Participation in Social Activities and Relationship between Walking Habits and Disability Incidence
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design, Setting, and Participants
2.2. Disability Determination
2.3. Measurement of Physical and Social Activity
2.4. Potential Confounding Factors
2.5. Statistical Analysis
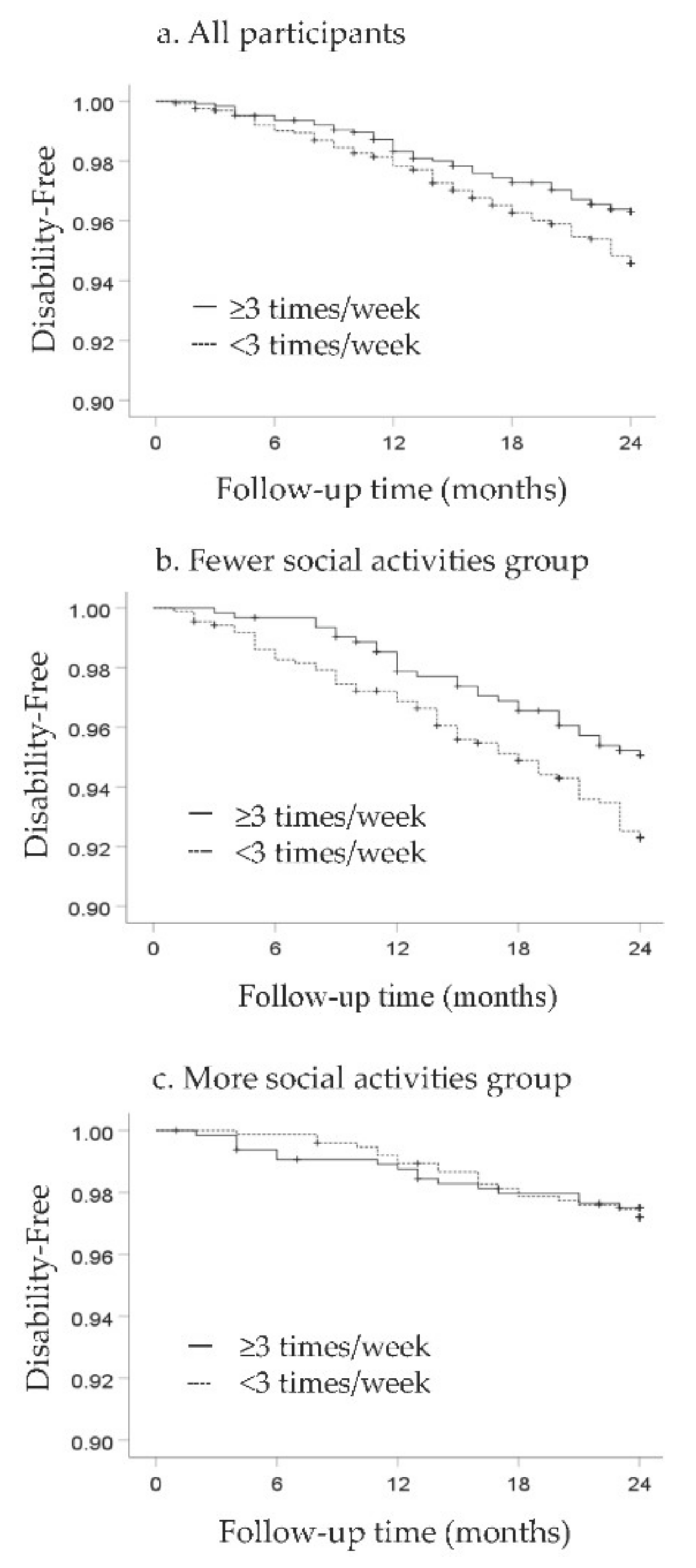
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- United Nations Department of Economic and Social Affairs Population Division. World Population Prospects: The 2019 Revision Population Database. Available online: http://esa.un.org/unpd/wpp/index.htm (accessed on 3 May 2020).
