High-Intensity Laser Therapy (HILT) as an Emerging Treatment for Vulvodynia and Chronic Musculoskeletal Pain Disorders: A Systematic Review of Treatment Efficacy
Abstract
:1. Introduction
Objectives
2. Materials and Methods
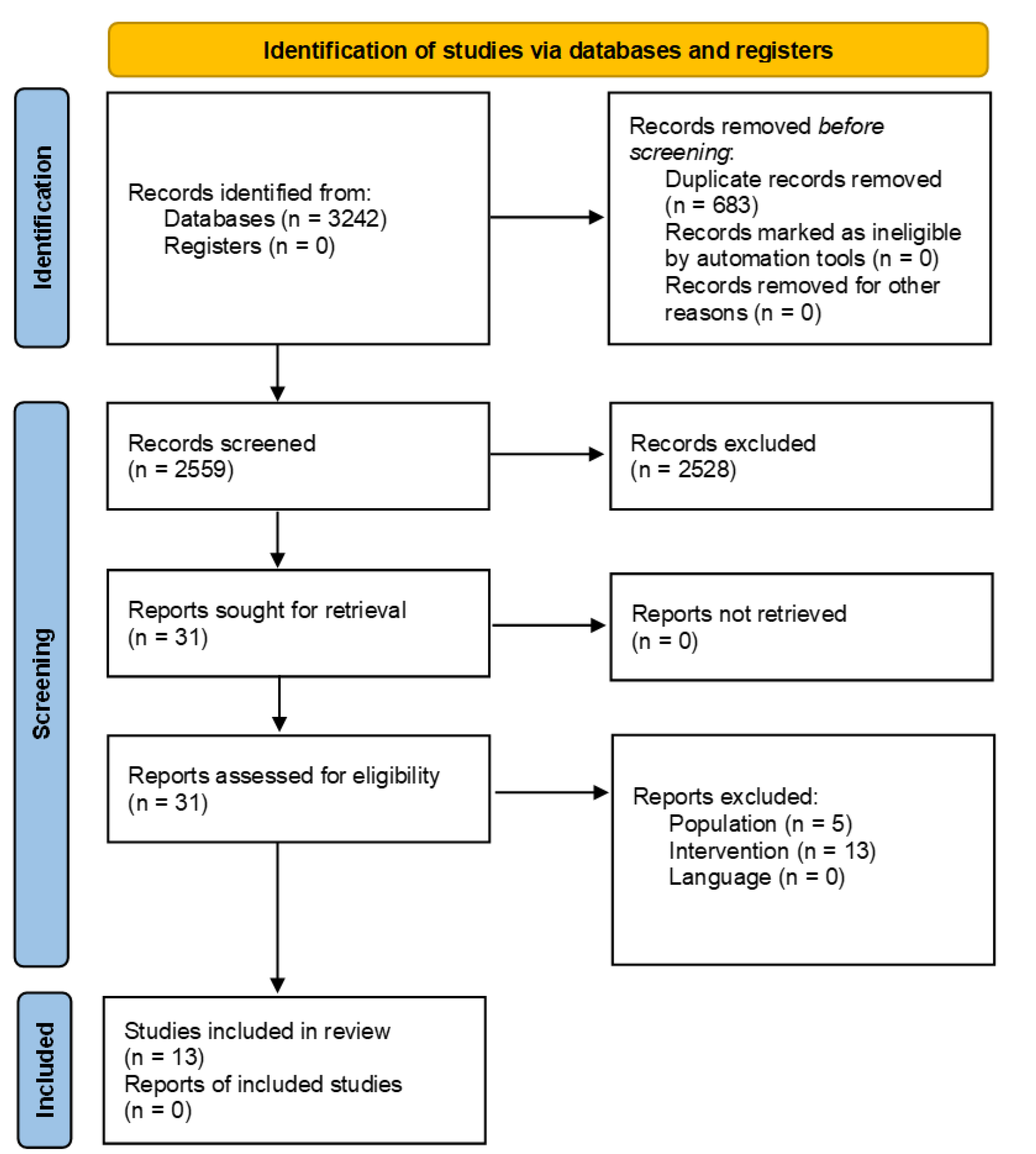
2.1. Identification and Selection of Trials
2.2. Eligibility Criteria
2.3. Data Extraction and Management
2.4. Data Analysis and Quality of Evidence
2.5. Assessment of Risk of Bias
3. Results
3.1. Search Results
3.2. Vulvodynia Study Summary
3.3. Characteristics of Included Musculoskeletal Pain Studies
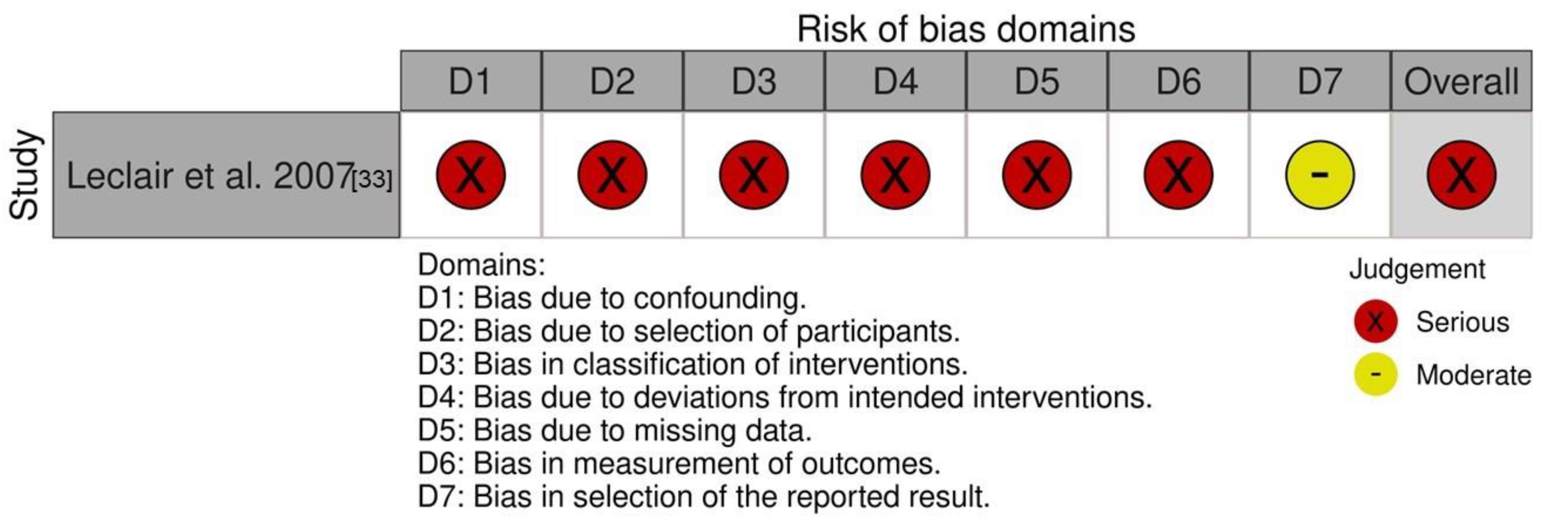
3.4. Quality Assessment/Risk of Bias in the Included Musculoskeletal Pain Studies
3.5. Comparators and Co-Interventions
3.6. Outcomes
3.6.1. Primary Outcome—Pain
3.6.2. Secondary Outcome—Function
3.6.3. Time-Dependent Improvements within HILT Groups
3.6.4. Treatment Efficiency Considering Laser Parameters and Dosimetry
3.6.5. Adverse Events
3.6.6. Effect Sizes and Clinical Significance
3.6.7. Quality of Evidence
4. Discussion
4.1. HILT and Biological Effects on Tissues and Pain
4.2. Clinical Importance of the Results
4.3. Methodological Considerations
4.4. Research Implications and Recommendations for Future Studies
4.5. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Search Strings
Appendix B. GRADE Assessment
| HILT Compared to Placebo/Active Comparator for the Treatment of Chronic Musculoskeletal Pain | |||||||
|---|---|---|---|---|---|---|---|
| Certainty Assessment | Summary of Findings | ||||||
| Participants(Studies) Follow-up | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Overall Certainty of Evidence | Impact |
| Pain (assessed with: VAS, NRS) | |||||||
| 726 (13 RCTs) | not serious a | not serious | not serious | Serious b | none c | ⨁⨁⨁◯ Moderate | HILT may relieve pain in chronic musculoskeletal pain conditions. |
| Function (assessed with: ODI, MODQ, RMQ, PDI, NDI, JFLS-20) | |||||||
| 726 (13 RCTs) | not serious a | not serious | not serious | Serious b | none c | ⨁⨁⨁◯ Moderate | HILT may improve function in chronic musculoskeletal pain conditions. |
| JFLS-20: Jaw Functional Limitation Scale 20; MODQ: Modified Oswestry Disability Questionnaire; NDI: Neck disability index; ODI; Oswestry Disability Index; PDI: Pain disability Index; RDQ: Roland disability questionnaire; VAS: visual analogue scale; NRS: Numeric rating scale, PDI: Pain Disability Index Explanations a. Most of the studies (7 out of 13) had a low risk of bias or some concern. Five studies had an increase in their overall risk of bias because they omitted to report the concealment method (unclear concealment). Five studies had an increase in their overall risk of bias because blinding was impossible (comparing HILT to another treatment modality) and patient-reported outcomes were used (inevitable to assess pain and function). A downgrade in the risk score is automatically attributed in RoB 2.0 when patients become assessors of their own condition via self-reported outcomes and when they cannot be blinded to their allocated interventions. Since these potential limitations are unlikely to lower confidence in the overall results, the evidence was not downgraded for the risk of bias. b. A narrative synthesis was conducted. Estimates may not be precise as the calculated effect sizes were not available for all included studies. c. A statistical evaluation of publication bias was not possible in this case. Although the review presents mostly positive studies, publication bias is unlikely due to the comprehensive search that has been completed. | |||||||
References
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2021, 396, 2006–2017. [Google Scholar] [CrossRef]
- Treede, R.D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2019, 160, 19–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pukall, C.F.; Goldstein, A.T.; Bergeron, S.; Foster, D.; Stein, A.; Kellogg-Spadt, S.; Bachmann, G. Vulvodynia: Definition, Prevalence, Impact, and Pathophysiological Factors. J. Sex. Med. 2016, 13, 291–304. [Google Scholar] [CrossRef]
