Exploration into the Influencing Factors for the Intention of the Public to Vaccinate against Infectious Diseases Based on the Theory of Planned Behavior—Example of the COVID-19 Vaccine
Abstract
1. Background
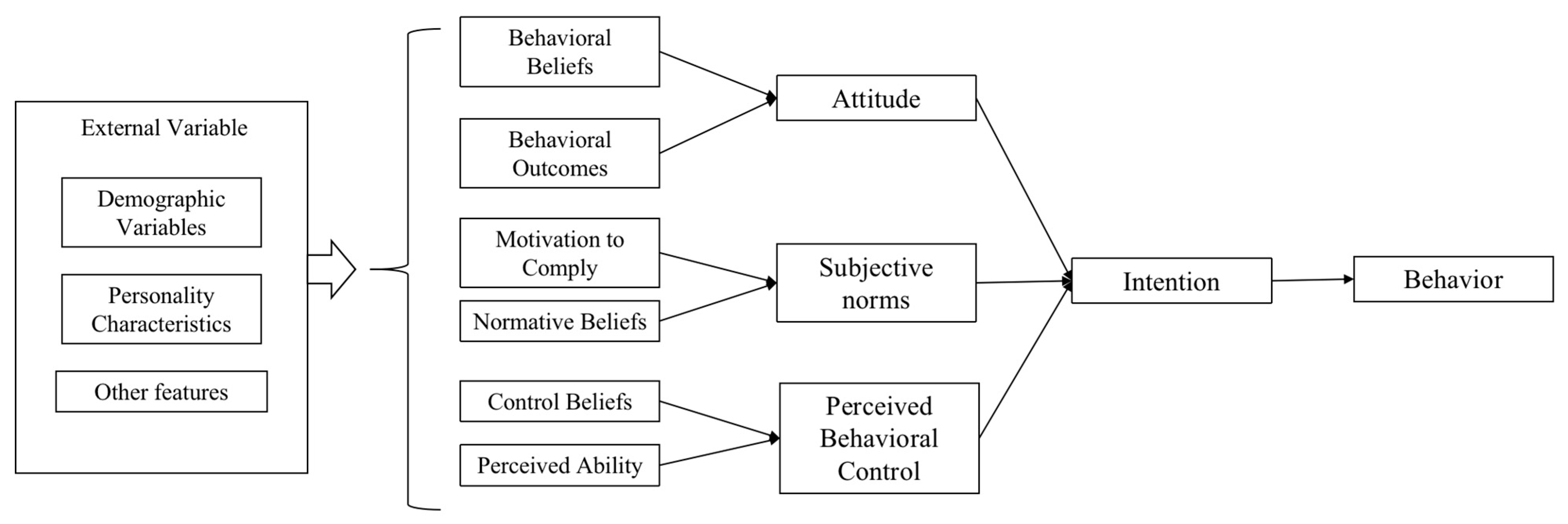
2. Materials and Methods
2.1. Participants and Procedures
2.2. Measures
3. Results
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhan, S.Y. Epidemiology; People’s Medical Publishing House: Beijing, China, 2017; pp. 208–209. [Google Scholar]
- How Was the British New Crown Variant That Caused Chaos in Europe Found? What Does It Mean for Vaccines. China Youth Daily. 22 December 2020. Available online: https://baijiahao.baidu.com/s?id=1686760629683256807&wfr=spider&for=pc (accessed on 4 March 2023).
- The Variant of the New Coronavirus Detected in India Has Spread to More than 40 Countries and Regions. Beijing Daily. 12 May 2021. Available online: http://henan.china.com.cn/news/2021-05/13/content_41559745.htm (accessed on 4 March 2023).
- About Omicron, the Authoritative Answer of the National Health Commission Is Here! CCTV News. 29 November 2021. Available online: https://content-static.cctvnews.cctv.com/snow-book/index.html?toc_style_id=feeds_default&share_to=copy_url&item_id=443257440784935416&track_id=E32059DA-05D6-444E-BD8A-2AE902E755EF_659879106725 (accessed on 4 March 2023).
