Healthier Indoor Environments for Vulnerable Occupants: Analysis of Light, Air Quality, and Airborne Disease Risk
Abstract
1. Introduction
1.1. State of the Art
1.2. Motivations of the Study
2. Materials and Methods
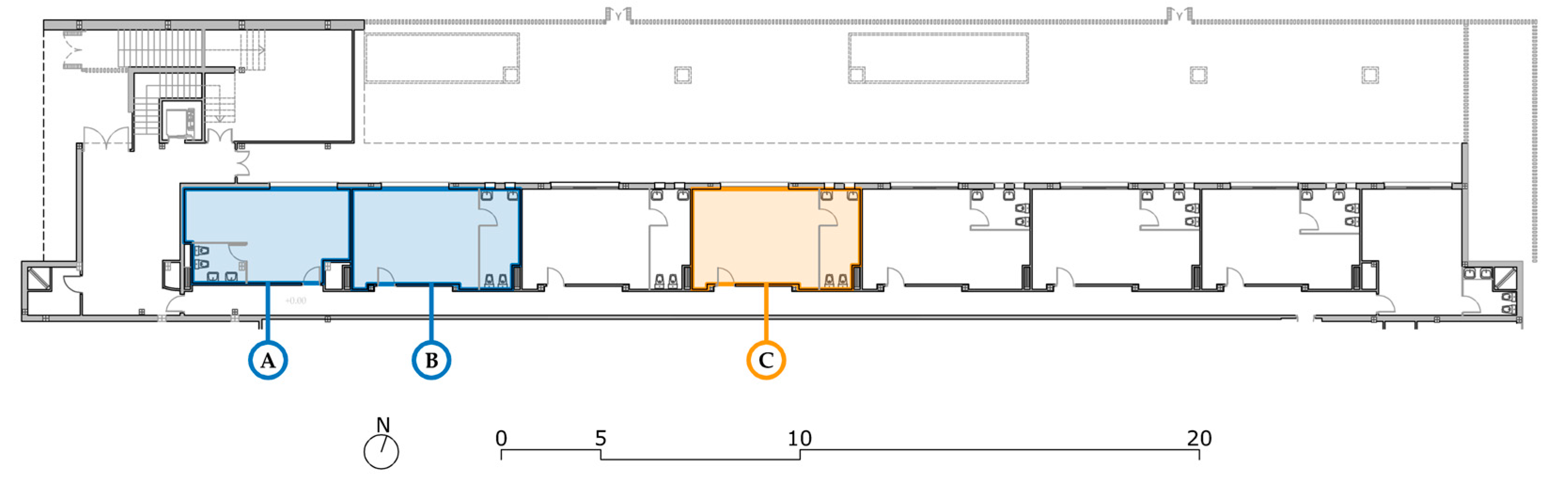
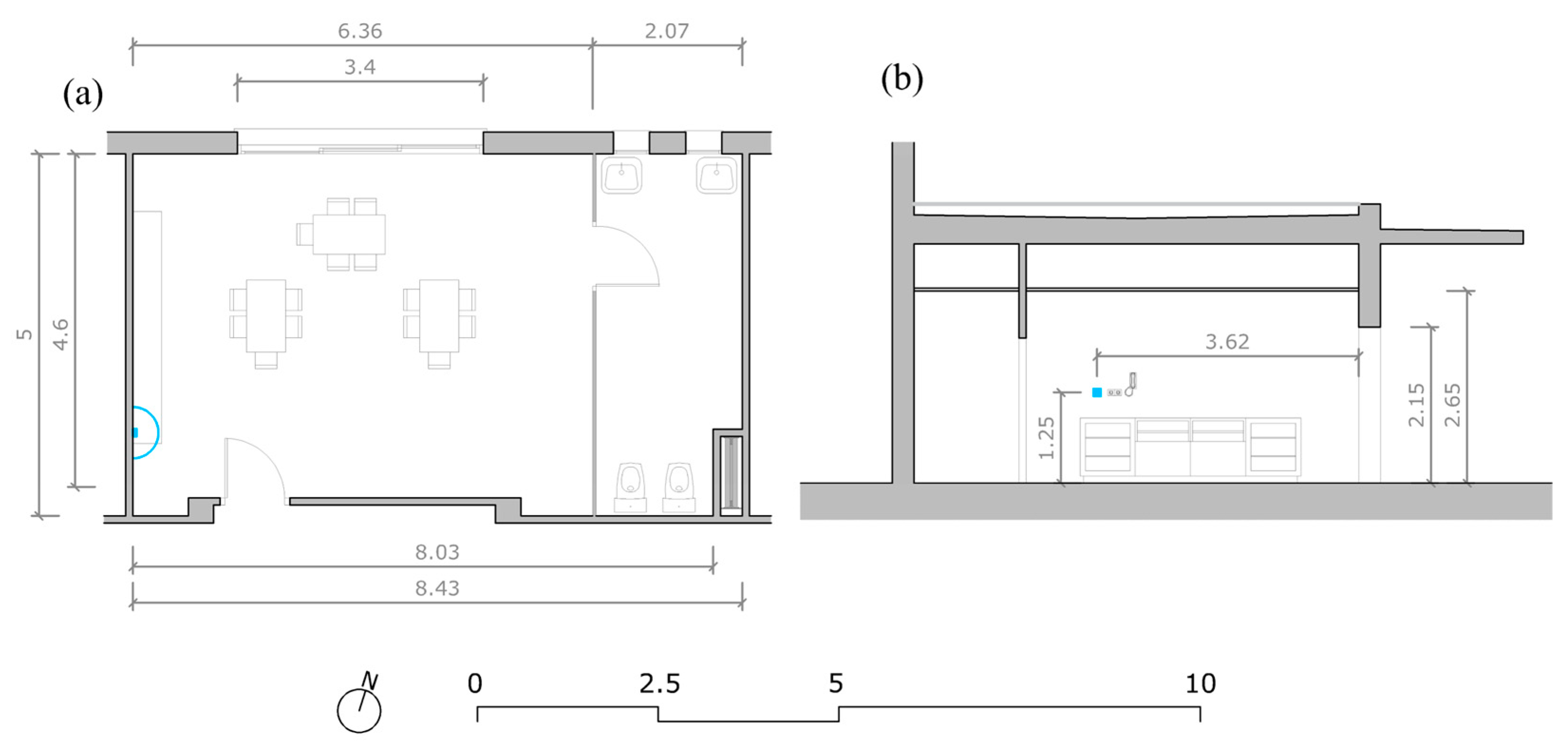
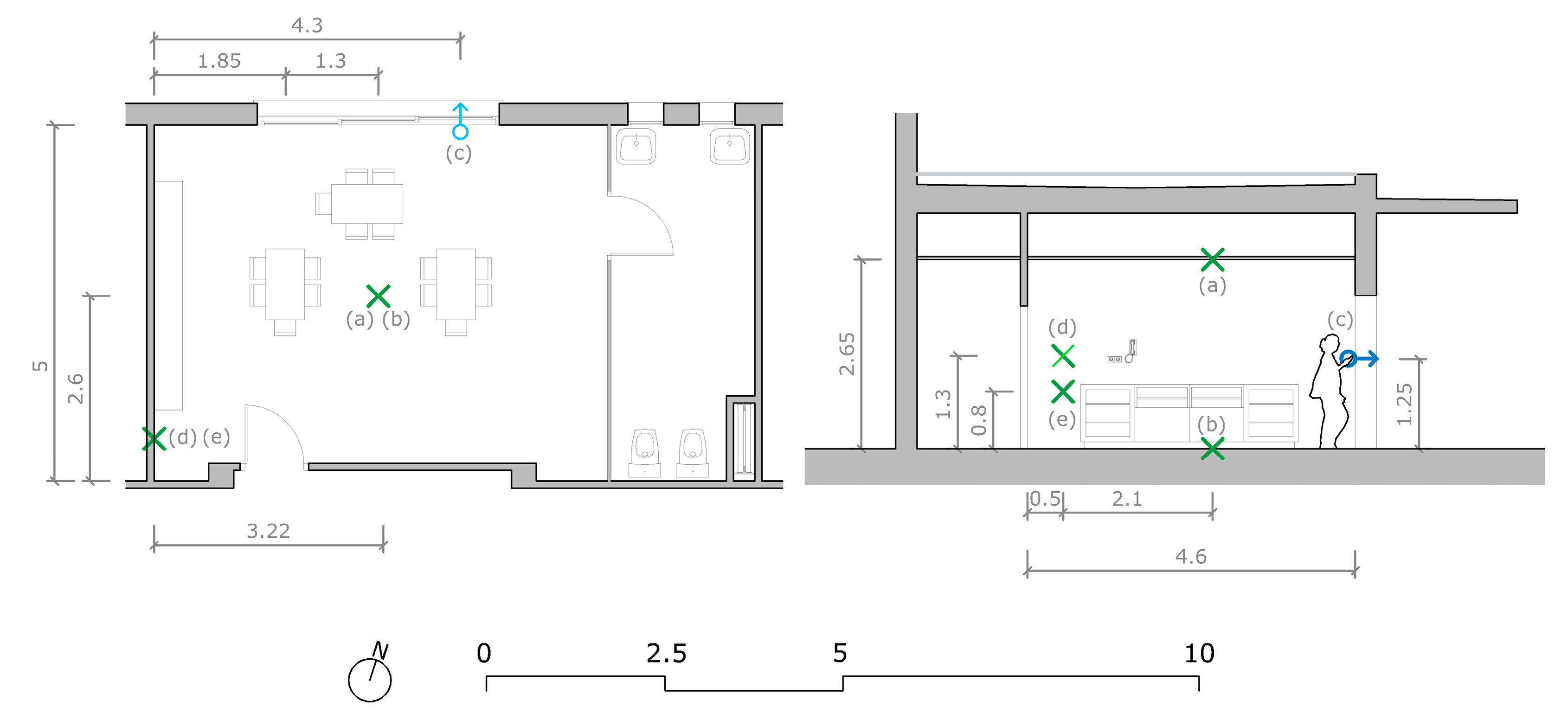
2.1. Case Study
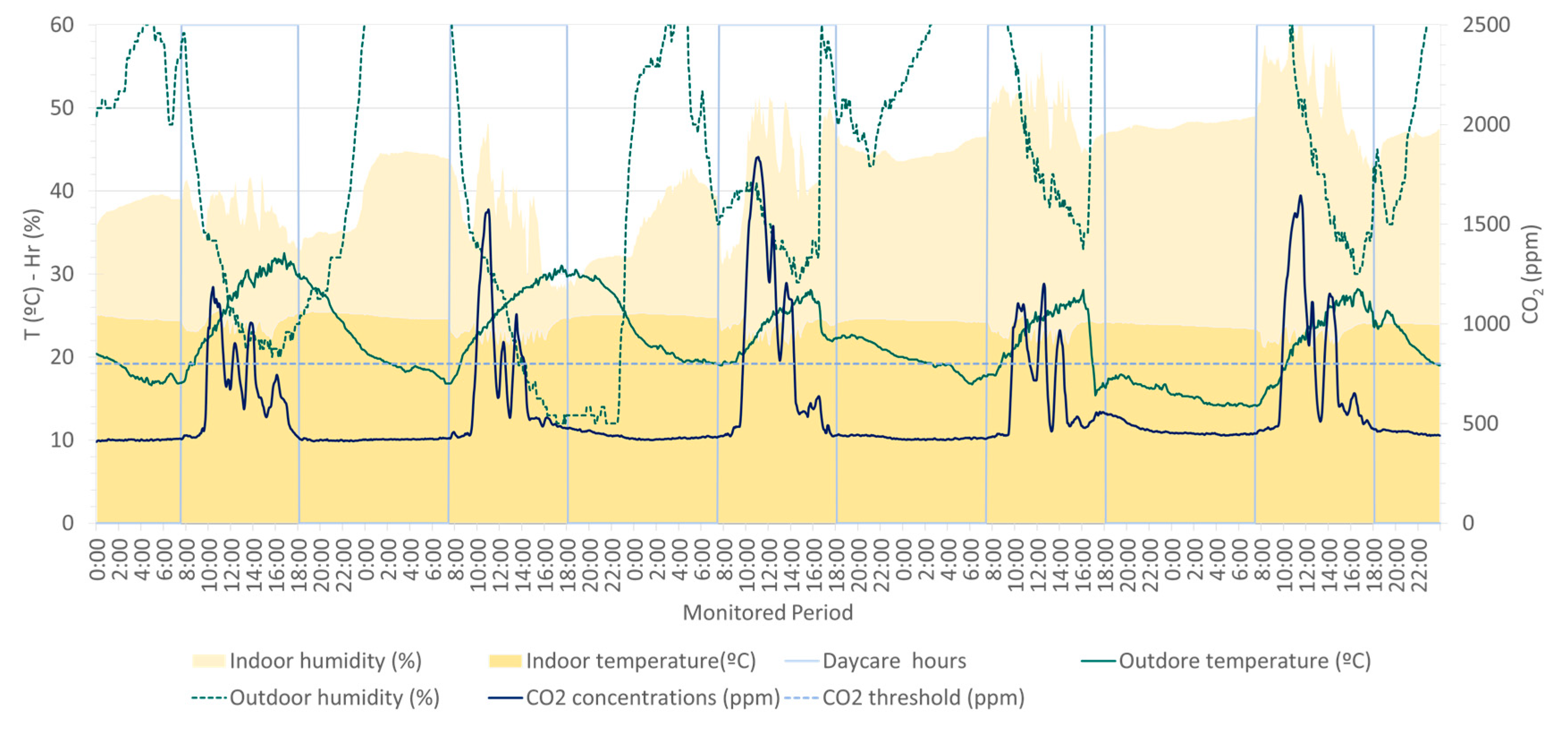
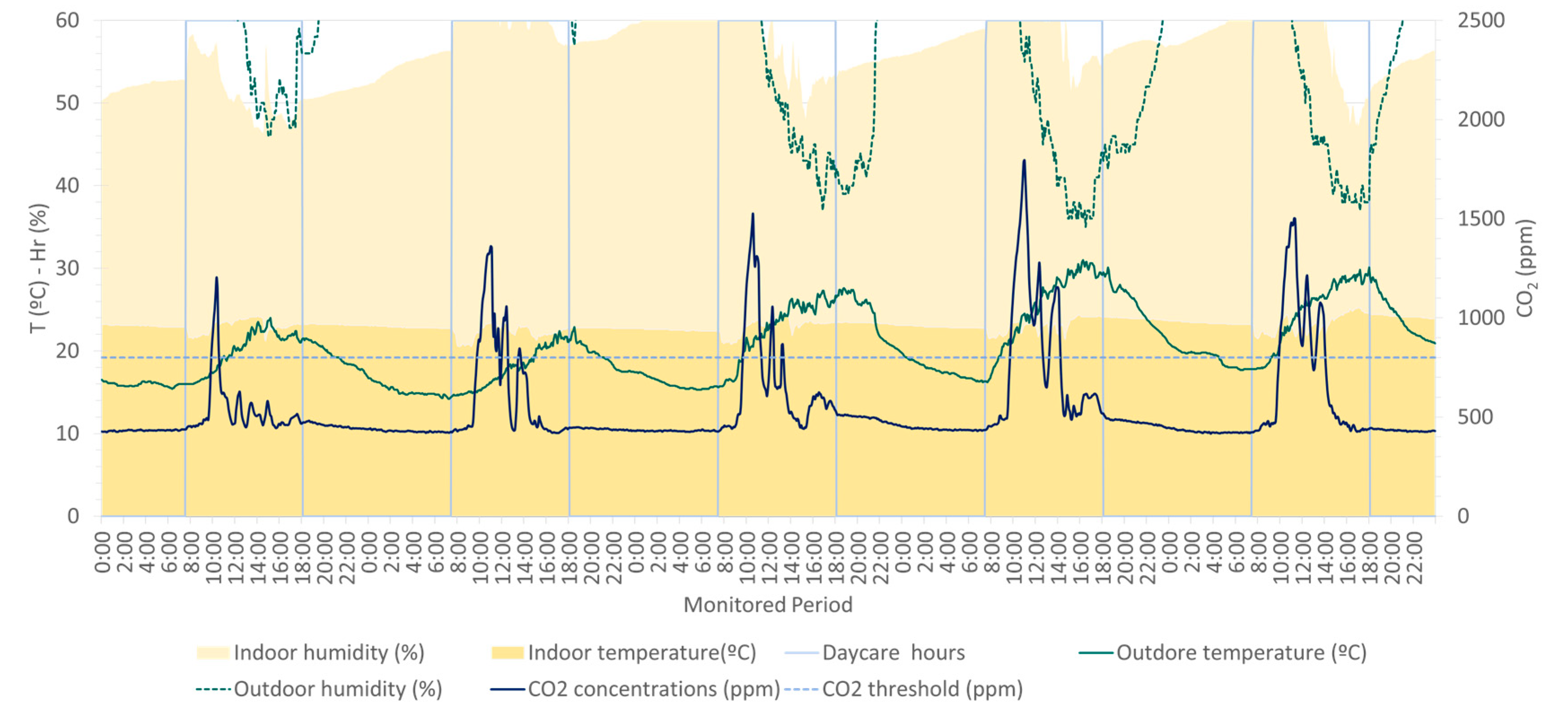
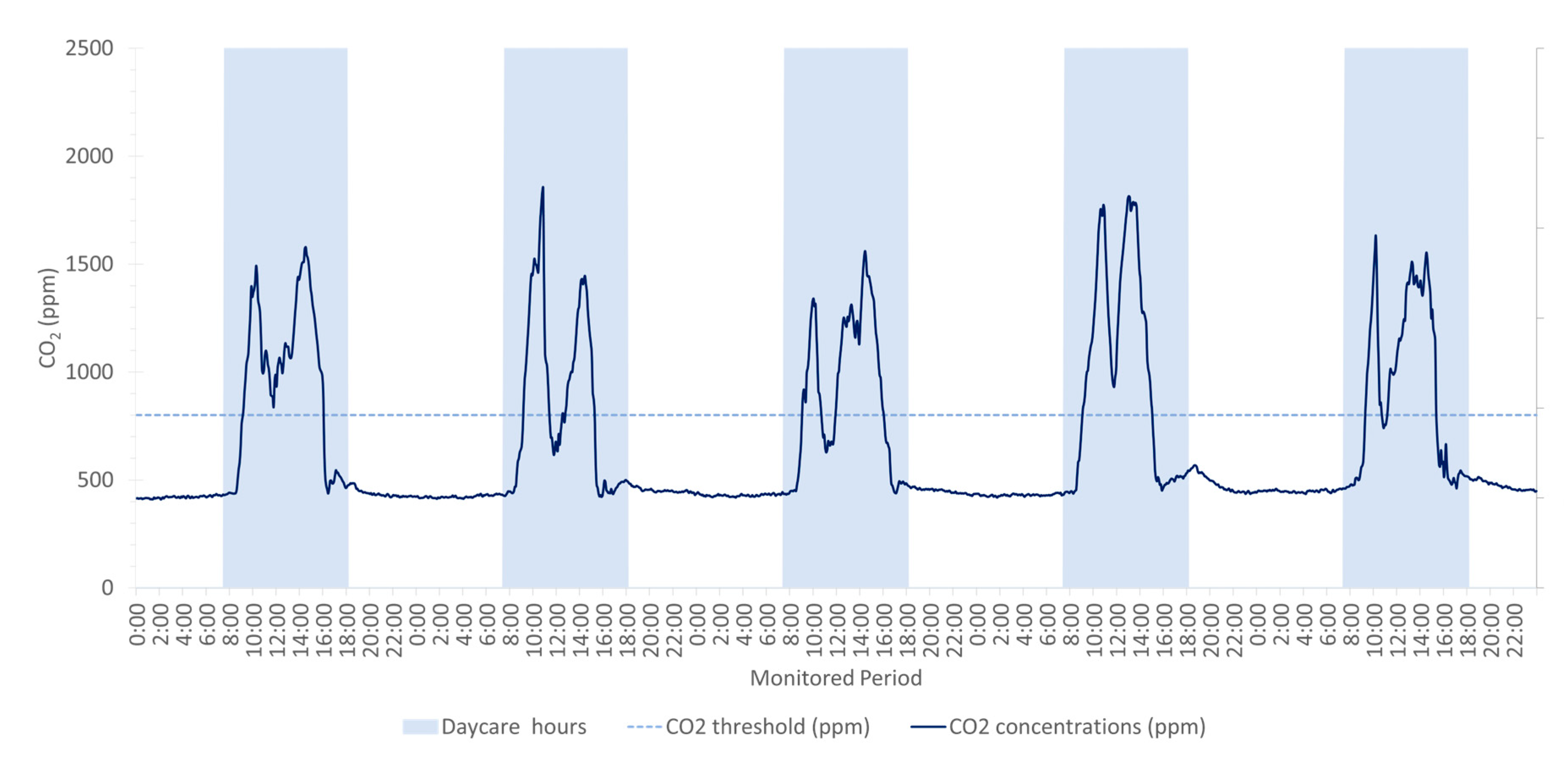
2.2. Air Quality and Thermal Comfort
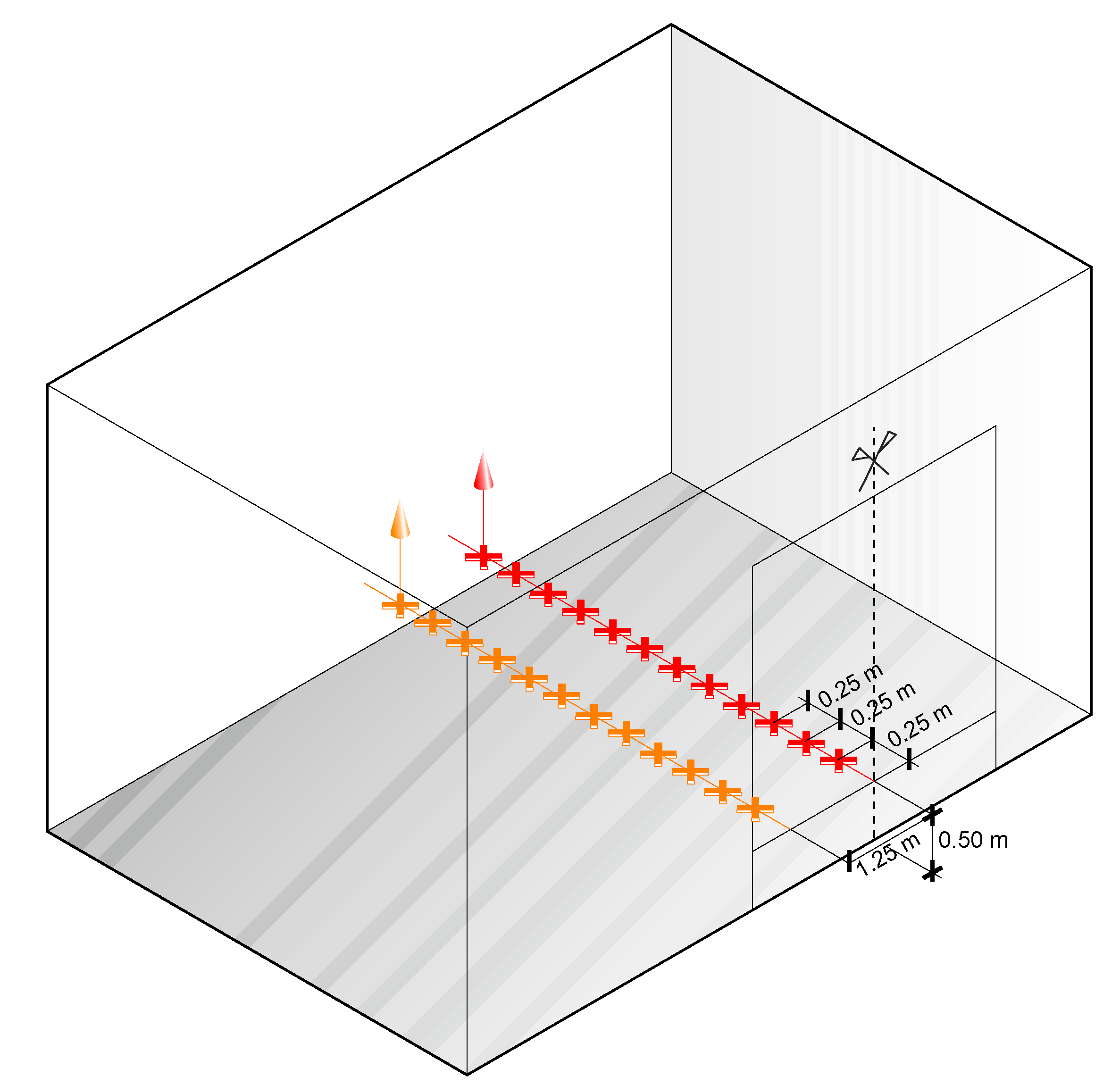
2.3. Relative Airborne Pathogen Risk Transmission
- Case 1: normal breathing, representing periods of minimal vocalization and relative quiet.
- Case 2: regular speaking, simulating typical days when infants intermittently cry, babble, or laugh.
- Case 3: loud speaking, representing scenarios with increased vocalization, which are less common given the age of the children.
