Changes in Articulatory Contact Pressure as a Function of Vocal Loudness
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Speech Stimuli
2.3. Instrumentation
2.4. Procedures
2.5. Analysis
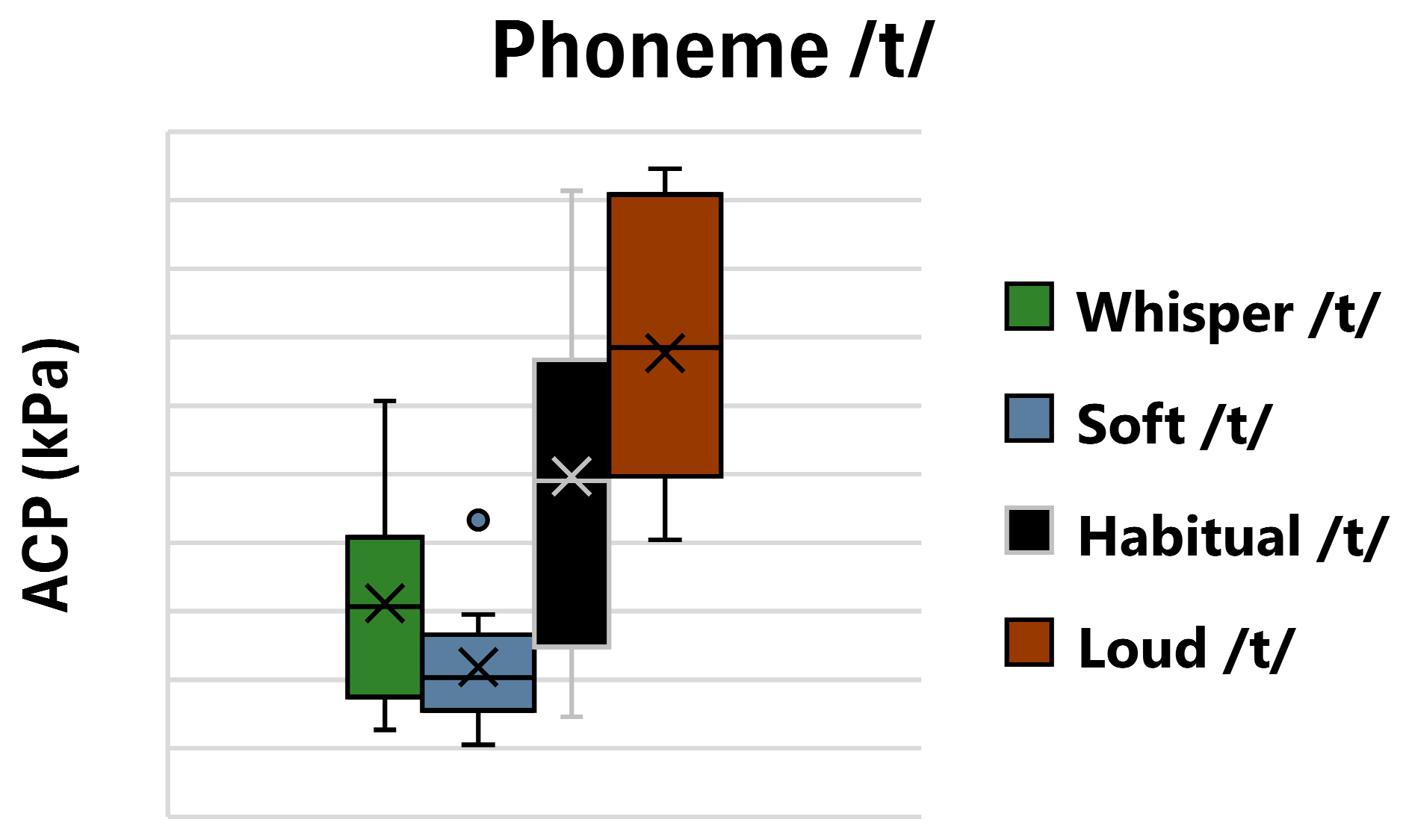
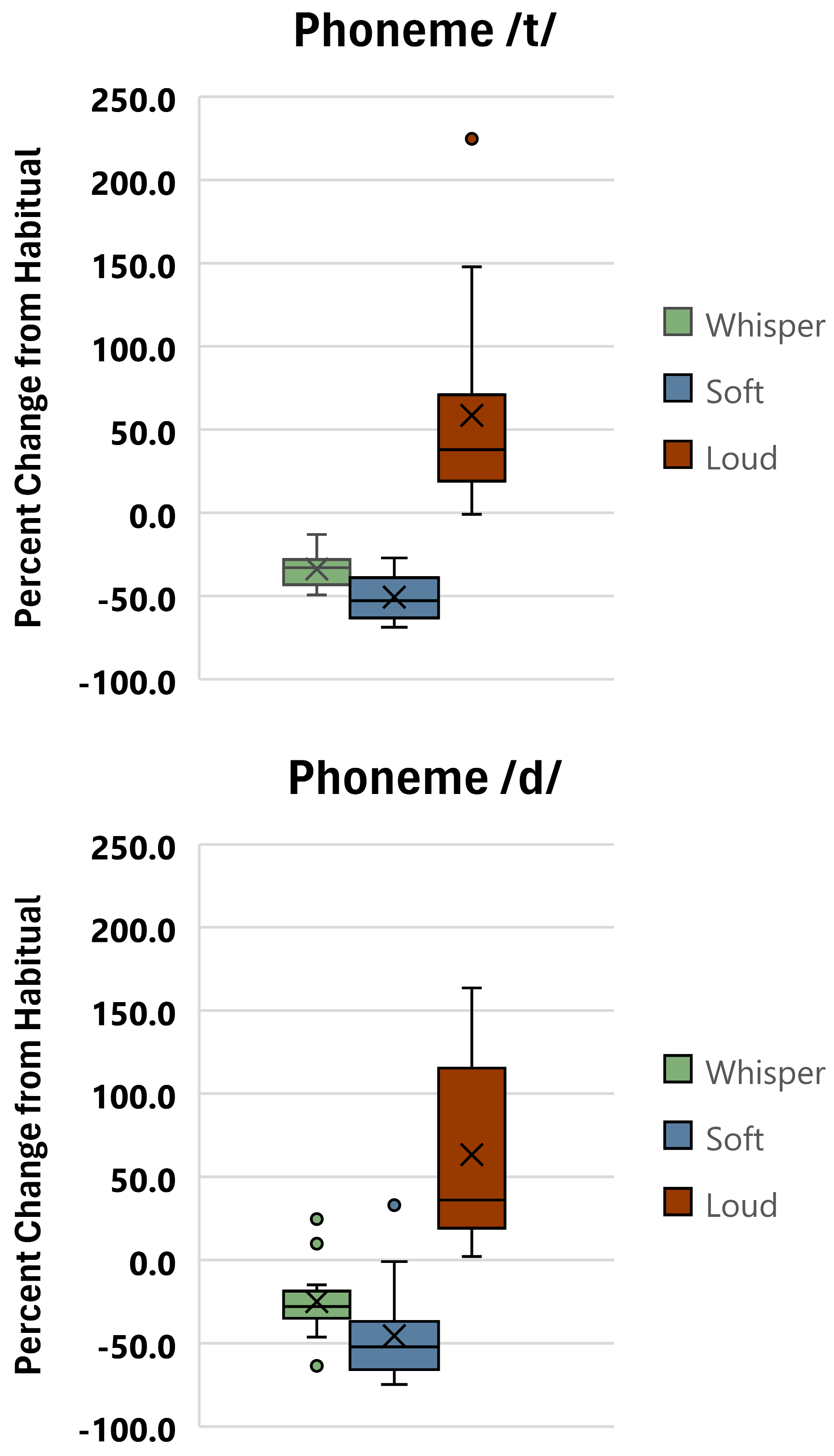
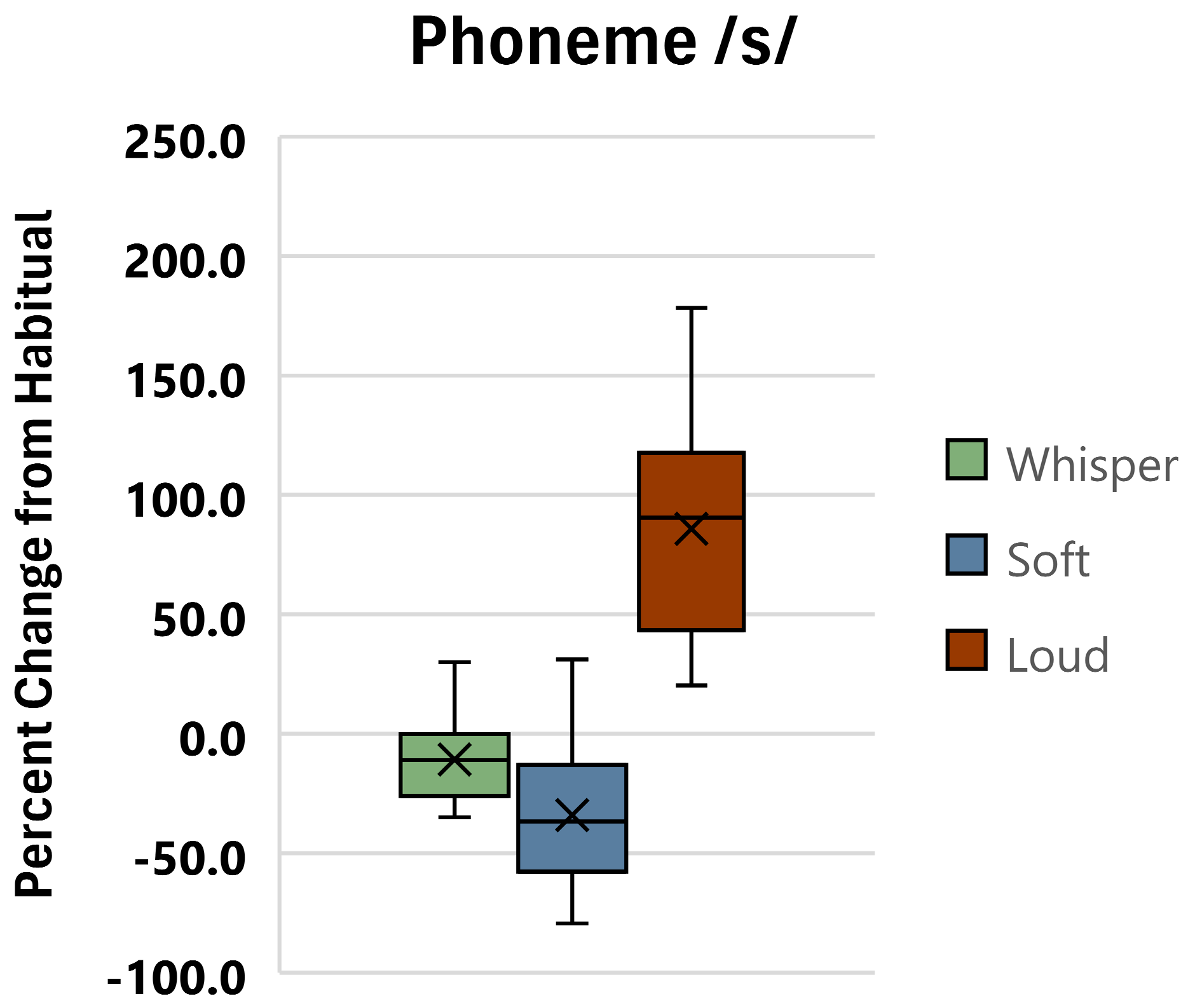
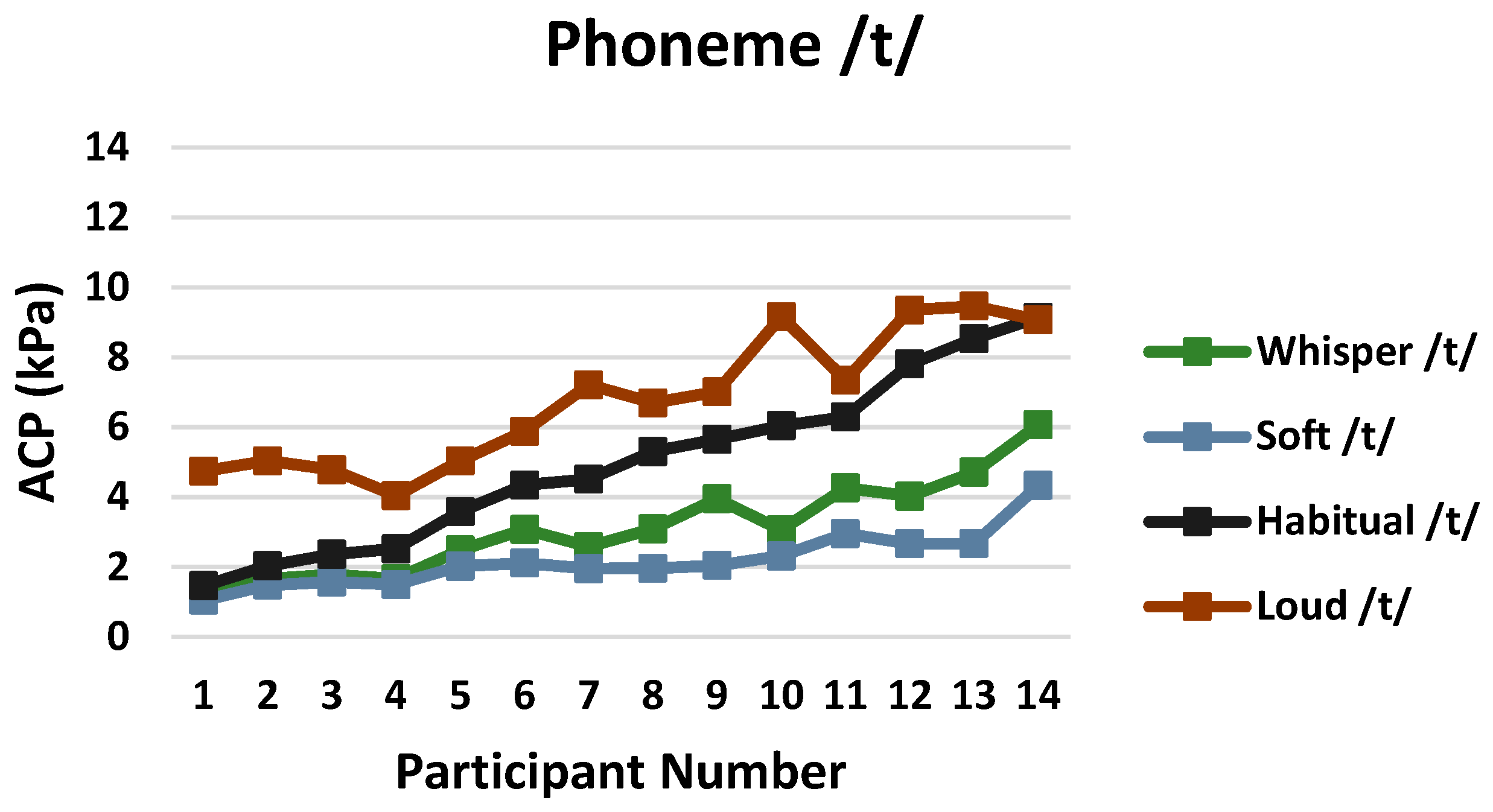
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kent, R.D.; Read, C. The Acoustic Analysis of Speech; Singular Publishing Group, Inc.: New York, NY, USA, 1992. [Google Scholar]
- Müller, E.M.; Milenkovic, P.H.; MacLeod, G.E. Perioral tissue mechanics during speech production International Association for Mathematics and Computers in Simulation. In Second IMACS International Symposium on Biomedical Systems Modeling; DeLisi, C., Eisenfeld, J., Eds.; Elsevier Science Publishers B.V.: Amsterdam, The Netherlands, 1985; pp. 363–371. [Google Scholar]
- Yoshioko, F.; Ozawa, S.; Sumita, Y.I.; Mukohyama, H.; Taniguchi, H. The pattern of tongue pressure against the palate during articulating glossal sounds in normal subjects and glossectomy patients. J. Med. Dent. Sci. 2004, 51, 19–25. [Google Scholar]
- Yano, J.; Kumakura, I.; Hori, K.; Tamine, K.I.; Ono, T. Differences in biomechanical features of tongue pressure production between articulation and swallow. J. Oral Rehabil. 2012, 39, 118–125. [Google Scholar] [CrossRef]
- Evitts, P.M.; Nichols, D.; Asbury, K.; Westhoff, T.; Dobrosielski, D.A. Relationship between fat distribution and tongue strength in persons with and without obstructive sleep apnea. Sleep Med. Disord. Int. J. 2018, 2, 109–113. [Google Scholar] [CrossRef]
