Identifying Users’ Needs to Design and Manufacture 3D-Printed Upper Limb Sockets: A Survey-Based Study
Abstract
1. Introduction
1.1. Prosthetic Arms
1.2. Fit Problems of Traditional Sockets
1.3. 3D-Printed Sockets
1.4. Importance of User Perception and Context
1.5. Hypotheses, Aim and Contribution
2. Methods
2.1. Participants
2.2. Questionnaire Design
2.3. Data Analysis
3. Results
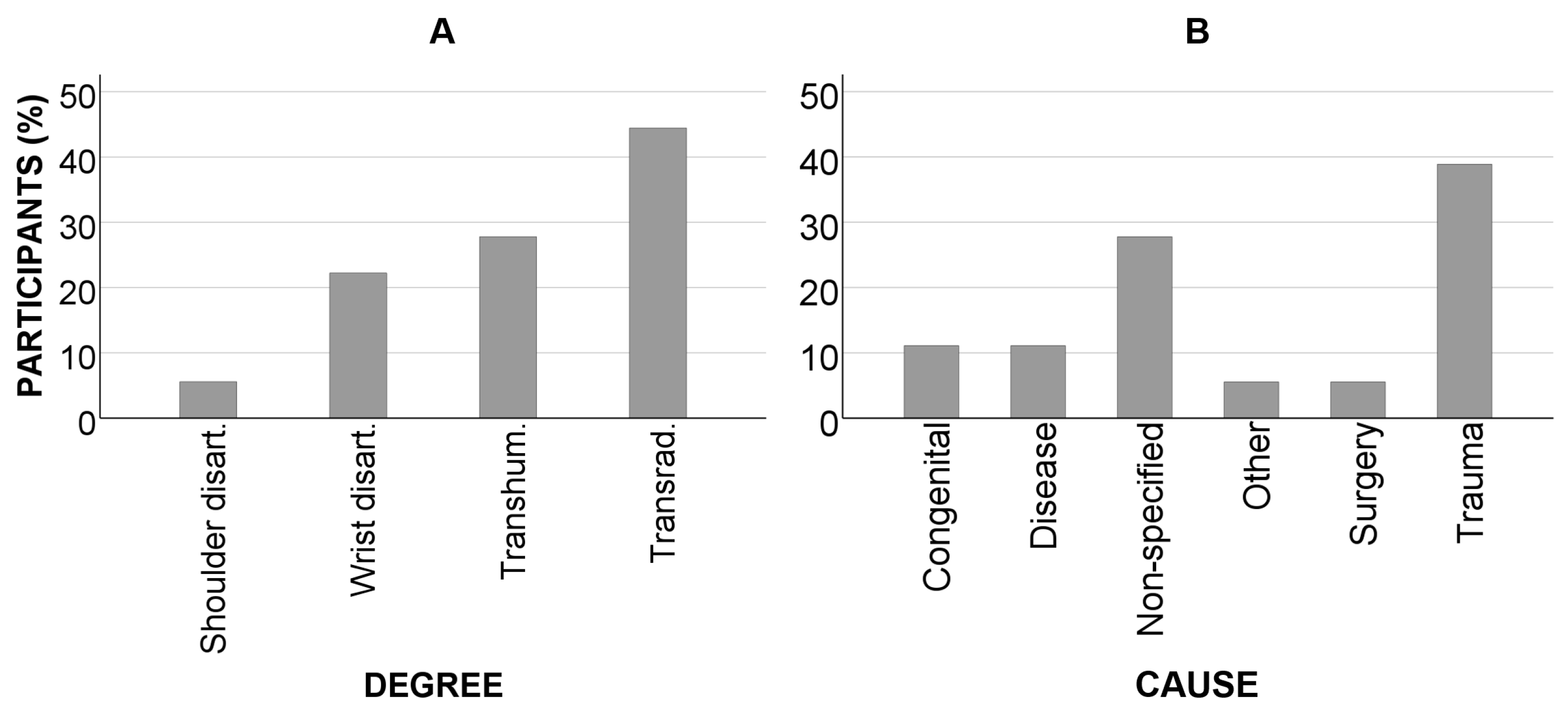
3.1. Sample Data
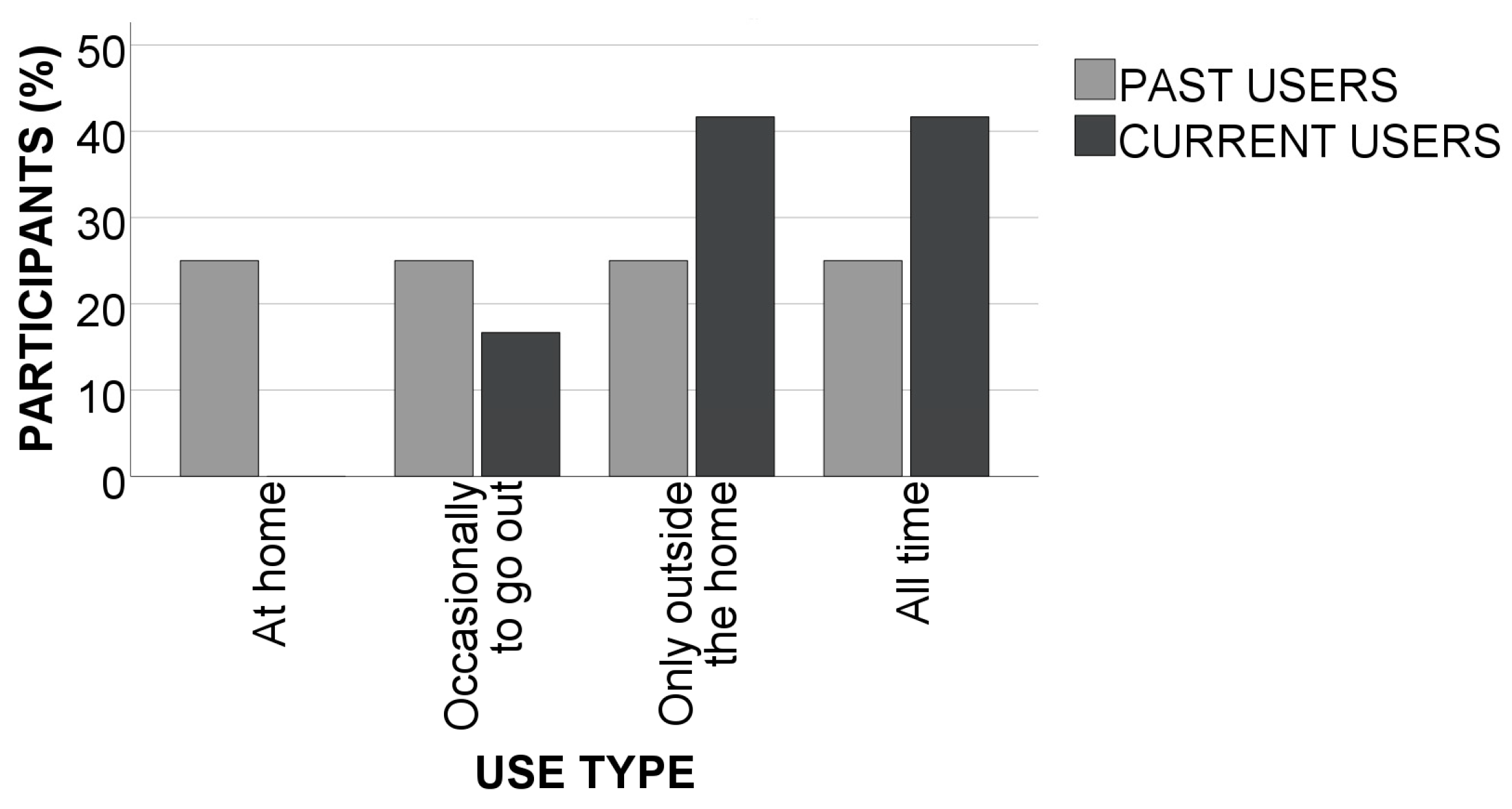
3.2. Prosthetic Use
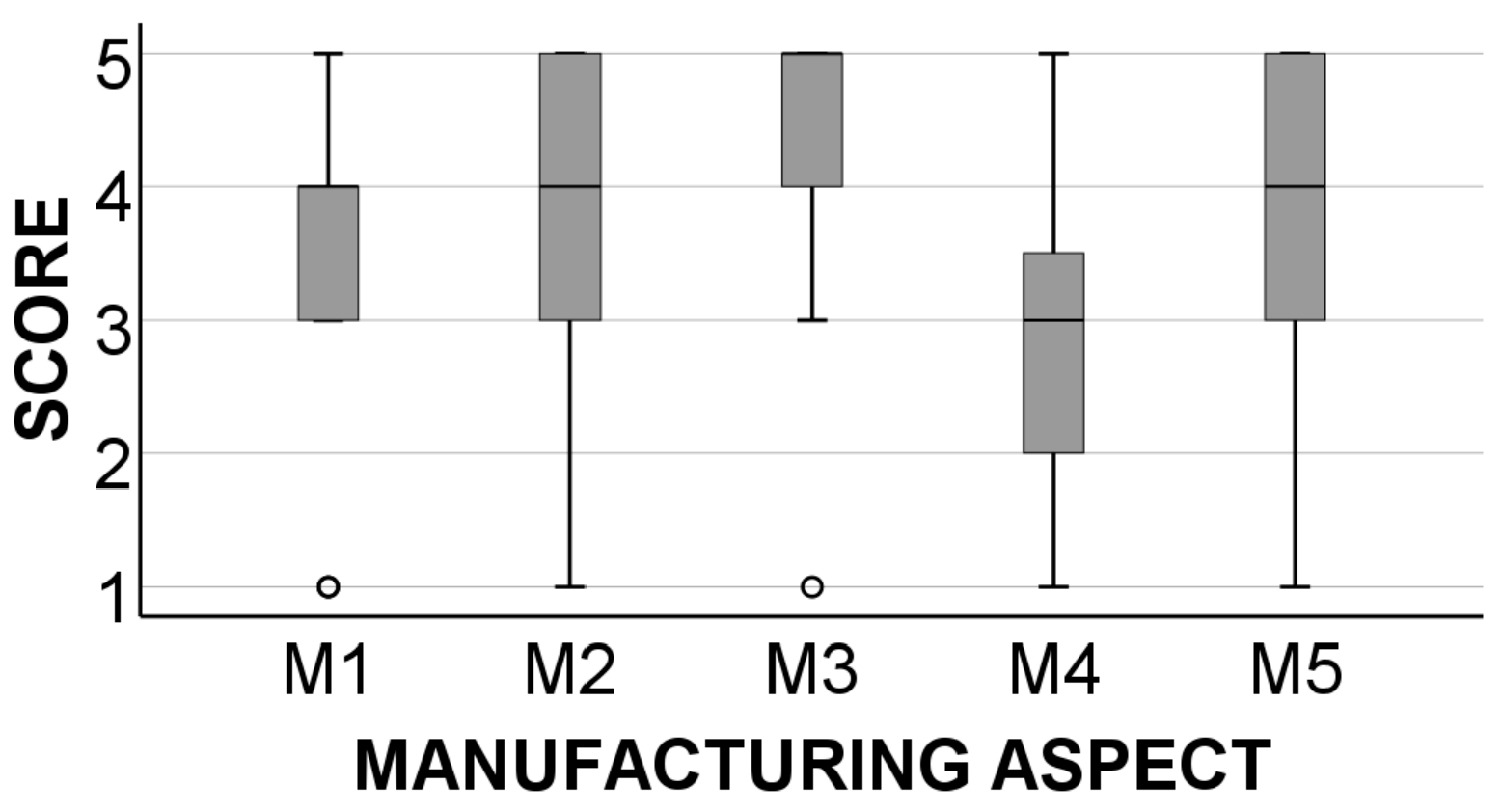
3.3. Manufacturing Aspects
3.4. Comfort Aspects
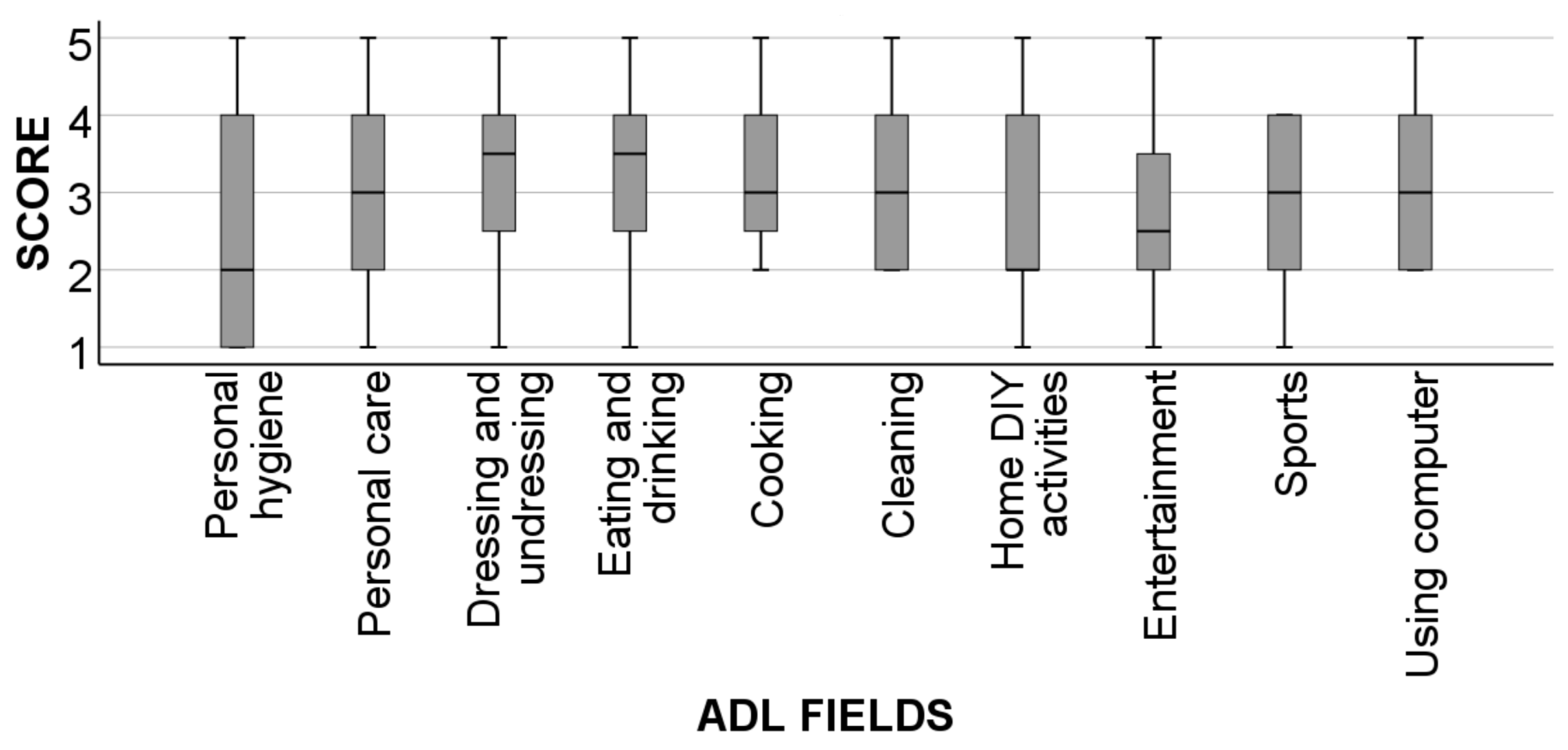
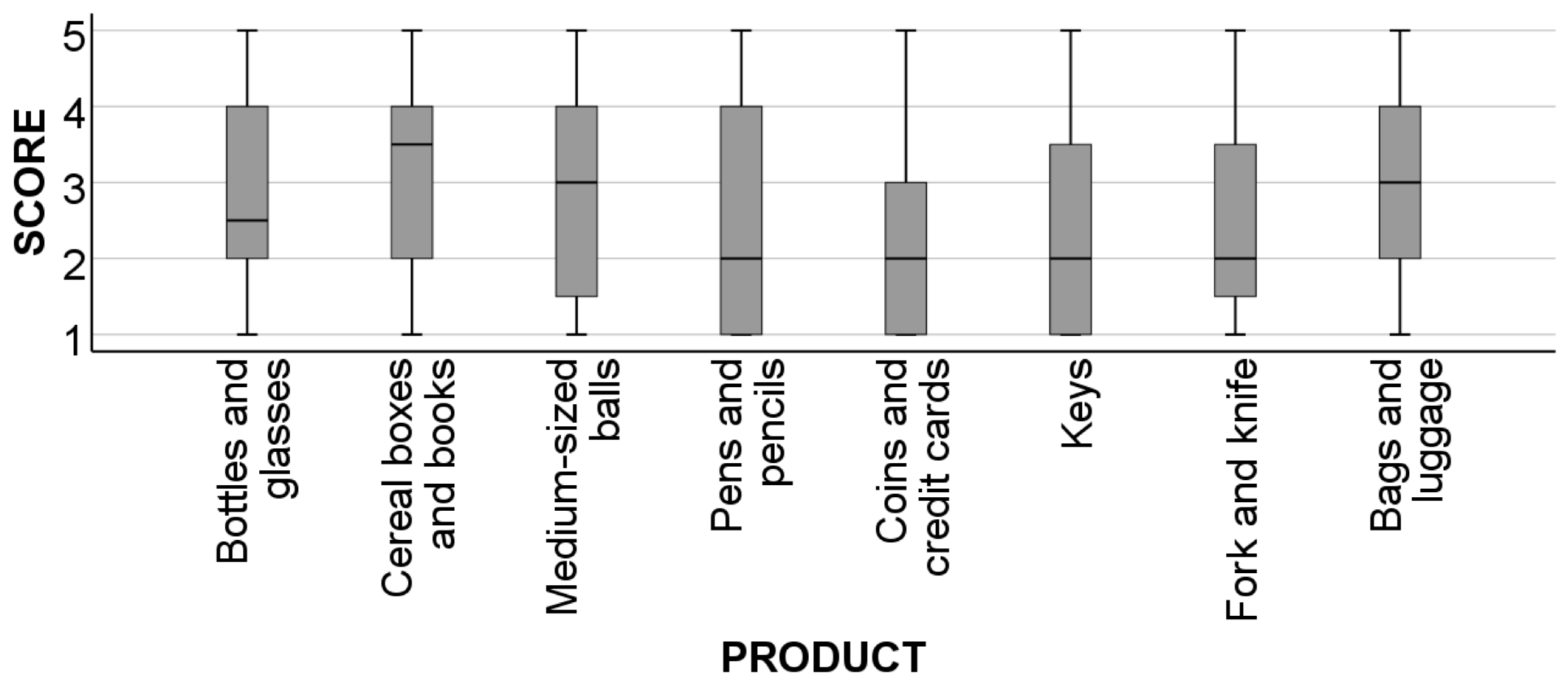
3.5. Functionality Aspects
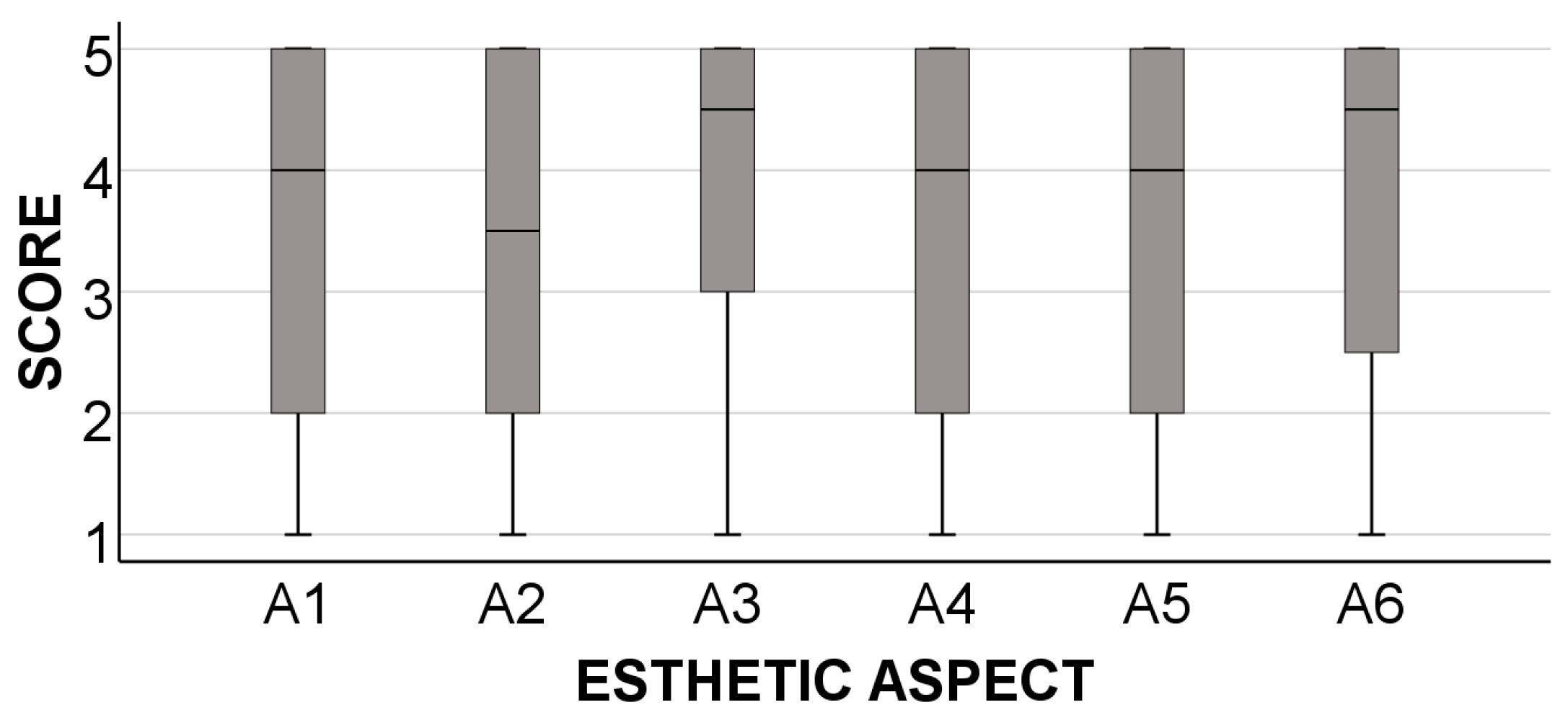
3.6. Esthetic Aspects
3.7. Durability and Cost
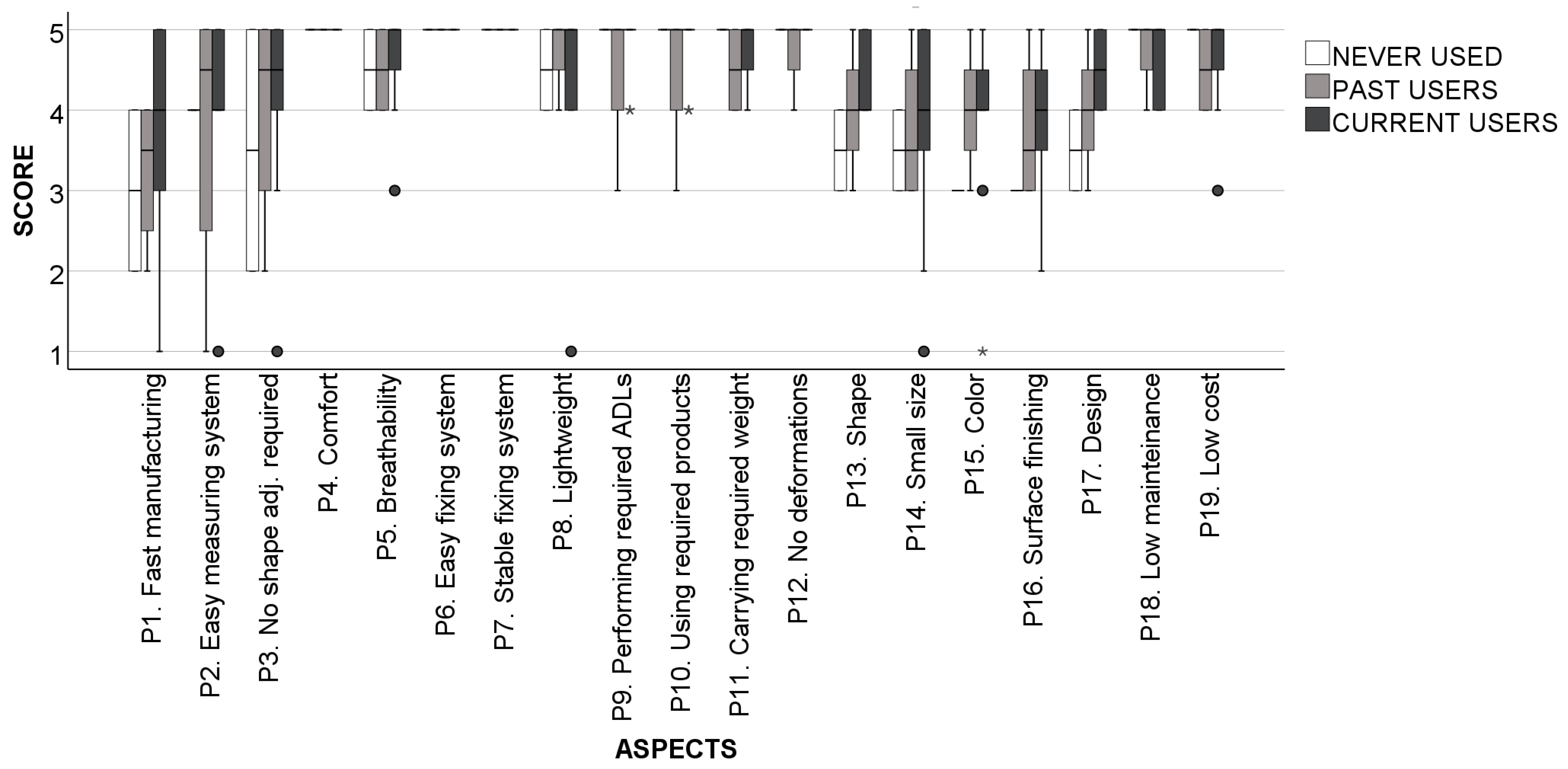
3.8. Importance of Specific Socket Properties
4. Discussion
4.1. Sample Data
4.2. Prosthetic Use
4.3. Manufacturing
4.4. Comfort
4.5. Functionality
4.6. Esthetics
4.7. Durability and Cost
4.8. Importance of Specific Socket Properties
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Academies of Sciences Engineering and Medicine. Chapter 4: Upper-Extremity Prostheses. In The Promise of Assistive Technology to Enhance Activity and Work Participation; Jette, A.M., Spicer, C.M., Flaubert, J.L., Eds.; National Academies Press: Washington, DC, USA, 2017; ISBN 978-0-309-45784-2. [Google Scholar]
- Kejlaa, G.H. Consumer concerns and the functional value of prostheses to upper limb amputees. Prosthet. Orthot. Int. 1993, 17, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Biddiss, E.; Chau, T. Upper-Limb Prosthetics: Critical factors in device abandonment. Am. J. Phys. Med. Rehabil. 2007, 86, 977–987. [Google Scholar] [CrossRef] [PubMed]
- Biddiss, E.A.; Chau, T.T. Upper limb prosthesis use and abandonment. Prosthet. Orthot. Int. 2007, 31, 236–257. [Google Scholar] [CrossRef]
