Abstract
Tinea gladiatorum (TG) is a fungal skin infection that occurs among wrestlers and other contact sport athletes with a varied prevalence rate. The most common causative factor responsible as well for local outbreaks of the infection is an anthropophilic dermatophyte species—Trichophyton tonsurans (T. tonsurans). The purpose of this study was to gather current data about TG, including epidemiology, possible diagnosing methods, clinical features, treatment approaches, and potential prevention techniques. We also performed a systematic review of studies describing TG incidence. The prevalence of the disease varied from 2.4% up to 100%. That wide range of variability forces medical practitioners to update knowledge about TG and points to the fact that it still may be a diagnostic and therapeutic challenge. Spreading awareness among athletes and trainers is one of the most important preventive steps.
1. Introduction
Tinea gladiatorum (TG; trichophytosis gladiatorum; tinea gladiatorum) is the most widespread fungal skin infection among contact sports athletes and the second most common skin infection in this group in general, after herpes gladiatorum (HSV infection) [,]. Specific factors such as skin-to-skin contact during training and competition, exposure to mechanical trauma (abrasions and cuts), and often asymptomatic course of the disease may increase the risk of contamination and local outbreaks [,]. According to a study conducted by Iranian scientists [], the most frequently identified pathogen causing TG was Trichophyton tonsurans (T. tonsurans) (92%) followed by Trichophyton rubrum (T. rubrum) (3.36%) and Trichophyton mentagrophytes (T. mentagrophytes) (1.89%). Kohl et al. [], during the evaluation of association of superficial dermatophytosis and athletic activities, reported that in 84% of the studied wrestling teams in the USA during the 1998–1999 season, at least one athlete was diagnosed to be a T. tonsurans carrier. T. tonsurans is a strongly transmissible, ubiquitous anthropophilic dermatophyte fungus that originated in South-East Asia and Australia. It is a microorganism that invades keratinized tissues [,].
The main issue of this study was to summarize the current knowledge about the epidemiology, diagnosing, clinical features, treatment, and prevention of tinea gladiatorum.
2. Materials and Methods
In this study, we performed a review of the literature concerning tinea gladiatorum incidence according to the PRISMA guidelines []. Three electronic databases (“PubMed”, “Scopus”, and “Web of Science”) were searched on 20 June 2022 for articles of any type published since 1992. The following medical subject heading (MeSH) terms were used: “tinea gladiatorum” OR “fungal infection” OR “dermatophyte” OR “dermatophytosis” OR “tinea corporis” OR “contact sports” OR “Trichophyton tonsurans” AND “wrestler(s)”. After the first search, we gathered 6859 articles. Later on, after removing duplicated articles, we obtained 5853 papers. After the first screening, we found 426 records; however, after a precise review of titles and abstracts and assessment of eligibility (during which all articles that were non-English or not concerning sufficient epidemiological data or concerning other fungi species were excluded immediately from the study), we extracted a total number of 22 elements which were included in our review. The PRISMA flow diagram was constructed (Figure 1). All initially searched articles were imported to Zotero 5.0, AGPL license.
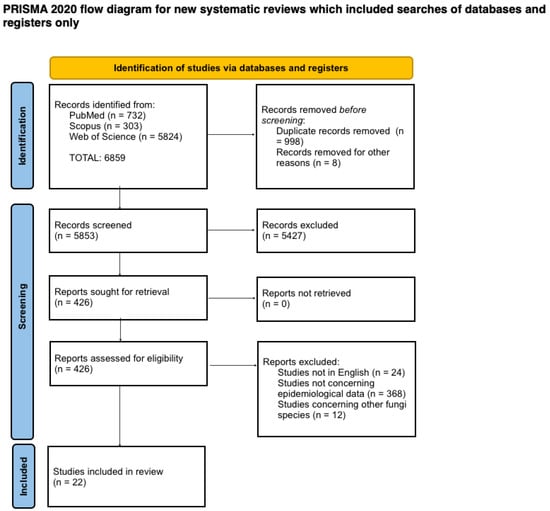
Figure 1.
PRISMA flow diagram.
3. Results
Of all collected articles, 22 records provided quantitative data about TG frequency among contact sports athletes. Results of our research are presented in Table 1. The analysis of the data revealed that the prevalence of dermatophytosis in wrestlers varied from 2.4% in Iran [] up to 100% in the USA [,]. What was underlined by most authors was that T. tonsurans was undoubtedly the pathogen responsible for most cases of the infection.

Table 1.
Tinea gladiatorum (TG) frequency among contact sports athletes.
4. Discussion
4.1. Pathophysiology
T. tonsurans is a microorganism of a filamentous fungi group, dermatophytes (subdivided into seven genera: Trichophyton, Microsporum, Epidermophyton, Paraphyton, Lophophyton, Arthroderma, and Nannizzia), which are keratinophilic and keratinolytic pathogens [,]. Based on their main host species, they are classified as anthropophilic, zoophilic, or geophilic. When involving skin infections, this type is called tinea or dermatophytosis. Many ways of transmission are possible (direct contact with infected humans, animals, or soils or indirectly via contaminated objects) [].
Dermatophytosis, such as TG, concerns the stratum corneum in cases where the skin is occupied []. T. tonsurans as a dermatophyte species is able to adhere to host keratinized tissues and to adjust to the local environment thanks to various fungal enzymes (collagenolytic, elastolytic, and mucolytic; lipases and nucleotidases) and proteins which are regulated by specific, multiple genes. The balance between their activation and repression, depending upon the host factors (such as skin pH), provide optimum conditions for disease development []. Fungal heat shock proteins and transcription factors (e.g., Hfs1) are significant, especially in the first phase of the infection. Thanks to them, pathogens can adapt to the acidic pH of the hosts′ skin, and later on in the course of the infection, it may be gradually altered into alkaline. In this specific environment, keratinolytic proteases operate at maximum efficiency and ensure the continuation of the infectious process [,].
When considering the scalp area, Trichophyton, including T. tonsurans, also infects the hair and hair follicles, which leads to endothrix hyphae invading the hair shaft as well as internalizing into the hair cell and being converted into arthroconidia (spores). They substitute hair cells almost entirely and are visible inside the hair. Sometimes, it leads to hair breaking off at or below the mouth of the follicle, leaving the residual part inside the follicle, which gives an impression of black dots on a smooth, bald background and thus a black-dot ringworm” appearance [,,,].
Molecular tests conducted by Sidrim et al. [] showed a potentially important role of melanin synthesis in T. tonsurans infection. Production of this molecule by fungi may act as an antioxidant that protects its cells from the negative impact of UV rays. It can help the pathogen to survive undamaged, e.g., in lesions that are directly exposed to the sun (on the scalp area) [].
