Abstract
Background: Concomitant acute ischemic stroke (AIS) caused by large vessel occlusion (LVO), and acute upper extremity arterial occlusion causing upper limb ischemia (ULI) is a rarely observed coincidence. The first-line treatment for AIS is mechanical thrombectomy (MT), with or without additional intravenous thrombolysis, while there are different pharmacological, surgical and endovascular treatment options for an acute occlusion of the UL arteries. Here, we describe the practicability, efficacy and safety of neurointerventional devices and techniques for MT of upper extremity arterial occlusions. Materials and Methods: A retrospective analysis of prospectively collected patient databases from four neurovascular centers was performed. Clinical and imaging data, as well as procedural parameters, were assessed. Results: Seven out of 6138 patients (incidence: 0.11%) presenting with an AIS due to the occlusion of craniocervical arteries requiring MT and a concomitant occlusion of the brachial (4/7), axillary (2/7), or ulnar (1/7) artery causing acute ULI were identified. Craniocervical MT was technically successful in all cases. Subsequent MT of the upper limb was performed using neurointerventional thrombectomy techniques, most frequently stent retriever thrombectomy (in 4/7 cases) and direct aspiration (in 7/7 cases). MT achieved successful recanalization in 6/7 cases, and the UL completely recovered in all six cases. In one case, recanalization was not successful, and the patient still had a marginally threatened extremity after the procedure, which improved after pharmacological therapy. Conclusion: In the rare case of AIS requiring MT and concomitant acute upper extremity arterial occlusion, MT of the UL arteries using neurointerventional devices and techniques is practical, effective, and safe.
1. Introduction
Together with intravenous thrombolysis, endovascular mechanical thrombectomy (MT) has become the first-line treatment for acute ischemic stroke (AIS) caused by large vessel occlusion (LVO) of the brain-supplying arteries []. Numerous studies have investigated the indications for MT and different MT techniques, which are now established to treat LVO [,,]. Another site which LVOs can occur is the upper extremity. There are several different treatment options for an acute upper extremity arterial occlusion causing acute upper limb ischemia, which include pharmacological, surgical and endovascular approaches [,,]. A rarely reported coincidence is an LVO of the craniocervical arteries causing an AIS, and a concomitant acute occlusion of the upper extremity arteries causing acute upper limb ischemia [,]. The ischemic tolerance of the brain is much lower than that of the extremities, which is why the LVO causing AIS should always be targeted first. After completion of the MT of the craniocervical LVO, it may be necessary to transfer the patient to another operation room, another medical department, or even to another hospital for the treatment of the upper extremity arterial occlusion. This transfer can be very time-consuming, and can substantially impair both the outcome of the patient’s upper limb and also the neurological outcome of the patient. A reasonable treatment option would appear to be the treatment of a concomitant upper extremity arterial occlusion in the same treatment session as applying neurointerventional MT techniques using the associated devices. However, this approach has not yet been the focus of research. This study aimed to assess the practicability and efficacy of neurointerventional devices and techniques for mechanical thrombectomy of acute upper extremity arterial occlusions.
2. Materials and Methods
Institutional review board approval was received, according to the guidelines of the local ethics committee. The need for individual patient consent was waived by each site due to the retrospective nature of this study. A retrospective analysis of prospectively maintained stroke databases for four high-volume neurointerventional centers was performed to identify all patients who presented with a concomitant MT-treated AIS, and an upper extremity arterial occlusion treated by endovascular means in the same treatment session. Patients with chronic occlusions of the upper extremity arteries, either pre-known or suspected by computed tomography angiography (CTA), were not included in this analysis.