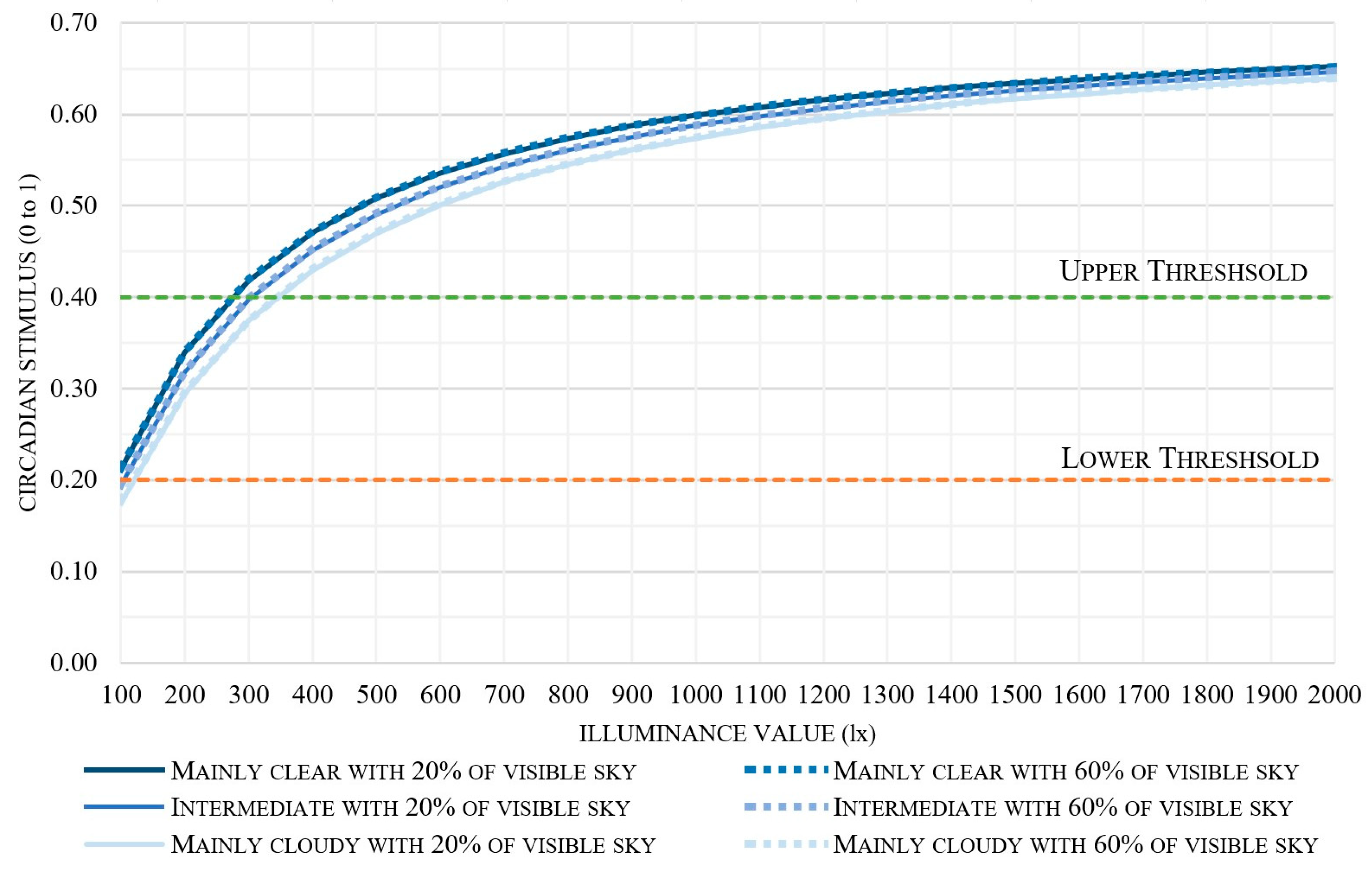
2.4. Circadian Stimulus
2.4.1. Calculation Metrics of Illumination
- Spectral sensitivity: it characterizes the spectral sensitivity of the retinal circuit, defining “circadian light” (CL) as a single, instantaneous photometric quantity.
- Empirical data: the model utilizes published psychophysical studies of nocturnal melatonin suppression using lights of different spectral power distributions.
- Neurophysiological basis: it accounts for the participation of intrinsically photosensitive retinal ganglion cells (ipRGCs), as well as rods and cones, in circadian phototransduction via neural connections in the retina.
- Spectral opponency: the model includes spectral opponent mechanisms in the distal retina that provide synaptic connections to the ipRGCs.