4.2. Epidemiology
Dermatophytic skin infections are one of the most frequent infections worldwide, also among contact sports athletes. Comparing data that we collected during our paper′s preparation, the range of positive mycological test results in groups of wrestlers varied significantly between different countries. The most noticeable dissimilarity was observed among athletes in the USA (results ranged from 4.3% to 100%) [,,,,,,,] and Turkey (from 4.2% to 90.6%) [,,,]. We also noted a diversity among Iranian studies (from 2.4% to 68.3%) [,,,,,]. There are limited data concerning the incidence of TG in other countries—only individual studies have been performed. A research involving French combat sports players showed that 37.4% of the results of mycological tests of the examined group were positive []. A similar study on Spanish athletes detected a fungal infection in 44.1% of analyzed individuals []. The percentage of positive results was relatively higher in Mexican and Swedish investigations (respectively: 57.1% [] and 73.7% []). In 2015, Hiruma et al. [] demonstrated a review of their work results concerning the epidemiology of T. tonsurans infection in Japan. They created a group of a total of 1000 judo wrestlers and tested them for T. tonsurans infection presence. The results showed that 11.5% of combat sports players were positive and 40% of that positive group presented the symptoms of tinea corporis for more than half a year. Moreover, to compare the prevalence of T. tonsurans infection among athletes in other disciplines, they tested 497 students in a university department of sport science—T. tonsurans infection was detected in combat sports players alone. Outcomes of this study indicate the need for rising patient awareness, especially among that specific group.
Bassiri-Jahromi et al. [] in their study of superficial fungal infection in Iranian athletes demonstrated that in almost 4.3% of cases, tinea corporis was present not only among athletes but also among their family members. Thus, during wrestlers’ diagnosing and treatment, the social and domestic dimension of the contagiousness need to be taken into consideration. It concerns especially large families, herded in the crowded living conditions or facing social or financial problems, which stays in line with other authors’ observations [,].
Despite the fact that T. tonsurans is a predominant infectious factor responsible for TG cases, there are also several papers describing the role of other dermatophyte species such as T. mentagrophytes [,]. In 2000, Skorepová et al. [] published a report informing about a case of two patients (wrestlers) with skin lesions diagnosed as TG. The probable primary source of infection was a pet rabbit owned by one of the athlete’s girlfriend, and the disease spread further by skin-to-skin contact. Symptoms of dermatophytosis were also present in four other members of the same wrestling team. T. mentagrophytes was diagnosed as a pathogen responsible for the infection.
It is also worth noticing that T. rubrum appears to be the most common causative agent of dermatophytosis [] overall and yet it is described as the second most frequent pathogen among wrestlers with fungal infections []. Considering the above mentioned evidence, T. rubrum may be considered as a future candidate for a prevalent TG-inducing factor.
4.3. Risk Factors
So far, many risk factors of TG have been identified including, e.g., age, sex, skin type, hereditary factors, and hyperhidrosis []. The group of Shiraki et al. [] in 2006 also described some other variables, such as a failure to wear headgear during combat, a failure to wash clothes at least once a week, and a history of scalp and neck involvement. Several of those assumptions were confirmed by the research of Turkish scientists []. They observed a potential role of not wearing headgear and lack of bedding laundering in local outbreak development. Training conditions are also certainly not without significance. Many athletes practice in tight, enclosed, and humid spaces. On the one hand, it may be a part of endurance training, but alongside increased sweating and risk of skin injury, it may also escalate the chance of skin-to-skin dermatophyte transmission [,].
The relevance of wrestling mat and wrestling hall contamination is an extensively debated factor. Some authors imply that contamination of wrestling mats with T. tonsurans plays a great role in dermatophytosis spread [,]. Constant contact between wrestlers’ feet and mats should point to the lower extremities area as the mostly affected body parts. According to a meta-analysis of TG cases conducted by Kermani et al. [], the trunk, scalp, and face are three predominant disease locations, which would exclude the above mentioned hypothesis.
Nevertheless, colonies of T. tonsurans have been repeatedly isolated from sampled wrestling mats [,]. It is believed that training mats may be the vector of the pathogen but may not be a reservoir if the cleaning routine is proper [].
4.4. Clinical Features
4.4.1. Location
Most lesions on wrestlers are found on the surface of the trunk, head, and neck and on the upper extremities—which are points of contact between competitors—whereas the lower limbs are a rather untypical location [,,]. Historically, the term tinea gladiatorum has been limited to tinea corporis in the trunk area. However, while preparing our study, we collected data describing T. tonsurans infections concerning other body areas of wrestlers, such as the head (tinea capitis), face (tinea faciei) (Figure 2), groins (tinea cruris), feet (tinea pedis), and nails (tinea unguium) [,,].

Figure 2.
Clinical picture of TG—annular lesion with raised borders, slight scaling, and mild erythema. Courtesy of Prof. J. C. Szepietowski.
4.4.2. Lesion Characteristics
Lesions caused by dermatophytes are usually clinically distinctive and can be differentiated by experienced dermatologists. Nevertheless, the clinical picture of dermatophyte infection may differ and depend on the pathogen’s species, the affected anatomic area, and the immunological response of the patient [,]. Taking into consideration all above mentioned evidence, disease manifestation diverges from asymptomatic carriers with no perceptible symptoms to patients presenting acute inflammatory reactions. T. tonsurans infection may imitate other skin conditions such as impetigo []. In contact sports athletes, dermatophytic lesions can also mimic abrasions resulting from, e.g., mat burns. The quantity of lesions is often underestimated, especially in cases when they occur on the surface of the back and the scalp where self-observation is rather difficult []. Types of lesions according to the possible site of infection are presented in Table 2.

Table 2.
Types of lesions according to the possible site of infection.
Trunk
Lesions on the surface of the trunk can be described as well-defined and annular scaling papules and/or plaques with raised borders, mild erythema, and a clear center. Lesions may vary in size, usually ranging from 1 to 5 cm, but larger lesions can also occur. They can be single as well as multiple [,,,,]. Three clinical types are distinguished: tinea circinata type, eczema marginatum type, and plaque-like type []. Early lesions might be difficult to differentiate from atopic dermatitis, psoriasis, early herpes gladiatorum, or acneiform papules. Additionally, sometimes they heal spontaneously, leaving the patient unaware of remaining a pathogen transmitter [,,].
Scalp
A typical clinical picture of T. tonsurans infection in the scalp area can be generally characterized as a ‘black-dot’-pattern alopecia with a scaling, patchy distribution of hair loss or scalp inflammation. In some cases, lesions on the scalp are accompanied by erythematous, scaly macules or annular plaques on the face [,].
In this particular region, TG can be divided into three major clinical types []:
- Black-dot ringworm type—a result of a hair invasion (endothrix) []. In dermoscopic assessment, they can be found as a “comma-shaped” hair—a short hair with homogenous pigmentation and thickness [,,]. Rarely, it is reported on other body sites such as the trunk or extremities [,,];
- Seborrheic type—it can mainly be characterized by scalp scaling and the presence of crusts;
- Kerion celsi type—a rare inflammatory manifestation of tinea capitis which represents a delayed T cell-mediated hypersensitivity reaction. It is an intense immune response to the infection caused by dermatophytes which results in limited, infiltrated, suppurative, and tender lesions. Sometimes, cervical lymphadenopathy and id reactions are also reported. If not treated, it may cause scarring alopecia. Kerion celsi needs to be differentiated from cellulitis, seborrheic dermatitis, and carbuncle. Most cases concern the pediatric population. Sporadically, lesions may also arise on other parts of the body, e.g., eyebrows or vulva [,,,,,].
