Reliability and Validity of the Orthotic Deformation Test
Abstract
1. Introduction
2. Materials and Methods
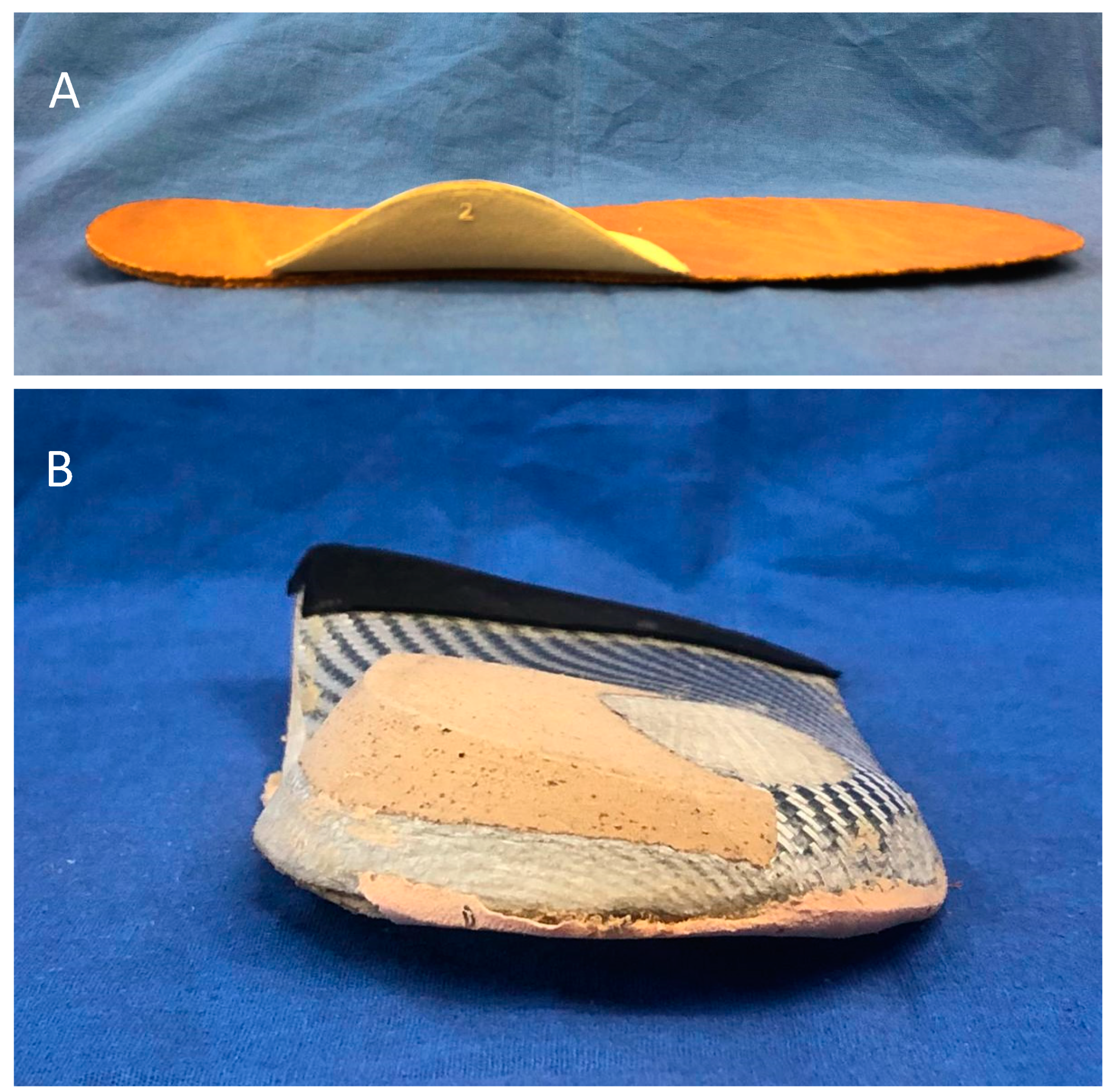
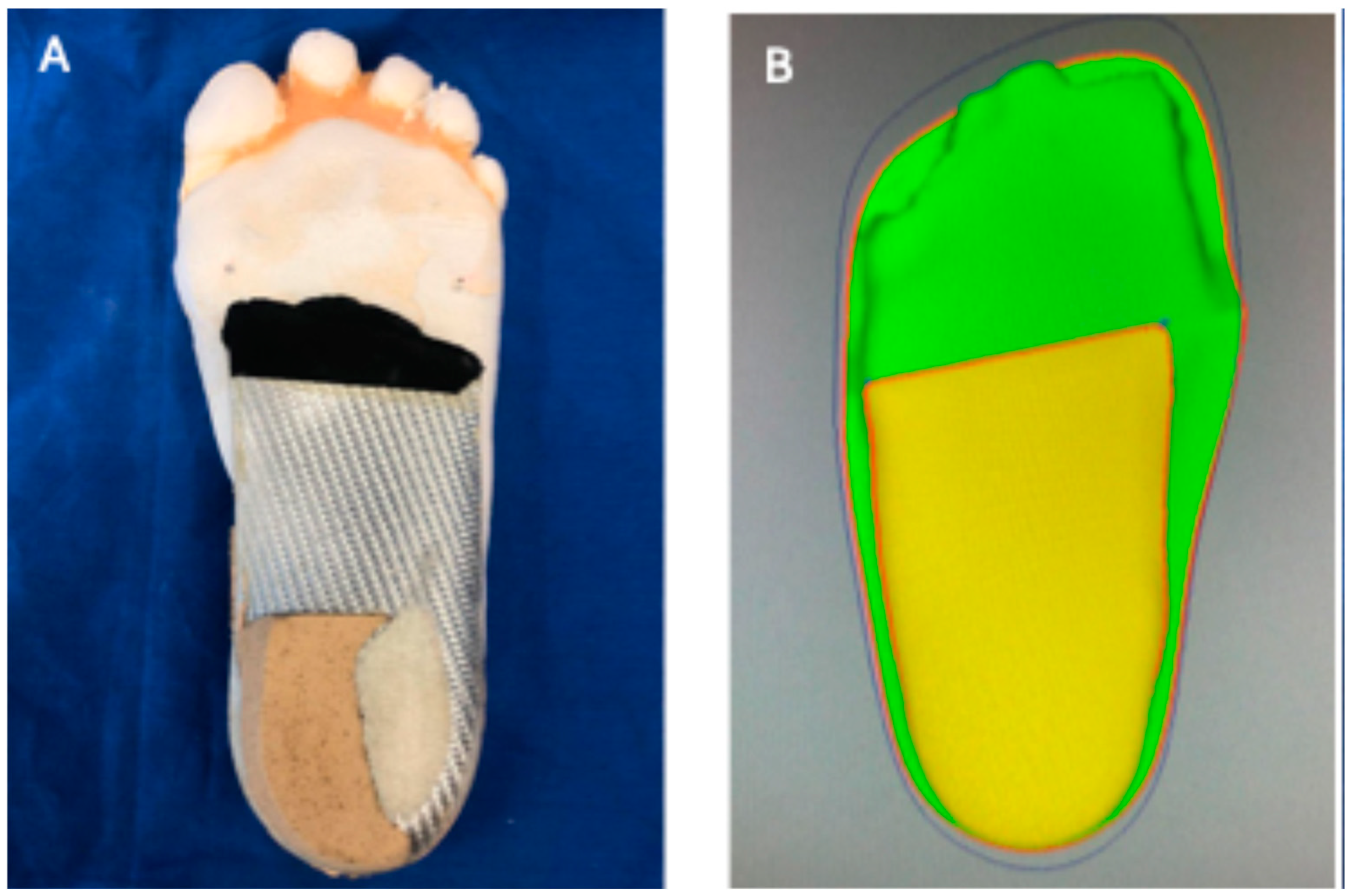
2.1. Custom Foot Orthoses
2.2. Manual Orthotic Deformation Test
2.3. Device Compression Test
2.4. Data Analysis
3. Results
3.1. Custom Foot Orthoses
3.2. Interobserver Reliability (Manual Test)
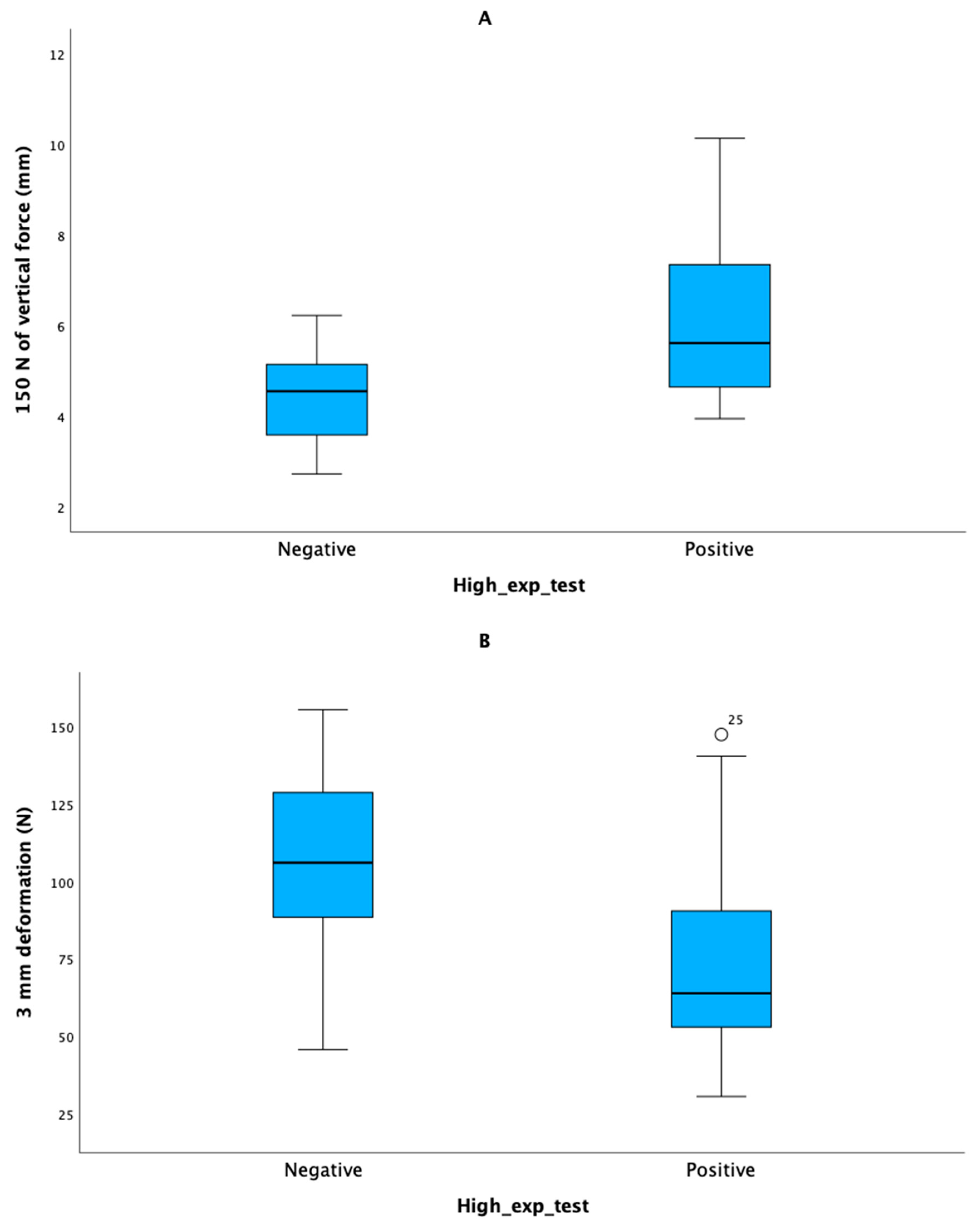
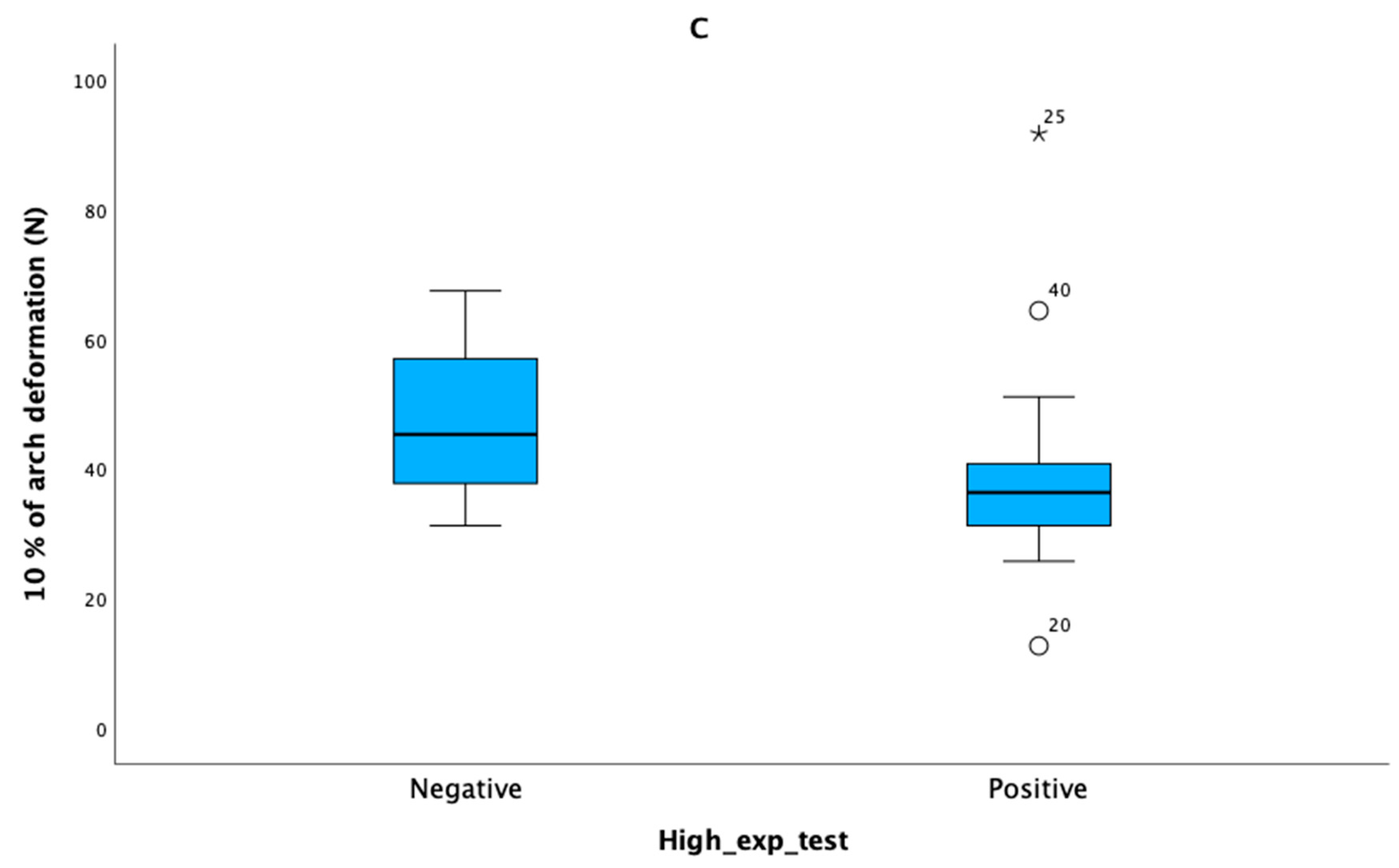
3.3. Compression Test
3.4. Validity
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Manfredi-Márquez, M.J.; Tavara-Vidalón, S.P.; Tavaruela-Carrión, N.; Gómez Benítez, M.A.; Fernandez-Seguín, L.M.; Ramos-Ortega, J. Study of Windlass Mechanism in the Lower Limb Using Inertial Sensors. Int. J. Environ. Res. Public Health 2023, 20, 3220. [Google Scholar] [CrossRef] [PubMed]
- Aquino, A.; Payne, C. Function of the plantar fascia. Foot 1999, 9, 72–78. [Google Scholar] [CrossRef]
- Stearne, S.M.; McDonald, K.A.; Alderson, J.A.; North, I.; Oxnard, C.E.; Rubenson, J. The Foot’s Arch and the Energetics of Human Locomotion. Sci. Rep. 2016, 6, 19403. [Google Scholar] [CrossRef] [PubMed]
- Orejana-Garcia, A.; Pérez-Monzó, F. Tissue stress model. Clinical applications in foot pathology. Rev. Esp. Pod. 2018, 29, 101–112. [Google Scholar] [CrossRef]
- Hawke, F.; Burns, J.; Radford, J.A.; du Toit, V. Custom-made foot orthoses for the treatment of foot pain. Cochrane Database Syst. Rev. 2008, 3, CD006801. [Google Scholar] [CrossRef]
- Razeghi, M.; Batt, M.E. Biomechanical analysis of the effect of orthotic shoe inserts: A review of the literature. Sports Med. 2000, 29, 425–438. [Google Scholar] [CrossRef]
