Featured Application
The results of this work can be used to design, evaluate, and treat specific phobias using augmented reality.
Abstract
Augmented Reality (AR) is helpful for overcoming the challenges of in vivo exposure therapy for Specific Phobia (SP). Specifically, Projection-based AR exposure therapy (P-ARET) allows the individual to face the feared animal without intrusive hardware, the phobic stimulus can be controlled, and it can maximize “variability”, producing a positive effect in the generalization of the results. The goal of this work is to assess the feasibility of P-ARET for SP, comparing multiple stimuli (MS) versus single stimulus (SS) conditions and evaluating the participants’ user experience. Adherence to a daily monitoring app (Emotional Monitor) and preliminary efficacy of the P-ARET treatment were assessed. Four participants diagnosed with SP of cockroaches (DSM-5) were randomly assigned to different baselines. Episodic and daily evaluations were performed. Participants considered the MS condition more aversive but more effective than the SS condition. Adherence to the mobile app was 83% for three participants and 55% for the remaining person. Analyses of non-overlap of all pairs and changes in the functionality levels showed a decrease in the SP symptoms at post-treatment and follow-ups. This study offers preliminary feasibility results for a novel form of P-ARET to treat participants with cockroach phobia, which may also apply to other phobias.
1. Introduction
In vivo exposure therapy (iVET) is widely regarded as the most effective treatment for specific phobia (SP) [1], one of the most prevalent anxiety disorders globally [2]. Despite this, iVET faces several barriers to implementation in clinical practice, including low acceptance, high dropout rates, poor accessibility, and administering challenges in implementing it in a clinical setting [3].
The use of mixed realities, such as Virtual Reality (VR) and augmented reality (AR), improves the limitations mentioned, particularly in terms of access and acceptability.
Regarding increased acceptability, randomized clinical trial results showed that AR exposure was an effective and accepted treatment for SP [4].
The previous results should motivate further investigation with mixed realities so that SP can replicate the findings in other contexts and with innovations that increase the acceptability. The present study taps into the latter goal.
The developed projection-based AR exposure therapy (P-ARET) system [5] for small animal phobia [6] treatment enables patients to confront the feared animal (cockroach) in the real environment, projected onto a table within the treatment room. This design eliminates the need for helmets or glasses. Participants can interact with the stimulus using his or her bodies or tools, like a glass, fostering a natural interaction. Additionally, the system includes interactive activities (e.g., capturing, chasing, and killing) and environmental games. The phobic stimulus is customizable in terms of size, color, movement, and quantity, allowing the clinician to control its actions (such as dying or flapping) via a laptop. Also, it allows the phobic stimulus to be manipulated and modified in a controlled manner. This concept of stimulus “variability” is an important contributor to the effectiveness of the exposure technique [7,8].
The variability of context and stimuli seems crucial for generalizing learning. These enable individuals with SP to apply the skills learned to novel or diverse situations and stimuli that were not part of the traditional exposure therapy process [7,9].
Moreover, a growing body of scientific evidence has used this ecological momentary assessment (EMA) to collect experience in real-life contexts to assess anxiety disorders [10]. This approach may be particularly beneficial for individuals with SPs [11] to be able to assess their symptoms in a real context. In the present work, they face these fears, especially in the daily assessment of their fear of cockroaches. During these momentary assessments, participants are not directly exposed to cockroaches but are instead asked questions throughout the day based on hypothetical encounters with cockroaches. However, it is possible that during this period, participants may encounter real-life situations where they come across cockroaches, such as on the street, at home, or in the workplace, or engage in activities that typically trigger their anxiety, like walking outside at night or taking out the trash. These real-world experiences allow participants to respond more authentically to questions than they would in a controlled laboratory setting, thus providing a more accurate measure of their phobia progression and responses to stimuli.
This study aimed to explore the feasibility of using P-ARET to present a variety of phobic stimuli to participants diagnosed with cockroach phobia. A key study goal was to compare participants’ experience with multiple stimuli (MS) versus single stimulus (SS) conditions. As a secondary objective, we analyzed the adherence to a daily monitoring app (Emotional Monitor). A final secondary goal was to assess the preliminary efficacy of the P-ARET treatment.
2. Materials and Methods
2.1. Study Design
This study employed a single-case, multiple-baseline, AB design, where A represents the baseline phase and B represents the treatment phase. Although three individuals are generally sufficient to mitigate threats to internal validity in multiple-baseline designs, including four participants is preferred to enhance replication reliability [12]. In such designs, participants are assigned to different baseline durations to ensure at least three replications of the treatment effects [13]. All participants start the baseline phase on the same day, with the treatment phase systematically introduced on different days for each participant. In this study, an independent researcher determined the duration of the baseline phase using an online program (https://randomizer.org/) (accessed on 1 September 2020). The duration of the baseline (A) phase ranged from 8 to 16 days to ensure a minimum of five evaluations in each phase, as recommended by the guidelines [14]. Specifically, the four baseline durations were 10, 9, 13, and 12 days for each participant, respectively. Day 1 of the baseline phase corresponds to the day of the screening interview for each participant. The treatment phase begins the day after the baseline phase ends (on days 11, 10, 14, and 13 for each participant, respectively). Two sessions per week were conducted over a three-week period. After the treatment phase, a post-evaluation and two follow-ups (at 1 month and 6 months) were conducted.
