Designing Hand Orthoses: Advances and Challenges in Material Extrusion
Abstract
:1. Introduction
2. Method
2.1. Requirement Collection
2.2. Narrative Review
- The paper is accessible to the authors and is a scientific article written in English.
- The described device is a hand orthosis produced via MEX printing.
- The device is intended for medical purposes.
- The study presents the mechanical aspects of the designed hand orthosis.
- The study includes a figure illustrating the designed device.
- The study provides sufficient information on the design choices.
3. Hand Orthosis Development
3.1. Orthosis Manufacturing
- Which anatomical structures are impacted, and how will the splint address them?
- What therapeutic objectives should the splint achieve?
- What is the recommended duration and schedule for wearing the splint?
- When and under what conditions should the splint be adjusted?
- What key factors must be considered during the fitting process to ensure optimal function and comfort?
- What is the correct positioning of the splint to achieve the desired therapeutic outcome?
- Are there any contraindications or potential risks associated with this splint that need to be addressed?
- What monitoring and maintenance protocols are required for the splint, including who is responsible and the frequency of checks?
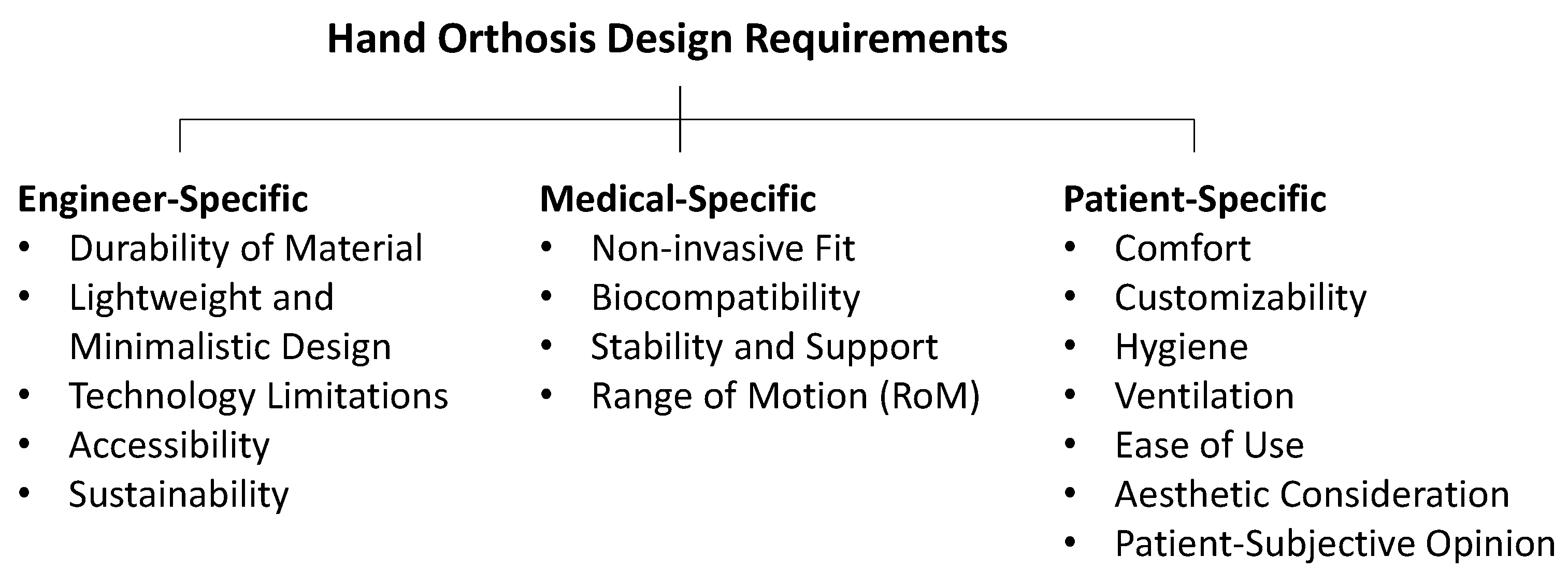
3.2. Design Requirements
3.2.1. Engineer-Specific
3.2.2. Medical-Specific
3.2.3. Patient-Specific
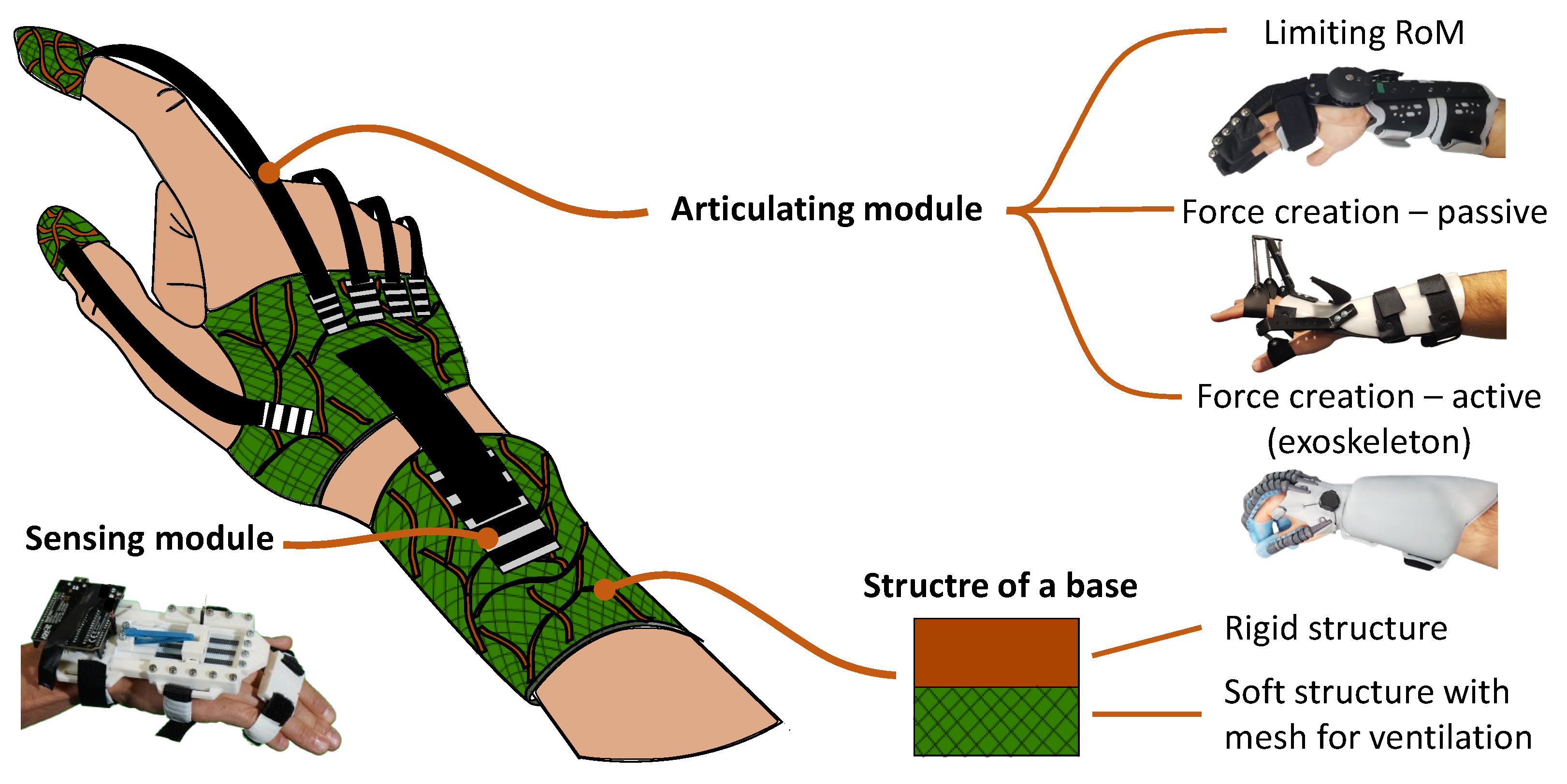
3.3. Diverse Designs of Hand Orthoses
4. Current Approaches in 3D-Printed Hand Orthotics
4.1. Static Orthoses
4.2. Dynamic Orthoses
4.3. Introduction of Modular Design
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ADL | Activities of Daily Living |
| AM | Additive Manufacturing |
| DfAM | Design for Additive Manufacturing |
| FFF | Fused Filament Fabrication |
| MCP | Metacarpophalangeal |
| MEX | Material Extrusion |
| MJF | Multi Jet Fusion |
| PIP | Proximal Interphalangeal |
| RoM | Range of Motion |
| SLA | Stereolithography |
| SLS | Selective Laser Sintering |
References
- Plessis, T.D.; Djouani, K.; Oosthuizen, C. A Review of Active Hand Exoskeletons for Rehabilitation and Assistance. Robotics 2021, 10, 40. [Google Scholar] [CrossRef]
- Choo, Y.J.; Boudier-Revéret, M.; Chang, M.C. 3D printing technology applied to orthosis manufacturing: Narrative review. Ann. Palliat. Med. 2020, 9, 4262–4270. [Google Scholar] [CrossRef] [PubMed]
- Portnova, A.A.; Mukherjee, G.; Peters, K.M.; Yamane, A.; Steele, K.M. Design of a 3D-printed, open-source wrist-driven orthosis for individuals with spinal cord injury. PLoS ONE 2018, 13, e0193106. [Google Scholar] [CrossRef] [PubMed]