- Cheung, R.T.H.; Chung, R.C.K.; Ng, G.Y.F. Efficacies of different external controls for excessive foot pronation: A meta-analysis. Br. J. Sports Med. 2011, 45, 743–751. [Google Scholar] [CrossRef]
- Healy, A.; Farmer, S.; Pandyan, A.; Chockalingam, N. A systematic review of randomised controlled trials assessing effectiveness of prosthetic and orthotic interventions. PLoS ONE 2018, 13, e0192094. [Google Scholar] [CrossRef]
- Burns, J.; Wegener, C.; Begg, L.; Vicaretti, M.; Fletcher, J. Randomized trial of custom orthoses and footwear on foot pain and plantar pressure in diabetic peripheral arterial disease. Diabet. Med. 2009, 26, 893–899. [Google Scholar] [CrossRef]
- Paton, J.S.; Stenhouse, E.A.; Bruce, G.; Zahra, D.; Jones, R.B. A comparison of customised and prefabricated insoles to reduce risk factors for neuropathic diabetic foot ulceration: A participant-blinded randomised controlled trial. J. Foot Ankle Res. 2012, 5, 31. [Google Scholar] [CrossRef]
- Ruiz-Ramos, M.; Orejana-García, A.M.; Vives-Merino, I.; Bravo-Llatas, C.; Lázaro-Martínez, J.L.; Molines-Barroso, R.J. Effectiveness of the Fixtoe Device(R) in plantar pressure reduction: A preliminary study. BMC Musculoskelet. Disord. 2022, 23, 475. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.Y.; Liu, Q.L.; Yick, K.L.; Yip, J.; Ng, S.P. Analysis of Diabetic Foot Deformation and Plantar Pressure Distribution of Women at Different Walking Speeds. Int. J. Environ. Res. Public Health 2023, 20, 3688. [Google Scholar] [CrossRef] [PubMed]