According to an Irish study conducted on the pediatric population, T. tonsurans infection accounted for 75.8% of tinea capitis cases []. In adults, the sebum consists of, i.a., triglycerides and short-chain fatty acids, which play a great role in preventing infection because of their fungistatic features [].
4.5. Quality of Life
Like many other skin conditions, dermatophytosis also has an undeniable impact on patients’ quality of life. According to the study performed in 2013 to assess the global burden of disease, superficial fungal infection is the fourth most frequent cause of illness globally [,]. Dermatophytosis significantly impacts patients’ quality of life by inducing psychosocial consequences such as embarrassment, low self-esteem, anxiety, and depression, the main explanation of which is attributed to pruritus and aesthetic matters [,]. In 2019, the group of Narang et al. [] performed a study investigating the quality of life of patients with dermatophytosis. A total of 196 subjects participated in this survey. The mean total Dermatology Life Quality Index (DLQI) score reached 13.41 ± 7.56 points (range 0–30 points). Items described to be mostly influenced were “symptoms and feelings”, “daily activities”, “leisure”, and “personal relationships”. Both age and body surface area had a significant impact on patients’ quality of life (QoL) (p ≤ 0.05). Mushtaq et al. [] also proved that the DLQI score may be influenced by the severity of the disease.
4.6. Diagnosis
In most cases, the diagnosis is made on the basis of the clinical picture. In some wrestling teams, not only were the physicians and the wrestlers themselves involved in the diagnostic process, but the coaches were also included. What is more, some of them admitted to deciding if the athlete is permitted to continue with training without a doctor′s consultation [].
The obligatory first step of dermatophytosis diagnosis should be a precise clinical examination conducted by a physician, preceded by taking an extensive patient history (possible vectors; contact with infected persons and animals; hobbies; socioeconomic situation). Typical morphological figures as well as the pattern of lesion distribution may be helpful in distinguishing the disease.
Another basic mycological test that is widely performed is a microscopic inspection of material, such as skin scrapings, hair, or nails in KOH mounts (potassium hydroxide). A 10–20% KOH solution acts as a macerating agent and allows the diagnostician to observe dermatophyte hyphae []. Sometimes also, specific stains (e.g., Parkerink, Chicago blue) may be used in specimens to mark fungal elements []. Histological examination performed with the use of periodic acid schiff (PAS) stain can reveal signs of tinea [].
There are also many methods that support medical practitioners and let them approach the specific diagnosis. For instance, inspection with Wood′s light allows to screen for Microsporum canis infection [], and dermatoscopy enables to differentiate tinea capitis from other dermatoses []. The latter is also used in cases of onychomycosis (distinguishing post-traumatic damages from fungal infection [,,]) or to exclude tinea nigra in palmar or plantar lesions []. Other more advanced techniques of fungi detection are optical coherence tomography and confocal laser scanning. The most important advantages of their use are non-invasiveness and immediate real-time test results. On the other hand, particular technical skills are needed to understand and properly interpret those outcomes. The availability of these methods is, however, rather low [,].
Tracing epidemics is one of the most important tasks and challenges of public health and modern epidemiology. Moreover, helping to determine the source of infection may be crucial in restricting the spread of the pathogen []. A classical procedure of dermatophyte identification is growing a culture on a specific medium such as Sabouraud dextrose agar. One of the agar plates should also contain cycloheximide to prevent bacteria and non-dermatophyte mold contamination [] (Figure 3 and Figure 4).
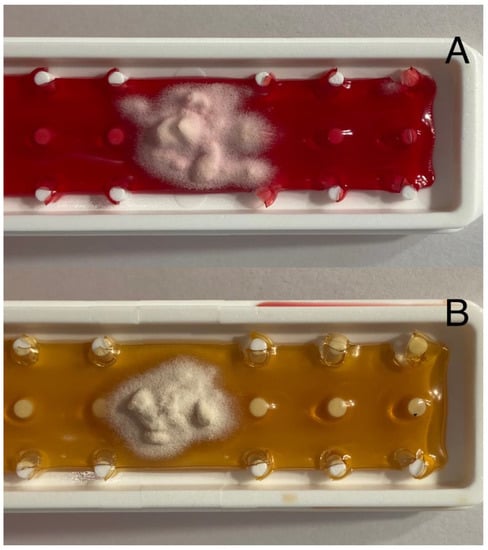
Figure 3.
Pictures of Trichophyton tonsurans culture: (A) Fungiset agar growth medium with actidione (cycloheximide) and phenol red; (B) Sabouraud dextrose agar growth medium with chloramphenicol. Courtesy of Prof. J. C. Szepietowski.
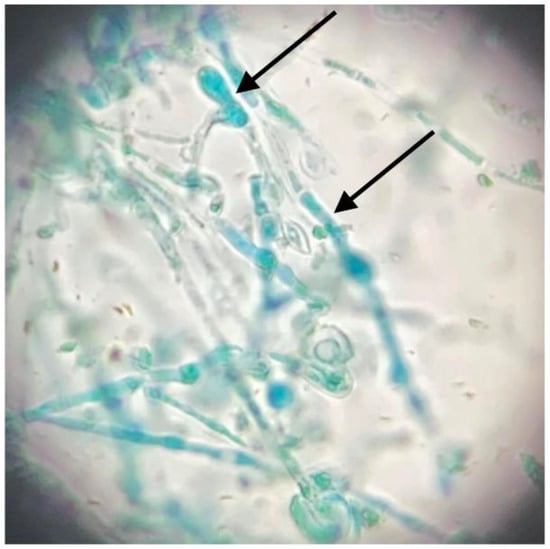
Figure 4.
Microscopic picture of microculture: numerous microconidia, including club-shaped ones (pointed by black arrows). Courtesy of Prof. J. C. Szepietowski.
Molecular biology methods are presumably the most rapidly developing branches of laboratory diagnostics and are widely used for identifying particular microorganisms as well as dermatophytes. To obtain results confirming the presence of specific species of the pathogen, different parts of fungal DNA are used []. Genetic methods involve the polymerase chain reaction (PCR) fingerprinting technique with single arbitrary primers, the analysis of restriction fragment length polymorphism (RFLP) of mitochondrial DNA, or comparison of ribosomal DNA sequences []. An analysis of T. tonsurans strain’s molecular marker polymorphisms (e.g., NTS (non-transcripted spacer) regions of ribosomal RNA gene (rDNA)) performed by American researchers presented significant strain-specific genetic variations []. Different strains may present dissimilarities in pathogenicity which exert an impact on the minimum inhibitory concentration (MIC) of antimycotics []. Furthermore, divergence in genes and recognizing them brings information about virulence of the fungi and specific infection patterns [].
