An Overview of Tools and Technologies for Anxiety and Depression Management Using AI
Abstract
:1. Introduction
- Can artificial intelligence effectively aid in the identification and management of symptoms associated with anxiety and depression by addressing the limitations of traditional diagnostic methods and providing continuous, personalized support for improved mental health outcomes?
- Which artificial intelligence techniques are currently employed for symptom management of anxiety and depression, and how is their efficacy evaluated?
- What potential benefits and dangers are arising from the utilization of these technologies by individuals and health care practitioners?
2. Background: The Role of Informatics and AI in Mental Health
3. Methods
4. Results of Overview
4.1. Natural Language Processing (NLP)
4.2. Predictive Analysis
4.3. AI Methodologies and Tools Utilized for Anxiety and Depression Management
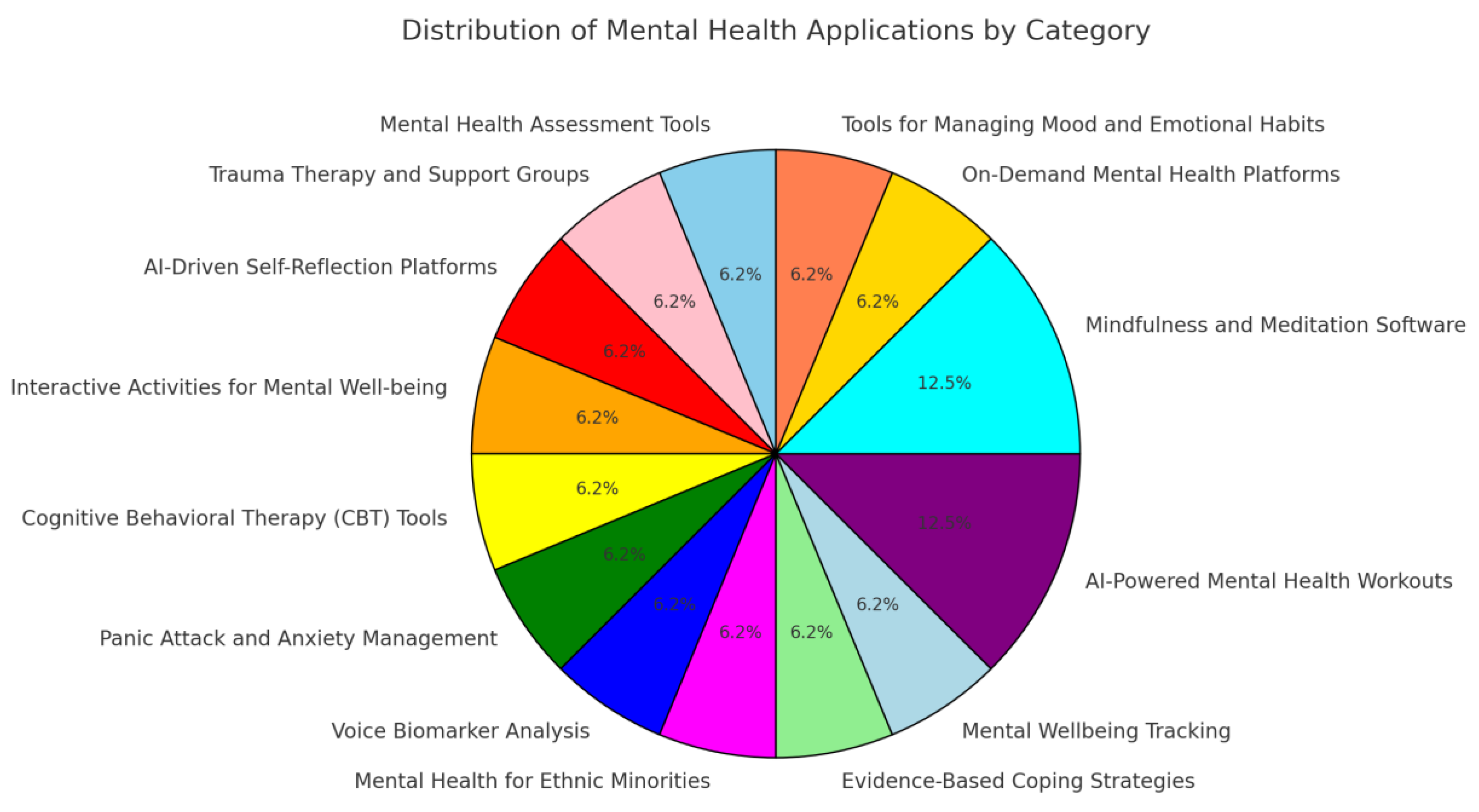
4.3.1. Mobile Apps
4.3.2. Chatbots
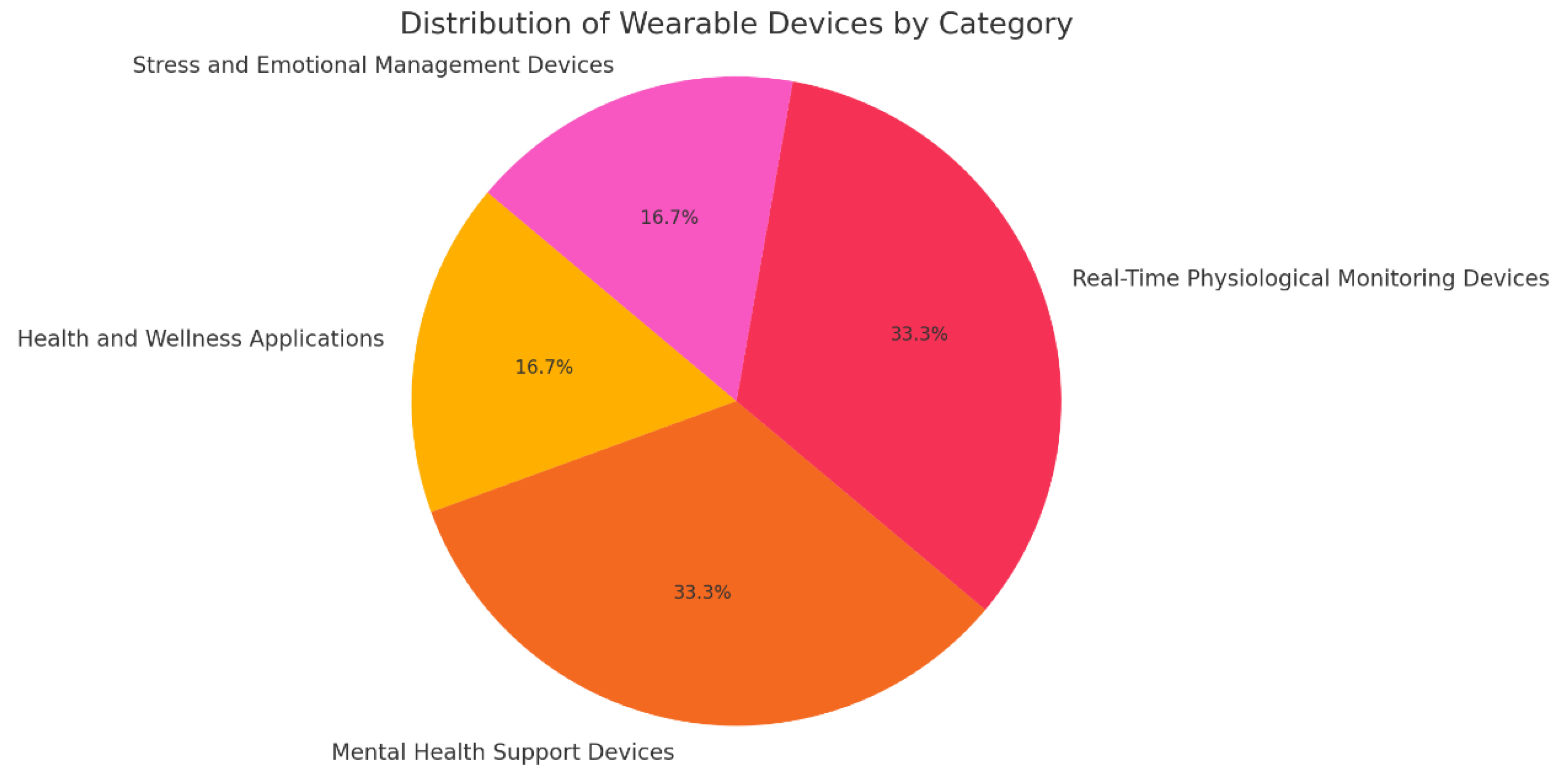
4.3.3. Wearables and Biosignals
4.4. Virtual Reality (VR) Therapies