- Morin, M.; Binik, Y.M.; Bourbonnais, D.; Khalife, S.; Ouellet, S.; Bergeron, S. Heightened Pelvic Floor Muscle Tone and Altered Contractility in Women With Provoked Vestibulodynia. J. Sex. Med. 2017, 14, 592–600. [Google Scholar] [CrossRef]
- Bornstein, J.; Goldstein, A.T.; Stockdale, C.K.; Bergeron, S.; Pukall, C.; Zolnoun, D.; Coady, D.; Consensus vulvar pain terminology committee of the International Society for the Study of Vulvovaginal Disease. 2015 ISSVD, ISSWSH, and IPPS Consensus Terminology and Classification of Persistent Vulvar Pain and Vulvodynia. J. Sex. Med. 2016, 13, 607–612. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, A.T.; Pukall, C.F.; Brown, C.; Bergeron, S.; Stein, A.; Kellogg-Spadt, S. Vulvodynia: Assessment and Treatment. J. Sex. Med. 2016, 13, 572–590. [Google Scholar] [CrossRef] [PubMed]
- Falsetta, M.L.; Foster, D.C.; Bonham, A.D.; Phipps, R.P. A review of the available clinical therapies for vulvodynia management and new data implicating proinflammatory mediators in pain elicitation. BJOG 2017, 124, 210–218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thibault-Gagnon, S.; Morin, M. Active and Passive Components of Pelvic Floor Muscle Tone in Women with Provoked Vestibulodynia: A Perspective Based on a Review of the Literature. J. Sex. Med. 2015, 12, 2178–2189. [Google Scholar] [CrossRef]
- Mense, S. Muscle pain: Mechanisms and clinical significance. Dtsch. Arztebl. Int. 2008, 105, 214–219. [Google Scholar] [CrossRef]
- Gerdle, B.; Ghafouri, B.; Ernberg, M.; Larsson, B. Chronic musculoskeletal pain: Review of mechanisms and biochemical biomarkers as assessed by the microdialysis technique. J. Pain Res. 2014, 7, 313–326. [Google Scholar] [CrossRef] [Green Version]
- Sharma, H.; Ji, E.; Yap, P.; Vilimas, P.; Kyloh, M.; Spencer, N.J.; Haberberger, R.V.; Barry, C.M. Innervation Changes Induced by Inflammation in the Murine Vagina. Neuroscience 2018, 372, 16–26. [Google Scholar] [CrossRef] [Green Version]
- Stockdale, C.K.; Lawson, H.W. 2013 Vulvodynia Guideline update. J. Low. Genit. Tract Dis. 2014, 18, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Mester, E.; Szende, B.; Gartner, P. The effect of laser beams on the growth of hair in mice. Radiobiol. Radiother. 1968, 9, 621–626. [Google Scholar]
- Mester, E.; Nagylucskay, S.; Doklen, A.; Tisza, S. Laser stimulation of wound healing. Acta Chir. Acad. Sci. Hung. 1976, 17, 49–55. [Google Scholar] [PubMed]
- Monici, M.; Cialdai, F.; Fusi, F.; Romano, G.; Pratesi, R. Effects of pulsed Nd:YAG laser at molecular and cellular level. A study on the basis of Hilterapia. Energy Health 2009, 3, 26–33. [Google Scholar]
- Alayat, M.S.; Elsodany, A.M.; Miyajan, A.F.; Alzhrani, A.A.; Alzhrani, H.M.S.; Maqliyah, A.M. Changes in local skin temperature after the application of a pulsed Nd:YAG laser to healthy subjects: A prospective crossover controlled trial. Lasers Med. Sci. 2019, 34, 1681–1688. [Google Scholar] [CrossRef] [PubMed]
- Zati, A.; Fortuna, D.; Valent, A.; Filippi, M.; Bilotta, T. High Intensity Laser Therapy (HILT) Versus TENS and NSAIDs in Low Back Pain: Clinical Study; SPIE: Florence, Italy, 2004; Volume 5610. [Google Scholar]
- Preti, M.; Vieira Batista, P.; Digesu, A.; Mourad, S. ISSVD/ICS Comments on the FDA Communication on the Use of Energy-Based Devices to Perform Vaginal ‘Rejuvenation’ or Vaginal Cosmetic Procedures. 2018. Available online: https://3b64we1rtwev2ibv6q12s4dd-wpengine.netdna-ssl.com/wp-content/uploads/2018/08/2018_08_05-ISSVD_ICS.pdf (accessed on 30 February 2022).
- FDA Warns Against Use of Energy-Based Devices to Perform Vaginal ‘Rejuvenation’ or Vaginal Cosmetic Procedures: FDA Safety Communication. Available online: https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm615013.htm (accessed on 7 September 2019).
