Effects of Different Fields of View and Rotation Angles on Radiation Doses to Highly Radiosensitive Organs in Children Using Dental Cone Beam Computed Tomography
Abstract
:Featured Application
Abstract
1. Introduction
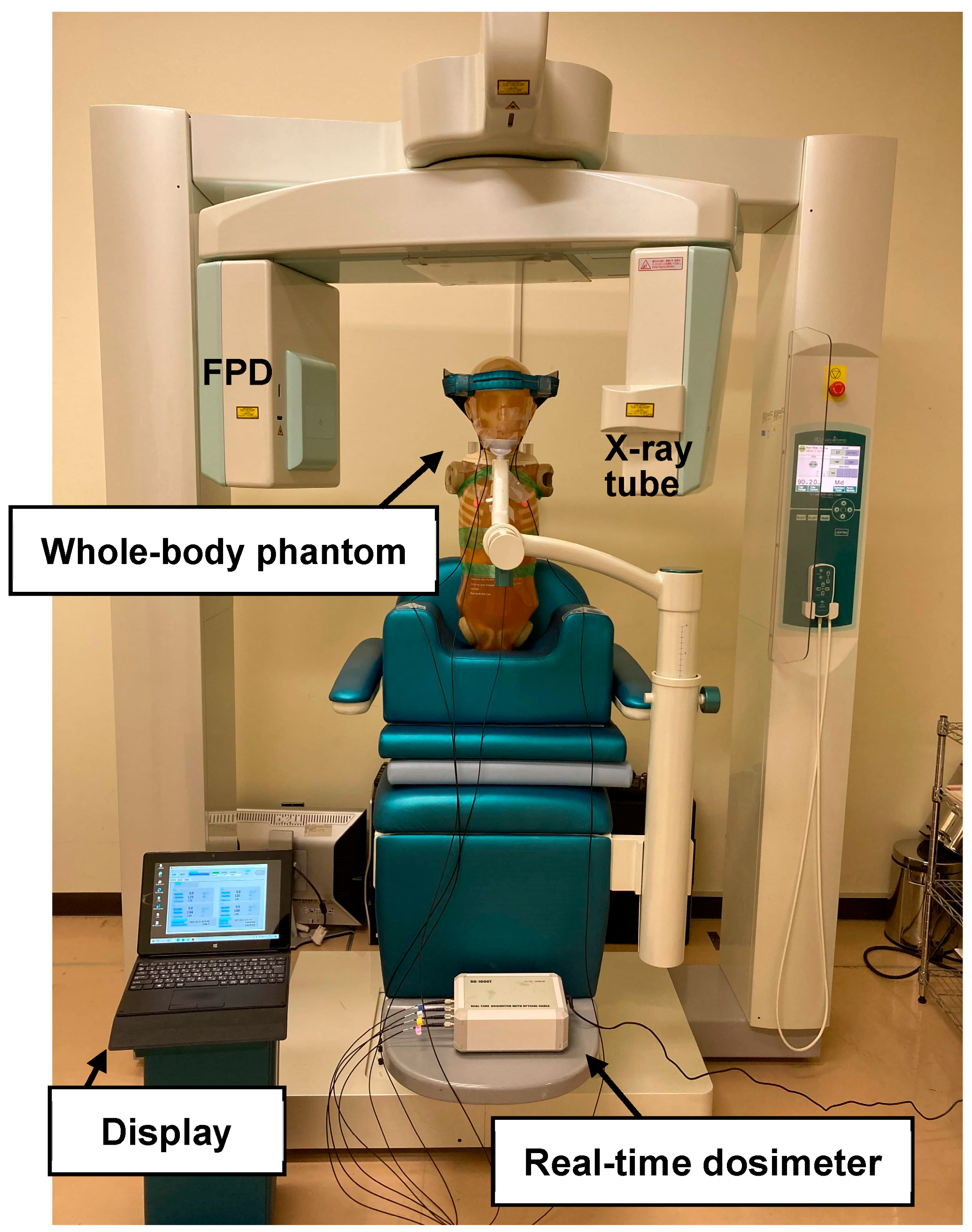
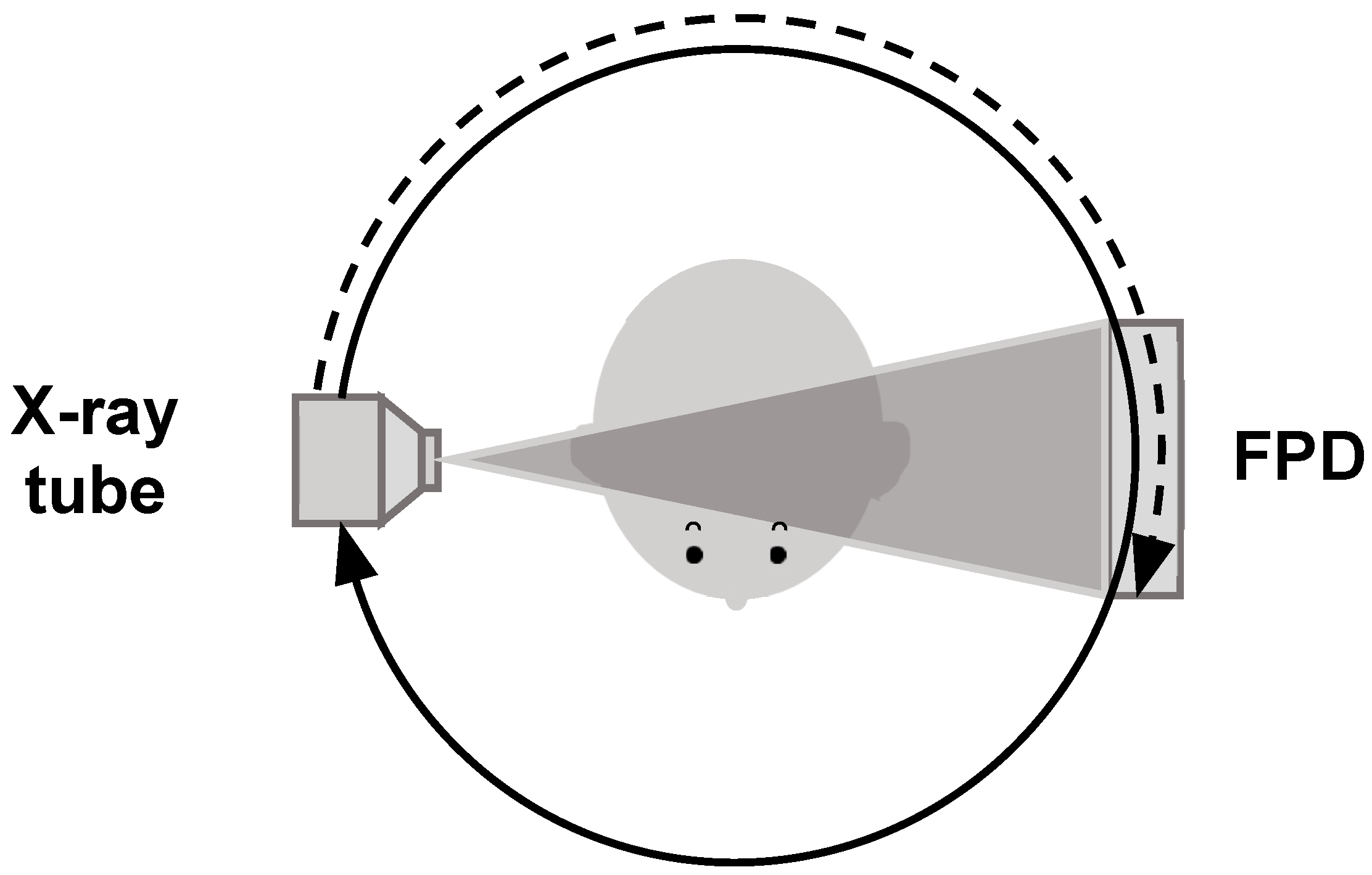
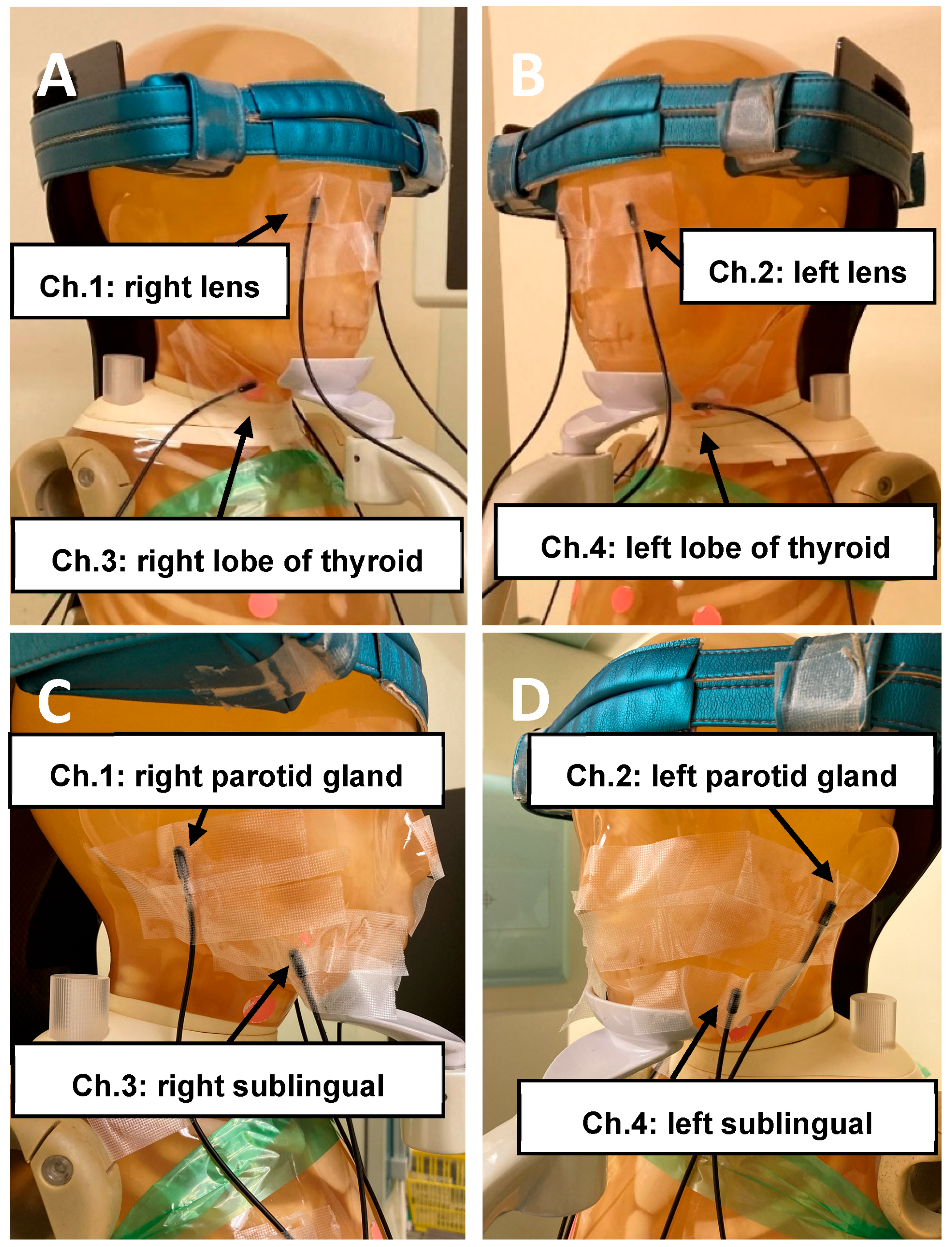
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- ICRP. Education and Training in Radiological Protection for Diagnostic and Interventional Procedures. ICRP Publication 113. Ann. ICRP 2009, 39, 7–68. [Google Scholar]
- Chida, K. What are useful methods to reduce occupational radiation exposure among radiological medical workers, especially for interventional radiology personnel? Radiol. Phys. Technol. 2022, 15, 101–115. [Google Scholar] [CrossRef] [PubMed]
