Stakeholder Perspectives of Australia’s National HPV Vaccination Program
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Key Stakeholder Interviews
3.1.1. Experience of 2 Dose Transition
3.1.2. Consent Forms
3.1.3. Delivery Models
3.1.4. Strategies for Aboriginal and Torres Strait Islander Students
“Health checks, you can get a T-shirt and … a gift voucher. But we’re not funded for that stuff and the best way, for Australia and getting their immunisations rate up, would be to offer an incentive.”(ACCHS Nurse Immuniser)
“Signing a consent document which is very wordy and in English, can be a barrier for some students to get their parents to sign or to have that full understanding of what … vaccines their children are having.”(Immunisation Public Health Nurse)
3.1.5. Strategies for Culturally and Linguistically Diverse Students
“We do have CALD resources in 15 different languages, but apart from that we don’t have specific program things, I don’t think. And also we don’t have any research about that particular community, how well they are accessing the HPV vaccine. Because it’s obviously not recorded on the AIR, it’s hard to get that data.”(State Immunisation Program Manager)
3.1.6. Strategies for Students with Lower Socioeconomic Status
3.1.7. Vaccine Hesitancy
3.1.8. Vaccine Coverage Target
3.2. Online Survey
3.2.1. Experience of 2 Dose Transition
“Schools are happy that we only need two visits to complete the series for the year. It is also easier to staff for two visits instead of three and costs less in wages for staff.”(Regional area local council nurse immuniser)
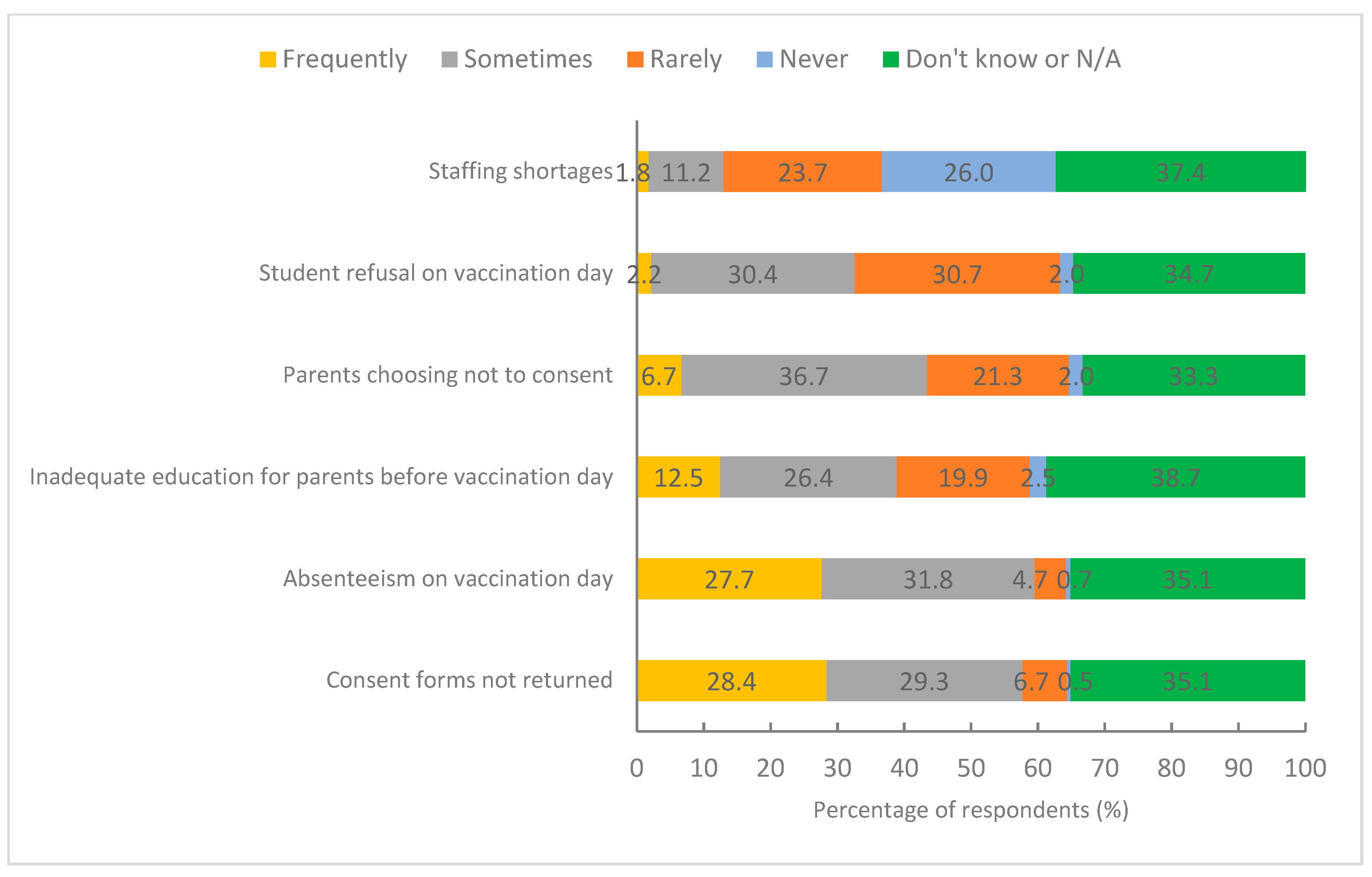
3.2.2. School-Based Vaccination Coverage
“Electronic consent forms would circumvent students not passing consent forms on to their parents and/or not returning them to the school. It would also eliminate the middle man (i.e., the school/teachers) & avoid issues such as failure to give consent forms to all students … and misplaced/lost consent forms.”(Regional area school-based nurse immuniser and practice nurse)
“Digital reminders and increased education sessions of both the students and parents prior to the vaccination. An info brochure is not enough, as many students don’t know what they are being vaccinated for at the time and don’t remember later on.”(Remote area women’s health nurse and immuniser)
3.2.3. Role of Primary Care
“The process to obtain vaccines is not straightforward, as GPs are not allowed to have any stock but rather have to order it in individually for each person. This creates potentially two visits to the GP, which they may choose to charge a fee for.”(Major city school-based nurse immuniser)