- At Present, the Domestic Epidemic Strains Are Still Mainly BA.5.2 and BF.7, and No New Variants Have Been Imported. China News. 30 January 2023. Available online: https://baijiahao.baidu.com/s?id=1756441286931162985&wfr=spider&for=pc (accessed on 4 March 2023).
- Zhong Nanshan: In the Future, It May Be Necessary to Get Regular COVID-19 Vaccines. The Paper. 20 May 2021. Available online: https://www.thepaper.cn/newsDetail_forward_12771276 (accessed on 4 March 2023).
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I.; Fishbein, M. Attitude-behavior relations: A theoretical analysis and review of empirical research. Psychol. Bull. 1977, 84, 888–918. [Google Scholar] [CrossRef]
- Zhang, X.; Wang, F.; Zhu, C.; Wang, Z. Willingness to Self-Isolate When Facing a Pandemic Risk: Model, Empirical Test, and Policy Recommendations. Int. J. Environ. Res. Public Health 2020, 17, 197. [Google Scholar] [CrossRef]
- Agarwal, V. A/H1N1 Vaccine Intentions in College Students: An Application of the Theory of Planned Behavior. J. Am. Coll. Health J. ACH 2014, 62, 416–424. [Google Scholar] [CrossRef]
- Liao, Q.; Cowling, B.; Lam, W.; Fielding, R. Factors affecting intention to receive and actual receipt of 2009 Pandemic (H1N1) Vaccine in Hong Kong: A longitudinal study. PLoS ONE 2011, 6, e17713. [Google Scholar] [CrossRef]
- Painter, J.E.; Gargano, L.M.; Sales, J.M.; Morfaw, C.; Jones, L.M.; Murray, D.; DiClemente, R.J.; Hughes, J.M. Correlates of 2009 H1N1 influenza vaccine acceptability among parents and their adolescent children. Health Educ. Res. 2011, 26, 751–760. [Google Scholar] [CrossRef]
- Lv, Z.Z. Health Education and Health Promotion; Peking University Press: Beijing, China, 2002; pp. 40–41. [Google Scholar]
- Fu, H. Science of Health Education; People’s Medical Publishing House: Beijing, China, 2019; p. 55. [Google Scholar]
- Lin, C.Y.; Imani, V.; Majd, N.R.; Ghasemi, Z.; Griffiths, M.D.; Hamilton, K.; Hagger, M.S.; Pakpour, A.H. Using an integrated social cognition model to predict COVID-19 preventive behaviours. Br. J. Health Psychol. 2020, 25, 981–1005. [Google Scholar] [CrossRef]
- Barile, J.P.; Guerin, R.J.; Fisher, K.A.; Tian, L.H.; Okun, A.H.; Vanden Esschert, K.L.; Jeffers, A.; Gurbaxani, B.M.; Thompson, W.W.; Prue, C.E. Theory-Based Behavioral Predictors of Self-Reported Use of Face Coverings in Public Settings during the COVID-19 Pandemic in the United States. Ann. Behav. Med. 2021, 55, 82–88. [Google Scholar] [CrossRef]
- Wong, L.P.; Alias, H.; Wong, P.F.; Lee, H.Y.; AbuBakar, S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum. Vaccines Immunother. 2020, 6, 2204–2214. [Google Scholar] [CrossRef] [PubMed]
- Shmueli, L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health 2021, 21, 804–817. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Ajzen, I. Constructing a TPB Questionnaire: Conceptual and Methodological Considerations. 2006, pp. 1–14. Available online: https://www.semanticscholar.org/paper/Constructing-a-TpB-Questionnaire%3A-Conceptual-and-Ajzen/6074b33b529ea56c175095872fa40798f8141867 (accessed on 1 May 2023).