This study was registered at clinicaltrials.gov: NCT04553120 (7 January 2020) and received approval from the Universitat Jaume I Ethics Committee (CD/64/2019).
2.2. Procedure
2.2.1. Eligibility Criteria
Inclusion criteria were as follows: Participants must be over 18, meet DSM-5 criteria for cockroach phobia [15], have experienced the SP for at least 6 months, provide informed consent, score at least 4 on fear and avoidance scales of the diagnostic interviews administered (see below), and have a smartphone with Android operating system (necessary for the app).
Exclusion Criteria included: Participants were excluded if they had severe mental disorders requiring urgent psychological care, substance dependence or abuse, psychosis or severe organic illness, were undergoing similar treatment, could place their hands in a terrarium with one cockroach, were changing medications during the study, and if they had a smartphone with an operating system different from Android (iPhone, for which the app is still not available).
2.2.2. Recruitment, Randomization, and Blinding
Recruiting was completed via online advertisements on social networks and newspapers. In addition, this study was introduced to individuals seeking support at the Emotional Disorders Clinic at Universitat Jaume I. Individuals who were interested in participating received detailed study information and underwent an eligibility assessment. An independent researcher randomly assigned those who met the inclusion criteria and signed the online consent form to one of the baselines.
2.2.3. Participants
The study participants were three women and one man. Their mean age was 31.5, ranging from 21 to 46. Table 1 reports more details.

Table 1.
Characteristics of the participants.
Participant 1 (P1) was a 46-year-old woman, married, with a daughter. She had finished secondary school studies and worked in an administrative position in an office. Her fear of cockroaches started in childhood and intensified over time. In the initial interview, P1 showed extreme fear of cockroaches, mentioning that she regularly checked every corner of her house for cockroaches and plugged up any holes they might use to get inside.
Participant 2 (P2) was a 21-year-old single woman in her last year of psychology study. Her fear of cockroaches started in childhood. During the screening interview, P2 described feeling extreme anxiety and losing control when she saw a cockroach and explained that if she saw one, it would be on her mind for days.
Participant 3 (P3) was a 28-year-old single man studying for a civil service examination. His fear of cockroaches began as a child, although he couldn’t recall a specific trigger. P3 explained that he had never killed a cockroach. He had traps all over the house, and when cockroaches fell into the traps, his father got rid of them once they were dead.
Participant 4 (P4) was a 31-year-old single woman working as a physiotherapist. Her fear of cockroaches started when P4 was a child, and she thought it was because she spent long periods at her grandparents’ country house, where cockroaches appeared daily. She has managed to kill a cockroach but with intense discomfort.
2.2.4. Assessment Measures
Some evaluations were conducted at various time points: screening, pre-treatment, post-treatment, and at one- and six-month follow-ups. The app carried out others daily (see Table 2) [14].

Table 2.
App assessment items.
Episodic assessment conducted at screening, pre-treatment, post-treatment, and one- and six-month follow-ups.
Baseline episodic assessment: Demographic characteristics such as age, sex, educational level, employment, and marital status were collected at the beginning of the study (first day of the baseline phase).
Diagnosis. The Anxiety Disorders Interview Schedule for DSM-IV-TR [16] is a specific diagnostic semi-structured interview designed to assess SP based on DSM-IV-TR criteria. This interview includes additional measures such as perceived interference and distress, rated on a scale from 0 to 8 (wherein 0 = “Not at all” and 8 = “Very severe”).
The DSM-5 version was not used due to the unavailability of the Spanish DSM-5 interview during the study, although the diagnostic criteria remain unchanged. The tool has demonstrated strong psychometric properties and reliability for most anxiety disorders [17,18].
Behavioral Avoidance Test (BAT). This adapted test [19] asks participants to confront one real cockroach. Consistent with the instructions, we encourage them to approach and interact with the animal inside a transparent plastic terrarium. Before the test, anxiety levels, subjective avoidance, and belief in fear-related thoughts are rated (from 0 to 10). The dependent variable in this test is the “performance”, which is the distance to the terrarium (in meters) and the degree of interaction with the cockroach. Performance is determined by proximity to the cockroach (in meters) and the level of interaction, rated from 0 (no entry) to 12 (entire interaction with the animal).
Ecological and momentary assessment with the app: The Emotional Monitor App, available on the Google Play store (https://play.google.com/store/apps/details?id=monitoremocional.code&hl=ca&gl=US) (accessed on 20 January 2022), was used to assess daily symptoms associated with cockroach phobia. This app was developed to be used with the Android 6.0 version operating system or later. Evaluation with the app started from the baseline phase (screening day) and lasted until day 34. Each day, participants were given a two-hour window (8–10 pm) to complete four items related to their symptoms: fear, avoidance, dangerousness, and coping ability. The specific items can be found in Table 2.