Identification of dermatophytes can also be performed based on mass spectrometry (MS) methods such as matrix assisted laser desorption/ionization time-of-flight (MALDI-TOF) analysis. In this assay, fungal material is evaporated by a laser beam and ionized particles are analyzed by mass spectrometry according to their time of flight [,]. Erhard et al. [] in 2007 proved that the results of species identification by MALDI-TOF mass spectrometry are comparable with those obtained by using molecular methods (fungal DNA sequencing). Nevertheless, MALDI-TOF MS has also some limitations such as reliability on the quality of the reference spectra library [].
The variety of methods for detection and identification of dermatophyte species and strains is constantly expanding. However, that process would not be possible without comparison to most efficient and reliable classical mycological techniques. It should also be emphasized that mycological tests are essential for proper tinea management.
4.7. Treatment
Management of dermatophytic infections consists of topical antifungals individually when disease is limited or oral therapeutics individually or in combination with topical agents in disseminated or resistant cases.
4.7.1. Topical
Numerous topical antifungal formulations that are effective in tinea gladiatorum treatment have been reported. Most topical antifungals are prescribed once or twice daily for 2–4 weeks []. In 2013, Rotta et al. [] created a meta-analysis of the efficacy of antifungal treatment of 14 different topical antifungals. Their study included 65 randomized controlled trials, where pharmaceuticals were compared with one another and with placebo. No statistically significant differences between the antifungals were reported based on the result of mycological cure at the end of treatment. To achieve a long-lasting recovery, butenafine and terbinafine were found to be superior to clotrimazole, oxiconazole, and sertaconazole; terbinafine to ciclopirox; and naftifine to oxiconazole. A similar result to terbinafine antifungal activity was also shown by luliconazole []. A Cochrane review concerning topical antifungals demonstrated that terbinafine and naftifine in monotherapy are effective in dermatophytic infections and adverse effects occur rarely. Other antifungals such as azoles were reported to be effective ways of management as well []. Not only is the drug part of the preparation important but also the medium. Research conducted on lipid-based amphotericin B gel or microemulsion has shown promising results [,]. A novel film-forming terbinafine solution presented fungicidal effects that lasted almost 2 weeks after only a single application [].
4.7.2. Systemic
Although topical agents are a first-line treatment, in some cases, this kind of therapy may be unsuccessful, and lesions can also be so vast that local pharmaceuticals appear to be helpless. Some locations, such as the back of the trunk, are also difficult to self-reach []. In those patients, oral antifungals need to be prescribed. It also concerns patients with affected surface of the scalp (tinea capitis).
Itraconazole and terbinafine are the most commonly chosen pharmaceuticals. Daily doses are 100–200 mg and 250 mg per day, respectively, used for 1–2 weeks [].
Other alternatives are fluconazole (150–200 mg once weekly) and griseofulvin (500–1000 mg daily). The latter is no longer used in some European countries []. Those options, however, demand long-term use (2–4 weeks) [].
In 2020, the group of Kermani et al. [] performed a study to assess the in vitro activity of the most common antifungals used against T. tonsurans obtained from wrestlers with different types of dermatophytosis (tinea corporis, tinea capitis, tinea manuum, tinea faciei, and ținea cruris). They tested eight most commonly prescribed antifungal agents and concluded that tolnaftate and itraconazole had the most potent antifungal activity (concerning T. tonsurans infection). Fluconazole seemed to present the weakest effect [].
However, what should definitely be alarming is that with each year, there is an increasing number of reports informing about dermatophyte resistance and tolerance of antifungals [,]. Some mechanisms responsible for that which were lately outlined are, e.g., drug efflux, drug degeneration, overexpression of chaperones, target mutation, and biofilm formation. Factors increasing the possibility of drug resistance are long-term therapy and discontinuation of treatment against a doctor′s recommendations []. Even more disturbing is the fact that also a cross-resistance was described, showing decreased sensitivity to allylamines and azoles. The group of Singh et al. [] reported a considerably high terbinafine resistance rate of 32% among 63 T. interdigitale isolates and cross-resistance to itraconazole, fluconazole, sertaconazole, voriconazole, and griseofulvin.
4.8. Prevention
Diagnosed infection leads to the loss of competition and practice time which may influence athletes’ both physical and mental condition. It can also affect the whole team [,]. There are methods and measures that are undertaken to prevent disease transmission and to limit local outbreaks. Those strategies, including wrestling mat sanitization (benzalkonium chloride might be particularly effective []), washing by wrestlers immediately after the practice, pretreatment with barrier foam before an encounter, and mandatory skin inspection protocols preceding each competition, might spectacularly decrease the number of TG cases [,,,]. In 2009, American scientists from Toledo published the results of their prospective longitudinal study that was conducted among a group of 373 wrestlers between 1997 and 2007 and concerned the evaluation of the use of prophylactic oral fluconazole in reducing the frequency of tinea gladiatorum. Athletes received 100 mg fluconazole in tablets for 3 days prior to the wrestling season opening. That 3-day dosage was repeated in week 6. Over the course of the study, the incidence rate of TG decreased from 67.4% to 3.5%. No adverse effects of the intervention were observed []. Another possibility described in the literature is itraconazole pulse therapy. The group of Hanzen et al. [] created a survey in which they prescribed wrestling team members oral itraconazole, 200 mg, twice a day for 1 day every 2 weeks. No signs of active tinea were found among examined athletes during the follow-up period (half of a wrestling season). To prevent infection, talcum powders may also be used, often combined with antifungals such as clotrimazole or terbinafine. They absorb excessive amounts of sweat, reduce the moisture of the skin, and simultaneously act against dermatophytes []. Moreover, authors have underlined the obvious role of athletes’ and trainers′ education in outbreak prevention [,].
5. Conclusions
Tinea gladiatorum was and continues to be one of the most frequent infectious skin diseases among wrestlers. Although the infection does not cause serious life-threatening consequences, it may influence individual and team sport goals. It also impacts patient quality of life. Over the course of years, many risk factors have been found, and what is more, contact sports athletes, trainers, and medical practitioners taking care of them has shown that awareness of fungal skin infections definitely has increased. A precise physical examination followed by proper mycological tests forms the basis of tinea gladiatorum diagnosis. Both topical and systemic antifungals’ formulations allow dermatologists to choose the best line of treatment and to escalate it if required. Preventive steps need to be undertaken to limit the amount of new cases and restrain local outbreaks. Not only athletes themselves but also their family members must be taken into account as potential pathogen carriers.
Author Contributions
Conceptualization, J.C.S. and A.Z.; methodology, J.C.S. and A.Z.; formal analysis, A.Z.; investigation, A.Z.; writing—original draft preparation, A.Z.; writing—review and editing, M.G. and J.C.S. All authors have read and agreed to the published version of the manuscript.