4.5. Therapies Using Augmented Reality (AR)
4.6. LLMs in the Treatment of Anxiety and Depression
4.6.1. The Potential of Large Language Models
4.6.2. Examining the Ethical Considerations and Potential Biases
4.6.3. Prospects for the Future and Suggestions for Improvement
4.6.4. Enhancing the Accuracy and Efficiency of Psychiatric and Psychological Care
5. Evaluation of AI Tools—Case Studies
5.1. Quantitative Evaluation
5.2. Practical Impact of AI Tools on Users’ Daily Lives
5.3. Accessibility
5.4. User Experience
6. Discussion, Challenges, and Limitations
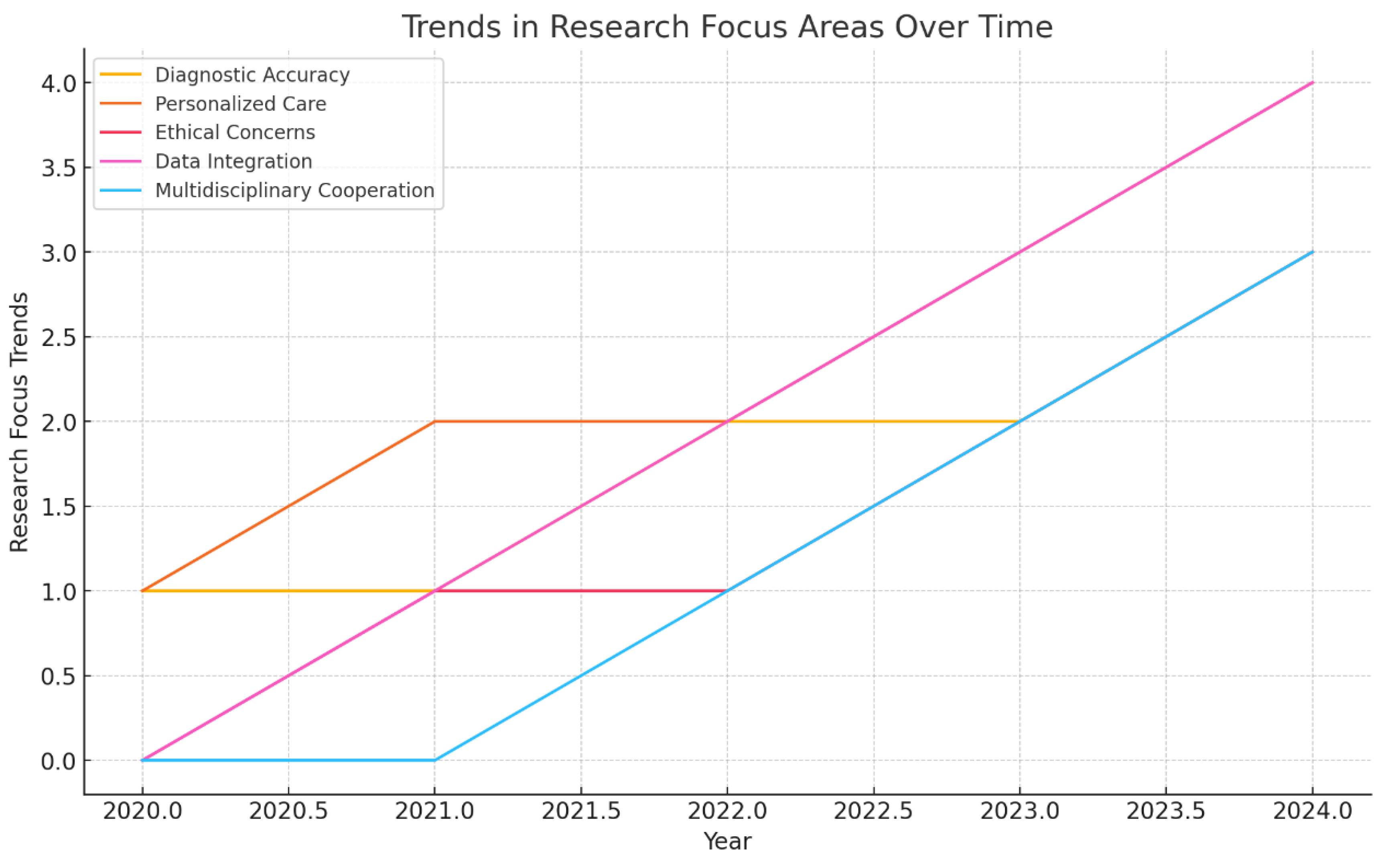
7. Conclusions and Future Orientations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lederbogen, F.; Kirsch, P.; Haddad, L.; Streit, F.; Tost, H.; Schuch, P.; Meyer-Lindenberg, A. City living and urban upbringing affect neural social stress processing in humans. Nature 2011, 474, 498–501. [Google Scholar] [CrossRef] [PubMed]
- Healthline. Anxiety Chest Pain: Symptoms, Home Remedies, and More. Available online: https://www.healthline.com/health/anxiety/anxiety-chest-pain#see-a-doctor (accessed on 3 December 2019).