2.3. Intervention
The intervention was based on exposure to cockroaches using P-ARET, incorporating both single stimulus (SS) exposure, where the same one projected cockroach was used, and multiple stimuli (MS) exposure, featuring variations in the number, shape, color, and movement of the cockroaches (Figure 1). Participants were equally divided to start with either modality (SS or MS exposure). Each participant was randomly assigned to the two conditions, ensuring that each condition was applied three times per participant.

Figure 1.
Example of the MS condition on the left and the SS condition on the right.
The treatment was implemented during six weekly individual sessions lasting approximately one hour. The main elements included psychoeducation, exposure to the feared stimulus, modeling, cognitive restructuring, reinforcement, and relapse prevention. Following Öst’s guidelines [19], the exposure session was conducted gradually, in a planned and controlled manner.
The goal of the exposure treatment was for participants to face their phobic situation in a safe environment, which helped them to challenge the negative consequences they anticipated.
2.4. Calculations and Analyses
First, we assessed the participants’ user experience for single vs. multiple AR stimuli. We used the Non-overlap of All Pairs (NAP) to measure the impact of the P-ARET treatment on the daily items in the app (see Table 3). NAP is the preferred statistical approach to assess the effects of an intervention in single-case designs. It compares the degree of improvement (non-overlap) across all the points in the 5 baseline phase compared to all the measurements in the treatment phase [20].

Table 3.
Timeline.
The NAP analyzes the percentage of data that present with an improvement or a deterioration (ranging from 0 to 100), where higher scores reflect more improvement (less overlap between phases). To calculate the NAP index, we used the Single Case Research website (http://www.singlecaseresearch.org/calculators/nap) (accessed on 6 December 2022).