- Tagliaferri, V.; Trovalusci, F.; Guarino, S.; Venettacci, S. Environmental and Economic Analysis of FDM, SLS and MJF Additive Manufacturing Technologies. Materials 2019, 12, 4161. [Google Scholar] [CrossRef] [PubMed]
- Toth, L.; Schiffer, A.; Nyitrai, M.; Pentek, A.; Told, R.; Maroti, P. Developing an anti-spastic orthosis for daily home-use of stroke patients using smart memory alloys and 3D printing technologies. Mater. Des. 2020, 195, 109029. [Google Scholar] [CrossRef]
- Oud, T.A.M.; Lazzari, E.; Gijsbers, H.J.H.; Gobbo, M.; Nollet, F.; Brehm, M.A. Effectiveness of 3D-printed orthoses for traumatic and chronic hand conditions: A scoping review. PLoS ONE 2021, 16, e0260271. [Google Scholar] [CrossRef]
- Binedell, T.; Subburaj, K. Design for Additive Manufacturing of Prosthetic and Orthotic Devices. In Revolutions in Product Design for Healthcare. Design Science and Innovation; Subburaj, K., Sandhu, K., Ćuković, S., Eds.; Springer: Singapore, 2022; pp. 75–99. [Google Scholar] [CrossRef]
- Hassan, B.B.; Wong, M.S. Contemporary and Future Development of 3D Printing Technology in the Field of Assistive Technology, Orthotics and Prosthetics. Can. Prosthetics Orthot. J. 2023, 6, 42225. [Google Scholar] [CrossRef]
- Borgianni, Y.; Pradel, P.; Berni, A.; Obi, M.; Bibb, R. An investigation into the current state of education in Design for Additive Manufacturing. J. Eng. Des. 2022, 33, 461–490. [Google Scholar] [CrossRef]
- Koesling, C. Schienenbehandlung. Schienenarten. In Ergotherapie in Orthopädie, Traumatologie und Rheumatologie, 2nd ed.; Koesling, C., Herzka, T.B., Eds.; Georg Thieme Verlag: Stuttgart, Germany, 2018; pp. 116–122. [Google Scholar]
- Bohli, E. Schienenbehandlung in der Handtherapie, 1st ed.; Huber: Bern, Switzerland, 2012; pp. 43–44. [Google Scholar]
- Ziem, I. Ergotherapie in der Handrehabilitation, 1st ed.; Huber: Bern, Switzerland, 2008; p. 25. [Google Scholar]
- Jacobs, M.A.; Coverdale, J. Concepts of Orthotic Fundamentals. Function of Orthoses and Objectives for Intervention. In Orthotic Intervention for the Hand and Upper Extremity. Splinting Principles and Process, 2nd ed.; Jacobs, M.A., Austin, N.M., Eds.; Wolters Kluwer Health/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2014; pp. 2–25. [Google Scholar]
- Knaus, W. Schienen in der Handtherapie. Statische-, Dynamische- und Übungsschienen; Verlag Modernes Lernen: Dortmund, Germany, 2011; p. 21. [Google Scholar]
- Coppard, B.M. Foundations of Orthotics. In Introduction to Orthotics. A Clinical Reasoning & Problem-Solving Approach, 5th ed.; Coppard, B.M., Lohman, H.L., Eds.; Elsevier: St. Louis, MO, USA, 2020; pp. 1–12. [Google Scholar]
- Schröder, B. Kurze Schienenkunde. Geschichte. In Handtherapie, 2nd ed.; Schröder, B., Bade, H., Eds.; Thieme: Stuttgart, Germany, 2008; pp. 38–49. [Google Scholar]