- Searl, J.; Evitts, P.M.; Davis, W.J. Articulatory contact pressure between the tongue and palate during normal speech production. J. Med. Speech-Lang. Pathol. 2007, 15, 279–293. [Google Scholar]
- McGlone, R.; Proffit, W. Lingual Pressures Associated with Speaker Consistency and Syllable Variations. Phonetica 1967, 10, 606–615. [Google Scholar] [CrossRef]
- Searl, J.; Knollhoff, S. Articulation contact pressures scaled to the physiologic range of the tongue in amyotrophic lateral sclerosis: A pilot study. J. Commun. Disord. 2019, 82, 105937. [Google Scholar] [CrossRef]
- Searl, J. Sense of Effort and Articulatory Contact Pressure Associated with Talking by Individuals Using Tracheoesophageal Speech. Folia Phoniatr. Logop. 2020, 72, 218–227. [Google Scholar] [CrossRef]
- Ng, M.L.; Tong ET, S.; Yu, K.M. Articulatory Contact Pressure during Bilabial Plosive Production in Esophageal and Tracheoesophageal Speech. Folia Phoniatr. Logop. 2019, 71, 1–6. [Google Scholar] [CrossRef] [PubMed]
- You, E.M.L.; Yip, P.P.S. Effect of Noise on Vocal Loudness and Pitch in Natural Environments: An Accelerometer (Ambulatory Phonation Monitor) Study. J. Voice 2016, 30, 389–393. [Google Scholar] [CrossRef]
- Hazan, V.; Tuomainen, O.; Kim, J.; Davis, C.; Sheffield, B.; Brungart, D. Clear speech adaptations in spontaneous speech produced by young and older adults. J. Acoust. Soc. Am. 2018, 144, 1331–1346. [Google Scholar] [CrossRef]
- Zahorik, P.; Kelly, J.W. Accurate vocal compensation for sound intensity loss with increasing distance in natural environments. J. Acoust. Soc. Am. 2007, 122, EL143–EL150. [Google Scholar] [CrossRef] [PubMed]
