Effects of Low Load Blood Flow Restriction Training on Post-Surgical Musculoskeletal Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Abstract
:1. Introduction
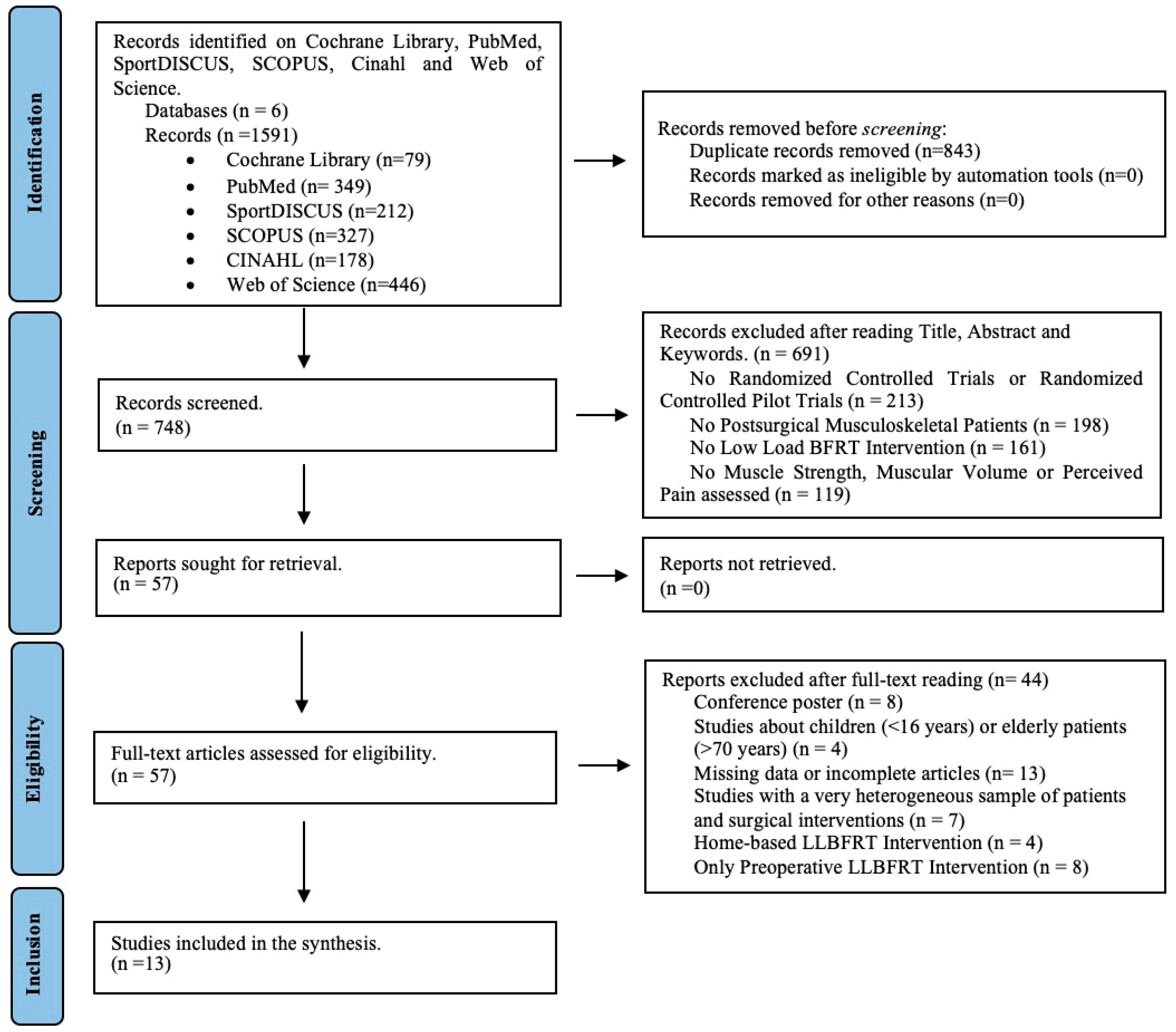
2. Materials and Methods
2.1. Study Design
2.2. Data Sources and Search Strategy
2.3. Study Selection
2.4. Data Extraction
2.5. Risk of Bias and Quality Assessment
2.6. Data Synthesis and Analysis
| Author and Year | Study Design | GRADE | Journal (JCI) | N | N (Intervention—Control) and %AOP | Surgery |
|---|---|---|---|---|---|---|
| Hughes et al., 2019 [32] | RCT | High | Sports Medicine (2.11) | 24 | I (LL-BFR 80% AOP n = 12) and C (HLT n = 12) | ACL reconstruction |
| Vieira de Melo et al., 2022 [39] | RCT | High | Journal of Rehabilitation Medicine (1.03) | 24 | I (LL-BFR 80% AOP n = 12) and C (HLT n = 12) | ACL reconstruction |
| Jack et al., 2023 [40] | RCT | High | Sports Health | 32 | I (LL-BFR 80% AOP n = 17) and C (LLT n = 15) | ACL reconstruction |
| Li et al., 2023 [41] | RCPT | High * | BMC Musculoskeletal Disorders (0.77) | 23 | I (LL-BFRT 80%AOP n = 8 and 40%AOP n = 9) and C (RT n = 6) | ACL reconstruction |
| Park et al., 2022 [42] | RCT | High | Medicine (0.38) | 42 | I (LL-BFRT 80%AOP n = 13 and 40%AOP n = 14) and C (LLT n = 15) | High tibial osteotomy |
| Ke et al., 2022 [43] | RCT | High | Frontiers in Physiology (1.00) | 38 | I (LL-BFRT 80% AOP n = 19) and C (LLT n = 19) | Knee arthroscopy (meniscectomy) |
| Mason et al., 2022 [44] | RCT | High * | Journal of Sport Rehabilitation (0.92) | 17 | I (LLBFRT 80% AOP n = 8) and C (LLT n = 9) | Knee arthroscopy (meniscal repair or chondral surgery) |
| Tennent et al., 2017 [45] | RCPT | High | Clinical Journal of Sport Medicine (1.27) | 17 | I (LL-BFRT 80% AOP n = 10) and C (Protocol of Standard Physical Therapy n = 7) | Knee arthroscopy |
| Fan et al., 2023 [46] | RCT | High * | Annals of Medicine (0.98) | 35 | I (LLBFRT 40–80%AOP n = 17) and C (LLT n = 18) | ORIF for distal radius fracture |
| Sgromolo et al., 2020 [47] | RCT | Moderate | Journal of Wrist Surgery (0.29) | 9 | I (LL-BFRT 50%AOP n = 5) and C (Standard Protocol of Physical Therapy n = 4) | ORIF for distal radius fracture |
| Erickson et al., 2024 [48] | RCT | High | Medicine and Science in Sports and Exercise | 48 | I (LL-BFRT 60%AOP n = 23) and C (RT n = 25) | ACL reconstruction |
| Jung et al., 2022 [49] | RCT | High | Applied Sciences | 24 | I (LL-BFRT 40%AOP n = 12) and Standard Protocol of Physical Therapy n = 12) | ACL reconstruction |
| Okoroha et al., 2023 [50] | RCT | High | The Orthopaedic Journal of Sport Medicine | 38 | I (LL-BFRT 80%AOP n = 16) and C (Standard Protocol of Physical Therapy n = 22) | ACL reconstruction |
| Author and Year | Protocol of BFR Training (Exercise, Sets and Repetitions) | Load | Rest | Frequency of Sessions and Length of Intervention |
|---|---|---|---|---|
| Hughes et al., 2019 [33] | Unilateral Leg Press 0–90° ROM 4 × (30,15,15,15) | 30% RM | 30 s between sets | 16 sessions in 8 weeks (2 times/week) |