- Wilton, J. Hand Splinting Orthotic Intervention—Principles of Design and Fabrication. In Hand Splinting Orthotic Intervention, 2nd ed.; Vivid Publishing: Fremantle, Australia, 2013; pp. 33–47. [Google Scholar]
- Austin, N.M. Equipment and Materials. In Orthotic Intervention for the Hand and Upper Extremity. Splinting Principles and Process, 2nd ed.; Jacobs, M.A., Austin, N.M., Eds.; Wolters Kluwer Health/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2014; pp. 84–106. [Google Scholar]
- Fess, E.E.; McCollum, M. The influence of splinting on healing tissues. J. Hand Ther. 1998, 11, 157–161. [Google Scholar] [CrossRef]
- Marotta, N.; Demeco, A.; Marinaro, C.; Moggio, L.; Pino, I.; Barletta, M.; Petraroli, A.; Ammendolia, A. Comparative Effectiveness of Orthoses for Thumb Osteoarthritis: A Systematic Review and Network Meta-analysis. Arch. Phys. Med. Rehabil. 2021, 102, 502–509. [Google Scholar] [CrossRef]
- Fess, E.; Gettle, K.; Philips, C.; Janson, R. Hand and Upper Extremity Splinting Principles & Methods; Mosby Elsevier: St. Louis, MO, USA, 2005. [Google Scholar]
- Hirth, M.J.; Howell, J.W.; O’Brien, L. Relative motion orthoses in the management of various hand conditions: A scoping review. J. Hand Ther. 2016, 29, 405–432. [Google Scholar] [CrossRef] [PubMed]
- Salibian, A.A.; Bruckman, K.C.; Bekisz, J.M.; Mirrer, J.; Thanik, V.D.; Hacquebord, J.H. Management of Unstable Distal Radius Fractures: A Survey of Hand Surgeons. J. Wrist Surg. 2019, 8, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Kogler, G.F.; Bridges, M.; Hilliard, J.E.; Chui, K.K. Materials and Technology. In Orthotics and Prosthetics in Rehabilitation, 4th ed.; Chui, K.K., Jorge, M.M., Yen, S.C., Lusardi, M.M., Eds.; Elsevier: St. Louis, MO, USA, 2020; pp. 144–163. [Google Scholar] [CrossRef]
- der Windt, J.W.V.; Akkerman, W.; Hofstra, M.; Meussen, P. Reduced pain and improved daily activities for individuals with hand osteoarthritis using a silicone wrist hand orthosis. J. Hand Ther. 2023, 36, 669–677. [Google Scholar] [CrossRef] [PubMed]
- Gerrard, J.M.; Bonanno, D.R.; Whittaker, G.A.; Landorf, K.B. Effect of different orthotic materials on plantar pressures: A systematic review. J. Foot Ankle Res. 2020, 13, 35. [Google Scholar] [CrossRef] [PubMed]
- Paracuollo, M.; Coscione, A.V.; Coppola, A.; Pellegrino, G.; Pellegrino, A. Clinical and Radiographic Outcomes of Distal Radius Fracture Treatment with Carbon-Fiber-Reinforced-Polymer Volar Plates (CFR-PEEK): Analysis of 40 Cases. Lo Scalpello J. 2022, 36, 185–190. [Google Scholar] [CrossRef]
- Austin, N.M. Fabrication Process. In Orthotic Intervention for the Hand and Upper Extremity. Splinting Principles and Process, 2nd ed.; Jacobs, M.A., Austin, N.M., Eds.; Wolters Kluwer Health/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2014; pp. 107–124. [Google Scholar]