- Ding, N.B. Anxiety disorders and phobias: A cognitive perspective. Health Soc. Work 1988, 13, 76–77. [Google Scholar] [CrossRef]
- Skapinakis, P.; Bellos, S.; Oikonomou, A.; Dimitriadis, G.; Gkikas, P.; Perdikari, E.; Mavreas, V. Depression and its relationship with coping strategies and illness perceptions during the Covid-19 lockdown in Greece: A cross-sectional survey of the population. Depress. Res. Treat. 2020, 3158954. [Google Scholar] [CrossRef] [PubMed]
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2020, 20, 1537–1545. [Google Scholar] [CrossRef] [PubMed]
- Alberts, N.M.; Leisenring, W.M.; Flynn, J.S.; Whitton, J.; Gibson, T.M.; Jibb, L.; Armstrong, G.T. Wearable Respiratory Monitoring and Feedback for Chronic Pain in Adult Survivors of Childhood Cancer: A Feasibility Randomized Controlled Trial From the Childhood Cancer Survivor Study. JCO Clin. Cancer Inform. 2020, 4, 1014–1026. [Google Scholar] [CrossRef]
- Odgers, C.L.; Jensen, M.R. Annual Research Review: Adolescent mental health in the digital age: Facts, fears, and future directions. J. Child Psychol. Psychiatry 2020, 61, 336–348. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Mittal, D.; Reaves, C.M.; Haynes, T.F.; Han, X.; Morris, S.; Sullivan, G. Mental health stigma and primary health care decisions. Psychiatry Res. 2014, 218, 35–38. [Google Scholar] [CrossRef]
- Fitzpatrick, K.K.; Darcy, A.; Vierhile, M. Delivering Cognitive Behavior Therapy to Young Adults With Symptoms of Depression and Anxiety Using a Fully Automated Conversational Agent (Woebot): A Randomized Controlled Trial. JMIR Ment. Health 2017, 4, e19. [Google Scholar] [CrossRef]
- Lattie, E.G.; Nicholas, J.; Knapp, A.A.; Skerl, J.J.; Kaiser, S.M.; Mohr, D.C. Opportunities for and Tensions Surrounding the Use of Technology-Enabled Mental Health Services in Community Mental Health Care. Adm. Policy Ment. Health Ment. Health Serv. Res. 2020, 47, 138–149. [Google Scholar] [CrossRef]
- Morales, A.; Barbosa, M.; Morás, L.; Cazella, S.C.; Sgobbi, L.F.; Sene, I.; Marques, G. Occupational Stress Monitoring Using Biomarkers and Smartwatches: A Systematic Review. Sensors 2022, 22, 6633. [Google Scholar] [CrossRef]
- Sadeh-Sharvit, S.; Del Camp, T.; Horton, S.E.; Hefner, J.D.; Berry, J.M.; Grossman, E.; Hollon, S.D. Effects of an Artificial Intelligence Platform for Behavioral Interventions on Depression and Anxiety Symptoms: Randomized Clinical Trial. J. Med. Internet Res. 2023, 25, e46781. [Google Scholar] [CrossRef] [PubMed]
- Barua, P.D.; Vicnesh, J.; Lih, O.S.; Palmer, E.E.; Yamakawa, T.; Kobayashi, M.; Acharya, U.R. Artificial intelligence assisted tools for the detection of anxiety and depression leading to suicidal ideation in adolescents: A review. Cogn Neurodyn. 2024, 18, 1–22. [Google Scholar] [CrossRef]
- Rani, K.; Vishnoi, H.; Mishra, M. A Mental Health Chatbot Delivering Cognitive Behavior Therapy and Remote Health Monitoring Using NLP And AI. In Proceedings of the 2023 International Conference on Disruptive Technologies (ICDT), Greater Noida, India, 11–12 May 2023; pp. 313–317. [Google Scholar] [CrossRef]
- Sandhu, D.E. Compute Depression and Anxiety Among Students in Pakistan, Using Machine Learning. Lahore Garrison Univ. Res. J. Comput. Sci. Inf. Technol. 2022, 6, 4–11. [Google Scholar] [CrossRef]
- Lee, E.E.; Torous, J.; De Choudhury, M.; Depp, C.A.; Graham, S.A.; Kim, H.C.; Jeste, D.V. Artificial Intelligence for Mental Health Care: Clinical Applications, Barriers, Facilitators, and Artificial Wisdom. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2021, 6, 856–864. [Google Scholar] [CrossRef] [PubMed]
- Mohr, D.C.; Burns, M.N.; Schueller, S.M.; Clarke, G.; Klinkman, M. Behavioral Intervention Technologies: Evidence review and recommendations for future research in mental health. Gen. Hosp. Psychiatry 2013, 35, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Ewbank, M.P.; Cummins, R.; Tablan, V.; Bateup, S.; Catarino, A.; Martin, A.J.; Blackwell, A.D. Quantifying the Association Between Psychotherapy Content and Clinical Outcomes Using Deep Learning. JAMA Psychiatry 2020, 77, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Kleine, A.K.; Lermer, E.; Cecil, J.; Heinrich, A.; Gaube, S. Advancing mental health care with AI-enabled precision psychiatry tools: A patent review. Comput. Hum. Behav. Rep. 2023, 12, 100322. [Google Scholar] [CrossRef]
- Tausczik, Y.R.; Pennebaker, J.W. The psychological meaning of words: LIWC and computerized text analysis methods. J. Lang. Soc. Psychol. 2010, 29, 24–54. [Google Scholar] [CrossRef]
- Lovejoy, C.A.; Buch, V.; Maruthappu, M. Technology and mental health: The role of artificial intelligence. Eur. Psychiatry 2019, 55, 1–3. [Google Scholar] [CrossRef]
- Rowe, N.C.; Chan, A.L. Rating whole-body suspiciousness factors in automated surveillance of a public area. In Proceedings of the 2011 International Conference on Image Processing, Computer Vision, and Pattern Recognition, Las Vegas, NV, USA, 18–21 July 2011; Volume 1, pp. 317–322. [Google Scholar]
- Goldberg, S.B.; Flemotomos, N.; Martinez, V.R.; Tanana, M.J.; Kuo, P.B.; Pace, B.T.; Atkins, D.C. Machine learning and natural language processing in psychotherapy research: Alliance as example use case. J. Couns. Psychol. 2020, 67, 438–448. [Google Scholar] [CrossRef]
- Nemesure, M.D.; Heinz, M.V.; Huang, R.; Jacobson, N.C. Predictive modeling of depression and anxiety using electronic health records and a novel machine learning approach with artificial intelligence. Sci. Rep. 2021, 11, 1980. [Google Scholar] [CrossRef] [PubMed]
- Ku, W.L.; Min, H. Evaluating Machine Learning Stability in Predicting Depression and Anxiety Amidst Subjective Response Errors. Healthcare 2024, 12, 625. [Google Scholar] [CrossRef] [PubMed]
- Sharma, G.; Schlosser, L.; Jones, B.D.M.; Blumberger, D.M.; Gratzer, D.; Husain, M.O.; Husain, M.I. Brief App-Based Cognitive Behavioral Therapy for Anxiety Symptoms in Psychiatric Inpatients: Feasibility Randomized Controlled Trial. JMIR Form. Res. 2022, 6, e38460. [Google Scholar] [CrossRef] [PubMed]
- Inkster, B.; Sarda, S.; Subramanian, V. An Empathy-Driven, Conversational Artificial Intelligence Agent (Wysa) for Digital Mental Well-Being: Real-World Data Evaluation Mixed-Methods Study. JMIR mHealth uHealth 2018, 6, e12106. [Google Scholar] [CrossRef] [PubMed]
- Mehta, A.; Niles, A.N.; Vargas, J.H.; Marafon, T.; Couto, D.D.; Gross, J.J. Acceptability and Effectiveness of Artificial Intelligence Therapy for Anxiety and Depression (Youper): Longitudinal Observational Study. J. Med. Internet Res. 2021, 23, e26771. [Google Scholar] [CrossRef] [PubMed]
- Pentina, I.; Xie, T.; Hancock, T.; Bailey, A. Consumer–machine relationships in the age of artificial intelligence: Systematic literature review and research directions. Psychol. Mark. 2023, 40, 1593–1614. [Google Scholar] [CrossRef]
- Callahan, L. Lifeline Ally. Theresanaiforthat.com. 2023. Available online: https://theresanaiforthat.com/gpt/lifeline-ally/ (accessed on 30 September 2024).
- YesChat. Humorous Psychological Companion—Free, Humorous, Empathetic AI Chat. 2023. Available online: https://www.yeschat.ai (accessed on 30 September 2024).
- Romanovskyi, O.; Pidbutska, N.; Knysh, A. Elomia chatbot: The effectiveness of artificial intelligence in the fight for mental health. CEUR Workshop Proc. 2021, 2870, 1215–1224. [Google Scholar]
- Fulmer, R.; Joerin, A.; Gentile, B.; Lakerink, L.; Rauws, M. Using Psychological Artificial Intelligence (Tess) to Relieve Symptoms of Depression and Anxiety: Randomized Controlled Trial. JMIR Ment. Health 2018, 5, e64. [Google Scholar] [CrossRef]
- “I’m Fine. Everything Is Fine.”. 2024. Available online: https://www.kintsugihealth.com/ (accessed on 30 September 2024).