In terms of NAP interpretation, we used the cutoffs based on the findings from a series of single-case studies [20]: below 38% (<25th percentile of lower reported NAP scores) would be interpreted as poor treatment effects; scores from 38% to 68% (25th–50th percentile) would be interpreted as mild-to-moderate effects; scores between 69% and 96% (50th–75th percentile) would correspond to moderate-to-large effects; and scores over 96% (>75th percentile) should be interpreted as very large effects. Our group successfully implemented these cutoffs in past research [21].
The app’s adherence was measured by the percentage of daily responses completed. Changes in the levels of functionality on all the variables of the BAT were also analyzed. Given that not all the data required to apply the Reliable Change Index were available, we apply criterion “b” (b = Mfunctional ± 2SDfunctional), proposed by Jacobson and Truax [22], which establishes a cutoff point between functionality and dysfunctionality after the intervention. The calculation of the cutoff point in patients with cockroach phobia was based on the data by Botella et al. [4].
3. Results
3.1. User Experience
Half (50%) of participants preferred the SS option, whereas the other 50% chose the MS option. However, all the participants considered the MS condition more effective and would recommend it to a friend, and they also considered it more aversive.
3.2. Adherence to the Emotional Monitor App
The participants had to respond to daily assessments in the app for 34 days (the whole treatment duration). Three of them completed the evaluation 83% of the time, and one answered the daily app prompts 55.5% of the time.
3.3. Non-Overlap Analyses (NAP)
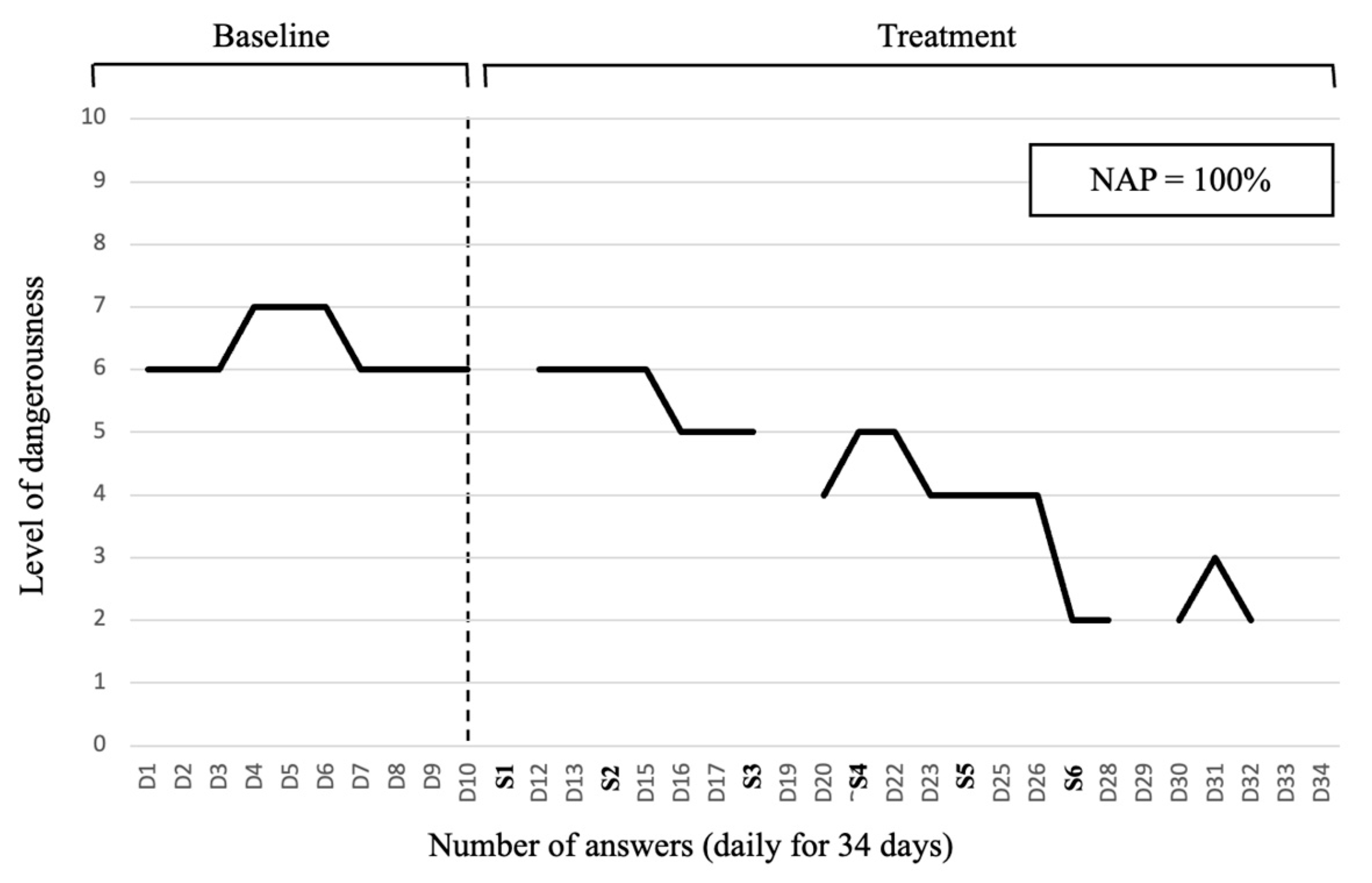
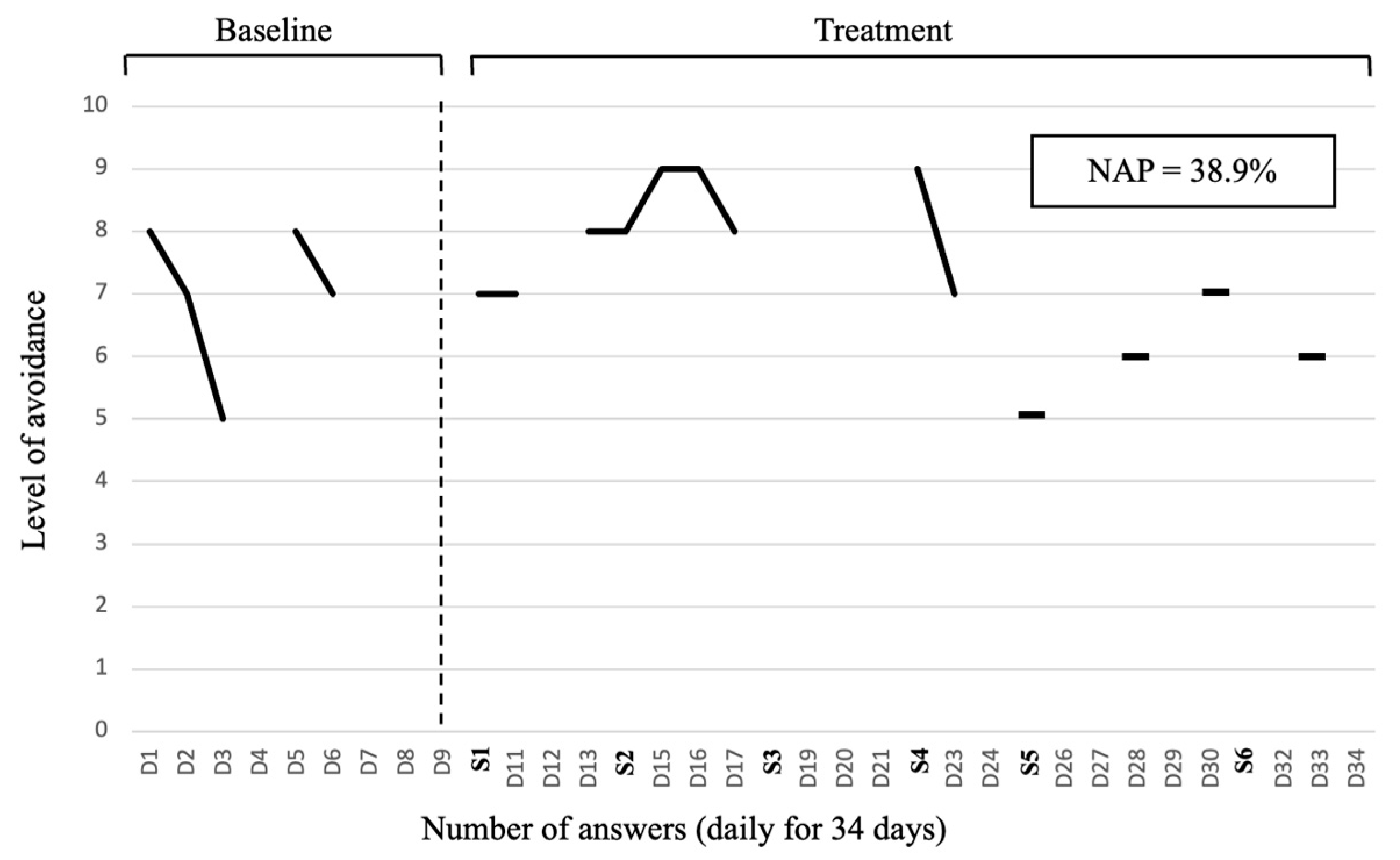
The NAP analyses results are presented in Table 4. P1 obtained a large treatment effect on the measures of fear (Item 1), avoidance (Item 2), and dangerousness (Item 3) and a moderate-to-large effect on coping ability (Item 4). P2 showed a mild-to-moderate reduction in fear and avoidance (Items 1 and 2), a moderate-to-large effect on dangerousness (Item 3), and a large treatment effect on coping ability (Item 4). P3 obtained a moderate-to-large effect on all the outcomes (Items 1, 2, 3, and 4), whereas P4 showed a moderate-to-large improvement in fear and ability to cope (Items 1 and 4) and mild-to-moderate intervention effects on avoidance and dangerousness (Items 2 and 3).

