The Epidemiology of Influenza and the Associated Vaccines Development in China: A Review
Abstract
:1. Introduction
2. Influenza Epidemiology in China
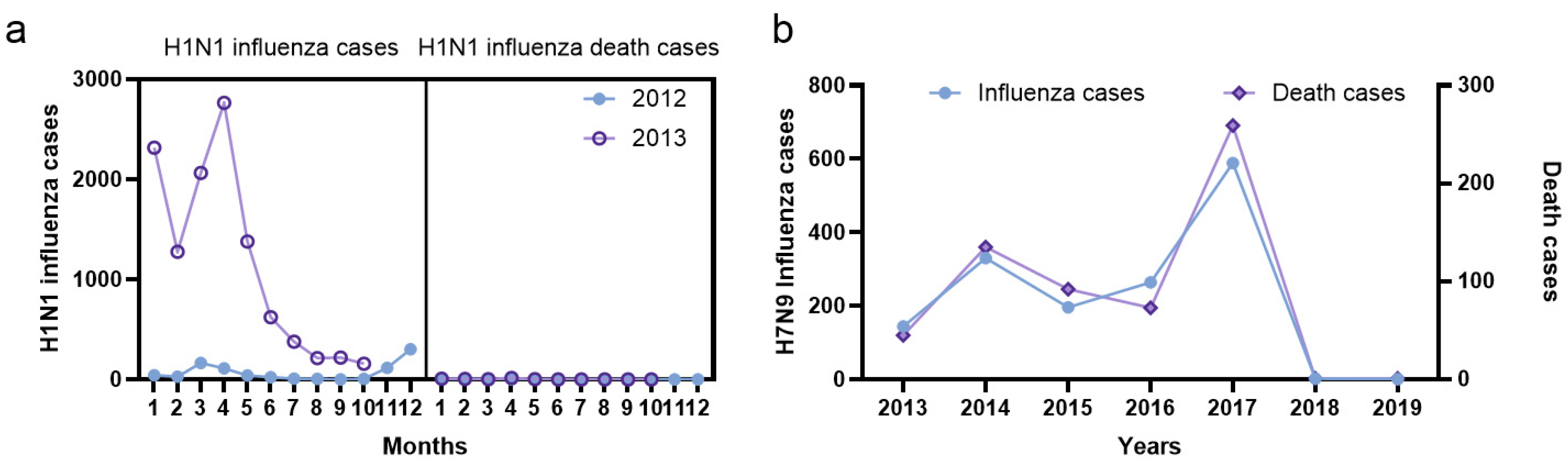
2.1. Annual and Monthly Influenza Infection and Death Cases
2.2. Regional and Subtype Prevalence of Influenza
2.3. Pandemic Influenza and Highly Pathogenic Avian Influenza Systematically Reported
3. Influenza Disease Burden
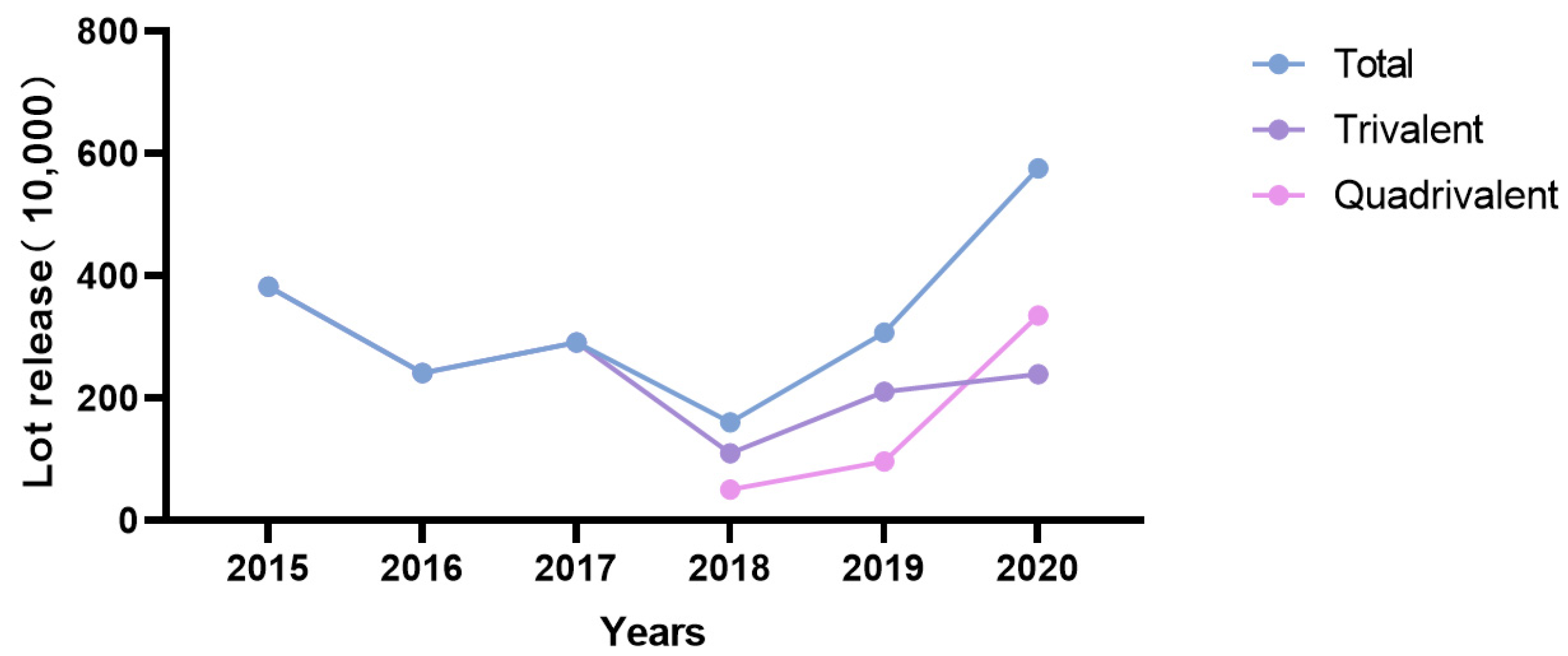
4. Influenza Vaccine Production and Batch Issuance in China
5. Analysis of Influenza Vaccination Status and Vaccination Rate in China
6. Development Trend of Influenza Vaccines in China
6.1. Development of Influenza Virus Split Vaccines for Different Populations
6.2. Novel Subunit Vaccines
6.3. Development of Live Attenuated Influenza Vaccines
6.4. Adjuvanted Influenza Vaccines
6.5. Development of a Universal Influenza Vaccine
6.6. Cell Culture-Based Influenza Vaccines
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Doyon-Plourde, P.; Fakih, I.; Tadount, F.; Fortin, É.; Quach, C. Impact of influenza vaccination on healthcare utilization—A systematic review. Vaccine 2019, 37, 3179–3189. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Hong, K.J.; Kim, H.; Nam, J.H. Influenza vaccines: Past, present, and future. Rev. Med. Virol. 2022, 32, e2243. [Google Scholar] [CrossRef] [PubMed]
- Peiris, J.S.; de Jong, M.D.; Guan, Y. Avian influenza virus (H5N1): A threat to human health. Clin. Microbiol. Rev. 2007, 20, 243–267. [Google Scholar] [CrossRef] [Green Version]
- Li, C.; Chen, H. H7N9 Influenza Virus in China. Cold Spring Harb. Perspect. Med. 2021, 11, a038349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Near, A.M.; Tse, J.; Young-Xu, Y.; Hong, D.K.; Reyes, C.M. Burden of influenza hospitalization among high-risk groups in the United States. BMC Health Serv. Res. 2022, 22, 1209. [Google Scholar] [CrossRef] [PubMed]
- Clohisey, S.; Baillie, J.K. Host susceptibility to severe influenza A virus infection. Crit. Care 2019, 23, 303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Center for Disease Control and Prevention. Flu Vaccination Coverage, United States, 2020–2021 Influenza Season. 2021. Available online: https://www.cdc.gov/flu/fluvaxview/coverage-2021estimates.htm (accessed on 22 September 2022).