2.4.2. Measuring Campaign
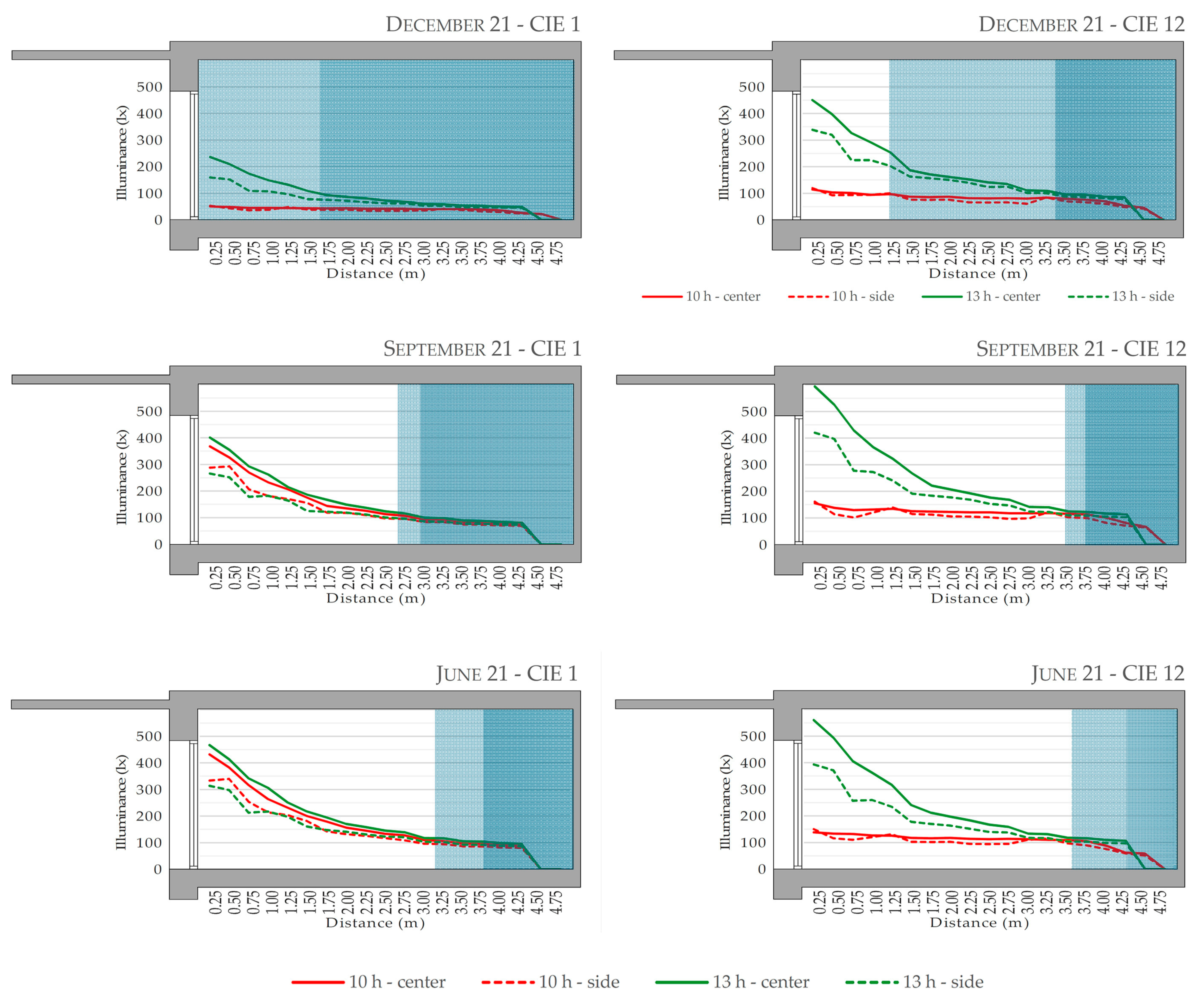
2.4.3. Virtual Model
3. Results
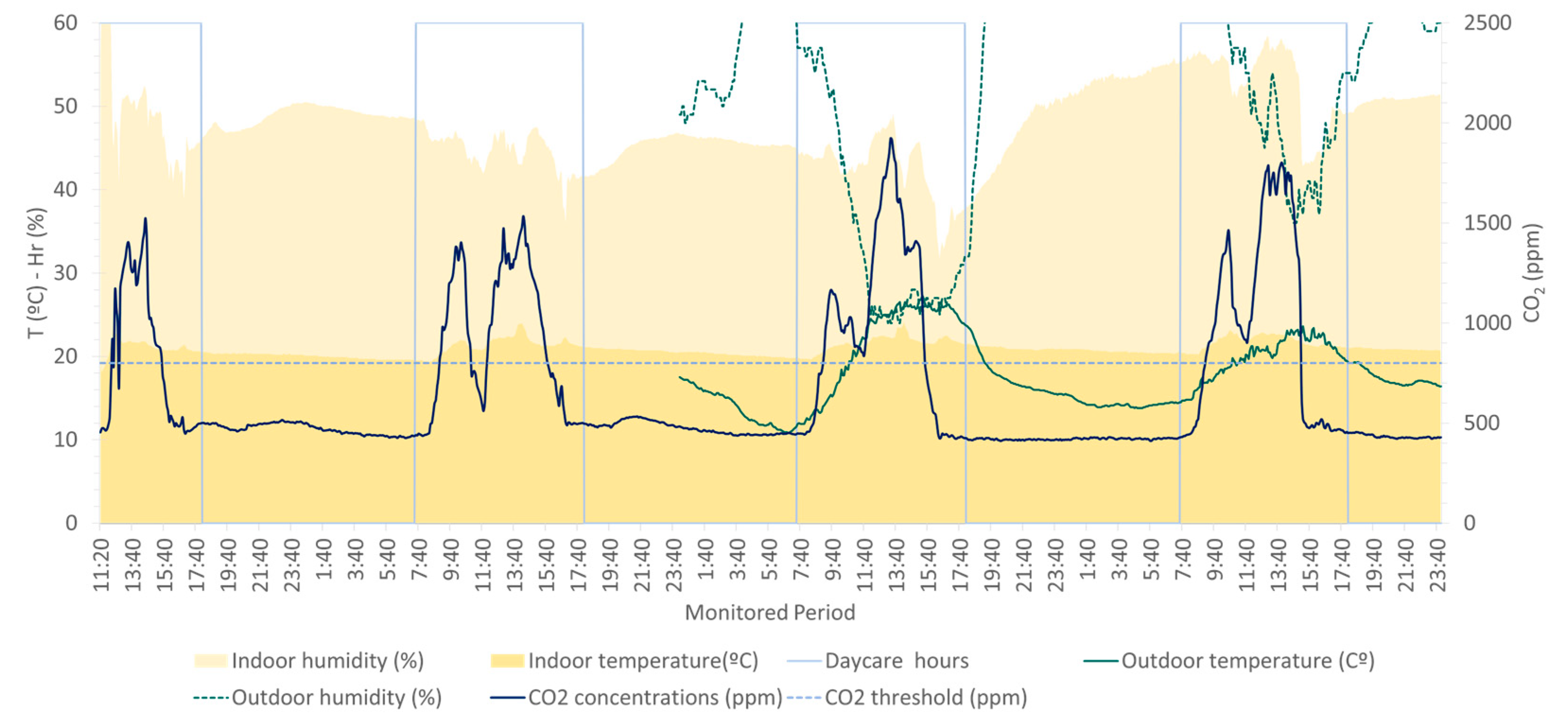
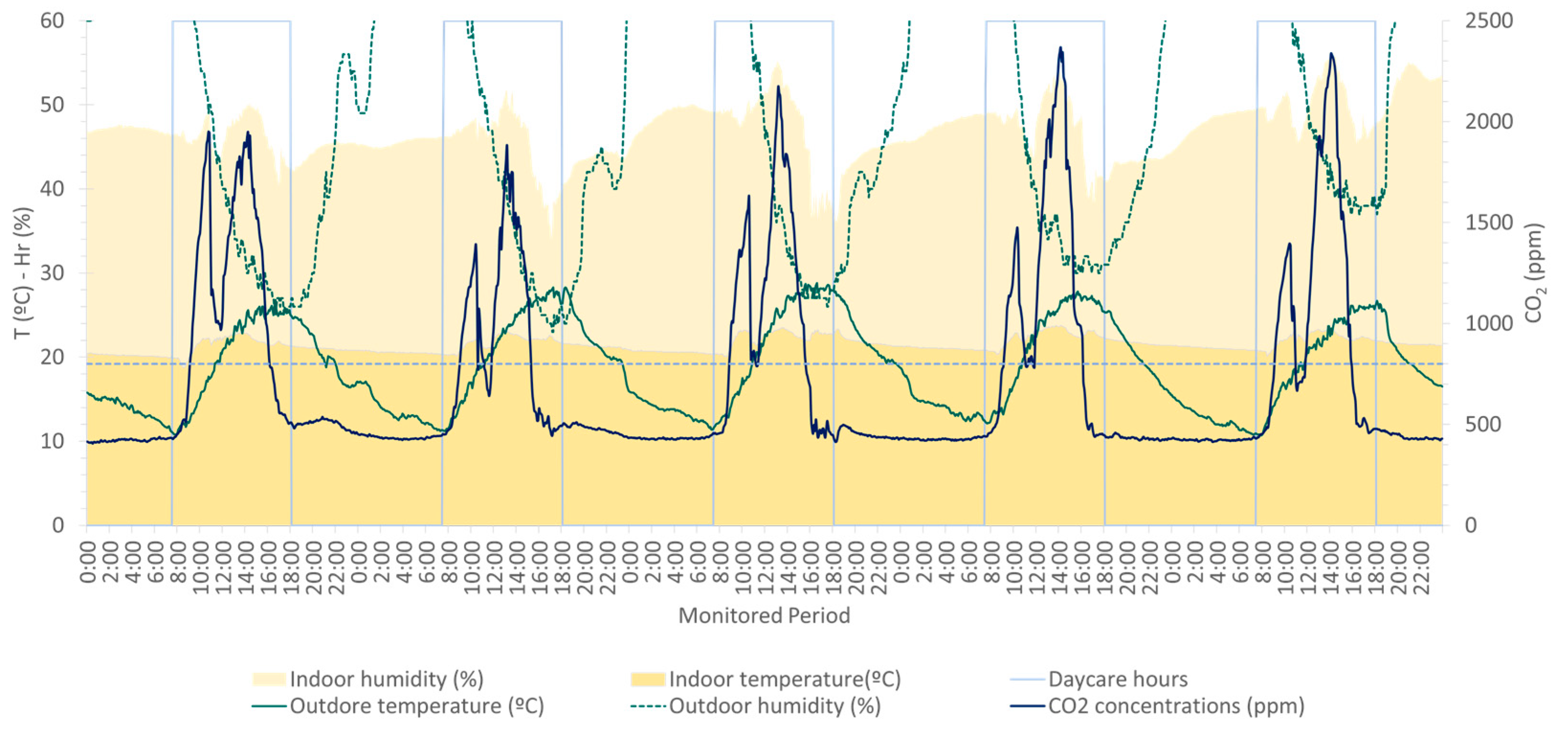
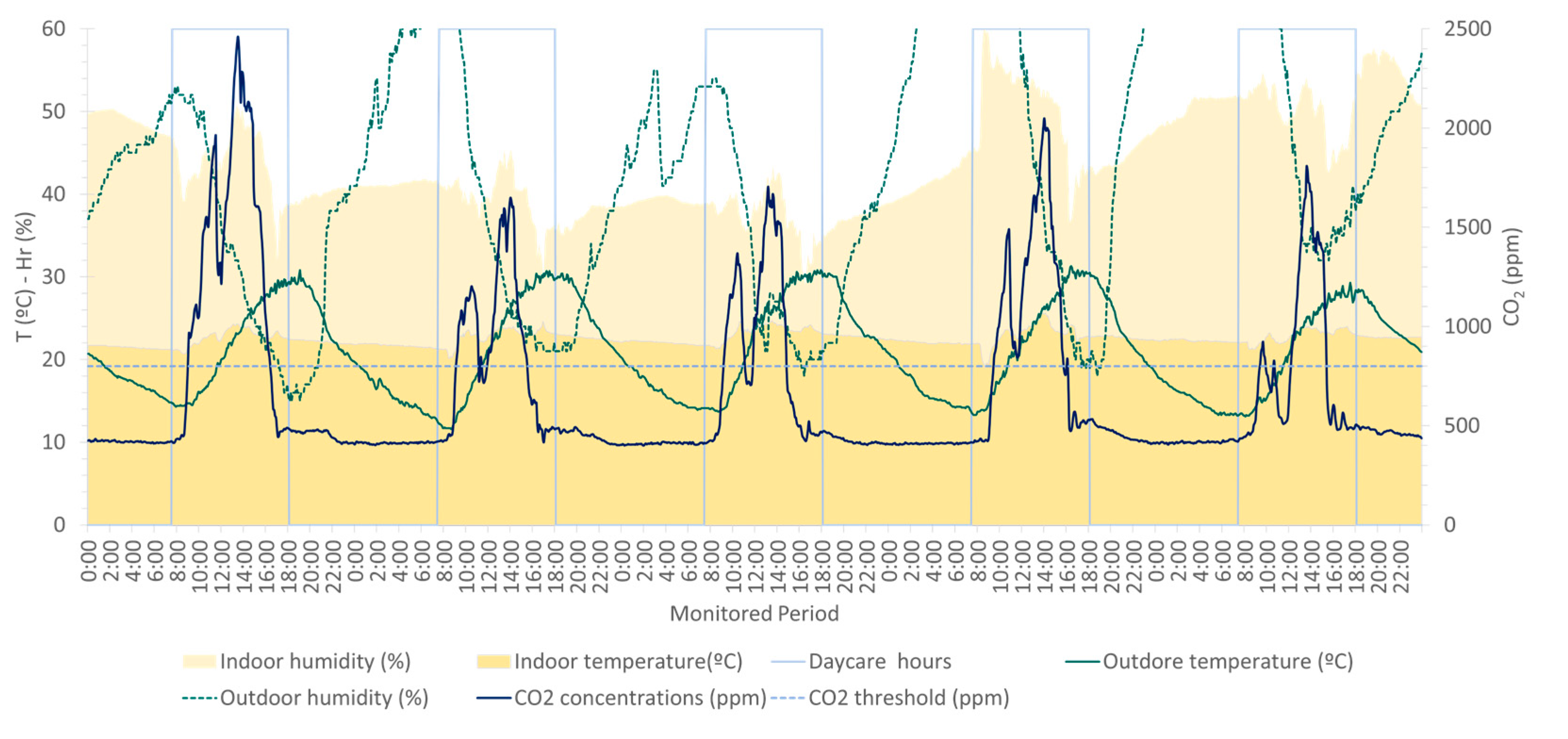
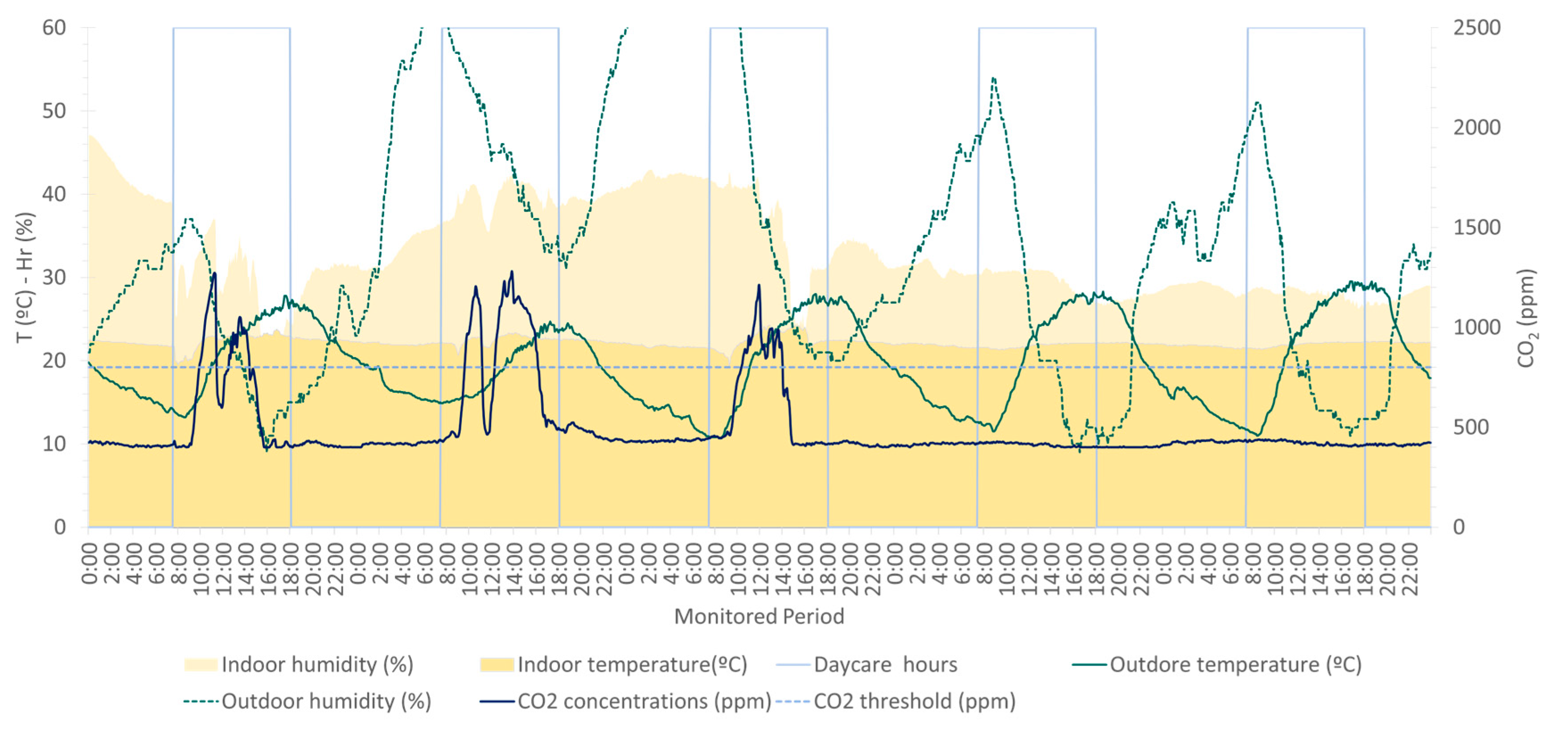
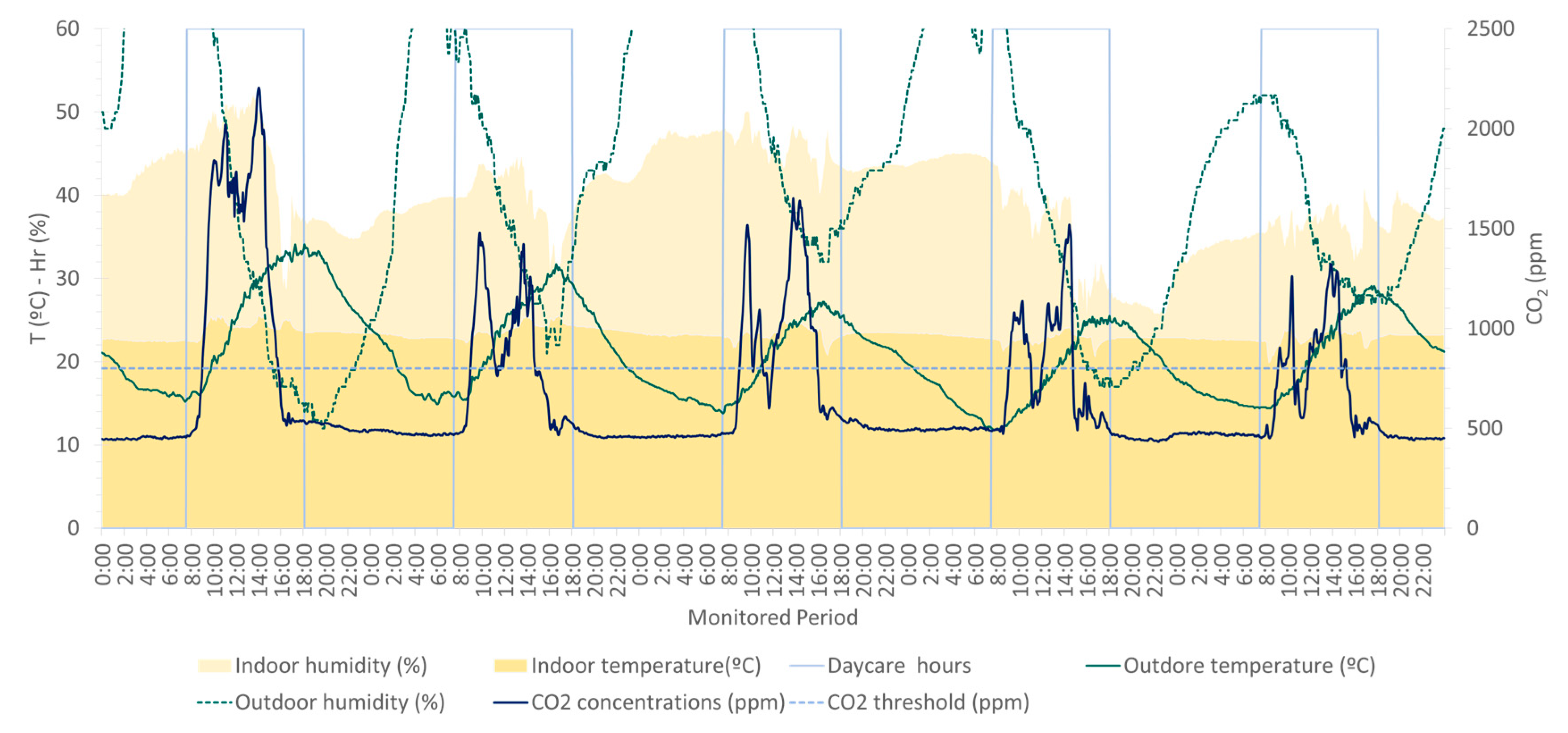
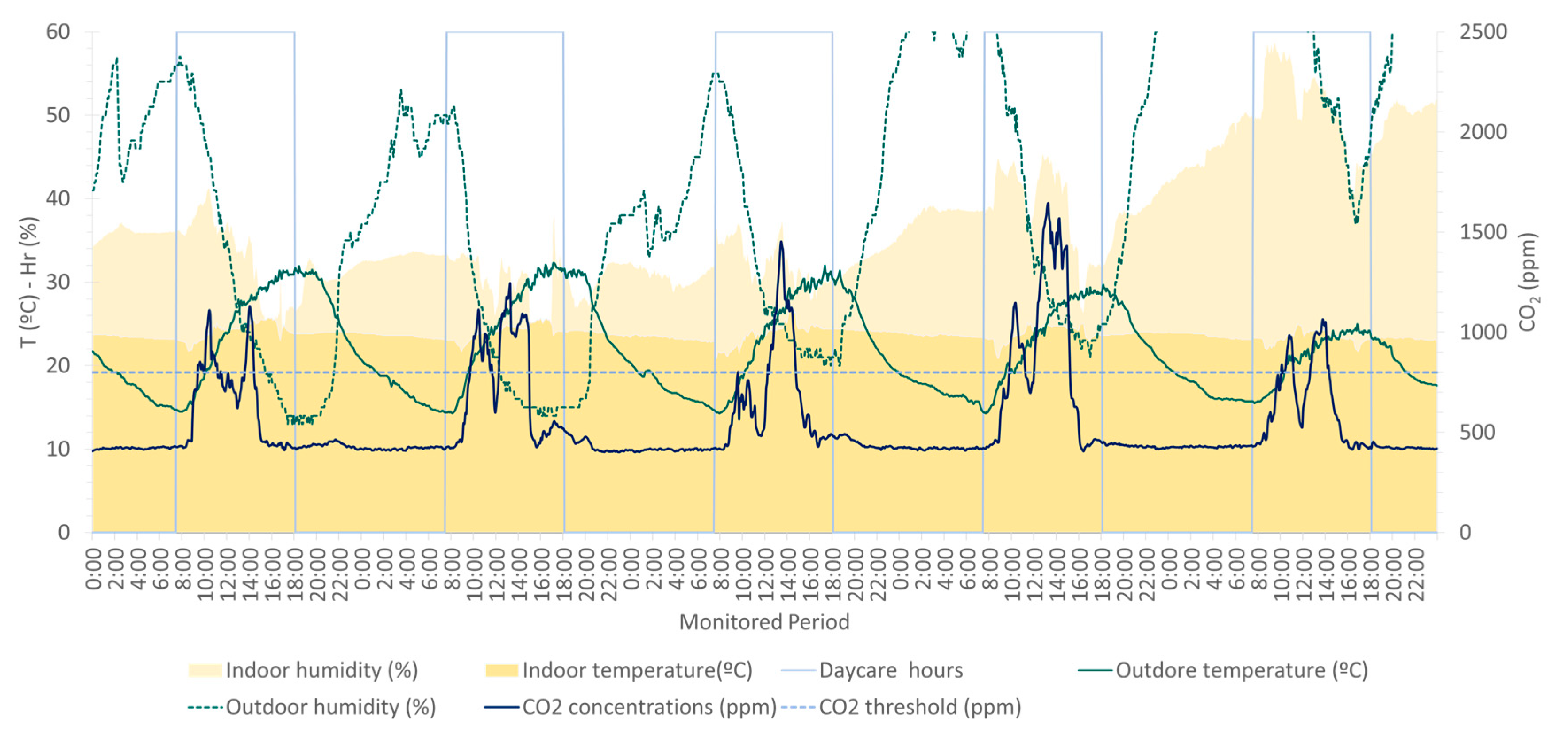
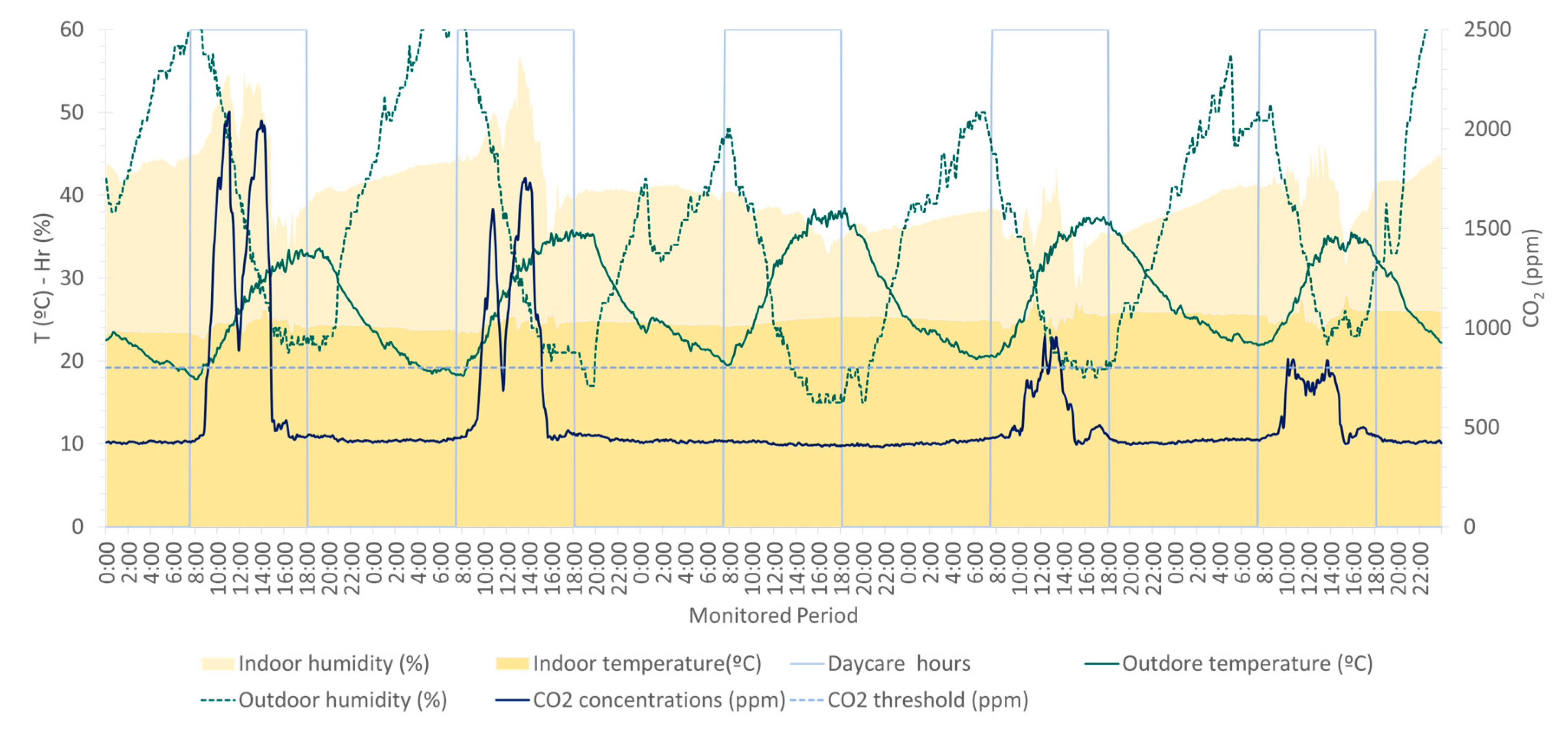
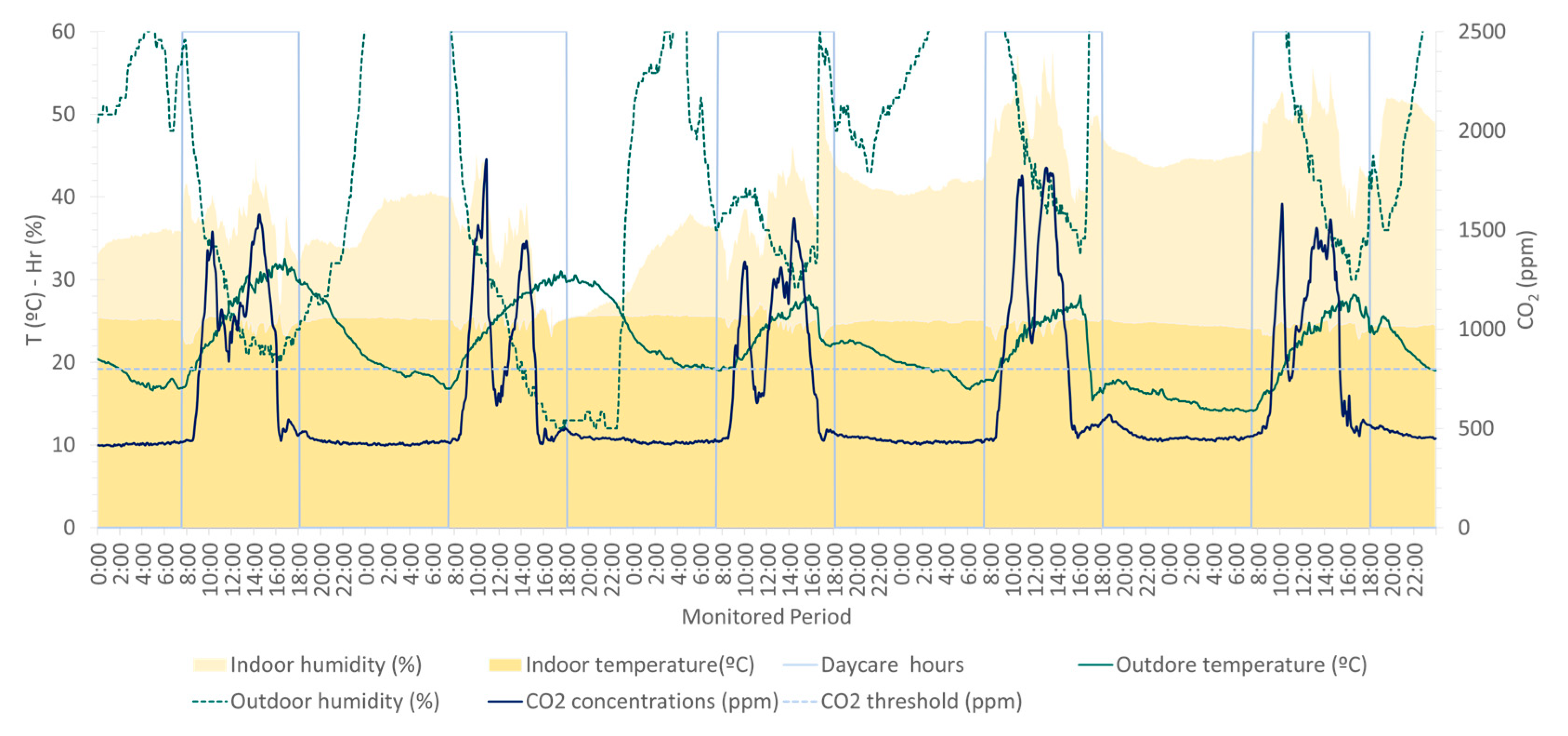
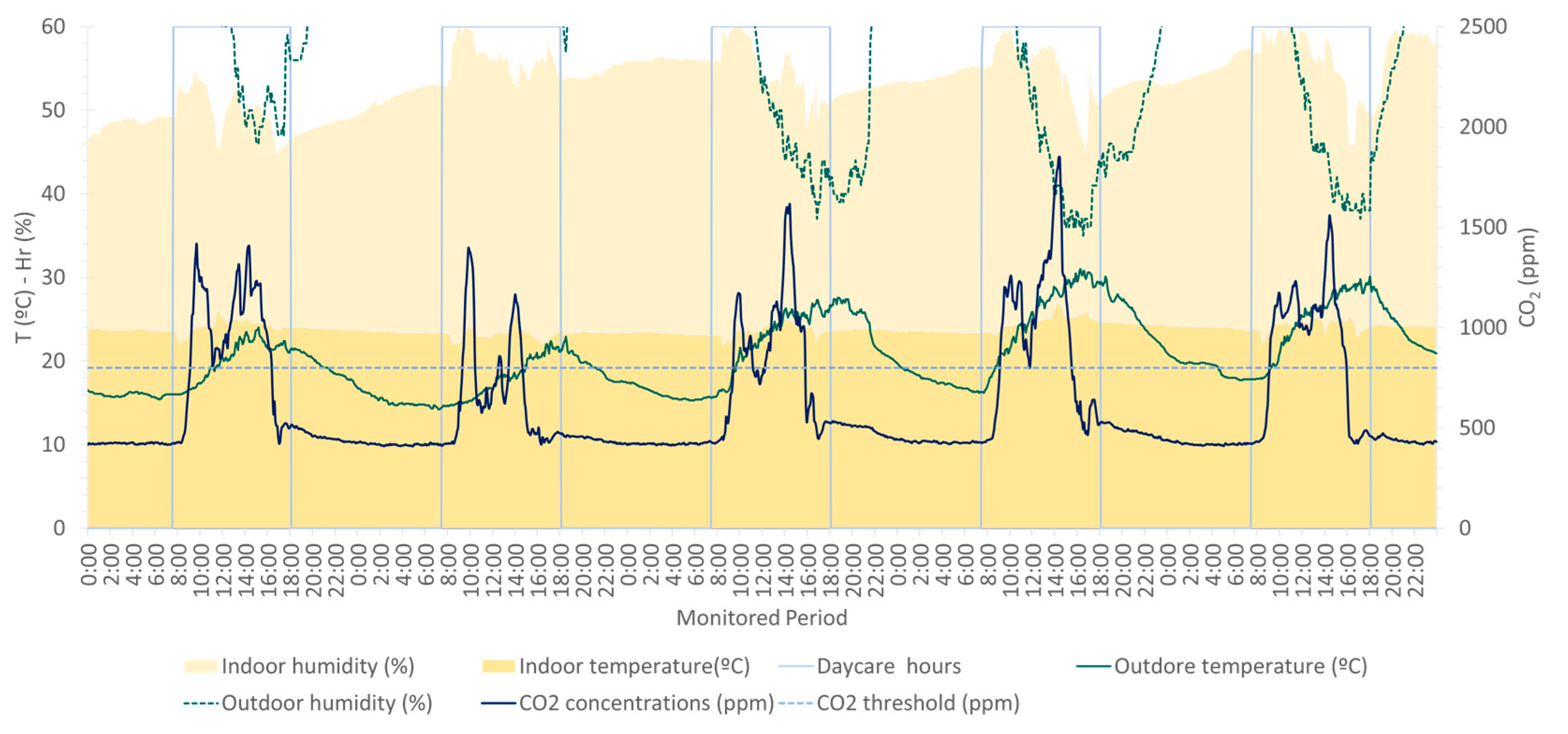
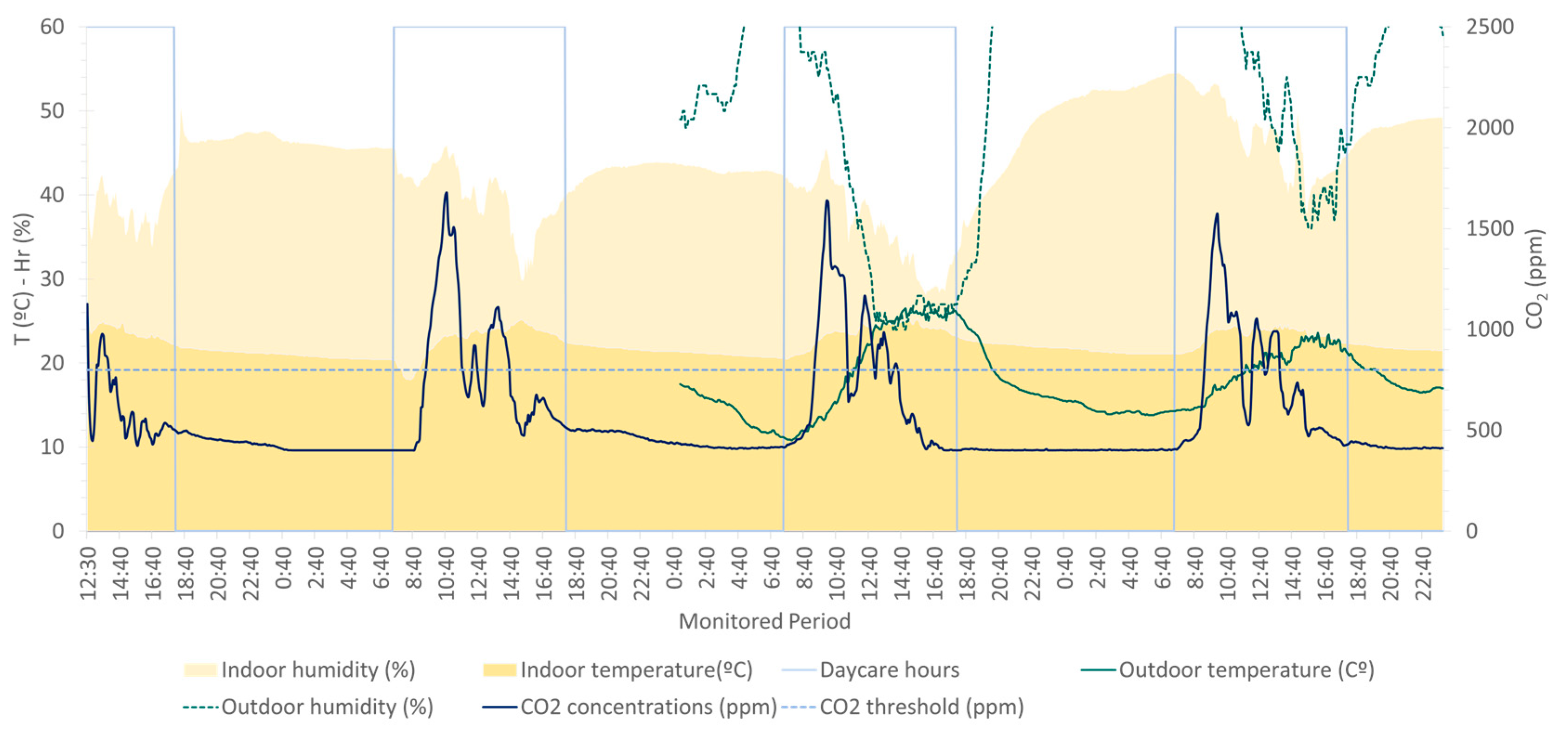
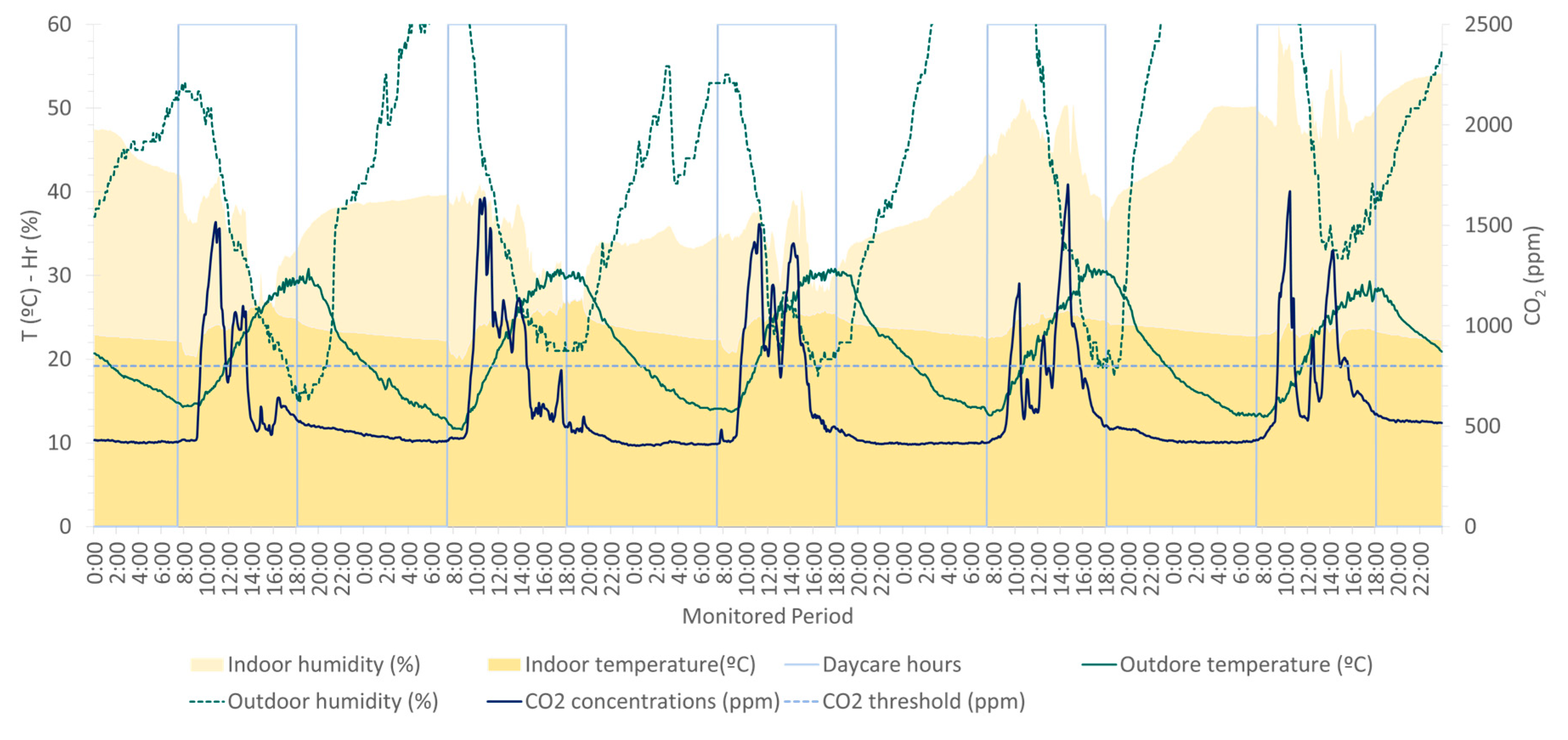
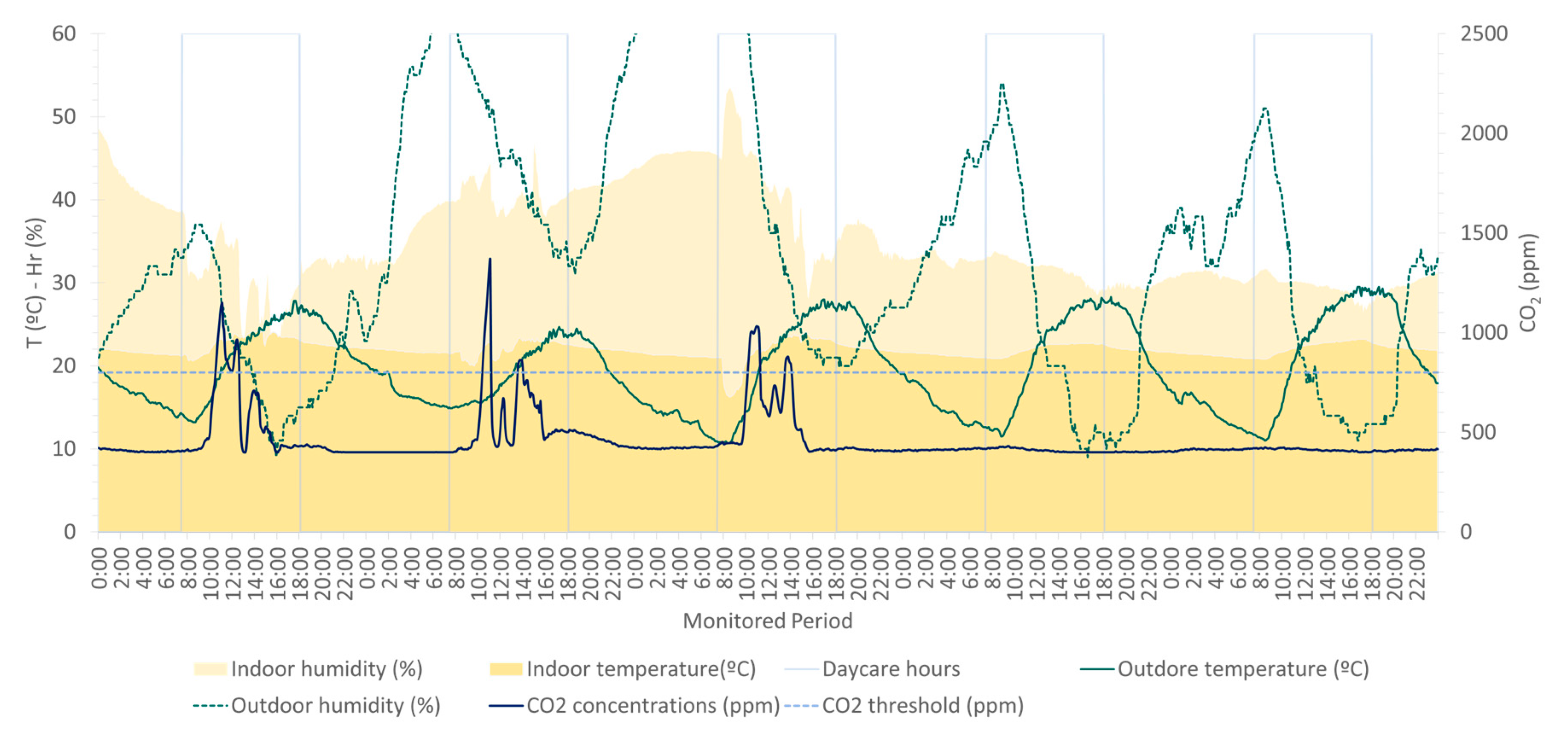
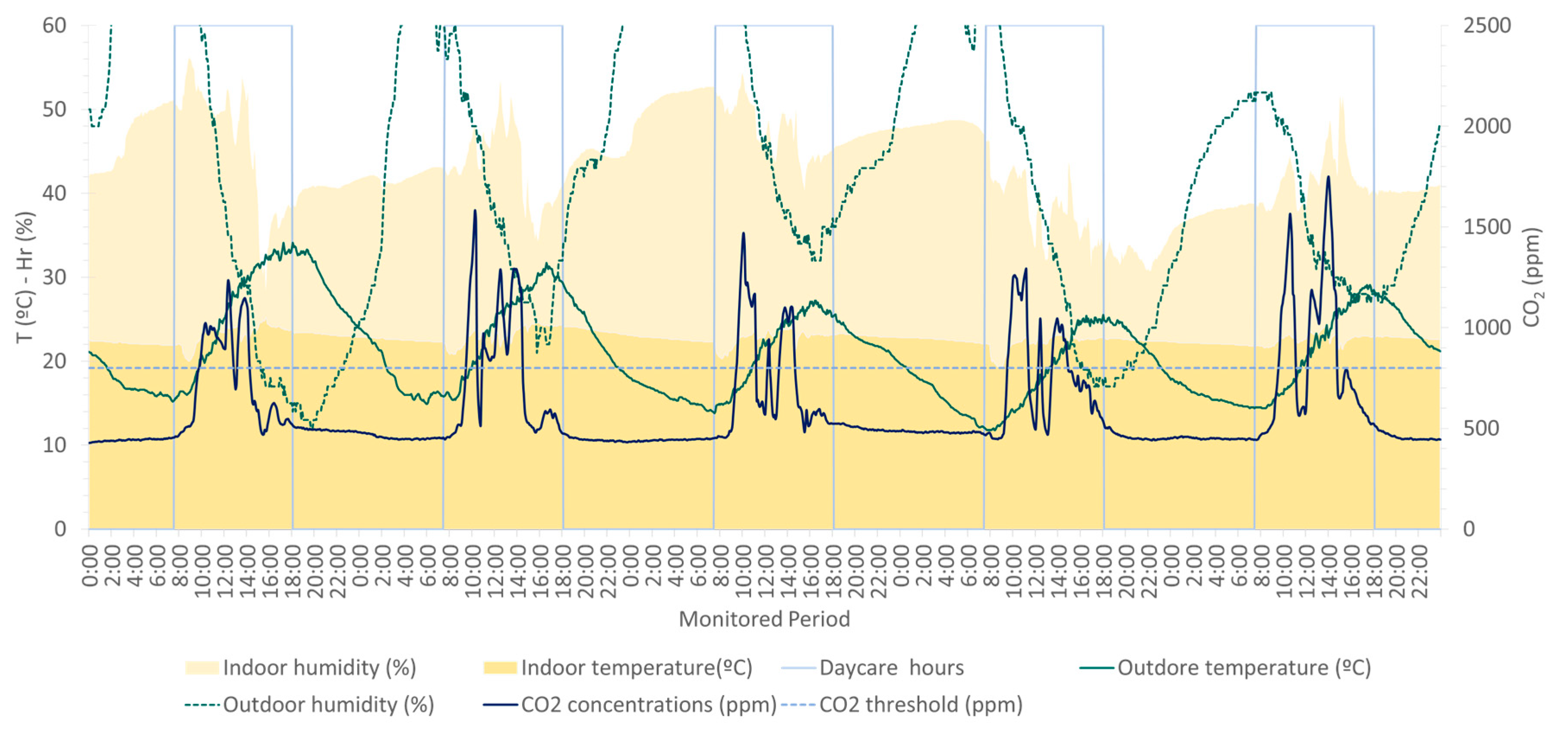
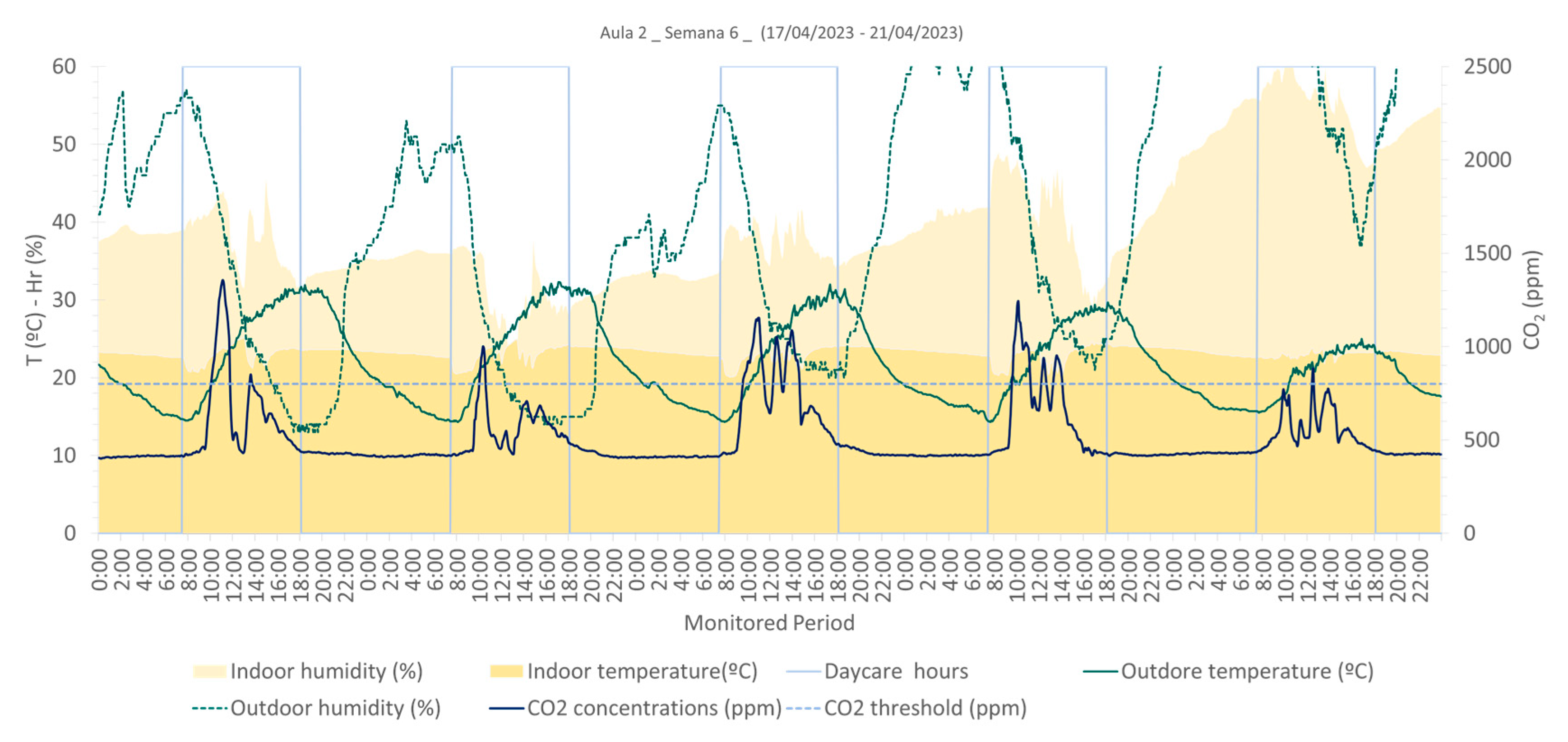
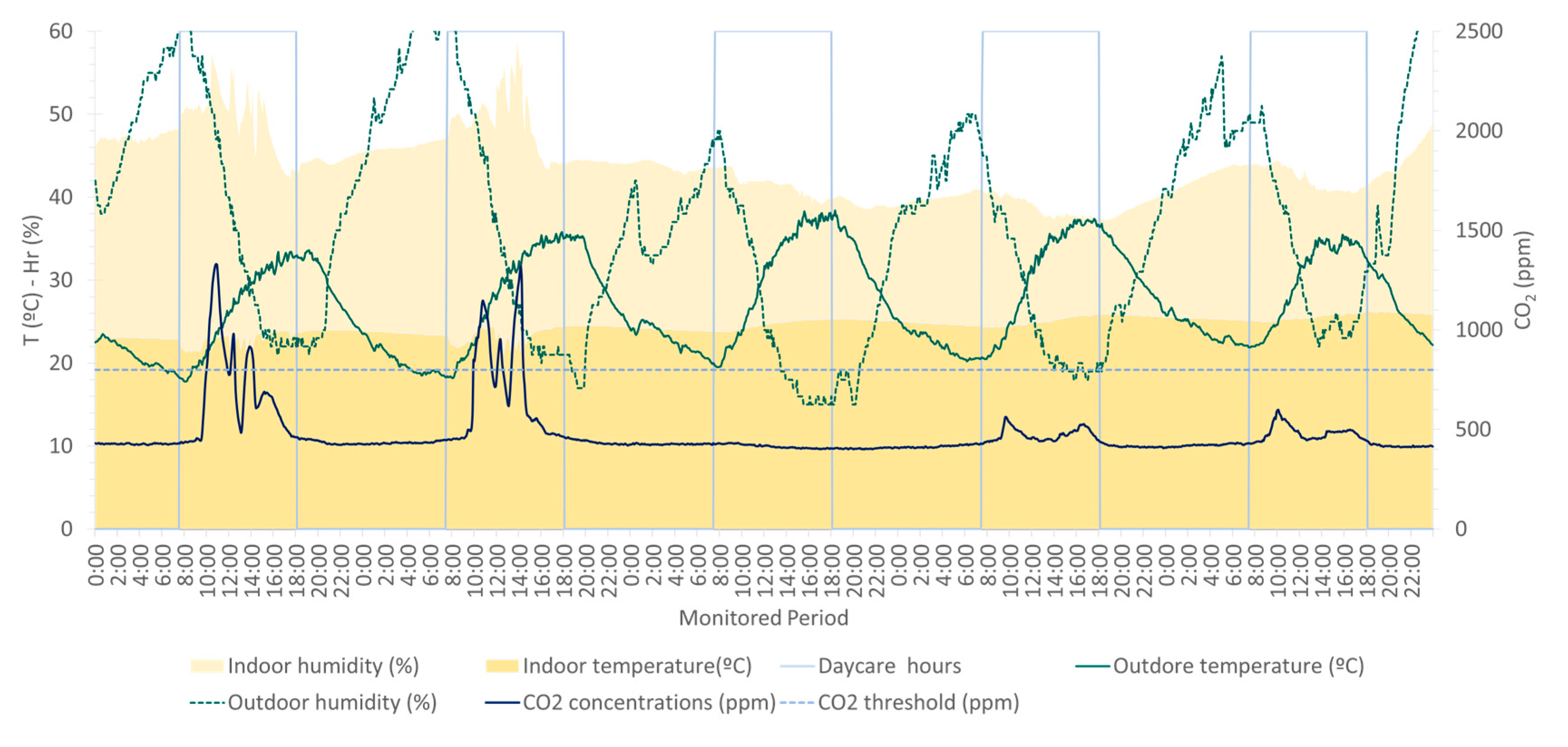
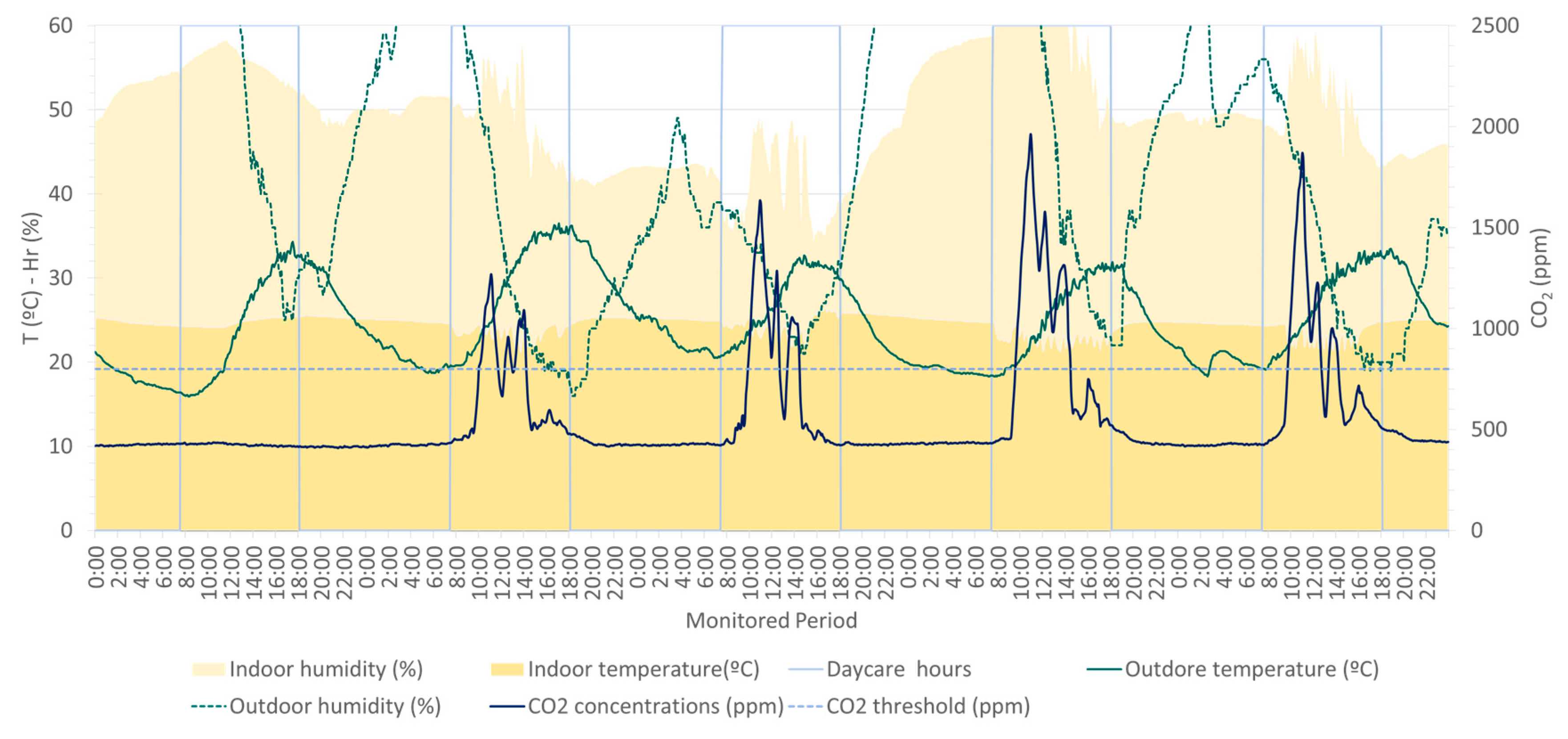
3.1. Thermal Comfort
3.2. Air Renewal Efficiency
3.3. Relative Airborne Pathogen Risk Transmission
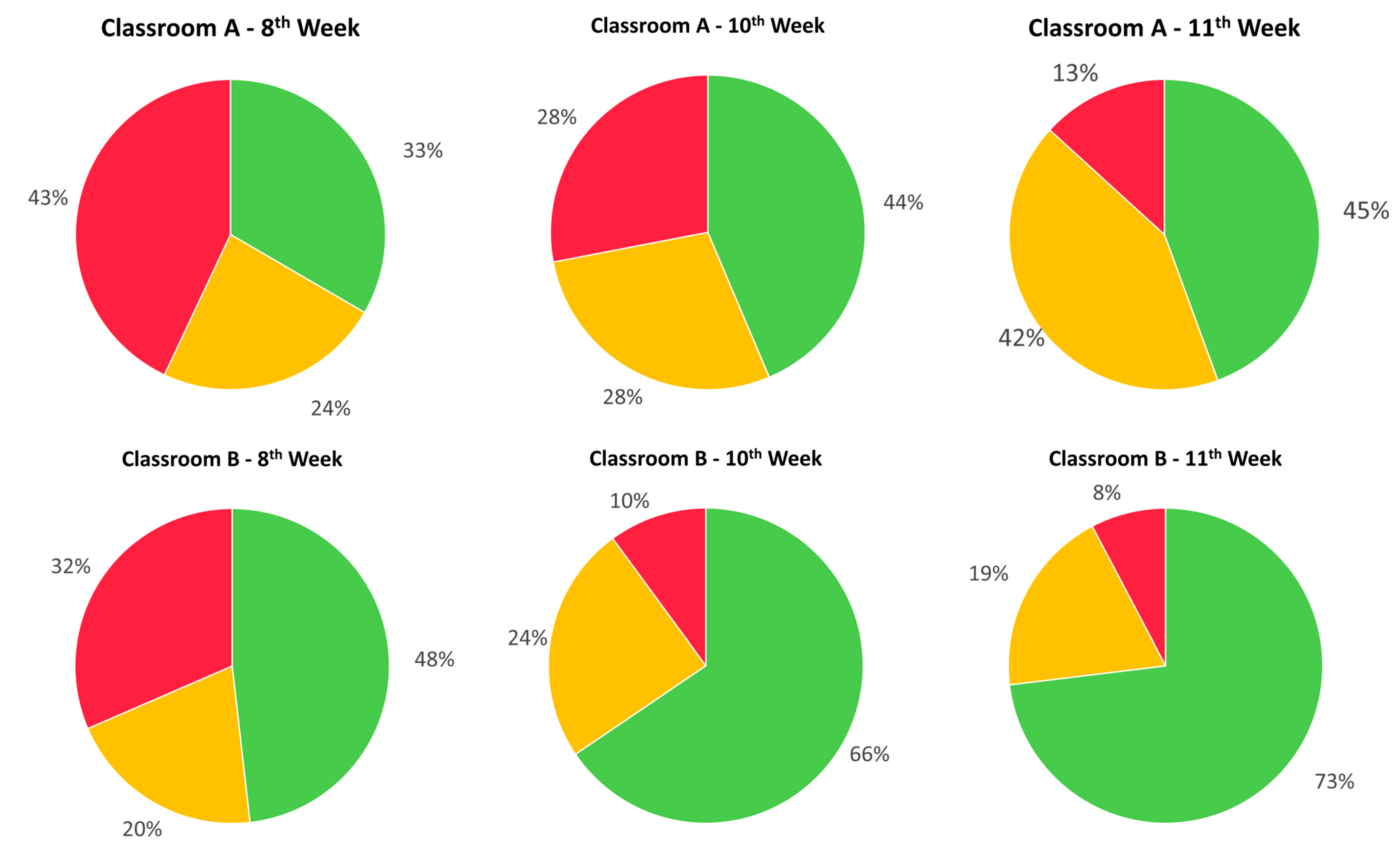
3.4. Circadian Stimulus
4. Discussion
4.1. Thermal Comfort
4.2. Air Renewal Efficiency
4.3. Relative Airborne Pathogen Risk Transmission
4.4. Circadian Stimulus
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A


Appendix B


References
- Fernández-Agüera, J.; Campano, M.Á.; Domínguez-Amarillo, S.; Acosta, I.; Sendra, J.J. CO2 Concentration and Occupants’ Symptoms in Naturally Ventilated Schools in Mediterranean Climate. Buildings 2019, 9, 197. [Google Scholar] [CrossRef]
- Qian, H.; Miao, T.; Liu, L.; Zheng, X.; Luo, D.; Li, Y. Indoor Transmission of SARS-CoV-2. Indoor Air 2021, 31, 639–645. [Google Scholar] [CrossRef]
- Morawska, L.; Cao, J. Airborne Transmission of SARS-CoV-2: The World Should Face the Reality. Environ. Int. 2020, 139, 105730. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.C.; Prather, K.A.; Sznitman, J.; Jimenez, J.L.; Lakdawala, S.S.; Tufekci, Z.; Marr, L.C. Airborne Transmission of Respiratory Viruses. Science 2021, 373, eabd9149. [Google Scholar] [CrossRef] [PubMed]
- Annesi-Maesano, I.; Hulin, M.; Lavaud, F.; Raherison, C.; Kopferschmitt, C.; De Blay, F.; Charpin, D.A.; Denis, C. Poor Air Quality in Classrooms Related to Asthma and Rhinitis in Primary Schoolchildren of the French 6 Cities Study. Thorax 2012, 67, 682–688. [Google Scholar] [CrossRef] [PubMed]
- Almeida, S.M.; Canha, N.; Silva, A.; Do Carmo Freitas, M.; Pegas, P.; Alves, C.; Evtyugina, M.; Pio, C.A. Children Exposure to Atmospheric Particles in Indoor of Lisbon Primary Schools. Atmos. Environ. 2011, 45, 7594–7599. [Google Scholar] [CrossRef]
- Ismail, I.F.; Adnan, A.I.Z.; Al-Mekhlafi, A.M.Q.; Mohamed, B.A.M.A.; Nasir, N.F.; Hariri, A.; Isa, N.M. Indoor Air Quality (IAQ) in Educational Institutions: A Review on Risks of Poor IAQ, Sampling Strategies, and Building-Related Health Symptoms. J. Saf. Health Ergon. 2020, 2, 1–9. [Google Scholar]
- Wolkoff, P.; Azuma, K.; Carrer, P. Health, Work Performance, and Risk of Infection in Office-like Environments: The Role of Indoor Temperature, Air Humidity, and Ventilation. Int. J. Hyg. Environ. Health 2021, 233, 113709. [Google Scholar] [CrossRef]
- ASHRAE Board of Directors. ASHRAE Position Document on Indoor Carbon Dioxide; ASHRAE Board of Directors: Peachtree Corners, GA, USA, 2022. [Google Scholar]
- Peng, Z.; Jimenez, J.L. Exhaled CO2 as a COVID-19 Infection Risk Proxy for Different Indoor Environments and Activities. Environ. Sci. Technol. Lett. 2021, 8, 392–397. [Google Scholar] [CrossRef]
- Fantozzi, F.; Lamberti, G.; Leccese, F.; Salvadori, G. Monitoring CO2 Concentration to Control the Infection Probability Due to Airborne Transmission in Naturally Ventilated University Classrooms. Arch. Sci. Rev. 2022, 65, 306–318. [Google Scholar] [CrossRef]
- Rodríguez, D.; Urbieta, I.R.; Velasco, Á.; Campano-Laborda, M.Á.; Jiménez, E. Assessment of Indoor Air Quality and Risk of COVID-19 Infection in Spanish Secondary School and University Classrooms. Build. Environ. 2022, 226, 109717. [Google Scholar] [CrossRef] [PubMed]