- Daly, W.; Voo, L.; Rosenbaum-Chou, T.; Arabian, A.; Boone, D. Socket pressure and discomfort in upper-limb prostheses: A preliminary study. J. Prosthet. Orthot. 2014, 26, 99–106. [Google Scholar] [CrossRef]
- Ghoseiri, K.; Safari, M.R. Prevalence of heat and perspiration discomfort inside prostheses: Literature review. J. Rehabil. Res. Dev. 2014, 51, 855–867. [Google Scholar] [CrossRef] [PubMed]
- Dudkiewicz, I.; Gabrielov, R.; Seiv-Ner, I.; Zelig, G.; Heim, M. Evaluation of prosthetic usage in upper limb amputees. Disabil. Rehabil. 2004, 26, 60–63. [Google Scholar] [CrossRef] [PubMed]
- Burger, H. Marinček Upper limb prosthetic use in Slovenia. Prosthet. Orthot. Int. 1994, 18, 25–33. [Google Scholar] [CrossRef]
- Afzal, S.; Altaf, M.; Fatima, N.; Bukhari, B.; Nasir, M.; Khan, S. Skin problems of amputees using upper limb prosthesis. Rawal Med. J. 2022, 47, 53–55. [Google Scholar]
- Baumgartner, B.L. Design of an Adjustable Temporary Socket for a Transradial Prosthesis. Ph.D. Thesis, Technische Universität Wien, Vienna, Austria, 2022. [Google Scholar]
- Gu, Y.; Yang, D.; Osborn, L.; Candrea, D.; Liu, H.; Thakor, N. An adaptive socket with auto-adjusting air bladders for interfacing transhumeral prosthesis: A pilot study. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2019, 233, 812–822. [Google Scholar] [CrossRef] [PubMed]
- Baldock, M.; Pickard, N.; Prince, M.; Kirkwood, S.; Chadwell, A.; Howard, D.; Dickinson, A.; Kenney, L.; Gill, N.; Curtin, S. Adjustable prosthetic sockets: A systematic review of industrial and research design characteristics and their justifications. J. Neuroeng. Rehabil. 2023, 20, 147. [Google Scholar] [CrossRef]
- Haggstrom, E.E.; Hansson, E.; Hagberg, K. Comparison of prosthetic costs and service between osseointegrated and conventional suspended transfemoral prostheses. Prosthet. Orthot. Int. 2013, 37, 152–160. [Google Scholar] [CrossRef]
- e-NABLE Enabling The Future Project Website. Available online: https://enablingthefuture.org/ (accessed on 25 April 2024).