- Christensen, K.; Doblhammer, G.; Rau, R.; Vaupel, J.W. Ageing populations: The challenges ahead. Lancet 2009, 374, 1196–1208. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health, Labor and Welfare. Report on Various Current States around LTCI (Kaigo Hoken Seido wo Meguru Genjonitsuite). Available online: https://www.mhlw.go.jp/content/12601000/000482328.pdf (accessed on 3 May 2020).
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Otobe, Y.; Suzuki, M.; Koyama, S.; Kikuchi, T.; Kusumi, H.; Arai, H. Effect of the COVID-19 Epidemic on Physical Activity in Community-Dwelling Older Adults in Japan: A Cross-Sectional Online Survey. J. Nutr. Health Aging 2020, 24, 948–950. [Google Scholar] [CrossRef] [PubMed]
- Tison, G.H.; Avram, R.; Kuhar, P.; Abreau, S.; Marcus, G.M.; Pletcher, M.J.; Olgin, J.E. Worldwide Effect of COVID-19 on Physical Activity: A Descriptive Study. Ann. Intern. Med. 2020. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Morris, J.N.; Hardman, A.E. Walking to health. Sports Med. 1997, 23, 306–332. [Google Scholar] [CrossRef]
- Fancourt, D.; Steptoe, A. Comparison of physical and social risk-reducing factors for the development of disability in older adults: A population-based cohort study. J. Epidemiol. Community Health 2019, 73, 906–912. [Google Scholar] [CrossRef] [Green Version]
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Otobe, Y.; Suzuki, M.; Koyama, S.; Kikuchi, T.; Kusumi, H.; Arai, H. Letter to the Editor: Recovery of Physical Activity among Older Japanese Adults since the First Wave of the COVID-19 Pandemic. J. Nutr. Health Aging 2020, 24, 1036–1037. [Google Scholar] [CrossRef] [PubMed]
- Arai, S.; Pedlar, A. Moving beyond individualism in leisure theory: A critical analysis of concepts of community and social engagement. Leis. Stud. 2003, 22, 185–202. [Google Scholar] [CrossRef]
- Cabinet Office Japan. Annual Report on the Ageing Society. Available online: https://www8.cao.go.jp/kourei/whitepaper/w-2019/html/zenbun/s2_2_3.html (accessed on 2 April 2020).
- Fratiglioni, L.; Paillard-Borg, S.; Winblad, B. An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol. 2004, 3, 343–353. [Google Scholar] [CrossRef]
- Hikichi, H.; Kondo, N.; Kondo, K.; Aida, J.; Takeda, T.; Kawachi, I. Effect of a community intervention programme promoting social interactions on functional disability prevention for older adults: Propensity score matching and instrumental variable analyses, JAGES Taketoyo study. J. Epidemiol. Community Health 2015, 69, 905–910. [Google Scholar] [CrossRef]
- Makizako, H.; Shimada, H.; Tsutsumimoto, K.; Lee, S.; Doi, T.; Nakakubo, S.; Hotta, R.; Suzuki, T. Social Frailty in Community-Dwelling Older Adults as a Risk Factor for Disability. J. Am. Med. Dir. Assoc. 2015, 16, 1003.e7–1003.e11. [Google Scholar] [CrossRef]
- Merema, M.R. An Update on Social Activity and Depression in the Elderly: A Brief Review of Recent Findings and Key Issues. Healthy Aging Clin. Care Elder. 2014, 6, 11–15. [Google Scholar] [CrossRef] [Green Version]
- Shimada, H.; Makizako, H.; Doi, T.; Tsutsumimoto, K.; Suzuki, T. Incidence of Disability in Frail Older Persons with or Without Slow Walking Speed. J. Am. Med. Dir. Assoc. 2015, 16, 690–696. [Google Scholar] [CrossRef]
- Shimada, H.; Makizako, H.; Lee, S.; Doi, T.; Lee, S.; Tsutsumimoto, K.; Harada, K.; Hotta, R.; Bae, S.; Nakakubo, S.; et al. Impact of Cognitive Frailty on Daily Activities in Older Persons. J. Nutr. Health Aging 2016, 20, 729–735. [Google Scholar] [CrossRef]
- Tsutsui, T.; Muramatsu, N. Care-needs certification in the long-term care insurance system of Japan. J. Am. Geriatr. Soc. 2005, 53, 522–527. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.; Lee, S.; Harada, K.; Makino, K.; Chiba, I.; Katayama, O.; Shinkai, Y.; Park, H.; Shimada, H. Engagement in Lifestyle Activities is Associated with Increased Alzheimer’s Disease-Associated Cortical Thickness and Cognitive Performance in Older Adults. J. Clin. Med. 2020, 9, 1424. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Walk Score. Walk Score®: Drive less. Live more. Available online: www.walkscore.com/ (accessed on 18 June 2020).