“There is no interaction between local schools and my practice. I will not know which children have missed out on the day of vaccine in their school, unless they are self-presenting to my clinic.”(Major city General Practitioner)
3.2.4. Priority Populations
“Return of consent forms and attendance very poor. Many verbal consents are obtained on site. This is very time consuming due to the high number we do … Liaising with Aboriginal Health and Community Health Centres has been successful to a degree.”(Major city school-based nurse immuniser)
“Difficulty getting information from school on the language spoken at home and so the correct consent form to give to the family. Lack of understanding on what the vaccine is for. Even when a self-addressed envelope was sent to parents from one school for easy return to us, the rate was still very low of returned cards.”(Regional area school-based nurse immuniser)
“We find that we often get lower uptake in schools in areas of socioeconomic disadvantage—less consent forms returned for the first dose as well as increased absenteeism.”(Regional area school-based nurse immuniser)
3.2.5. Vaccine Hesitancy
3.2.6. Coverage Target
“I feel there should be more responsibility on the schools/teachers to assist with the return of consent forms. The ones that have no desire to chase up consent forms have no consequences, return rates are low, vaccination rates are low and it’s almost impossible for us to chase up these students.”(Major city school-based nurse immuniser)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Martel, C.; Plummer, M.; Vignat, J.; Franceschi, S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int. J. Cancer 2017, 141, 664–670. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhatia, N.; Lynde, C.; Vender, R.; Bourcier, M. Understanding Genital Warts: Epidemiology, Pathogenesis, and Burden of Disease of Human Papillomavirus. J. Cutan. Med. Surg. 2013, 17, S47–S54. [Google Scholar] [CrossRef] [PubMed]
- Fortes, H.R.; von Ranke, F.M.; Escuissato, D.L.; Araujo Neto, C.A.; Zanetti, G.; Hochhegger, B.; Souza, C.A.; Marchiori, E. Recurrent respiratory papillomatosis: A state-of-the-art review. Respir. Med. 2017, 126, 116–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Arbyn, M.; Weiderpass, E.; Bruni, L.; de Sanjosé, S.; Saraiya, M.; Ferlay, J.; Bray, F. Estimates of incidence and mortality of cervical cancer in 2018: A worldwide analysis. Lancet Glob. Health 2020, 8, e191–e203. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. Available online: https://www.who.int/publications/i/item/9789240014107 (accessed on 28 August 2022).