- Ryabov, R.; Malakh, M.; Trachtenberg, M.; Wohl, S.; Oliveira, G. Self-perceived and Acoustic Voice Characteristics of Russian-English Bilinguals. J. Voice 2016, 30, 772.e1–772.e8. [Google Scholar] [CrossRef] [PubMed]
- Nevo, L.; Nevo, C.; Oliveira, G. A comparison of vocal parameters in adult bilingual Hebrew-English speakers. CoDAS 2015, 27, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Lewandowski, E.M.; Nygaard, L.C. Vocal alignment to native and non-native speakers of English. J. Acoust. Soc. Am. 2018, 144, 620–633. [Google Scholar] [CrossRef]
- Van Nuffelen, G.; de Bodt, M.; Vanderwegen, J.; van de Heyning, P.; Wuyts, F. Effect of Rate Control on Speech Production and Intelligibility in Dysarthria. Folia Phoniatr. Logop. 2010, 62, 110–119. [Google Scholar] [CrossRef]
- Yorkston, K.M.; Hammen, V.L.; Beukelman, D.R.; Traynor, C.D. The Effect of Rate Control on the Intelligibility and Naturalness of Dysarthric Speech. J. Speech Hear. Disord. 1990, 55, 550–560. [Google Scholar] [CrossRef]
- Behrman, A.; Cody, J.; Elandary, S.; Flom, P.; Chitnis, S. The Effect of SPEAK OUT! and The LOUD Crowd on Dysarthria Due to Parkinson’s Disease. Am. J. Speech-Lang. Pathol. 2020, 29, 1448–1465. [Google Scholar] [CrossRef]
- Ramig Halpern, A.; Spielman, J.; Fox, C.; Freeman, K. Speech treatment in Parkinson’s disease: Randomized controlled trial (RCT). Mov. Disord. 2018, 33, 1777–1791. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Theodoros, D.; Finch, E.; Cardell, E. Be clear: A new intensive speech treatment for adults with nonprogressive dysarthria. Am. J. Speech-Lang. Pathol. 2016, 25, 97–110. [Google Scholar] [CrossRef]
- Whitfield, J.A.; Goberman, A.M. Articulatory-acoustic vowel space: Application to clear speech in individuals with Parkinson’s disease. J. Commun. Disord. 2014, 51, 19–28. [Google Scholar] [CrossRef]
