1. Introduction
Cardiorespiratory fitness (CRF) is a strong health indicator [
1,
2,
3,
4,
5,
6]. A low CRF level entails the risk of adverse cardiovascular events [
2]. In adults, CRF is regarded as a predictor of general mortality and it is negatively correlated with hypertension and diabetes [
7,
8,
9,
10,
11,
12,
13]. Low CRF in young people is related e.g., to obesity, which increases the risk of cardiovascular diseases [
14] and metabolic syndrome characteristics [
15,
16]. Studies have also revealed that improved CRF leads to better health results regardless of body mass index (BMI) [
9]. A higher physical fitness index in adults significantly reduces the metabolic risk for a particular body fat level [
17]. Preventive measures against cardiovascular diseases which are intended to optimise CRF are also implemented in low-risk groups (10% risk of ischaemic heart disease occcurrence within the next 10 years) [
18,
19,
20]. The authors of many studies emphasise the significance of lifelong physical activity to improve or maintain the appropriate level of CRF [
19,
21,
22]. In early adulthood, a high CRF level provides the most benefit related to survival. The maximum oxygen consumption (VO
2max) is the main CRF criterion measurement [
15]. A direct measurement of the factor is regarded as the best indicator of aerobic fitness [
23,
24]. Since the implementation of VO
2max direct measurement is quite complex, maximal oxygen uptake tends to be forecasted based on indirect measurements, using predictive models [
23,
25,
26]. A 20 m shuttle run test (20 m SRT) is often used to measure cardivascular fitness [
22,
23,
27,
28]. Therefore, it seems reasonable to model the index using various mathematical methods. A predictive model may help to identify the level of CRF without costly equipment and specialised research time. The prediction of the VO
2max parameter may become an important element of health monitoring and fitness improvement in young healthy people.
In the literature, there are many papers that focus on the prediction of this indicator using, among other factors, the results of resistance tests, anthropometric parameters or physical activity indicators [
15,
23,
29]. Therefore, the VO
2max predictive models may be classified as both exercise and non-exercise models. Exercise models make predictions based on the result of an endurance test with maximum or submaximal intensity [
15,
23,
30,
31,
32,
33,
34]. In the literature, there are also prediction models based on ergometric tests [
35,
36]. The most popular predictors include age, sex and BMI [
25]. Most of the published models are based on multiple regression or machine learning methods.
In this paper, the authors present different models to predict VO2max based on the result of the 20 m shuttle run test and anthropometric parameters. The aim of the work is to determine the optimal predictive model to estimate VO2max for young healthy people (students). The models may be used e.g., by a Physical Education teacher for CRF monitoring. To the best of our knowledge, these are the first studies for such a large group (n = 308) using the direct measurement of oxygen uptake. Data was collected at five large universities in various parts of Poland.
3. Results
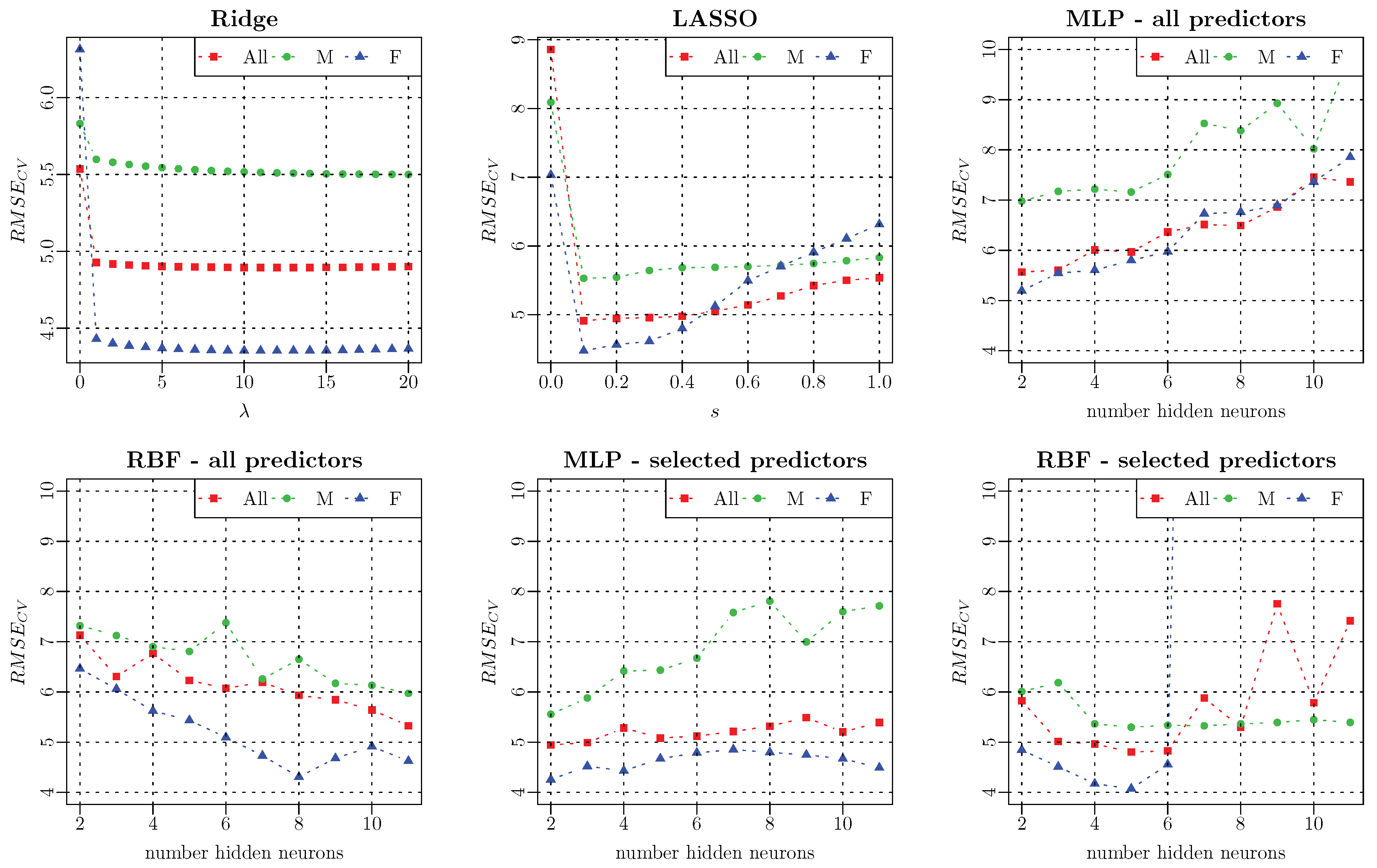
All models were evaluated using the prediction error
calculated during cross-validation (
Table 3 and
Table 4).
