The Novel Technique of Uniportal Endoscopic Interlaminar Contralateral Approach for Coexisting L5-S1 Lateral Recess, Foraminal, and Extraforaminal Stenosis and Its Clinical Outcomes
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Patients
- Patients with radiating root pain, back pain, and neurogenic claudication and a minimum of 6 weeks of failed conservative treatment.
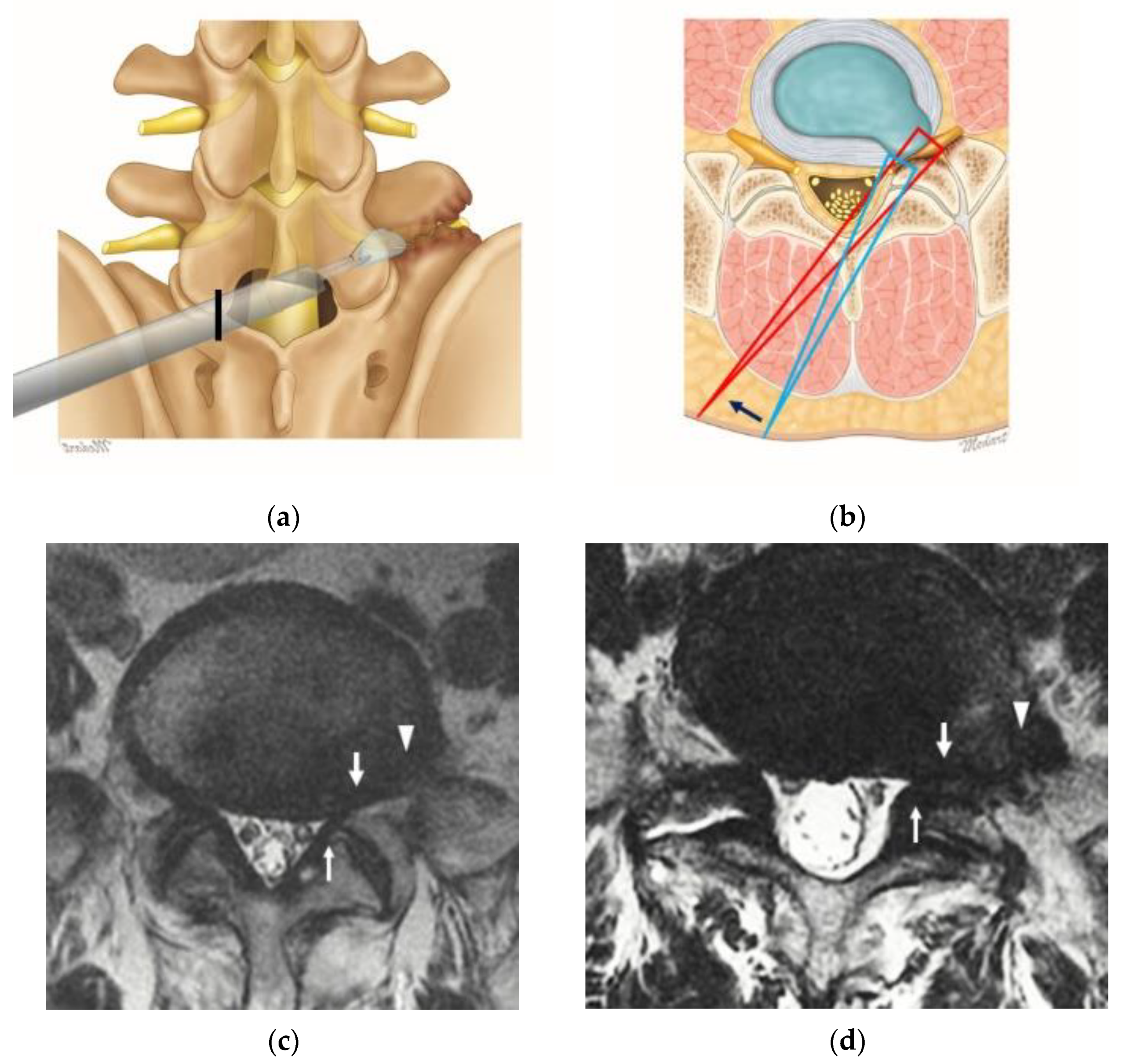
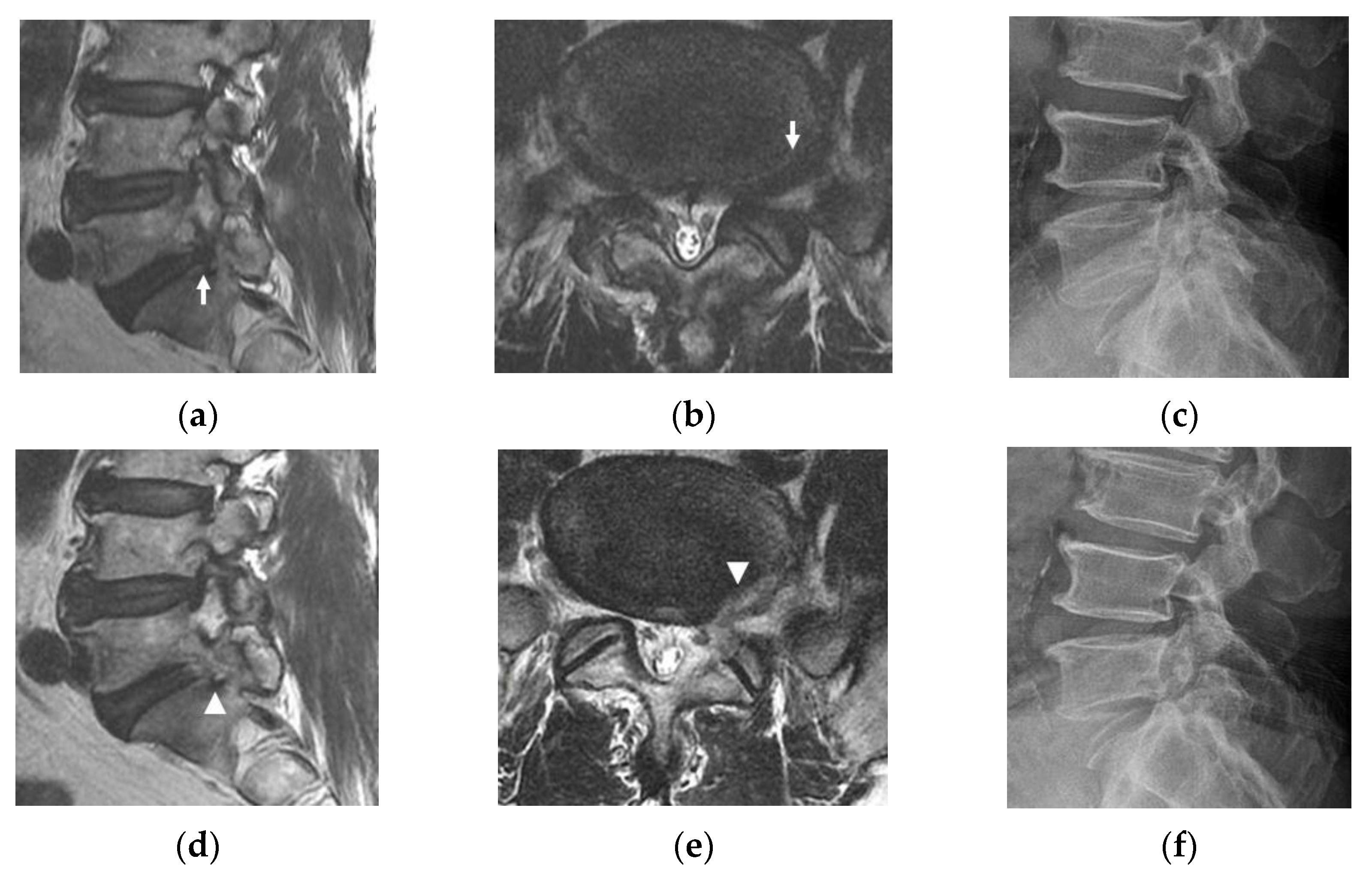
- Patients with L5 radiculopathy due to foraminal and extraforaminal stenosis at the L5-S1 level confirmed by MRI (Figure 1c,d).
- Patients with accompanying lateral recess stenosis at the same side with foraminal pathology, which simultaneously compress the L5 and S1 roots (Figure 1c,d).
- Patients with stable isthmic or degenerative spondylolisthesis, with less than 10% ventral displacement on dynamic radiography.
- Lumbosacral transitional vertebra with stenosis at the L5-S1 level.
- Other lumbar operations (fusion, decompression, discectomy, multi-level ICELF) at different levels performed simultaneously (patients with previous decompression or discectomy at the index level were included.)
- Accompanying lumbar lateral recess stenosis inducing L5 nerve root compression at the L4-L5 level.