- Fairley, M. The O&P Edge: 3D Printing of Upper-Limb Prosthetics: Present Reality, Future Potential. Available online: https://www.oandp.com/articles/2015-11_01.asp (accessed on 1 January 2024).
- Rogers, B.; Bosker, G.W.; Crawford, R.H.; Faustini, M.C.; Neptune, R.R.; Walden, G.; Gitter, A.J. Advanced trans-tibial socket fabrication using selective laser sintering. Prosthet. Orthot. Int. 2007, 31, 88–100. [Google Scholar] [CrossRef]
- ISO 10328:2016; Prosthetic Structural Testing of Lowerlimb Prostheses Requirements and Test Methods. International Organization for Standardization: Geneva, Switzerland, 2016.
- Mio, R.; Sanchez, M.; Valverde, Q.; Lara, J.; Rumiche, F. Mechanical testing methods for body-powered upper-limb prostheses: A case study. Adv. Sci. Technol. Eng. Syst. 2019, 4, 61–68. [Google Scholar] [CrossRef]
- Ismail, R.; Taqriban, R.B.; Ariyanto, M.; Atmaja, A.T.; Sugiyanto; Caesarendra, W.; Glowacz, A.; Irfan, M.; Glowacz, W. Affordable and Faster Transradial Prosthetic Socket Production Using Photogrammetry and 3D Printing. Electronics 2020, 9, 1456. [Google Scholar] [CrossRef]
- Olsen, J.; Day, S.; Dupan, S.; Nazarpour, K.; Dyson, M. 3D-Printing and Upper-Limb Prosthetic Sockets: Promises and Pitfalls. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 527–535. [Google Scholar] [CrossRef]
- Sang, Y.; Li, X.; Gan, Y.; Su, D.; Luo, Y. A novel socket design for upper-limb prosthesis. Int. J. Appl. Electromagn. Mech. 2014, 45, 881–886. [Google Scholar] [CrossRef]
- Górski, F.; Wichniarek, R.; Kuczko, W.; Żukowska, M. Study on properties of automatically designed 3D-printed customized prosthetic sockets. Materials 2021, 14, 5240. [Google Scholar] [CrossRef]
- Taqriban, R.B.; Ismail, R.; Ariyanto, M.; Putra, A.F.Y.S. 3D Model of Photogrammetry Technique for Transtibial Prosthetic Socket Design Development. In Proceedings of the 2019 2nd International Seminar on Research of Information Technology and Intelligent Systems, ISRITI 2019, Yogyakarta, Indonesia, 5–6 December 2019; pp. 456–461. [Google Scholar] [CrossRef]