- Allen, J.G.; MacNaughton, P.; Satish, U.; Santanam, S.; Vallarino, J.; Spengler, J.D. Associations of Cognitive Function Scores with Carbon Dioxide, Ventilation, and Volatile Organic Compound Exposures in Office Workers: A Controlled Exposure Study of Green and Conventional Office Environments. Environ. Health Perspect. 2016, 124, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Wargocki, P.; Wyon, D. The Effects of Moderately Raised Classroom Temperatures and Classroom Ventilation Rate on the Performance of Schoolwork by Children. HVAC&R Res. 2007, 13, 193–220. [Google Scholar] [CrossRef]
- Satish, U.; Mendell, M.J.; Shekhar, K.; Hotchi, T.; Sullivan, D. Is CO2 an Indoor Pollutant? Direct Effects of Low-to-Moderate CO2 Concentrations on Human Decision-Making Performance. Environ. Health Perspect. 2012, 120, 1671–1678. [Google Scholar] [CrossRef]
- Bakó-Biró, Z.; Clements-Croome, D.J.; Kochhar, N.; Awbi, H.B.; Williams, M.J. Ventilation Rates in Schools and Pupils’ Performance. Build. Environ. 2012, 48, 215–223. [Google Scholar] [CrossRef]
- Simoni, M.; Annesi-Maesano, I.; Sigsgaard, T.; Norback, D.; Wieslander, G.; Nystad, D.; Cancianie, M.; Sestini, P.; Viegi, G. School Air Quality Related to Dry Cough, Rhinitis and Nasal Patency in Children. Eur. Respir. J. 2010, 35, 742–749. [Google Scholar] [CrossRef]
- Wargocki, P.; Wyon, D.P.; Sundell, J.; Clausen, G.; Fanger, P.O. The Effects of Outdoor Air Supply Rate in an Office on Perceived Air Quality, Sick Building Syndrome (SBS) Symptoms and Productivity. Indoor Air 2001, 10, 222–236. [Google Scholar] [CrossRef]
- Burge, P.S. Sick Building Syndrome. Occup. Environ. Med. 2004, 61, 185–190. [Google Scholar] [CrossRef]
- Erdmann, C.A.; Apte, M.G. Mucous Membrane and Lower Respiratory Building Related Symptoms in Relation to Indoor Carbon Dioxide Concentrations in the 100-Building BASE Dataset. Indoor Air 2004, 14, 127–134. [Google Scholar] [CrossRef]
- Azuma, K.; Kagi, N.; Yanagi, U.; Osawa, H. Effects of Low-Level Inhalation Exposure to Carbon Dioxide in Indoor Environments: A Short Review on Human Health and Psychomotor Performance. Environ. Int. 2018, 121, 51–56. [Google Scholar] [CrossRef]
- Seppänen, O.A.; Fisk, W.J.; Mendell, M.J. Association of Ventilation Rates and CO2 Concentrations with Health and Other Responses in Commercial and Institutional Buildings. Indoor Air 1999, 9, 226–252. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Amarillo, S.; Fernández-Agüera, J.; González, M.M.; Cuerdo-Vilches, T. Overheating in Schools: Factors Determining Children’s Perceptions of Overall Comfort Indoors. Sustainability 2020, 12, 5772. [Google Scholar] [CrossRef]
- Campano, M.A. Confort Térmico y Eficiencia Energética en Espacios Con Alta Carga Interna Climatizados: Aplicación a Espacios Docentes No Universitarios en Andalucía. Doctoral Thesis, Universidad de Sevilla, Seville, Spain, 2015. [Google Scholar]
- Campano-Laborda, M.Á.; Domínguez-Amarillo, S.; Fernández-Agüera, J.; Acosta, I. Indoor Comfort and Symptomatology in Non-University Educational Buildings: Occupants’ Perception. Atmosphere 2020, 11, 357. [Google Scholar] [CrossRef]
- Haddrell, A.; Oswin, H.; Otero-Fernandez, M.; Robinson, J.F.; Cogan, T.; Alexander, R.; Mann, J.F.S.; Hill, D.; Finn, A.; Davidson, A.D.; et al. Ambient Carbon Dioxide Concentration Correlates with SARS-CoV-2 Aerostability and Infection Risk. Nat. Commun. 2024, 15, 3487. [Google Scholar] [CrossRef]
- Buonanno, G.; Morawska, L.; Stabile, L. Quantitative Assessment of the Risk of Airborne Transmission of SARS-CoV-2 Infection: Prospective and Retrospective Applications. Environ. Int. 2020, 145, 106112. [Google Scholar] [CrossRef]
- Buonanno, G.; Stabile, L.; Morawska, L. Estimation of Airborne Viral Emission: Quanta Emission Rate of SARS-CoV-2 for Infection Risk Assessment. Environ. Int. 2020, 141, 105794. [Google Scholar] [CrossRef]
- Peng, Z.; Rojas, A.L.P.; Kropff, E.; Bahnfleth, W.; Buonanno, G.; Dancer, S.J.; Kurnitski, J.; Li, Y.; Loomans, M.G.L.C.; Marr, L.C.; et al. Practical Indicators for Risk of Airborne Transmission in Shared Indoor Environments and Their Application to COVID-19 Outbreaks. Environ. Sci. Technol. 2022, 56, 1125–1137. [Google Scholar] [CrossRef]