- Matias, G.; Taylor, R.J.; Haguinet, F.; Schuck-Paim, C.; Lustig, R.L.; Fleming, D.M. Modelling estimates of age-specific influenza-related hospitalisation and mortality in the United Kingdom. BMC Public Health 2016, 16, 481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mertz, D.; Kim, T.H.; Johnstone, J.; Lam, P.P.; Science, M.; Kuster, S.P.; Fadel, S.A.; Tran, D.; Fernandez, E.; Bhatnagar, N.; et al. Populations at risk for severe or complicated influenza illness: Systematic review and meta-analysis. BMJ (Clin. Res. Ed.) 2013, 347, f5061. [Google Scholar] [CrossRef] [Green Version]
- Iuliano, A.D.; Roguski, K.M.; Chang, H.H.; Muscatello, D.J.; Palekar, R.; Tempia, S.; Cohen, C.; Gran, J.M.; Schanzer, D.; Cowling, B.J.; et al. Estimates of global seasonal influenza-associated respiratory mortality: A modelling study. Lancet 2018, 391, 1285–1300. [Google Scholar] [CrossRef]
- Paget, J.; Danielle Iuliano, A.; Taylor, R.J.; Simonsen, L.; Viboud, C.; Spreeuwenberg, P. Estimates of mortality associated with seasonal influenza for the European Union from the GLaMOR project. Vaccine 2022, 40, 1361–1369. [Google Scholar] [CrossRef]
- Ruf, B.R.; Knuf, M. The burden of seasonal and pandemic influenza in infants and children. Eur. J. Pediatr. 2014, 173, 265–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doherty, M.; Buchy, P.; Standaert, B.; Giaquinto, C.; Prado-Cohrs, D. Vaccine impact: Benefits for human health. Vaccine 2016, 34, 6707–6714. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Su, J.R.; McNeil, M.M.; Welsh, K.J.; Marquez, P.L.; Ng, C.; Yan, M.; Cano, M.V. Myopericarditis after vaccination, Vaccine Adverse Event Reporting System (VAERS), 1990–2018. Vaccine 2021, 39, 839–845. [Google Scholar] [CrossRef] [PubMed]
- Shu, Y.; Song, Y.; Wang, D.; Greene, C.M.; Moen, A.; Lee, C.K.; Chen, Y.; Xu, X.; McFarland, J.; Xin, L.; et al. A ten-year China-US laboratory collaboration: Improving response to influenza threats in China and the world, 2004–2014. BMC Public Health 2019, 19, 520. [Google Scholar] [CrossRef] [Green Version]
- Geng, Y.; Li, G.; Zhang, L. The Impact of COVID-19 Interventions on Influenza and Mycobacterium Tuberculosis Infection. Front. Public Health 2021, 9, 672568. [Google Scholar] [CrossRef]
- Lei, H.; Xu, M.; Wang, X.; Xie, Y.; Du, X.; Chen, T.; Yang, L.; Wang, D.; Shu, Y. Nonpharmaceutical Interventions Used to Control COVID-19 Reduced Seasonal Influenza Transmission in China. J. Infect. Dis. 2020, 222, 1780–1783. [Google Scholar] [CrossRef]
- Zheng, L.; Qi, J.; Wu, J.; Zheng, M. Changes in Influenza Activity and Circulating Subtypes during the COVID-19 Outbreak in China. Front. Med. 2022, 9, 829799. [Google Scholar] [CrossRef]
- National Administration of Disease Control and Prevention. Influenza (Seasonal). Available online: http://www.nhc.gov.cn/jkj/pgzdt/new_list_2.shtml (accessed on 22 September 2022).