- Australian Centre for the Prevention of Cervical Cancer. Development of Australia’s National Cervical Cancer Elimination Strategy. Available online: https://acpcc.org.au/elimination/ (accessed on 18 September 2022).
- Hall, M.T.; Simms, K.T.; Lew, J.B.; Smith, M.A.; Brotherton, J.M.; Saville, M.; Frazer, I.H.; Canfell, K. The projected timeframe until cervical cancer elimination in Australia: A modelling study. Lancet Public Health 2019, 4, e19–e27. [Google Scholar] [CrossRef] [Green Version]
- Whop, L.J.; Smith, M.A.; Butler, T.L.; Adcock, A.; Bartholomew, K.; Goodman, M.T.; Winer, R.L.; Milosevic, E.; Lawton, B. Achieving cervical cancer elimination among Indigenous women. Prev. Med. 2021, 144, 106314. [Google Scholar] [CrossRef]
- NHMRC Centre of Research Excellence in Cervical Cancer Control. Cervical Cancer Elimination Progress Report: Australia’s Progress towards the Elimination of Cervical Cancer as a Public Health Problem. Available online: https://www.cervicalcancercontrol.org.au/wp-content/uploads/2021/03/2021-C4-CRE-Elim-Report.pdf (accessed on 28 August 2022).
- The Kirby Institute. Genital Warts Surveillance Network Report 2004–2015. Available online: https://kirby.unsw.edu.au/report/genital-warts-surveillance-network-report-2004-2015 (accessed on 3 November 2022).
- Smith, M.A.; Liu, B.; McIntyre, P.; Menzies, R.; Dey, A.; Canfell, K. Fall in genital warts diagnoses in the general and indigenous Australian population following implementation of a national human papillomavirus vaccination program: Analysis of routinely collected national hospital data. J. Infect. Dis. 2015, 211, 91–99. [Google Scholar] [CrossRef] [Green Version]
- Drolet, M.; Bénard, É.; Pérez, N.; Brisson, M. Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: Updated systematic review and meta-analysis. Lancet 2019, 394, 497–509. [Google Scholar] [CrossRef] [Green Version]
- Novakovic, D.; Cheng, A.T.L.; Zurynski, Y.; Booy, R.; Walker, P.J.; Berkowitz, R.; Harrison, H.; Black, R.; Perry, C.; Vijayasekaran, S.; et al. A Prospective Study of the Incidence of Juvenile-Onset Recurrent Respiratory Papillomatosis After Implementation of a National HPV Vaccination Program. J. Infect. Dis. 2018, 217, 208–212. [Google Scholar] [CrossRef]
- Meites, E.; Stone, L.; Amiling, R.; Singh, V.; Unger, E.R.; Derkay, C.S.; Markowitz, L.E. Significant Declines in Juvenile-onset Recurrent Respiratory Papillomatosis Following Human Papillomavirus (HPV) Vaccine Introduction in the United States. Clin. Infect. Dis. 2021, 73, 885–890. [Google Scholar] [CrossRef]
- Toh, Z.Q.; Kosasih, J.; Russell, F.M.; Garland, S.M.; Mulholland, E.K.; Licciardi, P.V. Recombinant human papillomavirus nonavalent vaccine in the prevention of cancers caused by human papillomavirus. Infect. Drug Resist. 2019, 12, 1951–1967. [Google Scholar] [CrossRef] [Green Version]
- Kamolratanakul, S.; Pitisuttithum, P. Human Papillomavirus Vaccine Efficacy and Effectiveness against Cancer. Vaccines 2021, 9, 1413. [Google Scholar] [CrossRef]
- Mensah, F.A.; Mehta, M.R.; Lewis, J.S., Jr.; Lockhart, A.C. The Human Papillomavirus Vaccine: Current Perspective and Future Role in Prevention and Treatment of Anal Intraepithelial Neoplasia and Anal Cancer. Oncologist 2016, 21, 453–460. [Google Scholar] [CrossRef] [Green Version]
- Nielsen, K.J.; Jakobsen, K.K.; Jensen, J.S.; Grønhøj, C.; Von Buchwald, C. The Effect of Prophylactic HPV Vaccines on Oral and Oropharyngeal HPV Infection-A Systematic Review. Viruses 2021, 13, 1339. [Google Scholar] [CrossRef]
- Australian Government Department of Health and Aged Care. Government Funds Gardasil. Available online: https://www.pbs.gov.au/info/news/2006/11/aust-govt-funds-gardasil (accessed on 18 September 2022).