Figure 1 presents validation errors in relation to the parameters of the models. For Ridge models, this parameter is the lambda parameter
with a step of 1, in the case of the Lasso regression, the parameter
has a step of
. Artificial neural networks (MLP and RBF) were evaluated for the number of neurons in the hidden layer
.
By analysing the results for the models identified based on all variables (
Table 3), it may be observed that the most accurate model for women was obtained using the RBF type neural network with eight neurons in the hidden layer (
[mL·kg
−1·min
−1]). The best model making predictions among men were based on the whole collection of variables which generates an error of
[mL·kg
−1·min
−1]. This was calculated with Ridge regression for
. A similar observation may be made for the most accurate model for all data where the Ridge regression (
) is also the one which generates the smallest error (
[mL·kg
−1·min
−1]). The following stage of the analysis involved variable selection methods to improve the predictive capacity of the presented models, determine optimal input collections, and consequently to identify the factors which determine the VO
2max prediction in the analysed group. The models determined by means of Lasso and stepwise regression were evaluated using LOOCV (
Table 4). The application of variable selection methods improved the predictive capacity of the OLS model. The error level for the female group was
[mL·kg
−1·min
−1] when the bidirectional method was used, while, for males, the model obtained with forward regression turned out to be more precise—
[mL·kg
−1·min
−1]. For all data, the forward and bidirectional methods determined the same input data for which the error generated by the model amounted to
[mL·kg
−1·min
−1]. The identified input collections were used to calculate new neural networks (
Table 4). Neural networks for selected variables are characterised by a smaller prediction error than the networks identified based on all variables. RBF models generate the value of
[mL·kg
−1·min
−1] for women,
[mL·kg
−1·min
−1] for men and
[mL·kg
−1·min
−1] for all participants. The models obtained for females and males demonstrate the poorest fitness among all analysed models, while the model for all data is worse than the OLS model (forward, bidirectional). The equations for optimal linear models are presented in
Table 5.
4. Discussion
The paper presents mathematical models for the prediction of VO
2max based on a 20 m SRT and anthropometric parameters. All models were developed and cross-validated using a sample of 308 healthy young people (aged 19–27). The models obtained are classified as “maximal models” [
49] and that is why errors in this group of models were compared with errors presented by other authors. The majority of papers with VO
2max maximal predictive models present a common model for females and males [
15,
30,
31]. An analysis of errors for predictive models in which sex was the input variable revealed that the error
[mL·kg
−1·min
−1] is a result which does not deviate from errors presented in other papers (
Table 6). The calculated model is more accurate than the model proposed by Mahar [
30] and Silva [
15]. It is however less accurate than the models proposed in papers by Akay [
31,
50]. The optimal model for the whole group used the following factors for prediction: sex (
), distance (20 m SRT) (
), body height (
) and content of adipose tissue (
).