- Yu, H.; Alonso, W.J.; Feng, L.; Tan, Y.; Shu, Y.; Yang, W.; Viboud, C. Characterization of regional influenza seasonality patterns in China and implications for vaccination strategies: Spatio-temporal modeling of surveillance data. PLoS Med. 2013, 10, e1001552. [Google Scholar] [CrossRef]
- Li, Y.; Reeves, R.M.; Wang, X.; Bassat, Q.; Brooks, W.A.; Cohen, C.; Moore, D.P.; Nunes, M.; Rath, B.; Campbell, H.; et al. Global patterns in monthly activity of influenza virus, respiratory syncytial virus, parainfluenza virus, and metapneumovirus: A systematic analysis. Lancet Glob. Health 2019, 7, e1031–e1045. [Google Scholar] [CrossRef]
- Azziz Baumgartner, E.; Dao, C.N.; Nasreen, S.; Bhuiyan, M.U.; Mah, E.M.S.; Al Mamun, A.; Sharker, M.A.; Zaman, R.U.; Cheng, P.Y.; Klimov, A.I.; et al. Seasonality, timing, and climate drivers of influenza activity worldwide. J. Infect. Dis. 2012, 206, 838–846. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, W.; Cheng, Y.; Chen, T.; Li, X.; Tan, M.; Wei, H.; Zeng, X.; Xie, Y.; Liu, J.; Xiao, N.; et al. Characterization of Influenza Viruses-China, 2019–2020. China CDC Wkly. 2020, 2, 856–861. [Google Scholar] [CrossRef]
- Diamond, C.; Gong, H.; Sun, F.Y.; Liu, Y.; Quilty, B.J.; Jit, M.; Yang, J.; Yu, H.; Edmunds, W.J.; Baguelin, M. Regional-based within-year seasonal variations in influenza-related health outcomes across mainland China: A systematic review and spatio-temporal analysis. BMC Med. 2022, 20, 58. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Chan KK, Y.; Xu, B.; Lu, M.; Xu, B. Spatial, Temporal and Genetic Dynamics Characteristics of Influenza B Viruses in China, 1973–2018. Virol. Sin. 2020, 35, 14–20. [Google Scholar] [CrossRef]
- Huang, W.; Li, X.; Tan, M.; Cheng, Y.; Chen, T.; Wei, H.; Zeng, X.; Xie, Y.; Liu, J.; Xiao, N.; et al. Epidemiological and Virological Surveillance of Seasonal Influenza Viruses—China, 2020–2021. China CDC Wkly. 2021, 3, 918–922. [Google Scholar] [CrossRef] [PubMed]
- Shan, X.; Wang, Y.; Song, R.; Wei, W.; Liao, H.; Huang, H.; Xu, C.; Chen, L.; Li, S. Spatial and temporal clusters of avian influenza a (H7N9) virus in humans across five epidemics in mainland China: An epidemiological study of laboratory-confirmed cases. BMC Infect. Dis. 2020, 20, 630. [Google Scholar] [CrossRef]
- Chow, E.J.; Uyeki, T.M.; Chu, H.Y. The effects of the COVID-19 pandemic on community respiratory virus activity. Nat. Reviews. Microbiol. 2022, 1–16. [Google Scholar] [CrossRef]
- Yi, H.; Yang, Y.; Zhang, L.; Zhang, M.; Wang, Q.; Zhang, T.; Zhang, Y.; Qin, Y.; Peng, Z.; Leng, Z.; et al. Improved influenza vaccination coverage among health-care workers: Evidence from a web-based survey in China, 2019/2020 season. Hum. Vaccin. Immunother. 2021, 17, 2185–2189. [Google Scholar] [CrossRef]
- Shang, M.; Lafond, K.E.; McFarland, J.; Zhou, S.; Klena, J.; Widdowson, M.A. Influenza-associated paediatric respiratory hospitalizations in China, 1996–2012: A systematic analysis. West. Pac. Surveill. ResponseJ. WPSAR 2018, 9, 35–43. [Google Scholar] [CrossRef]
- Li, J.; Chen, Y.; Wang, X.; Yu, H. Influenza-associated disease burden in mainland China: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 2886. [Google Scholar] [CrossRef]
- Li, L.; Liu, Y.; Wu, P.; Peng, Z.; Wang, X.; Chen, T.; Wong, J.Y.T.; Yang, J.; Bond, H.S.; Wang, L.; et al. Influenza-associated excess respiratory mortality in China, 2010–2015: A population-based study. Lancet Public Health 2019, 4, e473–e481. [Google Scholar] [CrossRef] [Green Version]