- Ginger.io: An App That Monitors Your Mental Health. 2018. Available online: https://d3.harvard.edu/platform-digit/submission/ginger-io-an-app-that-monitors-your-mental-health/ (accessed on 30 September 2024).
- Headspace for Organizations. Mental Healthcare for Every Moment [Internet]. Available online: https://organizations.headspace.com/ (accessed on 30 September 2024).
- Chrome Web Store. Breathhh: Workplace Wellbeing Companion. 2024. Available online: https://chromewebstore.google.com/detail/breathhh-workplace-wellbe/niipedbmjiopjpmjcpigiflabghcckeo/reviews (accessed on 30 September 2024).
- Mental Health Starts with You. 2024. Available online: https://minddoc.com/us/en (accessed on 30 September 2024).
- Crunchbase. Ladder. 2024. Available online: https://www.crunchbase.com/organization/ladder-433e (accessed on 20 September 2024).
- Calm Your Mind. Change Your Life. 2024. Available online: https://www.calm.com/ (accessed on 30 September 2024).
- Panic Attack and Anxiety Relief. 2024. Available online: https://www.rootd.io/ (accessed on 30 September 2024).
- Kalisperakis, E.; Karantinos, T.; Lazaridi, M.; Garyfalli, V.; Filntisis, P.P.; Zlatintsi, A.; Efthymiou, N.; Mantas, A.; Mantonakis, L.; Mougiakos, T.; et al. Smartwatch digital phenotypes predict positive and negative symptom variation in a longitudinal monitoring study of patients with psychotic disorders. Front. Psychiatry 2023, 14, 1024965. [Google Scholar] [CrossRef]
- Overcome Negative Thoughts, Stress & Life’s Challenges! 2024. Available online: https://www.happify.com/ (accessed on 30 September 2024).
- Deepwander. Available online: https://thataicollection.com/en/application/deepwander/ (accessed on 30 September 2024).
- Your Virtual Self-Care Partner. 2024. Available online: https://mindwell.ai/en/treatments/anxiety-treatment (accessed on 2 September 2024).
- Space of Mind: Affordable PTSD Facilitated Peer Support. 2024. Available online: https://www.spaceofmind.com (accessed on 30 September 2024).
- Psychiatry.org. MoodPath. 2019. Available online: https://www.psychiatry.org (accessed on 30 September 2024).
- Samsung. Measure Your Stress Level with Samsung Health. 2024. Available online: https://www.samsung.com/us/support/answer/ANS00080574/ (accessed on 15 August 2024).
- MoodTools. 2024. Available online: https://moodtools.org/ (accessed on 15 August 2024).
- Kawadler, J.M.; Hemmings, N.R.; Ponzo, S.; Morelli, D.; Bird, G.; Plans, D. Effectiveness of a smartphone app (Biobase) for reducing anxiety and increasing mental well-being: Pilot feasibility and acceptability study. JMIR Form. Res. 2020, 4, e18067. [Google Scholar] [CrossRef]
- Spire Health. Welcome to Health Tag. 2024. Available online: https://www.spirehealth.com/patient-setup (accessed on 12 August 2024).
- Moodmetric. Smart Ring for Stress Measurement and Management. 2024. Available online: https://smartringnews.com/smart-ring-products/moodmetric/ (accessed on 30 September 2024).
- Fisher Wallace. A Superdevice for Depression and Anxiety. 2024. Available online: https://www.fisherwallace.com/ (accessed on 20 August 2024).
- González Ramírez, M.L.; García Vázquez, J.P.; Rodríguez, M.D.; Padilla-López, L.A.; Galindo-Aldana, G.M.; Cuevas-González, D. Wearables for Stress Management: A Scoping Review. Healthcare 2023, 11, 2369. [Google Scholar] [CrossRef] [PubMed]
- Gomes, N.; Pato, M.; Lourenço, A.R.; Datia, N. A Survey on Wearable Sensors for Mental Health Monitoring. Sensors 2023, 23, 1330. [Google Scholar] [CrossRef] [PubMed]
- Becker, T.D.; Torous, J.B. Recent Developments in Digital Mental Health Interventions for College and University Students. Curr. Treat. Options Psychiatry 2019, 6, 210–220. [Google Scholar] [CrossRef]
- Bautista, J.; Liu, M.; Alvarez, M.; Schueller, S.M. Multi-Media Field Test: Cognitive-Behavioral Therapy at Our Fingertips: Sanvello Provides On-Demand Support for Mental Health. Cogn. Behav. Pract. 2024. [CrossRef]
- Liu, L. What Makes Inflection’s Pi a Great Companion Chatbot. Medium. 2023. Available online: https://medium.com/@lindseyliu/what-makes-inflections-pi-a-great-companion-chatbot-8a8bd93dbc43 (accessed on 30 September 2024).
- Bakker, D.R.; Rickard, N. MoodMission: A Mobile App for Managing Anxiety and Depression. Monash Lens. 2024. Available online: https://au.reachout.com/tools-and-apps/moodmission (accessed on 12 August 2024).
- New MindShift™ CBT App Gives Canadians Free Anxiety Relief. 10 May 2024. Available online: https://www.anxietycanada.com/articles/new-mindshift-cbt-app-gives-canadians-free-anxiety-relief/ (accessed on 25 August 2024).
- Sanvello: Anxiety Depression APK for Android. 12 May 2024. Available online: https://pacifica-stress-anxiety.en.softonic.com/android (accessed on 25 August 2024).
- App: Phobos, AR. 2024. Available online: https://thomasmore.be/en/exp-zw/mw/app-phobos-ar (accessed on 25 August 2024).
- Mercer, S.W.; Reynolds, W.J. Empathy and quality of care. Br. J. Gen. Pract. 2002, 52, S9–S12. [Google Scholar]
- Oshevwe, Y.; Oluwatoyin, A.F.; Paschal, C.M.; Chinaemelum, O.C.; Tolulope, S.O. The role of technology in enhancing mental health advocacy: A systematic review. Int. J. Appl. Res. Soc. Sci. 2024, 6, 37–50. [Google Scholar] [CrossRef]
- Sigurðardóttir, S.; Helgadóttir, F.D.; Menzies, R.E.; Sighvatsson, M.B.; Menzies, R.G. Improving adherence to a web-based cognitive-behavioural therapy program for social anxiety with group sessions: A randomised control trial. Internet Interv. 2022, 28, 100535. [Google Scholar] [CrossRef]
- Youper. Clinically Validated AI for Mental Healthcare. 2023. Available online: https://www.youper.ai (accessed on 30 September 2024).
- Solis, E. How Mental Health Apps Are Handling Personal Information. New America. 2024. Available online: https://www.newamerica.org/oti/blog/how-mental-health-apps-are-handling-personal-information/ (accessed on 25 August 2024).
- Lu, L.; Zhang, J.; Xie, Y.; Gao, F.; Xu, S.; Wu, X.; Ye, Z. Wearable health devices in health care: Narrative systematic review. JMIR mHealth uHealth 2020, 8, e18907. [Google Scholar] [CrossRef]
- Cheng, Y.; Wang, K.; Xu, H.; Li, T.; Jin, Q.; Cui, D. Recent developments in sensors for wearable device applications. Anal. Bioanal. Chem. 2021, 413, 6037–6057. [Google Scholar] [CrossRef]
- Smith, E.N.; Santoro, E.; Moraveji, N.; Susi, M.; Crum, A.J. Integrating wearables in stress management interventions: Promising evidence from a randomized trial. Int. J. Stress Manag. 2020, 27, 172–182. [Google Scholar] [CrossRef]
- Ponzo, S.; Morelli, D.; Kawadler, J.M.; Hemmings, N.R.; Bird, G.; Plans, D. Efficacy of the Digital Therapeutic Mobile App BioBase to Reduce Stress and Improve Mental Well-Being Among University Students: Randomized Controlled Trial. JMIR mHealth uHealth 2020, 8, e17767. [Google Scholar] [CrossRef] [PubMed]
- University of Tennessee. Artificial Intelligence (AI) Tools. 2024. Available online: https://research.utk.edu/research-integrity/artificial-intelligence-ai-tools/ (accessed on 12 September 2024).