Patient demographics, cardiovascular risk factors, neurological presentation (pre-morbid modified Rankin Scale (mRS) and National Institutes of Health Stroke Score (NIHSS)), and symptoms of the upper extremity arterial occlusion were assessed. The location of the craniocervical and the upper extremity arterial occlusions were recorded, along with the Alberta stroke program early CT score (ASPECTS) []. For the assessment of the pre- and post-interventional perfusion of the affected vessels, the modified Thrombolysis in Cerebral Infarction (mTICI) scale was used for the cerebral vessels, and the Thrombolysis in Limb Infarction (TILI) scale was used for the upper extremity vessels [,]. The TILI scale was defined as follows: TILI 0: no reperfusion, TILI 1: No filling of distal vessels, TILI 2a: reperfusion of >1/3 of the vascular territory of the initially occluded vessel, TILI 2b: residual perfusion deficits in ≤1/3 of the vascular territory of the initially occluded vessel, TILI 3: complete reperfusion with filling of all distal vessels. Technical success was defined as the successful completion of the procedure and mTICI ≥ 2b for the craniocervical occlusion and TILI ≥ 2b for the upper extremity arterial occlusion. The number of MT maneuvers, the MT techniques, the MT devices and the procedure times were recorded for the craniocervical and the upper extremity occlusions, respectively. Post-interventional assessments included the etiology of the stroke (according to the TOAST classification []), the clinical status of the extremity on discharge (according to the Rutherford classification []), and the neurological outcome of the patients (NIHSS at discharge and mRS at discharge and 3 months).
3. Results
A total of 6138 patients diagnosed with an AIS due to an LVO were treated by MT in four neurovascular centers between January 2016 and February 2021. Of this population, seven patients presented with a concomitant upper extremity arterial occlusion, which was also treated by endovascular means in the same treatment session, resulting in an estimated incidence of 0.11%. Patients who presented with this coincidence and in whom the upper extremity arterial occlusion was not treated endovascularly (e.g., surgical treatment or no treatment) could not be identified.
The baseline characteristics are summarized in Table 1. Mean age was 76.4 ± 10.2 years, with a female–male ratio of 4:3. Mean baseline NIHSS was 16 ± 6 (range, 9–24), and the mean baseline ASPECTS was 8 ± 2 (range, 6–10). Arterial hypertension (6/7) and atrial fibrillation (5/7) were the most frequently present cardiovascular risk factors. A large thrombus burden, defined as thrombus, which could not be completely removed with one productive MT maneuver, was observed in 5 of the 7 patients. These patients presented either with more than one LVO (patients #2 and #3), with an occlusion of the common carotid artery (CCA) or with a carotid T occlusion. The most frequent location of the upper extremity arterial occlusion was the brachial artery (4/7), followed by the axillary (2/7) and the ulnar artery (1/7). In 5/7 patients, cardioembolism was the most likely etiology of the stroke.

Table 1.
Baseline characteristics.
The procedural characteristics of the craniocervical occlusions are summarized in Table 2. Femoral access was used for all interventions. The MT of the craniocervical occlusion was technically successful in all cases. For the craniocervical occlusions, 4.1 ± 3.5 MT maneuvers were required for reperfusion, ranging from one to nine maneuvers. Especially for the patients with large thrombus burden, multiple maneuvers had to be performed (n = 9 in patient #1, n = 3 in patient #2, n = 9 in patient #3, and n = 1 in patients #6 and #7, respectively). In one case (patient #2), PTA and stenting of a high-grade stenosis of the proximal internal carotid artery was required. During craniocervical MT, one complication occurred: a dissection of the cervical vertebral artery (V2-segment), which was treated pharmacologically by the administration of heparin and aspirin. Due to the only minor hemodynamic effects and good flow via the contralateral vertebral artery, no interventional treatment was necessary.

Table 2.
Procedural characteristics.
The procedural characteristics of the upper extremity arterial occlusions are also summarized in Table 2. Three example cases are illustrated in Figure 1, Figure 2 and Figure 3. The procedure time for the upper extremity arterial occlusions was 38.9 ± 22.4 min. The number of MT maneuvers performed was 2.9 ± 1.4, ranging from 1 to 4 maneuvers. MT using a stent retriever was performed in 4/7 cases, while MT using direct aspiration was performed at least once in every case. In one case, after several unsuccessful MT maneuvers with conventional techniques, a double stent retriever thrombectomy, with two stent retrievers positioned parallel in the occluded vessel, was successfully performed. In a further case, after several unsuccessful MT maneuvers, the distal brachial artery could be recanalized by wire manipulation, using the tip of a 0.035-inch guidewire (Radifocus Glidewire Advantage; Terumo, Leuven, Belgium). This maneuver resulted in a transient perforation without any flow disruption or clinically visible or palpable hematoma. No further complications were observed. MT of the upper extremity arterial occlusion was technically successful in 6/7 cases (85.7%). Of the successful cases, complete reperfusion with filling of all distal vessels (TILI 3) was achieved in only one patient, and there were residual perfusion deficits (TILI 2b) in the remaining five cases. The case in which the recanalization was not successful was an occlusion of the ulnar artery, which persisted after a direct aspiration thrombectomy attempt. A pharmacological treatment with intravenous prostaglandin E1 for 4 days was started immediately after the procedure.