- Peng, Z.; Feng, L.; Carolyn, G.M.; Wang, K.; Zhu, G.; Zhang, Y.; Hu, J.; Huang, Y.; Pan, H.; Guo, N.; et al. Characterizing the epidemiology, virology, and clinical features of influenza in China’s first severe acute respiratory infection sentinel surveillance system, February 2011–October 2013. BMC Infect. Dis. 2015, 15, 143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bekkat-Berkani, R.; Wilkinson, T.; Buchy, P.; Dos Santos, G.; Stefanidis, D.; Devaster, J.M.; Meyer, N. Seasonal influenza vaccination in patients with COPD: A systematic literature review. BMC Pulm. Med. 2017, 17, 79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gong, H.; Shen, X.; Yan, H.; Lu, W.Y.; Zhong, G.J.; Dong, K.G.; Yang, J.; Yu, H.J. Estimating the disease burden of seasonal influenza in China, 2006–2019. Zhonghua Yi Xue Za Zhi 2021, 101, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Feng, L.; Feng, S.; Chen, T.; Yang, J.; Lau, Y.C.; Peng, Z.; Li, L.; Wang, X.; Wong, J.Y.T.; Qin, Y.; et al. Burden of influenza-associated outpatient influenza-like illness consultations in China, 2006–2015: A population-based study. Influenza Other Respi Viruses 2020, 14, 162–172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, J.; Xu, F.; Lu, L.; Lu, M.; Miao, L.; Gao, T.; Ji, W.; Suo, L.; Liu, D.; Ma, R.; et al. Safety and Effectiveness of a 2009 H1N1 Vaccine in Beijing. N. Engl. J. Med. 2010, 363, 2416–2423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- TWG, I.V.; National Immunization Advisory Committee; Technical Working Group. Technical guidelines for seasonal influenza vaccination in China (2020–2021). Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua Liuxingbingxue Zazhi 2020, 41, 1555–1576. (In Chinese) [Google Scholar]
- Yang, X.K.; Zhang, Y.Q.; Feng, D.; Xia, Z.; Fan, S.M.; Zhao, H.T.; Qin, Y.; Zheng, J.D.; Peng, Z.B. Analysis on the characteristics of influenza vaccine batch administration in China from 2007 to 2020. Int. J. Virol. 2021, 28, 364–368. (In Chinese) [Google Scholar]
- Zhang, X.L. National approval system of biological products. Chin. J. New Drugs 2004, 13, 2. (In Chinese) [Google Scholar]
- Liu, S.Z.; Shao, M.; Qiu, P.; Yuan, L.Y.; Fang, H.H.; Li, C.G. Summary and quality analysis of influenza vaccine batch from 2006 to 2009. Chin. J. Biol. Prod. 2011, 24, 1118–1120. (In Chinese) [Google Scholar]
- Hao, M.; Liu, S.Z.; Qiu, P.; Liu, C.N.; Yuan, L.Y.; Xu, K.W.; Li, C.G. Summary and quality analysis of influenza vaccine batch in 2011. Chin. J. Biol. Prod. 2012, 25, 1242–1244. (In Chinese) [Google Scholar]
- Fan, J.; Cong, S.; Wang, N.; Bao, H.; Wang, B.; Feng, Y.; Lv, X.; Zhang, Y.; Zha, Z.; Yu, L.; et al. Influenza vaccination rate and its association with chronic diseases in China: Results of a national cross-sectional study. Vaccine 2020, 38, 2503–2511. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Atkins, K.E.; Feng, L.; Pang, M.; Zheng, Y.; Liu, X.; Cowling, B.J.; Yu, H. Seasonal influenza vaccination in China: Landscape of diverse regional reimbursement policy, and budget impact analysis. Vaccine 2016, 34, 5724–5735. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, H.; Ren, X.; Tian, K.; Yu, J.; Zhu, A.; Zhang, L.; Gao, G.F.; Li, Z. The Impact and Vaccination Coverage of Seasonal Influenza among Children Aged 6–59 Months in China in 2017–2018: An Internet Panel Survey. Vaccines 2022, 10, 630. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Ren, X.; Ye, C.; Tian, K.; Feng, L.; Song, Y.; Cowling, B.J.; Li, Z. Influenza Vaccination Coverage among Registered Nurses in China during 2017–2018: An Internet Panel Survey. Vaccines 2019, 7, 134. [Google Scholar] [CrossRef]
- Rong, H.; Lai, X.; Ma, X.; Hou, Z.; Li, S.; Jing, R.; Zhang, H.; Peng, Z.; Feng, L.; Fang, H. Seasonal Influenza Vaccination and Recommendation: The Difference between General Practitioners and Public Health Workers in China. Vaccines 2020, 8, 265. [Google Scholar] [CrossRef]