- Norman, D.; Draper, S. User Centered System Design: New Perspectives on Human-Computer Interaction; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1985. [Google Scholar]
- Bispo, R.; Branco, V. Designing out Stigma: The Potential of Contradictory Symbolic Imagery. In Proceedings of the 5th International Conference on Inclusive Design (Include ‘09), London, UK, 5–8 April 2009; pp. 532–537. [Google Scholar]
- Parette, P.; Scherer, M. Assistive Technology Use and Stigma. Educ. Train. Dev. Disabil. 2004, 39, 217–226. [Google Scholar]
- Schröppel, T.; Miehling, J.; Wartzack, S. The role of product development in the battle against product-related stigma—A literature review. J. Eng. Des. 2021, 32, 247–270. [Google Scholar] [CrossRef]
- Crandall, C.S.; Coleman, R. Aids-Related Stigmatization and the Disruption of Social Relationships. J. Soc. Pers. Relatsh. 1992, 9, 163–177. [Google Scholar] [CrossRef]
- Norman, D.A. Emotional Design: Why We Love (or Hate) Everyday Things; Basic Books: New York, NY, USA, 2004; ISBN 13-9780465051359. [Google Scholar]
- Jefferies, P.; Gallagher, P.; Philbin, M. Being “just normal”: A grounded theory of prosthesis use. Disabil. Rehabil. 2018, 40, 1754–1763. [Google Scholar] [CrossRef] [PubMed]
- Truijen, S.; Saeys, W.; Haring, E.; Feys, H.; Meyvis, E.; Van den Eynde, A.; Vaes, K.; van Breda, E.; Schaerlaken, E.; Verwulgen, S. The Design of the Paediatric Prosthesis: Assessment of Stigma-Inducing Factors in Primary School Children, Using a Questionnaire. In Advances in Intelligent Systems and Computing; Springer: Cham, Switzerland, 2020; pp. 869–881. [Google Scholar]
- Copeland, C.; Reyes, C.C.; Peck, J.L.; Srivastava, R.; Zuniga, J.M. Functional performance and patient satisfaction comparison between a 3D printed and a standard transradial prosthesis: A case report. Biomed. Eng. Online 2022, 21, 7. [Google Scholar] [CrossRef] [PubMed]