- Chida, K.; Saito, H.; Otani, H.; Kohzuki, M.; Takahashi, S.; Yamada, S.; Shirato, K.; Zuguchi, M. Relationship between fluoroscopic time, dose—Area product, body weight, and maximum radiation skin dose in cardiac interventional procedures. Am. J. Roentgenol. 2006, 186, 774–778. [Google Scholar] [CrossRef] [PubMed]
- ICRP. Radiological Protection in Medicine. ICRP Publication 105. Ann. ICRP 2007, 37, 1–63. Available online: https://www.icrp.org/publication.asp?id=ICRP%20Publication%20105 (accessed on 26 August 2024).
- ICRP. ICRP Statement on Tissue Reactions/Early and Late Effects of Radiation in Normal Tissues and Organs—Threshold Doses for Tissue Reactions in a Radiation Protection Context. ICRP Publication 118. Ann. ICRP 2012, 41, 1–322. Available online: https://www.icrp.org/publication.asp?id=ICRP%20Publication%20118 (accessed on 26 August 2024). [CrossRef]
- International Commission on Radiological Protection (ICRP). Statement on Tissue Reactions. Available online: https://www.icrp.org/page.asp?id=123) (accessed on 26 August 2024).
- IAEA TECDOC No.1731 Implications for Occupational Radiation Protection of the New Dose Limit for the Lens of the Eye; TECDOC Series. 2013. Available online: https://wwwpub.iaea.org/mtcd/publications/pdf/te-1731_web.pdf (accessed on 26 August 2024).
