Serum Metabolic Correlates of the Antibody Response in Subjects Receiving the Inactivated COVID-19 Vaccine
Abstract
1. Introduction
2. Methods
2.1. Sample Collection
2.2. Detection of Anti-SARS-CoV-2 Receptor Binding Domain (RBD) Neutralizing Responses, Antibodies, and IgG
2.3. Liquid Chromatography–Mass Spectrometry (LC-MS) Sample Procedure
2.4. Data Processing and Statistical Analysis
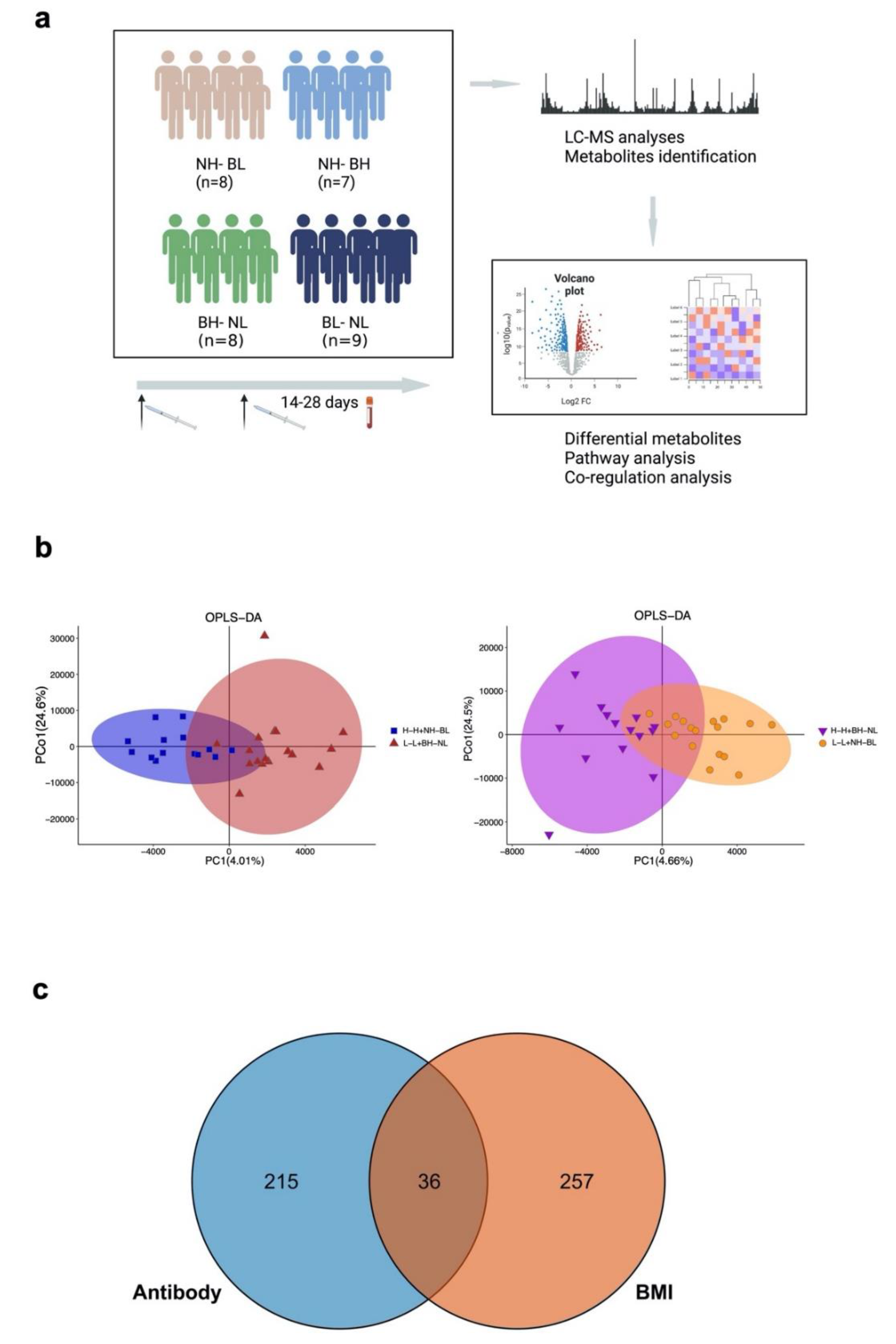
3. Results
3.1. Demographic Characteristics and Immune Response after Two-dose Vaccination
3.2. Metabolites Detection among Two-dose Vaccines
3.3. Differential Expression Metabolites between High- and Low-Antibody Groups
3.4. Differential Expression Metabolites between the High- and Low-BMI Groups
3.5. Interaction between the Antibodies and BMI Mediated by Metabolites
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Corrado, M.; Pearce, E.L. Targeting memory T cell metabolism to improve immunity. J. Clin. Investig. 2022, 132, e148546. [Google Scholar] [CrossRef]
- O’Neill, L.A.; Kishton, R.J.; Rathmell, J. A guide to immunometabolism for immunologists. Nat. Rev. Immunol. 2016, 16, 553–565. [Google Scholar] [CrossRef] [PubMed]
- Collins, J.M.; Jones, D.P.; Sharma, A.; Khadka, M.; Liu, K.H.; Kempker, R.R.; Prideaux, B.; Maner-Smith, K.; Tukvadze, N.; Shah, N.S.; et al. TCA cycle remodeling drives proinflammatory signaling in humans with pulmonary tuberculosis. PLoS Pathog. 2021, 17, e1009941. [Google Scholar] [CrossRef] [PubMed]
- Collins, J.M.; Siddiqa, A.; Jones, D.P.; Liu, K.; Kempker, R.R.; Nizam, A.; Shah, N.S.; Ismail, N.; Ouma, S.G.; Tukvadze, N.; et al. Tryptophan catabolism reflects disease activity in human tuberculosis. JCI Insight 2020, 5, e137131. [Google Scholar] [CrossRef] [PubMed]
- Johns Hopkins University. Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. Available online: https://www.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 (accessed on 5 October 2020).
- Frasca, D.; Reidy, L.; Romero, M.; Diaz, A.; Cray, C.; Blomberg, B.B. The majority of SARS-CoV-2-specific antibodies in COVID-19 patients with obesity are autoimmune and not neutralizing. Int. J. Obes. Lond. 2022, 46, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Frasca, D.; Reidy, L.; Cray, C.; Diaz, A.; Romero, M.; Kahl, K.; Blomberg, B.B. Influence of obesity on serum levels of SARS-CoV-2-specific antibodies in COVID-19 patients. PLoS ONE 2021, 16, e0245424. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Shu, T.; Yang, X.; Song, J.-X.; Zhang, M.; Yao, C.; Liu, W.; Huang, M.; Yu, Y.; Yang, Q.; et al. Plasma metabolomic and lipidomic alterations associated with COVID-19. Natl. Sci. Rev. 2020, 7, 1157–1168. [Google Scholar] [CrossRef]