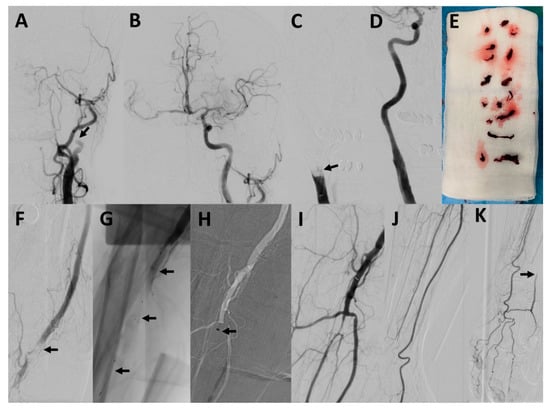
Figure 1.
Mechanical thrombectomy of concomitant occlusions of the internal carotid artery, common carotid artery and brachial artery. Patient #2 presented with a left-sided occlusion of the internal carotid artery ((A), arrow), a right-sided occlusion of the common carotid artery ((C), arrow) and an occlusion of the right brachial artery (F, arrow). An occlusion of the V2-segment of the left vertebral artery was also present (not shown) but was not recanalized. After successful recanalization of the left internal carotid artery using direct aspiration (B); with only poor collateralization of the territory of the right internal carotid artery) and of the right common carotid artery using aspiration, balloon dilatation and stenting (D), harboring a lot of thrombus material (E), the right upper limb occlusion was targeted. The brachial artery could be recanalized using one stent retriever maneuver (Neva-T stent retriever marked with arrows in (G) and 3 aspiration maneuvers (arrow pointing at the tip of a 6F Sofia aspiration catheter in (H)). Thrombectomy of the brachial artery was technically successful (I), also harboring several large thrombi (E). The radial artery could not be completely recanalized, but was filled retrogradely (J,K).
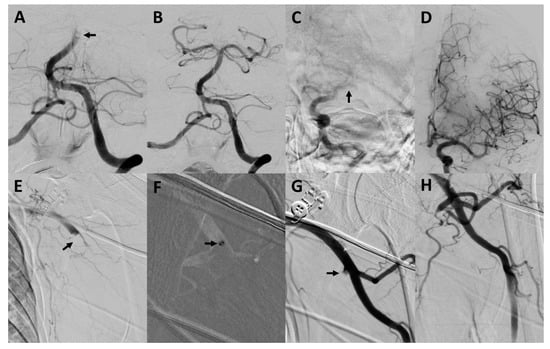
Figure 2.
Mechanical thrombectomy of concomitant occlusions of the basilar artery, middle cerebral artery and axillary artery. Patient #3 presented with an occlusion of the distal basilar artery ((A), arrow), a left-sided occlusion of the M1-segment of the middle cerebral artery ((C), arrow) and an occlusion of the left-sided distal axillary artery ((E), arrow). After successful recanalization of the basilar (B) and middle cerebral artery (D), recanalization of the axillary artery was performed. In total, 4 direct aspiration maneuvers were performed for recanalization (arrow in (F) pointing at the tip of a 9F Merci catheter), including an aspiration maneuver for recanalization of the subscapular artery using a 6F Sofia aspiration catheter (arrow in (G)). An angiogram of the recanalized axillary artery is presented in (H).
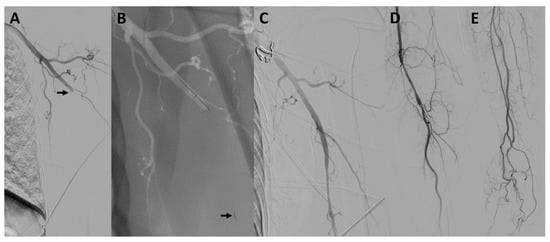
Figure 3.
Mechanical thrombectomy of concomitant occlusions of the left carotid T and the axillary artery. Patient #6 presented with an occlusion of the carotid T, which could be successfully recanalized with one thrombectomy maneuver (not shown). Digital subtraction angiography showed a concomitant occlusion of the left axillary artery (arrow in (A)). A microwire/microcatheter was navigated into the occluded vessel and an Embo Trap II 5 × 33 mm stent retriever was deployed within the occlusion (arrow pointing at the distal tip of the stent retriever in (B)). The occlusion was successfully recanalized with one stent retriever maneuver without any residual occlusion (C–E).