- Perrot, S.; Cohen, M.; Barke, A.; Korwisi, B.; Rief, W.; Treede, R.D. The IASP classification of chronic pain for ICD-11: Chronic secondary musculoskeletal pain. Pain 2019, 160, 77–82. [Google Scholar] [CrossRef]
- Song, H.J.; Seo, H.J.; Lee, Y.; Kim, S.K. Effectiveness of high-intensity laser therapy in the treatment of musculoskeletal disorders: A systematic review and meta-analysis of randomized controlled trials. Medicine 2018, 97, e13126. [Google Scholar] [CrossRef]
- Alayat, M.S.M.; Alshehri, M.A.; Shousha, T.M.; Abdelgalil, A.A.; Alhasan, H.; Khayyat, O.K.; Al-Attar, W.S. The effectiveness of high intensity laser therapy in the management of spinal disorders: A systematic review and meta-analysis. J. Back Musculoskelet. Rehabil. 2019, 32, 869–884. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Standards for the design and conduct of systematic reviews with low-level laser therapy for musculoskeletal pain and disorders. Photomed. Laser Surg. 2006, 24, 759–760. [CrossRef] [PubMed] [Green Version]
- Glazov, G.; Yelland, M.; Emery, J. Low-level laser therapy for chronic non-specific low back pain: A meta-analysis of randomised controlled trials. Acupunct. Med. 2016, 34, 328–341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterne, J.A.; Hernan, M.A.; Reeves, B.C.; Savovic, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Hillsdale, N.J., Ed.; Lawrence Erlbaum Associates: New York, NY, USA, 1988. [Google Scholar]
- Sawilowsky, S.S. New effect size rules of thumb. J. Mod. Appl. Stat. Methods 2009, 8, 3. [Google Scholar] [CrossRef]
- Balshem, H.; Helfand, M.; Schünemann, H.J.; Oxman, A.D.; Kunz, R.; Brozek, J.; Vist, G.E.; Falck-Ytter, Y.; Meerpohl, J.; Norris, S.; et al. GRADE guidelines: 3. Rating the quality of evidence. J. Clin. Epidemiol. 2011, 64, 401–406. [Google Scholar] [CrossRef]
- Murad, M.H.; Mustafa, R.A.; Schünemann, H.J.; Sultan, S.; Santesso, N. Rating the certainty in evidence in the absence of a single estimate of effect. Evid. Based Med. 2017, 22, 85–87. [Google Scholar] [CrossRef] [Green Version]
- Schünemann, H.; Brożek, J.; Guyatt, G.; Oxman, A. (Eds.) GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations; Updated October 2013. Available online: Guidelinedevelopment.org/handbook (accessed on 20 February 2022).
- Higgins, J.P.; Sterne, J.; Savović, J.; Page, M.J.; Hróbjartsson, A.; Boutron, I.; Reeves, B.; Eldridge, S. A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst. Rev. 2016, 10 (Suppl. 1), 29–31. [Google Scholar]
- Leclair, C.M.; Goetsch, M.F.; Lee, K.K.; Jensen, J.T. KTP-nd:YAG laser therapy for the treatment of vestibulodynia: A follow-up study. J. Reprod. Med. 2007, 52, 53–58. [Google Scholar]
- Alayat, M.S.; Atya, A.M.; Ali, M.M.; Shosha, T.M. Long-term effect of high-intensity laser therapy in the treatment of patients with chronic low back pain: A randomized blinded placebo-controlled trial. Lasers Med. Sci. 2014, 29, 1065–1073. [Google Scholar] [CrossRef]
- Alayat, M.S.; Mohamed, A.A.; Helal, O.F.; Khaled, O.A. Efficacy of high-intensity laser therapy in the treatment of chronic neck pain: A randomized double-blind placebo-control trial. Lasers Med. Sci. 2016, 31, 687–694. [Google Scholar] [CrossRef]
- Alayat, M.S.; Elsoudany, A.M.; Ali, M.E. Efficacy of Multiwave Locked System Laser on Pain and Function in Patients with Chronic Neck Pain: A Randomized Placebo-Controlled Trial. Photomed. Laser Surg. 2017, 35, 450–455. [Google Scholar] [CrossRef] [PubMed]
- Basford, J.R.; Sheffield, C.G.; Harmsen, W.S. Laser therapy: A randomized, controlled trial of the effects of low-intensity Nd: YAG laser irradiation on musculoskeletal back pain. Arch. Phys. Med. Rehabil. 1999, 80, 647–652. [Google Scholar] [CrossRef]
- Choi, H.-W.; Lee, J.; Lee, S.; Choi, J.; Lee, K.; Kim, B.-K.; Kim, G.-J. Effects of high intensity laser therapy on pain and function of patients with chronic back pain. J. Phys. Ther. Sci. 2017, 29, 1079–1081. [Google Scholar] [CrossRef] [Green Version]
- Conte, P.S.A.; Fiore, P.; Lopresto, A.; Mazzaracchio, M. Treatment of chronic low back pain: Back school versus Hilterapia. Energy Health 2009, 3, 10–13. [Google Scholar]
- Dundar, U.; Turkmen, U.; Toktas, H.; Solak, O.; Ulasli, A.M. Effect of high-intensity laser therapy in the management of myofascial pain syndrome of the trapezius: A double-blind, placebo-controlled study. Lasers Med. Sci. 2015, 30, 325–332. [Google Scholar] [CrossRef]
- Fiore, P.; Panza, F.; Cassatella, G.; Russo, A.; Frisardi, V.; Solfrizzi, V.; Ranieri, M.; Di Teo, L.; Santamato, A. Short-term effects of high-intensity laser therapy versus ultrasound therapy in the treatment of low back pain: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2011, 47, 367–373. [Google Scholar] [PubMed]
- Gocevska, M.; Nikolikj-Dimitrova, E.; Gjerakaroska-Savevska, C. Effects of High-Intensity Laser in Treatment of Patients with Chronic Low Back Pain. Open Access Maced. J. Med. Sci. 2019, 7, 949–954. [Google Scholar] [CrossRef]
- Abdelbasset, W.K.; Nambi, G.; Alsubaie, S.F.; Abodonya, A.M.; Saleh, A.K.; Ataalla, N.N.; Ibrahim, A.A.; Tantawy, S.A.; Kamel, D.M.; Verma, A.; et al. A Randomized Comparative Study between High-Intensity and Low-Level Laser Therapy in the Treatment of Chronic Nonspecific Low Back Pain. Evid. Based Complement. Altern. Med. 2020, 2020, 1350281. [Google Scholar] [CrossRef] [PubMed]
- Abdelbasset, W.K.; Nambi, G.; Elsayed, S.H.; Alrawaili, S.M.; Ataalla, N.N.; Abodonya, A.M.; Saleh, A.K.; Moawd, S.A. Short-term clinical efficacy of the pulsed Nd: YAG laser therapy on chronic nonspecific low back pain: A randomized controlled study. Medicine 2020, 99, e22098. [Google Scholar] [CrossRef]
- Abdelbasset, W.K.; Nambi, G.; Elsayed, S.H.; Soliman, G.S.; Alessi, A.A.; Alsalem, I.N.; Alwadai, S.M. A Prospective Comparative Study of Pulsed High-Intensity Laser Therapy and Pulsed Electromagnetic Field on Chronic Nonspecific Low Back Pain. Photobiomodul. Photomed. Laser Surg. 2021, 39, 362–368. [Google Scholar] [CrossRef]