- Lee, W.; Ahn, J.H.; Park, H.H.; Kim, H.N.; Kim, H.; Yoo, Y.; Shin, H.; Hong, K.S.; Jang, J.G.; Park, C.G.; et al. COVID-19-activated SREBP2 disturbs cholesterol biosynthesis and leads to cytokine storm. Signal Transduct. Target. Ther. 2020, 5, 186. [Google Scholar] [CrossRef]
- Waickman, A.T.; Victor, K.; Li, T.; Hatch, K.; Rutvisuttinunt, W.; Medin, C.; Gabriel, B.; Jarman, R.G.; Friberg, H.; Currier, J.R. Dissecting the heterogeneity of DENV vaccine-elicited cellular immunity using single-cell RNA sequencing and metabolic profiling. Nat. Commun. 2019, 10, 3666. [Google Scholar] [CrossRef]
- Diray-Arce, J.; Angelidou, A.; Jensen, K.J.; Conti, M.G.; Kelly, R.S.; Pettengill, M.A.; Liu, M.; van Haren, S.D.; McCulloch, S.D.; Michelloti, G.; et al. Bacille Calmette-Guérin vaccine reprograms human neonatal lipid metabolism in vivo and in vitro. Cell Rep. 2022, 39, 110772. [Google Scholar] [CrossRef]
- Li, S.; Sullivan, N.L.; Rouphael, N.; Yu, T.; Banton, S.; Maddur, M.S.; McCausland, M.; Chiu, C.; Canniff, J.; Dubey, S.; et al. Metabolic Phenotypes of Response to Vaccination in Humans. Cell 2017, 169, 862–877.e17. [Google Scholar] [CrossRef] [PubMed]
- Anastassopoulou, C.; Antoni, D.; Manoussopoulos, Y.; Stefanou, P.; Argyropoulou, S.; Vrioni, G.; Tsakris, A. Age and sex associations of SARS-CoV-2 antibody responses post BNT162b2 vaccination in healthcare workers: A mixed effects model across two vaccination periods. PLoS ONE 2022, 17, e0266958. [Google Scholar] [CrossRef] [PubMed]
- Levin, E.G.; Lustig, Y.; Cohen, C.; Fluss, R.; Indenbaum, V.; Amit, S.; Doolman, R.; Asraf, K.; Mendelson, E.; Ziv, A.; et al. Waning Immune Humoral Response to BNT162b2 Covid-19 Vaccine over 6 Months. N. Engl. J. Med. 2021, 385, e84. [Google Scholar] [CrossRef]
- Gaayeb, L.; Pinçon, C.; Cames, C.; Sarr, J.-B.; Seck, M.; Schacht, A.-M.; Remoué, F.; Hermann, E.; Riveau, G. Immune response to Bordetella pertussis is associated with season and undernutrition in Senegalese children. Vaccine 2014, 32, 3431–3437. [Google Scholar] [CrossRef]
