DNA Vaccines Encoding HTNV GP-Derived Th Epitopes Benefited from a LAMP-Targeting Strategy and Established Cellular Immunoprotection
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Viruses, Bacteria, Cells, the Inactivated Vaccine, and Peptides
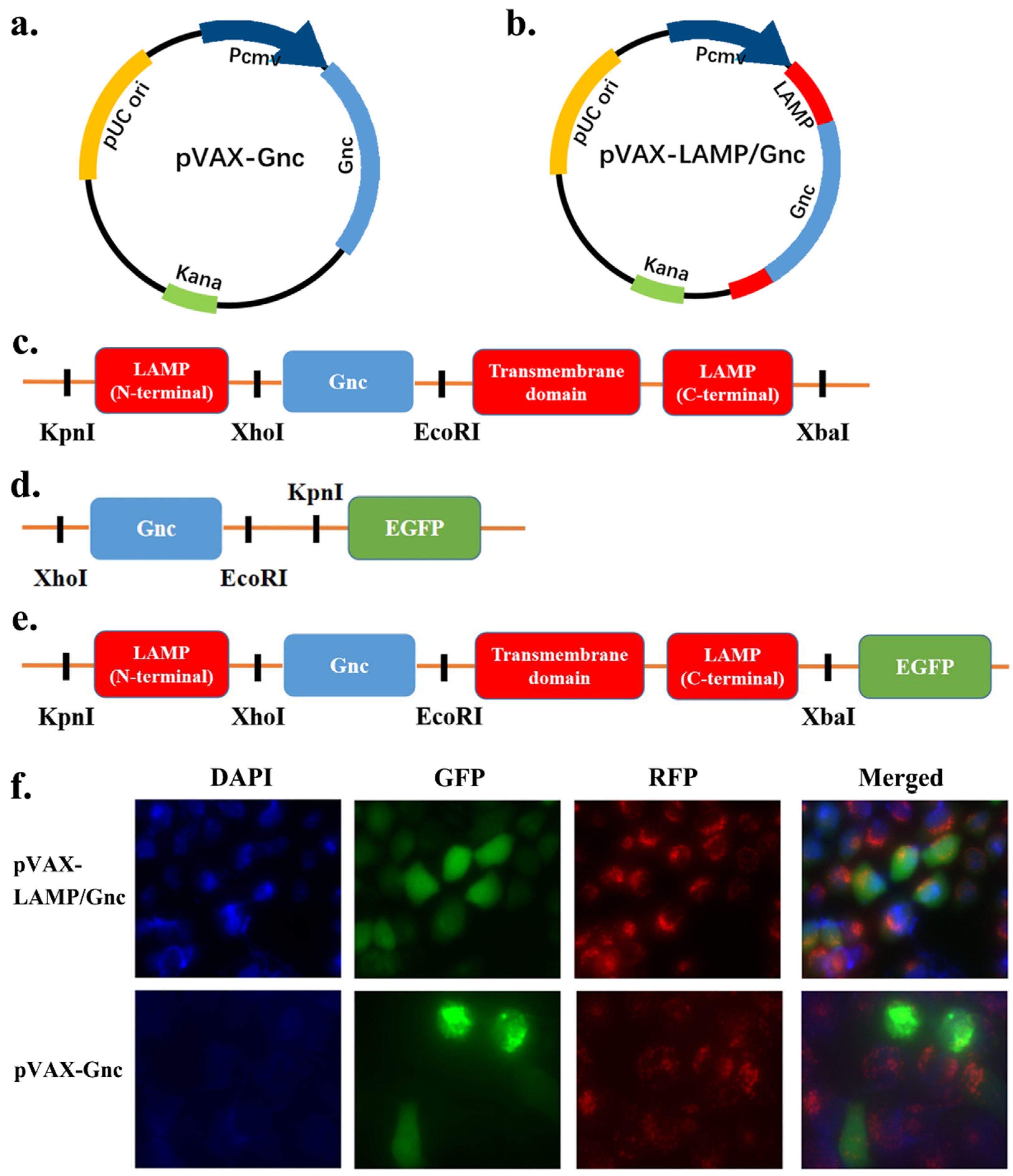
2.3. Construction of Recombinant DNA Vaccines
2.4. Expression Identification of DNA Vaccines
2.5. Physicochemical Property Analysis of DNA Vaccines
2.6. Animals and Immunization
2.7. Serum Neutralization Test
2.8. Enzyme-Linked Immunospot Assay (ELISpot)
2.9. Viral Challenge of Mice
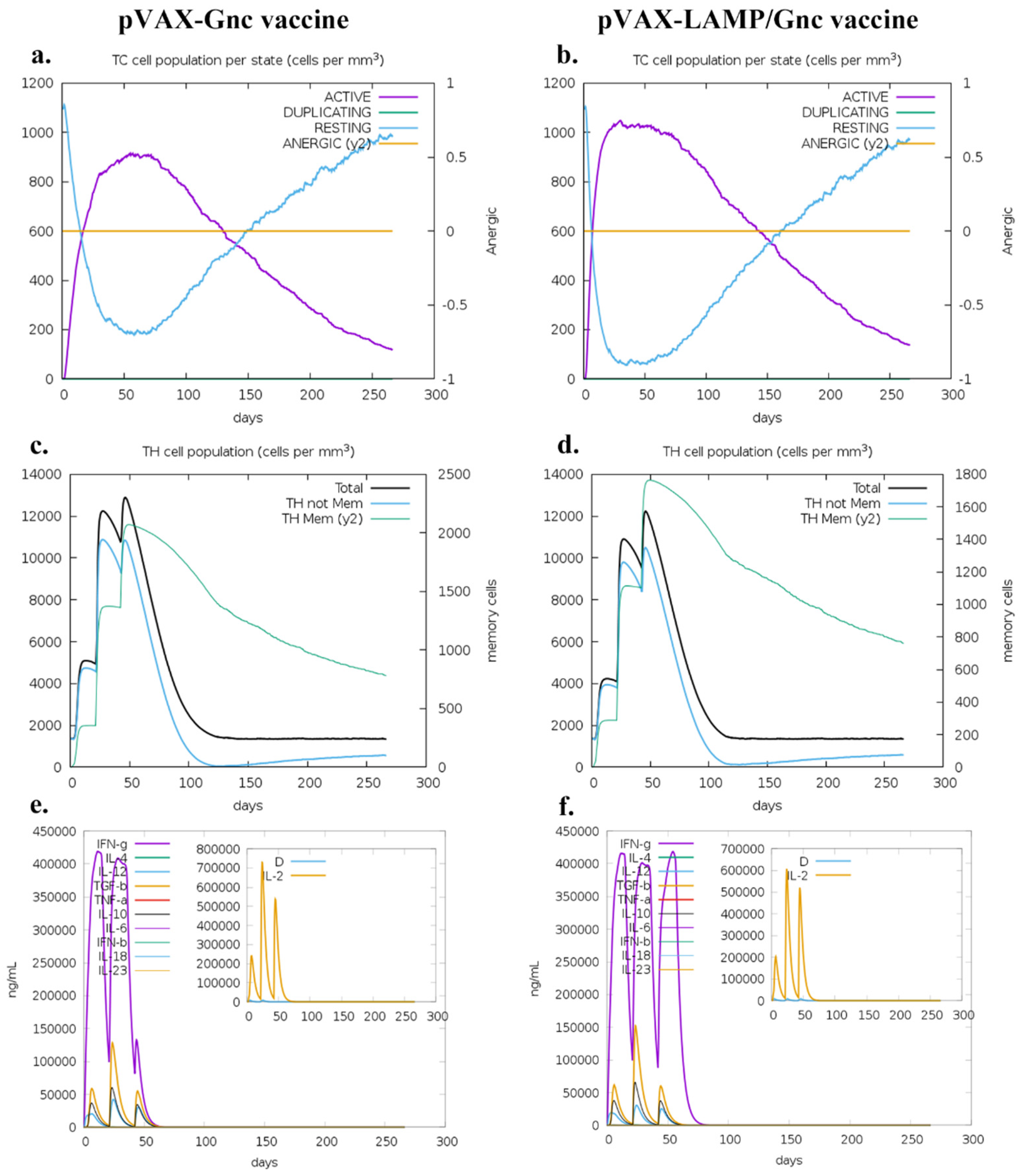
2.10. Immune Simulation after Three Doses of Vaccines
2.11. Hematoxylin and Eosin (H&E) Staining
3. Results
3.1. Rationale Design, Physicochemical Properties, and Structures of the Antigen Gnc
3.2. Synthesis and Expression of Recombinant DNA Plasmids
3.3. Protective Efficacy of Tandem Epitope Vaccines against HTNV Infection in BALB/c Mice
3.4. LAMP Targeting Enhances the Cellular Response to Gnc-Encoding DNA Vaccines with Incompetent Neutralization
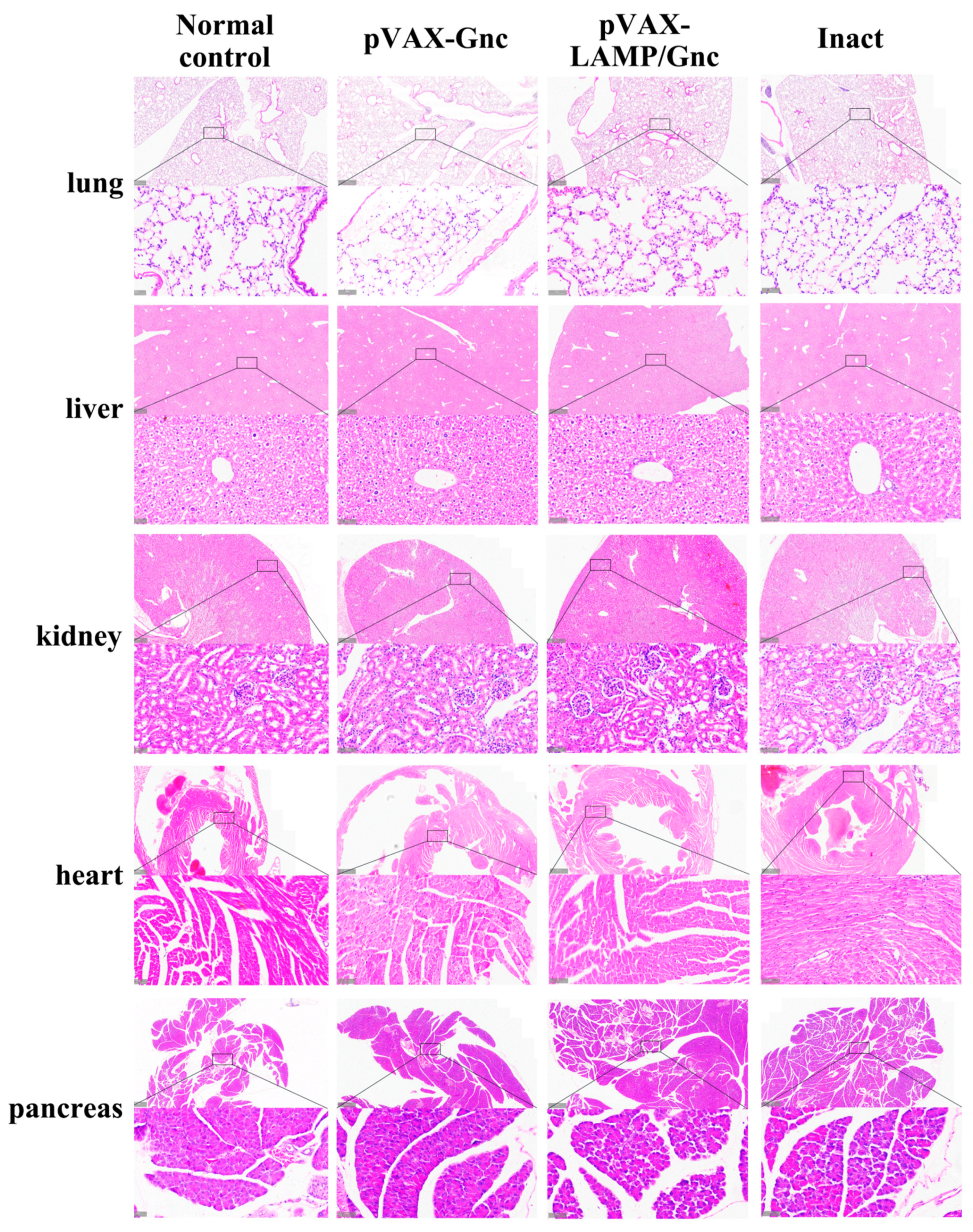
3.5. Determination of the Preliminary Safety of Candidate DNA Vaccines Encoding Gnc Using Histopathological Analysis
3.6. LAMP1 Strategy Enhanced the Immune Response of T-Cells in the Population
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vaheri, A.; Henttonen, H.; Mustonen, J. Hantavirus Research in Finland: Highlights and Perspectives. Viruses 2021, 13, 1452. [Google Scholar] [CrossRef]
- Koehler, F.C.; Blomberg, L.; Brehm, T.T.; Büttner, S.; Cornely, O.A.; Degen, O.; Di Cristanziano, V.; Dolff, S.; Eberwein, L.; Hoxha, E.; et al. Development and design of the Hantavirus registry—HantaReg—For epidemiological studies, outbreaks and clinical studies on hantavirus disease. Clin. Kidney J. 2021, 14, 2365–2370. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Mao, Z.; Yang, J.; Liu, S.; Liu, Y.; Qin, S.; Tian, H.; Guo, S.; Ren, J.; Shi, X.; et al. The changing epidemiology of hemorrhagic fever with renal syndrome in Southeastern China during 1963–2020: A retrospective analysis of surveillance data. PLoS Neglected Trop. Dis. 2021, 15, e0009673. [Google Scholar] [CrossRef]
- Toledo, J.; Haby, M.M.; Reveiz, L.; Sosa Leon, L.; Angerami, R.; Aldighieri, S. Evidence for Human-to-Human Transmission of Hantavirus: A Systematic Review. J. Infect. Dis. 2022, 226, 1362–1371. [Google Scholar] [CrossRef]
- Welke, R.W.; Sperber, H.S.; Bergmann, R.; Koikkarah, A.; Menke, L.; Sieben, C.; Krüger, D.H.; Chiantia, S.; Herrmann, A.; Schwarzer, R. Characterization of Hantavirus N Protein Intracellular Dynamics and Localization. Viruses 2022, 14, 457. [Google Scholar] [CrossRef]
