extensors in students from both groups. For the lateral flexors, we observed a different pattern, with the ratio increasing and representing an approximation of the neck strength in both sides, representing the tendency of lateral flexors to reach equivalent strength when exposed to clinical training, hence a ratio closer to 1. However, we expect this tendency to end and the imbalance to rise again as the students with neck pain accumulate more clinical practice hours. This assumption is based on the observation that sustained cervical rotation leads to increased activity in the contralateral flexor muscles [61]. This phenomenon is often associated with pain, which in turn is linked to deficits in neck strength and abnormal muscle activation patterns [62]. Such patterns are likely to contribute to the anticipated agonist/antagonist imbalance, a correlation that is further supported by previous findings of enhanced co-activation in antagonist muscles among patients with neck pain [54,60].
While our study did not gather data on the specific side of the pain, the results pre-sent an indication of an asymmetric response regarding neck strength output. This tendency is coherent with our expectations based on the asymmetrical nature of these students’ clinical practice since in our university’s clinical settings, students typically approach patients from the right side, often adopting a posture that involves neck flexion combined with left lateral flexion and rotation. The work-related factors, including neck posture, direction of exertion, and exertion level, are key determinants of neck functional capacities [1]. For neck-related occupational tasks, sustained exertions at submaximal or moderate force levels are more prevalent compared to exertions of high force. Consequently, changes in activity that result in reduced endurance might be more relevant for understanding the causation and prevention of neck pain [1].
While our study made efforts to address the shortcomings of previous research, it still faced some limitations. One notable limitation is the use of a HHD to measure neck strength, which, although valid, is not the gold-standard method for such assessments. Additionally, the presence of an unbalanced sex distribution in the neck pain group, while determined by the NMQ and mitigated by the normalization with the allometric scaling method, could still have introduced bias into the results. Furthermore, our study, though longitudinal in nature, covered only the first 15 weeks of a 60-week clinical training program. To effectively address these limitations, future research should consider utilizing an isokinetic dynamometer for measuring neck strength. This would not only provide a more precise assessment but also allow the exploration of critical variables such as force steadiness and the functional ratio of neck muscles in dental students. Additionally, extending the longitudinal aspect of the study to cover a broader period, ideally the entire two years of clinical training, would provide a more comprehensive understanding of the development and progression of neck pain and related issues. Moreover, future research should investigate other variables potentially associated with neck pain in dental students, including psychosocial aspects, academic performance, and alterations in motor behavior, including its impact on postural control adaptations and an analysis of neck activation patterns, allowing a more comprehensive understanding of the neuromuscular adaptations in dental students and their implications for educational and professional development outcomes.
5. Conclusions
In our study, we observed that all students increased their neck strength when exposed to their first semester of clinical training. Despite the observed effect, by the end of the first semester, students with neck pain exhibited a reduced rate of strength gain in the right lateral flexion movement. Regardless of their similar clinical training, the neck strength adaptations resulting from this exposure were less evident in the neck pain group. The neuromuscular adaptations to clinical practice seem to occur at a different rate in students with pain. The reduced rate of strength gain in one muscular group may not reflect immediate adaptive differences but could indicate the potential for more significant changes and impairments in the future, possibly leading to greater cervical strength differences as training progresses.
Author Contributions
Conceptualization, M.B.A., M.M., P.M.-A. and R.O.; data curation, M.B.A. and M.M.; formal analysis, M.B.A., P.M.-A. and R.O.; funding acquisition, M.B.A. and R.O.; investigation, M.B.A. and M.M.; methodology, M.B.A., M.M., P.M.-A. and R.O.; project administration, M.B.A.; resources, M.B.A.; supervision, P.M.-A. and R.O.; validation, P.M.-A. and R.O.; writing—original draft, M.B.A.; writing—review and editing, M.B.A., M.M., P.M.-A. and R.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research was developed within the scope of the Egas Moniz Multidisciplinary Research Center (CiiEM) and funded by Portugal’s national funds through the FCT—Foundation for Science and Technology, I.P. under the project 10.54499/UIDB/04585/2020.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by Egas Moniz School of Health & Science Ethics Committee (Approval No. CEEM-1122, 27 September 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original data presented in the study are openly available in Mendeley Data at https://data.mendeley.com/datasets/hm7xw26kjd/1, accessed on 2 January 2024.
