Development of the Dyskinesia Impairment Mobility Scale to Measure Presence and Severity of Dystonia and Choreoathetosis during Powered Mobility in Dyskinetic Cerebral Palsy
Abstract
:Featured Application
Abstract
1. Introduction
2. Materials and Methods
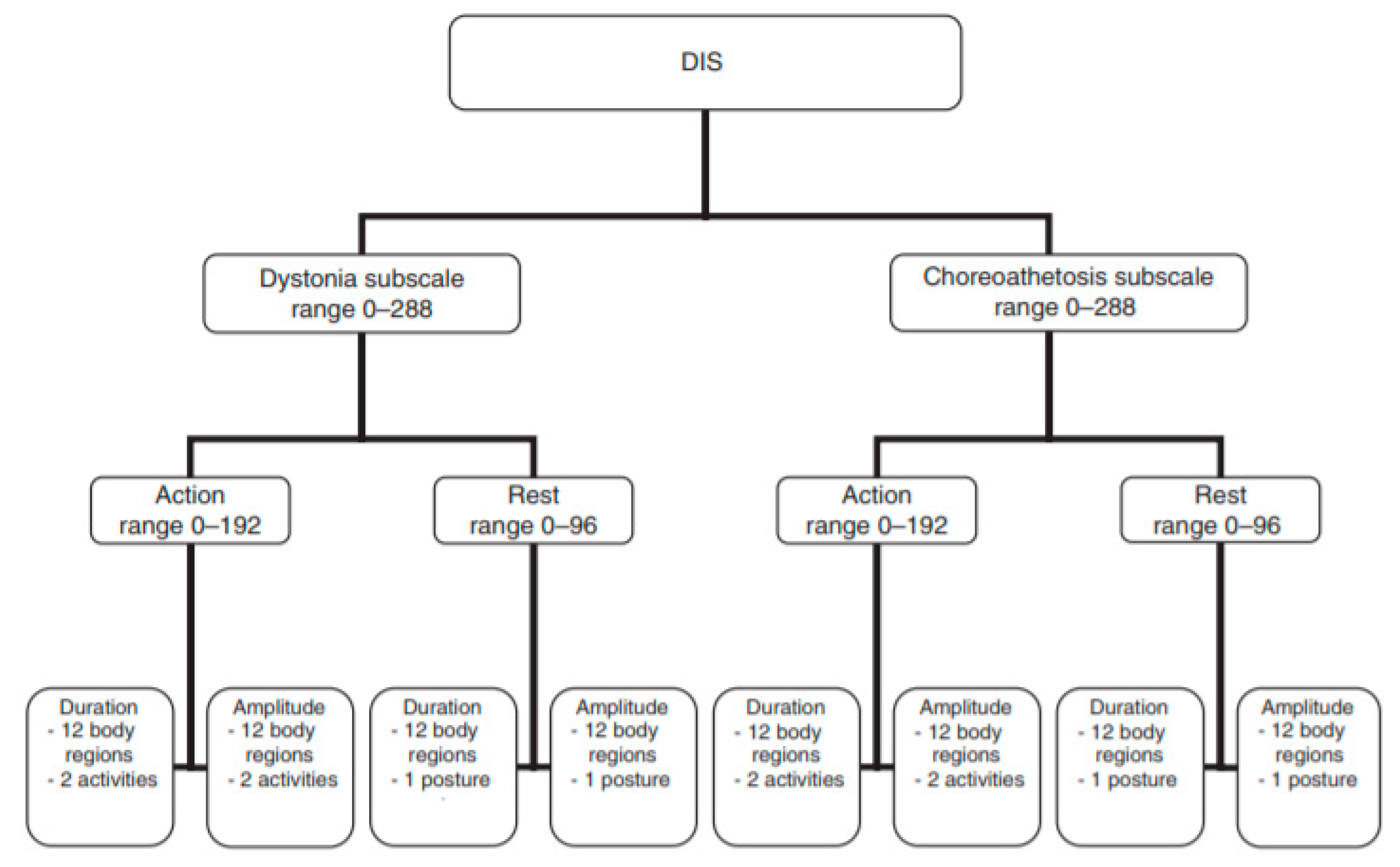
2.1. Development of the Dyskinesia Impairment Mobility Scale (DIMS)
2.2. Reliability and Validity
2.2.1. Participants
2.2.2. Data Collection
2.2.3. Procedure of Scoring and Analyzing data
2.2.4. Statistical Analysis
3. Results
3.1. Interrater Reliability of the DIMS
3.2. Test-Retest Reliability of the DIMS
3.3. Internal Consistency
3.4. Concurrent Validity
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
Appendix B
| Gender (M/F) | Age (yo) | GMFCS | MACS | Experience with Powered Mobility (Years) | |
|---|---|---|---|---|---|
| P01 | M | 19 | 4 | 4 | 10 |
| P02 | M | 16 | 4 | 4 | 6 |
| P03 | F | 6 | 4 | 4 | 1.5 |
| P04 | F | 21 | 5 | 4 | 6 |
| P05 | F | 8 | 4 | 5 | 1 |
Appendix C


Appendix D
| Duration | Amplitude | ∑(D + A) | ||||
|---|---|---|---|---|---|---|
| ICC | 95% CI; p–value | ICC | 95% CI; p–value | ICC | 95% CI; p–value | |
| Dystonia | 0.91 | 0.74–0.98; 0.000 | 0.89 | 0.69–0.97; 0.000 | 0.89 | 0.70–0.97; 0.000 |
| Choreoathetosis | 0.95 | 0.85–0.99; 0.000 | 0.96 | 0.90–0.99; 0.000 | 0.96 | 0.88–0.99; 0.000 |
| DIS Training | 0.94 | 0.83–0.98; 0.000 | 0.95 | 0.86–0.99; 0.000 | 0.96 | 0.88–0.99; 0.000 |
Appendix E
| Duration | Amplitude | ∑(D + A) | |||||
|---|---|---|---|---|---|---|---|
| ICC | 95% CI; p-value | ICC | 95% CI; p-value | ICC | 95% CI; p-value | ||
| DIMS | |||||||
| Total score | 0.81 | 0.00–0.98; 0.059 | 0.88 | 0.17–0.99; 0.028 | 0.87 | 0.03–0.99; 0.037 | |
| DIMS-D SUBSCALE | |||||||
| 1 | Neck | 0.82 | 0.00–198; 0.072 | 0.97 | 0.78–0.99; 0.001 | 0.92 | 0.37–0.99; 0.018 |
| 2 | Arm RP | 0.94 | 0.43–0.99; 0.005 | 0.97 | 0.57–0.99; 0.001 | 0.96 | 0.45–0.99; 0.001 |
| 3 | Arm LP | 0.64 | 0.00–0.96; 0.070 | 0.75 | 0.00–0.97; 0.007 | 0.69 | 0.00–0.96; 0.023 |
| 4 | Arm RD | 0.87 | 0.00–0.99; 0.051 | 0.91 | 0.18–0.90; 0.026 | 0.89 | 0.00–0.99; 0.036 |
| 5 | Arm LD | 0.88 | 0.09–0.99; 0.016 | 0.83 | 0.00–0.98; 0.066 | 0.88 | 0.14–0.99; 0.030 |
| Total score | 0.90 | 0.26–0.99; 0.022 | 0.94 | 0.35–0.99; 0.004 | 0.93 | 0.42–0.99; 0.006 | |
| DIMS-CA SUBSCALE | |||||||