| Vieira de Melo et al., 2022 [39] | Leg Press and Knee Flexion on chair 4 × (30,15,15,15) | 30% RM | 30 s between sets | 24 sessions in 12 weeks (2 times/week) |
| Jack et al., 2023 [40] | W2-W5: Quadriceps contractions, CKC Knee extensions and bilateral leg press 4 × (30,15,15,15) W5-W12: Single leg hamstring curl, single leg press, ball squat, split lunge and box step-up 4 × (30,15,15,15) | 30% RM | 30 s between sets | 24 sessions in 12 weeks (2 times/week) |
| Li et al., 2023 [41] | 2 Quadriceps exercises with elastic bands and barbells (30,15,15,15) | 30% RM | 30 s between sets | 16 sessions in 8 weeks (2 times/week) |
| Park et al., 2022 [42] | NWB (W0-W6): Quadriceps and Hamstring “Setting”, Four-Way Straigh, Quadriceps Extension with Theraband and Hamstring Curl with Theraband 4 × (30,15,15,15) FWB (W6-W12): Leg Extension with machine, Hamstring Curl with machine, Leg Press, Squat and Lunge 4 × (30,15,15,15) | 30% RM | 3 min of perfusion between 5 sets | 24 sessions in 12 weeks (2 times/week) |
| Ke et al., 2022 [43] | Knee Flexion and Extension sliding leg and Squat 0–90° 4 × (30,15,15,15) | 30% RM | 30 s between sets | 16 sessions in 8 Weeks (2 times/week) |
| Mason et al., 2022 [44] | W1-W2: Isometric Quadriceps until 10 times straight leg and Straigh Leg Flexion/Extension/Aduction and Abduction 4 × (30,15,15,15) W3-W4: Knee Extension (90–45°) 4 × (30,15,15,15) W5-W6: Hamstrings Curl 4 × (30,15,15,15) W7-W12: Squat and Unilateral Leg Press (to 60° flexion) 4 × (30,15,15,15) | 30%RM | 30 s between sets and 2 min between exercises (without occlusion) | 24–36 sessions in 12 weeks (2–3 times/week) |
| Tennent et al., 2017 [45] | Leg Press, Knee Extension and Reverse Press 4 × (30,15,15,15) | 30% RM | 30 s between sets and 1 min between exercises | 12 sessions in 6 weeks |
| Fan et al., 2023 [46] | Griping, pinching, Wrist flexion and extension (30,15,15,15) | 20% RM | 30 s between sets and 1 min between exercises | 20 sessions in 4 weeks (5 times/week) |
| Sgromolo et al., 2020 [47] | Wrist Flexion/Extension over a foam wedge, Forearm pronation/supination with arm at side and elbow at 90°, Pinch strength with PG-60 Pinch Gauge and Grip Strength with JAMAR dynamometer 4 × (30,15,15,15) | 30% RM | 30 s between sets and 1 min between exercises | 16–24 sessions in 8 weeks (2–3 times/week) |
| Erikson et al., 2024 [48] | Knee extension, leg press, box step up/down, double limb squat (30,20,10) | 30% RM | 30 s between sets and 1–2 min between exercises | 48 sessions in 16 weeks (3 times/week) |
| Jung et al., 2022 [49] | FWB (wall squat, mini squat, half squat, lunge, step-up), leg extension and leg curl 4 × (30,15,15,15) | 10–30% RM | 30 s between sets and 2 min between exercises | 36 sessions in 12 weeks (3 times/week) |
| Okoroha et al., 2023 [50] | Supine quadriceps sets, side-lying hip abduction, calf raises, supine straight-leg raises, long-arc quadriceps sets (90–45° knee flexion) and quarter squats (30,15,15,15) | - | 30 s between sets | 24 weeks (2–3 times/week) |