- Carr, L.J.; Dunsiger, S.I.; Marcus, B.H. Validation of Walk Score for estimating access to walkable amenities. Br. J. Sports Med. 2011, 45, 1144–1148. [Google Scholar] [CrossRef]
- Google. What Is the Google AJAX Search API? Available online: http://code.google.com/apis/ajaxsearch/ (accessed on 7 April 2020).
- Van Holle, V.; Van Cauwenberg, J.; De Bourdeaudhuij, I.; Deforche, B.; Van de Weghe, N.; Van Dyck, D. Interactions between Neighborhood Social Environment and Walkability to Explain Belgian Older Adults’ Physical Activity and Sedentary Time. Int. J. Env. Res. Public Health 2016, 13, 569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kikuchi, H.; Nakaya, T.; Hanibuchi, T.; Fukushima, N.; Amagasa, S.; Oka, K.; Sallis, J.F.; Inoue, S. Objectively Measured Neighborhood Walkability and Change in Physical Activity in Older Japanese Adults: A Five-Year Cohort Study. Int. J. Environ. Res. Public Health 2018, 15, 1814. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amagasa, S.; Inoue, S.; Fukushima, N.; Kikuchi, H.; Nakaya, T.; Hanibuchi, T.; Sallis, J.F.; Owen, N. Associations of neighborhood walkability with intensity- and bout-specific physical activity and sedentary behavior of older adults in Japan. Geriatr. Gerontol. Int. 2019, 19, 861–867. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, J.A.; Moore, K.A.; Evenson, K.R.; Rodriguez, D.A.; Diez Roux, A.V. Walk Score(R) and Transit Score(R) and walking in the multi-ethnic study of atherosclerosis. Am. J. Prev. Med. 2013, 45, 158–166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Camhi, S.M.; Troped, P.J.; Garvey, M.; Hayman, L.L.; Must, A.; Lichtenstein, A.H.; Crouter, S.E. Associations between Walk Score and objective measures of physical activity in urban overweight and obese women. PLoS ONE 2019, 14, e0214092. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Twardzik, E.; Judd, S.; Bennett, A.; Hooker, S.; Howard, V.; Hutto, B.; Clarke, P.; Colabianchi, N. Walk Score and objectively measured physical activity within a national cohort. J. Epidemiol. Community Health 2019, 73, 549–556. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health, Labor and Welfare. Analysis of Regional Differences in the Rate of Level of Long-Term Care Accreditation (Youkaigo Ninteiritsu no Chiikisayoin ni Kansurubunseki). Available online: https://www5.cao.go.jp/keizai3/2018/09seisakukadai15-0.pdf (accessed on 15 April 2021).