- Guardado-Calvo, P.; Rey, F.A. The surface glycoproteins of hantaviruses. Curr. Opin. Virol. 2021, 50, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Serris, A.; Stass, R.; Bignon, E.A.; Muena, N.A.; Manuguerra, J.C.; Jangra, R.K.; Li, S.; Chandran, K.; Tischler, N.D.; Huiskonen, J.T.; et al. The Hantavirus Surface Glycoprotein Lattice and Its Fusion Control Mechanism. Cell 2020, 183, 442–456.e416. [Google Scholar] [CrossRef]
- Obando-Rico, C.J.; Valencia-Grajales, Y.F.; Bonilla-Aldana, D.K. Prevalence of orthohantavirus in rodents: A systematic review and meta-analysis. Travel Med. Infect. Dis. 2023, 51, 102504. [Google Scholar] [CrossRef] [PubMed]
- Pereira, P.D.C.; Diniz, D.G.; da Costa, E.R.; Magalhães, N.G.M.; da Silva, A.J.F.; Leite, J.G.S.; Almeida, N.I.P.; Cunha, K.N.; de Melo, M.A.D.; Vasconcelos, P.; et al. Genes, inflammatory response, tolerance, and resistance to virus infections in migratory birds, bats, and rodents. Front. Immunol. 2023, 14, 1239572. [Google Scholar] [CrossRef]
- Lv, C.L.; Tian, Y.; Qiu, Y.; Xu, Q.; Chen, J.J.; Jiang, B.G.; Li, Z.J.; Wang, L.P.; Hay, S.I.; Liu, W.; et al. Dual seasonal pattern for hemorrhagic fever with renal syndrome and its potential determinants in China. Sci. Total Environ. 2023, 859, 160339. [Google Scholar] [CrossRef]
- Luo, Y.; Lv, H.; Yan, H.; Zhu, C.; Ai, L.; Li, W.; Yi, J.; Zhang, L.; Tan, W. Meteorological change and hemorrhagic fever with renal syndrome epidemic in China, 2004–2018. Sci. Rep. 2022, 12, 20037. [Google Scholar] [CrossRef]
- Singh, S.; Numan, A.; Sharma, D.; Shukla, R.; Alexander, A.; Jain, G.K.; Ahmad, F.J.; Kesharwani, P. Epidemiology, virology and clinical aspects of hantavirus infections: An overview. Int. J. Environ. Health Res. 2022, 32, 1815–1826. [Google Scholar] [CrossRef] [PubMed]
- Tariq, M.; Kim, D.M. Hemorrhagic Fever with Renal Syndrome: Literature Review, Epidemiology, Clinical Picture and Pathogenesis. Infect. Chemother. 2022, 54, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Koehler, F.C.; Di Cristanziano, V.; Späth, M.R.; Hoyer-Allo, K.J.R.; Wanken, M.; Müller, R.U.; Burst, V. The kidney in hantavirus infection-epidemiology, virology, pathophysiology, clinical presentation, diagnosis and management. Clin. Kidney J. 2022, 15, 1231–1252. [Google Scholar] [CrossRef]
- Mir, S. Hantavirus Induced Kidney Disease. Front. Med. 2021, 8, 795340. [Google Scholar] [CrossRef]
- Liu, R.; Lv, Y.; Sun, W.; Li, M.; Ge, N.; Zhu, C.; Ding, Y.; Liu, Z.; Ma, R.; Huang, Y.; et al. Investigation of a subunit protein vaccine for HFRS based on a consensus sequence between envelope glycoproteins of HTNV and SEOV. Virus Res. 2023, 334, 199149. [Google Scholar] [CrossRef]
- Dzagurova, T.K.; Siniugina, A.A.; Ishmukhametov, A.A.; Egorova, M.S.; Kurashova, S.S.; Balovneva, M.V.; Deviatkin, A.A.; Tkachenko, P.E.; Leonovich, O.A.; Tkachenko, E.A. Pre-Clinical Studies of Inactivated Polyvalent HFRS Vaccine. Front. Cell. Infect. Microbiol. 2020, 10, 545372. [Google Scholar] [CrossRef]