Table 4.
Results of the NAP analyses of the Emotional Monitor App.
A visual example of a very large treatment effect on the level of perceived dangerousness can be seen in Figure 2. An example of a poor treatment effect on the level of avoidance can be seen in Figure 3.
Figure 2.
Participant 1: Evolution in the level of dangerousness. NAP: non-overlap of all pairs. D1–D34 refers to the days in which the treatment phase is evaluated with the app.
Figure 3.
Participant 2: Evolution in the level of avoidance. NAP: non-overlap of all pairs. D1–D34 refers to the days in which the treatment phase is evaluated with the app.
3.4. Change in the Levels of Functionality on the BAT
As Table 5 shows, the participants generally recovered or improved at all the assessment points for all the outcomes on the BAT. The treatment appears to be the most effective for avoidance and beliefs, followed by fear and performance. The results were generally maintained or even improved at the follow-ups.

Table 5.
Change in the BAT outcomes based on previous studies on the effectiveness of AR on cockroach phobia.
4. Discussion
The main goal of this study was to assess the feasibility of applying a P-ARET intervention for adults with cockroach phobia. We tested varying phobic stimuli and evaluated the participants’ user experience for treatment modalities. Furthermore, we evaluated the preliminary efficacy of the P-ARET and analyzed other outcomes related to the feasibility, such as adherence to a daily monitoring app.
First, the participants did not show a clear preference for either of the two treatment modalities (SS or MS). However, the four participants considered the MS version more effective and would recommend this option to a friend. Importantly, however, the participants also considered it more aversive than SS, probably due to the similarity to real-world situations and the number of different feared stimuli they had to face simultaneously.
Our study results are in line with previous works related to optimizing exposure therapy by using a variety of stimuli [7,9]. Patients find stimulation variability more useful and effective, and they report that this methodology makes the therapeutic process easier.
Adherence to the Emotional Monitor app was generally high, except for one participant who only registered about half of the days. The findings align with earlier research on the mobile application [21,22] and provide backing for the notion that conducting ecological momentary assessment through an app is viable. In the case of the participant with lower adherence rates, she mentioned that, on the baseline days, she was taking career exams and, therefore, found it difficult to complete the assessments.
Finally, regarding the preliminary efficacy of the P-ARET treatment, we found that it was effective for all the patients across all the outcomes, even in the long term. We found significant decreases in psychological and behavioral symptoms associated with the phobia throughout the treatment, at post-assessment, and at follow-ups. These reductions were evident in the data obtained from the mobile app and the BAT test, which are consistent with the idea that mixed realities are effective alternatives to iVET for SP [23].
Despite the positive results, individual variability in response to the treatment is noticeable. For example, P1 exhibited the most consistent and significant improvements across measures of fear, avoidance, and dangerousness, while P2 showed milder effects in fear and avoidance. About P2, it is important to note that this patient obtained the poorest adherence levels to the mobile app and indicated being in the middle of the exam period at university, which may have influenced the anxiety levels reported and engagement with therapy. Regarding P3, this patient obtained the most consistent improvements across outcomes, which were between moderate and large. Across patients, the poorest improvement for P1 was in coping, P2 and P3 obtained the poorest results in avoidance, and P4 showed a modest improvement in dangerousness.
Personal characteristics (e.g., personality, socioeconomic status, and previous clinical status, among others), external factors (e.g., positive or negative events), adherence to the therapeutic treatment, and their interaction might explain this variability in treatment outcomes, which justifies the need for personalized approaches and routine active monitoring to improve engagement and treatment effectiveness in real-time [24].
Although these study results should be interpreted cautiously due to the reduced sample size, the findings are encouraging.
Importantly, effect sizes and recovery rates were generally high, and improvements continued after the treatment ended. Specifically, we observed that the improvements were the largest one and six months after treatment, which is encouraging regarding the stability/maintenance of treatment effects. It shows that the participants could deal with situations related to cockroaches (less avoidance) and better manage fear and negative beliefs when facing real-life situations with the tools they learned during therapy. This study adds to existing evidence about the effectiveness of mixed realities in producing long-term changes in individuals with small animal phobias, and it suggests that these interventions are generally sufficient for the effective management of these problems [4].