3. Results
3.1. Characteristics of the Study
3.2. Participants Characteristics
3.3. Intervention Characteristics
3.4. Outcomes Assessment
3.5. Risk of Bias and Quality of Evidence Assessment
3.6. Muscle Strength
3.7. Muscle Size
3.8. Perceived Pain
4. Discussion
4.1. Low-Load Blood Flow Restriction Training and Muscle Strength
4.2. Low-Load Blood Flow Restriction Training and Muscle Volume
4.3. Influence of Low-Load Blood Flow Restriction Training on Perceived Pain
4.4. Strength and Limitations
4.5. Future Prospective
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A. Search Strategy
References
- Brych, V.; Vasylynets, M.; Dub, M. Some aspects of the potential adherence to rehabilitation of patients with musculoskeletal injuries. Wiad. Lek. 2022, 75, 1998–2002. [Google Scholar] [CrossRef] [PubMed]
- Jin, Z.; Wang, D.; Zhang, H.; Liang, J.; Feng, X.; Zhao, J.; Sun, L. Incidence trend of five common musculoskeletal disorders from 1990 to 2017 at the global, regional and national level: Results from the Global Burden of Disease Study 2017. Ann. Rheum. Dis. 2020, 79, 1014–1022. [Google Scholar] [CrossRef]
- Xu, D.; Zhou, H.; Quan, W.; Ma, X.; Chon, T.E.; Fernandez, J.; Gusztav, F.; Kovács, A.; Baker, J.S.; Gu, Y. New Insights Optimize Landing Strategies to Reduce Lower Limb Injury Risk. Cyborg Bionic Syst. 2024, 5, 0126. [Google Scholar] [CrossRef]
- Mason, J.S.; Owens, J.G.; Brown, W.J. Blood flow restriction training: Current and future applications for the rehabilitation of musculoskeletal injuries. Tech. Orthop. 2018, 33, 71. [Google Scholar] [CrossRef]
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 2006–2017. [Google Scholar] [CrossRef]
- Gehrig, L.M.B. Orthopedic surgery. Am. J. Surg. 2011, 202, 364–368. [Google Scholar] [CrossRef]
- Angelliaume, A.; Legallois, Y.; Harly, E.; Dartus, J.; Lavignac, P.; Chammas, P.-E.; Meynard, P. Orthopaedic and trauma surgery in the time of COVID-19 in France: A nationwide survey. Orthop. Traumatol. Surg. Res. 2023, 109, 103423. [Google Scholar] [CrossRef]
- Hughes, L.; Paton, B.; Rosenblatt, B.; Gissane, C.; Patterson, S.D. Blood flow restriction training in clinical musculoskeletal rehabilitation: A systematic review and meta-analysis. Br. J. Sports Med. 2017, 51, 1003–1011. [Google Scholar] [CrossRef]
- Norte, G.; Rush, J.; Sherman, D. Arthrogenic muscle inhibition: Best evidence, mechanisms, and theory for treating the unseen in clinical rehabilitation. J. Sport Rehabil. 2022, 31, 717–735. [Google Scholar] [CrossRef]
- Pietrosimone, B.; Lepley, A.S.; Kuenze, C.; Harkey, M.S.; Hart, J.M.; Blackburn, J.T.; Norte, G. Arthrogenic muscle inhibition following anterior cruciate ligament injury. J. Sport Rehabil. 2022, 31, 694–706. [Google Scholar] [CrossRef]