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.-L. Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef] [PubMed]
- Godin, G.; Vézina-Im, L.A.; Naccache, H. Determinants of Influenza Vaccination among Healthcare Workers. Infect. Control Hosp. Epidemiol. 2010, 31, 689–693. [Google Scholar] [CrossRef] [PubMed]
- Hauri, A.M.; Uphoff, H.; Gussmann, V.; Gawrich, S. Factors that affect influenza vaccine uptake among staff of long-term care facilities. Infect. Control Hosp. Epidemiol. 2006, 27, 638–641. [Google Scholar] [CrossRef]
- Lehmann, B.A.; Ruiter, R.; Dam, D.V.; Wicker, S.; Kok, G. Sociocognitive predictors of the intention of healthcare workers to receive the influenza vaccine in Belgian, Dutch and German hospital settings. J. Hosp. Infect. 2015, 89, 202–209. [Google Scholar] [CrossRef]
- Setbon, M.; Raude, J. Factors in vaccination intention against the pandemic influenza A/H1N1. Eur. J. Public Health 2010, 20, 490–494. [Google Scholar] [CrossRef]
- Robin, G.; Myers, L.B. Determinants of adults’ intention to vaccinate against pandemic swine flu. BMC Public Health 2011, 11, 15. [Google Scholar]
- Nowrouzi-Kia, B.; Mcgeer, A. External cues to action and influenza vaccination among post-graduate trainee physicians in Toronto, Canada. Vaccine 2014, 32, 3830–3834. [Google Scholar] [CrossRef]
- Rebmann, R.T.; Iqbal, A.; Anthony, M.J.; Knaup, R.C.; Wright, K.S.; Peters, E.B. H1N1 influenza vaccine compliance among hospital- and non-hospital-based healthcare personnel. Infect. Control Hosp. Epidemiol. 2012, 33, 737–744. [Google Scholar] [CrossRef]
- Corace, K.M.; Srigley, J.A.; Hargadon, D.P.; Yu, D.; MacDonald, T.K.; Fabrigar, L.R.; Garber, G.E. Using behavior change frameworks to improve healthcare worker influenza vaccination rates: A systematic review. Vaccine 2016, 34, 3235–3242. [Google Scholar] [CrossRef]
- Guidry, J.P.D.; Laestadius, L.I.; Vraga, E.K.; Miller, C.A.; Perrin, P.B.; Burton, C.W.; Ryan, M.; Fuemmeler, B.F.; Carlyle, K.E. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am. J. Infect. Control 2021, 49, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.C.; Fang, Y.; Cao, H.; Chen, H.; Hu, T.; Chen, Y.; Zhou, X.; Wang, Z. Behavioral Intention to Receive a COVID-19 Vaccination Among Chinese Factory Workers: Cross-sectional Online Survey. J. Med. Internet Res. 2021, 23, e24673. [Google Scholar] [CrossRef] [PubMed]
- Conner, M.; Armitage, C.J. Extending the Theory of Planned Behavior: A Review and Avenues for Further Research. J. Appl. Soc. Psychol. 2010, 28, 1429–1464. [Google Scholar] [CrossRef]
- Rosental, H.; Shmueli, L. Integrating Health Behavior Theories to Predict COVID-19 Vaccine Acceptance: Differences between Medical Students and Nursing Students. Vaccines 2021, 9, 783. [Google Scholar] [CrossRef] [PubMed]
- Berg, M.B.; Lin, L. Predictors of COVID-19 vaccine intentions in the United States: The role of psychosocial health constructs and demographic factors. Transl. Behav. Med. 2021, 11, 1782–1788. [Google Scholar] [CrossRef]