Acknowledgments
We would like to address our special thanks to André Júdice for his valuable support and to the participating students whose contributions were vital to the success of this study.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Chowdhury, S.K.; Zhou, Y.; Wan, B.; Reddy, C.; Zhang, X. Neck strength and endurance and associated personal and work-related factors. Human Factors 2022, 64, 1013–1026. [Google Scholar] [CrossRef] [PubMed]
- Ohlendorf, D.; Naser, A.; Haas, Y.; Haenel, J.; Fraeulin, L.; Holzgreve, F.; Erbe, C.; Betz, W.; Wanke, E.M.; Brueggmann, D.; et al. Prevalence of Musculoskeletal Disorders among Dentists and Dental Students in Germany. Int. J. Environ. Res. Public Health 2020, 17, 8740. [Google Scholar] [CrossRef]
- Lietz, J.; Kozak, A.; Nienhaus, A. Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in Western countries: A systematic literature review and meta-analysis. PLoS ONE 2018, 13, e0208628. [Google Scholar] [CrossRef]
- Feng, B.; Liang, Q.; Wang, Y.; Andersen, L.L.; Szeto, G. Prevalence of work-related musculoskeletal symptoms of the neck and upper extremity among dentists in China. BMJ Open 2014, 4, e006451. [Google Scholar] [CrossRef] [PubMed]
- Ohlendorf, D.; Haas, Y.; Naser, A.; Haenel, J.; Maltry, L.; Holzgreve, F.; Erbe, C.; Betz, W.; Wanke, E.M.; Brüggmann, D.; et al. Prevalence of Muscular Skeletal Disorders among Qualified Dental Assistants. Int. J. Environ. Res. Public Health 2020, 17, 3490. [Google Scholar] [CrossRef]
- Hayes, M.; Cockrell, D.; Smith, D. A systematic review of musculoskeletal disorders among dental professionals. Int. J. Dent. Hyg. 2009, 7, 159–165. [Google Scholar] [CrossRef]
- de Almeida, M.B.; Moleirinho-Alves, P.; Oliveira, R. Work-related musculoskeletal disorders among dental students: A cross-sectional study integrating the pain adaptation model. J. Public Health 2024, 1–8. [Google Scholar] [CrossRef]
- Kapitán, M.; Pilbauerová, N.; Vavřičková, L.; Šustová, Z.; Machač, S. Prevalence of musculoskeletal disorders symptoms among Czech dental students. Part 1: A questionnaire survey. Acta Med. 2019, 61, 131–136. [Google Scholar] [CrossRef]
- Aboalshamat, K.T. Nordic assessment of occupational disorders among dental students and dentists in Saudi Arabia. J. Int. Soc. Prev. Community Dent. 2020, 10, 561. [Google Scholar] [CrossRef]
- Ng, A.; Hayes, M.J.; Polster, A. Musculoskeletal disorders and working posture among dental and oral health students. Healthcare 2016, 4, 13. [Google Scholar] [CrossRef]
- Almeida, M.B.; Póvoa, R.; Tavares, D.; Alves, P.M.; Oliveira, R. Prevalence of musculoskeletal disorders among dental students: A systematic review and meta-analysis. Heliyon 2023, 9, e19956. [Google Scholar] [CrossRef] [PubMed]
- Suganthirababu, P.; Parveen, A.; Mohan Krishna, P.; Sivaram, B.; Kumaresan, A.; Srinivasan, V.; Vishnuram, S.; Alagesan, J.; Prathap, L. Prevalence of work-related musculoskeletal disorders among health care professionals: A systematic review. Work 2022, 74, 455–467. [Google Scholar] [CrossRef] [PubMed]
- Santos, R.R.; Garbin, C.A.S.; Batista, J.A.; Saliba, T.A.; Garbin, A.J.I. Prevalence of musculoskeletal pain in dental students and associated factors. Braz. J. Oral. Sci. 2019, 18, e191668. [Google Scholar] [CrossRef]
- Murtaza, F.; Habib, M.U.; Raza, M.A.; Jafri, M.R.; Shah, S.M. Prevalence of musculoskeletal disorders among dentistry students in clinical work environment of Lahore, Pakistan. Rawal Med. J. 2021, 46, 361. [Google Scholar]
