Seroepidemiology of Tetanus among Healthy People Aged 1–59 Years Old in Shaanxi Province, China
Abstract
:1. Introduction
2. Materials and Methods
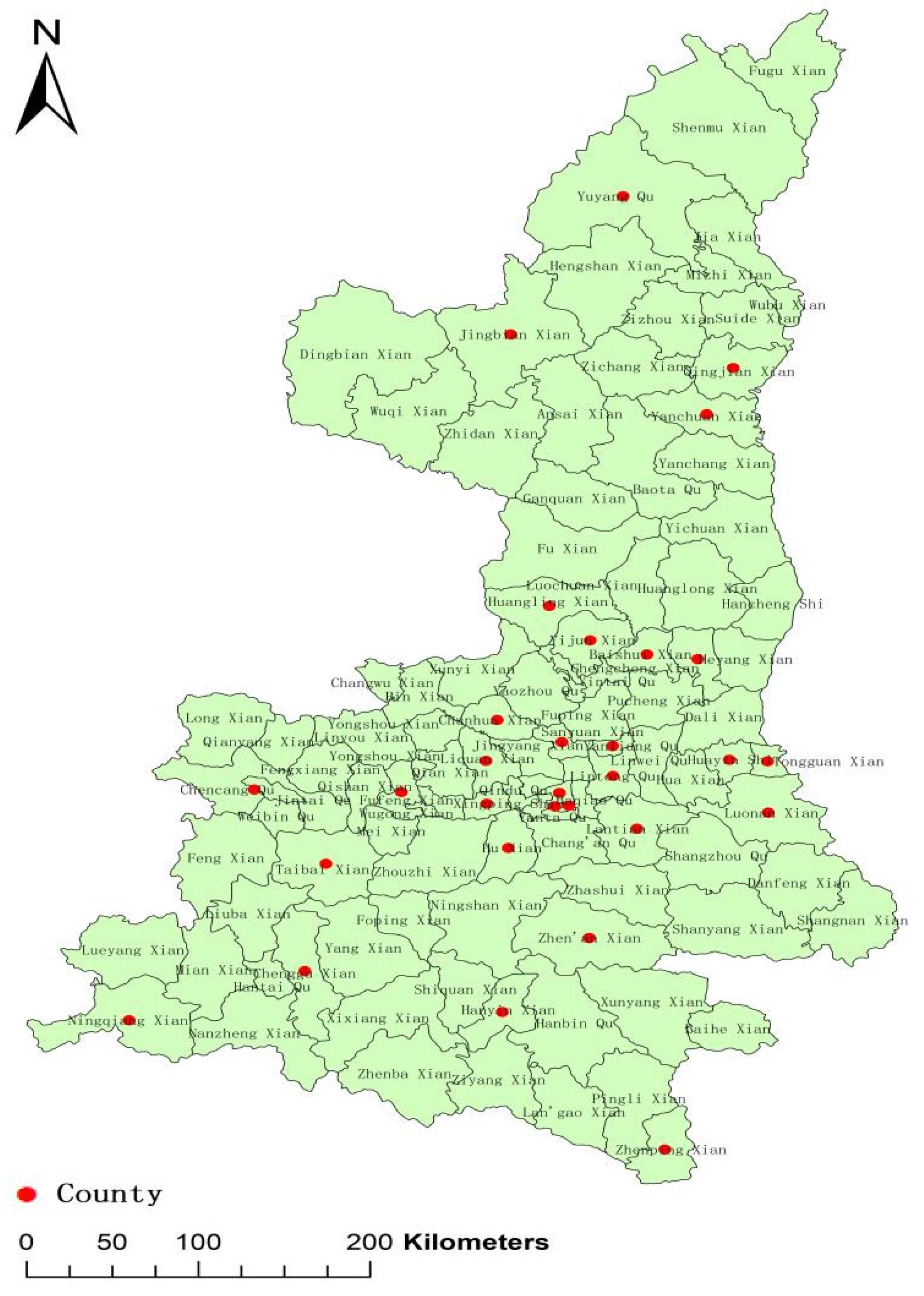
2.1. Subjects and Study Design
2.2. Data Collection
2.3. Laboratory Methods
2.4. Statistical Analysis
2.5. Ethical Approval
3. Results
3.1. SubsectionSociodemographic Characteristics of Study Population
3.2. Comparison among Subjects of Different Ages
3.3. Distribution among Recruitment Regions
3.4. Immunization History of TTCVs
3.5. Comparison of Different Doses
3.6. Antibody Level following Basic and Booster Immunization of TTCVs
3.7. Antibody Level According to the Interval since the Last Dose of TTCVs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khoury, A.; Cahill, J.D. Tetanus Vaccination 2020 and Collateral Protections against Pertussis and Diphtheria. Rhode Isl. Med. J. 2020, 103, 38–40. [Google Scholar]
- Yen, L.M.; Thwaites, C.L. Tetanus. Lancet 2019, 393, 1657–1668. [Google Scholar] [CrossRef]
- Finkelstein, P.; Teisch, L.; Allen, C.J.; Ruiz, G. Tetanus: A Potential Public Health Threat in Times of Disaster. Prehospital Disaster Med. 2017, 32, 339–342. [Google Scholar] [CrossRef] [PubMed]
- WHO. Tetanus vaccines: WHO position paper—February 2017. Wkly. Epidemiol. Rec. 2017, 92, 53–76. [Google Scholar]
- Liu, L.; Oza, S.; Hogan, D.; Chu, Y.; Perin, J.; Zhu, J.; Lawn, J.E.; Cousens, S.; Mathers, C.; Black, R.E. Global, regional, and national causes of under-5 mortality in 2000–15: An updated systematic analysis with implications for the Sustainable Development Goals. Lancet 2016, 388, 3027–3035. [Google Scholar] [CrossRef]
- Ning, G.; Gao, Y.; Xia, W.; Wu, D.; Li, J.; Li, Y.; Shao, Z.; Yin, Z. Epidemiology of neonatal tetanus in China during 2010–2017. Chin. J. Vaccines Immun. 2018, 24, 379–382. [Google Scholar]
- Peck, M.; Gacic-Dobo, M.; Diallo, M.S.; Nedelec, Y.; Sodha, S.V.; Wallace, A.S. Global Routine Vaccination Coverage, 2018. Morb. Mortal. Wkly. Rep. 2019, 68, 937–942. [Google Scholar] [CrossRef]
- National Health Commission of the PRC. Immunization schedules and instructions for vaccines of the national immunization program (2021 version). Chin. J. Viral Dis. 2021, 11, 241–245. [Google Scholar]
- Song, X.; Li, M.; Wang, C.; Li, Y.; Yin, Z. Immunoprophylaxis of tetanus in China: Status, issues and prospects. Chin. J. Vaccines Immun. 2019, 25, 743–746. [Google Scholar]