| 1 | Neck | 0.96 | 0.66–0.99; 0.006 | 0.96 | 0.54–0.99; 0.008 | 0.96 | 0.63–0.99; 0.006 |
| 2 | Arm RP | 0.79 | 0.00–0.98; 0.087 | 0.86 | 0.04–0.98; 0.032 | 0.78 | 0.00–0.98; 0.084 |
| 3 | Arm LP | * | * | * | * | * | * |
| 4 | Arm RD | 0.77 | 0.00–0.98; 0.115 | 0.87 | 0.00–0.99; 0.048 | 0.83 | 0.00–0.98; 0.073 |
| 5 | Arm LD | 0.50 | 0.00–0.95; 0.290 | 0.67 | 0.00–0.97; 0.177 | 0.60 | 0.00–0.96; 0.229 |
| Total score | 0.62 | 0.00–0.96; 0.217 | 0.75 | 0.00–0.98; 0.130 | 0.71 | 0.00–0.97; 0.160 | |
References
- Livingstone, R.; Field, D. Systematic review of power mobility outcomes for infants, children and adolescents with mobility limitations. Clin. Rehabil. 2014, 28, 954–964. [Google Scholar] [CrossRef] [PubMed]
- Casey, J.; Paleg, G.; Livingstone, R. Facilitating Child Participation through Power Mobility. Br. J. Occup. Ther. 2013, 76, 158–160. [Google Scholar] [CrossRef]
- Livingstone, R.; Field, D. The child and family experience of power mobility: A qualitative synthesis. Dev. Med. Child Neurol. 2015, 57, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, R. A critical review of powered mobility assessment and training for children. Disabil. Rehabil. Assist. Technol. 2010, 5, 392–400. [Google Scholar] [CrossRef] [PubMed]
- Rodby–Bousquet, E.; Paleg, G.; Casey, J.; Wizert, A.; Livingstone, R. Physical risk factors influencing wheeled mobility in children with cerebral palsy: A cross-sectional study. BMC Pediatr. 2016, 16. [Google Scholar] [CrossRef]
- Sellier, E.; Platt, M.J.; Andersen, G.L.; Krageloh-Mann, I.; De La Cruz, J.; Cans, C. Decreasing prevalence in cerebral palsy: A multi-site European population-based study, 1980 to 2003. Dev. Med. Child Neurol. 2016, 58, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child Neurol. Suppl. 2007, 109, 8–14. [Google Scholar] [PubMed]
- Monbaliu, E.; Himmelmann, K.; Lin, J.P.; Ortibus, E.; Bonouvrie, L.; Feys, H.; Vermeulen, R.J.; Dan, B. Clinical presentation and management of dyskinetic cerebral palsy. Lancet Neurol. 2017, 16, 741–749. [Google Scholar] [CrossRef]
- Vanmechelen, I.; Bekteshi, S.; Bossier, K.; Feys, H.; Deklerck, J.; Monbaliu, E. Presence and severity of dystonia and choreoathetosis overflow movements in participants with dyskinetic cerebral palsy and their relation with functional classification scales. Disabil.Rehabil 2019, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Monbaliu, E.; De La Pena, M.G.; Ortibus, E.; Molenaers, G.; Deklerck, J.; Feys, H. Functional outcomes in children and young people with dyskinetic cerebral palsy. Dev. Med. Child Neurol. 2017, 59, 634–640. [Google Scholar] [CrossRef] [PubMed]