The promising positive symptom improvements observed in all four participants after six months could be attributed to several factors. However, it is possible that the combination of exposure sessions involving both single and multiple stimuli may have contributed to the results by facilitating the generalization of fear to more varied and unexpected situations similar to those encountered in real life [7]. Further investigation is required to determine whether this long-term improvement is solely due to exposure therapy with MS or if the combination of both SS and MS is more effective due to habituation and learning effects associated with the variability between sessions.
We think this study has many strengths. One of the strengths is the use of the mobile app, which allowed us to collect data from the participants in natural environments on a day-to-day basis rather than in laboratory conditions. This made it possible to obtain more ecological data and perform non-overlap calculations.
In addition, using P-ARET allowed the therapists to have greater control over the therapy and provide stimulation variability to optimize the treatment. Most importantly, this study evaluated participants’ user experience regarding these variations in stimuli, which is important because dropouts in exposure therapy for SP are alarmingly frequent [25,26]. Our feasibility results support the idea that P-ARET might be a feasible option to attempt to address SP effectively while potentially reducing dropout rates.
Therefore, reducing this fear has important clinical implications due to the large number of persons with fear-related conditions and the intense phobic symptoms and daily interference they generate.
Fear of cockroaches, in particular, tends to be normalized because the animal is associated with dirt, diseases, potential plagues, and a wide range of human pathogens like bacteria and viruses [27]. Compared with other phobia-inducing objects or situations (e.g., snakes, heights, illnesses, injuries, etc.), cockroaches provoke fear in a large number of people who live in tropical and humid places where they are common [28]. For example, a recent study by Grimaldos et al. [29] indicated that cockroaches were the most aversive animals compared to snakes and spiders. This fear can lead to important avoidance behaviors that limit life, which, unlike other fears, could be normalized by the patient or by other people due to the intrinsic pathogenic characteristics associated with the animal indicated above. This normalization might, in turn, negatively impact the seeking help process or might lead to seeking support only when it has reached extreme suffering and interference (e.g., stop going out at night, sell the house because one has seen cockroaches, etc.).
This study also has limitations. One of them is the fact that the app only works on Android devices, and the results of the present study, in terms of feasibility, support the development of the app for other operating systems. Another limitation is related to the sample size, given that all of the study data were obtained from a small sample of four participants. Confirming these data with a larger sample would be interesting now that feasibility and preliminary efficacy have been tested in a reduced number of individuals.
Also, it is possible that self-selection bias was present in this study, as participants were likely to have a predisposition to confront their phobia and actively work to overcome their fear. This inclination may not be representative of all people with cockroach phobia, as many tend to avoid exposure to the feared stimulus.
Additionally, while baseline assessments over different timeframes are used to mitigate internal validity, it is not entirely sure that the improvements observed are not influenced by spontaneous recovery in certain participants. So, it would be interesting for these findings to be supported in the future by studies that include control groups to evaluate the influence of time without treatment. Also, it would be interesting to study the effect of the between-session habituation effect for combining MS with SS. Finally, an uncontrollable limitation that affected the present study was the pandemic, which made recruitment difficult.
5. Conclusions
This study explored the feasibility and preliminary efficacy of P-ARET for adults with cockroach phobia. Key findings include a lack of preference for treatment modalities among participants, but they considered the MS version more effective, showed high adherence to the Emotional Monitor app, and showed significant efficacy of P-ARET in several outcomes. This study highlights the usefulness of mixed realities in exposure therapy, suggesting its effectiveness in managing phobias in the long term. Despite limitations, the present study shows the importance of variability in conducting exposure treatment for cockroach phobia.
The use of VR and AR offers a higher level of specificity, allowing for controlled and personalized exposure to phobic stimuli. This technology enables the selection of not only the necessary stimulus but also the associated details, such as color, size, and movement. Such personalized interaction enhances validity by replicating real-world scenarios in a safe environment while providing greater control over each step of the exposure intensity during treatment. This level of control makes the treatments more replicable, a feature that cannot be achieved with real stimuli.
Additionally, VR and AR could contribute to a more gradual exposure to feared stimuli, potentially reducing the aversion that patients feel when exposed to what they fear. This approach may help to lower the high rates of treatment abandonment, while also enhancing the effectiveness of each step within the exposure hierarchy and improving the overall treatment experience for patients.
Author Contributions
Conceptualization, J.B.-L., J.G., D.C. and S.Q.; Data curation, M.P.-B. and S.Q.; Formal analysis, C.S.-R., A.G.-P. and S.Q.; Funding acquisition, J.B.-L. and S.Q.; Investigation, M.P.-B., J.B.-L., J.G., C.S.-R., A.G.-P. and S.Q.; Methodology, M.P.-B., J.B.-L., J.G. and C.S.-R.; Project administration, J.B.-L. and S.Q.; Resources, D.C.; Software, D.C. and A.G.-P.; Supervision, J.B.-L., C.S.-R., A.G.-P. and S.Q.; Visualization, M.P.-B.; Writing—original draft, M.P.-B.; Writing—review and editing, M.P.-B., J.B.-L., J.G., C.S.-R. and S.Q. All authors have read and agreed to the published version of the manuscript.
