On Metacognition: Overconfidence in Word Recall Prediction and Its Association with Psychotic Symptoms in Patients with Schizophrenia
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Setting
2.2. Procedure and Data Collection
2.3. Statistical Analysis
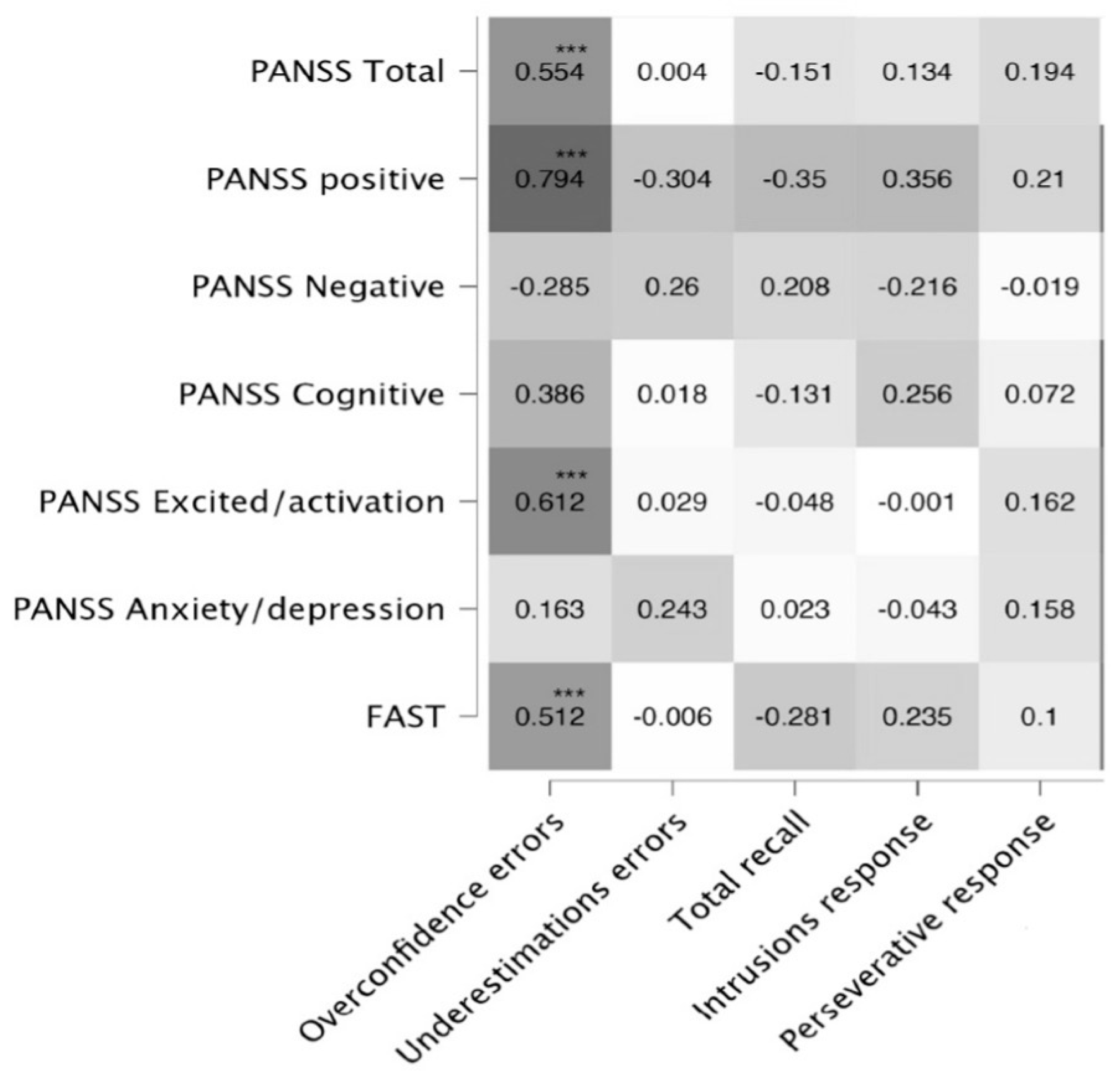
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McCutcheon, R.; Beck, K.; Jauhar, S.; Howes, O.D. Defining the Locus of Dopaminergic Dysfunction in Schizophrenia: A Meta-analysis and Test of the Mesolimbic Hypothesis. Schizophr. Bull. 2018, 44, 1301–1311. [Google Scholar] [CrossRef]
- David, A.S.; Halligan, P.W. Cognitive neuropsychiatry: Potential for progress. J. Neuropsychiatry Clin. Neurosci. 2000, 12, 506–510. [Google Scholar] [CrossRef]
- Frith, C. The self in action: Lessons from delusions of control. Conscious. Cogn. 2005, 14, 752–770. [Google Scholar] [CrossRef] [PubMed]
- Sandsten, K.E.; Nordgaard, J.; Kjaer, T.W.; Gallese, V.; Ardizzi, M.; Ferroni, F.; Petersen, J.; Parnas, J. Altered self-recognition in patients with schizophrenia. Schizophr. Res. 2020, 218, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Coltheart, M.; Davies, M. Failure of hypothesis evaluation as a factor in delusional belief. Cogn. Neuropsychiatry 2021, 26, 213–230. [Google Scholar] [CrossRef] [PubMed]
- McLeod, H.J.; Gumley, A.I.; Macbeth, A.; Schwannauer, M.; Lysaker, P.H. Metacognitive functioning predicts positive and negative symptoms over 12 months in first episode psychosis. J. Psychiatr. Res. 2014, 54, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.; Coltheart, M.; Langdon, R.; Breen, N. Monothematic delusions: Towards a two-factor account. Philos. Psychiatry Psychol. 2001, 8, 133–158. [Google Scholar] [CrossRef]
- Flores-Medina, Y.; Rosel-Vales, M.; Adame, G.A.; Ramírez-Bermúdez, J. The loss of familiarity: A case study of the comorbidities of capgras and fregoli. Neurocase 2021, 27, 385–390. [Google Scholar] [CrossRef]
- Frith, U.; Frith, C. What makes us social and what does it tell us about mental disorders? Cogn. Neuropsychiatry 2024, 29, 1–9. [Google Scholar] [CrossRef]
- Lau, H. Consciousness We Trust: The Cognitive Neuroscience of Subjective Experience; Oxford University Press: Oxford, UK, 2023. [Google Scholar] [CrossRef]
- Coltheart, M. The neuropsychology of delusions. Ann. N. Y. Acad. Sci. 2010, 1191, 16–26. [Google Scholar] [CrossRef]
- Gebreegziabhere, Y.; Habatmu, K.; Mihretu, A.; Cella, M.; Alem, A. Cognitive impairment in people with schizophrenia: An umbrella review. Eur. Arch. Psychiatry Clin. Neurosci. 2022, 272, 1139–1155. [Google Scholar] [CrossRef]