- Deepashini, H.; Omar, B.; Paungmali, A.; Amaramalar, N.; Ohnmar, H.; Leonard, J. An insight into the plantar pressure distribution of the foot in clinical practice: Narrative review. Pol. Ann. Med. 2014, 21, 51–56. [Google Scholar] [CrossRef]
- Haris, F.L.; Liau, B.-Y.; Jan, Y.-K.; Akbari, V.B.H.; Primanda, Y.; Lin, K.-H.; Lung, C.-W. A Review of the Plantar Pressure Distribution Effects from Insole Materials and at Different Walking Speeds. Appl. Sci. 2021, 11, 11851. [Google Scholar] [CrossRef]
- Mientjes, M.I.V.; Shorten, M. Contoured cushioning: Effects of surface compressibility and curvature on heel pressure distribution. Footwear Sci. 2011, 3, 23–32. [Google Scholar] [CrossRef]
- Whittaker, G.A.; Munteanu, S.E.; Menz, H.B.; Tan, J.M.; Rabusin, C.L.; Landorf, K.B. Foot orthoses for plantar heel pain: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 322–328. [Google Scholar] [CrossRef]
- Hajizadeh, M.; Desmyttere, G.; Carmona, J.-P.; Bleau, J.; Begon, M. Can foot orthoses impose different gait features based on geometrical design in healthy subjects? A systematic review and meta-analysis. Foot 2020, 42, 101646. [Google Scholar] [CrossRef]
- Kirby, K.A.; Spooner, S.K.; Scherer, P.R.; Schuberth, J.M. Foot orthoses. Foot Ankle Spec. 2012, 5, 334–343. [Google Scholar] [CrossRef]
- Naderi, A.; Degens, H.; Sakinepoor, A. Arch-support foot-orthoses normalize dynamic in-shoe foot pressure distribution in medial tibial stress syndrome. Eur. J. Sport. Sci. 2019, 19, 247–257. [Google Scholar] [CrossRef]
- Hornestam, J.F.; Souza, T.R.; Arantes, P.; Ocarino, J.; Silva, P.L. The Effect of Walking Speed on Foot Kinematics is Modified When Increased Pronation is Induced. J. Am. Podiatr. Med. Assoc. 2016, 106, 419–426. [Google Scholar] [CrossRef]