Funding
Funding for this study was provided by Grant Ministerio de Ciencia, Innovación y Universidades (Spain) (Programa Estatal I + D + i RTI2018-100993-B-I00) funded by MCIN/AEI/10.13039/501100011033 and by “ERDF A way of making Europe”, by the “European Union”.
Institutional Review Board Statement
The Research Ethics Committee of Universitat Jaume I (Castellón, Spain) approved this study on 13 December 2019 (CD/64/2019). It was carried out following the Helsinki Declaration and the Madrid Declaration of the World Psychiatric Association.
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
Data will be made available upon request.
Acknowledgments
The current project was supported by Plan 2021 de Promoción de la Investigación de la Universitat Jaume I [UJI-B2021-47], CIBEROBN, an initiative of the ISCIIII [CB06 03/0052], by the Grant Prometeo Programme for Research Groups of Excellence [CIPROM/2021/041—Project “IMPULSA”] (Conselleria d’Innovació, Universitats, Ciència i Societat Digital; Generalitat Valenciana) and Convocatòria 2023 d’ajudes a grups d’investigació actius en captació de recursos del pla estatal d’I + D + i (reference numbers: GACUJIMB/2023/15 and GACUJIMB/2023/19).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Nathan, P.; Gorman, J.M. A Guide to Treatments That Work; Oxford University Press: Oxford, UK, 2002. [Google Scholar]
- Witthauer, C.; Ajdacic-Gross, V.; Meyer, A.H.; Vollenweider, P.; Waeber, G.; Preisig, M.; Lieb, R. Associations of Specific Phobia and Its Subtypes with Physical Diseases: An Adult Community Study. BMC Psychiatry 2016, 16, 155. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Palacios, A.; Botella, C.; Hoffman, H.; Fabregat, S. Comparing Acceptance and Refusal Rates of Virtual Reality Exposure vs. in Vivo Exposure by Patients with Specific Phobias. Cyberpsychology Behav. Impact Internet Multimed. Virtual Real. Behav. Soc. 2007, 10, 722–724. [Google Scholar] [CrossRef] [PubMed]
- Botella, C.; Pérez-Ara, M.Á.; Bretón-López, J.; Quero, S.; García-Palacios, A.; Baños, R.M. In Vivo versus Augmented Reality Exposure in the Treatment of Small Animal Phobia: A Randomized Controlled Trial. PLoS ONE 2016, 11, e0148237. [Google Scholar] [CrossRef] [PubMed]
- Wrzesien, M.; Alcañiz, M.; Botella, C.; Burkhardt, J.-M.; Bretón-López, J.; Ortega, M.; Brotons, D.B. The Therapeutic Lamp: Treating Small-Animal Phobias. IEEE Comput. Graph. Appl. 2013, 33, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Wardenaar, K.J.; Lim, C.C.W.; Al-Hamzawi, A.O.; Alonso, J.; Andrade, L.H.; Benjet, C.; Bunting, B.; de Girolamo, G.; Demyttenaere, K.; Florescu, S.E.; et al. The Cross-National Epidemiology of Specific Phobia in the World Mental Health Surveys. Psychol. Med. 2017, 47, 1744–1760. [Google Scholar] [CrossRef]
- Craske, M.G.; Treanor, M.; Conway, C.C.; Zbozinek, T.; Vervliet, B. Maximizing Exposure Therapy: An Inhibitory Learning Approach. Behav. Res. Ther. 2014, 58, 10–23. [Google Scholar] [CrossRef]
- Shiban, Y.; Schelhorn, I.; Pauli, P.; Mühlberger, A. Effect of Combined Multiple Contexts and Multiple Stimuli Exposure in Spider Phobia: A Randomized Clinical Trial in Virtual Reality. Behav. Res. Ther. 2015, 71, 45–53. [Google Scholar] [CrossRef]
- Boehnlein, J.; Altegoer, L.; Muck, N.K.; Roesmann, K.; Redlich, R.; Dannlowski, U.; Leehr, E.J. Factors influencing the success of exposure therapy for specific phobia: A systematic review. Neurosci. Biobehav. Rev. 2020, 108, 796–820. [Google Scholar] [CrossRef]
- Walz, L.C.; Nauta, M.H.; aan het Rot, M. Experience Sampling and Ecological Momentary Assessment for Studying the Daily Lives of Patients with Anxiety Disorders: A Systematic Review. J. Anxiety Disord. 2014, 28, 925–937. [Google Scholar] [CrossRef]
- Alpers, G.W. Ambulatory assessment in panic disorder and specific phobia. Psychol. Assess. 2009, 21, 476. [Google Scholar] [CrossRef]
- Kratochwill, T.R.; Levin, J.R. (Eds.) Enhancing the Scientific Credibility of Single-Case Intervention Research: Randomization to the Rescue. Single-Case Intervention Research: Methodological and Statistical Advances; American Psychological Association: Washington, DC, USA, 2014; pp. 53–89. [Google Scholar] [CrossRef]
- Tate, R.L.; Perdices, M.; Rosenkoetter, U.; McDonald, S.; Togher, L.; Shadish, W.; Horner, R.; Kratochwill, T.; Barlow, D.H.; Kazdin, A.; et al. The Single-Case Reporting Guideline in BEhavioural Interventions (SCRIBE) 2016: Explanation and Elaboration. Arch. Sci. Psychol. 2016, 4, 10–31. [Google Scholar] [CrossRef]
- Kratochwill, T.R.; Hitchcock, J.; Horner, R.H.; Levin, J.R.; Odom, S.L.; Rindskopf, D.M.; Shadish, W.R. Single-Case Designs Technical Documentation. What Works Clearinghouse. 2010. Available online: https://files.eric.ed.gov/fulltext/ED510743.pdf (accessed on 7 September 2024).