- Engdahl, T.B.; Binshtein, E.; Brocato, R.L.; Kuzmina, N.A.; Principe, L.M.; Kwilas, S.A.; Kim, R.K.; Chapman, N.S.; Porter, M.S.; Guardado-Calvo, P.; et al. Antigenic mapping and functional characterization of human New World hantavirus neutralizing antibodies. eLife 2023, 12, e81743. [Google Scholar] [CrossRef]
- Hooper, J.W.; Brocato, R.L.; Kwilas, S.A.; Hammerbeck, C.D.; Josleyn, M.D.; Royals, M.; Ballantyne, J.; Wu, H.; Jiao, J.A.; Matsushita, H.; et al. DNA vaccine-derived human IgG produced in transchromosomal bovines protect in lethal models of hantavirus pulmonary syndrome. Sci. Transl. Med. 2014, 6, 264ra162. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Yuan, B.; Zhuang, R.; Zhang, Y.; Liu, B.; Zhang, C.; Zhang, Y.; Yu, H.; Yi, J.; Yang, A.; et al. Hantaan virus infection induces both Th1 and ThGranzyme B+ cell immune responses that associated with viral control and clinical outcome in humans. PLoS Pathog. 2015, 11, e1004788. [Google Scholar] [CrossRef] [PubMed]
- Jiang, D.B.; Zhang, J.P.; Cheng, L.F.; Zhang, G.W.; Li, Y.; Li, Z.C.; Lu, Z.H.; Zhang, Z.X.; Lu, Y.C.; Zheng, L.H.; et al. Hantavirus Gc induces long-term immune protection via LAMP-targeting DNA vaccine strategy. Antivir. Res. 2018, 150, 174–182. [Google Scholar] [CrossRef]
- Jiang, D.B.; Sun, L.J.; Cheng, L.F.; Zhang, J.P.; Xiao, S.B.; Sun, Y.J.; Yang, S.Y.; Wang, J.; Zhang, F.L.; Yang, K. Recombinant DNA vaccine of Hantavirus Gn and LAMP1 induced long-term immune protection in mice. Antivir. Res. 2017, 138, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Jiang, D.B.; Sun, Y.J.; Cheng, L.F.; Zhang, G.F.; Dong, C.; Jin, B.Q.; Song, C.J.; Ma, Y.; Zhang, F.L.; Yang, K. Construction and evaluation of DNA vaccine encoding Hantavirus glycoprotein N-terminal fused with lysosome-associated membrane protein. Vaccine 2015, 33, 3367–3376. [Google Scholar] [CrossRef]
- Shafqat, A.; Omer, M.H.; Ahmad, O.; Niaz, M.; Abdulkader, H.S.; Shafqat, S.; Mushtaq, A.H.; Shaik, A.; Elshaer, A.N.; Kashir, J.; et al. SARS-CoV-2 epitopes inform future vaccination strategies. Front. Immunol. 2022, 13, 1041185. [Google Scholar] [CrossRef] [PubMed]
- Ismail, S.; Abbasi, S.W.; Yousaf, M.; Ahmad, S.; Muhammad, K.; Waheed, Y. Design of a Multi-Epitopes Vaccine against Hantaviruses: An Immunoinformatics and Molecular Modelling Approach. Vaccines 2022, 10, 378. [Google Scholar] [CrossRef]
- Chikhlikar, P.; Barros de Arruda, L.; Maciel, M.; Silvera, P.; Lewis, M.G.; August, J.T.; Marques, E.T. DNA encoding an HIV-1 Gag/human lysosome-associated membrane protein-1 chimera elicits a broad cellular and humoral immune response in Rhesus macaques. PLoS ONE 2006, 1, e135. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.R.; Heo, L.; Seok, C. Effective protein model structure refinement by loop modeling and overall relaxation. Proteins 2016, 84 (Suppl. 1), 293–301. [Google Scholar] [CrossRef] [PubMed]
- Zaharieva, N.; Dimitrov, I.; Flower, D.R.; Doytchinova, I. VaxiJen Dataset of Bacterial Immunogens: An Update. Curr. Comput. -Aided Drug Des. 2019, 15, 398–400. [Google Scholar] [CrossRef]