- Redmond, A.C.; Landorf, K.B.; Keenan, A.M. Contoured, prefabricated foot orthoses demonstrate comparable mechanical properties to contoured, customised foot orthoses: A plantar pressure study. J. Foot Ankle Res. 2009, 2, 20. [Google Scholar] [CrossRef] [PubMed]
- Pelaez, A.S.T.; Farahpour, N.; Griffiths, I.B.; Moisan, G. Thick shells and medially wedged posts increase foot orthoses medial longitudinal arch stiffness: An experimental study. J. Foot Ankle Res. 2023, 16, 11. [Google Scholar] [CrossRef] [PubMed]
- Shahar, F.S.; Hamed-Sultan, M.T.; Lee, S.H.; Jawaid, M.; Md Shah, A.U.; Safri, S.N.A.; Sivasankaran, P.N. A review on the orthotics and prosthetics and the potential of kenaf composites as alternative materials for ankle-foot orthosis. J. Mech. Behav. Biomed. Mater. 2019, 99, 169–185. [Google Scholar] [CrossRef] [PubMed]
- Alfaro-Santafé, J.; Gómez-Bernal, A.; Lanuza-Cerzócimo, C.; Alfaro-Santafé, J.V.; Pérez-Morcillo, A.; Almenar-Arasanz, A.J. Effectiveness of Custom-Made Foot Orthoses vs. Heel-Lifts in Children with Calcaneal Apophysitis (Sever’s Disease): A CONSORT-Compliant Randomized Trial. Children 2021, 8, 963. [Google Scholar] [CrossRef]
- Jena, S.; Arunachalam, T.; Panda, S.K. Experimental and numerical investigation of a polypropylene orthotic device for assistance in level ground walking. Proc. Inst. Mech. Eng. H 2020, 234, 356–369. [Google Scholar] [CrossRef]
- Rogati, G.; Caravaggi, P.; Leardini, A.; Erani, P.; Fognani, R.; Saccon, G.; Boriani, L.; Baleani, M. A novel apparatus to assess the mechanical properties of Ankle-Foot Orthoses: Stiffness analysis of the Codivilla spring. J. Biomech. 2022, 142, 111239. [Google Scholar] [CrossRef]