- Kelly, S.; Paterson, A.; Bibb, R. A Review of Wrist Splint Designs for Additive Manufacture. In Proceedings of the 2015 14th Rapid Design, Prototyping and Manufacture Conference (RDPM 14), Loughborough, UK, 15–16 December 2015. [Google Scholar]
- Boser, Q.A.; Dawson, M.R.; Schofield, J.S.; Dziwenko, G.Y.; Hebert, J.S. Defining the design requirements for an assistive powered hand exoskeleton: A pilot explorative interview study and case series. Prosthetics Orthot. Int. 2021, 45, 161–169. [Google Scholar] [CrossRef]
- Farzad, M.; Naqui, Z.; MacDermid, J.; Cuypers, S. Sustainable practices in hand therapy: A global perspective. J. Hand Surg. (Eur. Vol.) 2024, 49, 1051–1056. [Google Scholar] [CrossRef]
- Kumar, A.; Chhabra, D. Adopting additive manufacturing as a cleaner fabrication framework for topologically optimized orthotic devices: Implications over sustainable rehabilitation. Clean. Eng. Technol. 2022, 10, 100559. [Google Scholar] [CrossRef]
- HKK-Bionics. Exomotion® Hand One GEN2. Available online: https://hkk-bionics.de/en/aids/ (accessed on 7 October 2024).
- Faller, L.M.; Deniz Varsavas, S.; Ali, A.M.J.; Michalec, P.; Lakshmi Gidugu, S.; Spintzyk, S.; Riemelmoser, F.O. iLEAD—Intelligent lightweight functional and hybrid 3D-printing for medical assistive devices: Current status focusing on the multi-material aspect. Mater. Today Proc. 2022, 70, 512–518. [Google Scholar] [CrossRef]
- Orfit. Wrist Immobilization Splint—With Slightly or Non-Sticky Materials. Available online: https://www.orfit.com/physical-rehabilitation/information/guides/wrist-immobilization-splint-with-slightly-or-non-sticky-materials (accessed on 7 October 2024).
- Sporlastic. MANU-CAST® ORGANIC P Wrist Brace with Thumb Fixation for Immobilization. Available online: https://www.sporlastic.de/en/product/item/manu-cast-organic-p/ (accessed on 7 October 2024).
- Manometric. Swanneck Ring. Available online: https://www.manometric.nl/en/products/ (accessed on 7 October 2024).
- Kremser. O-O-FH2 in Katalog 3D-Orthesen—Digitale Orthopädietechnik. Available online: https://ib-kremser.de/servicefertigung/katalog-3d-orthesen/ (accessed on 7 October 2024).
- Albrecht. CDS® ManuSan. Available online: https://albrechtgmbh.com/produkt/cds-manusan/ (accessed on 7 October 2024).
- Ortholand. Dinamic Hand—Wrist Splint ML-0617. Available online: https://www.ortholand.com.tr/en/ud/dinamik-el-bilek-splinti.html (accessed on 7 October 2024).
- Orfit. GVV Swing Traction Splint. Available online: https://www.orfit.com/physical-rehabilitation/information/guides/gvv-swing-traction-splint (accessed on 7 October 2024).