- Searl, J.; Evitts, P.M. Tongue–Palate Contact Pressure, Oral Air Pressure, and Acoustics of Clear Speech. J. Speech Lang. Hear. Res. 2013, 56, 826. [Google Scholar] [CrossRef] [PubMed]
- Casper, J.; Leonard, R. Understanding Voice Problems: A Physiological Perspective for Diagnosis and Treatment, 3rd ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2006. [Google Scholar]
- Fox, C.M.; Raming, L.O.; Ciucci, M.R.; Sapir, S.; McFarland, D.H.; Farley, B.G. The science and practice of LSVT/LOUD: Neural plasticity—Principled approach to treating individuals with parkinson disease and other nuerological disorders. Semin. Speech Lang. 2006, 27, 283–299. [Google Scholar] [CrossRef] [PubMed]
- Behrman, A.; Cody, J.; Chitnis, S.; Elandary, S. Dysarthria treatment for Parkinson’s disease: One-year follow-up of SPEAK OUT!® with the LOUD Crowd®. Logop. Phoniatr. Vocol. 2022, 47, 271–278. [Google Scholar] [CrossRef]
- Pu, T.; Huang, M.; Kong, X.; Wang, M.; Chen, X.; Feng, X.; Wei, C.; Weng, X.; Xu, F. Lee Silverman Voice Treatment to Improve Speech in Parkinson’s Disease: A Systemic Review and Meta-Analysis. In Parkinson’s Disease; Hindawi Limited: New York, NY, USA, 2021; Volume 2021. [Google Scholar] [CrossRef]
- Martel Sauvageau, V.; Roy, J.P.; Langlois, M.; Macoir, J. Impact of the LSVT on vowel articulation and coarticulation in Parkinson’s disease. Clin. Linguist. Phon. 2015, 29, 424–440. [Google Scholar] [CrossRef] [PubMed]
- Neel, A.T. Effects of loud and amplified speech on sentence and word intelligibility in Parkinson disease. J. Speech Lang. Hear. Res. 2009, 52, 1021–1033. [Google Scholar] [CrossRef]