- Fatone, S.; Owen, E.; Gao, F.; Shippen, G.; Orendurff, M.S.; Bjornson, K. Comparison of Sagittal Plane Stiffness of Nonarticulated Pediatric Ankle-Foot Orthoses Designed to be Rigid. J. Prosthet. Orthot. 2022, 34, e44–e49. [Google Scholar] [CrossRef]
- Choo, Y.J.; Chang, M.C. Commonly Used Types and Recent Development of Ankle-Foot Orthosis: A Narrative Review. Healthcare 2021, 9, 1046. [Google Scholar] [CrossRef]
- Kirby, K.A. Foot and Lower Extremity Biomechanics II: Precision Intricast Newsletters, 1997–2002; Precision Intricast Inc.: Payson, AZ, USA, 2002; Volume 2. [Google Scholar]
- Silva, R.; Veloso, A.; Alves, N.; Fernandes, C.; Morouço, P. A Review of Additive Manufacturing Studies for Producing Customized Ankle-Foot Orthoses. Bioengineering 2022, 9, 249. [Google Scholar] [CrossRef]
- Salles, A.S.; Gyi, D.E. An evaluation of personalised insoles developed using additive manufacturing. J. Sports Sci. 2013, 31, 442–450. [Google Scholar] [CrossRef]
- Nussbaum, M.A.; Johnson, H. Determination and evaluation of acceptable force limits in single-digit tasks. Hum. Factors 2002, 44, 545–556. [Google Scholar] [CrossRef] [PubMed]
- Barkoula, N.M.; Alcock, B.; Cabrera, N.O.; Peijs, T. Fatigue Properties of Highly Oriented Polypropylene Tapes and All-Polypropylene Composites. Polym. Polym. Compos. 2008, 16, 101–113. [Google Scholar] [CrossRef]
- Hallgren, K.A. Computing inter-rater reliability for observational data: An overview and tutorial. Tutor. Quant. Methods Psychol. 2012, 8, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Pearce, C.J.; Calder, J.D. Surgical anatomy of the midfoot. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Kirby, K.A. Longitudinal arch load-sharing system of the foot. Rev. Esp. Pod 2017, 28, 37–45. [Google Scholar] [CrossRef]