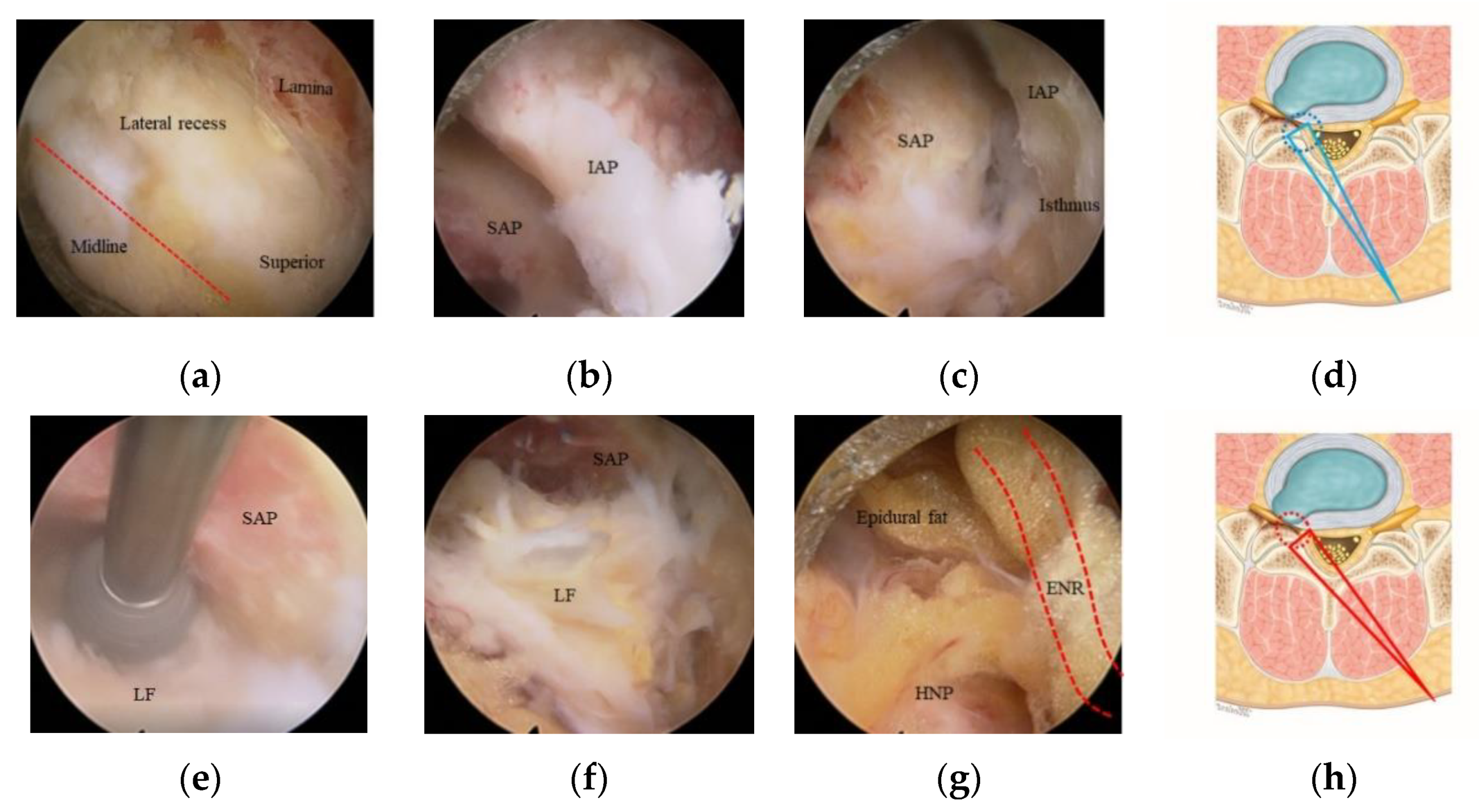
2.2. Surgical Procedures
2.3. Data Collection
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Genevay, S.; Atlas, S.J. Lumbar spinal stenosis. Best Pract. Res. Clin. Rheumatol. 2010, 24, 253–265. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Akiyama, M.; Koyanagi, I.; Niiya, Y.; Ihara, T.; Houkin, K. Double crush of L5 spinal nerve root due to L4/5 lateral recess stenosis and bony spur formation of lumbosacral transitional vertebra pseudoarticulation: A case report and review. NMC Case Rep. J. 2017, 4, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Kane, P.M.; Daniels, A.H.; Akelman, E. Double crush syndrome. J. Am. Acad. Orthop. Surg. 2015, 23, 558–562. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Patel, R.; Paudel, B.; Jang, J.-S.; Jang, I.-T.; Oh, S.-H.; Park, J.E.; Lee, S. Early outcomes of endoscopic contralateral foraminal and lateral recess decompression via an interlaminar approach in patients with unilateral radiculopathy from unilateral foraminal stenosis. World Neurosurg. 2017, 108, 763–773. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Singh, R.; Adsul, N.M.; Oh, S.W.; Noh, J.H.; Jang, I.T. Management of root-level double crush: Case report with technical notes on contralateral interlaminar foraminotomy with full endoscopic uniportal approach. World Neurosurg. 2019, 122, 505–507. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.H.; Kim, H.S.; Jang, I.-T. How I do it? Uniportal full endoscopic contralateral approach for lumbar foraminal stenosis with double crush syndrome. Acta Neurochir. 2019, 162, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Kim, H.S.; Kapoor, A.; Adsul, N.; Kim, K.J.; Choi, S.H.; Jang, J.-S.; Jang, I.-T.; Oh, S.-H. Feasibility of full endoscopic spine surgery in patients over the age of 70 years with degenerative lumbar spine disease. Neurospine 2018, 15, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Kim, J.Y.; Wu, P.H.; Jang, I.-T. Effect of dorsal root ganglion retraction in endoscopic lumbar decompressive surgery for foraminal pathology: A retrospective cohort study of interlaminar contralateral endoscopic lumbar foraminotomy and discectomy versus transforaminal endoscopic lumbar foraminotomy and discectomy. World Neurosurg. 2021. [Google Scholar] [CrossRef]
- Choi, K.C.; Kim, J.-S.; Ryu, K.-S.; Kang, B.U.; Ahn, Y.; Lee, S.-H. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation: Transforaminal versus interlaminar approach. Pain Physician 2013, 16, 547–556. [Google Scholar] [PubMed]