- Kyte, J.; Doolittle, R.F. A simple method for displaying the hydropathic character of a protein. J. Mol. Biol. 1982, 157, 105–132. [Google Scholar] [CrossRef]
- Stolfi, P.; Castiglione, F.; Mastrostefano, E.; Di Biase, I.; Di Biase, S.; Palmieri, G.; Prisco, A. In-silico evaluation of adenoviral COVID-19 vaccination protocols: Assessment of immunological memory up to 6 months after the third dose. Front. Immunol. 2022, 13, 998262. [Google Scholar] [CrossRef]
- Ragone, C.; Manolio, C.; Cavalluzzo, B.; Mauriello, A.; Tornesello, M.L.; Buonaguro, F.M.; Castiglione, F.; Vitagliano, L.; Iaccarino, E.; Ruvo, M.; et al. Identification and validation of viral antigens sharing sequence and structural homology with tumor-associated antigens (TAAs). J. Immunother. Cancer 2021, 9, e002694. [Google Scholar] [CrossRef]
- Rapin, N.; Lund, O.; Bernaschi, M.; Castiglione, F. Computational immunology meets bioinformatics: The use of prediction tools for molecular binding in the simulation of the immune system. PLoS ONE 2010, 5, e9862. [Google Scholar] [CrossRef]
- Cheng, P.; Xue, Y.; Wang, J.; Jia, Z.; Wang, L.; Gong, W. Evaluation of the consistence between the results of immunoinformatics predictions and real-world animal experiments of a new tuberculosis vaccine MP3RT. Front. Cell. Infect. Microbiol. 2022, 12, 1047306. [Google Scholar] [CrossRef] [PubMed]
- Singhal, J.; Madan, E.; Chaurasiya, A.; Srivastava, P.; Singh, N.; Kaushik, S.; Kahlon, A.K.; Maurya, M.K.; Marothia, M.; Joshi, P.; et al. Host SUMOylation Pathway Negatively Regulates Protective Immune Responses and Promotes Leishmania donovani Survival. Front. Cell. Infect. Microbiol. 2022, 12, 878136. [Google Scholar] [CrossRef]
- Naveed, M.; Yaseen, A.R.; Khalid, H.; Ali, U.; Rabaan, A.A.; Garout, M.; Halwani, M.A.; Al Mutair, A.; Alhumaid, S.; Al Alawi, Z.; et al. Execution and Design of an Anti HPIV-1 Vaccine with Multiple Epitopes Triggering Innate and Adaptive Immune Responses: An Immunoinformatic Approach. Vaccines 2022, 10, 869. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, M.R.; Gasteiger, E.; Bairoch, A.; Sanchez, J.C.; Williams, K.L.; Appel, R.D.; Hochstrasser, D.F. Protein identification and analysis tools in the ExPASy server. Methods Mol. Biol. (Clifton N.J.) 1999, 112, 531–552. [Google Scholar] [CrossRef]
- Tahir Ul Qamar, M.; Ismail, S.; Ahmad, S.; Mirza, M.U.; Abbasi, S.W.; Ashfaq, U.A.; Chen, L.L. Development of a Novel Multi-Epitope Vaccine Against Crimean-Congo Hemorrhagic Fever Virus: An Integrated Reverse Vaccinology, Vaccine Informatics and Biophysics Approach. Front. Immunol. 2021, 12, 669812. [Google Scholar] [CrossRef]
- Buchan, D.W.A.; Jones, D.T. The PSIPRED Protein Analysis Workbench: 20 years on. Nucleic Acids Res. 2019, 47, W402–W407. [Google Scholar] [CrossRef] [PubMed]