- National Centre for Immunisation Research and Surveillance. Significant Events in Human Papillomavirus (HPV) Vaccination Practice in Australia. Available online: https://www.ncirs.org.au/sites/default/files/2018-11/Human-papillomavirus-history-July-2018.pdf (accessed on 18 September 2022).
- Wnukowski-Mtonga, P.; Jayasinghe, S.; Chiu, C.; Macartney, K.; Brotherton, J.; Donovan, B.; Hall, M.; Smith, D.; Peterson, K.; Campbell-Lloyd, S.; et al. Scientific evidence supporting recommendations on the use of the 9-valent HPV vaccine in a 2-dose vaccine schedule in Australia. Commun. Dis. Intell. 2020, 44. [Google Scholar] [CrossRef]
- Australian Technical Advisory Group on Immunisation (ATAGI). Introduction of Gardasil9 in a 2-Dose Schedule under the School-Based National Immunisation Program (NIP). Available online: https://www.health.gov.au/sites/default/files/atagi-advice-gardasil-9-in-the-school-based-nip-atagi-advice-gardasil-9-in-the-school-based-nip.pdf (accessed on 28 August 2022).
- Australian Government Department of Health and Aged Care. HPV (Human Papillomavirus) Vaccine. Available online: https://www.health.gov.au/health-topics/immunisation/vaccines/human-papillomavirus-hpv-immunisation-service#:~:text=HPV%20vaccine%20is%20free%20under,doses%20of%20HPV%20vaccine%20free (accessed on 9 October 2022).
- Australian Government Department of Health and Aged Care. HPV Vaccination Records are Moving to the Australian Immunisation Register (AIR). Available online: https://www.health.gov.au/news/hpv-vaccination-records-are-moving-to-the-australian-immunisation-register-air (accessed on 18 September 2022).
- National Centre for Immunisation Research and Surveillance. Evaluation of the National Human Papillomavirus Vaccination Program. Available online: https://beta.health.gov.au/news-and-events/news/evaluation-of-the-national-hpv-program (accessed on 9 October 2022).
- Brotherton, J.; Hendry, A.; Dey, A.; Hull, B.P.; Beard, F. HPV vaccination coverage: Slightly improved two-dose schedule completion estimates and historical estimates lower on AIR than HPV Register. Aust. N. Z. J. Public Health 2022, 46, 394–400. [Google Scholar] [CrossRef]
- National Centre for Immunisation Research and Surveillance. Annual Immunisation Coverage Report 2020. Available online: https://www.ncirs.org.au/sites/default/files/2021-11/NCIRS%20Annual%20Immunisation%20Coverage%20report%202020.pdf (accessed on 9 October 2022).