- Demers, L.; Weiss-Lambrou, R.; Ska, B. Development of the Quebec User Evaluation of Satisfaction with assistive Technology (QUEST). Assist. Technol. 1996, 8, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Jarl, G.M.; Heinemann, A.W.; Norling Hermansson, L.M. Validity evidence for a modified version of the Orthotics and Prosthetics Users’ Survey. Disabil. Rehabil. Assist. Technol. 2012, 7, 469–478. [Google Scholar] [CrossRef] [PubMed]
- Manero, A.; Sparkman, J.; Dombrowski, M.; Smith, P.; Senthil, P.; Smith, S.; Rivera, V.; Chi, A. Evolving 3D-Printing Strategies for Structural and Cosmetic Components in Upper Limb Prosthesis. Prosthesis 2023, 5, 167–181. [Google Scholar] [CrossRef]
- Galati, M.; Minetola, P.; Marchiandi, G.; Atzeni, E.; Calignano, F.; Salmi, A.; Iuliano, L. A methodology for evaluating the aesthetic quality of 3D printed parts. Procedia CIRP 2019, 79, 95–100. [Google Scholar] [CrossRef]
- Galati, M.; Minetola, P. On the measure of the aesthetic quality of 3D printed plastic parts. Int. J. Interact. Des. Manuf. 2020, 14, 381–392. [Google Scholar] [CrossRef]
- Biddiss, E.; Chau, T. The roles of predisposing characteristics, established need, and enabling resources on upper extremity prosthesis use and abandonment. Disabil. Rehabil. Assist. Technol. 2007, 2, 71–84. [Google Scholar] [CrossRef] [PubMed]
- Schultz, A.E.; Baade, S.P.; Kuiken, T.A. Expert opinions on success factors for upper-limb prostheses. J. Rehabil. Res. Dev. 2007, 44, 483–489. [Google Scholar] [CrossRef]
- Wright, T.W.; Hagen, A.D.; Wood, M.B. Prosthetic usage in major upper extremity amputations. J. Hand Surg. Am. 1995, 20, 619–622. [Google Scholar] [CrossRef]
- Durance, J.P.; O’Shea, B.J. Upper limb amputees: A clinic profile. Disabil. Rehabil. 1988, 10, 68–72. [Google Scholar] [CrossRef]
- Ostlie, K.; Lesjø, I.M.; Franklin, R.J.; Garfelt, B.; Skjeldal, O.H.; Magnus, P. Prosthesis use in adult acquired major upper-limb amputees: Patterns of wear, prosthetic skills and the actual use of prostheses in activities of daily life. Disabil. Rehabil. Assist. Technol. 2012, 7, 479–493. [Google Scholar] [CrossRef]