- Rawat, M. Best AI Apps for Mental Health (2023). MarkTechPost. 2023. Available online: https://www.marktechpost.com/2023/04/11/best-ai-apps-for-mental-health-2023/ (accessed on 12 September 2024).
- Fisher Wallace. Have Depression, Anxiety or Insomnia? An Easy-to-Use Medical Device is Now Available for Use at Home. 2024. Available online: https://www.fisherwallace.com/pages/have-depression-anxiety-or-insomnia-an-easy-to-use-medical-device-is-now-available-for-use-at-home (accessed on 30 September 2024).
- Schröder, D.; Wrona, K.J.; Müller, F.; Heinemann, S.; Fischer, F.; Dockweiler, C. Impact of virtual reality applications in the treatment of anxiety disorders: A systematic review and meta-analysis of randomized-controlled trials. J. Behav. Ther. Exp. Psychiatry 2023, 81, 101893. [Google Scholar] [CrossRef] [PubMed]
- Jingili, N.; Oyelere, S.S.; Nyström, M.B.T.; Anyshchenko, L. A systematic review on the efficacy of virtual reality and gamification interventions for managing anxiety and depression. Front. Digit. Health 2023, 5, 1239435. [Google Scholar] [CrossRef]
- Baghaei, N.; Chitale, V.; Hlasnik, A.; Stemmet, L.; Liang, H.N.; Porter, R. Virtual Reality for Supporting the Treatment of Depression and Anxiety: Scoping Review. JMIR Ment. Health 2021, 8, e29681. [Google Scholar] [CrossRef]
- De Witte, N.A.J.; Joris, S.; Van Assche, E.; Van Daele, T. Technological and Digital Interventions for Mental Health and Wellbeing: An Overview of Systematic Reviews. Front. Digit. Health 2021, 3, 754337. [Google Scholar] [CrossRef]
- Ito, A.; Hiyoshi, F.; Kanie, A.; Maruyama, A.; Oba, M.S.; Kito, S. Feasibility Study of Virtual Reality–Based Cognitive Behavioral Therapy for Patients With Depression: Protocol for an Open Trial and Therapeutic Intervention. JMIR Res. Protoc. 2023, 12, e49698. [Google Scholar] [CrossRef]
- Oh, J.; Kim, M.; Park, H.; Oh, H. Are you depressed? Analyze user utterances to detect depressive emotions using DistilBERT. Appl. Sci. 2023, 13, 6223. [Google Scholar] [CrossRef]
- Newson, J.J.; Thiagarajan, T.C. Assessment of Population Well-Being With the Mental Health Quotient (MHQ): Development and Usability Study. JMIR Ment. Health 2020, 7, e17935. [Google Scholar] [CrossRef]
- Berenguer, C.; Baixauli, I.; Gómez, S.; Andrés, M.d.E.P.; De Stasio, S. Exploring the Impact of Augmented Reality in Children and Adolescents with Autism Spectrum Disorder: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 6143. [Google Scholar] [CrossRef]
- Suso-Ribera, C.; Fernández-Álvarez, J.; García-Palacios, A.; Hoffman, H.G.; Bretón-López, J.; Baños, R.M.; Botella, C. Virtual Reality, Augmented Reality, and in Vivo Exposure Therapy: A Preliminary Comparison of Treatment Efficacy in Small Animal Phobia. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Nicosia, J.; Wang, B.; Aschenbrenner, A.J.; Sliwinski, M.J.; Yabiku, S.T.; Roque, N.A.; Hassenstab, J. To BYOD or not: Are device latencies important for bring-your-own-device (BYOD) smartphone cognitive testing? Behav. Res. Methods 2023, 55, 2800–2812. [Google Scholar] [CrossRef] [PubMed]
- Ivanov, V.M.; Krivtsov, A.M.; Strelkov, S.V.; Smirnov, A.Y.; Shipov, R.Y.; Grebenkov, V.G.; Koskin, V.S. Practical Application of Augmented/Mixed Reality Technologies in Surgery of Abdominal Cancer Patients. J. Imaging 2022, 8, 183. [Google Scholar] [CrossRef] [PubMed]
- Lundin, R.M.; Yeap, Y.; Menkes, D.B. Adverse Effects of Virtual and Augmented Reality Interventions in Psychiatry: Systematic Review. JMIR Ment. Health 2023, 10, e43240. [Google Scholar] [CrossRef] [PubMed]
- Sawh, M. Stress Wearables: Best Devices That Monitor Stress and How They Work. Wareable. 2022. Available online: https://www.wareable.com/health-and-wellbeing/stress-monitoring-wearables-explained-7969 (accessed on 25 August 2024).
- Obradovich, N.; Khalsa, S.S.; Khan, W.U.; Suh, J.; Perlis, R.H.; Ajilore, O.; Paulus, M.P. Opportunities and risks of large language models in psychiatry. NPP—Digit. Psychiatry Neurosci. 2024, 2, 8. [Google Scholar] [CrossRef]
- Stavrianos, P.; Pavlopoulos, A.; Maglogiannis, I. Enabling speech emotional intelligence as a service in homecare platforms. Pervasive Healthcare: A Compendium of Critical Factors for Success; EAI/Springer Innovations in Communication and Computing; Springer: Cham, Switzerland, 2022; pp. 119–144. [Google Scholar] [CrossRef]
- Zlatintsi, A.; Filntisis, P.P.; Garou, C.; Efthymiou, N.; Maragos, P.; Menychtas, A.; Maglogiannis, I.; Tsanakas, P.; Sounapoglou, T.; Kalisperakis, E. E-Prevention: Advanced support system for monitoring and relapse prevention in patients with psychotic disorders analyzing long-term multimodal data from wearables and video captures. Sensors 2022, 22, 7544. [Google Scholar] [CrossRef]
- Gallos, P.; Menychtas, A.; Panagopoulos, C.; Kaselimi, M.; Temenos, A.; Rallis, I.; Doulamis, A.; Doulamis, N.; Bimpas, M.; Aggeli, A.; et al. Using mHealth technologies to promote public health and well-being in urban areas with blue-green solutions. Stud. Health Technol. Inform. 2022, 295, 566–569. [Google Scholar] [CrossRef]