In young males and females, regular physical exercise definitely improves CRF by increasing VO
2max and decreasing body fat percentage, leading to a better quality of life [
51,
52,
53,
54]. The VO
2max level varies significantly among individuals and mainly depends on genetic aspects, sex, age anthropometric properties of health, lifestyle and training status [
51,
52,
55,
56,
57,
58,
59]. Reference values may change over time and should be regularly updated/validated [
60]. The data may be found in papers analysing the results of cardiac stress tests carried out for large groups of healthy people [
8,
60,
61]. Typical values of VO
2max in young healthy male students amount to about 50 [mL·kg
−1·min
−1], and in women to about 40 [mL·kg
−1·min
−1] [
62]. CRF in terms of aerobic capacity is affected by the composition of the body. Low CRF in young adults with increased body fat could be a factor in the development of cardiovascular comorbidities later in middle age and old age [
63]. Bioimpedance is an alternative method to estimate the percentage of body fat, when compared to DXA (Dual Energy X-ray Absoptiometry), it is a gold standard method, as there is a high level of agreement [
64]. Simple use, lack of radiation and the relatively low cost of bioelectric impedance suggests that it is a feasible analysis for body fat measurement, especially in large populations [
65].
Besides a common model for females and males, this paper determines separate models for each group. It may be observed that the models for females are characterised by a significantly smaller error as compared to those for men. The RBF neural network with eight neurons in the hidden layer turned out to be the most accurate. It generates an error of
[mL·kg
−1·min
−1]. Bandyopadhyay [
66] presented similar studies in his paper. He described a multiple regression model whose prediction error amounted to 1.27 [mL·kg
−1·min
−1] (
Table 6). The model used speed and body height as predictors. Other studies concerning prediction among females were published by Chatterjee [
23], who calculated a model generating an error of 0.53 [mL·kg
−1·min
−1]. The model used only the maximum speed. When the errors obtained in this paper are compared with errors obtained by other authors, it may be concluded that their errors were significantly smaller. It shall be emphasized that the population analysed in the study was much larger and more diversified for the VO
2max level (
[mL·kg
−1·min
−1]). Moreover, cross-validation was used in the paper for evaluation, while in the papers discussed the model quality was evaluated by means of standard errors. That is why direct comparisons are impossible. The model calculated for women has the simplest structure and includes: distance (20 m SRT) (
), body height (
) and body fat (
). The model contains the same variables as the model for all participants save for sex, which is a constant.
Similarly to the female group, the RBF network turned out to be the best model for males, whereby in the male group the optimal network consists only of two neurons in the hidden layer. The network generates an error level of
[mL·kg
−1·min
−1]. Comparing the obtained results with other papers where models were calculated only for males, it may be observed that the parameter value does not deviate significantly from the published results (
Table 6). The optimal model for males calculated in the study generated greater errors than the models presented by Machado and Demadai [
67] (4.10 [mL·kg
−1·min
−1]) and Bandyopdhyay [
68] (1.41 [mL·kg
−1·min
−1]). The error obtained is still smaller than the error generated using the Costa model [
69] (7.20 [mL·kg
−1·min
−1]).
When comparing the errors of the calculated models, it should be emphasized that a direct comparison of the errors obtained in the studies is valid only when the same maximal test is used and when a similar study sample is employed [
70]. Therefore, it seems that the results obtained may only be compared with models which use 20 m SRT and are developed based on a population of healthy people aged 19–27 years, and are cross-validated. Cross-validation does not evaluate the fitness error but a generalisation error.
The model determined for males consisted of the following variables: distance (20 m SRT) (
), waist circumference (NIH protocol) (
), WHR (NIH protocol) (
), FFMI (
) and BSA (
). The obtained collection of predicators is not incidental and the significance of each variance for VO
2max is reflected in the literature. Waist circumference and WHR are popular indicators used for the evaluation of cardiovascular diseases [
71]. Waist circumference is also a predictor of visceral fat and indicator of central obesity [
72]. There remains no uniformly accepted measurement protocol, resulting in a variety of techniques employed throughout the published literature [
73,
74]. The most commonly used are four measurements of waist circumference defined by specific anatomic landmarks: (1) immediately below the lowest ribs, (2) at the narrowest waist, (3) the midpoint between the lowest rib and iliac crest, and (4) immediately above the iliac crest [
75,
76]. Measurements made at the umbilicus are also commonly used in clinical and research settings [
74]. Besides DXA and bioimpedance, different indicators based on anthropometric measurements are used for the evaluation of body fat content. The indicator that is often used in obesity studies is BMI [
39,
71,
77]. However, it presents some limitations. It neither evaluates the content of adipose tissue and its distribution in the body nor does it differentiate body fat content depending on age, sex and ethnic origin [
71,
78]. The identification of adipose tissue location is necessary to detect visceral (central) obesity, which increases the risk of cardiovascular diseases [
79]. That is why the qualitative supplementation of the classical concept of BMI may help to create reference values for FFMI for a given age category [
80]. BSA, a method for describing body size, is commonly used in medicine as a biometric unit [
81,
82].
The use of a predictive model makes it possible to determine the level of CFR without using expensive equipment and specialized research teams. The prediction of the VO2max parameter may be useful as an element of monitoring the health and physical performance of students of young healthy people.
The strongest points of presented paper are:
a large research group representing the population,
VO2max measurements made using direct methods,
the use of a large set of variables to determine the optimal predictors for VO2max estimation,
and obtaining a relatively small VO2max estimation error.
The limitations of the study are related to the using models in practice. VO2max estimation by the proposed models should be performed for healthy people of the same age as the research group.