- Dromey, C. Articulatory kinematics in patients with Parkinson Disease using different speech treatment approaches. J. Med. Speech-Lang. Pathol. 2000, 8, 155–161. [Google Scholar]
- Mefferd, A.S. Effects of speaking rate, loudness, and clarity modifications on kinematic endpoint variability. Clin. Linguist. Phon. 2019, 33, 570–585. [Google Scholar] [CrossRef] [PubMed]
- McClean, M.D. Patterns of Orofacial Movement Velocity across Variations in Speech Rate. J. Speech Lang. Hear. Res. 2000, 43, 205–216. [Google Scholar] [CrossRef]
- McClean, M.D.; Tasko, S.M. Association of Orofacial Muscle Activity and Movement during Changes in Speech Rate and Intensity. J. Speech Lang. Hear. Res. 2003, 46, 1387–1400. [Google Scholar] [CrossRef]
- Tasko, S.M.; McClean, M.D. Variations in Articulatory Movement with Changes in Speech Task. J. Speech Lang. Hear. Res. 2004, 47, 85–100. [Google Scholar] [CrossRef]
- Tjaden, K.; Wilding, G.E. Rate and Loudness Manipulations in Dysarthria. J. Speech Lang. Hear. Res. 2004, 47, 766–783. [Google Scholar] [CrossRef] [PubMed]
- Tjaden, K.; Sussman, J.E.; Wilding, G.E. Impact of Clear, Loud, and Slow Speech on Scaled Intelligibility and Speech Severity in Parkinson’s Disease and Multiple Sclerosis. J. Speech Lang. Hear. Res. 2014, 57, 779–792. [Google Scholar] [CrossRef] [PubMed]
- Nip, I.S.B. Articulatory and Vocal Fold Movement Patterns During Loud Speech in Children with Cerebral Palsy. J. Speech Lang. Hear. Res. 2024, 67, 477–493. [Google Scholar] [CrossRef]
- Konnai, R.; Scherer, R.C.; Peplinski, A.; Ryan, K. Whisper and Phonation: Aerodynamic Comparisons across Adduction and Loudness. J. Voice 2017, 31, 773.e11–773.e20. [Google Scholar] [CrossRef]