- Shimada, H.; Makizako, H.; Doi, T.; Tsutsumimoto, K.; Lee, S.; Suzuki, T. Cognitive Impairment and Disability in Older Japanese Adults. PLoS ONE 2016, 11, e0158720. [Google Scholar] [CrossRef]
- Otsuka, T.; Tomata, Y.; Zhang, S.; Sugiyama, K.; Tanji, F.; Sugawara, Y.; Tsuji, I. Association between social participation and incident risk of functional disability in elderly Japanese: The Ohsaki Cohort 2006. J. Psychosom. Res. 2018, 111, 36–41. [Google Scholar] [CrossRef]
- Wong, C.H.; Wong, S.F.; Pang, W.S.; Azizah, M.Y.; Dass, M.J. Habitual walking and its correlation to better physical function: Implications for prevention of physical disability in older persons. J. Gerontol. A Biol. Sci. Med. Sci. 2003, 58, 555–560. [Google Scholar] [CrossRef] [Green Version]
- Wiswell, R.A.; Hawkins, S.A.; Jaque, S.V.; Hyslop, D.; Constantino, N.; Tarpenning, K.; Marcell, T.; Schroeder, E.T. Relationship between physiological loss, performance decrement, and age in master athletes. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M618–M626. [Google Scholar] [CrossRef] [Green Version]
- Ohtori, S.; Ito, T.; Yamashita, M.; Murata, Y.; Morinaga, T.; Hirayama, J.; Kinoshita, T.; Ataka, H.; Koshi, T.; Sekikawa, T.; et al. Evaluation of low back pain using the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire for lumbar spinal disease in a multicenter study: Differences in scores based on age, sex, and type of disease. J. Orthop. Sci. 2010, 15, 86–91. [Google Scholar] [CrossRef]
- Doi, T.; Shimada, H.; Makizako, H.; Tsutsumimoto, K.; Verghese, J.; Suzuki, T. Motoric Cognitive Risk Syndrome: Association with Incident Dementia and Disability. J. Alzheimers Dis. 2017, 59, 77–84. [Google Scholar] [CrossRef] [Green Version]
- James, B.D.; Boyle, P.A.; Buchman, A.S.; Bennett, D.A. Relation of late-life social activity with incident disability among community-dwelling older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2011, 66, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Kanamori, S.; Kai, Y.; Aida, J.; Kondo, K.; Kawachi, I.; Hirai, H.; Shirai, K.; Ishikawa, Y.; Suzuki, K. Social participation and the prevention of functional disability in older Japanese: The JAGES cohort study. PLoS ONE 2014, 9, e99638. [Google Scholar] [CrossRef] [PubMed]
- Levasseur, M.; Richard, L.; Gauvin, L.; Raymond, E. Inventory and analysis of definitions of social participation found in the aging literature: Proposed taxonomy of social activities. Soc. Sci. Med. 2010, 71, 2141–2149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cudjoe, T.K.M.; Kotwal, A.A. “Social distancing” amidst a crisis in social isolation and loneliness. J. Am. Geriatr. Soc. 2020. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences, Engineering, Medicine. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System; National Academies Press: Washington, DC, USA, 2020. [Google Scholar]