- Seidman, L.J.; Mirsky, A.F. Evolving Notions of Schizophrenia as a Developmental Neurocognitive Disorder. J. Int. Neuropsychol. Soc. 2017, 23, 881–892. [Google Scholar] [CrossRef]
- Mam-Lam-Fook, C.; Danset-Alexandre, C.; Pedron, L.; Amado, I.; Gaillard, R.; Krebs, M.O. Neuropsychology of subjects with ultra-high risk (UHR) of psychosis: A critical analysis of the literature. Encephale 2017, 43, 241–253. [Google Scholar] [CrossRef] [PubMed]
- Mondragón-Maya, A.; Flores-Medina, Y.; González-Sánchez, D.; Hernández-Echeagaray, E. Similarities in cognitive impairment between recent- onset and chronic schizophrenia patients: A consideration for the neurodevelopmental hypothesis. Actas Esp. Psiquiatr. 2023, 51, 176–183. [Google Scholar] [PubMed]
- Van Assche, L.; Morrens, M.; Luyten, P.; Van de Ven, L.; Vandenbulcke, M. The neuropsychology and neurobiology of late-onset schizophrenia and very-late-onset schizophrenia-like psychosis: A critical review. Neurosci. Biobehav. Rev. 2017, 83, 604–621. [Google Scholar] [CrossRef]
- Lee, M.; Cernvall, M.; Borg, J.; Plavén-Sigray, P.; Larsson, C.; Erhardt, S.; Sellgren, C.M.; Fatouros-Bergman, H.; Cervenka, S. Cognitive Function and Variability in Antipsychotic Drug-Naive Patients with First-Episode Psychosis: A Systematic Review and Meta-Analysis. JAMA Psychiatry 2024, 81, 468–476, Erratum in: JAMA Psychiatry 2024, 81, 530. [Google Scholar] [CrossRef]
- Mollon, J.; David, A.S.; Morgan, C.; Frissa, S.; Glahn, D.; Pilecka, I.; Hatch, S.L.; Hotopf, M.; Reichenberg, A. Psychotic Experiences and Neuropsychological Functioning in a Population-based Sample. JAMA Psychiatry 2016, 73, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Fleming, S.M. Metacognition and Confidence: A Review and Synthesis. Annu. Rev. Psychol. 2024, 75, 241–268. [Google Scholar] [CrossRef]
- Lapate, R.C.; Samaha, J.; Rokers, B.; Postle, B.R.; Davidson, R.J. Perceptual metacognition of human faces is causally supported by function of the lateral prefrontal cortex. Commun. Biol. 2020, 3, 360. [Google Scholar] [CrossRef]
- Yeung, M.K. Stability and consistency of metamemory judgments within a session. Front. Psychol. 2022, 13, 917576. [Google Scholar] [CrossRef]
- Martiadis, V.; Pessina, E.; Raffone, F.; Iniziato, V.; Martini, A.; Scognamiglio, P. Metacognition in schizophrenia: A practical overview of psychometric metacognition assessment tools for researchers and clinicians. Front. Psychiatry. 2023, 14, 1155321. [Google Scholar] [CrossRef]
- Branch Coslett, H. Anosognosia and body representations forty years later. Cortex 2005, 41, 263–270. [Google Scholar] [CrossRef]