Funding
The study was subsidized by Wroclaw Medical University, Wrocław, Poland (SUBZ.C260.22.056).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data are included in the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hedayati, M.T.; Afshar, P.; Shokohi, T.; Aghili, R. A Study on Tinea Gladiatorum in Young Wrestlers and Dermatophyte Contamination of Wrestling Mats from Sari, Iran. Br. J. Sports Med. 2007, 41, 332–334. [Google Scholar] [CrossRef]
- Veraldi, S.; Valentini, D.; Faraci, A.G. Tinea Corporis Gladiatorum. Ital. J. Dermatol. Venereol. 2022, 157, 121–125. [Google Scholar] [CrossRef]
- Nowicka, D.; Baglaj-Oleszczuk, M.; Maj, J. Infectious Diseases of the Skin in Contact Sports. Adv. Clin. Exp. Med. 2020, 29, 1491–1495. [Google Scholar] [CrossRef]
- Bassiri-Jahromi, S.; Sadeghi, G.; Paskiaee, F.A. Evaluation of the Association of Superficial Dermatophytosis and Athletic Activities with Special Reference to Its Prevention and Control. Int. J. Dermatol. 2010, 49, 1159–1164. [Google Scholar] [CrossRef] [PubMed]
- Kermani, F.; Moosazadeh, M.; Hosseini, S.A.; Bandalizadeh, Z.; Barzegari, S.; Shokohi, T. Tinea Gladiatorum and Dermatophyte Contamination Among Wrestlers and in Wrestling Halls: A Systematic Review and Meta-Analysis. Curr. Microbiol. 2020, 77, 602–611. [Google Scholar] [CrossRef]
- Hiruma, J.; Ogawa, Y.; Hiruma, M. Trichophyton tonsurans Infection in Japan: Epidemiology, Clinical Features, Diagnosis and Infection Control. J. Dermatol. 2015, 42, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Salci, T.P.; Salci, M.A.; Marcon, S.S.; Salineiro, P.H.B.; Svidzinski, T.I.E. Trichophyton tonsurans in a Family Microepidemic. An. Bras. Dermatol. 2011, 86, 1003–1006. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Habibipour, R.; Leila, M.H.; Samaiyeh, B. Survey on Dermatophytosis in Wrestlers and Its Relationship with Wrestling Mats in Hamedan. Zahedan J. Res. Med. Sci. 2012, 14, 38–42. [Google Scholar]
- Stiller, M.J.; Klein, W.P.; Dorman, R.I.; Rosenthal, S. Tinea Corporis Gladiatorum: An Epidemic of Trichophyton tonsurans in Student Wrestlers. J. Am. Acad. Dermatol. 1992, 27, 632–633. [Google Scholar] [CrossRef]
- Werninghaus, K. Tinea Corporis in Wrestlers. J. Am. Acad. Dermatol. 1993, 28, 1022–1023. [Google Scholar] [CrossRef]
- Cohen, B.A.; Schmidt, C. Tinea Gladiatorum. N. Engl. J. Med. 1992, 327, 820. [Google Scholar] [CrossRef]
- Beller, M.; Gessner, B. an Outbreak of Tinea-Corporis Gladiatorum on a High-School Wrestling Team. J. Am. Acad. Dermatol. 1994, 31, 197–201. [Google Scholar] [CrossRef]
- Hradil, E.; Hersle, K.; Nordin, P.; Faergemann, J. An Epidemic of Tinea-Corporis Caused by Trichophyton tonsurans among Wrestlers in Sweden. Acta Derm. Venereol. 1995, 75, 305–306. [Google Scholar] [PubMed]
- Hazen, P.G.; Weil, M.L. Itraconazole in the Prevention and Management of Dermatophytosis in Competitive Wrestlers. J. Am. Acad. Dermatol. 1997, 36, 481–482. [Google Scholar] [CrossRef]
- Kohl, T.D.; Martin, D.C.; Berger, M.S. Comparison of Topical and Oral Treatments for Tinea Gladiatorum. Clin. J. Sport Med. 1999, 9, 161–166. [Google Scholar] [CrossRef]
- Pique, E.; Copado, R.; Cabrera, A.; Olivares, M.; Farina, M.; Escalonilla, P.; Soriano, M.; Requena, L. An Outbreak of Tinea Gladiatorum in Lanzarote. Clin. Exp. Dermatol. 1999, 24, 7–9. [Google Scholar]
- Adams, B.B. Tinea Corporis Gladiatorum: A Cross-Sectional Study. J. Am. Acad. Dermatol. 2000, 43, 1039–1041. [Google Scholar] [CrossRef]
- Poisson, D.M.; Rousseau, D.; Defo, D.; Estève, E. Outbreak of Tinea Corporis Gladiatorum, a Fungal Skin Infection Due to Trichophyton tonsurans, in a French High Level Judo Team. Eur. Surveill. Bull. Eur. Sur Mal. Transm. Eur. Commun. Dis. Bull. 2005, 10, 187–190. [Google Scholar] [CrossRef]
- Ergin, S.; Ergin, C.; Erdogan, B.; Kaleli, I.; Evliyaoglu, D. An Experience from an Outbreak of Tinea Capitis Gladiatorum Due to Trichophyton tonsurans. Clin. Exp. Dermatol. 2006, 31, 212–214. [Google Scholar] [CrossRef]
- Bassiri-Jahromi, S.; Khaksar, A. Outbreak of Tinea Gladiatorum in Wrestlers in Tehran (Iran). Indian J. Dermatol. 2008, 53, 132–136. [Google Scholar] [CrossRef] [PubMed]
- Ilkit, M.; Saracli, M.A.; Kurdak, H.; Turac-Bicer, A.; Yuksel, T.; Karakas, M.; Schuenemann, E.; Abdel-Rahman, S.M. Clonal Outbreak of Trichophyton tonsurans Tinea Capitis Gladiatorum among Wrestlers in Adana, Turkey. Med. Mycol. 2010, 48, 480–485. [Google Scholar] [CrossRef]
- Ilkit, M.; Gümral, R.; Saraçlı, M.A.; Burgut, R. Trichophyton tonsurans Scalp Carriage among Wrestlers in a National Competition in Turkey. Mycopathologia 2011, 172, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Aghamirian, M.R.; Ghiasian, S.A. A Clinico-Epidemiological Study on Tinea Gladiatorum in Iranian Wrestlers and Mat Contamination by Dermatophytes. Mycoses 2011, 54, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Ahmadinejad, Z.; Razzaghi, A.; Noori, A.; Hashemi, S.-J.; Asghari, R.; Ziaee, V. Prevalence of Fungal Skin Infections in Iranian Wrestlers. Asian J. Sports Med. 2013, 4, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Dogen, A.; Gumral, R.; Oksuz, Z.; Kaplan, E.; Serin, M.S.; Ilkit, M. Epidemiology of Dermatophytosis in Junior Combat and Non-Combat Sports Participants. Mycoses 2013, 56, 95–100. [Google Scholar] [CrossRef]