- Bioservo. Carbonhand®. Available online: https://www.bioservo.com/products/carbonhand (accessed on 7 October 2024).
- Sala, F.; Carminati, M.; D’Urso, G.; Giardini, C. A feasibility analysis of a 3D customized upper limb orthosis. Procedia CIRP 2022, 110, 207–212. [Google Scholar] [CrossRef]
- Rosen, D.; Kim, S. Design and Manufacturing Implications of Additive Manufacturing. J. Mater. Eng. Perform. 2021, 30, 6426–6438. [Google Scholar] [CrossRef]
- Vaneker, T.; Bernard, A.; Moroni, G.; Gibson, I.; Zhang, Y. Design for additive manufacturing: Framework and methodology. CIRP Ann. 2020, 69, 578–599. [Google Scholar] [CrossRef]
- Górski, F.; Wichniarek, R.; Kuczko, W.; Żukowska, M.; Lulkiewicz, M.; Zawadzki, P. Experimental studies on 3D printing of automatically designed customized wrist-hand orthoses. Materials 2020, 13, 4091. [Google Scholar] [CrossRef] [PubMed]
- Łukaszewski, K.; Raj, R.; Karwasz, A. Mechanical Evaluation of PET-G 3D-Printed Wrist-Hand Orthosis: An Integrated Experimental and Numerical Approach. Materials 2023, 16, 6132. [Google Scholar] [CrossRef] [PubMed]
- Msallem, B.; Sharma, N.; Cao, S.; Halbeisen, F.S.; Zeilhofer, H.F.; Thieringer, F.M. Evaluation of the dimensional accuracy of 3D-printed anatomical mandibular models using FFF, SLA, SLS, MJ, and BJ printing technology. J. Clin. Med. 2020, 9, 817. [Google Scholar] [CrossRef]
- Portnoy, S.; Barmin, N.; Elimelech, M.; Assaly, B.; Oren, S.; Shanan, R.; Levanon, Y. Automated 3D-printed finger orthosis versus manual orthosis preparation by occupational therapy students: Preparation time, product weight, and user satisfaction. J. Hand Ther. 2020, 33, 174–179. [Google Scholar] [CrossRef]
- Choi, W.; Jang, W.; Kim, J.; Hwang, S. A pilot study for usefulness of customized wrist splint by thermoforming manufacturing process using 3D printing: Focusing on comparative study with 3D scanning manufacturing process. In Proceedings of the RESNA Annual Conference, Arlington, VA, USA, 13–15 July 2018. [Google Scholar]
- Popescu, D.; Zapciu, A.; Tarba, C.; Laptoiu, D. Fast production of customized three-dimensional-printed hand splints. Rapid Prototyp. J. 2020, 26, 134–144. [Google Scholar] [CrossRef]
- Barros, M.O.; Walker, A.; Stanković, T. Computational design of an additively manufactured origami-based hand orthosis. Proc. Design Soc. 2022, 2, 1231–1242. [Google Scholar] [CrossRef]
- Chu, C.H.; Wang, I.J.; Sun, J.R.; Liu, C.H. Customized designs of short thumb orthoses using 3D hand parametric models. Assist. Technol. 2020, 34, 104–111. [Google Scholar] [CrossRef]
- Górski, F.; Kuczko, W.; Weiss, W.; Wichniarek, R.; Żukowska, M. Prototyping of an individualized multi-material wrist orthosis using fused deposition modelling. Adv. Sci. Technol. Res. J. 2019, 13, 39–47. [Google Scholar] [CrossRef]
- Zhou, M.; Sun, C.; Naghavi, S.A.; Wang, L.; Tamaddon, M.; Wang, J.; Liu, C. The design and manufacturing of a patient-specific wrist splint for rehabilitation of rheumatoid arthritis. Mater. Des. 2024, 238, 112704. [Google Scholar] [CrossRef]
- Paterson, A.M.; Bibb, R.; Campbell, R.I.; Bingham, G. Comparing additive manufacturing technologies for customised wrist splints. Rapid Prototyp. J. 2015, 21, 230–243. [Google Scholar] [CrossRef]
- Popescu, D.; Iacob, M.C.; Tarbă, C.; Lăptoiu, D.; Cotruţ, C.M. Exploring a novel material and approach in 3D-printed wrist-hand orthoses. J. Manuf. Mater. Process. 2024, 8, 29. [Google Scholar] [CrossRef]
- Lee, K.H.; Kim, D.K.; Cha, Y.H.; Kwon, J.Y.; Kim, D.H.; Kim, S.J. Personalized assistive device manufactured by 3D modelling and printing techniques. Disabil. Rehabil. Assist. Technol. 2019, 14, 526–531. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.; Vardakastani, V.; Kedgley, A.E.; Gardiner, M.D.; Vincent, T.L.; Culmer, P.R.; Alazmani, A. HAILO: A sensorised hand splint for the exploration of interface forces. IEEE Trans. Biomed. Eng. 2022, 69, 2850–2859. [Google Scholar] [CrossRef]
- Tan, X.; He, L.; Cao, J.; Chen, W.; Nanayakkara, T. A soft pressure sensor skin for hand and wrist orthoses. IEEE Robot. Autom. Lett. 2020, 5, 2192–2199. [Google Scholar] [CrossRef]
- Barmouz, M.; Uribe, L.V.; Ai, Q.; Azarhoushang, B. Design and fabrication of a novel 4D-printed customized hand orthosis to treat cerebral palsy. Med Eng. Phys. 2024, 123, 104087. [Google Scholar] [CrossRef]