- Chida, K.; Kaga, Y.; Haga, Y.; Kataoka, N.; Kumasaka, E.; Meguro, T.; Zuguchi, M. Occupational dose in interventional radiology procedures. Am. J. Roentgenol. 2013, 200, 138–141. [Google Scholar] [CrossRef]
- Haga, Y.; Chida, K.; Kaga, Y.; Sota, M.; Meguro, T.; Zuguchi, M. Occupational eye dose in interventional cardiology procedures. Sci. Rep. 2017, 7, 569. [Google Scholar] [CrossRef]
- Kato, M.; Chida, K.; Ishida, T.; Toyoshima, H.; Yoshida, Y.; Yoshioka, S.; Moroi, J.; Kinoshita, T. Occupational radiation exposure of the eye in neurovascular interventional physician. Radiat. Prot. Dosim. 2019, 185, 151–156. [Google Scholar] [CrossRef]
- Endo, M.; Haga, Y.; Sota, M.; Tanaka, A.; Otomo, K.; Murabayashi, Y.; Abe, M.; Kaga, Y.; Inaba, Y.; Suzuki, M.; et al. Evaluation of novel X-ray protective eyewear in reducing the eye dose to interventional radiology physicians. J. Radiat. Res. 2021, 62, 414–419. [Google Scholar] [CrossRef]
- Matsuzaki, S.; Moritake, T.; Morota, K.; Nagamoto, K.; Nakagami, K.; Kuriyama, T.; Kunugita, N. Development and assessment of an educational application for the proper use of ceiling-suspended radiation shielding screens in angiography rooms using augmented reality technology. Eur. J. Radiol. 2021, 143, 109925. [Google Scholar] [CrossRef]
- Fujibuchi, T. Radiation protection education using virtual reality for the visualisation of scattered distributions during radiological examinations. J. Radiol. Prot. 2021, 41, S317–S328. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, K.; Takei, Y.; Mori, H.; Kobayashi, I.; Noto, K.; Igarashi, T.; Suzuki, S.; Akahane, K. A multicenter study of radiation doses to the eye lenses of medical staff performing non-vascular imaging and interventional radiology procedures in Japan. Phys. Med. 2020, 74, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Lang, N.P.; Hill, R.W. Radiographs in periodontics. J. Clin. Periodontol. 1977, 4, 16–28. [Google Scholar] [CrossRef] [PubMed]
- Corbet, E.F.; Ho, D.K.L.; Lai, S.M.L. Radiographs in periodontal disease diagnosis and management. Aust. Dent. J. 2009, 54, S27–S43. [Google Scholar] [CrossRef] [PubMed]
- Erdelyi, R.A.; Duma, V.F.; Sinescu, C.; Dobre, G.M.; Bradu, A.; Podoleanu, A. Dental Diagnosis and Treatment Assessments: Between X-rays Radiography and Optical Coherence Tomography. Materials 2020, 13, 4825. [Google Scholar] [CrossRef]
- Preshaw, P.M. Detection and diagnosis of periodontal conditions amenable to prevention. BMC Oral Health 2015, 15, S5. [Google Scholar] [CrossRef]
- Otaka, Y.; Harata, Y.; Izawa, M.; Iwawaki, A.; Ishii, T.; Saka, H.; Kito, S. Reduction of operator exposure by rectangular collimation in portable intraoral radiography. Radiol. Phys. Technol. 2020, 13, 312–320. [Google Scholar] [CrossRef]
- Suomalainen, A.; Kiljunen, T.; Kaser, Y.; Peltola, J.; Kortesniemi, M. Dosimetry and image quality of four dental cone beam computed tomography scanners compared with multislice computed tomography scanners. Dentomaxillofac. Radiol. 2009, 38, 367–378. [Google Scholar] [CrossRef]
- Loubele, M.; Bogaerts, R.; Van Dijck, E.; Pauwels, R.; Vanheusden, S.; Suetens, P.; Marchal, G.; Sanderink, G.; Jacobs, R. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur. J. Radiol. 2009, 71, 461–468. [Google Scholar] [CrossRef]
- Li, Y.; Huang, B.; Cao, J.; Fang, T.; Liu, G.; Li, X.; Wu, J. Estimating radiation dose to major organs in dental x-ray examinations: A phantom study. Radiat. Prot. Dosim. 2020, 192, 328–334. [Google Scholar] [CrossRef]
- Shin, H.S.; Nam, K.C.; Park, H.; Choi, H.U.; Kim, H.Y.; Park, C.S. Effective doses from panoramic radiography and CBCT (cone beam CT) using dose area product (DAP) in dentistry. Dentomaxillofac. Radiol. 2014, 43, 20130439. [Google Scholar] [CrossRef]
- Deman, P.; Atwal, P.; Duzenli, C.; Thakur, Y.; Ford, N.L. Dose measurements for dental cone-beam CT: A comparison with MSCT and panoramic imaging. Phys. Med. Biol. 2014, 59, 3201–3222. [Google Scholar] [CrossRef] [PubMed]
- Smita, S.B.; Sara, A.; Basim, A.; Abdullah, A.; Abdullah, A.; Atul, B.; Ayoub, A. CBCT in Pediatric Dentistry: Awareness and Knowledge of Its Correct Use in Saudi Arabia. Appl. Sci. 2022, 12, 335. [Google Scholar] [CrossRef]
- David, A.; Iga, S.; Bartusik-Aebisher, D. Temporary Skeletal Anchorage Devices and Cone Beam Tomography in Orthodontics—Current Application and New Directions of Development. Appl. Sci. 2024, 14, 5028. [Google Scholar] [CrossRef]
- ICRP. Radiological Protection in Cone Beam Computed Tomography (CBCT). ICRP Publication 129. Ann. ICRP 2015, 44, 9–127. Available online: https://www.icrp.org/publication.asp?id=ICRP%20Publication%20129 (accessed on 26 August 2024).