- Bonifaz, A.; Araiza, J.; Tirado Sánchez, A.; Barbosa Zamora, A.; Gómez Sáenz, A.; Méndez Juárez, A. Tinea Gladiatorum Due to Trichophyton tonsurans in a School Wrestling Team in Mexico: A Case Series. Curr. Med. Mycol. 2020, 6, 62–65. [Google Scholar] [CrossRef]
- Kermani, F.; Moosazadeh, M.; Hedayati, M.T.; Abastabar, M.; Haghani, I.; Aghili, S.R.; Shokohi, T. Molecular Epidemiology of Tinea Gladiatorum in Contact Sports in Northern Iran. Mycoses 2020, 63, 509–516. [Google Scholar] [CrossRef]
- Berg, M.A.; Miner, M.; Roberts, W.O. Tinea Gladiatorum Prevalence among Wrestlers in the Era of Required Skin Inspection. Asian J. Sports Med. 2021, 12, 1–4. [Google Scholar] [CrossRef]
- Kheffache, H.; Seklaoui, N.; Bouchara, J.P.; Boukhemza-Zemmouri, N.; Boukhemza, M. Tinea Capitis at the University Hospital of Tizi-Ouzou, Algeria, and First Isolation of Trichophyton tonsurans. J. Mycol. Med. 2020, 30, 101040. [Google Scholar] [CrossRef]
- de Hoog, G.S.; Dukik, K.; Monod, M.; Packeu, A.; Stubbe, D.; Hendrickx, M.; Kupsch, C.; Stielow, J.B.; Freeke, J.; Göker, M.; et al. Toward a Novel Multilocus Phylogenetic Taxonomy for the Dermatophytes. Mycopathologia 2017, 182, 5–31. [Google Scholar] [CrossRef] [PubMed]
- Brasch, J. Diagnosis of Dermatophytosis. Curr. FUNGAL Infect. Rep. 2014, 8, 198–202. [Google Scholar] [CrossRef]
- Martinez-Rossi, N.M.; Peres, N.T.A.; Rossi, A. Pathogenesis of Dermatophytosis: Sensing the Host Tissue. Mycopathologia 2017, 182, 215–227. [Google Scholar] [CrossRef]
- Martinez-Rossi, N.M.; Peres, N.T.A.; Bitencourt, T.A.; Martins, M.P.; Rossi, A. State-of-the-Art Dermatophyte Infections: Epidemiology Aspects, Pathophysiology, and Resistance Mechanisms. J. Fungi 2021, 7, 629. [Google Scholar] [CrossRef] [PubMed]
- Shimoyama, H.; Nakashima, C.; Hase, M.; Sei, Y. A Case of Tinea Corporis Due to Trichophyton tonsurans That Manifested as Impetigo. Med. Mycol. J. 2016, 57, E59–E61. [Google Scholar] [CrossRef][Green Version]
- Dinulos, J.G.H. Superficial Fungal Infections. In Habif’s Clinical Dermatology; Elsevier Inc.: Amsterdam, The Netherlands, 2021; pp. 483–524.e1. [Google Scholar]
- Mochizuki, T.; Kawasaki, M.; Anzawa, K.; Kojima, K.; Hatta, J.; Tababe, H.; Higaki, S.; Fujita, S. Extra-Scalp Black Dot Ringworm Caused by Trichophyton tonsurans Among Contact Sports Players. Mycopathologia 2012, 173, 241–244. [Google Scholar] [CrossRef] [PubMed]
- Sidrim, J.J.C.; Rocha, M.F.G.; Leite, J.J.G.; Maranhão, F.C.d.A.; Lima, R.A.C.; Castelo-Branco, D.d.S.C.M.; Bandeira, T.d.J.P.G.; Cordeiro, R.d.A.; Brilhante, R.S.N. Trichophyton tonsurans Strains from Brazil: Phenotypic Heterogeneity, Genetic Homology, and Detection of Virulence Genes. Can. J. Microbiol. 2013, 59, 754–760. [Google Scholar] [CrossRef]
- Bassiri-Jahromi, S.; Khaksar, A. Prevalence of Cutaneous Fungal Infections among Sports-Active Individuals. Ann. Trop. Med. Public Health 2011, 3, 53. [Google Scholar] [CrossRef]
- Gits-Muselli, M.; Benderdouche, M.; Hamane, S.; Mingui, A.; De Chauvin, M.F.; Guigue, N.; Picat, M.-Q.; Bourrat, E.; Petit, A.; Bagot, M.; et al. Continuous Increase of Trichophyton tonsurans as a Cause of Tinea Capitis in the Urban Area of Paris, France: A 5-Year-Long Study. Med. Mycol. 2017, 55, 476–484. [Google Scholar] [CrossRef]
- Skorepová, M.; Stork, J.; Hrabáková, J. Case Reports. Tinea Gladiatorum Due to Trichophyton Mentagrophytes. Mycoses 2002, 45, 431–433. [Google Scholar] [CrossRef]
- Mølenberg, D.; Deleuran, M.; Sommerlund, M. Connubial Tinea Gladiatorum Due to Trichophyton Mentagrophytes. Mycoses 2010, 53, 533–534. [Google Scholar] [CrossRef] [PubMed]
- Shiraki, Y.; Hiruma, M.; Hirose, N.; Sugita, T.; Ikeda, S. A Nationwide Survey of Trichophyton tonsurans Infection among Combat Sport Club Members in Japan Using a Questionnaire Form and the Hairbrush Method. J. Am. Acad. Dermatol. 2006, 54, 622–626. [Google Scholar] [CrossRef] [PubMed]
- Poisson, D.M.; Da Silva, N.J.; Rousseau, D.; Esteve, E. Tinea Corporis Gladiatorum: Specificity and Epidemiology. J. Mycol. Med. 2007, 17, 177–182. [Google Scholar] [CrossRef]
- Shiraki, Y.; Hiruma, M.; Hirose, N.; Ikeda, S. Commonly Affected Body Sites in 92 Japanese Combat Sports Participants with Trichophyton tonsurans Infection. Mycoses 2009, 52, 339–342. [Google Scholar] [CrossRef] [PubMed]
- Landry, G.L.; Chang, C.J. Herpes and Tinea in Wrestling: Managing Outbreaks, Knowing When to Disqualify. Phys. Sportsmed. 2004, 32, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Adams, B.B. Tinea Corporis Gladiatorum. J. Am. Acad. Dermatol. 2002, 47, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Ely, J.W.; Rosenfeld, S.; Stone, M.S. Diagnosis and Management of Tinea Infections. Am. Fam. Physician 2014, 90, 702–710. [Google Scholar]