- Liu, H.; Tan, Y.; Zhang, M.; Peng, Z.; Zheng, J.; Qin, Y.; Guo, Z.; Yao, J.; Pang, F.; Ma, T.; et al. An Internet-Based Survey of Influenza Vaccination Coverage in Healthcare Workers in China, 2018/2019 Season. Vaccines 2019, 8, 6. [Google Scholar] [CrossRef] [Green Version]
- Jiang, M.; Gong, Y.; Fang, Y.; Yao, X.; Feng, L.; Zhu, S.; Peng, J.; Shi, X. Parental Preferences of Influenza Vaccination for Children in China: A National Survey with a Discrete Choice Experiment. Int. J. Environ. Res. Public Health 2022, 19, 2145. [Google Scholar] [CrossRef]
- Wang, Q.; Yue, N.; Zheng, M.; Wang, D.; Duan, C.; Yu, X.; Zhang, X.; Bao, C.; Jin, H. Influenza vaccination coverage of population and the factors influencing influenza vaccination in mainland China: A meta-analysis. Vaccine 2018, 36, 7262–7269. [Google Scholar] [CrossRef]
- Fan, R.; Huang, X.; Nian, X.; Ou, Z.; Zhou, J.; Zhang, J.; Zeng, P.; Zhao, W.; Deng, J.; Chen, W.; et al. Safety and immunogenicity of a quadrivalent influenza vaccine in adults aged 60 years or above: A phase III randomized controlled clinical study. Hum. Vaccin. Immunother. 2022, 18, 1–9. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, Y.; Wu, H.; Huang, L.; Yu, H.; Xie, Z.; Zhang, H.; Zhang, W.; Chen, X.; Zhang, H.; et al. Safety and immunogenicity of a quadrivalent inactivated subunit non-adjuvanted influenza vaccine: A randomized, double-blind, active-controlled phase 1 clinical trial. Vaccine 2021, 39, 3871–3878. [Google Scholar] [CrossRef] [PubMed]
- Mu, X.; Hu, K.; Shen, M.; Kong, N.; Fu, C.; Yan, W.; Wei, A. Protection against influenza A virus by vaccination with a recombinant fusion protein linking influenza M2e to human serum albumin (HSA). J. Virol. Methods 2016, 228, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Sano, K.; Ainai, A.; Suzuki, T.; Hasegawa, H. The road to a more effective influenza vaccine: Up to date studies and future prospects. Vaccine 2017, 35, 5388–5395. [Google Scholar] [CrossRef]
- Wang, S.; Zheng, Y.; Jin, X.; Gan, Z.; Shao, Y.; Zhu, C.; Hu, X.; Liang, Z.; Chen, Y.; Xing, B.; et al. Efficacy and safety of a live attenuated influenza vaccine in Chinese healthy children aged 3–17 years in one study center of a randomized, double-blind, placebo-controlled phase 3 clinical trial, 2016/17 season. Vaccine 2020, 38, 5979–5986. [Google Scholar] [CrossRef]
- Ambrose, C.S.; Luke, C.; Coelingh, K. Current status of live attenuated influenza vaccine in the United States for seasonal and pandemic influenza. Influenza Other Respir Viruses 2008, 2, 193–202. [Google Scholar] [CrossRef] [PubMed]
- O’Hagan, D.T.; Ott, G.S.; Nest, G.V.; Rappuoli, R.; Giudice, G.D. The history of MF59® adjuvant: A phoenix that arose from the ashes. Expert Rev. Vaccines 2013, 12, 13–30. [Google Scholar] [CrossRef] [PubMed]
- Essink, B.; Fierro, C.; Rosen, J.; Figueroa, A.L.; Zhang, B.; Verhoeven, C.; Edelman, J.; Smolenov, I. Immunogenicity and safety of MF59-adjuvanted quadrivalent influenza vaccine versus standard and alternate B strain MF59-adjuvanted trivalent influenza vaccines in older adults. Vaccine 2020, 38, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Zhang, P.; Bai, S.; Lv, M.; Wang, J.; Chen, W.; Wu, J. Immune Responses to Adjuvanted H7N9 Split Antigen in Aged Mice. Viral Immunol. 2021, 34, 112–116. [Google Scholar] [CrossRef]
- Ou, H.; Yao, H.; Yao, W.; Wu, N.; Wu, X.; Han, C.; Cheng, L.; Chen, K.; Chen, H.; Li, L. Analysis of the immunogenicity and bioactivities of a split influenza A/H7N9 vaccine mixed with MF59 adjuvant in BALB/c mice. Vaccine 2016, 34, 2362–2370. [Google Scholar] [CrossRef] [Green Version]
- Ju, Y.; Fan, H.; Liu, J.; Hu, J.; Li, X.; Li, C.; Chen, L.; Gao, Q.; Gao, G.F.; Meng, S. Heat shock protein gp96 adjuvant induces T cell responses and cross-protection to a split influenza vaccine. Vaccine 2014, 32, 2703–2711. [Google Scholar] [CrossRef]