- Hidalgo-Rivas, J.A.; Theodorakou, C.; Carmichael, F.; Murray, B.; Payne, M.; Horner, K. Use of cone beam CT in children and young people in three United Kingdom dental hospitals. Int. J. Paediatr. Dent. 2014, 24, 336–348. [Google Scholar] [CrossRef]
- Ebru, A.; Büşra, K.E. Reasons for requesting cone-beam computed tomography in children and adolescents: A 10-year. Biotechnol. Biotechnol. Equip. 2022, 36, 858–864. [Google Scholar] [CrossRef]
- Pearce, M.S.; Salotti, J.A.; Little, M.P.; McHugh, K.; Lee, C.; Kim, K.P.; Howe, N.L.; Ronckers, C.M.; Rajaraman, P.; Sir Craft, A.W.; et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: A retrospective cohort study. Lancet 2012, 380, 499–505. [Google Scholar] [CrossRef]
- Mathews, J.D.; Forsythe, A.V.; Brady, Z.; Butler, M.W.; Goergen, S.K.; Byrnes, G.B.; Giles, G.G.; Wallace, A.B.; Anderson, P.R.; Guiver, T.A.; et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: Data linkage study of 11 million Australians. BMJ 2013, 346, f2360. [Google Scholar] [CrossRef]
- Brenner, D.; Elliston, C.; Hall, E.; Berdon, W. Estimated risks of radiation-induced fatal cancer from pediatric CT. Am. J. Roentgenol. 2001, 176, 289–296. [Google Scholar] [CrossRef]
- Higuchi, K.; Fujimura, T. Radiation exposure dose outside the irradiation field due to differences in pediatric head computed tomography scanning methods. Radiol. Phys. Technol. 2021, 14, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Nemoto, M.; Chida, K. Reducing the Breast Cancer Risk and Radiation Dose of Radiography for Scoliosis in Children: A Phantom Study. Diagnostics 2020, 10, 753. [Google Scholar] [CrossRef] [PubMed]
- Chida, K.; Ohno, T.; Kakizaki, S.; Takegawa, M.; Yuuki, H.; Nakada, M.; Takahashi, S.; Zuguchi, M. Radiation dose to the pediatric cardiac catheterization and intervention patient. Am. J. Roentgenol. 2010, 195, 1175–1179. [Google Scholar] [CrossRef] [PubMed]
- ICRP. Radiological Protection in Paediatric Diagnostic and Interventional Radiology. ICRP Publication 121. Ann. ICRP 2013, 42, 1–63. Available online: https://www.icrp.org/publication.asp?id=ICRP%20Publication%20121 (accessed on 26 August 2024).
- Theodorakou, C.; Walker, A.; Horner, K.; Pauwels, R.; Bogaerts, R.; Jacobs, R. Estimation of paediatric organ and effective doses from dental cone beam CT using anthropomorphic phantoms. Br. J. Radiol. 2012, 85, 153–160. [Google Scholar] [CrossRef]
- Pauwels, R.; Cockmartin, L.; Ivanauskaité, D.; Urbonienė, A.; Gavala, S.; Donta, C.; Tsiklakis, K.; Jacobs, R.; Bosmans, H.; Bogaerts, R.; et al. Estimating cancer risk from dental cone-beam CT exposures based on skin dosimetry. Phys. Med. Biol. 2014, 59, 3877–3891. [Google Scholar] [CrossRef]
- Gallichan, N.; Albadri, S.; Dixon, C.; Jorgenson, K. Trends in CBCT current practice within three UK paediatric dental de-partments. Eur. Arch. Paediatr. Dent. 2020, 21, 537–542. [Google Scholar] [CrossRef]
- Yiğit, T.; Yüksel, H.T.; Evirgen, Ş.; Kaçmaz, I.; Türkmenoğlu, A. Evaluation of use of cone beam computed tomography in paediatric patients: A cross-sectional study. Int. J. Paediatr. Dent. 2023, 33, 468–476. [Google Scholar] [CrossRef]
- Rallan, M.; Rallan, N.S.; Goswami, M.; Rawat, K. Surgical management of multiple supernumerary teeth and an impacted maxillary permanent central incisor. BMJ Case Rep. 2013, 2013, bcr2013009995. [Google Scholar] [CrossRef]
- Sharma, A.; Singh, V.P. Supernumerary Teeth in Indian Children: A Survey of 300 Cases. Int. J. Dent. 2012, 2012, 745265. [Google Scholar] [CrossRef]
- Rajab, L.D.; Hamdan, M.A. Supernumerary Teeth in Indian Children: A Survey of 300 Cases. Int. J. Paediatr. Dent. 2002, 12, 244–254. [Google Scholar] [CrossRef] [PubMed]
- SEDENTEXCT Radiation Protection no 172. Cone Beam CT for Dental and Maxillofacial Radiology. Evidence-Based Guidelines. Luxembourg: European Commission. Available online: https://www.orthodont-cz.cz/data/files/sedentexct(1).pdf (accessed on 7 April 2023).