- Buchan, D.W.; Minneci, F.; Nugent, T.C.; Bryson, K.; Jones, D.T. Scalable web services for the PSIPRED Protein Analysis Workbench. Nucleic Acids Res. 2013, 41, W349–W357. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Yan, R.; Roy, A.; Xu, D.; Poisson, J.; Zhang, Y. The I-TASSER Suite: Protein structure and function prediction. Nat. Methods 2015, 12, 7–8. [Google Scholar] [CrossRef]
- Roy, A.; Kucukural, A.; Zhang, Y. I-TASSER: A unified platform for automated protein structure and function prediction. Nat. Protoc. 2010, 5, 725–738. [Google Scholar] [CrossRef]
- Heo, L.; Park, H.; Seok, C. GalaxyRefine: Protein structure refinement driven by side-chain repacking. Nucleic Acids Res. 2013, 41, W384–W388. [Google Scholar] [CrossRef]
- Kopp, J.; Bordoli, L.; Battey, J.N.; Kiefer, F.; Schwede, T. Assessment of CASP7 predictions for template-based modeling targets. Proteins 2007, 69 (Suppl. 8), 38–56. [Google Scholar] [CrossRef] [PubMed]
- Kryshtafovych, A.; Monastyrskyy, B.; Fidelis, K. CASP prediction center infrastructure and evaluation measures in CASP10 and CASP ROLL. Proteins 2014, 82 (Suppl. 2), 7–13. [Google Scholar] [CrossRef]
- Chen, V.B.; Arendall, W.B., 3rd; Headd, J.J.; Keedy, D.A.; Immormino, R.M.; Kapral, G.J.; Murray, L.W.; Richardson, J.S.; Richardson, D.C. MolProbity: All-atom structure validation for macromolecular crystallography. Acta Crystallographica. Sect. D Biol. Crystallogr. 2010, 66, 12–21. [Google Scholar] [CrossRef]
- Doytchinova, I.A.; Flower, D.R. VaxiJen: A server for prediction of protective antigens, tumour antigens and subunit vaccines. BMC Bioinform. 2007, 8, 4. [Google Scholar] [CrossRef] [PubMed]
- Kanekiyo, M.; Gillespie, R.A.; Midgett, M.; O’Malley, K.J.; Williams, C.; Moin, S.M.; Wallace, M.; Treaster, L.; Cooper, K.; Syeda, H.; et al. Refined semi-lethal aerosol H5N1 influenza model in cynomolgus macaques for evaluation of medical countermeasures. iScience 2023, 26, 107830. [Google Scholar] [CrossRef]
- Umukoro, E.; Alukal, J.J.; Pak, K.; Gutierrez, J. State of the Art: Test all for Anti-Hepatitis D Virus and Reflex to Hepatitis D Virus RNA Polymerase Chain Reaction Quantification. Clin. Liver Dis. 2023, 27, 937–954. [Google Scholar] [CrossRef] [PubMed]
- Hormazábal, J.; Nuñez-Franz, L.; Rubilar, P.; Apablaza, M.; Vial, C.; Cortés, L.J.; González, N.; Vial, P.; Said, M.; González, C.; et al. Factors influencing neutralizing antibody response to the original SARS-CoV-2 virus and the Omicron variant in a high vaccination coverage country, a population-based study. Vaccine 2023, 15, 100372. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.; Zhang, J.; Zhang, J.; Wang, Y.; Sun, Y.; Wang, Y.; Wang, Y.; Yang, D.; Qiao, X.; Liu, X.; et al. A Comprehensive Investigation of Glycoprotein-Based Nucleic Acid Vaccines for Hantaan Virus. NPJ Vaccines, 2024; in press. [Google Scholar] [CrossRef]
- Chakma, C.R.; Good-Jacobson, K.L. Requirements of IL-4 during the Generation of B Cell Memory. J. Immunol. 2023, 210, 1853–1860. [Google Scholar] [CrossRef]