- Fan, C.; Xia, W.; Wen, N.; Hao, L.; Luo, H.; Liang, X. Analysis on Epidemiological Characteristics of Neonatal Tetanus in China, 2008~2009. Chin. J. Vaccines Immun. 2011, 17, 258–260. [Google Scholar]
- Ergonul, O.; Egeli, D.; Kahyaoglu, B.; Bahar, M.; Etienne, M.; Bleck, T. An unexpected tetanus case. Lancet Infect. Dis. 2016, 16, 746–752. [Google Scholar] [CrossRef]
- Umemoto, D.; Shibata, Y.; Mori, H.; Shindo, K. Tetanus: The clinical features of 11 cases. Rinsho Shinkeigaku 2021, 61, 537–542. [Google Scholar] [CrossRef] [PubMed]
- Filia, A.; Bella, A.; von Hunolstein, C.; Pinto, A.; Alfarone, G.; Declich, S.; Rota, M.C. Tetanus in Italy 2001–2010: A continuing threat in older adults. Vaccine 2014, 32, 639–644. [Google Scholar] [CrossRef] [PubMed]
- Riccò, M.; Cattani, S.; Veronesi, L.; Colucci, M.E. Knowledge, attitudes, beliefs and practices of construction workers towards tetanus vaccine in Northern Italy. Ind. Health 2016, 54, 554–563. [Google Scholar] [CrossRef]
- Tong, L.; Jia, Q.; Li, B.; Li, Z.; Qi, J.; Guo, Z.; Liu, Y. Investigation of the baseline tetanus antibody level and its persistence in a military unit. Vaccine 2021, 39, 4328–4334. [Google Scholar] [CrossRef]
- Wu, Y.; Gao, Y.; Zhu, B.; Zhou, H.; Shi, Z.; Wang, J.; Wang, H.; Shao, Z. Antitoxins for diphtheria and tetanus decline more slowly after vaccination with DTwP than with DTaP: A study in a Chinese population. Vaccine 2014, 32, 2570–2573. [Google Scholar] [CrossRef]
- Xu, Y.; Liu, Y.; Du, J.; Zheng, W.; Liu, S.; Zhang, X.; Wang, J.; Che, X.; Gu, W.; Jiang, W. Seroepidemiology of tetanus in Hangzhou from 2009 to 2018. Hum. Vaccines Immunother. 2020, 16, 2670–2676. [Google Scholar] [CrossRef]
- Liu, Q.; Dou, Q.; Wang, W.; Yang, J.; Guo, Y.; Zhang, Y. Tetanus antibody levels in healthy people in Henan province, 2016–2018. Chin. J. Vaccines Immun. 2021, 27, 387–390. [Google Scholar]
- Ang, L.W.; James, L.; Goh, K.T. Prevalence of diphtheria and tetanus antibodies among adults in Singapore: A national serological study to identify most susceptible population groups. J. Public Health 2016, 38, 99–105. [Google Scholar] [CrossRef]
- Rapisarda, V.; Bracci, M.; Nunnari, G.; Ferrante, M.; Ledda, C. Tetanus immunity in construction workers in Italy. Occup. Med. 2014, 64, 217–219. [Google Scholar] [CrossRef]
- Sung, H.; Jang, M.J.; Bae, E.Y.; Han, S.B.; Kim, J.H.; Kang, J.H.; Park, Y.J.; Ma, S.H. Seroepidemiology of tetanus in Korean adults and adolescents in 2012. J. Infect. Chemother. 2014, 20, 397–400. [Google Scholar] [CrossRef] [PubMed]