- Moore, S.E.; Collinson, A.C.; Fulford, A.J.; Jalil, F.; Siegrist, C.-A.; Goldblatt, D.; Hanson, L.; Prentice, A.M. Effect of month of vaccine administration on antibody responses in The Gambia and Pakistan. Trop. Med. Int. Health 2006, 11, 1529–1541. [Google Scholar] [CrossRef]
- Jones, R.P.; Ponomarenko, A. Roles for Pathogen Interference in Influenza Vaccination, with Implications to Vaccine Effectiveness (VE) and Attribution of Influenza Deaths. Infect. Dis. Rep. 2022, 14, 76. [Google Scholar] [CrossRef] [PubMed]
- Murugan, S.; Jakka, P.; Namani, S.; Mujumdar, V.; Radhakrishnan, G. The neurosteroid pregnenolone promotes degradation of key proteins in the innate immune signaling to suppress inflammation. J. Biol. Chem. 2019, 294, 4596–4607. [Google Scholar] [CrossRef]
- Abdrabou, W.; Dieng, M.M.; Diawara, A.; Sermé, S.S.; Almojil, D.; Sombié, S.; Henry, N.B.; Kargougou, D.; Manikandan, V.; Soulama, I.; et al. Metabolome modulation of the host adaptive immunity in human malaria. Nat. Metab. 2021, 3, 1001–1016. [Google Scholar] [CrossRef]
- Lee, J.H.; Ulrich, B.; Cho, J.; Park, J.; Kim, C.H. Progesterone Promotes Differentiation of Human Cord Blood Fetal T Cells into T Regulatory Cells but Suppresses Their Differentiation into Th17 Cells. J. Immunol. 2011, 187, 1778–1787. [Google Scholar] [CrossRef]
- Hierweger, A.M.; Engler, J.B.; Friese, M.A.; Reichardt, H.M.; Lydon, J.; DeMayo, F.; Mittrücker, H.; Arck, P.C. Progesterone modulates the T-cell response via glucocorticoid receptor-dependent pathways. Am. J. Reprod. Immunol. 2019, 81, e13084. [Google Scholar] [CrossRef]
- Su, S.; Hua, D.; Li, J.P.; Zhang, X.N.; Bai, L.; Cao, L.B.; Shu, H.B. Modulation of innate immune response to viruses including SARS-CoV-2 by progesterone. Signal Transduct. Target Ther. 2022, 25, 137. [Google Scholar] [CrossRef]
- Baumruker, T.; Prieschl, E. Sphingolipids and the regulation of the immune response. Semin. Immunol. 2002, 14, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Huang, F.-C. The Role of Sphingolipids on Innate Immunity to Intestinal Salmonella Infection. Int. J. Mol. Sci. 2017, 18, 1720. [Google Scholar] [CrossRef]
- Brown, E.M.; Ke, X.; Hitchcock, D.; Jeanfavre, S.; Avila-Pacheco, J.; Nakata, T.; Arthur, T.D.; Fornelos, N.; Heim, C.; Franzosa, E.A.; et al. Bacteroides-Derived Sphingolipids Are Critical for Maintaining Intestinal Homeostasis and Symbiosis. Cell Host Microbe 2019, 25, 668–680.e7. [Google Scholar] [CrossRef] [PubMed]