- Salminger, S.; Stino, H.; Pichler, L.H.; Gstoettner, C.; Sturma, A.; Mayer, J.A.; Szivak, M.; Aszmann, O.C. Current rates of prosthetic usage in upper-limb amputees–have innovations had an impact on device acceptance? Disabil. Rehabil. 2022, 44, 3708–3713. [Google Scholar] [CrossRef]
- Dudek, N.L.; Marks, M.B.; Marshall, S.C.; Chardon, J.P. Dermatologic conditions associated with use of a lower-extremity prosthesis. Arch. Phys. Med. Rehabil. 2005, 86, 659–663. [Google Scholar] [CrossRef]
- Barnes, G.H. Skin health and stump hygiene. Artif. Limbs 1956, 3, 4–19. [Google Scholar]
- Lake, C.; Supan, T.J. The Incidence of Dermatological Problems in the Silicone Suspension Sleeve User. J. Prosthet. Orthot. 1997, 9, 97–106. [Google Scholar] [CrossRef]
- Huff, E.A.; Ledoux, W.R.; Berge, J.S.; Klute, G.K. Measuring Residual Limb Skin Temperatures at the Skin-Prosthesis Interface. JPO J. Prosthet. Orthot. 2008, 20, 170–173. [Google Scholar] [CrossRef]
- Makin, T.; London Plasticity Lab. Phantom Limbs and Brain Plasticity in Amputees. In Oxford Research Encyclopedia of Neuroscience; Oxford University Press: Oxford, UK, 2020. [Google Scholar]
- Jordan, P.W. Designing Pleasurable Products; CRC Press: Boca Raton, FL, USA, 2000; ISBN 9781135734114. [Google Scholar]
- Bouffard, J.; Vincent, C.; Boulianne, É.; Lajoie, S.; Mercier, C. Interactions between the phantom limb sensations, prosthesis use, and rehabilitation as seen by amputees and health professionals. J. Prosthetics Orthot. 2012, 24, 25–33. [Google Scholar] [CrossRef]






| Never Used Prosthetics (2 Participants) | Abandoned Prosthetics (4 Participants) |
|---|---|
| Learned to perform *ADLs without prosthesis | The prosthesis appeared non-functional with shoulder disarticulation; it merely served a cosmetic purpose. |
| The prosthesis appeared non-functional with a damaged brachial plexus; it merely served a cosmetic purpose and hindered the performance of ADLs rather than helping them. | |