- Lorthe, E.; Bellon, M.; Michielin, G.; Berthelot, J.; Zaballa, M.E.; Pennacchio, F.; Bekliz, M.; Laubscher, F.; Arefi, F.; Perez-Saez, J.; et al. Epidemiological, Virological and Serological Investigation into a SARS-CoV-2 Outbreak (Alpha Variant) in a Primary School: A Prospective Longitudinal Study. PLoS ONE 2022, 17, e0272663. [Google Scholar] [CrossRef]
- Lorthe, E.; Bellon, M.; Berthelot, J.; Michielin, G.; L’Huillier, A.G.; Posfay-Barbe, K.M.; Azman, A.S.; Guessous, I.; Maerkl, S.J.; Eckerle, I.; et al. A SARS-CoV-2 Omicron (B.1.1.529) Variant Outbreak in a Primary School in Geneva, Switzerland. Lancet 2022, 22, 767–768. [Google Scholar] [CrossRef]
- Božič, A.; Kanduč, M. Relative Humidity in Droplet and Airborne Transmission of Disease. J. Biol. Phys. 2021, 47, 1–29. [Google Scholar] [CrossRef]
- Raines, K.S.; Doniach, S.; Bhanot, G. The Transmission of SARS-CoV-2 Is Likely Comodulated by Temperature and by Relative Humidity. PLoS ONE 2021, 16, e0255212. [Google Scholar] [CrossRef] [PubMed]
- Ahlawat, A.; Wiedensohler, A.; Mishra, S.K. An Overview on the Role of Relative Humidity in Airborne Transmission of Sars-Cov-2 in Indoor Environments. Aerosol Air Qual. Res. 2020, 20, 1856–1861. [Google Scholar] [CrossRef]
- Aganovic, A.; Bi, Y.; Cao, G.; Drangsholt, F.; Kurnitski, J.; Wargocki, P. Estimating the Impact of Indoor Relative Humidity on SARS-CoV-2 Airborne Transmission Risk Using a New Modification of the Wells-Riley Model. Build. Environ. 2021, 205, 108278. [Google Scholar] [CrossRef] [PubMed]
- Campano, M.Á.; Fernández-Agüera, J.; Domínguez-Amarillo, S.; Acosta, I.; Sendra, J.J. Covid Riskairborne, a Tool to Test the Risk of Aerosol Transmission of SARS-CoV-2 under Different Scenarios: A Pre-School Classroom Case Study. In Proceedings of the 3rd International Conference on Comfort at the Extremes: Covid, Climate Change and Ventilation, Comfort at the Extremes, Edinburgh, UK, 5 September 2022; pp. 22–34. [Google Scholar]
- Westwood, E.; Smith, S.; Mann, D.; Pattinson, C.; Allan, A.; Staton, S. The Effects of Light in Children: A Systematic Review. J. Environ. Psychol. 2023, 89, 102062. [Google Scholar] [CrossRef]
- Wong, S.D.; Wright, K.P.; Spencer, R.L.; Vetter, C.; Hicks, L.M.; Jenni, O.G.; LeBourgeois, M.K. Development of the Circadian System in Early Life: Maternal and Environmental Factors. J. Physiol. Anthr. 2022, 41, 22. [Google Scholar] [CrossRef]
- Ángeles-Castellanos, M.; Vázquez Ruiz, S.; Palma, M.; Ubaldo, L.; Cervantes, G.; Rojas-Granados, A.; Escobar, C. Development of Biological Rhythms in the Newborn Child. Rev. Fac. Med. (México) 2023, 56, 26–35. [Google Scholar]
- Akacem, L.D.; Wright, K.P.; LeBourgeois, M.K. Sensitivity of the Circadian System to Evening Bright Light in Preschool-Age Children. Physiol. Rep. 2018, 6, e13617. [Google Scholar] [CrossRef]
- Medic, G.; Wille, M.; Hemels, M. Short- and Long-Term Health Consequences of Sleep Disruption. Nat. Sci. Sleep 2017, 9, 151–161. [Google Scholar] [CrossRef]
- Figueiro, M.G.; Pedler, D. Cardiovascular Disease and Lifestyle Choices: Spotlight on Circadian Rhythms and Sleep. Prog. Cardiovasc. Dis. 2023, 77, 70–77. [Google Scholar] [CrossRef]
- LeBourgeois, M.K.; Hartstein, L.E.; Wong, S.D.; Ricker, A.A. Optimal Sleep and Circadian Habits in Infants and Children. In Encyclopedia of Sleep and Circadian Rhythms; Elsevier: Amsterdam, The Netherlands, 2023; pp. 102–109. [Google Scholar]
- Pauley, S.M. Lighting for the Human Circadian Clock: Recent Research Indicates That Lighting Has Become a Public Health Issue. Med. Hypotheses 2004, 63, 588–596. [Google Scholar] [CrossRef]
- Rea, M.S.; Figueiro, M.G.; Bierman, A.; Bullough, J.D. Circadian Light. J. Circadian Rhythm. 2010, 8, 2. [Google Scholar] [CrossRef] [PubMed]
- Gradisar, M.; Dohnt, H.; Gardner, G.; Paine, S.; Starkey, K.; Menne, A.; Slater, A.; Wright, H.; Hudson, J.L.; Weaver, E.; et al. A Randomized Controlled Trial of Cognitive-Behavior Therapy Plus Bright Light Therapy for Adolescent Delayed Sleep Phase Disorder. Sleep 2011, 34, 1671–1680. [Google Scholar] [CrossRef]