- Cudjoe, T.K.; Roth, D.L.; Szanton, S.L.; Wolff, J.L.; Boyd, C.M.; Thorpe, R.J., Jr. The epidemiology of social isolation: National health and aging trends study. J. Gerontol. Ser. B 2020, 75, 107–113. [Google Scholar] [CrossRef] [Green Version]
- Chen, S.; Calderon-Larranaga, A.; Saadeh, M.; Dohrn, I.M.; Welmer, A.K. Correlations of subjective and social wellbeing with sedentary behavior and physical activity in older adults—A population-based study. J. Gerontol. A Biol. Sci. Med. Sci. 2021. [Google Scholar] [CrossRef]
| Variable | Total | Participants Free of Disability | Participants with Disability | Participants Who Died or Relocated | p-Value | Post Hoc |
|---|---|---|---|---|---|---|
| (n = 2873) | (n = 2693) | (n = 133) | (n = 47) | |||
| Mean age at baseline, years | 73.1 ± 5.9 | 72.7 ± 5.7 | 80.2 ± 5.8 | 76.8 ± 7.3 | <0.001 * | Free < Died or relocated <Disability |
| Female sex, number (%) | 1618 (56.3) | 1518 (56.4) | 78 (58.6) | 22 (46.8) | 0.364 | |
| Medication use, number | 2.9 ± 2.6 | 2.8 ± 2.5 | 4.1 ± 2.6 | 4.0 ± 3.2 | <0.001 * | Free < Disability, Died or relocated |
| Chronic disease | ||||||
| Heart disease, no (%) | 2408 (83.8) | 2262 (84.0) | 106 (79.7) | 40 (85.1) | 0.410 | |
| Diabetes, no (%) | 2467 (85.9) | 2315 (86.0) | 113 (85.0) | 39 (83.0) | 0.805 | |
| Hyperlipidemia, no (%) | 1990 (69.3) | 1857 (69.0) | 97 (72.9) | 36 (76.6) | 0.345 | |
| Spinal diseases, no (%) | 2320 (80.8) | 2182 (81.1) | 105 (78.9) | 33 (70.2) | 0.145 | |
| Cohabitation status, no (%) | 341 (11.9) | 308 (11.4) § | 24 (18.0) ‡ | 9 (19.1) | 0.021 | |
| Years of education, years | 11.0 ± 2.3 | 11.1 ± 2.3 | 10.0 ± 2.3 | 10.2 ± 2.7 | <0.001 * | Disability, Died or relocated < Free |
| Physical function | ||||||
| Grip strength, kg | 27.3 ± 7.6 | 27.5 ± 7.6 | 23.5 ± 6.8 | 26.5 ± 7.1 | <0.001 * | Disability < Free |
| Cognitive function | ||||||
| Mini-Mental State Examination score | 27.0 ± 2.7 | 27.1 ± 2.5 | 24.8 ± 3.4 | 25.2 ± 3.8 | <0.001 * | Disability, Died or relocated < Free |
| Body mass index, kg/m2 | 23.5 ± 3.3 | 23.5 ± 3.3 | 23.1 ± 3.9 | 22.9 ± 4.0 | 0.330 | |
| Metabolic parameters | ||||||
| Total serum protein, g/dL | 7.4 ± 0.4 | 7.5 ± 0.4 | 7.4 ± 0.5 | 7.4 ± 0.6 | 0.253 | |
| Glycated hemoglobin, % | 5.8 ± 0.7 | 5.8 ± 0.6 | 5.8 ± 0.7 | 5.8 ± 0.6 | 0.955 | |
| Walk score | 67.9 ± 11.6 | 68.0 ± 11.6 | 67.0 ± 13.0 | 67.3 ± 11.5 | 0.665 | |
| Participants who walked ≥3 times per week | 1255 (43.7) | 1186 (44.0) | 46 (34.6) § | 23 (48.9) | 0.077 | |
| Social activity | ||||||
| Officer of a senior club or neighborhood association, yes (%) | 799 (27.8) | 758 (28.1) | 32 (24.1) | 9 (19.1) | 0.242 | |
| Attending a regional event, yes (%) | 653 (22.7) | 628 (23.3) ‡ | 17 (12.8) § | 8 (17.0) | 0.012 † | |
| Engage in environmental beautification activities, yes (%) | 779 (27.1) | 735 (27.3) | 35 (26.3) | 9 (19.1) | 0.450 | |