- Ekici, Ö.; Dündar, Ü.; Büyükbosna, M. Effectiveness of high-intensity laser therapy in patients with myogenic temporomandibular joint disorder: A double-blind, placebo-controlled study. J. Stomatol. Oral Maxillofac. Surg. 2021, 123, e90–e96. [Google Scholar] [CrossRef] [PubMed]
- Dworkin, R.H.; Turk, D.C.; Wyrwich, K.W.; Beaton, D.; Cleeland, C.S.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Kerns, R.D.; Ader, D.N.; et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J. Pain 2008, 9, 105–121. [Google Scholar] [CrossRef] [PubMed]
- Ostelo, R.W.; de Vet, H.C. Clinically important outcomes in low back pain. Best Pract. Res. Clin. Rheumatol. 2005, 19, 593–607. [Google Scholar] [CrossRef]
- Stratford, P.; Riddle, D.; Binkley, J.; Spadoni, G.; Westaway, M.; Padfield, B. Using the Neck Disability Index to make decisions concerning individual patients. Physiother. Can. 1999, 51, 107–112. [Google Scholar]
- Soer, R.; Reneman, M.F.; Vroomen, P.C.; Stegeman, P.; Coppes, M.H. Responsiveness and minimal clinically important change of the Pain Disability Index in patients with chronic back pain. Spine 2012, 37, 711–715. [Google Scholar] [CrossRef]
- Reynolds, B.; Puentedura, E.J.; Kolber, M.J.; Cleland, J.A. Effectiveness of Cervical Spine High-Velocity, Low-Amplitude Thrust Added to Behavioral Education, Soft Tissue Mobilization, and Exercise for People With Temporomandibular Disorder With Myalgia: A Randomized Clinical Trial. J. Orthop. Sports Phys. Ther. 2020, 50, 455–465. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, Y.L.; Chou, L.W.; Chang, P.L.; Yang, C.C.; Kao, M.J.; Hong, C.Z. Low-level laser therapy alleviates neuropathic pain and promotes function recovery in rats with chronic constriction injury: Possible involvements in hypoxia-inducible factor 1α (HIF-1α). J. Comp. Neurol. 2012, 520, 2903–2916. [Google Scholar] [CrossRef] [PubMed]
- Cidral-Filho, F.J.; Martins, D.F.; Moré, A.O.; Mazzardo-Martins, L.; Silva, M.D.; Cargnin-Ferreira, E.; Santos, A.R. Light-emitting diode therapy induces analgesia and decreases spinal cord and sciatic nerve tumour necrosis factor-α levels after sciatic nerve crush in mice. Eur. J. Pain 2013, 17, 1193–1204. [Google Scholar] [CrossRef] [PubMed]
- Jimbo, K.; Noda, K.; Suzuki, K.; Yoda, K. Suppressive effects of low-power laser irradiation on bradykinin evoked action potentials in cultured murine dorsal root ganglion cells. Neurosci. Lett. 1998, 240, 93–96. [Google Scholar] [CrossRef]
- Bjordal, J.M.; Lopes-Martins, R.A.; Iversen, V.V. A randomised, placebo controlled trial of low level laser therapy for activated Achilles tendinitis with microdialysis measurement of peritendinous prostaglandin E2 concentrations. Br. J. Sports Med. 2006, 40, 76–80, discussion 76–80. [Google Scholar] [CrossRef] [Green Version]
- Chow, R.; Armati, P.; Laakso, E.L.; Bjordal, J.M.; Baxter, G.D. Inhibitory effects of laser irradiation on peripheral mammalian nerves and relevance to analgesic effects: A systematic review. Photomed. Laser Surg. 2011, 29, 365–381. [Google Scholar] [CrossRef] [PubMed]
- Pukall, C.F.; Strigo, I.A.; Binik, Y.M.; Amsel, R.; Khalifé, S.; Bushnell, M.C. Neural correlates of painful genital touch in women with vulvar vestibulitis syndrome. Pain 2005, 115, 118–127. [Google Scholar] [CrossRef] [PubMed]
- Puta, C.; Schulz, B.; Schoeler, S.; Magerl, W.; Gabriel, B.; Gabriel, H.H.; Miltner, W.H.; Weiss, T. Somatosensory abnormalities for painful and innocuous stimuli at the back and at a site distinct from the region of pain in chronic back pain patients. PLoS ONE 2013, 8, e58885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laakso, E.L.; Cramond, T.; Richardson, C.; Galligan, J.P. Plasma ACTH and & β-endorphin levels in response to low level laser therapy (LLLT) for myofascial trigger points. Laser Ther. 1994, 6, 133–141. [Google Scholar] [CrossRef] [Green Version]
- Sadownik, L.A. Etiology, diagnosis, and clinical management of vulvodynia. Int. J. Womens Health 2014, 6, 437–449. [Google Scholar] [CrossRef] [Green Version]
- Roldán-Jiménez, C.; Pérez-Cruzado, D.; Neblett, R.; Gatchel, R.; Cuesta-Vargas, A. Central Sensitization in Chronic Musculoskeletal Pain Disorders in Different Populations: A Cross-Sectional Study. Pain Med. 2020, 21, 2958–2963. [Google Scholar] [CrossRef]
- Niemz, M.H. Laser-Tissue Interactions; Springer: Berlin/Heidelberg, Germany, 2007; Volume 322. [Google Scholar]
- Valent, A. Management of chronic Achilles tendinopathy with High Intensity Laser Therapy (HILT) and eccentric exercises. Energy Health. 2014. Available online: https://www.asalaser.com/sites/default/files/ricerca/documenti/management_chronic_achilles_tendinopathy_hilt.pdf (accessed on 30 February 2022).
- Baxter, G.D. Therapeutic Lasers: Theory and Practice; Churchill Livingstone: Edinburgh, NY, USA, 1994. [Google Scholar]
- Wu, X.; Moges, H.; DeTaboada, L.; Anders, J. Comparison of the effects of pulsed and continuous wave light on axonal regeneration in a rat model of spinal cord injury. Lasers Med. Sci. 2012, 27, 525–528. [Google Scholar] [CrossRef]
- Ilic, S.; Leichliter, S.; Streeter, J.; Oron, A.; DeTaboada, L.; Oron, U. Effects of power densities, continuous and pulse frequencies, and number of sessions of low-level laser therapy on intact rat brain. Photomed. Laser Surg. 2006, 24, 458–466. [Google Scholar] [CrossRef]
- Denegar, C.R.; Saliba, E.; Saliba, S. Therapeutic Modalities for Musculoskeletal Injuries, 4th ed.; Human Kinetics, Inc.: Champaign, IL, USA, 2015; pp. 265–272. [Google Scholar]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef]
- Dworkin, R.H.; Turk, D.C.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Katz, N.P.; Kerns, R.D.; Stucki, G.; Allen, R.R.; Bellamy, N.; et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005, 113, 9–19. [Google Scholar] [CrossRef]
- Pukall, C.F.; Bergeron, S.; Brown, C.; Bachmann, G.; Wesselmann, U. Recommendations for Self-report Outcome Measures in Vulvodynia Clinical Trials. Clin. J. Pain 2016, 33, 756–765. [Google Scholar] [CrossRef] [PubMed]