- Crowley, K.A.; Myers, R.; Magda, L.A.; Morse, S.S.; Brandt-Rauf, P.; Gershon, R.R.M. Prevalence and factors associated with 2009 to 2011 influenza vaccinations at a university medical center. Am. J. Infect. Control 2013, 41, 824–830. [Google Scholar] [CrossRef]
- Esteves-Jaramillo, A.; Omer, S.B.; Gonzalez-Diaz, E.; Salmon, D.A.; Hixson, B.; Navarro, F.; Kawa, S.; Frew, P.; Morfin-Otero, R.; Noriega, E.R.; et al. Acceptance of a Vaccine Against Novel Influenza A (H1N1) Virus Among Health Care Workers in Two Major Cities in Mexico. Arch. Med. Res. 2009, 40, 705–711. [Google Scholar] [CrossRef]
- Askarian, M.; Khazaeipour, Z.; Mclaws, M.L. Influenza vaccination uptake among students and clinical staff of a university in Iran. Int. J. Infect. Dis. 2008, 13, 476–482. [Google Scholar] [CrossRef]
- Armitage, C.J. Time to retire the theory of planned behaviour? A commentary on Sniehotta, Presseau and Araújo-Soares. Health Psychol Rev. 2015, 9, 151–155. [Google Scholar] [CrossRef]
| Characteristics | n | % | |
|---|---|---|---|
| Gender | Male | 1114 | 53.10 |
| Female | 984 | 46.90 | |
| Age group | 18–29 | 928 | 44.23 |
| 30–39 | 862 | 41.09 | |
| 40–49 | 238 | 11.34 | |
| ≥50 | 70 | 3.34 | |
| Education levels | High School | 180 | 8.58 |
| University | 1738 | 82.84 | |
| Postgraduate | 180 | 8.58 | |
| Marital status | Unmarried | 799 | 38.08 |
| Married | 1299 | 61.92 | |
| Per capita monthly household income (yuan) | <2999 | 154 | 7.34 |
| 3000–4999 | 370 | 17.64 | |
| 5000–9999 | 678 | 32.32 | |
| 10,000–14,999 | 407 | 19.40 | |
| ≥15,000 | 489 | 23.31 | |
| Previous COVID-19 vaccination behavior | Not vaccinated | 1238 | 59.01 |
| Vaccinated | 860 | 40.99 |
| Characteristics | ATT | SNs | PBC | Intention |
|---|---|---|---|---|
| Gender | ||||
| Male | 4.40 ± 0.44 | 4.09 ± 0.57 | 3.70 ± 0.73 | 4.52 ± 0.54 |
| Female | 4.40 ± 0.38 | 4.02 ± 0.59 | 3.62 ± 0.74 | 4.45 ± 0.59 |
| t | 0.004 | 2.814 | 2.477 | 2.739 |
| p | 0.997 | 0.005 | 0.013 | 0.006 |
| Age groups | ||||
| 18–29 | 4.38 ± 0.39 | 4.02 ± 0.57 | 3.58 ± 0.74 | 4.51 ± 0.52 |
| 30–39 | 4.40 ± 0.42 | 4.10 ± 0.56 | 3.73 ± 0.71 | 4.47 ± 0.56 |
| 40–49 | 4.43 ± 0.46 | 4.05 ± 0.69 | 3.79 ± 0.74 | 4.46 ± 0.68 |
| ≥50 | 4.45 ± 0.42 | 4.00 ± 0.59 | 3.61 ± 0.68 | 4.37 ± 0.72 |
| F | 1.524 | 2.780 | 9.376 | 1.728 |
| p | 0.206 | 0.041 | <0.001 | 0.161 |
| Education levels | ||||
| High School | 4.38 ± 0.46 | 3.97 ± 0.68 | 3.59 ± 0.79 | 4.39 ± 0.63 |
| University | 4.40 ± 0.41 | 4.06 ± 0.57 | 3.67 ± 0.73 | 4.48 ± 0.57 |
| Postgraduate | 4.43 ± 0.37 | 4.07 ± 0.51 | 3.71 ± 0.71 | 4.58 ± 0.44 |
| F | 0.679 | 1.592 | 1.350 | 5.531 |
| p | 0.507 | 0.205 | 0.259 | 0.004 |
| Marital status | ||||
| Unmarried | 4.35 ± 0.41 | 3.98 ± 0.60 | 3.52 ± 0.75 | 4.48 ± 0.59 |
| Married | 4.42 ± 0.41 | 4.10 ± 0.56 | 3.75 ± 0.71 | 4.49 ± 0.54 |
| t | −3.745 | −4.629 | −7.103 | −0.536 |