- Maglogiannis, I.; Zlatintsi, A.; Menychtas, A.; Papadimatos, D.; Filntisis, P.P.; Efthymiou, N.; Retsinas, G.; Tsanakas, P.; Maragos, P. An intelligent cloud-based platform for effective monitoring of patients with psychotic disorders. In Artificial Intelligence Applications and Innovations: 16th IFIP WG 12.5 International Conference, AIAI 2020, Neos Marmaras, Greece, June 5–7, 2020, Proceedings, Part II 16; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Squires, M.; Tao, X.; Elangovan, S.; Gururajan, R.; Zhou, X.; Acharya, U.R.; Li, Y. Deep learning and machine learning in psychiatry: A survey of current progress in depression detection, diagnosis and treatment. Brain Inform. 2023, 10, 10. [Google Scholar] [CrossRef]
- Xie, W.; Wang, C.; Lin, Z.; Luo, X.; Chen, W.; Xu, M.; Cheng, M. Multimodal fusion diagnosis of depression and anxiety based on CNN-LSTM model. Comput. Med. Imaging Graph. 2022, 102, 102128. [Google Scholar] [CrossRef]
- Shoumy, N.J.; Ang, L.M.; Seng, K.P.; Rahaman, D.M.; Zia, T. Multimodal big data affective analytics: A comprehensive survey using text, audio, visual and physiological signals. J. Netw. Comput. Appl. 2020, 149, 102447. [Google Scholar] [CrossRef]
- Xiao, H.; Zhou, F.; Liu, X.; Liu, T.; Li, Z.; Liu, X.; Huang, X. A comprehensive survey of large language models and multimodal large language models in medicine. arXiv 2024, arXiv:2405.08603. [Google Scholar]
- Zadgaonkar, A.; Keskar, R.; Kakde, O. Towards a machine learning model for detection of dementia using lifestyle parameters. Appl. Sci. 2023, 13, 10630. [Google Scholar] [CrossRef]
- Zhang, W.; Lin, T.; Liu, J.; Shu, F.; Li, H.; Zhang, L.; Zhuang, Y. HyperLLaVA: Dynamic visual and language expert tuning for multimodal large language models. arXiv 2024, arXiv:2403.13447. [Google Scholar]
- Chen, J.; Jiang, Y.; Yang, D.; Li, M.; Wei, J.; Qian, Z.; Zhang, L. Can LLMs’ tuning methods work in the medical multimodal domain? arXiv 2024, arXiv:2403.06407. [Google Scholar]
- Wu, Y.; Xiang, Y.; Huo, S.; Gong, Y.; Liang, P. LoRA-SP: Streamlined partial parameter adaptation for resource efficient fine-tuning of large language models. In Proceedings of the Third International Conference on Algorithms, Microchips, and Network Applications (AMNA 2024), Jinan, China, 8–10 March 2024; pp. 488–496. [Google Scholar]
- Wang, Y.; Chen, W.; Han, X.; Lin, X.; Zhao, H.; Liu, Y.; Yang, H. Exploring the reasoning abilities of multimodal large language models (mllms): A comprehensive survey on emerging trends in multimodal reasoning. arXiv 2024, arXiv:2401.06805. [Google Scholar]
- Shajari, S.; Kuruvinashetti, K.; Komeili, A.; Sundararaj, U. The emergence of AI-based wearable sensors for digital health technology: A review. Sensors 2023, 23, 9498. [Google Scholar] [CrossRef]
- Spitzer, M.; Dattner, I.; Zilcha-Mano, S. Digital twins and the future of precision mental health. Front. Psychiatry 2023, 14, 1082598. [Google Scholar] [CrossRef]
- Vallée, A. Envisioning the future of personalized medicine: Role and realities of digital twins. J. Med. Internet Res. 2024, 26, e50204. [Google Scholar] [CrossRef]
- GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [Google Scholar] [CrossRef]
- Abd-alrazaq, A.; AlSaad, R.; Aziz, S.; Ahmed, A.; Denecke, K.; Househ, M.; Sheikh, J. Wearable Artificial Intelligence for Anxiety and Depression: Scoping Review. J. Med. Internet Res. 2023, 25, e42672. [Google Scholar] [CrossRef]
- Su, L. Access and Engagement of MoodTools, an mHealth Application for Depression; Georgia State University: Atlanta, GA, USA, 2020. [Google Scholar] [CrossRef]
- Muñoz, S.; Iglesias, C. Detection of the severity level of depression signs in text combining a feature-based framework with distributional representations. Appl. Sci. 2023, 13, 11695. [Google Scholar] [CrossRef]
- Karkosz, S.; Szymański, R.; Sanna, K.; Michałowski, J. Effectiveness of a Web-based and Mobile Therapy Chatbot on Anxiety and Depressive Symptoms in Subclinical Young Adults: A Randomized Controlled Trial (Preprint). JMIR Form. Res. 2023, 8, e47960. [Google Scholar] [CrossRef] [PubMed]
- Balcombe, L.; de Leo, D. Psychological screening and tracking of athletes and digital mental health solutions in a hybrid model of care: Mini review. JMIR Form. Res. 2020, 4, e22755. [Google Scholar] [CrossRef] [PubMed]
- Firth, J.; Torous, J.; Nicholas, J.; Carney, R.; Pratap, A.; Rosenbaum, S.; Sarris, J. The efficacy of smartphone-based mental health interventions for depressive symptoms: A meta-analysis of randomized controlled trials. World Psychiatry 2017, 16, 287–298. [Google Scholar] [CrossRef]
- Schueller, S.M.; Neary, M.; O’Loughlin, K.; Adkins, E.C. Discovery of and Interest in Health Apps Among Those with Mental Health Needs: Survey and Focus Group Study. J. Med. Internet Res. 2018, 20, e10141. [Google Scholar] [CrossRef]
- Schyff, E.L.; Ridout, B.; Amon, K.L.; Forsyth, R.; Campbell, A.J. Providing Self-Led Mental Health Support Through an Artificial Intelligence–Powered Chat Bot (Leora) to Meet the Demand of Mental Health Care. J. Med. Internet Res. 2023, 25, e46448. [Google Scholar] [CrossRef]
- Grimm, B.; Talbot, B.; Larsen, L. PHQ-V/GAD-V: Assessments to identify signals of depression and anxiety from patient video responses. Appl. Sci. 2022, 12, 9150. [Google Scholar] [CrossRef]
- Ahmed, A.; Aziz, S.; Toro, C.T.; Alzubaidi, M.; Irshaidat, S.; Serhan, H.A.; Househ, M. Machine learning models to detect anxiety and depression through social media: A scoping review. Comput. Methods Programs Biomed. Updat. 2022, 2, 100066. [Google Scholar] [CrossRef]
- Brooks, M. AI Tool Flags Anxiety, Depression in Healthcare Workers. Medscape. 2023. Available online: https://www.medscape.com/viewarticle/998047?form=fpf (accessed on 12 August 2024).