- Smith, M.A.; Winch, K.; Canfell, K.; Brotherton, J.M. Effective HPV vaccination coverage in Australia by number of doses and two-dose spacing: What if one or two doses are sufficient? Tumour Virus Res. 2021, 11, 200216. [Google Scholar] [CrossRef]
- Whop, L.J.; Butler, T.L.; Brotherton, J.M.L.; Anderson, K.; Cunningham, J.; Tong, A.; Garvey, G. Study protocol: Yarning about HPV Vaccination: A qualitative study of factors influencing HPV vaccination among Aboriginal and Torres Strait Islander adolescents in Australia. BMJ Open 2021, 11, e047890. [Google Scholar] [CrossRef]
- Selvey, L.A.; Roux, F.; Burns, S. Potential process improvements to increase coverage of human papillomavirus vaccine in schools—A focus on schools with low vaccine uptake. Vaccine 2020, 38, 2971–2977. [Google Scholar] [CrossRef]
- Burns, S.; Selvey, L.; Roux, F. Influences to HPV completion via a school-based immunisation program. Sex Educ. 2021, 21, 253–268. [Google Scholar] [CrossRef]
- Davies, C.; Stoney, T.; Hutton, H.; Parrella, A.; Kang, M.; Macartney, K.; Leask, J.; McCaffery, K.; Zimet, G.; Brotherton, J.M.L.; et al. School-based HPV vaccination positively impacts parents’ attitudes toward adolescent vaccination. Vaccine 2021, 39, 4190–4198. [Google Scholar] [CrossRef] [PubMed]
- Marshall, H.S.; Collins, J.; Sullivan, T.; Tooher, R.; O’Keefe, M.; Skinner, S.R.; Watson, M.; Burgess, T.; Ashmeade, H.; Braunack-Mayer, A. Parental and societal support for adolescent immunization through school based immunization programs. Vaccine 2013, 31, 3059–3064. [Google Scholar] [CrossRef] [PubMed]
- Netfa, F.; Tashani, M.; Booy, R.; King, C.; Rashid, H.; Skinner, S.R. Knowledge, Attitudes and Perceptions of Immigrant Parents Towards Human Papillomavirus (HPV) Vaccination: A Systematic Review. Trop. Med. Infect. Dis. 2020, 5, 58. [Google Scholar] [CrossRef] [Green Version]
- Netfa, F.; King, C.; Davies, C.; Rashid, H.; Tashani, M.; Booy, R.; Skinner, S.R. Knowledge, Attitudes, and Perceptions of the Arabic-Speaking Community in Sydney, Australia, toward the Human Papillomavirus (HPV) Vaccination Program: A Qualitative Study. Vaccines 2021, 9, 940. [Google Scholar] [CrossRef]
- Vujovich-Dunn, C.; Skinner, S.R.; Brotherton, J.; Wand, H.; Sisnowski, J.; Lorch, R.; Veitch, M.; Sheppeard, V.; Effler, P.; Gidding, H.; et al. School-Level Variation in Coverage of Co-Administered dTpa and HPV Dose 1 in Three Australian States. Vaccines 2021, 9, 1202. [Google Scholar] [CrossRef]
- Hull, B.; Hendry, A.; Dey, A.; Brotherton, J.; Macartney, K.; Beard, F. Annual Immunisation Coverage Report 2017. Commun. Dis. Intell. 2019, 43. [Google Scholar] [CrossRef]
- Australian Government Department of Health and Aged Care. National Preventive Health Strategy 2021–2030. Available online: https://www.health.gov.au/resources/publications/national-preventive-health-strategy-2021-2030 (accessed on 14 October 2022).
- Brisson, M.; Bénard, É.; Drolet, M.; Bogaards, J.A.; Baussano, I.; Vänskä, S.; Jit, M.; Boily, M.C.; Smith, M.A.; Berkhof, J.; et al. Population-level impact, herd immunity, and elimination after human papillomavirus vaccination: A systematic review and meta-analysis of predictions from transmission-dynamic models. Lancet Public Health 2016, 1, e8–e17. [Google Scholar] [CrossRef] [Green Version]
- Bruni, L.; Saura-Lázaro, A.; Montoliu, A.; Brotons, M.; Alemany, L.; Diallo, M.S.; Afsar, O.Z.; LaMontagne, D.S.; Mosina, L.; Contreras, M.; et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010-2019. Prev. Med. 2021, 144, 106399. [Google Scholar] [CrossRef]
- World Health Organization. Meeting of the Strategic Advisory Group of Experts on Immunization, April 2022: Conclusions and Recommendations. Available online: https://www.who.int/publications/i/item/who-wer9724-261-276 (accessed on 14 October 2022).