- Kader, Ç.; Balci, M.; Erbay, A. Evaluation of tetanus antibody levels in adults in Yozgat, Turkey. Turk. J. Med. Sci. 2016, 46, 646–650. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.; Ghanem-Uzqueda, A.; Hoff, N.A.; Ashbaugh, H.; Doshi, R.H.; Mukadi, P.; Budd, R.; Higgins, S.G.; Randall, C.; Gerber, S.; et al. Tetanus seroprotection among children in the Democratic Republic of the Congo, 2013–2014. PLoS ONE 2022, 17, e0268703. [Google Scholar] [CrossRef]
- Makumbi, F.; Byabagambi, J.; Muwanika, R.; Kigozi, G.; Gray, R.; Galukande, M.; Bagaya, B.; Ssebagala, D.; Karamagi, E.; Rahimzai, M.; et al. Prevalence of protective tetanus antibodies and immunological response following tetanus toxoid vaccination among men seeking medical circumcision services in Uganda. PLoS ONE 2018, 13, e0209167. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Choi, J.H. Tetanus-diphtheria-acellular pertussis vaccination for adults: An update. Clin. Exp. Vaccine Res. 2017, 6, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Weinberger, B. Adult vaccination against tetanus and diphtheria: The European perspective. Clin. Exp. Immunol. 2017, 187, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Wu, Y.; He, Q. The serological surveillance of tetanus antibodies among Guangzhou people in 2016. J. Trop. Med. 2018, 18, 1242–1245. [Google Scholar]
- Liang, J.L.; Tiwari, T.; Moro, P.; Messonnier, N.E.; Reingold, A.; Sawyer, M.; Clark, T.A. Prevention of Pertussis, Tetanus, and Diphtheria with Vaccines in the United States: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 2018, 67, 1–44. [Google Scholar] [CrossRef]
- Amanna, I.J.; Carlson, N.E.; Slifka, M.K. Duration of humoral immunity to common viral and vaccine antigens. N. Engl. J. Med. 2007, 357, 1903–1915. [Google Scholar] [CrossRef]
- Swanson, K.A.; Schmitt, H.J.; Jansen, K.U.; Anderson, A.S. Adult vaccination. Hum. Vaccines Immunother. 2015, 11, 150–155. [Google Scholar] [CrossRef]
- Hall, C.; Abramovitz, L.M.; Bukowinski, A.T.; Ricker, A.A.; Khodr, Z.G.; Gumbs, G.R.; Wells, N.Y.; Conlin, A.M.S. Safety of tetanus, diphtheria, and acellular pertussis vaccination among pregnant active duty U.S. military women. Vaccine 2020, 38, 1982–1988. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) in pregnant women—Advisory Committee on Immunization Practices (ACIP), 2012. Morb. Mortal. Wkly. Rep. 2013, 62, 131–135. [Google Scholar]