- Cheng, T.; Thielen, M.; Poppinga, S.; Tahouni, Y.; Wood, D.; Steinberg, T.; Menges, A.; Speck, T. Bio-inspired motion mechanisms: Computational design and material programming of self-adjusting 4D-printed wearable systems. Adv. Sci. 2021, 8, 2100411. [Google Scholar] [CrossRef]
- Bos, R.A.; Haarman, C.J.; Stortelder, T.; Nizamis, K.; Herder, J.L.; Stienen, A.H.; Plettenburg, D.H. A structured overview of trends and technologies used in dynamic hand orthoses. J. NeuroEng. Rehabil. 2016, 13, 62. [Google Scholar] [CrossRef]
- Chang, K.; Chang, J.H.; Huang, M.W.; Lee, L.Y. Innovative orthosis for phalanx extension neurofacilitation (iOPEN)—Development of a 3D-printed hand orthosis for chronic stroke patient. In Proceedings of the 2018 IEEE International Conference on Applied System Invention (ICASI), Chiba, Japan, 13–17 April 2018; pp. 1175–1177. [Google Scholar] [CrossRef]
- Merchant, R.; Cruz-Ortiz, D.; Ballesteros-Escamilla, M.; Chairez, I. Integrated wearable and self-carrying active upper limb orthosis. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2018, 232, 172–184. [Google Scholar] [CrossRef]
- Yang, Y.S.; Tseng, C.H.; Fang, W.C.; Han, I.W.; Huang, S.C. Effectiveness of a new 3D-printed dynamic hand–wrist splint on hand motor function and spasticity in chronic stroke patients. J. Clin. Med. 2021, 10, 4549. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.Y.; Pan, L.H.; Yang, W.W.; Huang, L.Y.; Sun, P.C.; Chen, C.S. Biomechanical evaluation of three-dimensional printed dynamic hand device for patients with chronic stroke. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 1246–1252. [Google Scholar] [CrossRef] [PubMed]
- Yeh, P.C.; Chen, C.H.; Chen, C.S. Using a 3D-printed hand orthosis to improve three-jaw chuck hand function in individuals with cervical spinal cord injury: A feasibility study. IEEE Trans. Neural Syst. Rehabil. Eng. 2023, 31, 2552–2559. [Google Scholar] [CrossRef] [PubMed]
- Cui, L.; Phan, A.; Allison, G. Design and fabrication of a three dimensional printable non-assembly articulated hand exoskeleton for rehabilitation. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 4627–4630. [Google Scholar] [CrossRef]
- Esposito, D.; Centracchio, J.; Andreozzi, E.; Savino, S.; Gargiulo, G.D.; Naik, G.R.; Bifulco, P. Design of a 3D-printed hand exoskeleton based on force-myography control for assistance and rehabilitation. Machines 2022, 10, 57. [Google Scholar] [CrossRef]
- Dragusanu, M.; Troisi, D.; Villani, A.; Prattichizzo, D.; Malvezzi, M. Design and prototyping of an underactuated hand exoskeleton with fingers coupled by a gear-based differential. Front. Robot. AI 2022, 9, 862340. [Google Scholar] [CrossRef]
- Chen, Z.H.; Yang, Y.L.; Lin, K.W.; Sun, P.C.; Chen, C.S. Functional assessment of 3D-printed multifunction assistive hand device for chronic stroke patients. IEEE Trans. Neural Syst. Rehabil. Eng. 2022, 30, 1261–1266. [Google Scholar] [CrossRef]
- Risangtuni, A.G.; Suprijanto, S.; Nazaruddin, Y.Y.; Mahyuddin, A.I. Dual-mode 3D printed dynamic wrist driven orthosis for hand therapy exercises. Front. Mech. Eng. 2023, 9, 1286304. [Google Scholar] [CrossRef]
- Ang, B.W.; Yeow, C. 3D printed soft pneumatic actuators with intent sensing for hand rehabilitative exoskeletons. In Proceedings of the 2019 International Conference on Robotics and Automation (ICRA), Montreal, QC, Canada, 20–24 May 2019; pp. 841–846. [Google Scholar] [CrossRef]
- Ang, B.W.K.; Yeow, C.H. Print-it-yourself (PIY) glove: A fully 3D printed soft robotic hand rehabilitative and assistive exoskeleton for stroke patients. In Proceedings of the 2017 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Vancouver, BC, Canada, 24–28 September 2017; pp. 1219–1223. [Google Scholar] [CrossRef]
- Lin, L.; Zhang, F.; Yang, L.; Fu, Y. Design and modeling of a hybrid soft-rigid hand exoskeleton for poststroke rehabilitation. Int. J. Mech. Sci. 2021, 212, 106831. [Google Scholar] [CrossRef]
- Bützer, T.; Lambercy, O.; Arata, J.; Gassert, R. Fully wearable actuated soft exoskeleton for grasping assistance in everyday activities. Soft Robot. 2021, 8, 128–143. [Google Scholar] [CrossRef]
- Nycz, C.J.W.; Bützer, T.; Lambercy, O.; Arata, J.; Fischer, G.S.; Gassert, R. Design and characterization of a lightweight and fully portable remote actuation system for use with a hand exoskeleton. IEEE Robot. Autom. Lett. 2016, 1, 976–983. [Google Scholar] [CrossRef]