- Fritz, J.M.; Irrgang, J.J. A comparison of a modified Oswestry low back pain disability questionnaire and the Quebec back pain disability scale. Phys. Ther. 2001, 81, 776–788. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, J.W.; Yeom, J.S.; Kim, K.J.; Kim, H.J.; Chung, S.K.; Kang, H.S. A practical MRI grading system for lumbar foraminal stenosis. Am. J. Roentgenol. 2010, 194, 1095–1098. [Google Scholar] [CrossRef] [PubMed]
- Ito, M.; Tadano, S.; Kaneda, K. A biomechanical definition of spinal segmental instability taking personal and disc level differences into account. Spine 1993, 18, 2295–2304. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.Y.; Lee, S.H.; Lee, H.Y. Prevention of development of postoperative dysesthesia in transforaminal percutaneous endoscopic lumbar discectomy for intracanalicular lumbar disc herniation: Floating retraction technique. Minim. Invas. Neurosurg. 2011, 54, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Zhou, Y.; Zhang, Z. Postoperative dysesthesia in minimally invasive transforaminal lumbar interbody fusion: A report of five cases. Eur. Spine J. 2016, 25, 1595–1600. [Google Scholar] [CrossRef] [PubMed]
- Lewandrowski, K.-U.; Álvaro, D.; Calderaro, A.L.; Dos Santos, T.S.; Bergamaschi, J.P.M.; León, J.F.R.; Yeung, A. Dysethesia due to irritation of the dorsal root ganglion following lumbar transforaminal endoscopy: Analysis of frequency and contributing factors. Clin. Neurol. Neurosurg. 2020, 197, 106073. [Google Scholar] [CrossRef] [PubMed]
- Boden, S.D.; Martin, C.; Rudolph, R.; Kirkpatrick, J.S.; Moeini, S.M.R.; Hutton, W.C. Increase of motion between lumbar vertebrae after excision of the capsule and cartilage of the facets. A cadaver study. J. Bone Jt. Surg. Am. Vol. 1994, 76, 1847–1853. [Google Scholar] [CrossRef] [PubMed]
- Abumi, K.; Panjabi, M.M.; Kramer, K.M.; Duranceau, J.; Oxland, T.; Crisco, J.J. Biomechanical evaluation of lumbar spinal stability after graded facetectomies. Spine 1990, 15, 1142–1147. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, M.; Wakao, N.; Kamiya, M.; Hirasawa, A.; Osuka, K.; Joko, M.; Kawanami, K.; Takayasu, M. Lumbar extraforaminal entrapment: Performance characteristics of detecting the foraminal spinal angle using oblique coronal MRI. A multicenter study. Spine 2015, 15, 895–900. [Google Scholar] [CrossRef] [PubMed]
- Holm, E.K.; Bünger, C.; Foldager, C.B. Symptomatic lumbosacral transitional vertebra: A review of the current literature and clinical outcomes following steroid injection or surgical intervention. SICOT J 2017, 3, 71. [Google Scholar] [CrossRef] [PubMed]



| Parameters | Patients (n = 48) |
|---|---|
| Age, years (range) | 67.6 ± 9.7 (41–87) |
| Sex (male/female) | 21/27 |
| Follow-up period, months (range) | 10.9 ± 4.9 (6–24) |
| Operation time, mins (range) | 73. 5 ± 6.4 (56–97) |
| Foraminal stenosis (grade) | |