| Teaching, yes (%) | 263 (9.2) | 254 (9.4) ‡ | 8 (6.0) | 1 (2.1) | 0.099 | |
| Supporting activity, yes (%) | 430 (15.0) | 413 (15.3) ‡ | 10 (7.5) § | 7 (14.9) | 0.048 | |
| Working, yes (%) | 900 (31.3) | 874 (32.5) ‡ | 16 (12.0) § | 10 (21.3) | <0.001 † | |
| Go to karaoke, yes (%) | 632 (22.0) | 598 (22.2) | 30 (22.6) | 4 (8.5) § | 0.079 | |
| Eating out or tea party with friends, yes (%) | 2232 (77.7) | 2111 (78.4) ‡ | 93 (69.9) § | 28 (59.6) § | 0.001 † | |
| Go shopping with a friend, yes (%) | 1375 (47.9) | 1308 (48.6) ‡ | 55 (41.4) | 12 (25.5) § | 0.002 † | |
| Talk to a friend (including phone), yes (%) | 2616 (91.1) | 2457 (91.2) | 117 (88.0) | 42 (89.4) | 0.401 | |
| Attending an event or concerts, yes (%) | 1454 (50.6) | 1399 (51.9) ‡ | 39 (29.3) § | 16 (34.0) § | <0.001 † | |
| Go traveling, yes (%) | 1337 (46.5) | 1287 (47.8) ‡ | 37 (27.8) § | 13 (27.7) § | <0.001 † | |
| Social activity, items | 4.7 ± 2.5 | 4.8 ± 2.5 | 3.7 ± 2.4 | 3.4 ± 2.3 | <0.001 † | Disability, Died or relocated < Free |
| Variable | Participants Who Walked ≥3 Times per Week | Participants Who Walked <3 Times per Week | p-Value |
|---|---|---|---|
| (n = 1255) | (n = 1618) | ||
| Mean age at baseline, years | 73.4 ± 5.6 | 72.9 ± 6.2 | 0.012 * |
| Female sex, number (%) | 643 (51.2) § | 975 (60.3) ‡ | <0.001 † |
| Medication use, number | 3.0 ± 2.5 | 2.9 ± 2.5 | 0.390 |
| Chronic disease | |||
| Heart disease, no (%) | 1044 (83.2) | 1364 (84.3) | 0.421 |
| Diabetes, no (%) | 1074 (85.6) | 1393 (86.1) | 0.694 |
| Hyperlipidemia, no (%) | 867 (69.1) | 1123 (69.4) | 0.833 |
| Spinal diseases, no (%) | 1036 (82.7) ‡ | 1284 (79.4) § | 0.027 † |
| Cohabitation status, no (%) | 142 (11.3) | 199 (12.3) | 0.418 |
| Years of education | 11.1 ± 2.4 | 11.0 ± 2.3 | 0.308 |
| Physical function | |||
| Grip strength, kg | 27.8 ± 7.6 | 26.8 ± 7.5 | 0.270 |
| Cognitive function | |||
| Mini-Mental State Examination score | 26.9 ± 2.7 | 27.0 ± 2.6 | 0.148 |
| Body mass index, kg/m2 | 23.3 ± 3.1 | 23.6 ± 3.5 | 0.002 * |
| Metabolic parameters | |||
| Total serum protein, g/dL | 7.4 ± 0.4 | 7.4 ± 0.4 | 0.923 |
| Glycated hemoglobin, % | 5.8 ± 0.7 | 5.8 ± 0.6 | 0.592 |
| Walk score | 68.0 ± 11.6 | 68.0 ± 11.7 | 0.960 |
| Social activity | |||
| Officer of a senior club or neighborhood association, yes (%) | 401 (32.0) ‡ | 398 (24.6) § | <0.001 † |
| Attending a regional event, yes (%) | 320 (25.5) ‡ | 333 (20.6) § | 0.002 † |
| Engage in environmental beautification activities, yes (%) | 389 (31.0) ‡ | 390 (24.1) § | <0.001 † |
| Teaching, yes (%) | 141 (11.2) ‡ | 122 (7.5) § | 0.001 † |
| Supporting activity, yes (%) | 205 (16.3) | 225 (13.9) | 0.070 |
| Working, yes (%) | 326 (26.0) § | 574 (35.5) ‡ | <0.001 † |
| Go to karaoke, yes (%) | 315 (25.1) ‡ | 317 (19.6) § | <0.001 † |
| Eating out or tea party with friends, yes (%) | 973 (77.5) | 1259 (77.8) | 0.857 |