| Rejection in childhood; learned to perform ADLs without prosthesis | The prosthesis was rejected after a period of use in childhood. The individual felt that the prosthesis restricted elbow movement. They learned to perform ADLs without the prosthesis. |
| It was abandoned after a challenging adaption period because the individual was capable of performing all ADLs without the need for a prosthesis. |
| ID | Aspect |
|---|---|
| M1 | The socket was ready in a short period of time (OPUS-S-14) |
| M2 | The residual limb morphology measurement was comfortable |
| M3 | The residual limb morphology measurement was not invasive |
| M4 | Almost no fit adjustments were required after the final shape |
| M5 | In general, I am satisfied with the socket manufacturing process |
| ID | Aspect |
|---|---|
| C1 | The socket is comfortable and does not cause any skin wound (OPUS-S-3, OPUS-S-8) |
| C2 | The socket has an appropriate weight given its characteristics (QUEST-2) |
| C3 | The socket is breathable and does not cause excess sweating |
| C4 | The socket has a good fixing system and there are no unexpected displacements. (QUEST-4) |
| C5 | The socket has a good fixing system and the motion control is not lost 1 (QUEST-4) |
| C6 | The socket does not cause pain (OPUS-S-9) |
| C7 | The process of fixing and removing the socket is comfortable (OPUS-S-4, QUEST-3) |
| C8 | In general, I am satisfied with socket comfort (QUEST-7) |
| ID | Aspect |
|---|---|
| F1 | The socket allows me to perform all the ADLs I need (OPUS-F) |
| F2 | The socket allows me to perform ADLs with all the products I need (OPUS-F) |
| F3 | The socket has enough rigidity and does not deform while performing high-stress tasks |
| F4 | In general, I am satisfied with socket functionality (OPUS-F) |
| ID | Aspect |
|---|---|
| A1 | I like the socket’s shape (OPUS-S-5) |
| A2 | The socket size is not excessive (OPUS-S-5, QUEST-1) |