- Rodríguez, P.; Campano, M.A.; Domníguez-Amarillo, S.; Acosta, I.J. Optimization of Window Design in Hospital Rooms for Effective Access to Daylight. E3S Web of Conferences 2024, 487, 02002. [Google Scholar] [CrossRef]
- Logan, R.W.; McClung, C.A. Rhythms of Life: Circadian Disruption and Brain Disorders across the Lifespan. Nat. Rev. Neurosci. 2019, 20, 49–65. [Google Scholar] [CrossRef]
- Miike, T.; Oniki, K.; Toyoura, M.; Tonooka, S.; Tajima, S.; Kinoshita, J.; Saruwatari, J.; Konishi, Y. Disruption of Circadian Sleep/Wake Rhythms in Infants May Herald Future Development of Autism Spectrum Disorder. Clocks Sleep 2024, 6, 170–182. [Google Scholar] [CrossRef]
- Martinez-Cayuelas, E.; Gavela-Pérez, T.; Rodrigo-Moreno, M.; Losada-Del Pozo, R.; Moreno-Vinues, B.; Garces, C.; Soriano-Guillén, L. Sleep Problems, Circadian Rhythms, and Their Relation to Behavioral Difficulties in Children and Adolescents with Autism Spectrum Disorder. J. Autism Dev. Disord. 2024, 54, 1712–1726. [Google Scholar] [CrossRef]
- Bullough, J.D.; Rea, M.S.; Figueiro, M.G. Of Mice and Women: Light as a Circadian Stimulus in Breast Cancer Research. Cancer Causes Control 2006, 17, 375–383. [Google Scholar] [CrossRef]
- Wong, I.L. A Review of Daylighting Design and Implementation in Buildings. Renew. Sustain. Energy Rev. 2017, 74, 959–968. [Google Scholar] [CrossRef]
- Ghisi, E.; Tinker, J.A. An Ideal Window Area Concept for Energy Efficient Integration of Daylight and Artificial Light in Buildings. Build. Environ. 2005, 40, 51–61. [Google Scholar] [CrossRef]
- Reinhart, C.F.; Mardaljevic, J.; Rogers, Z. Dynamic Daylight Performance Metrics for Sustainable Building Design. LEUKOS-J. Illum. Eng. Soc. N. Am. 2006, 3, 7–31. [Google Scholar] [CrossRef]
- Acosta, I.; Leslie, R.P.; Figueiro, M.G. Analysis of Circadian Stimulus Allowed by Daylighting in Hospital Rooms. Light. Res. Technol. 2017, 49, 49–61. [Google Scholar] [CrossRef]
- Acosta, I.; Campano, M.Á.; Leslie, R.; Radetsky, L. Daylighting Design for Healthy Environments: Analysis of Educational Spaces for Optimal Circadian Stimulus. Sol. Energy 2019, 193, 584–596. [Google Scholar] [CrossRef]
- Campano, M.Á.; García-Martín, G.; Acosta, I.; Bustamante, P. Designing Intensive Care Unit Windows in a Mediterranean Climate: Efficiency, Daylighting, and Circadian Response. Appl. Sci. 2024, 14, 9798. [Google Scholar] [CrossRef]
- Sendra Salas, J.J.; Acosta García, I.J.; Domínguez Amarillo, S. Luz, Salud y Bienestar En La Arquitectura Hospitalaria: La Iluminación Biodinámica Para Fomentar La Regulación Del Ritmo Circadiano. In Inhabiting Hospitals: Welfare Beyond Comfort. New Trends in Healthcare Design; Chías Navarro, P., Abad Balboa, T., Eds.; Editorial Universidad de Alcalá: Alcalá de Henares, Spain, 2021; pp. 112–127. ISBN 9788418254307. [Google Scholar]
- Figueiro, M.G.; Steverson, B.; Heerwagen, J.; Kampschroer, K.; Hunter, C.M.; Gonzales, K.; Plitnick, B.; Rea, M.S. The Impact of Daytime Light Exposures on Sleep and Mood in Office Workers. Sleep Health 2017, 3, 204–215. [Google Scholar] [CrossRef]
- Jalali, M.S.; Jones, J.R.; Tural, E.; Gibbons, R.B. Human-Centric Lighting Design: A Framework for Supporting Healthy Circadian Rhythm Grounded in Established Knowledge in Interior Spaces. Buildings 2024, 14, 1125. [Google Scholar] [CrossRef]
- BOE-A-2006-5515; Ministerio de Fomento del Gobierno de España Real Decreto 314/2006, de 17 de Marzo, Por El Que Se Aprueba El Código Técnico de La Edificación. Ministerio de Fomento del Gobierno de España: Madrid, Spain, 2006.
- Ministerio de la Presidencia del Gobierno de España. Ministerio de la Presidencia del Gobierno de España Real Decreto 1027/2007, de 20 de Julio, Por El Que Se Aprueba El Reglamento de Instalaciones Térmicas En Los Edificios. In BOE no 207, 2007 29th August; Ministerio de la Presidencia del Gobierno de España: Madrid, Spain, 2021; pp. 35931–35984. [Google Scholar]
- Ministerio de la Presidencia del Gobierno de España. Gobierno de España Real Decreto 1826/2009, de 11 de Diciembre, Por El Que Se Modifica El Reglamento de Instalaciones Térmicas En Los Edificios, Aprobado Por El Real Decreto 1027/2007. In Boletín Oficial del Estado; Ministerio de la Presidencia del Gobierno de España: Madrid, Spain, 2009; Volume 298, pp. 104924–104927. [Google Scholar]