- Rodby-Bousquet, E.; Hägglund, G. Use of manual and powered wheelchair in children with cerebral palsy: A cross-sectional study. BMC Pediatr. 2010, 10, 59. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, R.; Paleg, G. Practice considerations for the introduction and use of power mobility for children. Dev. Med. Child Neurol 2014, 56, 210–221. [Google Scholar] [CrossRef] [PubMed]
- Giesbrecht, E.M.; Wilson, N.; Schneider, A.; Bains, D.; Hall, J.; Miller, W.C. Preliminary Evidence to Support a “Boot Camp” Approach to Wheelchair Skills Training for Clinicians. Arch. Phys. Med. Rehabil. 2015, 96, 1158–1161. [Google Scholar] [CrossRef] [PubMed]
- Monbaliu, E.; Ortibus, E.; De Cat, J.; Dan, B.; Heyrman, L.; Prinzie, P.; De Cock, P.; Feys, H. The Dyskinesia Impairment Scale: A new instrument to measure dystonia and choreoathetosis in dyskinetic cerebral palsy. Dev. Med. Child Neurol 2012, 54, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Monbaliu, E.; Ortibus, E.; Prinzie, P.; Dan, B.; De Cat, J.; De Cock, P.; Feys, H. Can the Dyskinesia Impairment Scale be used by inexperienced raters? A reliability study. Eur. J. Paediatr. Neurol. 2013, 17, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Vanmechelen, I.; Dan, B.; Feys, H.; Monbaliu, E. Test-retest reliability of the Dyskinesia Impairment Scale: Can dystonia and choreoathetosis be reliably measured over time in dyskinetic cerebral palsy? Dev. Med. Child Neurol. 2019. under review. [Google Scholar]
- Palisano, R.J.; Avery, L.; Gorter, J.W.; Galuppi, B.; McCoy, S.W. Stability of the Gross Motor Function Classification System, Manual Ability Classification System, and Communication Function Classification System. Dev. Med. Child Neurol. 2018, 60, 1026–1032. [Google Scholar] [CrossRef] [PubMed]
- Kirby, R.L.; Smith, C.; Routhier, F.; Best, K.L.; Cowan, R.; Giesbrecht, E.; Koontz, A.; MacKenzie, D.; Mortenson, B.; Parker, K.; et al. The Wheelchair Skills Program Manual Version 5.0. Available online: www.wheelchairskillsprogram.ca/eng/manual.php (accessed on 15 February 2018).
- Kinovea 0.8.15. Available online: www.kinovea.org (accessed on 10 September 2018).