- Malonis, R.J.; Lai, J.R.; Vergnolle, O. Peptide-Based Vaccines: Current Progress and Future Challenges. Chem. Rev. 2020, 120, 3210–3229. [Google Scholar] [CrossRef]
- Frei, J.C.; Wirchnianski, A.S.; Govero, J.; Vergnolle, O.; Dowd, K.A.; Pierson, T.C.; Kielian, M.; Girvin, M.E.; Diamond, M.S.; Lai, J.R. Engineered Dengue Virus Domain III Proteins Elicit Cross-Neutralizing Antibody Responses in Mice. J. Virol. 2018, 92, 10–1128. [Google Scholar] [CrossRef]
- Burton, D.R.; Poignard, P.; Stanfield, R.L.; Wilson, I.A. Broadly neutralizing antibodies present new prospects to counter highly antigenically diverse viruses. Science 2012, 337, 183–186. [Google Scholar] [CrossRef]
- Kwong, P.D.; Wilson, I.A. HIV-1 and influenza antibodies: Seeing antigens in new ways. Nat. Immunol. 2009, 10, 573–578. [Google Scholar] [CrossRef] [PubMed]
- Sun, B.; Zhang, J.; Wang, J.; Liu, Y.; Sun, H.; Lu, Z.; Chen, L.; Ding, X.; Pan, J.; Hu, C.; et al. Comparative Immunoreactivity Analyses of Hantaan Virus Glycoprotein-Derived MHC-I Epitopes in Vaccination. Vaccines 2022, 10, 564. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Lu, Z.; Xuan, G.; Liu, N.; Wang, T.; Liu, Y.; Lan, M.; Xu, J.; Feng, Y.; Xu, S.; et al. Integrative Analysis of HTNV Glycoprotein Derived MHC II Epitopes by In Silico Prediction and Experimental Validation. Front. Cell. Infect. Microbiol. 2021, 11, 671694. [Google Scholar] [CrossRef]
- Jiang, C.; Li, J.; Zhang, W.; Zhuang, Z.; Liu, G.; Hong, W.; Li, B.; Zhang, X.; Chao, C.C. Potential association factors for developing effective peptide-based cancer vaccines. Front. Immunol. 2022, 13, 931612. [Google Scholar] [CrossRef]
- Cervantes-Torres, J.; Rosales-Mendoza, S.; Cabello, C.; Montero, L.; Hernandez-Aceves, J.; Granados, G.; Calderón-Gallegos, A.; Zúñiga-Flores, F.; Ruiz-Rivera, M.; Abarca-Magaña, J.C.; et al. Towards the development of an epitope-focused vaccine for SARS-CoV-2. Vaccine 2022, 40, 6489–6498. [Google Scholar] [CrossRef] [PubMed]
- Sabatino, D. Medicinal Chemistry and Methodological Advances in the Development of Peptide-Based Vaccines. J. Med. Chem. 2020, 63, 14184–14196. [Google Scholar] [CrossRef]
- Shalash, A.O.; Toth, I.; Skwarczynski, M. The potential of developing a protective peptide-based vaccines against SARS-CoV-2. Drug Dev. Res. 2022, 83, 1251–1256. [Google Scholar] [CrossRef]
- Zagorski, K.; Pandey, K.; Rajaiah, R.; Olwenyi, O.A.; Bade, A.N.; Acharya, A.; Johnston, M.; Filliaux, S.; Lyubchenko, Y.L.; Byrareddy, S.N. Modular nanoarray vaccine for SARS-CoV-2. Nanomed. Nanotechnol. Biol. Med. 2022, 46, 102604. [Google Scholar] [CrossRef]