| Go shopping with a friend, yes (%) | 601 (47.9) | 774 (47.8) | 0.978 |
| Talk to a friend (including phone), yes (%) | 1151 (91.7) | 1465 (90.5) | 0.276 |
| Attending an event or concerts, yes (%) | 673 (53.6) ‡ | 781 (48.3) § | 0.004 † |
| Go traveling, yes (%) | 613 (48.8) ‡ | 724 (44.7) § | 0.029 † |
| Social activity, number | 4.9 ± 2.6 | 4.6 ± 2.4 | 0.001 * |
| All Participants | Number of Participants | Incident Disability Rate | Model 1 (Crude Model) | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | |||
| Participants who walked <3 times per week | 1255 | 46 (3.7%) | 1.00 | 1.00 | 1.00 | ||||||
| Participants who walked ≥3 times per week | 1618 | 87 (5.4%) | 0.68 | 0.47–0.97 | 0.032 | 0.70 | 0.49–1.00 | 0.050 | 0.67 | 0.46–0.96 | 0.030 |
| Fewer social activities group (0–4 activities) | Number of participants | Incident disability rate | Model 1 (Crude Model) | Model 2 | Model 3 | ||||||
| HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | |||
| Participants who walked <3 times per week | 613 | 30 (4.9%) | 1.00 | 1.00 | 1.00 | ||||||
| Participants who walked ≥3 times per week | 866 | 66 (7.6%) | 0.63 | 0.41–0.97 | 0.037 | 0.68 | 0.44–1.06 | 0.086 | 0.63 | 0.40–0.98 | 0.041 |
| More social activities group (5–12 activities) | Number of participants | Incident disability rate | Model 1 (Crude Model) | Model 2 | Model 3 | ||||||
| HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | |||
| Participants who walked <3 times per week | 642 | 16 (2.5%) | 1.00 | 1.00 | 1.00 | ||||||
| Participants who walked ≥3 times per week | 752 | 21 (2.8%) | 0.90 | 0.47–1.72 | 0.737 | 0.78 | 0.41–1.51 | 0.466 | 0.71 | 0.36–1.38 | 0.310 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Katayama, O.; Lee, S.; Bae, S.; Makino, K.; Chiba, I.; Harada, K.; Shinkai, Y.; Shimada, H. Participation in Social Activities and Relationship between Walking Habits and Disability Incidence. J. Clin. Med. 2021, 10, 1895. https://doi.org/10.3390/jcm10091895
Katayama O, Lee S, Bae S, Makino K, Chiba I, Harada K, Shinkai Y, Shimada H. Participation in Social Activities and Relationship between Walking Habits and Disability Incidence. Journal of Clinical Medicine. 2021; 10(9):1895. https://doi.org/10.3390/jcm10091895
Chicago/Turabian StyleKatayama, Osamu, Sangyoon Lee, Seongryu Bae, Keitaro Makino, Ippei Chiba, Kenji Harada, Yohei Shinkai, and Hiroyuki Shimada. 2021. "Participation in Social Activities and Relationship between Walking Habits and Disability Incidence" Journal of Clinical Medicine 10, no. 9: 1895. https://doi.org/10.3390/jcm10091895
APA StyleKatayama, O., Lee, S., Bae, S., Makino, K., Chiba, I., Harada, K., Shinkai, Y., & Shimada, H. (2021). Participation in Social Activities and Relationship between Walking Habits and Disability Incidence. Journal of Clinical Medicine, 10(9), 1895. https://doi.org/10.3390/jcm10091895