- Felemban, R.A.; Sofi, R.A.; Alhebshi, S.A.; Alharbi, S.G.; Farsi, N.J.; Abduljabbar, F.H.; Farsi, J.M. Prevalence and predictors of musculoskeletal pain among undergraduate students at a dental school in Saudi Arabia. Clin. Cosmet. Investig. Dent. 2021, 13, 39–46. [Google Scholar] [CrossRef]
- Bernabé, E.; Hay, R.J.; Wolfe, C.D.; Shibuya, K. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1260–1344. [Google Scholar] [CrossRef]
- Hoy, D.; March, L.; Woolf, A.; Blyth, F.; Brooks, P.; Smith, E.; Vos, T.; Barendregt, J.; Blore, J.; Murray, C. The global burden of neck pain: Estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 2014, 73, 968–974. [Google Scholar] [CrossRef] [PubMed]
- Côté, P.; van der Velde, G.; Cassidy, J.D.; Carroll, L.J.; Hogg-Johnson, S.; Holm, L.W.; Carragee, E.J.; Haldeman, S.; Nordin, M.; Hurwitz, E.L. The burden and determinants of neck pain in workers: Results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008, 33, S60–S74. [Google Scholar] [CrossRef]
- Peck, C.; Murray, G.; Gerzina, T. How does pain affect jaw muscle activity? The Integrated Pain Adaptation Model. Aust. Dent. J. 2008, 53, 201–207. [Google Scholar] [CrossRef]
- Murray, G.M.; Peck, C.C. Orofacial pain and jaw muscle activity: A new model. J. Orofac. Pain. 2007, 21, 263–278, discussion 279–288. [Google Scholar]
- Wytra̦żek, M.; Huber, J.; Lisiński, P. Changes in muscle activity determine progression of clinical symptoms in patients with chronic spine-related muscle pain. A complex clinical and neurophysiological approach. Funct. Neurol. 2011, 26, 141. [Google Scholar] [PubMed]
- O’Leary, S.; Falla, D.; Jull, G. The relationship between superficial muscle activity during the cranio-cervical flexion test and clinical features in patients with chronic neck pain. Man. Ther. 2011, 16, 452–455. [Google Scholar] [CrossRef]
- Gilchrist, I.; Storr, M.; Chapman, E.; Pelland, L. Neck muscle strength training in the risk management of concussion in contact sports: Critical appraisal of application to practice. J. Athl. Enhanc. 2015, 19, 2. [Google Scholar] [CrossRef]
- Park, K.-N.; Jung, D.-Y.; Kim, S.-H. Trapezius and serratus anterior muscle strength in violinists with unilateral neck pain. J. Back. Musculoskelet. Rehabil. 2020, 33, 631–636. [Google Scholar] [CrossRef] [PubMed]
- Kahlaee, A.H.; Ghamkhar, L.; Nourbakhsh, M.R.; Arab, A.M. Strength and Range of Motion in the Contralateral Side to Pain and Pain-Free Regions in Unilateral Chronic Nonspecific Neck Pain Patients. Am. J. Phys. Med. Rehabil. 2020, 99, 133–141. [Google Scholar] [CrossRef]
- Jull, G.A.; O’leary, S.P.; Falla, D.L. Clinical assessment of the deep cervical flexor muscles: The craniocervical flexion test. J. Manip. Physiol. Ther. 2008, 31, 525–533. [Google Scholar] [CrossRef] [PubMed]
- Ylinen, J.; Takala, E.-P.; Kautiainen, H.; Nykänen, M.; Häkkinen, A.; Pohjolainen, T.; Karppi, S.-L.; Airaksinen, O. Association of neck pain, disability and neck pain during maximal effort with neck muscle strength and range of movement in women with chronic non-specific neck pain. Eur. J. Pain. 2004, 8, 473–478. [Google Scholar] [CrossRef]
- Wang, D.M.; Li, C.; Hatchard, N.; Chang Chien, G.C.; Alm, J. Lower trapezius muscle function in people with and without shoulder and neck pain: A systematic review. J. Osteopath. Med. 2023, 123, 73–89. [Google Scholar] [CrossRef] [PubMed]
- Falla, D.; Jull, G.; Hodges, P. Training the cervical muscles with prescribed motor tasks does not change muscle activation during a functional activity. Man. Ther. 2008, 13, 507–512. [Google Scholar] [CrossRef]