- Lu, P.J.; O’Halloran, A.; Ding, H.; Liang, J.L.; Williams, W.W. National and State-Specific Td and Tdap Vaccination of Adult Populations. Am. J. Prev. Med. 2016, 50, 616–626. [Google Scholar] [CrossRef] [PubMed]
- Kharbanda, E.O.; Vazquez-Benitez, G.; Lipkind, H.S.; Klein, N.P.; Cheetham, T.C.; Naleway, A.L.; Lee, G.M.; Hambidge, S.; Jackson, M.L.; Omer, S.B.; et al. Maternal Tdap vaccination: Coverage and acute safety outcomes in the vaccine safety datalink, 2007–2013. Vaccine 2016, 34, 968–973. [Google Scholar] [CrossRef] [PubMed]

| Subgroup | n | GMC [IU/mL, (95% CI)] | Z, p | Proportion [n (%)] | Positive Rate (≥0.01 IU/mL) [n (%)] | χ2, p | |||
|---|---|---|---|---|---|---|---|---|---|
| <0.01 IU/mL | 0.01–0.1 IU/mL | ≥0.1 IU/mL | |||||||
| Age(years) | 1–2 | 189 | 0.16 | 5,200,000 *, <0.01 | 5(2.65) | 71(37.57) | 113(59.79) | 184(97.35) | 308.944 #, <0.01 |
| 3–4 | 274 | 0.10 | 11(4.01) | 127(46.35) | 136(49.64) | 263(95.99) | |||
| 5–6 | 309 | 0.16 | 8(2.59) | 113(36.57) | 188(60.84) | 301(97.41) | |||
| 7–9 | 435 | 0.16 | 11(2.53) | 143(32.87) | 281(64.60) | 424(97.47) | |||
| 10–19 | 1080 | 0.05 | 114(10.56) | 644(59.63) | 322(29.81) | 966(89.44) | |||
| 20–29 | 1393 | 0.03 | 198(14.21) | 1025(73.58) | 170(12.20) | 1195(85.79) | |||
| 30–39 | 755 | 0.02 | 146(19.34) | 568(75.23) | 41(5.43) | 609(80.66) | |||
| 40–49 | 1018 | 0.02 | 250(24.56) | 737(72.40) | 31(3.05) | 768(75.44) | |||
| 50–59 | 986 | 0.02 | 262(26.57) | 706(71.60) | 18(1.83) | 724(73.43) | |||
| Total | 6439 | 0.03 | 1005(15.61) | 4134(64.20) | 1300(20.19) | 5434(84.39) | |||
| City | n | GMC [IU/mL, (95% CI)] | χ2, p | Proportion [n (%)] | Positive Rate (≥0.01 IU/mL) [n (%)] | χ2, p | ||
|---|---|---|---|---|---|---|---|---|
| <0.01 IU/mL | 0.01–0.1 IU/mL | ≥0.1 IU/mL | ||||||
| Xi’an | 1356 | 0.03 | 146.417 *, <0.01 | 348 (25.66) | 712 (52.51) | 296 (21.83) | 1008 (74.34) | 304.3 #, <0.01 |
| Tongchuan | 226 | 0.03 | 49 (21.68) | 129 (57.08) | 48 (21.24) | 177 (78.32) | ||
| Baoji | 677 | 0.03 | 160 (23.63) | 366 (54.06) | 151 (22.30) | 517 (76.37) | ||
| Xianyang | 889 | 0.03 | 146 (16.42) | 589 (66.25) | 154 (17.32) | 743 (83.58) | ||
| Weinan | 883 | 0.04 | 80 (9.06) | 632 (71.57) | 171 (19.37) | 803 (90.94) | ||
| Yan’an | 423 | 0.03 | 86 (20.33) | 277 (65.48) | 60 (14.18) | 337 (79.67) | ||
| Hanzhong | 455 | 0.04 | 45 (9.89) | 316 (69.45) | 94 (20.66) | 410 (90.11) | ||
| Yulin | 669 | 0.04 | 30 (4.48) | 502 (75.04) | 137 (20.48) | 639 (95.52) | ||