| Variables | Criteria |
|---|---|
| Population | Inclusion: -Vulvodynia population: studies involving women with vulvodynia or superficial dyspareunia. -Chronic primary musculoskeletal pain population: Eligible studies comprised (1) nonspecific chronic low back pain, (2) neck pain, or (3) myofascial pain and myofascial trigger point pain. |
| Exclusion: -Vulvodynia population: studies involving minor women, pregnant women, women who have undergone organ or bone marrow transplants, or women with other pelvic pain conditions, such as chronic pelvic pain different than vulvodynia, endometriosis, sexually transmitted infections, other vulvovaginal infections, cancer, dermatologic conditions, genitourinary syndrome of menopause (including vulvo-vaginal atrophy), or deep dyspareunia. -Chronic primary musculoskeletal pain population: studies involving participants with widespread musculoskeletal pain (e.g., fibromyalgia), systemic illness/inflammatory condition (e.g., rheumatoid arthritis), or headache. Excluded trials were those also examining patients with low back pain due to specific pathological entities including: (1) specific spinal pathology, (i.e., spondylosis, infection, tumor, osteoporosis, fracture including spondylolisthesis), structural deformity (including scoliotic deformities), inflammatory disorder, or (2) neurological encroachment (radicular or cauda-equina syndrome). * | |
| Intervention | Studies evaluating HILT therapy as the primary intervention were included. |
| Comparator | Studies including co-interventions were allowed if applied equally to both laser and control groups. |
| Outcomes | (1) Pain intensity (e.g., pain during intercourse), (2) Functional disability (e.g., sexual function), (3) Participant’s perceived improvement. We also looked at adverse events (worsening of pain, dropouts). |
| Timing | There were no restrictions based on the length of follow-up of outcomes. |
| Setting | There were no restrictions based on type of setting. |
| Design | Given the limited literature available on the effectiveness of laser treatment in women with vulvodynia, randomized controlled trials (RCTs), prospective and retrospective cohorts, case reports, and study protocols were included in the review. Only RCTs were included for the musculoskeletal population. |
| Language | There were no language restrictions. |
| Studies | Sample Size: N Total, Gender (M/F) | Mean Age (Years) | Study Groups | Outcomes | Time Points | Relevant Results |
|---|---|---|---|---|---|---|
| Vestibulodynia | ||||||
| Leclair et al., 2007 [34] | 37 0/37 | 33 | (1) HILT (2) HILT then surgery (3) Surgery then HILT Comparator: N/A | 17-item survey designed by the authors | 2.8 yFU (1–6) | 68% of participants reported a decrease in the pain associated with vestibulodynia after HILT treatment. 63% expressed satisfaction with HILT treatment, and 38% stated that they would recommend laser therapy to a friend with the same problem. |
| Nonspecific Chronic Low Back Pain | ||||||
| Abdelbasset et al., 2020 [45] | 35 22/13 | 40 HILT 39 SL | (1) HILT + EX (2) SL + EX Comparator: SL | VAS, ODI PDI | Pre Post | Significant improvements in pain and function were observed in the HILT + EX group, whereas the SL group showed no significant changes. Comparison between the groups post-intervention: The HILT + EX group scored significantly better in comparison to the SL + EX group for pain and function. |
| Abdelbasset et al., 2020 [44] | 60 42/18 | 32 LLLT 34 HILT 33 EX | (1) HILT + EX (2) LLLT + EX (3) EX Comparators: (1) LLLT Infrared, 850 nm laser with 800 mW power, 30 min/session, delivering 1200 J (2) EX home exercise training: strengthening exercises for back and abdominal muscles, stretching exercises for back muscles, at least twice per week | VAS ODI | Pre Post | Significant improvements were observed in the HILT + EX and LLLT + EX groups in both pain and function, whereas the EX group showed no significant changes. Comparison between the three groups post-intervention: a significant difference in all outcome measures. Comparison between the LLLT + EX and HILT + EX groups post-intervention: no significant differences through post hoc analysis. |
| Abdelbasset et al., 2021 [46] | 51 Nr | 36 HILT 36 EMF 37 EX | (1) HILT + EX (2) EMF + EX (3) EX Comparators: (1) EMF: 30 Hz pulse frequency, for 30 min/session, delivering 14 µT (2) EX: home exercise program: abdominal, back, pelvic muscle stretching, flexibility, mobility and strengthening, 3 x/week | VAS, MODQ, PDI | Pre Post | Significant improvements were observed in the HILT + EX and EMF + EX groups in both pain and function, whereas the EX group showed no significant changes. Comparison between the groups post-intervention: The HILT + EX group scored significantly better in comparison to the EMF + EX group for pain and function. Within-group percent of change for pain and function were greater in the HILT + EX group when compared to the EMF + EX group. |
| Alayat et al., 2014 [35] | 72 72/0 | 33 | (1) HILT + EX (2) SL + EX (3) HILT Comparator: SL | VAS, RDQ, MODQ | Pre, Post, 12 wFU | Significant improvements in both pain and function were observed in all 3 groups post-treatment and the results remained consistent at 12 w. Comparison between the groups post-intervention: The HILT + EX group had a larger decrease in pain than the SL + EX group, with the smallest effect experienced by the HILT group, at both 4 w and 12 w. HILT + EX showed a higher improvement in functional outcomes than SL + EX, while no significant difference was found between SL + EX and HILT alone. |
| Basford, 1999 [38] | 61 31/28 | 48 HILT, 48 SL | (1) HILT (2) SL Comparator: SL | VAS, ODI | Pre, Post, 4 wFU | Significant improvements in pain and function were observed in both groups. Comparison between the groups post-intervention: The HILT group scored significantly better in comparison to the SL group for pain and function. |