The outcome parameters are summarized in Table 3. One patient developed an intracerebral hemorrhage into the infarcted brain tissue after the procedure. A favorable neurological outcome (mRS ≤ 2 at 3 months) was achieved in 2/7 patients. In all cases with technically successful MT of the upper extremity arterial occlusion, the extremity was viable after the intervention. Only in the case in which the MT was not successful was the extremity was still marginally threatened postinterventionally. The pharmacological treatment resulted in an improvement in the extremity and rendered any further interventional therapy unnecessary.

Table 3.
Outcome.
The post-procedural medical antithrombotic management consisted of 100 mg of aspirin daily (lifelong) for all patients and additionally 75 mg of clopidogrel daily (for 30 days) for patient #2 because of the carotid artery stenting.
4. Discussion
Concomitant AIS caused by an LVO and an acute upper extremity arterial occlusion causing acute upper limb ischemia is a rarely observed coincidence [,]. Treating the LVO causing AIS first is of the utmost importance. However, the subsequent treatment of the upper extremity occlusion can be managed differently.
This study examined data from seven patients treated in four high-volume neurovascular centers. After the completion of endovascular treatment of an AIS, MT of the upper limb arteries in the same treatment session, using similar neurointerventional devices and techniques, was technically and clinically successful in 6 out of 7 cases, with only one minor complication.
Based on the fact that 5 out of 7 patients presented with a large thrombus burden, and cardioembolic stroke was the suspected etiology in another five patients (different patient subsets), we can suspect that large cardiac thrombi might be the reason for this dual event. After detachment of the thrombus in the heart, shattering of the thrombus in the aortic arch with subsequent multiple vessel occlusions is a possible explanation for the investigated coincidence. However, the relatively low case numbers in this study do not allow any certain conclusions to be drawn regarding the etiology of the investigated coincidence.
The first-line treatment for AIS caused by an LVO is mechanical thrombectomy (MT), while there are several different pharmacological, surgical and endovascular treatment options for an acute occlusion of the upper limb arteries. A common pharmacological treatment option is the selective endovascular infusion of thrombolytic drugs, such as recombinant tissue-type plasminogen activator (rt-PA), into the occluded vessel []. One of the most frequently applied surgical treatments is thrombo-embolectomy, commonly using the Fogarty technique: transverse brachial arteriotomy in the fossa cubiti and removal of thromboembolic material with a balloon catheter []. An effective endovascular recanalization technique is rheolytic thrombectomy [,]. The mechanism of rheolytic thrombectomy is a high-pressure saline jet in conjunction with aspiration. All of these treatment options carry certain potential drawbacks, which limit their application in the case of a concomitant AIS. The admission of rt-PA, which is often also used systemically for the treatment of the AIS, can increase the risk of intracranial hemorrhage, and is thus contraindicated in most cases. Surgical thrombo-embolectomy usually requires the transfer of the patient to another department or to another operation room, which can be time-consuming and impair the outcome of the patient’s limb. Moreover, any additional surgical procedure after a stroke may interfere with the neurological recovery of the patient. Neurointerventionalists do not regularly perform rheolytic thrombectomy, and the devices for rheolytic thrombectomy are often not available in the neurointerventional angiography suite. However, this technique might be a reasonable alternative if MT using neurointerventional techniques fails.
In the case of concomitant craniocervical LVO and an acute upper extremity arterial occlusion, after completion of the neurointerventional procedures, the arterial access route is already established, and the devices are already unpacked or even in place for MT of the upper extremity occlusion, which makes this approach highly time- and cost-effective. According to the results of our study, the neuro-interventionalist can effectively use the devices and techniques for the upper extremities, similar to cerebral thrombectomy. More aggressive MT techniques, which bear a higher risk of hemorrhagic complications in the brain, such as wire manipulation or double stent retriever techniques, can be used earlier and more liberally in the limb because of the comparatively far lower impact of hemorrhagic complications.