- Jenkinson, P.M.; Fotopoulou, A. Understanding Babinski’s anosognosia: 100 years later. Cortex 2014, 61, 1–4. [Google Scholar] [CrossRef][Green Version]
- Marková, I.S.; Berrios, G.E. The assessment of insight in clinical psychiatry: A new scale. Acta Psychiatr. Scand. 1992, 86, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Quesque, F.; Apperly, I.; Baillargeon, R.; Baron-Cohen, S.; Becchio, C.; Bekkering, H.; Bernstein, D.; Bertoux, M.; Bird, G.; Bukowski, H.; et al. Defining key concepts for mental state attribution. Commun. Psychol. 2024, 2, 29. [Google Scholar] [CrossRef]
- Eisenacher, S.; Zink, M. The Importance of Metamemory Functioning to the Pathogenesis of Psychosis. Front. Psychol. 2017, 8, 304. [Google Scholar] [CrossRef] [PubMed]
- Lungu, P.F.; Lungu, C.M.; Ciobîcă, A.; Balmus, I.M.; Boloș, A.; Dobrin, R.; Luca, A.C. Metacognition in Schizophrenia Spectrum Disorders-Current Methods and Approaches. Brain Sci. 2023, 13, 1004. [Google Scholar] [CrossRef] [PubMed]
- Lysaker, P.H.; Kukla, M.; Dubreucq, J.; Gumley, A.; McLeod, H.; Vohs, J.L.; Buck, K.D.; Minor, K.S.; Luther, L.; Leonhardt, B.L.; et al. Metacognitive deficits predict future levels of negative symptoms in schizophrenia controlling for neurocognition, affect recognition, and self-expectation of goal attainment. Schizophr. Res. 2015, 168, 267–272. [Google Scholar] [CrossRef]
- Davies, G.; Greenwood, K. A meta-analytic review of the relationship between neurocognition, metacognition and functional outcome in schizophrenia. J. Ment. Health 2020, 29, 496–505. [Google Scholar] [CrossRef]
- Luria, A.R. Las Funciones Corticales Superiores del Hombre; Fontana: CDMX, México, 1986. [Google Scholar]
- Vilkki, J.; Servo, A.; Surma-aho, O. Word list learning and prediction of recall after frontal lobe lesions. Neuropsychology 1998, 12, 268–277. [Google Scholar] [CrossRef]
- Rezigalla, A.A. Observational Study Designs: Synopsis for Selecting an Appropriate Study Design. Cureus 2020, 12, e6692. [Google Scholar] [CrossRef] [PubMed]
- Flores-Lázaro, J.C.; Ostrosky-Solís, F.; Lozano, A. BANFE-2. Batería Neuropsicológica de Funciones Ejecutivas y Lóbulos Frontales, 2nd ed.; Manual Moderno: CDMX, México, 2014. [Google Scholar]
- Fresán, A.; De la Fuente-Sandoval, C.; Loyzaga, C.; García-Anaya, M.; Meyenberg, N.; Nicolini, H.; Apiquian, R. A forced five-dimensional factor analysis and concurrent validity of the Positive and Negative Syndrome Scale in Mexican schizophrenic patients. Schizophr. Res. 2005, 72, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Luján-Lujan, E.M.; García-León, M.Á.; Rodriguez-Cano, E.; Huertas-Martínez, S.; Roldan-Merino, J.; Puig-Llobet, M.; Miguel-Ruiz, M.D.; Salvador, R.; Vieta, E.; Pomarol-Clotet, E. Validity of the Functioning Assessment Short Tests (FAST), in patients with schizophrenia. Rev. Psiquiatr. Salud. Ment. (Engl. Ed.) 2022, 15, 157–166. [Google Scholar] [CrossRef]