- Austin, S.F.; Frøsig, A.; Buus, N.; Lincoln, T.; von Malachowski, A.; Schlier, B.; Simonsen, E. Service User Experiences of Integrating a Mobile Solution (IMPACHS) Into Clinical Treatment for Psychosis. Qual. Health Res. 2021, 31, 942–954. [Google Scholar] [CrossRef]
- Gelfgren, S.; Ineland, J.; Cocq, C. Social media and disability advocacy organizations caught between hopes and realities. Disabil. Soc. 2022, 37, 1085–1106. [Google Scholar] [CrossRef]
- Chou, Y.H.; Lin, C.; Lee, S.H.; Lee, Y.F.; Cheng, L.C. User-Friendly Chatbot to Mitigate the Psychological Stress of Older Adults During the COVID-19 Pandemic: Development and Usability Study. JMIR Form. Res. 2024, 8, e49462. [Google Scholar] [CrossRef] [PubMed]
- Abd-alrazaq, A.; Alhuwail, D.; Schneider, J.; Toro, C.T.; Ahmed, A.; Alzubaidi, M.; Househ, M. The performance of artificial intelligence-driven technologies in diagnosing mental disorders: An umbrella review. npj Digit. Med. 2022, 5, 87. [Google Scholar] [CrossRef] [PubMed]
- Andrews, G.; Cuijpers, P.; Craske, M.G.; McEvoy, P.; Titov, N. Computer Therapy for the Anxiety and Depressive Disorders Is Effective, Acceptable and Practical Health Care: A Meta-Analysis. PLoS ONE 2010, 5, e13196. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.; Hassan, A.; Aziz, S.; Abd-alrazaq, A.A.; Ali, N.; Alzubaidi, M.; Househ, M. Chatbot features for anxiety and depression: A scoping review. Health Inform. J. 2023, 29, 146045822211467. [Google Scholar] [CrossRef]

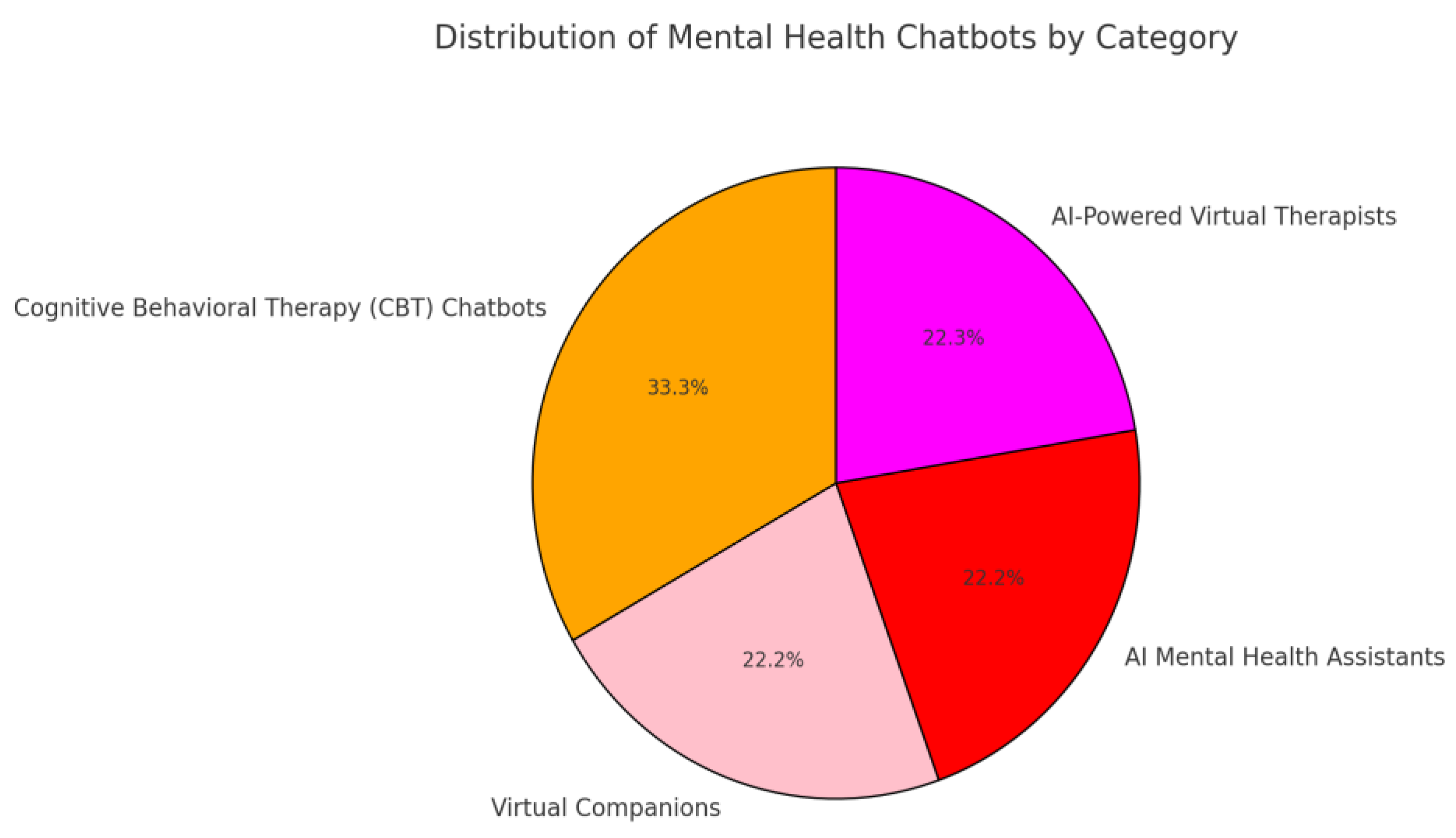

| CHATBOTS | Woebot | Woebot is an AI-driven chatbot that assists individuals in managing their mental well-being through the application of cognitive behavioral therapy approaches. The application offers mood monitoring, daily assessments, and tailored dialogues. As the current leading application, Woebot is likely to continue improving and expanding [9]. |
| Wysa | Wysa is an AI chatbot that utilizes cognitive behavioral therapy techniques to offer support for mental health. Its features include guided meditation, mood tracking, and tailored conversations. Wysa is widely used by individuals seeking mental health support and has garnered positive reviews [27]. | |
| Youper | Youper exemplifies the integration of artificial intelligence (AI) into the realm of mental health care. As a health technology business, the firm aims to ensure that mental health treatment is accessible and affordable for all individuals. Youper AI assistant interacts with individuals in meaningful dialogues to assess their psychological condition and offers tailored remedies based on the gathered information. This groundbreaking approach guarantees that people receive customized assistance, highlighting the transformative capacity of AI in revolutionizing mental health care [28]. | |
| Replika | Replika is an artificial intelligence chatbot that constructs a virtual representation of users by analyzing their personality traits. Its ultimate goal is to help users cope with stress and improve their mental health. It is suitable for individuals who desire to engage in profound and contemplative conversations with a companion. It offers users a safe space for self-reflection and emotional assistance, fostering meaningful connections and understanding. Replika has emerged as a powerful tool for those seeking alternative methods to safeguard and improve their mental well-being [29]. | |
| Lifeline Ally | A friendly chatbot that focuses on preventing and supporting depression [30]. | |
| Humorous Psychological Companion | The Humorous Psychological Companion is a distinctive combination of a digital assistant and conversational partner, particularly created to aid individuals who are dealing with depression or related emotional conditions. It serves not just as an AI chatbot but also as a sympathetic, clever, and empathetic friend. The primary objective of this platform is aid, motivation, and a cheerful conversation to mitigate emotions of sorrow or isolation [31]. | |
| Elomia | Elomia is an AI-powered virtual therapist who has been trained in thousands of consultations, offering quality advice and support. Users can discuss their problems, ask questions, and obtain recommendations for mental health exercises. According to research, Elomia can help with anxiety, depression, low self-esteem, loneliness, relationship issues, burnout, and sleep problems. Whenever users need someone to talk to or seek guidance, Elomia listens, helps identify concerns, and suggest solutions, helping to regain confidence and acceptance of emotions [32]. | |
| Tess | Tess, on the other hand, is a mental health chatbot that provides treatment and support to people experiencing symptoms of depression and anxiety [33]. | |
| Meru Health | Meru Health is an artificial intelligence app that offers treatments for depression, anxiety, and stress. It provides personalized treatment regimens that meet the specific needs of each user, as well as online counseling and guidance [34]. | |
| APPLICATIONS | Ginger | Ginger is an on-demand mental health platform that provides counseling, support, and advice. It offers chat therapy, individualized care plans, and video sessions with licensed therapists [35]. |
| Headspace | Headspace, mindfulness and meditation software, makes individualized recommendations using artificial intelligence algorithms. It offers daily reminders, sleep sounds, and guided meditations to help users stick to their mental health goals [36]. | |
| Breathhh | Breathhh is a Chrome plugin that uses artificial intelligence to deliver mental health workouts tailored to an individual’s online activities and behavior. Through the surveillance and examination of user interactions, Breathhh is able to ascertain the optimal moments to introduce stress alleviation methods and tactics. This innovative method blends artificial cognitive intelligence with the tangible assistance of mental health, facilitating a smooth and effortless incorporation of self-care into users’ everyday schedules [37]. | |
| Sanvello | Sanvello is an app for mental well-being that tracks users’ moods and helps them understand their situation. It offers individualized mental health care. It also provides basic principles through the use of ambient noise. Through a community where users may engage in conversations with others facing similar problems, it also offers peer-to-peer help [15]. | |
| MindDoc | MindDoc provides a number of tools to help different facets of mental health, such as enhancing positive coping mechanisms, tracking mood, or monitoring general well-being. Her area of expertise is understanding mental health issues like sleeplessness, eating disorders, anxiety, and depression. It is simple to obtain helpful materials, exercises, and customized recommendations thanks to the user-friendly layout [38]. | |
| MoodMission | This program is designed to aid users in overcoming depression and anxiety by implementing evidence-based coping strategies. MoodMission facilitates personal growth and self-empowerment by suggesting tailored assignments that correspond to the emotions and experiences expressed by the user. By successfully completing missions, users improve their understanding of their mental health and discover new techniques to efficiently manage difficult tasks [10]. | |
| Ladder | Ladder is a health application that uses artificial intelligence to assist users in comprehending the correlation between their behaviors, emotions, and their general state of well-being. The software’s most compelling attribute lies in its origin and purpose, since it was developed only by and for individuals belonging to ethnic minority groups. This multifunctional device incorporates an exercise tracker to facilitate the development of beneficial routines, while its cognitive journal promotes emotional mindfulness and introspection [39]. | |