- Schirmer, M.; Garner, A.; Vlamakis, H.; Xavier, R.J. Microbial genes and pathways in inflammatory bowel disease. Nat. Rev. Microbiol. 2019, 17, 497–511. [Google Scholar] [CrossRef]
- Van der Wielen, M.; Van Damme, P.; Chlibek, R.; Smetana, J.; von Sonnenburg, F. Hepatitis A/B vaccination of adults over 40 years old: Comparison of three vaccine regimens and effect of influencing factors. Vaccine 2006, 24, 5509–5515. [Google Scholar] [CrossRef] [PubMed]
- Roome, A.J.; Walsh, S.J.; Cartter, M.L.; Hadler, J.L. Hepatitis B vaccine responsiveness in Connecticut public safety personnel. JAMA 1993, 270, 2931–2934. [Google Scholar] [CrossRef]
- Yang, S.; Tian, G.; Cui, Y.; Ding, C.; Deng, M.; Yu, C.; Xu, K.; Ren, J.; Yao, J.; Li, Y.; et al. Factors influencing immunologic response to hepatitis B vaccine in adults. Sci. Rep. 2016, 6, 27251. [Google Scholar] [CrossRef]
- Sheridan, P.A.; Paich, H.A.; Handy, J.; Karlsson, E.A.; Hudgens, M.G.; Sammon, A.B.; Holland, L.A.; Weir, S.; Noah, T.L.; Beck, M.A. Obesity is associated with impaired immune response to influenza vaccination in humans. Int. J. Obes. 2012, 36, 1072–1077. [Google Scholar] [CrossRef]
- Muskiet, F.A.J.; Carrera-Bastos, P.; Pruimboom, L.; Lucia, A.; Furman, D. Obesity and Leptin Resistance in the Regulation of the Type I Interferon Early Response and the Increased Risk for Severe COVID-19. Nutrients 2022, 14, 1388. [Google Scholar] [CrossRef]
- Namazi, M.R. Cytochrome-P450 enzymes and autoimmunity: Expansion of the relationship and introduction of free radicals as the link. J. Autoimmune Dis. 2009, 6, 4. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulou, E.; Pircalabioru, G.G.; Bezirtzoglou, E. The Role of Cytochromes P450 in Infection. Front. Immunol. 2018, 9, 89. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Choi, F.F.K.; Zhou, Y.; Leung, F.P.; Tan, S.; Lin, S.; Xu, H.; Jia, W.; Sung, J.J.Y.; Cai, Z.; et al. Metabolite profiling of plasma and urine from rats with TNBS-induced acute colitis using UPLC-ESI-QTOF-MS-based metabonomics—A pilot study. FEBS J. 2012, 279, 2322–2338. [Google Scholar] [CrossRef] [PubMed]
- Gong, H.; Zhang, S.; Li, Q.; Zuo, C.; Gao, X.; Zheng, B.; Lin, M. Gut microbiota compositional profile and serum metabolic phenotype in patients with primary open-angle glaucoma. Exp. Eye Res. 2020, 191, 107921. [Google Scholar] [CrossRef] [PubMed]