- Ministerio de la Presidencia, Relaciones con las Cortes y Memoria Democrática del Gobierno de España. Real Decreto 178/2021, de 23 de Marzo, Por El Que Se Modifica El Real Decreto 1027/2007, De 20 De Julio, Por El Que Se Aprueba El Reglamento de Instalaciones Térmicas En Los Edificios. In BOE no 71, 2021 24th March; Ministerio, Relaciones con las Cortes y Memoria Democrática de la Presidencia del Gobierno de España: Madrid, Spain, 2021; pp. 33748–33793. ISBN 8428332320. [Google Scholar]
- Fanger, P. Thermal Comfort: Analysis and Applications in Environmental Engineering; Copenhagen Danish Technical Press: Copenhagen, Denmark, 1970. [Google Scholar]
- ISO 7730:2005; Ergonomics of the Thermal Environment—Analytical Determination and Interpretation of Thermal Comfort Using Calculation of the PMV and PPD Indices and Local Thermal Comfort Criteria. International Organization for Standardization: Geneva, Switzerland, 2005.
- Campano, M.Á.; Domínguez-Amarillo, S.; Fernández-Agüera, J.; Sendra, J.J. Thermal Perception in Mild Climate: Adaptive Thermal Models for Schools. Sustainability 2019, 11, 3948. [Google Scholar] [CrossRef]
- Guedes, M.C.; Matias, L.; Santos, C.P. Thermal Comfort Criteria and Building Design: Field Work in Portugal. Renew. Energy 2009, 34, 2357–2361. [Google Scholar] [CrossRef]
- Matias, L. Desenvolvimento de um Modelo Adaptativo Para Definição das Condições de Conforto Térmico em Portugal; Universidade Técnica de Lisboa: Lisboa, Portugal, 2010. [Google Scholar]
- Du Bois, D.; Du Bois, E.F. A Formula to Estimate the Approximate Surface Area If Height and Weight Be Known. 1916. Nutrition 1989, 5, 303–311. [Google Scholar]
- ISO 8996:2021; Ergonomics of the Thermal Environment–Determination of Metabolic Rate. International Organization for Standardization: Geneva, Switzerland, 2021.
- Campano-Laborda, M.Á.; Domínguez-Amarillo, S.; Acosta García, I.; Fernández-Agüera, J.J.; Bustamante Rojas, P.; Sendra Salas, J.J.; Jiménez Palacios, J.L.; Velarde Rodríguez, J.D.; Acosta García, I.; Bustamante Rojas, P.; et al. COVID Risk Airborne. Available online: www.covidairbornerisk.com (accessed on 15 December 2021).
- Rudnick, S.N.; Milton, D.K. Risk of Indoor Airborne Infection Transmission Estimated from Carbon Dioxide Concentration. Indoor Air 2003, 13, 237–245. [Google Scholar] [CrossRef]
- Morawska, L.; Johnson, G.R.; Ristovski, Z.D.; Hargreaves, M.; Mengersen, K.; Corbett, S.; Chao, C.Y.H.; Li, Y.; Katoshevski, D. Size Distribution and Sites of Origin of Droplets Expelled from the Human Respiratory Tract during Expiratory Activities. J. Aerosol Sci. 2009, 40, 256–269. [Google Scholar] [CrossRef]
- Lyngse, F.P.; Kirkeby, C.T.; Denwood, M.; Christiansen, L.E.; Mølbak, K.; Møller, C.H.; Skov, R.L.; Krause, T.G.; Rasmussen, M.; Sieber, R.N.; et al. Household Transmission of SARS-CoV-2 Omicron Variant of Concern Subvariants BA.1 and BA.2 in Denmark. Nat. Commun. 2022, 13, 5760. [Google Scholar] [CrossRef] [PubMed]
- Du, Z.; Hong, H.; Wang, S.; Ma, L.; Liu, C.; Bai, Y.; Adam, D.C.; Tian, L.; Wang, L.; Lau, E.H.Y.; et al. Reproduction Number of the Omicron Variant Triples That of the Delta Variant. Viruses 2022, 14, 4–8. [Google Scholar] [CrossRef] [PubMed]
- Campano-Laborda, M.Á.; Jiménez, J.-L.; Fernández-Agüera, J.; Bustamante, P. Estimación Del Riesgo Relativo de Transmisión de Enfermedades Aéreas Mediante El Modelo de Wells-Riley. In Calidad del Aire en los Edificios Para el Bienestar: Estrategias de Aplicación Práctica; Campano, M.Á., Fernández-Agüera, J., Sendra, J.J., Eds.; Octaedro: Madrid, Spain, 2023; p. 180. ISBN 978-84-19506-74-0. [Google Scholar]
- Brainard, G.C.; Hanifin, J.P.; Greeson, J.M.; Byrne, B.; Glickman, G.; Gerner, E.; Rollag, M.D. Action Spectrum for Melatonin Regulation in Humans: Evidence for a Novel Circadian Photoreceptor. J. Neurosci. 2001, 21, 6405–6412. [Google Scholar] [CrossRef]