- Bakos, R.M.; Leite, L.L.; Reinehr, C.; Escobar, G.F. Dermoscopy of Skin Infestations and Infections (Entomodermoscopy)—Part II: Viral, Fungal and Other Infections. An. Bras. Dermatol. 2021, 96, 746–758. [Google Scholar] [CrossRef]
- Schechtman, R.C.; Valgas Silva, N.D.; Quaresma, M.V.; Bernardes Filho, F.; Bucard, A.M.; Sodre, C.T. Dermatoscopic Findings as a Complementary Tool in the Differential Diagnosis of the Etiological Agent of Tinea Capitis. An. Bras. Dermatol. 2015, 90, 13–15. [Google Scholar] [CrossRef]
- Mapelli, E.T.M.; Gualandri, L.; Cerri, A.; Menni, S. Comma Hairs in Tinea Capitis: A Useful Dermatoscopic Sign for Diagnosis of Tinea Capitis. Pediatr. Dermatol. 2012, 29, 223–224. [Google Scholar] [CrossRef]
- Fujita, S.; Mochizuki, T. A case of black dot ringworm on the right forearm caused by Trichophyton tonsurans. Nihon Ishinkin Gakkai Zasshi 2007, 48, 91–95. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Volleková, A.; Kolibasova, K.; Baronáková, A.; Bojcúnová, V. An Unusual “Black-Dot” Trichophytosis Corporis in a Man. Bratisl. Lek. Listy 1997, 98, 43–45. [Google Scholar] [PubMed]
- Gomez-Moyano, E.; Fernandez-Sanchez, A.M.; Crespo-Erchiga, V.; Martinez-Pilar, L. Kerion Celsi Caused by Trichophyton tonsurans with Dermatophytid Reaction. Rev. Iberoam. Micol. 2021, 38, 151–152. [Google Scholar] [CrossRef] [PubMed]
- Lapergola, G.; Breda, L.; Chiesa, P.L.; Mohn, A.; Giannini, C. Kerion Celsi Caused by Trichophyton tonsurans in a Child. Lancet Infect. Dis. 2018, 18, 812. [Google Scholar] [CrossRef]
- Tonin, B.; Geat, D.; Girolomoni, G. A Case of Kerion Celsi Caused by Trichophyton tonsurans. Pediatr. Int. Off. J. Jpn. Pediatr. Soc. 2020, 62, 1007–1008. [Google Scholar] [CrossRef]
- Trovato, L.; Oliveri, S.; Domina, M.; Patamia, I.; Scalia, G.; De Pasquale, R. Molecular Diagnosis of Kerion Celsi Caused by Trichophyton tonsurans in a Italian Child. Med. Mycol. Case Rep. 2019, 24, 72–74. [Google Scholar] [CrossRef]
- Kitajima, M.; Mizuno, K.; Adachi, T.; Adachi, M. A Case of Kerion Celsi Due to Trichophyton tonsurans. J. Dermatol. 2012, 39, 182. [Google Scholar]
- Pinto, V.; Marinaccio, M.; Serratì, A.; D’Addario, V.; Saracino, V.; De Marzo, P. Kerion of the vulva. Report of a case and review of the literature. Minerva Ginecol. 1993, 45, 501–505. [Google Scholar] [PubMed]
- Hackett, B.C.; O’Connell, K.; Cafferkey, M.; O’Donnell, B.F.; Keane, F.M. Tinea Capitis in a Paediatric Population. Ir. Med. J. 2006, 99, 294–295. [Google Scholar]
- Global Burden of Disease Study 2013 Collaborators. Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 354 Diseases and Injuries for 195 Countries and Territories, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef]
- Narang, T.; Bhattacharjee, R.; Singh, S.; Jha, K.; Kavita; Mahajan, R.; Dogra, S. Quality of Life and Psychological Morbidity in Patients with Superficial Cutaneous Dermatophytosis. Mycoses 2019, 62, 680–685. [Google Scholar] [CrossRef] [PubMed]
- Khanyte, A.; Faleiro, K.; Pai, V. ANALYSIS OF DERMATOLOGY LIFE QUALITY INDEX IN DERMATOPHYTOSIS. J. Evol. Med. Dent. Sci. Jemds 2019, 8, 915–918. [Google Scholar] [CrossRef]
- Mushtaq, S.; Faizi, N.; Amin, S.S.; Adil, M.; Mohtashim, M. Impact on Quality of Life in Patients with Dermatophytosis. Australas. J. Dermatol. 2020, 61, e184–e188. [Google Scholar] [CrossRef]
- Kohl, T.D.; Giesen, D.P.; Moyer, J., Jr.; Lisney, M. Tinea Gladiatorum: Pennsylvania’s Experience. Clin. J. Sport Med. 2002, 12, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Côbo, E.C.; Silva, J.C.; Cota, U.A.; Machado, J.R.; Castellano, L.R. Evaluation of a Modified Microscopic Direct Diagnosis of Dermatophytosis. J. Microbiol. Methods 2010, 81, 205–207. [Google Scholar] [CrossRef] [PubMed]
- Tambosis, E.; Lim, C. A Comparison of the Contrast Stains, Chicago Blue, Chlorazole Black, and Parker Ink, for the Rapid Diagnosis of Skin and Nail Infections. Int. J. Dermatol. 2012, 51, 935–938. [Google Scholar] [CrossRef]
- Al-Amiri, A.; Chatrath, V.; Bhawan, J.; Stefanato, C.M. The Periodic Acid-Schiff Stain in Diagnosing Tinea: Should It Be Used Routinely in Inflammatory Skin Diseases? J. Cutan. Pathol. 2003, 30, 611–615. [Google Scholar] [CrossRef]
- Piraccini, B.M.; Balestri, R.; Starace, M.; Rech, G. Nail Digital Dermoscopy (Onychoscopy) in the Diagnosis of Onychomycosis. J. Eur. Acad. Dermatol. Venereol. Jeadv 2013, 27, 509–513. [Google Scholar] [CrossRef]
- Bodman, M.A. Point-of-Care Diagnosis of Onychomycosis by Dermoscopy. J. Am. Podiatr. Med. Assoc. 2017, 107, 413–418. [Google Scholar] [CrossRef]
- Nail Dermoscopy (onychoscopy) Findings in the Diagnosis of Primary Onychomycosis: A Cross-Sectional Study. Indian Journal of Dermatology, Venereology and Leprology. Available online: https://ijdvl.com/nail-dermoscopy-onychoscopy-findings-in-the-diagnosis-of-primary-onychomycosis-a-cross-sectional-study/ (accessed on 22 April 2022).