- Rubin, A.D.; Praneetvatakul, V.; Gherson, S.; Moyer, C.A.; Sataloff, R.T. Laryngeal hyperfunction during whispering: Reality or myth? J. Voice 2006, 20, 121–127. [Google Scholar] [CrossRef]
- Searl, J. Comparison of Transducers and Intraoral Placement Options for Measuring Lingua-Palatal Contact Pressure during Speech. J. Speech Lang. Hear. Res. 2003, 46, 1444–1456. [Google Scholar] [CrossRef] [PubMed]
- Whitehill, T.L.; Lee, A.S.; Chun, J.C. Direct magnitude estimation and interval scaling of hypernasality. J. Speech Lang. Hear. Res. 2002, 45, 80–88. [Google Scholar] [CrossRef]
- Schiavetti, N.; Sacco, P.R.; Metz, D.E.; Sitler, R.W. Direct magnitude estimation and interval scaling of stuttering severity. J. Speech Hear. Res. 1983, 26, 568–573. [Google Scholar] [CrossRef]
- Lee, Y.W.; Kim, G.H. Usefulness of Direct Magnitude Estimation (DME) and Acoustic Analysis in Measuring Dysphonia Severity. J. Voice 2024, in press. [Google Scholar] [CrossRef]
- Pallant, J. SPSS Survival Manual: A Step by Step Guide to Data Analysis Using IBM SPSS, 7th ed.; Routledge: London, UK, 2020. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Earlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Dromey, C.; Ramig, L.O. Intentional Changes in Sound Pressure Level and Rate. J. Speech Lang. Hear. Res. 1998, 41, 1003–1018. [Google Scholar] [CrossRef]
- Searl, J. Bilabial Contact Pressure and Oral Air Pressure during Tracheoesophageal Speech. Ann. Otol. Rhinol. Laryngol. 2007, 116, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Borrie, S.; McAuliffe, M.; Tillard, G.; Ormond, T.; Anderson, T.; Hornibrook, J. Effect of Lee Silverman Voice Treatment (LSVT) on articulation in speakers with Parkinson’s Disease. N. Z. J. Speech-Lang. Ther. 2007, 62, 29–36. [Google Scholar]