- Wilkinson, B.G.; Donnenwerth, J.J.; Peterson, A.R. Use of Blood Flow Restriction Training for Postoperative Rehabilitation. Curr. Sports Med. Rep. 2019, 18, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Gerber, J.P.; Marcus, R.L.; Leland, E.D.; Lastayo, P.C. The use of eccentrically biased resistance exercise to mitigate muscle impairments following anterior cruciate ligament reconstruction: A short review. Sports Health 2009, 1, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Nitzsche, N.; Stäuber, A.; Tiede, S.; Schulz, H. The effectiveness of blood-flow restricted resistance training in the musculoskeletal rehabilitation of patients with lower limb disorders: A systematic review and meta-analysis. Clin. Rehabil. 2021, 35, 1221–1234. [Google Scholar] [CrossRef]
- Watson, R.; Sullivan, B.; Stone, A.; Jacobs, C.; Malone, T.; Heebner, N.; Noehren, B. Blood Flow Restriction Therapy: An Evidence-Based Approach to Postoperative Rehabilitation. JBJS Rev. 2022, 10, e22.00062. [Google Scholar] [CrossRef]
- Buckthorpe, M.; Gokeler, A.; Herrington, L.; Hughes, M.; Grassi, A.; Wadey, R.; Patterson, S.; Compagnin, A.; La Rosa, G.; Della Villa, F. Optimising the Early-Stage Rehabilitation Process Post-ACL Reconstruction. Sports Med. 2024, 54, 49–72. [Google Scholar] [CrossRef]
- Pua, Y.H.; Mentiplay, B.F.; Clark, R.A.; Ho, J.Y. Associations Among Quadriceps Strength and Rate of Torque Development 6 Weeks Post Anterior Cruciate Ligament Reconstruction and Future Hop and Vertical Jump Performance: A Prospective Cohort Study. J. Orthop. Sports Phys. Ther. 2017, 47, 845–852. [Google Scholar] [CrossRef]
- Slysz, J.T.; Burr, J.F. The Effects of Blood Flow Restricted Electrostimulation on Strength and Hypertrophy. J. Sport Rehabil. 2018, 27, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Takarada, Y.; Takazawa, H.; Sato, Y.; Takebayashi, S.; Tanaka, Y.; Ishii, N. Effects of resistance exercise combined with moderate vascular occlusion on muscular function in humans. J. Appl. Physiol. 2000, 88, 2097–2106. [Google Scholar] [CrossRef]
- Ladlow, P.; Coppack, R.J.; Dharm-Datta, S.; Conway, D.; Sellon, E.; Patterson, S.D.; Bennett, A.N. Low-load resistance training with blood flow restriction improves clinical outcomes in musculoskeletal rehabilitation: A single-blind randomized controlled trial. Front. Physiol. 2018, 9, 1269. [Google Scholar] [CrossRef]
- Lixandrão, M.E.; Ugrinowitsch, C.; Berton, R.; Vechin, F.C.; Conceição, M.S.; Damas, F.; Libardi, C.A.; Roschel, H. Magnitude of muscle strength and mass adaptations between high-load resistance training versus low-load resistance training associated with blood-flow restriction: A systematic review and meta-analysis. Sports Med. 2018, 48, 361–378. [Google Scholar] [CrossRef]
- Loenneke, J.P.; Wilson, J.M.; Marín, P.J.; Zourdos, M.C.; Bemben, M.G. Low intensity blood flow restriction training: A meta-analysis. Eur. J. Appl. Physiol. 2012, 112, 1849–1859. [Google Scholar] [CrossRef]
- Lorenz, D.S.; Bailey, L.; Wilk, K.E.; Mangine, R.E.; Head, P.; Grindstaff, T.L.; Morrison, S. Blood flow restriction training. J. Athl. Train. 2021, 56, 937–944. [Google Scholar] [PubMed]