| Choi, 2017 [39] | 20 Nr | 48 HILT, 47 CPT | (1) HILT+ CPT (2) CPT Comparator: CPT: 20 min; hot pack, 15 min. interference wave and 5 min; deep heat injection using ultrasonic waves 3 times per week for 4 weeks. | VAS, ODI | Pre, Post | Significant improvements in pain and function were observed in both groups. Comparison between the groups post-intervention: The HILT + CPT group scored significantly better in comparison to the CPT group for both pain and function. |
| Conte, 2009 [40] | 56 Nr | Nr (range 18–65) | (1) HILT + EX (2) EX Comparator: EX: back school (upper and lower limb stretches, Klapp kneeling position, costal and diaphragm ventilation, muscle strengthening, exercises in front of the mirror to find neutral posture) | VAS, MODQ | Pre, Post | Significant improvements in pain and function were observed in both groups. Comparison between the groups post-intervention: The HILT + EX group scored significantly better in comparison to the EX group for pain and function. |
| Fiore, 2011 [42] | 30 11/19 | 51 | (1) HILT (2) US Comparator: US: 2 W/cm2 for 10 min. | VAS, ODI | Pre, Post | Significant improvements in pain and function were observed in both groups. Comparison between the groups post-intervention: The HILT group scored significantly better in comparison to the US group for pain and function. |
| Gocevska, 2019 [43] | 54 29/25 | 55 HILT | (1) HILT + EX (2) US + EX Comparator: US: 0.5 W/cm2 for 5 min. | NRS, ODI | Pre, Post, 12 wFU | Significant improvements in pain and function were observed in both groups post-treatment and the results remained consistent at 12 w. Comparison between the groups post-intervention: The HILT + EX group scored significantly better in comparison to US + EX for pain and function at both post-treatment and 12 w. |
| Neck Pain | ||||||
| Alayat et al., 2016 [36] | 60 60/0 | 36 HILT, 25 SL | (1) HILT + EX (2) SL + EX Comparator: SL | VAS, NDI | Pre, Post | Significant improvements in pain and function were observed in both groups. Comparison between the groups post-intervention: The HILT + EX group scored significantly better in comparison to the SL + EX group for both pain and function. |
| Alayat, 2017 [37] | 75 75/0 | 46 | (1) HILT (MLS) +EX (2) LLLT + EX (3) SL + EX Comparators: (1) SL (2) LLLT Infrared, 830 nm laser with 800 mW power, 30 min/session, delivering 300 J | VAS, NDI | Pre, Post | Significant improvements in pain and function were observed in all 3 groups. Comparison between the three groups post-intervention: The greatest improvement in both pain and function was seen in the HILT (MLS) + EX group, followed by LLLT + EX, then SL + EX. |
| Myofascial Pain Syndrome | ||||||
| Dundar, 2015 [41] | 76 0/76 | 40 HILT 38 SL | (1) HILT + EX (2) SL + EX Comparator: SL | VAS, NDI | Pre, 1 wFU, 9 wFU | Significant improvements in pain and function were observed in both groups. Comparison between the groups post-intervention: The HILT + EX group showed a greater improvement in pain and function than the SL + EX group. |
| Myogenic Temporomandibular Joint Disorder | ||||||
| Ekici et al., 2021 [47] | 76 Nr | 32 HILT 30 SL | (1) HILT (2) SL Comparator: SL | VAS, JFLS-20 | Pre, 1 wFU, 9 wFU | Significant improvements in pain and function were observed in both groups. Comparison between the groups post-intervention: Percentage changes yielded a significantly greater improvement in pain and function in the HILT group in comparison to the SL group. |
| Study | Type of Laser Wavelength (nm) Application Mode | Peak Power Ppeak (Pulsed); N/A for CW | Frequency (Hz)/ Pulse Duration (µs) | Energy per Pulse (E) Ppeak × t (laser Pulse Duration) | Energy Dose (J) per Point/ per All Points/ per Scanning/ per Treatment/ Accumulated Energy from All Sessions (J) | Treatment Time per Point/ per ST (All Points)/ per SC per Session/ no. Sessions/ no. Sessions per Week/Total No. Weeks | Average Power (Pulsed) or Output Power (CW)/ Scanning Phase | Average Power (Pulsed) or Output Power (CW) ST per All Points/ ST per Point | Area (cm2)/ Spot Size (cm2) | Average Power Density (mW/cm2) SC Scanning | Average Power Density (mW/cm2) ST per All Points/ ST per Point | Dose Density (J/cm2) SC | Dose Density (J/cm2) ST per All Points/ ST per Point |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Leclair et al., 2007 [33] | Pulsed KTP-Nd:YAG 532 Nr | Nr | Nr/ 15 ms | Nr | Nr | 2.84 sessions (range 1–8) | Nr | Nr | Nr 0.4 | Nr | Nr | 10 (Nr if SC or ST) | |
| Abdelbasset et al., 2020 [44] | Pulsed- Nd:YAG 1064 SC | Nr | Nr/Nr | Nr | N/A/ N/A/ 300 first 2 weeks 120–150 next 4 weeks/ 3240–3600 | N/A/ N/A/ 75 s first 2 weeks 30 s next 4 weeks/ 18 sessions 3 x/week 6 weeks | (6–12 W) 8 W first 2 weeks 6 W next 4 weeks | N/A | 30 N/A | 200–266.7 | N/A | 6 | N/A |
| Abdelbasset et al., 2020 [43] | Pulsed Ga-Ar 1064 SC | Nr | Nr/Nr | Nr | N/A/ N/A/ 1200/ 2800 | N/A/ N/A/ 15 min 24 sessions 2 x/week 12 weeks | (12 W) 1.33 | N/A | Nr/ N/A | Nr | N/A | 150 | N/A |
| Abdelbasset et al., 2021 [45] | Nd: YAG 1064 nm Pulsed B | 3 kW | 10–40/ 120 | 0.35 J | 25/ 200/ 2800/ 3000/ 48,000 | 14 s/ 112 s/ 788 s/ 15 min. 16 sessions 2 x/week 8 weeks | (10.5 W) 3.55 SC | 1.79 W ST all points/ 1.79 W ST per point | 60 0.2 | 220 | 1118 ST 8950 ST point | 0.61; 0.71; 0.81 SC | 125 ST all points/ 0.61 ST per point |
| Alayat et al., 2014 [34] | Pulsed- Nd:YAG 1064 B | 3 kW | 10–40/ 120–150 | 0.36 J– 0.45 J | 25/ 200/ 2800/ 3000/ 36,000 | 14 s/ 112 s/ 788 s/ 15 min. 12 sessions 3 x/week 4 weeks | (3.6–18 W) 3.55 SC | 1.79 W ST all points/ 1.79 W ST per point | Nr 0.2 | ? SC | 1118 ST 8950 ST point | 0.61; 0.71; 0.81 SC | 125 ST all points/ 0.61 ST per point |
| Alayat et al., 2016 [35] | Pulsed- Nd:YAG 1064 B | 3 kW | 10–40/ 120–150 | 0.36 J– 0.45 J | 25/ 200/ 2050/ 2250/ 27,000 | 14 s/ 112 s/ 788 s/ 15 min. 12 sessions 2 x/weeks 6 weeks | (3.6–18 W) 2.6 SC | 1.79 ST all points/ 1.79 ST per point | 75 0.2 | 34.7 SC | 1118 ST 8950 ST point | 27.3 SC | 125 ST all points/ 0.51 ST per point |