| A3 | The socket color is appropriate (OPUS-S-5) |
| A4 | I like the socket surface finishing (OPUS-S-5) |
| A5 | The socket design is attractive and does not look like orthopedic (OPUS-S-5) |
| A6 | I had the chance of choosing between different socket designs (OPUS-S-15) |
| A7 | In general, I am satisfied with the socket’s appearance (OPUS-S-5) |
| ID | Properties |
|---|---|
| P1 | Fast manufacturing |
| P2 | Easy anthropometric measurement process |
| P3 | No need for shape adjustments |
| P4 | Comfort (not causing skin wounds) |
| P5 | Breathability |
| P6 | Easy fixing system |
| P7 | Stable fixing system |
| P8 | Lightweight |
| P9 | Allows me to perform the ADLs I need |
| P10 | Allows me to use the products I need |
| P11 | Allows me to carry the weight I need |
| P12 | Has enough rigidity and does not deform while performing high-stress tasks |
| P13 | Attractive shape |
| P14 | Small size |
| P15 | Appropriate color |
| P16 | Appropriate surface finishing |
| P17 | Attractive design |
| P18 | Low maintenance required |
| P19 | Low cost |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roda-Sales, A.; Llop-Harillo, I. Identifying Users’ Needs to Design and Manufacture 3D-Printed Upper Limb Sockets: A Survey-Based Study. Appl. Sci. 2024, 14, 3708. https://doi.org/10.3390/app14093708
Roda-Sales A, Llop-Harillo I. Identifying Users’ Needs to Design and Manufacture 3D-Printed Upper Limb Sockets: A Survey-Based Study. Applied Sciences. 2024; 14(9):3708. https://doi.org/10.3390/app14093708
Chicago/Turabian StyleRoda-Sales, Alba, and Immaculada Llop-Harillo. 2024. "Identifying Users’ Needs to Design and Manufacture 3D-Printed Upper Limb Sockets: A Survey-Based Study" Applied Sciences 14, no. 9: 3708. https://doi.org/10.3390/app14093708
APA StyleRoda-Sales, A., & Llop-Harillo, I. (2024). Identifying Users’ Needs to Design and Manufacture 3D-Printed Upper Limb Sockets: A Survey-Based Study. Applied Sciences, 14(9), 3708. https://doi.org/10.3390/app14093708