| Grade 0 | 0 |
| Grade 1 | 16 (33%) |
| Grade 2 | 20 (42%) |
| Grade 3 | 12 (25%) |
| Grade 2 + 3 | 32 (67%) |
| Combined pathologies, n (complication) | |
| Isthmic spondylolisthesis | 4 (n = 1, instability) |
| Adjacent segment disease | 1 (n = 1, POD grade 2) |
| Previous operation | TELD (n = 1, POD grade 1), hemilaminectomy (n = 1, no POD) |
| Complication Type | Patient |
|---|---|
| Revision operation, n | 2 (TLIF) |
| Segmental instability, n | 2 |
| Incidental durotomy, n | 2 |
| Hematoma, n | 1 |
| Postoperative dysesthesia, total, n (%) | 6 (12.5%) |
| Grade 1 | 4 (8.3%) |
| Grade 2 | 2 (4.2%) |
| Grade 3 | 0 |
| Parameter | Value | p-Value |
|---|---|---|
| Visual analog scale | ||
| Preoperative | 7.2 ± 1.3 (5–9) | - |
| Follow-up at 1 month | 3.2 ± 0.7 (1–4) | <0.001 * |
| Follow-up at 3 months | 2.4 ± 0.9 (1–3) | <0.001 * |
| Final follow-up | 2.3 ± 1.0 (1–3) | <0.001 * |
| Oswestry Disability Index | ||
| Preoperative | 72.3 ± 9.5 (56–84) | - |
| Follow-up at 1 month | 32.6 ± 6.6 (24–62) | <0.001 * |
| Follow-up at 3 months | 27.5 ± 5.2 (18–46) | <0.001 * |
| Final follow-up | 25.8 ± 5.5 (14–52) | <0.001 * |
| MacNab criteria at final follow-up, n (%) | Total, n = 48 | |
| Excellent | 11 (23%) | - |
| Good | 35 (73%) | - |
| Fair | 2 (4%) | - |
| Poor | 0 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.Y.; Kim, H.S.; Jeon, J.B.; Lee, J.H.; Park, J.H.; Jang, I.-T. The Novel Technique of Uniportal Endoscopic Interlaminar Contralateral Approach for Coexisting L5-S1 Lateral Recess, Foraminal, and Extraforaminal Stenosis and Its Clinical Outcomes. J. Clin. Med. 2021, 10, 1364. https://doi.org/10.3390/jcm10071364
Kim JY, Kim HS, Jeon JB, Lee JH, Park JH, Jang I-T. The Novel Technique of Uniportal Endoscopic Interlaminar Contralateral Approach for Coexisting L5-S1 Lateral Recess, Foraminal, and Extraforaminal Stenosis and Its Clinical Outcomes. Journal of Clinical Medicine. 2021; 10(7):1364. https://doi.org/10.3390/jcm10071364
Chicago/Turabian StyleKim, Ji Yeon, Hyeun Sung Kim, Jun Bok Jeon, Jun Hyung Lee, Jun Hwan Park, and Il-Tae Jang. 2021. "The Novel Technique of Uniportal Endoscopic Interlaminar Contralateral Approach for Coexisting L5-S1 Lateral Recess, Foraminal, and Extraforaminal Stenosis and Its Clinical Outcomes" Journal of Clinical Medicine 10, no. 7: 1364. https://doi.org/10.3390/jcm10071364
APA StyleKim, J. Y., Kim, H. S., Jeon, J. B., Lee, J. H., Park, J. H., & Jang, I.-T. (2021). The Novel Technique of Uniportal Endoscopic Interlaminar Contralateral Approach for Coexisting L5-S1 Lateral Recess, Foraminal, and Extraforaminal Stenosis and Its Clinical Outcomes. Journal of Clinical Medicine, 10(7), 1364. https://doi.org/10.3390/jcm10071364