- Saraf, A.; Goyal, M.; Goyal, K. Blood Flow Restriction Training—An Overview and Implication in New Generation Physical Therapy: A Narrative Review. J. Lifestyle Med. 2022, 12, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Slysz, J.; Stultz, J.; Burr, J.F. The Efficacy of Blood Flow Restricted Exercise: A Systematic Review & Meta-analysis. J. Sci. Med. Sport 2016, 19, 669–675. [Google Scholar] [CrossRef]
- Vopat, B.G.; Vopat, L.M.; Bechtold, M.M.; Hodge, K.A. Blood Flow Restriction Therapy: Where We Are and Where We Are Going. J. Am. Acad. Orthop. Surg. 2020, 28, E493–E500. [Google Scholar] [CrossRef]
- Miller, B.C.; Tirko, A.W.; Shipe, J.M.; Sumeriski, O.R.; Moran, K. The systemic effects of blood flow restriction training: A systematic review. Int. J. Sports Phys. Ther. 2021, 16, 978–990. [Google Scholar] [CrossRef]
- Cognetti, D.J.; Sheean, A.J.; Owens, J.G. Blood flow restriction therapy and its use for rehabilitation and return to sport: Physiology, application, and guidelines for implementation. Arthrosc. Sports Med. Rehabil. 2022, 4, e71–e76. [Google Scholar] [CrossRef] [PubMed]
- Centner, C.; Wiegel, P.; Gollhofer, A.; König, D. Effects of blood flow restriction training on muscular strength and hypertrophy in older individuals: A systematic review and meta-analysis. Sports Med. 2019, 49, 95–108. [Google Scholar] [CrossRef]
- Song, J.S.; Spitz, R.W.; Yamada, Y.; Bell, Z.W.; Wong, V.; Abe, T.; Loenneke, J.P. Exercise-induced Hypoalgesia and Pain Reduction Following Blood Flow Restriction: A Brief Review. Phys. Ther. Sport 2021, 50, 89–96. [Google Scholar]
- Ohta, H.; Kurosawa, H.; Ikeda, H.; Iwase, Y.; Satou, N.; Nakamura, S. Low-Load Resistance Muscular Training with Moderate Restriction of Blood Flow After Anterior Cruciate Ligament Reconstruction. Acta Orthop. Scand. 2003, 74, 62–68. [Google Scholar] [CrossRef]
- Wengle, L.; Migliorini, F.; Leroux, T.; Chahal, J.; Theodoropoulos, J.; Betsch, M. The Effects of Blood Flow Restriction in Patients Undergoing Knee Surgery: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2022, 50, 2824–2833. [Google Scholar] [CrossRef]
- Minniti, M.C.; Statkevich, A.P.; Kelly, R.L.; Rigsby, V.P.; Exline, M.M.; Rhon, D.I.; Clewley, D. The safety of blood flow restriction training as a therapeutic intervention for patients with musculoskeletal disorders: A systematic review. Am. J. Sports Med. 2020, 48, 1773–1785. [Google Scholar] [CrossRef]
- Hughes, L.; Rosenblatt, B.; Haddad, F.; Gissane, C.; McCarthy, D.; Clarke, T.; Ferris, G.; Dawes, J.; Paton, B.; Patterson, S.D. Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: A UK National Health Service randomized controlled trial. Sports Med. 2019, 49, 1787–1805. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Lewin, S.; Bohren, M.; Rashidian, A.; Munthe-Kaas, H.; Glenton, C.; Colvin, C.J.; Garside, R.; Noyes, J.; Booth, A.; Tunçalp, Ö.; et al. Applying GRADE-CERQual to qualitative evidence synthesis findings—Paper 2: How to make an overall CERQual assessment of confidence and create a Summary of Qualitative Findings table. Implement. Sci. 2018, 13, 68. [Google Scholar] [CrossRef]