- Seabury, R.D.; Bearden, C.E.; Ventura, J.; Subotnik, K.L.; Nuechterlein, K.H.; Cannon, T.D. Confident memory errors and disrupted reality testing in early psychosis. Schizophr. Res. 2021, 238, 170–177. [Google Scholar] [CrossRef]
- Peters, M.J.; Hauschildt, M.; Moritz, S.; Jelinek, L. Impact of emotionality on memory and meta-memory in schizophrenia using video sequences. J. Behav. Ther. Exp. Psychiatry 2013, 44, 77–83. [Google Scholar] [CrossRef]
- Moritz, S.; Woodward, T.S.; Whitman, J.C.; Cuttler, C. Confidence in errors as a possible basis for delusions in schizophrenia. J. Nerv. Ment. Dis. 2005, 193, 9–16. [Google Scholar] [CrossRef]
- Moritz, S.; Woodward, T.S.; Rodriguez-Raecke, R. Patients with schizophrenia do not produce more false memories than controls but are more confident in them. Psychol. Med. 2006, 36, 659–667. [Google Scholar] [CrossRef]
- Poletti, M.; Gebhardt, E.; Raballo, A. Developmental dynamic interplay between executive functions and psychotic risk. Appl. Neuropsychol. Child. 2021, 10, 194–197. [Google Scholar] [CrossRef]
- Bloemen, A.J.P.; Oldehinkel, A.J.; Laceulle, O.M.; Ormel, J.; Rommelse, N.N.J.; Hartman, C.A. The association between executive functioning and psychopathology: General or specific? Psychol. Med. 2018, 48, 1787–1794. [Google Scholar] [CrossRef] [PubMed]
- Snyder, H.R.; Friedman, N.P.; Hankin, B.L. Transdiagnostic mechanisms of psychopathology in youth: Executive functions, dependent stress, and rumination. Cognit. Ther. Res. 2019, 43, 834–851. [Google Scholar] [CrossRef]
- White, L.K.; Moore, T.M.; Calkins, M.E.; Wolf, D.H.; Satterthwaite, T.D.; Leibenluft, E.; Pine, D.S.; Gur, R.C.; Gur, R.E. An Evaluation of the Specificity of Executive Function Impairment in Developmental Psychopathology. J. Am. Acad. Child. Adolesc. Psychiatry 2017, 56, 975–982. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.K. Associations of symptoms, neurocognition, and metacognition with insight in schizophrenia spectrum disorders. Compr. Psychiatry 2016, 65, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Corlett, P.R.; Fletcher, P. Modelling delusions as temporally-evolving beliefs. Cogn. Neuropsychiatry 2021, 26, 231–241. [Google Scholar] [CrossRef]