Data on MT of arterial limb occlusion using neurointerventional techniques or devices are rare. One study investigating MT of acute arterial limb occlusions by applying MT using a retrievable stent, without the coincidence of a concomitant AIS, was published by Zhou et al. []. In this study, they report 17 patients suffering from acute occlusions of the upper extremity arteries, treated using the Solitaire AB stent (Medtronic, Minneapolis, MN, USA). The occluded arteries could be successfully recanalized in 88.2% of the cases, with a mean number of three thrombectomy maneuvers. For neurointerventional MT procedures, the Solitaire AB stent was replaced by newer devices, such as the Solitaire X stent retriever (Medtronic) or other stent retrievers of newer generations from other manufacturers. Furthermore, in the study by Zhou et al., the access devices are different from those of neurointerventional MT procedures (e.g., triaxial system, balloon-guide catheters, aspiration catheters and low-profile microcatheters).
This study has several limitations. Given the low frequency of the investigated coincidence, the case numbers are low. However, this study includes data from four high-volume neurovascular centers, and is the largest study reporting on this topic at present. Furthermore, certain bias exists as a result of the retrospective nature of this work. Another drawback is the lack of imaging follow-up (e.g., ultrasonography) and the lack of clinical mid- or long-term follow-up of the patients’ limbs.
5. Conclusions
Concomitant LVO causing AIS, and acute upper extremity arterial occlusion causing acute upper limb ischemia, is a rarely observed coincidence. After completing the MT of the LVO, MT of the upper limb arteries in the same treatment session, using neurointerventional devices and techniques, is practical, effective, and safe for patients presenting with this coincidence.
Author Contributions
All listed authors contributed to the work. D.F.V. and M.A.M. acquired, analyzed and interpreted data for the work; designed the study; drafted the manuscript and approved the final manuscript. C.U., V.M., T.B., H.H. and M.B. acquired and analyzed data for the work and approved the final manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. Institutional review board approval was received, according to the guidelines of the local ethics committee.
Informed Consent Statement
The need for individual patient consent was waived by each site due to the retrospective nature of this study.
Data Availability Statement
All relevant data are included in this article.
Conflicts of Interest
D.F.V. has received travel support outside this work from MicroVention, Stryker and Cerenovus. C.U. has received travel/accommodation/meeting expenses unrelated to activities listed: MicroVention, Stryker. H.H. is co-founder and shareholder of phenox GmbH. M.B. reports board membership: D.S.M.B. Vascular Dynamics; consultancy: Roche, Guerbet, Codman; grants/grants pending: D.F.G, Hopp Foundation, Novartis, Siemens, Guerbet, Stryker, Covidien; payment for lectures (including service on speakers bureaus): Novartis, Roche, Guerbet, Teva, Bayer, Codman; M.A.M. has received consulting honoraria, speaker honoraria, and travel support outside this work from Codman, Covidien/Medtronic, MicroVention, Phenox, and Stryker. All other authors have nothing to disclosure.
References
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. Guidelines for the Early Management of Patients with Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2019, 50, e344–e418. [Google Scholar] [CrossRef] [PubMed]
- Lapergue, B.; Blanc, R.; Gory, B.; Labreuche, J.; Duhamel, A.; Marnat, G.; Saleme, S.; Costalat, V.; Bracard, S.; Desal, H.; et al. Effect of Endovascular Contact Aspiration vs. Stent Retriever on Revascularization in Patients with Acute Ischemic Stroke and Large Vessel Occlusion: The ASTER Randomized Clinical Trial. JAMA 2017, 318, 443–452. [Google Scholar] [CrossRef] [PubMed]
- Maus, V.; Behme, D.; Kabbasch, C.; Borggrefe, J.; Tsogkas, I.; Nikoubashman, O.; Wiesmann, M.; Knauth, M.; Mpotsaris, A.; Psychogios, M.N. Maximizing First-Pass Complete Reperfusion with SAVE. Clin. Neuroradiol. 2018, 28, 327–338. [Google Scholar] [CrossRef] [PubMed]