- Piliouras, P.; Allison, S.; Rosendahl, C.; Buettner, P.G.; Weedon, D. Dermoscopy Improves Diagnosis of Tinea Nigra: A Study of 50 Cases. Australas. J. Dermatol. 2011, 52, 191–194. [Google Scholar] [CrossRef]
- Rothmund, G.; Sattler, E.C.; Kaestle, R.; Fischer, C.; Haas, C.J.; Starz, H.; Welzel, J. Confocal Laser Scanning Microscopy as a New Valuable Tool in the Diagnosis of Onychomycosis - Comparison of Six Diagnostic Methods. Mycoses 2013, 56, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Hui, D.; Sun, X.-c.; Xu, A.-e. Evaluation of Reflectance Confocal Microscopy in Dermatophytosis. Mycoses 2013, 56, 130–133. [Google Scholar] [CrossRef] [PubMed]
- Sakata, Y.; Ushigami, T.; Anzawa, K.; Mochizuki, T. Molecular Epidemiology of Trichophyton tonsurans, the Causative Dermatophyte of the Tinea Gladiatorum Epidemic in Japan between 2011 and 2015. Jpn. J. Infect. Dis. 2018, 71, 140–144. [Google Scholar] [CrossRef]
- Saldaña, M.; Bonifaz, A. Tinea Gladiatorum: An Update. Curr. Fungal Infect. Rep. 2019, 13, 191–195. [Google Scholar] [CrossRef]
- Jensen, R.H.; Arendrup, M.C. Molecular Diagnosis of Dermatophyte Infections. Curr. Opin. Infect. Dis. 2012, 25, 126–134. [Google Scholar] [CrossRef] [PubMed]
- El Fari, M.; Graser, Y.; Presber, W.; Tietz, H. An Epidemic of Tinea Corporis Caused by Trichophyton tonsurans among Children (Wrestlers) in Germany. Mycoses 2000, 43, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Gaedigk, A.; Gaedigk, R.; Abdel-Rahman, S. Genetic Heterogeneity in the RRNA Gene Locus of Trichophyton tonsurans. J. Clin. Microbiol. 2003, 41, 5478–5487. [Google Scholar] [CrossRef][Green Version]
- Gnat, S.; Lagowski, D.; Nowakiewicz, A.; Dyląg, M.; Osińska, M.; Sawicki, M. Detection and Identification of Dermatophytes Based on Currently Available Methods—a Comparative Study. J. Appl. Microbiol. 2021, 130, 278–291. [Google Scholar] [CrossRef]
- Erhard, M.; Hipler, U.-C.; Burmester, A.; Brakhage, A.A.; Wöstemeyer, J. Identification of Dermatophyte Species Causing Onychomycosis and Tinea Pedis by MALDI-TOF Mass Spectrometry. Exp. Dermatol. 2008, 17, 356–361. [Google Scholar] [CrossRef]
- El-Gohary, M.; van Zuuren, E.J.; Fedorowicz, Z.; Burgess, H.; Doney, L.; Stuart, B.; Moore, M.; Little, P. Topical Antifungal Treatments for Tinea Cruris and Tinea Corporis. Cochrane Database. Syst. Rev. 2014, 8, CD009992. [Google Scholar] [CrossRef]
- Rotta, I.; Ziegelmann, P.K.; Otuki, M.F.; Riveros, B.S.; Bernardo, N.L.M.C.; Correr, C.J. Efficacy of Topical Antifungals in the Treatment of Dermatophytosis: A Mixed-Treatment Comparison Meta-Analysis Involving 14 Treatments. Jama Dermatol. 2013, 149, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.K.; Daigle, D. A Critical Appraisal of Once-Daily Topical Luliconazole for the Treatment of Superficial Fungal Infections. Infect. Drug Resist. 2016, 9, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Ateeq Ahmad, S.S. Topical Delivery of Lipid Based Amphotericin B Gel in the Treatment of Fungal Infection: A Clinical Efficacy, Safety and Tolerability Study in Patients. J. Clin. Exp. Dermatol. Res. 2014, 5, 1000248. [Google Scholar] [CrossRef]
- Butani, D.; Yewale, C.; Misra, A. Amphotericin B Topical Microemulsion: Formulation, Characterization and Evaluation. Colloids Surf. B Biointerfaces 2014, 116, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Li, R.Y.; Wang, A.P.; Xu, J.H.; Xi, L.Y.; Fu, M.H.; Zhu, M.; Xu, M.L.; Li, X.Q.; Lai, W.; Liu, W.D.; et al. Efficacy and Safety of 1% Terbinafine Film-Forming Solution in Chinese Patients with Tinea Pedis: A Randomized, Double-Blind, Placebo-Controlled, Multicenter, Parallel-Group Study. Clin. Drug Investig. 2014, 34, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Estève, E.; Rousseau, D.; Defo, D.; Poisson, D.-M. Outbreak of cutaneous dermatophytosis in the Judo French Programme in Orleans: September 2004–June 2005. Ann. Dermatol. Venereol. 2006, 133, 525–529. [Google Scholar] [CrossRef]
- Sacheli, R.; Harag, S.; Dehavay, F.; Evrard, S.; Rousseaux, D.; Adjetey, A.; Seidel, L.; Laffineur, K.; Lagrou, K.; Hayette, M.-P. Belgian National Survey on Tinea Capitis: Epidemiological Considerations and Highlight of Terbinafine-Resistant T. mentagrophytes with a Mutation on SQLE Gene. J. Fungi 2020, 6, 195. [Google Scholar] [CrossRef]
- Kermani, F.; Javidnia, J.; Hedayati, M.T.; Abastabar, M.; Haghani, I.; Didehdar, M.; Fami Zaghrami, M.; Shokohi, T. In Vitro Activities of Antifungal Drugs against a Large Collection of Trichophyton tonsurans Isolated from Wrestlers. Mycoses 2020, 63, 1321–1330. [Google Scholar] [CrossRef]
- Kimura, U.; Hiruma, M.; Kano, R.; Matsumoto, T.; Noguchi, H.; Takamori, K.; Suga, Y. Caution and Warning: Arrival of Terbinafine-Resistant Trichophyton Interdigitale of the Indian Genotype, Isolated from Extensive Dermatophytosis, in Japan. J. Dermatol. 2020, 47, e192–e193. [Google Scholar] [CrossRef]
- Singh, A.; Masih, A.; Khurana, A.; Singh, P.K.; Gupta, M.; Hagen, F.; Meis, J.F.; Chowdhary, A. High Terbinafine Resistance in Trichophyton Interdigitale Isolates in Delhi, India Harbouring Mutations in the Squalene Epoxidase Gene. Mycoses 2018, 61, 477–484. [Google Scholar] [CrossRef]
- Kohl, T.D.; Lisney, M. Tinea Gladiatorum: Wrestling’s Emerging Foe. Sports Med. Auckl. NZ 2000, 29, 439–447. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.; Wells, J.; Klein, R.; Sylvester, T.; Sunenshine, R.; Centers for Disease Control and Prevention (CDC). Notes from the Field: Outbreak of Skin Lesions among High School Wrestlers–Arizona, 2014. MMWR Morb. Mortal. Wkly. Rep. 2015, 64, 559–560. [Google Scholar]
- Brickman, K.; Einstein, E.; Sinha, S.; Ryno, J.; Guiness, M. Fluconazole as a Prophylactic Measure for Tinea Gladiatorum in High School Wrestlers. Clin. J. Sport Med. 2009, 19, 412–414. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).