| Kintsugi | Kintsugi employs an innovative method in the field of mental health treatment by utilizing cutting-edge voice biomarkers in speech analysis to promptly detect, rank, and tackle mental health concerns as they arise. This API-centric platform readily interfaces with contact centers, telemedicine systems, and remote patient monitoring apps, enabling enhanced accessibility to appropriate treatment as and when required. Through the identification of small alterations in speech patterns and vocal indicators, it is capable of precisely evaluating an individual’s psychological condition and guiding them towards the most suitable resources and assistance [34]. | |
| Calm | Calm has established itself as a highly regarded application for mental well-being, particularly for individuals grappling with anxiety and despair. This application offers a range of powerful resources, including sleep tales, meditation, and other methods, to assist users in managing their mental health difficulties. Users have the opportunity to investigate a range of characteristics that cater to their own requirements in order to enhance their overall state of being [40]. | |
| Rootd | Rootd is a novel application that provides valuable assistance to individuals experiencing panic attacks and anxiety. The Rootr feature of the app offers individuals a convenient way to manage stress and find immediate relief. Furthermore, Rootd provides a range of strategies, including exercises, routines, and healthy diets, to effectively promote mental health improvement. By implementing these strategies and utilizing these resources, users can gradually improve their capacity to manage stress and achieve a more harmonious lifestyle [41]. | |
| MindShift | MindShift is a very helpful mental health tool that helps users properly control their anxiety by applying tried-and-true methods from cognitive behavioral therapy. In addition to encouraging the development of constructive thinking patterns and the adoption of preventative actions to successfully manage stress-related difficulties, the program gives users the chance to practice mindfulness and relaxation. With MindShift’s exquisitely simple interface and numerous adaptable options, users can effortlessly develop relaxing routines and enhance their mental health in general [42]. | |
| Happify | Happify provides customers with interactive activities and games specifically intended to effectively alleviate stress and counteract negative thinking. The software offers customized analytics derived from an individual’s mental health data, guaranteeing tailored assistance that caters to their distinct requirements. Users may quickly access these activities and games at any time, allowing for seamless integration into their everyday routine. Happify enhances happiness and mental well-being, thereby enhancing an individual’s entire quality of life through its creative method [43]. | |
| Deepwander | Deepwander is an AI-driven platform or tool created to enhance self-reflection and individual development. It involves participants in interactive discussions intended at investigating their internal realm and directing them towards beneficial transformation. Deepwander utilizes a range of psychological strategies, including cognitive behavioral strategies, motivational interviewing, narrative therapy, and guided visualization, to assist users in altering negative thinking patterns, discovering motivation, restructuring their life narratives, and clarifying their objectives. In general, Deepwander appears to offer a systematic method for introspection and individual growth [44]. | |
| Mindwell | Mindwell AI is a mental health app designed to help users overcome stress. It combines science-based tools, AI-powered counseling, and a virtual self-care partner named Joy [45]. | |
| Space of Mind | Space of Mind is an online trauma therapy and support group designed to provide affordable PTSD treatment. This AI-powered platform offers a therapeutic space facilitated by a therapist where individuals can participate in anonymous group sessions to address their traumatic experiences and work towards transformative therapy [46]. | |
| Moodpath | Moodpath is a mental health assessment tool that helps individuals understand their mental well-being through science-based questions and assessments. It identifies early signs of depression, anxiety, and burnout, offering personalized diagnoses and access to support resources. Users gain insights into their mental health, trends, and tips, along with tailored action plans for long-term management. In addition, Moodpath offers meditations, self-care tips, and personalized plans, making it a valuable resource for managing mental health [47]. | |
| MoodKit | MoodKit is a mobile app designed to help individuals manage their mood and create healthy emotional habits. Developed by psychologists, MoodKit offers a variety of tools and resources based on the principles of cognitive behavioral therapy, a widely recognized and effective form of treatment for mood disorders [10]. | |
| WEARABLE DEVICES | Samsung Health | Samsung Health is an all-encompassing health and wellness application created by Samsung Electronics. The purpose of this application is to assist users in tracking and controlling several elements of their well-being and physical condition, such as exercise, nutrition, sleep, stress levels, and more. The application provides functionalities such as step monitoring, exercise monitoring, calorie calculation, sleep monitoring, and tools for managing stress [48]. |
| MoodTools | MoodTools is a mobile app designed to provide support and resources for people experiencing depression. It offers various tools and features that help users effectively manage their mood and mental health [49]. | |
| BioBase | BioBase is a wearable device designed to monitor and analyze physiological signals in real time, providing information about a person’s stress levels, energy, and overall well-being. It uses biometric sensors to monitor parameters such as heart rate variability (HRV), skin conductivity, and temperature, which are indicators of stress and arousal levels [50]. | |
| Spire Health Tag | The Spire Health Tag is a portable health device that monitors various aspects of well-being throughout the day. Small labels attach to clothes and track activity levels, breathing patterns, stress levels, and sleep quality. Using advanced sensors, Spire Health Tag provides real-time feedback and information about daily habits and how they affect overall health [51]. | |
| Moodmetric | Moodmetric is a wearable device designed to monitor and manage stress levels in real time. It measures electrodermal activity (EDA), the electrical activity of the skin caused by the activation of sweat glands, to provide information about stress and emotional arousal [52]. | |
| Fisher Wallace Stimulator | The Fisher Wallace Stimulator is a small device designed particularly to aid in the treatment of anxiety, depression, and insomnia. The procedure is applying gentle electrical stimulation to the brain using small electrodes placed on the forehead. The aim of this stimulation is to regulate the levels of neurotransmitters, such as serotonin and cortisol, which are associated with mood and anxiety. Multiple users have claimed positive results, such as reduced anxiety and improved mood, however, individual outcomes may vary [53]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pavlopoulos, A.; Rachiotis, T.; Maglogiannis, I. An Overview of Tools and Technologies for Anxiety and Depression Management Using AI. Appl. Sci. 2024, 14, 9068. https://doi.org/10.3390/app14199068
Pavlopoulos A, Rachiotis T, Maglogiannis I. An Overview of Tools and Technologies for Anxiety and Depression Management Using AI. Applied Sciences. 2024; 14(19):9068. https://doi.org/10.3390/app14199068
Chicago/Turabian StylePavlopoulos, Adrianos, Theodoros Rachiotis, and Ilias Maglogiannis. 2024. "An Overview of Tools and Technologies for Anxiety and Depression Management Using AI" Applied Sciences 14, no. 19: 9068. https://doi.org/10.3390/app14199068