| Alayat et al., 2017 [36] | Pulsed and CW Ga-Al-Ar 808–905 B | 1000 mW (CW) 25 W (Pulsed) Continuous and pulsed synchronously | N/A for CW 1500/Nr | Nr | 12.6/ 100.8/ 300/ 400.8/ 801.6 | 30 s/ 240 s/ 256 s/ 8 min 16 s/ 12 sessions/ 2 x/week 6 weeks | 0.5 W CW 0.054 W (54 mW)Pulsed Nr SC | 0.054–0.5 all points/ 0.054–0.5 per point | 75 3.14 | 0.72–6.67 SC | 2.15–19.9 ST 17.2–159.24 ST point | 4 SC | 4 ST (Nr if per all points or per point) |
| Basford et al., 1999 [37] | CW- Nd:YAG 1060 ST | N/A | N/A | N/A | 239/ 1912/ N/A 1912/ 22,944 | 90 s/ 360 s/ N/A 6 min. 12 sessions 3 x/weeks 4 weeks | (N/A–cont.) N/A | 5.31 W ST all points/ 2.66 W ST per point | N/A 4.9 | N/A | 14.75 ST 542 ST point | N/A | 48.77 ST all points/ 48.9 ST per point |
| Choi et al., 2017 [38] | Nr 1064 Nr Nr | Nr | Nr/Nr | Nr | Nr/ Nr | 10 min. 12 sessions 3 x/weeks 4 weeks | Nr | Nr | Nr | Nr | Nr | 1.378 (Nr if SC or ST) | |
| Conte et al., 2009 [39] | Pulsed Nd:YAG Nr B | Nr | Nr/Nr | Nr/Nr | 18–20/ 72–80/ 3000/ 3071–3080/ Nr/ | Nr | Nr | Nr/Nr | Nr Nr | Nr | Nr Nr | 0.66; 0.71; 0.76 SC | 0.66 (Nr if per point or all points) |
| Dundar et al., 2015 [40] | Pulsed- Nd:YAG 1064 B | 3.8 kW | 10–40/ 120–150 | 0.456 J– 0.57 J | 10/ 60/ 1000/ 1060/ 15,900 | 6 s/ 18 s/ 882 s/ 15 min. 15 sessions 5 x/weeks 3 weeks | (4.56–22.8 W) 1.13 SC | 3.33 ST all points 1.67 ST per point | 100 0.2 | 11.3 SC | 2775 ST 8 350 ST point | 0.36; 0.41; 0.51 SC | 50 ST all points/ 0.61 ST per point |
| Ekici et al., 2021 [46] | Pulsed Nd:YAG 1064 B | 3 kW | 10–40/ 120–150 | 0.36 J– 0.45 J | 5.51/ 33.1/ 996/ 1029.2/ 15,438 | 6 s/ 36 s/ 864 s/ 15 min 15 sessions 5 x/week 3 weeks | 10.5 W 1.15 SC | 0.92 ST all points 0.92 ST per point | 100 0.2 | 11.5 SC | 575 ST 4600 ST point | 0.36; 0.41; 0.51 SC | 27.6 ST all points/ 0.61 ST per point |
| Fiore et al., 2011 [41] | Pulsed- Nd:YAG 1064 B | 1 kW | Nr/ less than 150 | Nr | Nr/ Nr/ Nr/ 2600/ 39,000 | Nr/ Nr/ Nr/ 10 min. 15 sessions 5 x/weeks 3 weeks | (6 W) ? SC | ? ST all points/ ? ST per point | 100 0.2 | Nr | Nr | 0.71 (for all treatments Nr values of SC and ST phase) | |
| Gocevska et al., 2019 [42] | CW Nr 940 nm SC | Nr | Nr/ Nr | N/A | N/A/ N/A/ 2400/ 2400/ 24,000 | N/A/ N/A/ 15 min/ 15 min 10 sessions 5 x/weeks 2 weeks | 4 W | N/A | Nr N/A | Nr | N/A | 1.5 SC | N/A |
| Studies | Comparison Groups Group 1 vs. Group 2 | Outcome Measures | Time Point | Experimental Group 1 Mean ± SD | Comparator Group 2 Mean ± SD | Effect Size | 95% Confidence Interval |
|---|---|---|---|---|---|---|---|
| Abdelbasset et al., 2020 [44] | HILT + EX vs. SL + EX | VAS | Pre | 6.7 ± 1.6 | 6.9 ± 1.5 | N/A | N/A |
| HILT + EX vs. SL + EX | VAS | Post | 3.7 ± 1.1 | 6.1 ± 1.3 | 1.998 | 1.147–2.758 | |
| HILT + EX vs. SL + EX | ODI | Pre | 39.8 ± 14.3 | 38.6 ± 12.9 | N/A | N/A | |
| HILT + EX vs. SL + EX | ODI | Post | 19.3 ± 6.7 | 35.4 ± 11.5 | 1724 | 0.913–2.456 | |
| HILT + EX vs. SL + EX | PDI | Pre | 33.5 ± 10.7 | 34.3 ± 11.2 | N/A | N/A | |
| HILT + EX vs. SL + EX | PDI | Post | 24.7 ± 7.6 | 30.8 ± 9.8 | 0.698 | 0.000–1.364 | |
| Abdelbasset et al., 2020 [43] | HILT + EX vs. LLLT + EX | VAS | Pre | 6.3 ± 1.9 | 6.5 ± 1.7 | N/A | N/A |
| HILT + EX vs. LLLT + EX | VAS | Post | 3.5 ± 0.8 | 3.4 ± 0.9 | 0.117 | −0.505 to 0.735 | |
| HILT + EX vs. LLLT + EX | ODI | Pre | 37.3 ± 11.3 | 36.5 ± 12.7 | N/A | N/A | |
| HILT + EX vs. LLLT + EX | ODI | Post | 18.5 ± 7.2 | 17.8 ± 6.4 | 0.103 | −0.519 to 0.721 | |
| HILT + EX vs. EX | VAS | Pre | 6.3 ± 1.9 | 6.6 ± 1.6 | N/A | N/A | |
| HILT + EX vs. EX | VAS | Post | 3.5 ± 0.8 | 5.9 ± 1.8 | 1.723 | 0.967–2.411 | |
| HILT + EX vs. EX | ODI | Pre | 37.3 ± 11.3 | 36.2 ± 12.3 | N/A | N/A | |
| HILT + EX vs. EX | ODI | Post | 18.5 ± 7.2 | 34.6 ± 11.8 | 1.852 | 1.078–2.551 | |
| Abdelbasset et al., 2021 [45] | HILT + EX vs. EMF + EX | VAS | Pre | 7.4 ± 2.2 | 7.2 ± 1.9 | N/A | N/A |
| HILT + EX vs. EMF + EX | VAS | Post | 3.2 ± 1.2 | 5.1 ± 1.7 | 1.291 | 0.525–1.997 | |
| HILT + EX vs. EMF + EX | MODQ | Pre | 42.4 ± 12.7 | 41.8 ± 11.8 | N/A | N/A | |
| HILT + EX vs. EMF + EX | MODQ | Post | 23.6 ± 6.5 | 29.3 ± 8.7 | 0.742 | 0.031–1.419 | |
| HILT + EX vs. EMF + EX | PDI | Pre | 34.8 ± 11.4 | 34.5 ± 10.9 | N/A | N/A | |
| HILT + EX vs. EMF + EX | PDI | Post | 22.6 ± 7.2 | 27.2 ± 9.5 | 0.546 | −0.151 to 1217 | |
| HILT + EX vs. EX | VAS | Pre | 7.4 ± 2.2 | 6.8 ± 2.1 | N/A | N/A | |
| HILT + EX vs. EX | VAS | Post | 3.2 ± 1.2 | 6.3 ± 1.8 | 2.027 | 1.158–2.799 | |
| HILT + EX vs. EX | MODQ | Pre | 42.4 ± 12.7 | 40.5 ± 12.3 | N/A | N/A | |
| HILT + EX vs. EX | MODQ | Post | 23.6 ± 6.5 | 35.7 ± 10.6 | 1.376 | 0.599–2.088 | |
| HILT + EX vs. EX | PDI | Pre | 34.8 ± 11.4 | 33.9 ± 10.7 | N/A | N/A | |
| HILT + EX vs. EX | PDI | Post | 22.6 ± 7.2 | 30.5 ± 10.2 | 0.895 | 0.170–1.577 | |
| Alayat et al., 2014 [34] | HILT + EX vs. SL + EX | VAS | Pre | 8.36 ± 0.95 | 8.21 ± 1.1 | N/A | N/A |
| HILT + EX vs. SL + EX | VAS | Post | 2.04 ± 0.83 | 3.21 ± 0.83 | 1.410 | 0.801–2.018 | |
| HILT + EX vs. SL + EX | VAS | 12 wFu | 2.64 ± 1.25 | 3.71 ± 1.30 | 0.840 | 0.272–1.409 | |
| HILT + EX vs. HILT | VAS | Pre | 8.36 ± 0.95 | 8.35 ± 0.88 | N/A | N/A | |
| HILT + EX vs. HILT | VAS | Post | 2.04 ± 0.83 | 4.15 ± 2.03 | 1.454 | 0.81–2.097 | |
| HILT + EX vs. HILT | VAS | 12 wFu | 2.64 ± 1.25 | 5.65 ± 1.04 | 2.577 | 1.806–3.349 | |
| HILT + EX vs. SL + EX | RDQ | Pre | 15.46 ± 1.17 | 15.63 ± 1.56 | N/A | N/A | |
| HILT + EX vs. SL + EX | RDQ | Post | 4.43 ± 1.28 | 5.75 ± 0.99 | 1.142 | 0.554–1.73 | |
| HILT + EX vs. SL + EX | RDQ | 12 wFu | 5.5 ± 1.17 | 6.92 ± 0.78 | 1.407 | 0.798–2.015 | |
| HILT + EX vs. HILT | RDQ | Pre | 15.46 ± 1.17 | 15.4 ± 1.19 | N/A | N/A | |
| HILT + EX vs. HILT | RDQ | Post | 4.43 ± 1.28 | 6.35 ± 1.6 | 1.351 | 0.717–1.986 | |
| HILT + EX vs. HILT | RDQ | 12 wFu | 5.5 ± 1.17 | 7.35 ± 1.5 | 1.405 | 0.766–2.044 | |
| HILT + EX vs. SL + EX | MODQ | Pre | 34.11 ± 3.14 | 34.5 ± 2.93 | N/A | N/A | |
| HILT + EX vs. SL + EX | MODQ | Post | 13.9 ± 3.83 | 16.41 ± 3.01 | 0.722 | 0.159–1.285 | |
| HILT+EX vs. SL+EX | MODQ | 12 wFu | 15.14 ± 4.3 | 18.75 ± 3.07 | 0.954 | 0.379–1.529 | |
| HILT+EX vs. HILT | MODQ | Pre | 34.11 ± 3.14 | 35.55 ± 3.62 | N/A | N/A | |