- Zhang, H.; Zheng, H.; Guo, P.; Hu, L.; Wang, Z.; Wang, J.; Ju, Y.; Meng, S. Broadly Protective CD8+ T Cell Immunity to Highly Conserved Epitopes Elicited by Heat Shock Protein gp96-Adjuvanted Influenza Monovalent Split Vaccine. J. Virol. 2021, 95, e00507-21. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Ke, C.W.; Zou, L.R.; Jing, Z.; Xie, G.X.; Li, X. A novel emulsion adjuvant increases the immunogenic responses and protective efficacy of an inactivated influenza vaccine in BALB/c mice. Intervirology 2009, 52, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Sheng, Y.; Zhang, X.; Li, Z.; Yang, Y.; Wu, J.; Su, Z.; Ma, G.; Zhang, S. Oil-in-ionic liquid nanoemulsion-based intranasal delivery system for influenza split-virus vaccine. J. Control Release Off. J. Control Release Soc. 2022, 346, 380–391. [Google Scholar] [CrossRef] [PubMed]
- Song, T.; Xia, Y.; Du, Y.; Chen, M.W.; Qing, H.; Ma, G. Engineering the Deformability of Albumin-Stabilized Emulsions for Lymph-Node Vaccine Delivery. Adv. Mater. 2021, 33, 2100106. [Google Scholar] [CrossRef]
- Chen, Q.; Wu, N.; Gao, Y.; Wang, X.; Wu, J.; Ma, G. Alum Pickering Emulsion as Effective Adjuvant to Improve Malaria Vaccine Efficacy. Vaccines 2021, 9, 1244. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.; Wu, J.; Qing, S.; Zhang, X.; Zhang, L.; Yue, H.; Zeng, M.; Wang, B.; Yuan, Z.; Qiu, Y.; et al. Biosynthesis of Self-Assembled Proteinaceous Nanoparticles for Vaccination. Adv. Mater. 2020, 32, 2002940. [Google Scholar] [CrossRef]
- Wang, J.; Li, P.; Yu, Y.; Fu, Y.; Jiang, H.; Lu, M.; Sun, Z.; Jiang, S.; Lu, L.; Wu, M.X. Pulmonary surfactant-biomimetic nanoparticles potentiate heterosubtypic influenza immunity. Science 2020, 367, 852. [Google Scholar] [CrossRef]
- Guo, Y.; He, L.; Song, N.; Li, P.; Sun, S.; Zhao, G.; Tai, W.; Jiang, S.; Du, L.; Zhou, Y. Highly conserved M2e and hemagglutinin epitope-based recombinant proteins induce protection against influenza virus infection. Microbes Infect. 2017, 19, 641–647. [Google Scholar] [CrossRef]
- Wang, Q.; Zhang, Y.; Zou, P.; Wang, M.; Fu, W.; She, J.; Song, Z.; Xu, J.; Huang, J.; Wu, F. Self-Assembly M2e-Based Peptide Nanovaccine Confers Broad Protection Against Influenza Viruses. Front. Microbiol. 2020, 11, 1961. [Google Scholar] [CrossRef]
- Wang, Y.; Wu, J.; Xue, C.; Wu, Z.; Lin, Y.; Wei, Y.; Wei, X.; Qin, J.; Zhang, Y.; Wen, Z.; et al. A recombinant H7N9 influenza vaccine with the H7 hemagglutinin transmembrane domain replaced by the H3 domain induces increased cross-reactive antibodies and improved interclade protection in mice. Antivir. Res. 2017, 143, 97–105. [Google Scholar] [CrossRef]
- Kong, D.; Chen, T.; Hu, X.; Lin, S.; Gao, Y.; Ju, C.; Liao, M.; Fan, H. Supplementation of H7N9 Virus-Like Particle Vaccine with Recombinant Epitope Antigen Confers Full Protection against Antigenically Divergent H7N9 Virus in Chickens. Front. Immunol. 2022, 13, 785975. [Google Scholar] [CrossRef] [PubMed]
- Qiao, Y.; Zhang, Y.; Chen, J.; Jin, S.; Shan, Y. A biepitope, adjuvant-free, self-assembled influenza nanovaccine provides cross-protection against H3N2 and H1N1 viruses in mice. Nano Res. 2022, 15, 8304–8314. [Google Scholar] [CrossRef] [PubMed]
- Qi, M.; Zhang, X.-E.; Sun, X.; Zhang, X.; Yao, Y.; Liu, S.; Chen, Z.; Li, W.; Zhang, Z.; Chen, J.; et al. Intranasal Nanovaccine Confers Homo- and Hetero-Subtypic Influenza Protection. Small 2018, 14, 1703207. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Wang, H.; Chen, J.; Shao, Z.; He, B.; Chen, J.; Lan, J.; Chen, Q.; Chen, Z. Protection against homo and hetero-subtypic influenza A virus by optimized M2e DNA vaccine. Emerg. Microbes Infect. 2019, 8, 45–54. [Google Scholar] [CrossRef] [Green Version]