- Pauwels, R.; Zhang, G.; Theodorakou, C.; Walker, A.; Bosmans, H.; Jacobs, R.; Bogaerts, R.; Horner, K. Effective radiation dose and eye lens dose in dental cone beam CT: Effect of field of view and angle of rotation. Br. J. Radiol. 2014, 87, 20130654. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, E.; Wolf, U.; Heinicke, F.; Silva, M.A. Dosimetry of the cone beam computed tomography Veraviewepocs 3D compared with the 3D Accuitomo in different fields of view. Dentomaxillofac Radiol. 2008, 37, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Grüning, M.; Koivisto, J.; Mah, J.; Bumann, A. Impact of thyroid gland shielding on radiation doses in dental cone beam computed tomography with small and medium fields of view. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2022, 134, 245–253. [Google Scholar] [CrossRef]
- Hajem, S.; Brogårdh-Roth, S.; Nilsson, M.; Hellén-Halme, K. CBCT of Swedish children and adolescents at an oral and maxillofacial radiology department. A survey of requests and indications. Acta Odontol. Scand. 2020, 78, 38–44. [Google Scholar] [CrossRef]
- Ito, M.; Onodera, S.; Kojima, I.; Chida, K. Effect of different rotation angle on image quality in dental CBCT: Physical evaluation. Medical Imaging and Information Sciences (MII) 2022, 39, 38–42. (In Japanese) [Google Scholar] [CrossRef]
- Ito, M.; Chida, K.; Onodera, S.; Kojima, I.; Iikubo, M.; Kato, T.; Fujisawa, M.; Zuguchi, M. Evaluation of radiation dose and image quality for dental cone-beam computed tomography in pediatric patients. J. Radiol. Prot. 2023, 43, 031518. [Google Scholar] [CrossRef]
- UK Guidance National Diagnostic Reference Levels (NDRLs) from 13 October 2022, Updated 24 November 2022. Available online: www.gov.uk/government/publications/diagnostic-radiology-national-diagnostic-reference-levels-ndrls/ndrl) (accessed on 28 March 2023).
- Seehra, J.; Yaqoob, O.; Patel, S.; O’Neill, J.; Bryant, C.; Noar, J.; Morris, D.; Cobourne, M.T. National clinical guidelines for the management of unerupted maxillary incisors in children. Br. Dent. J. 2018, 224, 779–785. [Google Scholar] [CrossRef]
- Suresh, K.S.; Uma, H.L.; Nagarathna, J.; Kumar, P. Management of Ectopically Erupting Maxillary Incisors: A Case Series. Int. J. Clin. Pediatr. Dent. 2015, 8, 227–233. [Google Scholar] [CrossRef]
- Anthonappa, R.P.; Omer, R.S.; King, N.M. Characteristics of 283 supernumerary teeth in southern Chinese children. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 105, e48–e54. [Google Scholar] [CrossRef]
- Seehra, J.; DiBiase, A.T.; Patel, S.; Stephens, R.; Littlewood, S.J.; Spencer, R.J.; Frawley, T.; Benson, P.E.; Ireland, A.J.; Parvizi, F.; et al. Study protocol for the management of impacted maxillary central incisors: A multicentre randomised clinical trial: The iMAC Trial. Trials 2022, 23, 787. [Google Scholar] [CrossRef] [PubMed]
- Noda, T.; Takagi, M.; Hayashi-Sakai, S.; Taguchi, Y. Eruption disturbances in Japanese children and adolescents. Pediatr. Dent. J. 2006, 16, 50–56. [Google Scholar] [CrossRef]
- Einy, S.; Michaeli-Geller, G.; Aizenbud, D. Eruption Treatment of Impacted Teeth Following Surgical Obstruction Removal. Appl. Sci. 2022, 12, 449. [Google Scholar] [CrossRef]
- Nagaraj, K.; Upadhyay, M.; Yadav, S. Impacted maxillary central incisor, canine, and second molar with 2 supernumerary teeth and an odontoma. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 390–399. [Google Scholar] [CrossRef] [PubMed]