- Bahrami, A.A.; Payandeh, Z.; Khalili, S.; Zakeri, A.; Bandehpour, M. Immunoinformatics: In Silico Approaches and Computational Design of a Multi-epitope, Immunogenic Protein. Int. Rev. Immunol. 2019, 38, 307–322. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Liang, S.; Zhang, S.; Zhang, S.; Yu, Y.; Yao, H.; Liu, Y.; Zhang, W.; Liu, G. Development and evaluation of a multi-epitope subunit vaccine against group B Streptococcus infection. Emerg. Microbes Infect. 2022, 11, 2371–2382. [Google Scholar] [CrossRef] [PubMed]
- Bezu, L.; Kepp, O.; Cerrato, G.; Pol, J.; Fucikova, J.; Spisek, R.; Zitvogel, L.; Kroemer, G.; Galluzzi, L. Trial watch: Peptide-based vaccines in anticancer therapy. Oncoimmunology 2018, 7, e1511506. [Google Scholar] [CrossRef]
- Tang, M.; Cai, J.H.; Diao, H.Y.; Guo, W.M.; Yang, X.; Xing, S. The progress of peptide vaccine clinical trials in gynecologic oncology. Hum. Vaccines Immunother. 2022, 18, 2062982. [Google Scholar] [CrossRef]
- Su, Y.; Connolly, M.; Marketon, A.; Heiland, T. CryJ-LAMP DNA Vaccines for Japanese Red Cedar Allergy Induce Robust Th1-Type Immune Responses in Murine Model. J. Immunol. Res. 2016, 2016, 4857869. [Google Scholar] [CrossRef]
- Lenogue, K.; Walencik, A.; Laulagnier, K.; Molens, J.P.; Benlalam, H.; Dreno, B.; Coulie, P.; Pule, M.; Chaperot, L.; Plumas, J. Engineering a Human Plasmacytoid Dendritic Cell-Based Vaccine to Prime and Expand Multispecific Viral and Tumor Antigen-Specific T-Cells. Vaccines 2021, 9, 141. [Google Scholar] [CrossRef] [PubMed]
- Rigato, P.O.; Maciel, M., Jr.; Goldoni, A.L.; Piubelli, O.G.; Orii, N.M.; Marques, E.T.; August, J.T.; Duarte, A.J.; Sato, M.N. Maternal LAMP/p55gagHIV-1 DNA immunization induces in utero priming and a long-lasting immune response in vaccinated neonates. PLoS ONE 2012, 7, e31608. [Google Scholar] [CrossRef]
- Kravtsov, D.S.; Erbe, A.K.; Sondel, P.M.; Rakhmilevich, A.L. Roles of CD4+ T cells as mediators of antitumor immunity. Front. Immunol. 2022, 13, 972021. [Google Scholar] [CrossRef]
- Lopez, J.; Anna, F.; Authié, P.; Pawlik, A.; Ku, M.W.; Blanc, C.; Souque, P.; Moncoq, F.; Noirat, A.; Hardy, D.; et al. A lentiviral vector encoding fusion of light invariant chain and mycobacterial antigens induces protective CD4(+) T cell immunity. Cell Rep. 2022, 40, 111142. [Google Scholar] [CrossRef]
- Sandalova, T.; Sala, B.M.; Achour, A. Structural aspects of chemical modifications in the MHC-restricted immunopeptidome; Implications for immune recognition. Front. Chem. 2022, 10, 861609. [Google Scholar] [CrossRef]
- Van Laethem, F.; Bhattacharya, A.; Craveiro, M.; Lu, J.; Sun, P.D.; Singer, A. MHC-independent αβT cells: Lessons learned about thymic selection and MHC-restriction. Front. Immunol. 2022, 13, 953160. [Google Scholar] [CrossRef] [PubMed]
- Araújo, L.P.; Dias, M.E.C.; Scodeler, G.C.; Santos, A.S.; Soares, L.M.; Corsetti, P.P.; Padovan, A.C.B.; Silveira, N.J.F.; de Almeida, L.A. Epitope identification of SARS-CoV-2 structural proteins using in silico approaches to obtain a conserved rational immunogenic peptide. Immunoinformatics 2022, 7, 100015. [Google Scholar] [CrossRef]