- RIGBY, A.S. Statistical recommendations for papers submitted to Developmental Medicine & Child Neurology. Dev. Med. Child Neurol. 2010, 52, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice, 3rd ed.; Pearson/Prentice Hall: Upper Saddle River, NJ, USA, 2014. [Google Scholar]
- Gireaudeau, B. Negative Values of the Intraclass Correlation Coefficients Are Not Theoretically Possible. J. Clin. Epidemiol. 1996, 49, 1205–1206. [Google Scholar] [CrossRef]
- London King’s College. Available online: https://www.kcl.ac.uk/ioppn/depts/BiostatisticsHealthInformatics/SAS/faqs (accessed on 28 March 2019).
- Monbaliu, E.; de Cock, P.; Ortibus, E.; Heyrman, L.; Klingels, K.; Feys, H. Clinical patterns of dystonia and choreoathetosis in participants with dyskinetic cerebral palsy. Dev. Med. Child Neurol. 2016, 58, 138–144. [Google Scholar] [CrossRef] [PubMed]

| Duration | Amplitude | |
|---|---|---|
| Score 0 | D/CA is absent | D/CA is absent |
| Score 1 (<10%) | D/CA is occasionally present | D/CA is present in small ROM |
| Score 2 (≥10 <50%) | D/CA is frequently present | D/CA is present in moderate ROM |
| Score 3 (≥50 <90%) | D/CA is mostly present | D/CA is present in submaximal ROM |
| Score 4 (>90%) | D/CA is always present | D/CA is present in maximal ROM |
| Duration | Amplitude | ∑(D + A) | |||||
|---|---|---|---|---|---|---|---|
| ICC | 95% CI; p–value | ICC | 95% CI; p–value | ICC | 95% CI; p–value | ||
| DIMS | |||||||
| Total score | 0.62 | 0.00–0.96; 0.131 | 0.87 | 0.41–0.99; 0.001 | 0.87 | 0.35–0.99; 0.011 | |
| DIMS-D SUBSCALE | |||||||
| 1 | Neck | 0.60 | 0.00–0.96; 0.131 | 0.89 | 0.40–0.99; 0.000 | 0.83 | 0.27–0.98; 0.015 |
| 2 | Arm RP | 0.04 | 0.00–0.90; 0.443 | 0.88 | 0.36–0.99; 0.009 | 0.67 | 0.00–0.96; 0.099 |
| 3 | Arm LP | 0.15 | 0.00–0.91; 0.391 | 0.87 | 0.37–0.99; 0.010 | 0.67 | 0.00–0.96; 0.093 |
| 4 | Arm RD | 0.73 | 0.00–0.97; 0.074 | 0.78 | 0.13–0.97; 0.006 | 0.86 | 0.39–0.98; 0.005 |
| 5 | Arm LD | 0.57 | 0.00–0.96; 0.171 | 0.97 | 0.87–0.99; 0.000 | 0.89 | 0.37–0.99; 0.009 |
| Total score | 0.22 | 0.00–0.93; 0.370 | 0.85 | 0.35–0.98; 0.008 | 0.68 | 0.00–0.98; 0.098 | |
| DIMS-CA SUBSCALE | |||||||
| 1 | Neck | 0.96 | 0.55–0.99; 0.000 | 0.97 | 0.75–0.99; 0.000 | 0.96 | 0.63–0.99; 0.000 |
| 2 | Arm RP | 0.96 | 0.79–0.99; 0.000 | 0.80 | 0.20–0.98; 0.011 | 0.79 | 0.09–0.98; 0.001 |
| 3 | Arm LP | 0.98 | 0.88–0.99; 0.000 | 0.90 | 0.25–0.99; 0.000 | 0.96 | 0.65–0.99; 0.000 |
| 4 | Arm RD | 0.92 | 0.33–0.99; 0.000 | 0.81 | 0.16–0.98; 0.000 | 0.87 | 0.24–0.99; 0.000 |
| 5 | Arm LD | 0.92 | 0.45–0.99; 0.000 | 0.83 | 0.13–0.98; 0.000 | 0.88 | 0.23–0.99; 0.000 |
| Total score | 0.83 | 0.13–0.98; 0.000 | 0.73 | 0.04–0.97; 0.000 | 0.79 | 0.07–0.98; 0.000 | |
| Duration | Amplitude | ∑(D + A) | |||||
|---|---|---|---|---|---|---|---|
| ICC | 95% CI; p-value | ICC | 95% CI; p-value | ICC | 95% CI; p–value | ||