- Matthews, J.; Schröder, P.; Kaunitz, L.; van Boxtel, J.J.A.; Tsuchiya, N. Conscious access in the near absence of attention: Critical extensions on the dual-task paradigm. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2018, 373, 20170352. [Google Scholar] [CrossRef] [PubMed]
- Recht, S.; Mamassian, P.; de Gardelle, V. Metacognition tracks sensitivity following involuntary shifts of visual attention. Psychon. Bull. Rev. 2023, 30, 1136–1147. [Google Scholar] [CrossRef] [PubMed]
- Thompson, P.M.; Jahanshad, N.; Ching, C.R.; Salminen, L.E.; Thomopoulos, S.I.; Bright, J.; Baune, B.T.; Bertolín, S.; Bralten, J.; Bruin, W.B.; et al. ENIGMA and global neuroscience: A decade of large-scale studies of the brain in health and disease across more than 40 countries. Transl. Psychiatry 2020, 10, 100. [Google Scholar] [CrossRef] [PubMed]
- Candini, V.; Ghisi, M.; Bianconi, G.; Bulgari, V.; Carcione, A.; Cavalera, C.; Conte, G.; Cricelli, M.; Ferla, M.T.; Ferrari, C.; et al. Aggressive behavior and metacognitive functions: A longitudinal study on patients with mental disorders. Ann. Gen. Psychiatry 2020, 19, 36. [Google Scholar] [CrossRef] [PubMed]
- Bürgler, S.; Hennecke, M. Metacognition and polyregulation in daily self-control conflicts. Scand. J. Psychol. 2024, 65, 179–194. [Google Scholar] [CrossRef] [PubMed]
- Koren, D.; Harvey, P.D. Closing the Gap Between Cognitive Performance and Real-World Functional Outcome in Schizophrenia: The Importance of Metacognition. Curr. Psychiatry Rev. 2006, 2, 189–198. [Google Scholar] [CrossRef]
- Silberstein, J.; Harvey, P.D. Cognition, social cognition, and Self-assessment in schizophrenia: Prediction of different elements of everyday functional outcomes. CNS Spectr. 2019, 24, 88–93. [Google Scholar] [CrossRef]
- Silberstein, J.; Harvey, P.D. Impaired introspective accuracy in schizophrenia: An independent predictor of functional outcomes. Cogn. Neuropsychiatry 2019, 24, 28–39. [Google Scholar] [CrossRef] [PubMed]
- Lysaker, P.H.; Chernov, N.; Moiseeva, T.; Sozinova, M.; Dmitryeva, N.; Alyoshin, V.; Luther, L.; Karpenko, O.; Kostyuk, G. Clinical insight, cognitive insight and metacognition in psychosis: Evidence of mediation. J. Psychiatr. Res. 2021, 140, 1–6. [Google Scholar] [CrossRef] [PubMed]

| Demographics. N = 51 | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| Age (years) | 42.7 | 11.6 | 18 | 67 |
| Years of education | 11.9 | 2.6 | 6 | 16 |
| Age of onset (years) | 25.1 | 7.5 | 15 | 47 |
| Disorder duration (years) | 17.6 | 10.8 | 1 | 45 |
| Hospitalizations | 1.5 | 1.8 | 0 | 7 |
| Psychopathology and Functionality | ||||
| PANSS total | 79.6 | 26.7 | 36 | 150 |
| PANSS positive | 25.9 | 14.6 | 8 | 53 |