- Turc, G.; Bhogal, P.; Fischer, U.; Khatri, P.; Lobotesis, K.; Mazighi, M.; Schellinger, P.D.; Toni, D.; de Vries, J.; White, P.; et al. European Stroke Organisation (ESO)—European Society for Minimally Invasive Neurological Therapy (ESMINT) Guidelines on Mechanical Thrombectomy in Acute Ischaemic StrokeEndorsed by Stroke Alliance for Europe (SAFE). Eur. Stroke J. 2019, 4, 6–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turner, E.J.; Loh, A.; Howard, A. Systematic review of the operative and non-operative management of acute upper limb ischemia. J. Vasc. Nurs. 2012, 30, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Licht, P.B.; Balezantis, T.; Wolff, B.; Baudier, J.F.; Roder, O.C. Long-term outcome following thrombembolectomy in the upper extremity. Eur. J. Vasc. Endovasc. Surg. 2004, 28, 508–512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sultan, S.; Evoy, D.; Eldin, A.S.; Eldeeb, M.; Elmehairy, N. Atraumatic acute upper limb ischemia: A series of 64 patients in a Middle East tertiary vascular center and literature review. Vasc. Surg. 2001, 35, 181–197. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Choi, N.C.; Jang, I.S.; Kang, T.S.; Kang, C.; Jeong, J.H.; Kim, D.S. Simultaneous event of brachial artery occlusion and acute embolic stroke. Am. J. Emerg. Med. 2015, 33, e473–e474. [Google Scholar] [CrossRef] [PubMed]
- Khilchuk, A.A.; Vlasenko, S.V.; Scherbak, S.G.; Sarana, A.M.; Popov, V.V. Successful carotid thrombus aspiration, middle cerebral mechanical thrombectomy, and axillary artery clot disruption attempt in a patient with acute ischemic stroke and critical upper limb ischemia. Radiol. Case Rep. 2018, 13, 183–185. [Google Scholar] [CrossRef] [PubMed]
- Barber, P.A.; Demchuk, A.M.; Zhang, J.; Buchan, A.M. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet 2000, 355, 1670–1674. [Google Scholar] [CrossRef]
- Zhou, Y.; Sutedjo, J.; Gong, M.; Kong, J.; Zhao, B.; He, X.; Su, H. Solitaire AB thrombectomy system: Immediate results in 17 acute limb ischemia patients. Res. Sq. 2020. [Google Scholar] [CrossRef]
- Zaidat, O.O.; Yoo, A.J.; Khatri, P.; Tomsick, T.A.; von Kummer, R.; Saver, J.L.; Marks, M.P.; Prabhakaran, S.; Kallmes, D.F.; Fitzsimmons, B.F.; et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: A consensus statement. Stroke 2013, 44, 2650–2663. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adams, H.P., Jr.; Bendixen, B.H.; Kappelle, L.J.; Biller, J.; Love, B.B.; Gordon, D.L.; Marsh, E.E., 3rd. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993, 24, 35–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rutherford, R.B.; Baker, J.D.; Ernst, C.; Johnston, K.W.; Porter, J.M.; Ahn, S.; Jones, D.N. Recommended standards for reports dealing with lower extremity ischemia: Revised version. J. Vasc. Surg. 1997, 26, 517–538. [Google Scholar] [CrossRef] [Green Version]
- Cejna, M.; Salomonowitz, E.; Wohlschlager, H.; Zwrtek, K.; Bock, R.; Zwrtek, R. rt-PA thrombolysis in acute thromboembolic upper-extremity arterial occlusion. Cardiovasc. Interv. Radiol. 2001, 24, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.V.; Mortensen, L.S.; Lindholt, J.S.; Faergeman, O.; Henneberg, E.W.; Frost, L. Upper-limb thrombo-embolectomy: National cohort study in Denmark. Eur. J. Vasc. Endovasc. Surg. 2010, 40, 628–634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silva, J.A.; Ramee, S.R.; Collins, T.J.; Jenkins, J.S.; Lansky, A.J.; Ansel, G.M.; Dolmatch, B.L.; Glickman, M.H.; Stainken, B.; Ramee, E.; et al. Rheolytic thrombectomy in the treatment of acute limb-threatening ischemia: Immediate results and six-month follow-up of the multicenter AngioJet registry. Possis Peripheral AngioJet Study AngioJet Investigators. Catheter. Cardiovasc. Diagn. 1998, 45, 386–393. [Google Scholar] [CrossRef]
- Zeller, T.; Frank, U.; Burgelin, K.; Sinn, L.; Horn, B.; Schwarzwalder, U.; Roskamm, H.; Neumann, F.J. Treatment of acute embolic occlusions of the subclavian and axillary arteries using a rotational thrombectomy device. VASA 2003, 32, 111–116. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).