- Li, M.; He, B.; Liang, Z.; Zhao, C.G.; Chen, J.; Zhuo, Y.; Xu, G.; Xie, J.; Althoefer, K. An attention-controlled hand exoskeleton for the rehabilitation of finger extension and flexion using a rigid-soft combined mechanism. Front. Neurorobotics 2019, 13, 34. [Google Scholar] [CrossRef] [PubMed]
- Araujo, R.S.; Silva, C.R.; Netto, S.P.N.; Morya, E.; Brasil, F.L. Development of a low-cost EEG-controlled hand exoskeleton 3D printed on textiles. Front. Neurosci. 2021, 15, 661569. [Google Scholar] [CrossRef] [PubMed]
- Haarman, C.J.W.; Hekman, E.E.G.; Rietman, J.S.; Kooij, H.V.D. Mechanical design and feasibility of a finger exoskeleton to support finger extension of severely affected stroke patients. IEEE Trans. Neural Syst. Rehabil. Eng. 2023, 31, 1268–1276. [Google Scholar] [CrossRef] [PubMed]
- Bagneschi, T.; Chiaradia, D.; Righi, G.; Popolo, G.D.; Frisoli, A.; Leonardis, D. A soft hand exoskeleton with a novel tendon layout to improve stable wearing in grasping assistance. IEEE Trans. Haptics 2023, 16, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Burns, M.K.; Orden, K.V.; Patel, V.; Vinjamuri, R. Towards a wearable hand exoskeleton with embedded synergies. In Proceedings of the 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Jeju, Republic of Korea, 11–15 July 2017; pp. 213–216. [Google Scholar] [CrossRef]
- Dudley, D.R.; Knarr, B.A.; Siu, K.C.; Peck, J.; Ricks, B.; Zuniga, J.M. Testing of a 3D printed hand exoskeleton for an individual with stroke: A case study. Disabil. Rehabil. Assist. Technol. 2021, 16, 209–213. [Google Scholar] [CrossRef]
- Michalec, P.; Faller, L.M. 3-D-printing and reliability evaluation of an easy-to-fabricate position sensing system for printed functional wearable assistive devices. IEEE Sens. J. 2024, 24, 4137–4149. [Google Scholar] [CrossRef]
- Yang, Y.S.; Emzain, Z.F.; Huang, S.C. Biomechanical evaluation of dynamic splint based on pulley rotation design for management of hand spasticity. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 683–689. [Google Scholar] [CrossRef]
- Ates, S.; Haarman, C.J.W.; Stienen, A.H.A. SCRIPT passive orthosis: Design of interactive hand and wrist exoskeleton for rehabilitation at home after stroke. Auton. Robot. 2017, 41, 711–723. [Google Scholar] [CrossRef]
- Park, C.B.; Park, H.S. Portable 3D-printed hand orthosis with spatial stiffness distribution personalized for assisting grasping in daily living. Front. Bioeng. Biotechnol. 2023, 11, 895745. [Google Scholar] [CrossRef]
- Park, C.B.; Hwang, J.S.; Gong, H.S.; Park, H.S. A lightweight dynamic hand orthosis with sequential joint flexion movement for postoperative rehabilitation of flexor tendon repair surgery. IEEE Trans. Neural Syst. Rehabil. Eng. 2024, 32, 994–1004. [Google Scholar] [CrossRef]
- Bos, R.A.; Nizamis, K.; Plettenburg, D.H.; Herder, J.L. Design of an electrohydraulic hand orthosis for people with Duchenne muscular dystrophy using commercially available components. In Proceedings of the 2018 7th IEEE International Conference on Biomedical Robotics and Biomechatronics (Biorob), Enschede, The Netherlands, 26–29 August 2018; pp. 305–311. [Google Scholar] [CrossRef]
- Bos, R.A.; Nizamis, K.; Koopman, B.; Herder, J.L.; Sartori, M.; Plettenburg, D.H. A case study with Symbihand: An sEMG-controlled electrohydraulic hand orthosis for individuals with Duchenne muscular dystrophy. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 258–266. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, P.; Deshpande, A.D. Subject-specific assist-as-needed controllers for a hand exoskeleton for rehabilitation. IEEE Robot. Autom. Lett. 2018, 3, 508–515. [Google Scholar] [CrossRef]

| Orthosis Application | Design Explanation |
|---|---|
 [35] [35]Stabilization of the wrist after fracture such as a distal radial fracture, as well as for immobilization in the case of carpal tunnel syndrome or other signs of overuse in the wrist area. | Thermoplastic, customized rigid structure on the ventral side of a forearm and a hand. Velcro fasteners make it easier to put on and take off the splint independently. The recess around the MCP joint of the thumb and fingers 2–5 allows movement of a large part of the thumb and finger movements, but the orthosis restricts the overall mobility of the wrist. Stability is achieved by fixation over a half-length of the forearm. |
 [36] [36]Stabilization of the wrist and thumb after traumatic injuries of the thumb and arthrosis of the thumb saddle joint | Pre-fabricated splint which immobilizes the thumb up to the end joint. The rigid grid structure enables better ventilation, while padding improves wearer comfort. |