| Ankang | 454 | 0.04 | 41 (9.03) | 329 (72.47) | 84 (18.50) | 413 (90.97) | ||
| Shangluo | 407 | 0.05 | 20 (4.91) | 282 (69.29) | 105 (25.80) | 387 (95.09) | ||
| Total | 6439 | 0.03 | 1005 (15.61) | 4134 (64.20) | 1300 (20.19) | 5434 (84.39) | ||
| Subgroup | n | GMC [IU/mL, (95% CI)] | χ2, p | Proportion [n (%)] | Positive Rate (≥0.01 IU/mL) [n (%)] | χ2, p | |||
|---|---|---|---|---|---|---|---|---|---|
| <0.01 IU/mL | 0.01–0.1 IU/mL | ≥0.1 IU/mL | |||||||
| Immunization history | Yes | 2079 | 0.09 | 1641.475 *, <0.01 | 137 (6.59) | 940 (45.21) | 1002 (48.20) | 1942 (93.41) | 241.8 #, <0.01 |
| No | 2457 | 0.02 | 575 (23.40) | 1799 (73.22) | 83 (3.38) | 1882 (76.60) | |||
| Unknown | 1903 | 0.03 | 293 (15.40) | 1395 (73.31) | 215 (11.30) | 1610 (84.60) | |||
| Total | 6439 | 0.03 | 1005 (15.61) | 4134 (64.20) | 1300 (20.19) | 5434 (84.39) | |||
| Subgroup | n | GMC [IU/mL, (95% CI)] | Z, p | Proportion [n (%)] | Positive Rate (≥0.01 IU/mL) [n (%)] | χ2, p | |||
|---|---|---|---|---|---|---|---|---|---|
| <0.01 IU/mL | 0.01–0.1 IU/mL | ≥0.1 IU/mL | |||||||
| Doses | 1 | 56 | 0.03 | 688000 *, <0.01 | 4 (7.14) | 45 (80.36) | 7 (12.50) | 52 (92.86) | 13.799 #, <0.01 |
| 2 | 12 | 0.04 | 3 (25.00) | 7 (58.33) | 2 (16.67) | 9 (75.00) | |||
| 3 | 143 | 0.06 | 15 (10.49) | 76 (53.15) | 52 (36.36) | 128 (89.51) | |||
| 4 | 814 | 0.10 | 39 (4.79) | 372 (45.70) | 403 (49.51) | 775 (95.21) | |||
| 5 | 1039 | 0.10 | 74 (7.12) | 430 (41.39) | 535 (51.49) | 965 (92.88) | |||
| Total | 2064 | 0.09 | 135 (6.54) | 930 (45.06) | 999 (48.40) | 1929 (93.46) | |||
| Interval | n | GMC [IU/mL, (95% CI)] | Z, p | Proportion [n (%)] | Positive Rate (≥0.01 IU/mL) [n (%)] | χ2, p | ||
|---|---|---|---|---|---|---|---|---|
| <0.01 IU/mL | 0.01–0.1 IU/mL | ≥0.1 IU/mL | ||||||
| 0- | 134 | 0.31 | Z = 140200 *, <0.01 | 3 (2.24) | 26 (19.40) | 105 (78.36) | 131 (97.76) | 54.136 #, <0.01 |
| 1- | 137 | 0.18 | 0 (0.00) | 41 (29.93) | 96 (70.07) | 137 (100.00) | ||
| 2- | 114 | 0.16 | 2 (1.75) | 34 (29.82) | 78 (68.42) | 112 (98.25) | ||
| 3- | 71 | 0.15 | 2 (2.82) | 27 (38.03) | 42 (59.15) | 69 (97.18) | ||
| 4- | 93 | 0.11 | 4 (4.30) | 38 (40.86) | 51 (54.84) | 89 (95.70) | ||
| 5- | 75 | 0.08 | 4 (5.33) | 39 (52.00) | 32 (42.67) | 71 (94.67) | ||
| 6- | 60 | 0.06 | 11 (18.33) | 28 (46.67) | 21 (35.00) | 49 (81.67) | ||
| 7- | 63 | 0.06 | 8 (12.70) | 27 (42.86) | 28 (44.44) | 55 (87.30) | ||