- American Psychiatric Association. Anxiety Disorders. In Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association: Washington, DC, USA, 2013; Volume 5. [Google Scholar] [CrossRef]
- Brown, T.A.; Di Nardo, P.; Barlow, D.H. Anxiety Disorders Interview Schedule Adult Version (ADIS-IV): Client Interview Schedule; Oxford University Press: New York, NY, USA, 1994. [Google Scholar]
- Antony, M.M.; Orsillo, S.M.; Roemer, L. (Eds.) Practitioner’s Guide to Empirically Based Measures of Anxiety; Springer Science & Business Media: Berlin, Germany, 2001. [Google Scholar]
- Di Nardo, P.A.; Moras, K.; Barlow, D.H.; Rapee, R.M.; Brown, T.A. Reliability of DSM-III-R Anxiety Disorder Categories. Arch. Gen. Psychiatry 1993, 50, 251. [Google Scholar] [CrossRef] [PubMed]
- Öst, L.-G.; Hellström, K. One-session therapist-directed exposure vs. self-exposure in the treatment of spider phobia. Behav. Res. Ther. 1991, 33, 959–965. [Google Scholar] [CrossRef]
- Parker, R.I.; Vannest, K.J.; Davis, J.L. Effect Size in Single-Case Research: A Review of Nine Nonoverlap Techniques. Behav. Modif. 2011, 35, 303–322. [Google Scholar] [CrossRef]
- Tur, C.; Campos, D.; Suso-Ribera, C.; Kazlauskas, E.; Castilla, D.; Zaragoza, I.; García-Palacios, A.; Quero, S. An Internet-delivered Cognitive-Behavioral Therapy (iCBT) for Prolonged Grief Disorder (PGD) in adults: A multiple-baseline single-case experimental design study. Internet Interv. 2022, 29, 100558. [Google Scholar] [CrossRef]
- Jacobson, N.S.; Truax, P. Clinical Significance: A Statistical Approach to Defining Meaningful Change in Psychotherapy Research. J. Consult. Clin. Psychol. 1991, 59, 12–19. [Google Scholar] [CrossRef]
- Suso-Ribera, C.; Fernández-Álvarez, J.; García-Palacios, A.; Hoffman, H.G.; Bretón-López, J.; Baños, R.M.; Quero, S.; Botella, C. Virtual Reality, Augmented Reality, and in Vivo Exposure Therapy: A Preliminary Comparison of Treatment Efficacy in Small Animal Phobia. Cyberpsychology Behav. Soc. Netw. 2019, 22, 31–38. [Google Scholar] [CrossRef]
- Gual-Montolio, P.; Martínez-Borba, V.; Bretón-López, J.M.; Osma, J.; Suso-Ribera, C. How Are Information and Communication Technologies Supporting Routine Outcome Monitoring and Measurement-Based Care in Psychotherapy? A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 3170. [Google Scholar] [CrossRef]
- Choy, Y.; Fyer, A.J.; Lipsitz, J.D. Treatment of Specific Phobia in Adults. Clin. Psychol. Rev. 2007, 27, 266–286. [Google Scholar] [CrossRef]
- Serrano, B.; Botella, C.; Wiederhold, B.K.; Baños, R.M. Virtual reality and anxiety disorders treatment: Evolution and future perspectives. In Virtual Reality for Psychological and Neurocognitive Interventions; Rizzo, A.S., Bouchard, S., Eds.; Springer: Berlin/Heidelberg, Germany, 2019; pp. 47–84. [Google Scholar] [CrossRef]
- Baumholtz, M.A.; Parish, L.C.; Witkowski, J.A.; Nutting, W.B. The medical importance of cockroaches. Int. J. Dermatol. 1997, 36. [Google Scholar] [CrossRef]
- Bueno-Marí, R.; Bernués-Bañeres, A.; Peris-Felipo, F.J.; Moreno-Marí, J.; Jiménez-Peydró, R. American Cockroach Control Assays in the Municipal Sewerage System of Valencia (Spain). Pol. J. Entomol. 2013, 82, 143–150. [Google Scholar] [CrossRef]
- Grimaldos, J.; Duque, A.; Palau-Batet, M.; Pastor, M.C.; Bretón-López, J.; Quero, S. Cockroaches Are Scarier than Snakes and Spiders: Validation of an Affective Standardized Set of Animal Images (ASSAI). Behav. Res. Methods 2021, 53, 2338–2350. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).