- Wenke, R.J.; Theodoros, D.; Cornwell, P. The short- and long-term effectiveness of the LSVT for dysarthria following TBI and stroke. Brain Inj. 2008, 22, 339–352. [Google Scholar] [CrossRef] [PubMed]



| Phoneme | Loudness Condition | Statistic | Loudness Condition | ||
|---|---|---|---|---|---|
| Soft | Habitual | Loud | |||
| /t/ | Whisper | Z | −3.296 | −3.297 | −3.296 |
| p | <0.001 | <0.001 | <0.001 | ||
| Soft | Z | -- | −3.297 | −3.297 | |
| p | -- | <0.001 | <0.001 | ||
| Habitual | Z | -- | -- | −3.233 | |
| p | -- | -- | 0.001 | ||
| /d/ | Whisper | Z | −3.297 | −2.417 | −3.296 |
| p | <0.001 | 0.016 | <0.001 | ||
| Soft | Z | -- | −3.170 | −3.297 | |
| p | -- | 0.002 | <0.001 | ||
| Habitual | Z | -- | -- | −3.170 | |
| p | -- | -- | 0.002 | ||
| /s/ | Whisper | Z | −2.794 | −2.323 | −3.297 |
| p | 0.005 | 0.020 | <0.001 | ||
| Soft | Z | -- | −2.88 | −3.296 | |
| p | -- | 0.004 | <0.001 | ||
| Habitual | Z | -- | -- | −3.297 | |
| p | -- | -- | <0.001 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Searl, J.; Evitts, P. Changes in Articulatory Contact Pressure as a Function of Vocal Loudness. Appl. Sci. 2024, 14, 8853. https://doi.org/10.3390/app14198853
Searl J, Evitts P. Changes in Articulatory Contact Pressure as a Function of Vocal Loudness. Applied Sciences. 2024; 14(19):8853. https://doi.org/10.3390/app14198853
Chicago/Turabian StyleSearl, Jeff, and Paul Evitts. 2024. "Changes in Articulatory Contact Pressure as a Function of Vocal Loudness" Applied Sciences 14, no. 19: 8853. https://doi.org/10.3390/app14198853