- St Hilaire, M.A.; Ámundadóttir, M.L.; Rahman, S.A.; Rajaratnam, S.M.W.; Rüger, M.; Brainard, G.C.; Czeisler, C.A.; Andersen, M.; Gooley, J.J.; Lockley, S.W. The Spectral Sensitivity of Human Circadian Phase Resetting and Melatonin Suppression to Light Changes Dynamically with Light Duration. Proc. Natl. Acad. Sci. USA 2022, 119, e2205301119. [Google Scholar] [CrossRef]
- Microsoft Corporation Microsoft Excel (v. Office 365); Microsoft Corporation: Redmond (Washington), USA. 2024. Available online: https://www.office.com/ (accessed on 5 December 2023).
- Icahn School of Medicine at Mount Sinai. Light and Health Research Center CS Calculator (2.0). Available online: https://cscalc.light-health.org/ (accessed on 28 October 2024).
- Rea, M.S.; Nagare, R.; Figueiro, M.G. Modeling Circadian Phototransduction: Retinal Neurophysiology and Neuroanatomy. Front. Neurosci. 2021, 14, 615305. [Google Scholar] [CrossRef]
- Rea, M.S.; Nagare, R.; Figueiro, M.G. Modeling Circadian Phototransduction: Quantitative Predictions of Psychophysical Data. Front. Neurosci. 2021, 15, 615322. [Google Scholar] [CrossRef]
- Rea, M.S.; Figueiro, M.G.; Bullough, J.D.; Bierman, A. A Model of Phototransduction by the Human Circadian System. Brain Res. Rev. 2005, 50, 213–228. [Google Scholar] [CrossRef]
- Darula, S.; Kittler, R. CIE General Sky Standard Defining Luminance Distributions. In Proceedings of the International Building Performance Simulation Association (IBPSA), Montreal, QC, Canada, 11–13 September 2002; pp. 11–13. [Google Scholar]
- ISO 15469:2004; Spatial Distribution of Daylight-CIE Standard General Sky. Commission Internationale de l’Éclairage, Ed.; International Organization for Standardization: Geneva, Switzerland, 2004.
- UNE 171380:2024; Medición en Continuo de CO2 en Interiores Para la Prevención en Salud y Mejora del Bienestar. AENOR-Asociación Española de Normalización y Certificación: Madrid, Spain, 2024.
- Muelas, Á.; Remacha, P.; Pina, A.; Tizné, E.; El-Kadmiri, S.; Ruiz, A.; Aranda, D.; Ballester, J. Analysis of Different Ventilation Strategies and CO2 Distribution in a Naturally Ventilated Classroom. Atmos. Environ. 2022, 283, 119176. [Google Scholar] [CrossRef]
- Muelas, Á.; Pina, A.; Remacha, P.; Tizné, E.; Aranda, D.; Ruiz, A.; Ballester, J. Guía Práctica de Ventilación en Aulas: Ya Tengo el Analizador de CO2… ¿Y Ahora Qué? LIFTEC/Univ. Zaragoza/CSIC: Zaragoza, Spain, 2020; Available online: https://drive.google.com/file/d/1o1qElJ7qijQA85eyvgn_TvyJlDgwirjf/view (accessed on 3 September 2024).



| Exhalation of Infectious Occupant | Inhalation of Susceptible Occupant | |||
|---|---|---|---|---|
| Scenario | Activity | ERq—85th Percentile (q/h) | Activity | Inhaled Flow Rate (m3/h) |
| Case 1 | Resting, oral breathing | 41.4 (1 year-old) | Resting | 0.28 |
| Case 2 | Resting, speaking | 194.7 (1 year-old) | Resting | 0.28 |
| Case 3 | Resting, speaking loudly | 1255.4 (1 year-old) | Resting | 0.28 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Martín, G.; Romero-Lara, F.; Campano, M.Á.; Acosta, I.; Bustamante, P. Healthier Indoor Environments for Vulnerable Occupants: Analysis of Light, Air Quality, and Airborne Disease Risk. Appl. Sci. 2025, 15, 1217. https://doi.org/10.3390/app15031217
García-Martín G, Romero-Lara F, Campano MÁ, Acosta I, Bustamante P. Healthier Indoor Environments for Vulnerable Occupants: Analysis of Light, Air Quality, and Airborne Disease Risk. Applied Sciences. 2025; 15(3):1217. https://doi.org/10.3390/app15031217
Chicago/Turabian StyleGarcía-Martín, Guillermo, Fátima Romero-Lara, Miguel Ángel Campano, Ignacio Acosta, and Pedro Bustamante. 2025. "Healthier Indoor Environments for Vulnerable Occupants: Analysis of Light, Air Quality, and Airborne Disease Risk" Applied Sciences 15, no. 3: 1217. https://doi.org/10.3390/app15031217
APA StyleGarcía-Martín, G., Romero-Lara, F., Campano, M. Á., Acosta, I., & Bustamante, P. (2025). Healthier Indoor Environments for Vulnerable Occupants: Analysis of Light, Air Quality, and Airborne Disease Risk. Applied Sciences, 15(3), 1217. https://doi.org/10.3390/app15031217