- Wang, W.; Huang, B.; Wang, X.; Tan, W.; Ruan, L. Improving Cross-Protection against Influenza Virus Using Recombinant Vaccinia Vaccine Expressing NP and M2 Ectodomain Tandem Repeats. Virol. Sin. 2019, 34, 583–591. [Google Scholar] [CrossRef]
- Minor, P.D.; Engelhardt, O.G.; Wood, J.; Robertson, J.S.; Blayer, S.; Colegate, T.; Fabry, L.; Heldens, J.G.M.; Kino, Y.; Kistner, O.; et al. Current challenges in implementing cell-derived influenza vaccines: Implications for production and regulation, July 2007, NIBSC, Potters Bar, UK. Vaccine 2009, 27, 2907–2913. [Google Scholar] [CrossRef]
- Pérez Rubio, A.; Eiros, J.M. Cell culture-derived flu vaccine: Present and future. Hum. Vaccin. Immunother. 2018, 14, 1874–1882. [Google Scholar] [CrossRef] [Green Version]
- Rajaram, S.; Boikos, C.; Gelone, D.K.; Gandhi, A. Influenza vaccines: The potential benefits of cell-culture isolation and manufacturing. Ther. Adv. Vaccines Immunother. 2020, 8, 2515135520908121. [Google Scholar] [CrossRef]
- Perdue, M.L.; Arnold, F.; Li, S.; Donabedian, A.; Cioce, V.; Warf, T.; Huebner, R. The future of cell culture-based influenza vaccine production. Expert Rev. Vaccines 2011, 10, 1183–1194. [Google Scholar] [CrossRef]
- Tey, D.; Heine, R.G. Egg allergy in childhood: An update. Curr. Opin. Allergy Clin. Immunol. 2009, 9, 244–250. [Google Scholar] [CrossRef]
- Frey, S.; Vesikari, T.; Szymczakiewicz-Multanowska, A.; Lattanzi, M.; Izu, A.; Groth, N.; Holmes, S. Clinical efficacy of cell culture–derived and egg-derived inactivated subunit influenza vaccines in healthy adults. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2010, 51, 997–1004. [Google Scholar] [CrossRef] [PubMed]
- Audsley, J.M.; Tannock, G.A. The role of cell culture vaccines in the control of the next influenza pandemic. Expert Opin. Biol. Ther. 2004, 4, 709–717. [Google Scholar] [CrossRef] [PubMed]
- Schild, G.C.; Oxford, J.S.; de Jong, J.C.; Webster, R.G. Evidence for host-cell selection of influenza virus antigenic variants. Nature 1983, 303, 706–709. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.M.; Wang, M.; Webster, R.G. Direct sequencing of the HA gene of influenza (H3N2) virus in original clinical samples reveals sequence identity with mammalian cell-grown virus. J. Virol. 1990, 64, 1808–1811. [Google Scholar] [CrossRef] [Green Version]
- Robertson, J.S.; Naeve, C.W.; Webster, R.G.; Bootman, J.S.; Newman, R.; Schild, G.C. Alterations in the hemagglutinin associated with adaptation of influenza B virus to growth in eggs. Virology 1985, 143, 166–174. [Google Scholar] [CrossRef]
- Nian, X.; Zhang, J.; Deng, T.; Liu, J.; Gong, Z.; Lv, C.; Yao, L.; Li, J.; Huang, S.; Yang, X. AddaVax Formulated with PolyI:C as a Potential Adjuvant of MDCK-based Influenza Vaccine Enhances Local, Cellular, and Antibody Protective Immune Response in Mice. AAPS PharmSciTech 2021, 22, 270. [Google Scholar] [CrossRef]
- Liu, J.; Shi, X.; Schwartz, R.; Kemble, G. Use of MDCK cells for production of live attenuated influenza vaccine. Vaccine 2009, 27, 6460–6463. [Google Scholar] [CrossRef]
- Tzeng, T.T.; Chen, P.L.; Weng, T.C.; Tsai, S.Y.; Lai, C.C.; Chou, H.I.; Chen, P.W.; Lu, C.C.; Liu, M.T.; Sung, W.C.; et al. Development of high-growth influenza H7N9 prepandemic candidate vaccine viruses in suspension MDCK cells. J. Biomed. Sci. 2020, 27, 47. [Google Scholar] [CrossRef] [Green Version]
- Sun, B.; Yu, X.; Kong, W.; Sun, S.; Yang, P.; Zhu, C.; Zhang, H.; Wu, Y.; Chen, Y.; Shi, Y.; et al. Production of influenza H1N1 vaccine from MDCK cells using a novel disposable packed-bed bioreactor. Appl. Microbiol. Biotechnol. 2013, 97, 1063–1070. [Google Scholar] [CrossRef]