| DIMS | |||||||
| Total score | 0.76 | 0.00–0.98; 0.112 | 0.84 | 0.00–0.98; 0.058 | 0.80 | 0.00–0.98; 0.079 | |
| DIMS-D SUBSCALE | |||||||
| 1 | Neck | 0.82 | 0.00–198; 0.072 | 0.97 | 0.78–0.99; 0.001 | 0.92 | 0.37–0.99; 0.018 |
| 2 | Arm RP | 0.94 | 0.43–0.99; 0.005 | 0.97 | 0.57–0.99; 0.001 | 0.96 | 0.45–0.99; 0.001 |
| 3 | Arm LP | 0.64 | 0.00–0.96; 0.070 | 0.75 | 0.00–0.97; 0.007 | 0.69 | 0.00–0.96; 0.023 |
| 4 | Arm RD | 0.87 | 0.00–0.99; 0.051 | 0.91 | 0.18–0.90; 0.026 | 0.89 | 0.00–0.99; 0.036 |
| 5 | Arm LD | 0.88 | 0.09–0.99; 0.016 | 0.83 | 0.00–0.98; 0.066 | 0.88 | 0.14–0.99; 0.030 |
| Total score | 0.90 | 0.26–0.99; 0.022 | 0.94 | 0.35–0.99; 0.004 | 0.93 | 0.42–0.99; 0.006 | |
| DIMS-CA SUBSCALE | |||||||
| 1 | Neck | 0.96 | 0.66–0.99; 0.006 | 0.96 | 0.54–0.99; 0.008 | 0.96 | 0.63–0.99; 0.006 |
| 2 | Arm RP | 0.79 | 0.00–0.98; 0.087 | 0.86 | 0.04–0.98; 0.032 | 0.78 | 0.00–0.98; 0.084 |
| 3 | Arm LP | 0.00* | 0.00–0.86; 0.631 | 0.00* | 0.00–0.90; 0.518 | 0.00* | 0.00–0.88; 0.611 |
| 4 | Arm RD | 0.77 | 0.00–0.98; 0.115 | 0.87 | 0.00–0.99; 0.048 | 0.83 | 0.00–0.98; 0.073 |
| 5 | Arm LD | 0.50 | 0.00–0.95; 0.290 | 0.67 | 0.00–0.97; 0.177 | 0.60 | 0.00–0.96; 0.229 |
| Total score | 0.38 | 0.00–0.94; 0.353 | 0.61 | 0.00–0.96; 0.223 | 0.51 | 0.00–0.95; 0.283 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bekteshi, S.; Konings, M.; Nica, I.G.; Gakopoulos, S.; Vanmechelen, I.; Aerts, J.-M.; Hallez, H.; Monbaliu, E. Development of the Dyskinesia Impairment Mobility Scale to Measure Presence and Severity of Dystonia and Choreoathetosis during Powered Mobility in Dyskinetic Cerebral Palsy. Appl. Sci. 2019, 9, 3481. https://doi.org/10.3390/app9173481
Bekteshi S, Konings M, Nica IG, Gakopoulos S, Vanmechelen I, Aerts J-M, Hallez H, Monbaliu E. Development of the Dyskinesia Impairment Mobility Scale to Measure Presence and Severity of Dystonia and Choreoathetosis during Powered Mobility in Dyskinetic Cerebral Palsy. Applied Sciences. 2019; 9(17):3481. https://doi.org/10.3390/app9173481
Chicago/Turabian StyleBekteshi, Saranda, Marco Konings, Ioana Gabriela Nica, Sotirios Gakopoulos, Inti Vanmechelen, Jean-Marie Aerts, Hans Hallez, and Elegast Monbaliu. 2019. "Development of the Dyskinesia Impairment Mobility Scale to Measure Presence and Severity of Dystonia and Choreoathetosis during Powered Mobility in Dyskinetic Cerebral Palsy" Applied Sciences 9, no. 17: 3481. https://doi.org/10.3390/app9173481
APA StyleBekteshi, S., Konings, M., Nica, I. G., Gakopoulos, S., Vanmechelen, I., Aerts, J.-M., Hallez, H., & Monbaliu, E. (2019). Development of the Dyskinesia Impairment Mobility Scale to Measure Presence and Severity of Dystonia and Choreoathetosis during Powered Mobility in Dyskinetic Cerebral Palsy. Applied Sciences, 9(17), 3481. https://doi.org/10.3390/app9173481