- Deeks, J.J.; Higgins, J.P.; Altman, D.G.; Group, C.S.M. Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2019; pp. 241–284. [Google Scholar]
- Vieira de Melo, R.F.; Komatsu, W.R.; de Freitas, M.S.; Vieira de Melo, M.E.; Cohen, M. Comparison of Quadriceps and Hamstring Muscle Strength after Exercises with and without Blood Flow Restriction Following Anterior Cruciate Ligament Surgery: A Randomized Controlled Trial. J. Rehabil. Med. 2022, 54, jrm00337. [Google Scholar] [CrossRef]
- Jack, R.A.; Lambert, B.S.; Hedt, C.A.; Delgado, D.; Goble, H.; McCulloch, P.C. Blood flow restriction therapy preserves lower extremity bone and muscle mass after ACL reconstruction. Sports Health A Multidiscip. Approach 2023, 15, 361–371. [Google Scholar] [CrossRef]
- Li, X.; Li, J.; Qing, L.; Wang, H.; Ma, H.; Huang, P. Effect of quadriceps training at different levels of blood flow restriction on quadriceps strength and thickness in the mid-term postoperative period after anterior cruciate ligament reconstruction: A randomized controlled external pilot study. BMC Musculoskelet. Disord. 2023, 24, 360. [Google Scholar] [CrossRef]
- Park, H.-S.; Song, J.-S.; Kim, E.-K. Effects of low-intensity resistance exercise with blood flow restriction after high tibial osteotomy in middle-aged women. Medicine 2022, 101, e32294. [Google Scholar] [CrossRef] [PubMed]
- Ke, J.; Zhou, X.; Yang, Y.; Shen, H.; Luo, X.; Liu, H.; Gao, L.; He, X.; Zhang, X. Blood flow restriction training promotes functional recovery of knee joint in patients after arthroscopic partial meniscectomy: A randomized clinical trial. Front. Physiol. 2022, 13, 1015853. [Google Scholar] [CrossRef]
- Mason, J.S.; Crowell, M.S.; Brindle, R.A.; Dolbeer, J.A.; Miller, E.M.; Telemeco, T.A.; Goss, D.L. The effect of blood flow restriction training on muscle atrophy following meniscal repair or chondral restoration surgery in active duty military: A randomized controlled trial. J. Sport Rehabil. 2022, 31, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Tennent, D.J.; Hylden, C.M.; Johnson, A.E.; Burns, T.C.; Wilken, J.M.; Owens, J.G. Blood Flow Restriction Training after Knee Arthroscopy: A Randomized Controlled Pilot Study. Clin. J. Sport Med. 2017, 27, 245–252. [Google Scholar] [CrossRef]
- Fan, Y.; Bai, D.; Cheng, C.; Tian, G. The effectiveness and safety of blood flow restriction training for the post-operation treatment of distal radius fracture. Ann. Med. 2023, 55, 2240329. [Google Scholar] [CrossRef]
- Sgromolo, N.M.; Cancio, J.M.; Rhee, P.C. Safety and Efficacy of Blood Flow Restriction Therapy after Operative Management of Distal Radius Fractures: A Randomized Controlled Study. J. Wrist Surg. 2020, 9, 345–352. [Google Scholar] [CrossRef]
- Erickson, L.N.; Owen, M.K.; Casadonte, K.R.; Anatova, T.; Lucas, K.; Spencer, K.; Brightwell, B.D.; Graham, M.C.; White, M.S.; Thomas, N.T.; et al. The Efficacy of Blood Flow Restriction Training to Improve Quadriceps Muscle Function after ACL Reconstruction. Med. Sci. Sports Exerc. 2024, 57, 227–237. [Google Scholar] [CrossRef] [PubMed]