- Australian Government Department of Health and Aged Care. Dashboard, Nursing and Midwifery Dashboards. Available online: https://hwd.health.gov.au/resources/dashboards/nhwds-nursing-factsheets.html (accessed on 4 November 2022).
- Hull, B.P.; Hendry, A.J.; Dey, A.; Bryant, K.; Radkowski, C.; Pellissier, S.; Macartney, K.; Beard, F.H. The impact of the COVID-19 pandemic on routine vaccinations in Victoria. Med. J. Aust. 2021, 215, 83–84. [Google Scholar] [CrossRef]

| Key Stakeholder Group | Participants n (%) |
|---|---|
| State and territory immunisation program managers and associated staff; and local council immunisation staff | 19 (45.2) |
| Aboriginal Community Controlled Health Service staff and remote area immunisation coordinators | 9 (21.4) |
| Australian Government Department of Health immunisation staff and Therapeutic Goods Administration * | 5 (11.9) |
| Australian Government Department of Health, Cervical Screening Section and state-level cervical screening program manager | 3 (7.1) |
| HPV vaccination researchers and sexual health physician | 3 (7.1) |
| Seqirus † | 3 (7.1) |
| Total | 42 (100) |
| Respondent Characteristics | Respondents n (%) |
|---|---|
| Occupation | |
| GP | 778 (51.4) |
| GP practice nurse | 210 (13.9) |
| School-based nurse immuniser | 166 (11.0) |
| Aboriginal Health Worker | 5 (0.3) |
| Other * | 354 (23.4) |
| Gender | |
| Female | 1319 (87.2) |
| Male | 189 (12.5) |
| Other | 5 (0.3) |
| Age group | |
| <25 years | 6 (0.4) |
| 25–34 years | 123 (8.1) |
| 35–44 years | 287 (19.0) |
| 45–54 years | 416 (27.5) |
| 55 years and over | 681 (45.0) |
| Location of employment | |
| New South Wales | 477 (31.5) |
| Victoria | 403 (26.6) |
| Queensland | 260 (17.2) |
| Western Australia | 184 (12.2) |
| South Australia | 115 (7.6) |
| Northern Territory | 26 (1.7) |
| Australian Capital Territory | 24 (1.6) |
| Tasmania | 19 (1.3) |
| Other | 14 (0.9) |
| Rurality of employment | |
| Major city | 911 (60.2) |
| Regional | 511 (33.8) |
| Remote | 91 (6.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Swift, C.; Dey, A.; Rashid, H.; Clark, K.; Manocha, R.; Brotherton, J.; Beard, F. Stakeholder Perspectives of Australia’s National HPV Vaccination Program. Vaccines 2022, 10, 1976. https://doi.org/10.3390/vaccines10111976
Swift C, Dey A, Rashid H, Clark K, Manocha R, Brotherton J, Beard F. Stakeholder Perspectives of Australia’s National HPV Vaccination Program. Vaccines. 2022; 10(11):1976. https://doi.org/10.3390/vaccines10111976
Chicago/Turabian StyleSwift, Caitlin, Aditi Dey, Harunor Rashid, Katrina Clark, Ramesh Manocha, Julia Brotherton, and Frank Beard. 2022. "Stakeholder Perspectives of Australia’s National HPV Vaccination Program" Vaccines 10, no. 11: 1976. https://doi.org/10.3390/vaccines10111976
APA StyleSwift, C., Dey, A., Rashid, H., Clark, K., Manocha, R., Brotherton, J., & Beard, F. (2022). Stakeholder Perspectives of Australia’s National HPV Vaccination Program. Vaccines, 10(11), 1976. https://doi.org/10.3390/vaccines10111976