- Tzeng, T.T.; Lai, C.C.; Weng, T.C.; Cyue, M.H.; Tsai, S.Y.; Tseng, Y.F.; Sung, W.C.; Lee, M.S.; Hu, A.Y. The stability and immunogenicity of inactivated MDCK cell-derived influenza H7N9 viruses. Vaccine 2019, 37, 7117–7122. [Google Scholar] [CrossRef]
- Zhang, Y.; Wu, P.; Feng, L.; Yang, P.; Pan, Y.; Feng, S.; Qin, Y.; Zheng, J.; Puig-Barbera, J.; Muscatello, D.; et al. Influenza vaccine effectiveness against influenza-associated hospitalization in 2015/16 season, Beijing, China. Vaccine 2017, 35, 3129–3134. [Google Scholar] [CrossRef] [PubMed]
- Krishnarajah, G.; Divino, V.; Postma, M.J.; Pelton, S.I.; Anupindi, V.R.; DeKoven, M.; Mould-Quevedo, J. Clinical and Economic Outcomes Associated with Cell-Based Quadrivalent Influenza Vaccine vs. Standard-Dose Egg-Based Quadrivalent Influenza Vaccines during the 2018–19 Influenza Season in the United States. Vaccines 2021, 9, 80. [Google Scholar] [CrossRef] [PubMed]
- Diaco, M.; Chang, L.J.; Seet, B.; Robertson, C.A.; Chit, A.; Mercer, M.; Greenberg, D.P.; Hollingsworth, R.; Samson, S.I. Introductory paper: High-dose influenza vaccine. Vaccine 2021, 39 (Suppl. S1), A1–A5. [Google Scholar] [CrossRef] [PubMed]
- Beran, J.; Reynales, H.; Poder, A.; Yu, C.Y.; Pitisuttithum, P.; Yuan, L.L.; Vermeulen, W.; Verhoeven, C.; Leav, B.; Zhang, B.; et al. Prevention of influenza during mismatched seasons in older adults with an MF59-adjuvanted quadrivalent influenza vaccine: A randomised, controlled, multicentre, phase 3 efficacy study. Lancet Infect. Dis. 2021, 21, 1027–1037. [Google Scholar] [CrossRef]


| Manufacturer | Type of Vaccine | Inoculation Method | Specification (mL) | User Group | Dose of Vaccination | Time to Market |
|---|---|---|---|---|---|---|
| Fosun Pharmaceutical | Trivalent split | Intramuscular | 0.25/0.5 | 6M-3Y/>3Y | 2/1 | 2005 |
| Sanofi China | Trivalent split | Intramuscular | 0.25/0.5 | 6M-3Y/>3Y | 2/1 | 2013 |
| Adimmune Corporation | Trivalent split | Intramuscular | 0.25/0.5 | 6M-3Y/>3Y | 2/1 | 2015 |
| Zhongyianke Biotech. Co., Ltd. | Trivalent subunit | Intramuscular | 0.5 | 3Y | 1 | 2010 |
| Changchun BCHT Biotechnology Co. | Trivalent attenuated (nasal spray) | Spray | 0.2 | 3–17Y | 1 | 2020 |
| Hualan Biological Engineering, Inc. | Trivalent split Tetravalent split | Intramuscular | 0.25/0.5 0.5 | 6M-3Y/>3Y >3Y | 2/1 1 | 2011/2008 2018 |
| Sinovac Biotech Ltd. | Trivalent split Tetravalent split | Intramuscular | 0.25/0.5 0.5 | 6M-3Y/>3Y >3Y | 2/1 1 | 2005 2020 |
| Changchun Institute of Biological Products Co., Ltd. | Trivalent split Tetravalent split | Intramuscular | 0.25/0.5 0.5 | 6M-3Y/>3Y >3Y | 2/1 1 | 2007/2004 2020 |
| Shanghai Institute of Biological Products Co., Ltd. | Trivalent split Tetravalent split | Intramuscular | 0.25/0.5 0.5 | 6M-3Y/>3Y >3Y | 2/1 1 | 2004/2001 2021 |
| GDK Biotechnology Co., Ltd. | Tetravalent split | Intramuscular | 0.5 | >3Y | 1 | 2019 |
| Wuhan Institute of Biological Products Co., Ltd. | Tetravalent split | Intramuscular | 0.5 | >3Y | 1 | 2020 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, J.; Nian, X.; Li, X.; Huang, S.; Duan, K.; Li, X.; Yang, X. The Epidemiology of Influenza and the Associated Vaccines Development in China: A Review. Vaccines 2022, 10, 1873. https://doi.org/10.3390/vaccines10111873
Zhang J, Nian X, Li X, Huang S, Duan K, Li X, Yang X. The Epidemiology of Influenza and the Associated Vaccines Development in China: A Review. Vaccines. 2022; 10(11):1873. https://doi.org/10.3390/vaccines10111873
Chicago/Turabian StyleZhang, Jiayou, Xuanxuan Nian, Xuedan Li, Shihe Huang, Kai Duan, Xinguo Li, and Xiaoming Yang. 2022. "The Epidemiology of Influenza and the Associated Vaccines Development in China: A Review" Vaccines 10, no. 11: 1873. https://doi.org/10.3390/vaccines10111873