- Jung, W.S.; Kim, S.H.; Nam, S.S.; Kim, J.W.; Moon, H.W. Effects of Rehabilitation Exercise with Blood Flow Restriction after Anterior Cruciate Ligament Reconstruction. Appl Sci. 2022, 12, 12058. [Google Scholar] [CrossRef]
- Okoroha, K.R.; Tramer, J.S.; Khalil, L.S.; Jildeh, T.R.; Abbas, M.J.; Buckley, P.J.; Lindell, C.; Moutzouros, V. Effects of a Perioperative Blood Flow Restriction Therapy Program on Early Quadriceps Strength and Patient-Reported Outcomes After Anterior Cruciate Ligament Reconstruction. Orthop. J. Sports Med. 2023, 11, 23259671231209694. [Google Scholar] [CrossRef]
- Curley, A.J.; Conroy, C.M.; West, R.V.; Chang, E.S. Postoperative use of blood flow restriction in orthopedics. Orthopedics 2021, 44, e694–e698. [Google Scholar] [CrossRef]
- Baker, B.S.; Stannard, M.S.; Duren, D.L.; Cook, J.L.; Stannard, J.P. Does blood flow restriction therapy in patients older than age 50 result in muscle hypertrophy, increased strength, or greater physical function? A systematic review. Clin. Orthop. Relat. Res. 2020, 478, 593–606. [Google Scholar] [CrossRef] [PubMed]
- Koc, B.B.; Truyens, A.; Heymans, M.J.L.F.; Jansen, E.J.P.; Schotanus, M.G.M. Effect of Low-Load Blood Flow Restriction Training After Anterior Cruciate Ligament Reconstruction: A Systematic Review. Int. J. Sports Phys. Ther. 2022, 17, 334–346. [Google Scholar] [CrossRef]
- Spada, J.M.; Paul, R.W.; Tucker, B.S. Blood Flow Restriction Training Preserves Knee Flexion and Extension Torque Following Anterior Cruciate Ligament Reconstruction: A Systematic Review. J. Orthop. 2022, 34, 233–239. [Google Scholar] [CrossRef]
- Kilgas, M.A.; Lytle, L.L.M.; Drum, S.N.; Elmer, S.J. Exercise with Blood Flow Restriction to Improve Quadriceps Function Long After ACL Reconstruction. Int. J. Sports Med. 2019, 40, 650–656. [Google Scholar] [CrossRef] [PubMed]
- Noyes, F.R.; Barber-Westin, S.D.; Sipes, L. Blood Flow Restriction Training Can Improve Peak Torque Strength in Chronic Atrophic Postoperative Quadriceps and Hamstrings Muscles. Arthrosc. J. Arthrosc. Relat. Surg. 2021, 37, 2860–2869. [Google Scholar] [CrossRef]
- Colapietro, M.; Portnoff, B.; Miller, S.J.; Sebastianelli, W.; Vairo, G.L. Effects of blood flow restriction training on clinical outcomes for patients with ACL reconstruction: A systematic review. Sports Health A Multidiscip. Approach 2023, 15, 260–273. [Google Scholar] [CrossRef]
- McGinniss, J.H.; Mason, J.S.; Morris, J.B.; Pitt, W.; Miller, E.M.; Crowell, M.S. The Effect of Blood Flow Restriction Therapy on Shoulder Function Following Shoulder Stabilization Surgery: A Case Series. Int. J. Sports Phys. Ther. 2022, 17, 1144–1155. [Google Scholar] [CrossRef]
- Wentzell, M. Post-operative rehabilitation of a distal biceps brachii tendon reattachment in a weightlifter: A case report. J. Can. Chiropr. Assoc. 2018, 62, 193–201. [Google Scholar]