 [37] [37]Limiting hyperextension in the case of a swan neck deformity of the fingers. | Minimalistic design based on three support points with a small area covered by the orthosis. It allows sliding of the orthosis on the finger. |
 [38] [38]Improved finger alignment in ulnar deviation from inflammatory and degenerative conditions. | Minimalist design that requires no additional fasteners thanks to wrapping around the hand. The bars between the fingers place the fingers in a physiological position. |
 [39] [39]Stabilization of the movement of the wrist in flexion and extension. Support of finger extension for people with joint contractures problems. | A chain mechanism, mounted on the dorsal side of the fingers, uses rubber bands to support finger extension without producing axial force on the finger joints. The wrist joint allows for wrist flexion and extension. This type of joint can be used to limit the RoM of the hand joint. The torsion spring in this joint can be activated to support extension, and deactivated when donning the orthosis. The position of the wrist joint can be adjusted using slotted holes placed on the forearm part. |
 [40] [40]Stabilization of the wrist with slight extension of the wrist. Support in finger extension after peripheral lesions of the radial nerve and associated radial nerve palsy. | A dorsal (exercise) splint that fixes the wrist in a slightly extended position to improve grasping and uses rubber or spring tension, which are placed on an outrigger to support extension of the fingers in the MCPs and support a physiological gripping function, without elastic elements gliding across the skin and creating an uncomfortable compression feeling due to occurring force. |
 [41] [41]Prevents hyperextension of the 4th and 5th MCPs after ulnar nerve injury. | Liver-shaped palm design allows free tissue movement and full RoM of fingers and thumb. The palm arc shape holds the splint firmly, with leather loops and elastic bands on the palm side maintaining physiologically favorable MCP positions for the 4th and 5th fingers. |
 [42] [42]Active support of thumb, middle finger, and ring finger flexion for people with central nervous system disorders. | Soft glove with integrated wire system to support hand closing. Wires go on the sides of the fingers, so they are not inhibited when grasping. The close-fitting textile design allows for a light device and natural haptic feeling. The motor units can be placed outside the hand, reducing the carried weight. Closed tips of the fingers allow the force to be transferred without sliding the glove across the finger and placing sensors. Pressure sensors are used to detect the intention of hand closing. |
 [33] [33]A robotic glove for the support of hand function after strokes and hand injuries. The fingers can be mobilized in flexion and extension. | Rigid glove with actuated joints placed on the dorsal side, leaving the palmar side free for grasping. The splint is attached to the forearm and the fingertips on the hand. Boa system used to facilitate donning/doffing the device with one hand. Actuators integrated on the forearm part to shift the weight and volume from the hand. They are controlled by an sEMG signal, with electrodes placed on the forearm. Soft elements used on the fingers to increase comfort. Wrist is fixed, which simplifies device control. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michalec, P.; Schusser, M.; Weidner, R.; Brandstötter, M. Designing Hand Orthoses: Advances and Challenges in Material Extrusion. Appl. Sci. 2024, 14, 9543. https://doi.org/10.3390/app14209543
Michalec P, Schusser M, Weidner R, Brandstötter M. Designing Hand Orthoses: Advances and Challenges in Material Extrusion. Applied Sciences. 2024; 14(20):9543. https://doi.org/10.3390/app14209543
Chicago/Turabian StyleMichalec, Paweł, Martin Schusser, Robert Weidner, and Mathias Brandstötter. 2024. "Designing Hand Orthoses: Advances and Challenges in Material Extrusion" Applied Sciences 14, no. 20: 9543. https://doi.org/10.3390/app14209543
APA StyleMichalec, P., Schusser, M., Weidner, R., & Brandstötter, M. (2024). Designing Hand Orthoses: Advances and Challenges in Material Extrusion. Applied Sciences, 14(20), 9543. https://doi.org/10.3390/app14209543