- Li, L.; Honda-Okubo, Y.; Petrovsky, N. Flavivirus DNA Vaccine Design and Adjuvant Selection. Methods Mol. Biol. (Clifton N.J.) 2021, 2183, 405–422. [Google Scholar] [CrossRef]
- Li, L.; Petrovsky, N. Molecular mechanisms for enhanced DNA vaccine immunogenicity. Expert Rev. Vaccines 2016, 15, 313–329. [Google Scholar] [CrossRef] [PubMed]
- Shantier, S.W.; Mustafa, M.I.; Abdelmoneim, A.H.; Fadl, H.A.; Elbager, S.G.; Makhawi, A.M. Novel multi epitope-based vaccine against monkeypox virus: Vaccinomic approach. Sci. Rep. 2022, 12, 15983. [Google Scholar] [CrossRef] [PubMed]
- Aiman, S.; Alhamhoom, Y.; Ali, F.; Rahman, N.; Rastrelli, L.; Khan, A.; Farooq, Q.U.A.; Ahmed, A.; Khan, A.; Li, C. Multi-epitope chimeric vaccine design against emerging Monkeypox virus via reverse vaccinology techniques- a bioinformatics and immunoinformatics approach. Front. Immunol. 2022, 13, 985450. [Google Scholar] [CrossRef]
- Parmar, M.; Thumar, R.; Sheth, J.; Patel, D. Designing multi-epitope based peptide vaccine targeting spike protein SARS-CoV-2 B1.1.529 (Omicron) variant using computational approaches. Struct. Chem. 2022, 33, 2243–2260. [Google Scholar] [CrossRef]
- Jiang, S.; Wu, S.; Zhao, G.; He, Y.; Guo, X.; Zhang, Z.; Hou, J.; Ding, Y.; Cheng, A.; Wang, B. Identification of a promiscuous conserved CTL epitope within the SARS-CoV-2 spike protein. Emerg. Microbes Infect. 2022, 11, 730–740. [Google Scholar] [CrossRef] [PubMed]



| Model | GDT-HA | RMSD | MolProbity | Clash Score | Poor Rotamers | Rama Favored |
|---|---|---|---|---|---|---|
| Model 1 | 1 | 0 | 3.611 | 20.1 | 17.7 | 67.2 |
| Refined 1 | 0.8981 | 0.525 | 2.642 | 31.4 | 1 | 84.9 |
| Refined 2 | 0.9112 | 0.517 | 2.624 | 32.9 | 1 | 86.9 |
| Refined 3 | 0.9031 | 0.529 | 2.685 | 31.7 | 1.2 | 86.7 |
| Refined 4 | 0.9009 | 0.528 | 2.715 | 31.1 | 1.2 | 84.7 |
| Refined 5 | 0.8998 | 0.532 | 2.575 | 28.9 | 0.7 | 86.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, D.; Zhang, J.; Shen, W.; Sun, Y.; Wang, Z.; Wang, J.; Zhang, J.; Zhang, G.; Zhang, G.; Wang, Y.; et al. DNA Vaccines Encoding HTNV GP-Derived Th Epitopes Benefited from a LAMP-Targeting Strategy and Established Cellular Immunoprotection. Vaccines 2024, 12, 928. https://doi.org/10.3390/vaccines12080928
Jiang D, Zhang J, Shen W, Sun Y, Wang Z, Wang J, Zhang J, Zhang G, Zhang G, Wang Y, et al. DNA Vaccines Encoding HTNV GP-Derived Th Epitopes Benefited from a LAMP-Targeting Strategy and Established Cellular Immunoprotection. Vaccines. 2024; 12(8):928. https://doi.org/10.3390/vaccines12080928
Chicago/Turabian StyleJiang, Dongbo, Junqi Zhang, Wenyang Shen, Yubo Sun, Zhenjie Wang, Jiawei Wang, Jinpeng Zhang, Guanwen Zhang, Gefei Zhang, Yueyue Wang, and et al. 2024. "DNA Vaccines Encoding HTNV GP-Derived Th Epitopes Benefited from a LAMP-Targeting Strategy and Established Cellular Immunoprotection" Vaccines 12, no. 8: 928. https://doi.org/10.3390/vaccines12080928