- Tsang, S.M.; Szeto, G.P.; Lee, R.Y. Altered spinal kinematics and muscle recruitment pattern of the cervical and thoracic spine in people with chronic neck pain during functional task. J. Electromyogr. Kinesiol. 2014, 24, 104–113. [Google Scholar] [CrossRef]
- Almeida, M.B.d.; Moreira, M.; Miranda-Oliveira, P.; Moreira, J.; Família, C.; Vaz, J.R.; Moleirinho-Alves, P.; Oliveira, R. Evolving Dynamics of Neck Muscle Activation Patterns in Dental Students: A Longitudinal Study. Sensors 2024, 24, 5689. [Google Scholar] [CrossRef]
- Tudini, F.; Myers, B.; Bohannon, R. Reliability and validity of measurements of cervical retraction strength obtained with a hand-held dynamometer. J. Man. Manip. Ther. 2019, 27, 222–228. [Google Scholar] [CrossRef]
- Mousavi, S.J.; Olyaei, G.R.; Talebian, S.; Sanjari, M.A.; Parnianpour, M. The effect of angle and level of exertion on trunk neuromuscular performance during multidirectional isometric activities. Spine 2009, 34, E170–E177. [Google Scholar] [CrossRef] [PubMed]
- Strimpakos, N. The assessment of the cervical spine. Part 2: Strength and endurance/fatigue. J. Bodyw. Mov. Ther. 2011, 15, 417–430. [Google Scholar] [CrossRef]
- Stark, T.; Walker, B.; Phillips, J.K.; Fejer, R.; Beck, R. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: A systematic review. PM&R 2011, 3, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Mentiplay, B.F.; Perraton, L.G.; Bower, K.J.; Adair, B.; Pua, Y.-H.; Williams, G.P.; McGaw, R.; Clark, R.A. Assessment of lower limb muscle strength and power using hand-held and fixed dynamometry: A reliability and validity study. PLoS ONE 2015, 10, e0140822. [Google Scholar] [CrossRef]
- Almeida, M.B.; Oliveira, C.; Ornelas, G.; Soares, T.; Souto, J.; Póvoa, R.; Ferreira, L.M.A.; Ricci-Vitor, A.L. Intra-Rater and Inter-Rater Reliability of the Kinvent Hand-Held Dynamometer in Young Adults. Med. Sci. Forum 2023, 22, 2012. [Google Scholar] [CrossRef]
- Vannebo, K.T.; Iversen, V.M.; Fimland, M.S.; Mork, P.J. Test-retest reliability of a handheld dynamometer for measurement of isometric cervical muscle strength. J. Back Musculoskelet. Rehabil. 2018, 31, 557–565. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Tudini, F. Magnitude, validity and responsiveness of dynamometer measured neck retraction strength in patients referred with neck pain to out-patient physical therapy. J. Phys. Ther. Sci. 2022, 34, 694–696. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Karaağaç, A.; Arslan, S.A.; Keskin, E.D. Assessment of pain, scapulothoracic muscle strength, endurance and scapular dyskinesis in individuals with and without nonspecific chronic neck pain: A cross-sectional study. J. Bodyw. Mov. Ther. 2023, 35, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Mesquita, C.C.; Ribeiro, J.C.; Moreira, P. Portuguese version of the standardized Nordic musculoskeletal questionnaire: Cross cultural and reliability. J. Public Health 2010, 18, 461–466. [Google Scholar] [CrossRef]
- Peek, K. The measurement of neck strength: A guide for sports medicine clinicians. Phys. Ther. Sport. 2022, 55, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Jaric, S. Muscle strength testing: Use of normalisation for body size. Sports Med. 2002, 32, 615–631. [Google Scholar] [CrossRef]
- Love, J.; Dropmann, D.; Selker, R. Jamovi, 2.4.8. 2023. Available online: https://www.jamovi.org (accessed on 13 January 2024).
- R Core Team. R: A Language and Environment for Statistical Computing, Version 4.1; R Foundation for Statistical Computing: Vienna, Austria, 2022. [Google Scholar]
- Fox, J.; Weisberg, S. CAR: Companion to Applied Regression. [R Package]. 2020. Available online: https://cran.r-project.org/package=car (accessed on 13 January 2024).