- Charles, D.; White, R.; Reyes, C.; Palmer, D. A systematic review of the effects of blood flow restriction training on quadriceps muscle atrophy and circumference post ACL reconstruction. Int. J. Sports Phys. Ther. 2020, 15, 882–891. [Google Scholar] [CrossRef]
- Lu, Y.; Patel, B.H.; Kym, C.; Nwachukwu, B.U.; Beletksy, A.; Forsythe, B.; Chahla, J. Perioperative Blood Flow Restriction Rehabilitation in Patients Undergoing ACL Reconstruction: A Systematic Review. Orthop. J. Sports Med. 2020, 8, 232596712090682. [Google Scholar] [CrossRef]
- Iversen, E.; Røstad, V.; Larmo, A. Intermittent blood flow restriction does not reduce atrophy following anterior cruciate ligament reconstruction. J. Sport Health Sci. 2016, 5, 115–118. [Google Scholar] [CrossRef] [PubMed]
- Hughes, L.; Patterson, S.D.; Haddad, F.; Rosenblatt, B.; Gissane, C.; McCarthy, D.; Clarke, T.; Ferris, G.; Dawes, J.; Paton, B. Examination of the comfort and pain experienced with blood flow restriction training during post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: A UK National Health Service trial. Phys. Ther. Sport 2019, 39, 90–98. [Google Scholar] [CrossRef] [PubMed]
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| (P) Participants | Patients who underwent musculoskeletal surgery | Children (<16 years) and the elderly (>75 years) Heterogeneous sample of patients |
| (I) Interventions | Low Load (<30% RM) Blood Flow Restriction Training | Heterogeneous sample of surgical interventions Home-based intervention Presurgical Intervention |
| (C) Comparisons | - | - |
| (O) Outcomes | Two variables at least, between muscle strength, muscle volume and pain, were analysed | |
| Study characteristics | Randomized Controlled Trial (RCT) or Randomized Controlled Pillot Trial (RCPT) | Conference posters or incomplete articles Missing relevant data |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos-Pérez, D.; Ochiana, N.; Carrasco-Páez, L.; Martínez-Díaz, I.C. Effects of Low Load Blood Flow Restriction Training on Post-Surgical Musculoskeletal Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Appl. Sci. 2025, 15, 3996. https://doi.org/10.3390/app15073996
Santos-Pérez D, Ochiana N, Carrasco-Páez L, Martínez-Díaz IC. Effects of Low Load Blood Flow Restriction Training on Post-Surgical Musculoskeletal Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Applied Sciences. 2025; 15(7):3996. https://doi.org/10.3390/app15073996
Chicago/Turabian StyleSantos-Pérez, Diego, Nicolae Ochiana, Luis Carrasco-Páez, and Inmaculada C. Martínez-Díaz. 2025. "Effects of Low Load Blood Flow Restriction Training on Post-Surgical Musculoskeletal Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials" Applied Sciences 15, no. 7: 3996. https://doi.org/10.3390/app15073996
APA StyleSantos-Pérez, D., Ochiana, N., Carrasco-Páez, L., & Martínez-Díaz, I. C. (2025). Effects of Low Load Blood Flow Restriction Training on Post-Surgical Musculoskeletal Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Applied Sciences, 15(7), 3996. https://doi.org/10.3390/app15073996