| PANSS negative | 17.7 | 10.9 | 7 | 43 |
| PANSS Cognitive | 22.6 | 8.2 | 8 | 41 |
| PANSS Anxiety/depression | 8.4 | 4.5 | 4 | 25 |
| PANSS Excited/activation | 7.2 | 5 | 4 | 25 |
| FAST | 41.9 | 18.46 | 6 | 72 |
| Mean | SD | Minimum | Maximum | |
|---|---|---|---|---|
| Overconfidence errors | 6 | 5.7 | 0 | 21 |
| Normative scores | 7 | 5 | 1 | 14 |
| Percentage of patients in the impairment classifications. | Normal 49% | Mild 2% | Moderate 13.7% | Severe 35.3% |
| Underestimation errors | 2.8 | 3.6 | 0 | 13 |
| Normative scores | 9 | 4 | 1 | 14 |
| Percentage of patients in the impairment classifications. | Normal 72.5% | Mild 5.9% | Moderate 3.9% | Severe 17.6% |
| Metamemory total errors | 10.1 | 4.12 | 2 | 21 |
| Total recall, memory assessment | 3 | 1 | 1 | 6 |
| Normative scores | 4 | 2 | 1 | 10 |
| Percentage of patients in the impairment classifications. | Normal 7.8% | Mild 13.7% | Moderate 33.3% | Severe 45.1% |
| Intrusions response | 2.3 | 3 | 0 | 11 |
| Perseverative response | 2.3 | 3.3 | 0 | 21 |
| Coefficients | Unstandardized | Standardized | t | p |
|---|---|---|---|---|
| Positive errors | 1.82 | 0.77 | 8.46 | <0.001 |
| Total errors | −0.49 | −0.17 | −1.08 | 0.28 |
| Intrusion response | 0.44 | 0.09 | 0.92 | 0.36 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flores-Medina, Y.; Ávila Bretherton, R.; Ramírez-Bermudez, J.; Saracco-Alvarez, R.; Flores-Ramos, M. On Metacognition: Overconfidence in Word Recall Prediction and Its Association with Psychotic Symptoms in Patients with Schizophrenia. Brain Sci. 2024, 14, 872. https://doi.org/10.3390/brainsci14090872
Flores-Medina Y, Ávila Bretherton R, Ramírez-Bermudez J, Saracco-Alvarez R, Flores-Ramos M. On Metacognition: Overconfidence in Word Recall Prediction and Its Association with Psychotic Symptoms in Patients with Schizophrenia. Brain Sciences. 2024; 14(9):872. https://doi.org/10.3390/brainsci14090872
Chicago/Turabian StyleFlores-Medina, Yvonne, Regina Ávila Bretherton, Jesús Ramírez-Bermudez, Ricardo Saracco-Alvarez, and Monica Flores-Ramos. 2024. "On Metacognition: Overconfidence in Word Recall Prediction and Its Association with Psychotic Symptoms in Patients with Schizophrenia" Brain Sciences 14, no. 9: 872. https://doi.org/10.3390/brainsci14090872
APA StyleFlores-Medina, Y., Ávila Bretherton, R., Ramírez-Bermudez, J., Saracco-Alvarez, R., & Flores-Ramos, M. (2024). On Metacognition: Overconfidence in Word Recall Prediction and Its Association with Psychotic Symptoms in Patients with Schizophrenia. Brain Sciences, 14(9), 872. https://doi.org/10.3390/brainsci14090872