- Sichting, F.; Ebrecht, F. The rise of the longitudinal arch when sitting, standing, and walking: Contributions of the windlass mechanism. PLoS ONE 2021, 16, e0249965. [Google Scholar] [CrossRef]
- Aquino, A.; Payne, C. Function of the windlass mechanism in excessively pronated feet. J. Am. Podiatr. Med. Assoc. 2001, 91, 245–250. [Google Scholar] [CrossRef]
- Paton, J.S. The relationship between navicular drop and first metatarsophalangeal joint motion. J. Am. Podiatr. Med. Assoc. 2006, 96, 313–317. [Google Scholar] [CrossRef]
- Fuller, E.A. The windlass mechanism of the foot. A mechanical model to explain pathology. J. Am. Podiatr. Med. Assoc. 2000, 90, 35–46. [Google Scholar] [CrossRef]
- Bolgla, L.A.; Malone, T.R. Plantar Fasciitis and the Windlass Mechanism: A Biomechanical Link to Clinical Practice. J. Athl. Train. 2004, 39, 77–82. [Google Scholar]
- Abdalbary, S.A.; Alhaskawi, A.; Zhou, H.; Dong, Y.; Tu, T.; Li, P.; Lu, H. Predictive Measurement for Windlass Change in Length and Selected Treatment Outcomes in Chronic Plantar Fasciitis. J. Vis. Exp. 2024, 205, e65368. [Google Scholar] [CrossRef] [PubMed]
- Aminian, G.; Safaeepour, Z.; Farhoodi, M.; Pezeshk, A.F.; Saeedi, H.; Majddoleslam, B. The effect of prefabricated and proprioceptive foot orthoses on plantar pressure distribution in patients with flexible flatfoot during walking. Prosthet. Orthot. Int. 2013, 37, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.N.; Miller, J.C. Statistics and Chemometrics for Analytical Chemistry, 6th ed.; Pearson Education Limited: Essex, UK, 2010; pp. 74–106. [Google Scholar]