- Radzikowska, U.; Rinaldi, A.O.; Çelebi, Z.C.; Karaguzel, D.; Wojcik, M.; Cypryk, K.; Akdis, M.; Akdis, C.A.; Sokolowska, M. The Influence of Dietary Fatty Acids on Immune Responses. Nutrients 2019, 11, 2990. [Google Scholar] [CrossRef]
- Wincent, E.; Le Bihanic, F.; Dreij, K. Induction and inhibition of human cytochrome P4501 by oxygenated polycyclic aromatic hydrocarbons. Toxicol. Res. 2016, 5, 788–799. [Google Scholar] [CrossRef]



| Name | Subclass | Antibody p Value | High-Antibody Group | BMI p Value | Low BMI Group | Interaction p Value |
|---|---|---|---|---|---|---|
| 2-Octen-4-one | Carbonyl compounds | 0.001 | up | 0.047 | up | 0.041 |
| 1-Phenyl-1-pentanone | Carbonyl compounds | 0.008 | up | 0.024 | up | 0.029 |
| Tetraethylene glycol | Ethers | 0.026 | up | 0.023 | up | 0.020 |
| 9,12-dioxo-dodecanoic acid | Fatty Acids and Conjugates | 0.042 | up | 0.011 | up | 0.003 |
| 3-Ethyltridecan-2-one | Oxygenated hydrocarbons | 0.033 | up | 0.001 | up | 0.012 |
| Cholic acid glucuronide | Steroidal glycosides | 0.023 | down | 0.002 | down | 0.048 |
| 3-Oxo-5β-chol-1-en-24-oic Acid | Unclassified | 0.018 | down | 0.003 | up | 0.024 |
| Nitrosobenzene | Unclassified | 0.015 | up | 0.018 | up | 0.045 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Yue, Q.; Zhu, H.; Song, J.; Li, D.; Liu, W.; Jiang, S.; Jiang, N.; Qiu, C.; Ai, J.; et al. Serum Metabolic Correlates of the Antibody Response in Subjects Receiving the Inactivated COVID-19 Vaccine. Vaccines 2022, 10, 1890. https://doi.org/10.3390/vaccines10111890
Zhang Y, Yue Q, Zhu H, Song J, Li D, Liu W, Jiang S, Jiang N, Qiu C, Ai J, et al. Serum Metabolic Correlates of the Antibody Response in Subjects Receiving the Inactivated COVID-19 Vaccine. Vaccines. 2022; 10(11):1890. https://doi.org/10.3390/vaccines10111890
Chicago/Turabian StyleZhang, Yi, Qiaoyan Yue, Haojing Zhu, Jieyu Song, Dingding Li, Wen Liu, Shujun Jiang, Ning Jiang, Chao Qiu, Jingwen Ai, and et al. 2022. "Serum Metabolic Correlates of the Antibody Response in Subjects Receiving the Inactivated COVID-19 Vaccine" Vaccines 10, no. 11: 1890. https://doi.org/10.3390/vaccines10111890
APA StyleZhang, Y., Yue, Q., Zhu, H., Song, J., Li, D., Liu, W., Jiang, S., Jiang, N., Qiu, C., Ai, J., Zhang, Y., & Zhang, W. (2022). Serum Metabolic Correlates of the Antibody Response in Subjects Receiving the Inactivated COVID-19 Vaccine. Vaccines, 10(11), 1890. https://doi.org/10.3390/vaccines10111890