- Lenth, R. EMMEANS: Estimated Marginal Means, aka Least-Squares Means. [R Package]. 2023. Available online: https://cran.r-project.org/web/packages/emmeans/emmeans.pdf (accessed on 10 September 2024).
- Catenaccio, E.; Mu, W.; Kaplan, A.; Fleysher, R.; Kim, N.; Bachrach, T.; Zughaft Sears, M.; Jaspan, O.; Caccese, J.; Kim, M. Characterization of neck strength in healthy young adults. PM&R 2017, 9, 884–891. [Google Scholar] [CrossRef]
- Koni, A.; Kufersin, M.; Ronchese, F.; Travan, M.; Cadenaro, M.; Filon, F.L. Approach to prevention of musculoskeletal symptoms in dental students: An interventional study. Med. Lav. 2018, 109, 276. [Google Scholar] [CrossRef] [PubMed]
- Faust, A.M.; Ahmed, S.N.; Johnston, L.B.; Harmon, J.B. Teaching methodologies for improving dental students’ implementation of ergonomic operator and patient positioning. J. Dent. Educ. 2021, 85, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Hanvold, T.N.; Wærsted, M.; Mengshoel, A.M.; Bjertness, E.; Stigum, H.; Twisk, J.; Veiersted, K.B. The effect of work-related sustained trapezius muscle activity on the development of neck and shoulder pain among young adults. Scand. J. Work. Environ. Health 2013, 39, 390–400. [Google Scholar] [CrossRef]
- Lee, K.-C.; Chiu, T.T.; Lam, T.-H. The role of fear-avoidance beliefs in patients with neck pain: Relationships with current and future disability and work capacity. Clin. Rehabil. 2007, 21, 812–821. [Google Scholar] [CrossRef]
- Folland, J.P.; Williams, A.G. The adaptations to strength training: Morphological and neurological contributions to increased strength. Sports Med. 2007, 37, 145–168. [Google Scholar] [CrossRef]
- Vila-Chã, C.; Falla, D. Strength training, but not endurance training, reduces motor unit discharge rate variability. J. Electromyogr. Kinesiol. 2016, 26, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Morton, R.W.; Colenso-Semple, L.; Phillips, S.M. Training for strength and hypertrophy: An evidence-based approach. Curr. Opin. Physiol. 2019, 11, 149–150. [Google Scholar] [CrossRef]
- Counts, B.R.; Buckner, S.L.; Dankel, S.J.; Jessee, M.B.; Mattocks, K.T.; Mouser, J.G.; Laurentino, G.C.; Loenneke, J.P. The acute and chronic effects of “NO LOAD” resistance training. Physiol. Behav. 2016, 164, 345–352. [Google Scholar] [CrossRef]
- Schoenfeld, B.J.; Grgic, J.; Ogborn, D.; Krieger, J.W. Strength and hypertrophy adaptations between low- vs. High-load resistance training: A systematic review and meta-analysis. J. Strength Cond. Res. 2017, 31, 3508–3523. [Google Scholar] [CrossRef]
- Hägg, G.M.; Ericson, M.; Odenrick, P. Physical load. In Work and Technology on Human Terms; 2009; pp. 129–189. Available online: https://portal.research.lu.se/en/publications/work-and-technology-on-human-terms (accessed on 10 September 2024).
- Bonilla-Barba, L.; Florencio, L.L.; Rodríguez-Jiménez, J.; Falla, D.; Fernández-de-Las-Peñas, C.; Ortega-Santiago, R. Women with mechanical neck pain exhibit increased activation of their superficial neck extensors when performing the cranio-cervical flexion test. Musculoskelet. Sci. Pract. 2020, 49, 102222. [Google Scholar] [CrossRef] [PubMed]
- Yajima, H.; Nobe, R.; Takayama, M.; Takakura, N. The mode of activity of cervical extensors and flexors in healthy adults: A cross-sectional study. Medicina 2022, 58, 728. [Google Scholar] [CrossRef]
- Benatto, M.T.; Florencio, L.L.; Bragatto, M.M.; Lodovichi, S.S.; Dach, F.; Bevilaqua-Grossi, D. Extensor/flexor ratio of neck muscle strength and electromyographic activity of individuals with migraine: A cross-sectional study. Eur. Spine J. 2019, 28, 2311–2318. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).