| HILT+EX vs. HILT | MODQ | Post | 13.9 ± 3.83 | 17.25 ± 3.14 | 0.941 | 0.337–1.545 | |
| HILT+EX vs. HILT | MODQ | 12 wFu | 15.14 ± 4.3 | 19.05 ± 2.96 | 1.028 | 0.418–1.637 | |
| Alayat et al., 2016 [35] | HILT + EX vs. SL + EX | VAS | Pre | 8.00 ± 0.79 | 7.83 ± 0.80 | N/A | N/A |
| HILT + EX vs. SL + EX | VAS | Post | 1.77 ± 0.73 | 2.83 ± 0.79 | 1.394 | 0.829–1.958 | |
| HILT + EX vs. SL + EX | NDI | Pre | 45.87 ± 5.12 | 47.97 ± 3.29 | N/A | N/A | |
| HILT + EX vs. SL + EX | NDI | Post | 7.80 ± 1.65 | 9.86 ± 1.48 | 1.314 | 0.756–1.872 | |
| Alayat et al., 2017 [36] | HILT(MLS) + EX vs. LLLT + EX | VAS | Pre | 39.76 ± Nr | 37.88 ± Nr | N/A | N/A |
| HILT(MLS) + EX vs. LLLT + EX | VAS | Post | 19.58 ± Nr | 38.90 ± Nr | Insufficient data | Insufficient data | |
| HILT(MLS) + EX vs. LLLT + EX | NDI | Pre | 37.80 ± Nr | 36.08 ± Nr | N/A | N/A | |
| HILT (MLS) + EX vs. LLLT + EX | NDI | Post | 17.82 ± Nr | 37.18 ± Nr | Insufficient data | Insufficient data | |
| HILT(MLS) + EX vs. SL + EX | VAS | Pre | 39.76 ± Nr | 36.36 ± Nr | N/A | N/A | |
| HILT(MLS) + EX vs. SL + EX | VAS | Post | 19.58 ± Nr | 55.52 ± Nr | 2.223 * | −1.303 to 5.748 * | |
| HILT(MLS) + EX vs. SL + EX | NDI | Pre | 37.80 ± Nr | 40.12 ± Nr | N/A | N/A | |
| HILT(MLS) + EX vs. SL + EX | NDI | Post | 17.82 ± Nr | 59.00 ± Nr | 2.63 * | −1.155 to 6.416 * | |
| Basford et al., 1999 [37] | HILT vs. SL | VAS | Pre | 35.2 ± Nr | 37.4 ± Nr | N/A | N/A |
| HILT vs. SL | VAS | Post | 17.1 ± Nr | 32.8 ± Nr | Insufficient data | Insufficient data | |
| HILT vs. SL | VAS | 4 wFu | 19.1 ± Nr | 35.1 ± Nr | Insufficient data | Insufficient data | |
| HILT vs. SL | ODI | Pre | 21 ± Nr | 26 ± Nr | N/A | N/A | |
| HILT vs. SL | ODI | Post | 13.3 ± Nr | 22.6 ± Nr | Insufficient data | Insufficient data | |
| HILT vs. SL | ODI | 4 wFu | 14.7 ± Nr | 22.9 ± Nr | Insufficient data | Insufficient data | |
| Choi et al., 2017 [38] | HILT + CPT vs. CPT | VAS | Pre | 7.0 ± 0.8 | 7.0 ± 0.8 | N/A | N/A |
| HILT + CPT vs. CPT | VAS | Post | 3.4 ± 0.8 | 6.2 ± 1.4 | 2.714 | 1.69–3.738 | |
| HILT+CPT vs. CPT | ODI | Pre | 31.6 ± 11.5 | 33.1 ± 13.0 | N/A | N/A | |
| HILT+CPT vs. CPT | ODI | Post | 19.0 ± 10.6 | 29.6 ± 10.7 | 0.997 | 0.197–1.797 | |
| Conte et al., 2009 [39] | HILT + EX vs. EX | VAS | Pre | 60 ± 19.5 | 63.32 ± 16.8 | N/A | N/A |
| HILT + EX vs. EX | VAS | Post | 27.9 ± 15 | 45.3 ± 14.3 | 1.187 | 0.619–1.755 | |
| HILT + EX vs. EX | MODQ | Pre | 21.39 ± 6.9 | 23.12 ± 6.98 | N/A | N/A | |
| HILT + EX vs. EX | MODQ | Post | 9.6 ± 5.98 | 16.6 ± 7.38 | 1.042 | 0.484–1.6 | |
| Dundar et al., 2015 [40] | HILT + EX vs. SL + EX | VAS at rest | Pre | 5.9 ± 1.4 | 5.7 ± 1.5 | N/A | N/A |
| HILT + EX vs. SL + EX | VAS at rest | 1 wFu | 2.7 ± 1.2 | 4.2 ± 1.6 | 1.063 | 0.579–1.546 | |
| HILT + EX vs. SL + EX | VAS at rest | 9 wFu | 2.6 ± 1.2 | 4.1 ± 1.4 | 1.152 | 0.663–1.64 | |
| HILT + EX vs. SL + EX | NDI | Pre | 32.6 ± 6.6 | 32.9 ± 8.3 | N/A | N/A | |
| HILT + EX vs. SL + EX | NDI | 1 wFu | 21.1 ± 6.3 | 26.6 ± 7.1 | 0.82 | 0.349–1.291 | |
| HILT + EX vs. SL + EX | NDI | 9 wFu | 20.3 ± 6.22 | 26.1 ± 6.7 | 0.898 | 0.423–1.373 | |
| Ekici et al., 2021 [46] | HILT vs. SL | VAS | Pre | 60.9 ± 21.9 | 59.3 ± 20.5 | N/A | N/A |
| HILT vs. SL | VAS | 1 wFu | 27.7 ± 19 | 56.8 ± 19.6 | 1.51 | 0.96–2.02 | |
| HILT vs. SL | VAS | 9 wFu | 26.3 ± 24 | 55 ± 18.8 | 1.33 | 0.8–1.83 | |
| HILT vs. SL | JFLS-20 | Pre | 72.15 ± 47.16 | 53.50 ± 33.86 | N/A | N/A | |
| HILT vs. SL | JFLS-20 | 1 wFu | Nr | Nr | Insufficient data | Insufficient data | |
| HILT vs. SL | JFLS-20 | 9 wFu | Nr | Nr | Insufficient data | Insufficient data | |
| Fiore et al., 2011 [41] | HILT vs. US | VAS | Pre | 7 ± Nr | 7 ± Nr | N/A | N/A |
| HILT vs. US | VAS | Post | 3 ± Nr | 4 ± Nr | Insufficient data | Insufficient data | |
| HILT vs. US | ODI | Pre | 28 ± Nr | 28 ± Nr | N/A | N/A | |
| HILT vs. US | ODI | Post | 12 ± Nr | 16 ± Nr | Insufficient data | Insufficient data | |
| Gocevska et al., 2019 [42] | HILT + EX vs. US + EX | NRS | Pre | 7.22 ± 8.85 | 6.96 ± 0.94 | N/A | N/A |
| HILT + EX vs. US + EX | NRS | Post | 2.11 ± 0.8 | 4.26 ± 1.06 | 2.290 | 1.603–2.976 | |
| HILT + EX vs. US + EX | NRS | 12 wFU | 1.89 ± 0.64 | 4.89 ± 0.85 | 3.987 | 3.065–4.909 | |
| HILT + EX vs. US + EX | ODI | Pre | 44.33 ± 3.92 | 45.22 ± 3.91 | N/A | N/A | |
| HILT + EX vs. US + EX | ODI | Post | 16.29 ± 4.85 | 26.74 ± 4.51 | 3.987 | 1.271–3.192 | |
| HILT + EX vs. US + EX | ODI | 12 wFU | 15.89 ± 4.58 | 26.63 ± 3.73 | 2.571 | 1.85–3.292 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Starzec-Proserpio, M.; Grigol Bardin, M.; Fradette, J.; Tu, L.M.; Bérubè-Lauzière, Y.; Paré, J.; Carroll, M.-S.; Morin, M. High-Intensity Laser Therapy (HILT) as an Emerging Treatment for Vulvodynia and Chronic Musculoskeletal Pain Disorders: A Systematic Review of Treatment Efficacy. J. Clin. Med. 2022, 11, 3701. https://doi.org/10.3390/jcm11133701
Starzec-Proserpio M, Grigol Bardin M, Fradette J, Tu LM, Bérubè-Lauzière Y, Paré J, Carroll M-S, Morin M. High-Intensity Laser Therapy (HILT) as an Emerging Treatment for Vulvodynia and Chronic Musculoskeletal Pain Disorders: A Systematic Review of Treatment Efficacy. Journal of Clinical Medicine. 2022; 11(13):3701. https://doi.org/10.3390/jcm11133701
Chicago/Turabian StyleStarzec-Proserpio, Małgorzata, Marcela Grigol Bardin, Julie Fradette, Le Mai Tu, Yves Bérubè-Lauzière, Josianne Paré, Marie-Soleil Carroll, and Mélanie Morin. 2022. "High-Intensity Laser Therapy (HILT) as an Emerging Treatment for Vulvodynia and Chronic Musculoskeletal Pain Disorders: A Systematic Review of Treatment Efficacy" Journal of Clinical Medicine 11, no. 13: 3701. https://doi.org/10.3390/jcm11133701
APA StyleStarzec-Proserpio, M., Grigol Bardin, M., Fradette, J., Tu, L. M., Bérubè-Lauzière, Y., Paré, J., Carroll, M.-S., & Morin, M. (2022). High-Intensity Laser Therapy (HILT) as an Emerging Treatment for Vulvodynia and Chronic Musculoskeletal Pain Disorders: A Systematic Review of Treatment Efficacy. Journal of Clinical Medicine, 11(13), 3701. https://doi.org/10.3390/jcm11133701