| 8- | 35 | 0.07 | 4 (11.43) | 19 (54.29) | 12 (34.29) | 31 (88.57) | ||
| 9- | 48 | 0.06 | 3 (6.25) | 29 (60.42) | 16 (33.33) | 45 (93.75) | ||
| 10- | 160 | 0.03 | 30 (18.75) | 96 (60.00) | 34 (21.25) | 130 (81.25) | ||
| Total | 990 | 0.10 | 71 (7.17) | 404 (40.81) | 515 (52.02) | 990 (92.83) | ||
| Interval | n | GMC [IU/mL, (95% CI)] | Z, p | Proportion [n (%)] | Positive Rate (≥0.01 IU/mL) [n (%)] | χ2, p | ||
|---|---|---|---|---|---|---|---|---|
| <0.01 IU/mL | 0.01–0.1 IU/mL | ≥0.1 IU/mL | ||||||
| 0- | 263 | 0.23 | 629900 *, <0.01 | 7 (2.66) | 68 (25.86) | 188 (71.48) | 256 (97.34) | 79.598 #, <0.01 |
| 1- | 296 | 0.13 | 6 (2.03) | 118 (39.86) | 172 (58.11) | 290 (97.97) | ||
| 2- | 250 | 0.15 | 4 (1.60) | 88 (35.20) | 158 (63.20) | 246 (98.40) | ||
| 3- | 212 | 0.11 | 7 (3.30) | 99 (46.70) | 106 (50.00) | 205 (96.70) | ||
| 4- | 186 | 0.11 | 7 (3.76) | 84 (45.16) | 95 (51.08) | 179 (96.24) | ||
| 5- | 103 | 0.10 | 7 (6.80) | 44 (42.72) | 52 (50.49) | 96 (93.20) | ||
| 6- | 79 | 0.07 | 11 (13.92) | 37 (46.84) | 31 (39.24) | 68 (86.08) | ||
| 7- | 85 | 0.07 | 9 (10.59) | 34 (40.00) | 42 (49.41) | 76 (89.41) | ||
| 8- | 64 | 0.07 | 5 (7.81) | 36 (56.25) | 23 (35.94) | 59 (92.19) | ||
| 9- | 71 | 0.07 | 4 (5.63) | 41 (57.75) | 26 (36.62) | 67 (94.37) | ||
| 10- | 301 | 0.04 | 50 (16.61) | 171 (56.81) | 80 (26.58) | 251 (83.39) | ||
| 20- | 66 | 0.03 | 9 (13.64) | 50 (75.76) | 7 (10.61) | 57 (86.36) | ||
| Total | 1976 | 0.10 | 126 (6.38) | 870 (44.03) | 980 (49.60) | 1850 (93.62) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, C.; Hu, W.; Ma, Y.; Li, L.; Si, Y.; Zhang, S. Seroepidemiology of Tetanus among Healthy People Aged 1–59 Years Old in Shaanxi Province, China. Vaccines 2022, 10, 1806. https://doi.org/10.3390/vaccines10111806
Zhang C, Hu W, Ma Y, Li L, Si Y, Zhang S. Seroepidemiology of Tetanus among Healthy People Aged 1–59 Years Old in Shaanxi Province, China. Vaccines. 2022; 10(11):1806. https://doi.org/10.3390/vaccines10111806
Chicago/Turabian StyleZhang, Chao, Weijun Hu, Yu Ma, Li Li, Yuan Si, and Shaobai Zhang. 2022. "Seroepidemiology of Tetanus among Healthy People Aged 1–59 Years Old in Shaanxi Province, China" Vaccines 10, no. 11: 1806. https://doi.org/10.3390/vaccines10111806
APA StyleZhang, C., Hu, W., Ma, Y., Li, L., Si, Y., & Zhang, S. (2022). Seroepidemiology of Tetanus among Healthy People Aged 1–59 Years Old in Shaanxi Province, China. Vaccines, 10(11), 1806. https://doi.org/10.3390/vaccines10111806