| N = 48 | Positive Values n (%) | Weighted Kappa | p-Value [CI95%] | Landis and Koch Scale |
|---|---|---|---|---|
| Low–moderate experience | 20(42)–22(46) | −0.99 | 0.493 [−0.378–0.181] | No agreement |
| Low–high experience | 20(42)–34(71) | −0.91 | 0.452 [−0.332–0.150] | No agreement |
| Moderate–high experience | 22(46)–34(71) | 0.517 | <0.001 [0.309–0.724] | Moderate agreement |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sierra-Rodríguez, A.; Molines-Barroso, R.J.; Martínez, M.A.; Abenojar-Buendía, J.; Lázaro-Martínez, J.L.; Orejana-García, A.M. Reliability and Validity of the Orthotic Deformation Test. Appl. Sci. 2024, 14, 8378. https://doi.org/10.3390/app14188378
Sierra-Rodríguez A, Molines-Barroso RJ, Martínez MA, Abenojar-Buendía J, Lázaro-Martínez JL, Orejana-García AM. Reliability and Validity of the Orthotic Deformation Test. Applied Sciences. 2024; 14(18):8378. https://doi.org/10.3390/app14188378
Chicago/Turabian StyleSierra-Rodríguez, Alejandra, Raúl J. Molines-Barroso, M. A. Martínez, Juana Abenojar-Buendía, José Luis Lázaro-Martínez, and Angel M. Orejana-García. 2024. "Reliability and Validity of the Orthotic Deformation Test" Applied Sciences 14, no. 18: 8378. https://doi.org/10.3390/app14188378
APA StyleSierra-Rodríguez, A., Molines-Barroso, R. J., Martínez, M. A., Abenojar-Buendía, J., Lázaro-Martínez, J. L., & Orejana-García, A. M. (2024). Reliability and Validity of the Orthotic Deformation Test. Applied Sciences, 14(18), 8378. https://doi.org/10.3390/app14188378