- Ericson, S.; Kurol, J. Longitudinal study and analysis of clinical supervision of maxillary canine eruption. Community Dent. Oral. Epidemiol. 1986, 14, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.A.; Zaki, H. Root Resorption of Adjacent Teeth Associated with Maxillary Canine Impaction in the Saudi Arabian Population: A Cross-Sectional Cone-Beam Computed Tomography Study. Appl. Sci. 2022, 12, 334. [Google Scholar] [CrossRef]
- Nikhil, P.; Seema, D.B.; Swara, H.S.; Bhavna, H.D. Supplementary Tooth: To Extract or Observe? Evidence Based Practice with the Literature Review. Adv. Hum. Biol. 2015, 5, 92–101. [Google Scholar] [CrossRef]
- Inaba, Y.; Nakamura, M.; Zuguchi, M.; Chida, K. Development of novel real-time radiation systems using 4-channel sensors. Sensors 2020, 20, 2741. [Google Scholar] [CrossRef]
- Kato, M.; Chida, K.; Nakamura, M.; Toyoshima, H.; Terata, K.; Abe, Y. New real-time patient radiation dosimeter for use in radiofrequency catheter ablation. J. Radiat. Res. 2019, 60, 215–220. [Google Scholar] [CrossRef]
- Nakamura, M.; Chida, K.; Zuguchi, M. Red emission phosphor for real-time skin dosimeter for fluoroscopy and interventional radiology. Med. Phys. 2014, 41, 101913. [Google Scholar] [CrossRef]
- Fontana, R.C.; Pasqual, E.; Miller, D.L.; Simon, S.L.; Cardis, E.; Thierry-Chef, I. Trends in Estimated Thyroid, Salivary Gland, Brain, and Eye Lens Doses From Intraoral Dental Radiography Over Seven Decades (1940 TO 2009). Health Phys. 2020, 118, 136–148. [Google Scholar] [CrossRef] [PubMed]
- International Commission on Radiation Units and Measurements. Tissue Substitutes in Radiation Dosimetry and Measurement; ICRU: Bethesda, MD, USA, 1989. [Google Scholar]
- Vogiatzi, T.; Menz, R.; Verna, C.; Bornstein, M.M.; Dagassan-Berndt, D. Effect of field of view (FOV) positioning and shielding on radiation dose in paediatric CBCT. Dentomaxillofac. Radiol. 2022, 51, 20210316. [Google Scholar] [CrossRef] [PubMed]


| Parameter | Value |
|---|---|
| Tube voltage (kV) | 90 |
| Tube current (mA) | 2, 3 |
| Field of view (cm) | 4 × 4, 6 × 6 |
| Rotation angle (°) | 360, 180 |
| FOV (cm) | 4 × 4 | 6 × 6 | ||||||
|---|---|---|---|---|---|---|---|---|
| Rotation Angle (°) | 360 | 180 | 360 | 180 | ||||
| Tube Current (mA) | 2 | 3 | 2 | 3 | 2 | 3 | 2 | 3 |
| Right lens | 0.08 ± 0.00 | 0.12 ± 0.00 | 0.03 ± 0.00 | 0.06 ± 0.00 | 0.20 ± 0.00 | 0.30 ± 4.96 × 10−3 | 0.07 ± 0.00 | 0.10 ± 0.00 |
| Left lens | 0.14 ± 0.00 | 0.19 ± 0.00 | 0.07 ± 0.00 | 0.09 ± 0.00 | 0.34 ± 4.80 × 10−3 | 0.46 ± 0.00 | 0.13 ± 4.80 × 10−3 | 0.18 ± 4.80 × 10−3 |
| Right lobe of thyroid | 0.22 ± 0.00 | 0.26 ± 0.00 | 0.12 ± 0.00 | 0.18 ± 0.00 | 0.61 ± 0.00 | 0.92 ± 0.00 | 0.30 ± 0.00 | 0.46 ± 0.00 |
| Left lobe of thyroid | 0.21 ± 0.00 | 0.32 ± 0.00 | 0.10 ± 0.00 | 0.14 ± 0.00 | 0.52 ± 9.04 × 10−3 | 0.78 ± 0.00 | 0.25 ± 0.00 | 0.37 ± 0.00 |
| Right parotid gland | 0.58 ± 4.96 × 10−3 | 0.84 ± 0.00 | 0.49 ± 0.00 | 0.75 ± 0.00 | 0.89 ± 0.00 | 1.31 ± 0.00 | 0.77 ± 4.96 × 10−3 | 1.13 ± 0.00 |
| Left parotid gland | 0.91 ± 4.80 × 10−3 | 1.30 ± 0.00 | 0.80 ± 0.00 | 1.16 ± 4.80 × 10−3 | 1.36 ± 4.80 × 10−3 | 1.95 ± 0.00 | 1.19 ± 0.00 | 1.72 ± 4.80 × 10−3 |
| Right sublingual gland | 0.22 ± 0.00 | 0.35 ± 4.94 × 10−3 | 0.13 ± 0.00 | 0.19 ± 4.94 × 10−3 | 1.58 ± 4.94 × 10−3 | 2.30 ± 0.00 | 1.14 ± 4.94 × 10−3 | 1.68 ± 4.94 × 10−3 |
| Left sublingual gland | 0.16 ± 0.00 | 0.27 ± 0.00 | 0.11 ± 0.00 | 0.17 ± 4.52 × 10−3 | 1.52 ± 4.52 × 10−3 | 2.26 ± 0.00 | 1.14 ± 0.00 | 1.70 ± 0.00 |