| p | <0.001 | <0.001 | <0.001 | 0.592 |
| Per capita monthly household income (yuan) | ||||
| <2999 | 4.34 ± 0.38 | 4.01 ± 0.54 | 3.53 ± 0.71 | 4.53 ± 0.51 |
| 3000–4999 | 4.40 ± 0.43 | 4.05 ± 0.58 | 3.60 ± 0.76 | 4.46 ± 0.58 |
| 5000–9999 | 4.39 ± 0.39 | 4.07 ± 0.56 | 3.64 ± 0.73 | 4.48 ± 0.57 |
| 10,000–14,999 | 4.40 ± 0.40 | 4.05 ± 0.61 | 3.73 ± 0.72 | 4.47 ± 0.58 |
| ≥15,000 | 4.42 ± 0.44 | 4.07 ± 0.58 | 3.73 ± 0.72 | 4.51 ± 0.54 |
| F | 1.218 | 0.419 | 4.174 | 0.654 |
| P | 0.301 | 0.795 | 0.002 | 0.624 |
| Previous COVID-19 vaccination behavior | ||||
| Not vaccinated | 4.36 ± 0.43 | 3.95 ± 0.62 | 3.51 ± 0.74 | 4.39 ± 0.62 |
| Vaccinated | 4.45 ± 0.38 | 4.21 ± 0.48 | 3.89 ± 0.65 | 4.62 ± 0.44 |
| t | −5.037 | −10.669 | −12.453 | −9.829 |
| p | 0.000 | <0.001 | <0.001 | <0.001 |
| Variable | Modeling 1 | Modeling 2 | Modeling 3 | |||
|---|---|---|---|---|---|---|
| B | β | B | β | B | β | |
| Constant | 4.441 ** | 4.074 ** | 1.300 ** | |||
| Gender | −0.074 * | −0.066 * | −0.074 * | −0.066 * | −0.044 * | −0.039 * |
| Educational level | 0.086 * | 0.063 * | 0.030 | 0.022 | 0.033 | 0.025 |
| Age group | −0.061 * | −0.085 * | −0.068 ** | −0.095 ** | −0.048 * | −0.067 * |
| Marital status | 0.071 * | 0.062 * | 0.052 | 0.045 | −0.038 | −0.033 |
| Per capita monthly household income | −0.008 | −0.018 | −0.011 | −0.024 | −0.005 | −0.011 |
| Vaccine knowledge | 0.039 ** | 0.112 ** | 0.01 7 * | 0.049 * | ||
| Previous COVID-19 vaccination behavior | 0.204 ** | 0.178 ** | 0.059 * | 0.052 * | ||
| ATT | 0.265 ** | 0.194 ** | ||||
| SN | 0.411 ** | 0.423 ** | ||||
| PBC | 0.079 ** | 0.103 ** | ||||
| ΔR2 | 0.013 | 0.048 | 0.345 | |||
| R2 | 0.013 | 0.061 | 0.399 | |||
| adjusted R2 | 0.011 | 0.058 | 0.397 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Z.; Li, Z.; Sun, X. Exploration into the Influencing Factors for the Intention of the Public to Vaccinate against Infectious Diseases Based on the Theory of Planned Behavior—Example of the COVID-19 Vaccine. Vaccines 2023, 11, 1092. https://doi.org/10.3390/vaccines11061092
Li Z, Li Z, Sun X. Exploration into the Influencing Factors for the Intention of the Public to Vaccinate against Infectious Diseases Based on the Theory of Planned Behavior—Example of the COVID-19 Vaccine. Vaccines. 2023; 11(6):1092. https://doi.org/10.3390/vaccines11061092
Chicago/Turabian StyleLi, Zeming, Zihan Li, and Xinying Sun. 2023. "Exploration into the Influencing Factors for the Intention of the Public to Vaccinate against Infectious Diseases Based on the Theory of Planned Behavior—Example of the COVID-19 Vaccine" Vaccines 11, no. 6: 1092. https://doi.org/10.3390/vaccines11061092
APA StyleLi, Z., Li, Z., & Sun, X. (2023). Exploration into the Influencing Factors for the Intention of the Public to Vaccinate against Infectious Diseases Based on the Theory of Planned Behavior—Example of the COVID-19 Vaccine. Vaccines, 11(6), 1092. https://doi.org/10.3390/vaccines11061092