| FOV (cm) | 4 × 4 | 6 × 6 | ||||||
|---|---|---|---|---|---|---|---|---|
| Rotation Angle (°) | 360 | 180 | 360 | 180 | ||||
| Tube Current (mA) | 2 | 3 | 2 | 3 | 2 | 3 | 2 | 3 |
| Right lens | 0.10 ± 4.96 × 10−3 | 0.17 ± 0.00 | 0.03 ± 0.00 | 0.06 ± 4.96 × 10−3 | 0.25 ± 0.00 | 0.34 ± 0.00 | 0.08 ± 0.00 | 0.11 ± 0.00 |
| Left lens | 0.13 ± 0.00 | 0.19 ± 0.00 | 0.05 ± 4.80 × 10−3 | 0.08 ± 0.00 | 0.29 ± 4.80 × 10−3 | 0.39 ± 0.00 | 0.12 ± 4.80 × 10−3 | 0.16 ± 4.80 × 10−3 |
| Right lobe of thyroid | 0.17 ± 9.87 × 10−3 | 0.30 ± 0.00 | 0.07 ± 0.00 | 0.14 ± 0.00 | 0.53 ± 0.00 | 0.78 ± 0.00 | 0.24 ± 4.94 × 10−3 | 0.38 ± 4.94 × 10−3 |
| Left lobe of thyroid | 0.17 ± 1.20 × 10−3 | 0.29 ± 0.00 | 0.08 ± 4.52 × 10−3 | 0.14 ± 0.00 | 0.49 ± 0.00 | 0.74 ± 0.00 | 0.24 ± 0.00 | 0.37 ± 0.00 |
| Right parotid gland | 0.66 ± 4.96 × 10−3 | 0.98 ± 4.96 × 10−3 | 0.57 ± 4.96 × 10−3 | 0.84 ± 4.96 × 10−3 | 1.02 ± 0.00 | 1.50 ± 0.00 | 0.83 ± 4.96 × 10−3 | 1.23 ± 0.00 |
| Left parotid gland | 0.89 ± 4.80 × 10−3 | 1.28 ± 4.80 × 10−3 | 0.80 ± 4.80 × 10−3 | 1.16 ± 0.00 | 1.33 ± 4.80 × 10−3 | 1.91 ± 0.00 | 1.17 ± 4.80 × 10−3 | 1.70 ± 4.80 × 10−3 |
| Right sublingual gland | 0.25 ± 0.00 | 0.41 ± 0.00 | 0.16 ± 0.00 | 0.25 ± 0.00 | 1.94 ± 4.94 × 10−3 | 2.84 ± 0.00 | 1.31 ± 0.00 | 1.91 ± 4.94 × 10−3 |
| Left sublingual gland | 0.18 ± 0.00 | 0.27 ± 0.00 | 0.12 ± 0.00 | 0.19 ± 4.52 × 10−3 | 1.39 ± 4.52 × 10−3 | 2.02 ± 0.00 | 1.10 ± 0.00 | 1.62 ± 4.52 × 10−3 |
| This Study | Pauwels et al. [45] | |||||||
|---|---|---|---|---|---|---|---|---|
| Position | Maxillary canine | Maxillary median | Maxillary canine | Maxillary median | ||||
| Tube voltage (kV) | 90 | 90 | 90 | 90 | ||||
| Tube current (mA) | 3 | 3 | 5 | 5 | ||||
| FOV (cm) | 4 × 4 | 6 × 6 | 4 × 4 | 6 × 6 | ||||
| Rotation angle (°) | 360 | 180 | 360 | 180 | 360 | 180 | 360 | 180 |
| Exposure time (s) | 17.5 | 9.0 | 17.5 | 9.0 | 17.5 | 9.0 | 17.5 | 9.0 |
| Lens | 38.3 ± 0.00 | 14.1 ± 0.50 | 72.7 ± 0.49 | 26.1 ± 0.48 | 174 | 95 | 608 | 288 |
| Thyroid | 51.1 ± 0.49 | 25.0 ± 0.00 | 147.4 ± 0.95 | 72.4 ± 0.00 | 108 | 50 | 175 | 88 |
| Parotid gland | 225.4 ± 0.98 | 199.5 ± 0.50 | 326.3 ± 0.50 | 284.3 ± 0.48 | - | - | - | - |
| Sublingual gland | 67.7 ± 0.00 | 43.7 ± 0.45 | 456.7 ± 2.26 | 338.0 ± 0.00 | - | - | - | - |
| Salivary gland | - | - | - | - | 845 | 573 | 2192 | 1583 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ito, M.; Kojima, I.; Iikubo, M.; Onodera, S.; Sai, M.; Fujisawa, M.; Kato, T.; Nakamura, M.; Zuguchi, M.; Chida, K. Effects of Different Fields of View and Rotation Angles on Radiation Doses to Highly Radiosensitive Organs in Children Using Dental Cone Beam Computed Tomography. Appl. Sci. 2024, 14, 9154. https://doi.org/10.3390/app14199154
Ito M, Kojima I, Iikubo M, Onodera S, Sai M, Fujisawa M, Kato T, Nakamura M, Zuguchi M, Chida K. Effects of Different Fields of View and Rotation Angles on Radiation Doses to Highly Radiosensitive Organs in Children Using Dental Cone Beam Computed Tomography. Applied Sciences. 2024; 14(19):9154. https://doi.org/10.3390/app14199154
Chicago/Turabian StyleIto, Misaki, Ikuho Kojima, Masahiro Iikubo, Shu Onodera, Masahiro Sai, Masaki Fujisawa, Toshiki Kato, Masaaki Nakamura, Masayuki Zuguchi, and Koichi Chida. 2024. "Effects of Different Fields of View and Rotation Angles on Radiation Doses to Highly Radiosensitive Organs in Children Using Dental Cone Beam Computed Tomography" Applied Sciences 14, no. 19: 9154. https://doi.org/10.3390/app14199154






