Comparison of the Complications, Reoperations, and Clinical Outcomes between Open Reduction and Internal Fixation and Total Elbow Arthroplasty for Distal Humeral Fractures in the Elderly: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
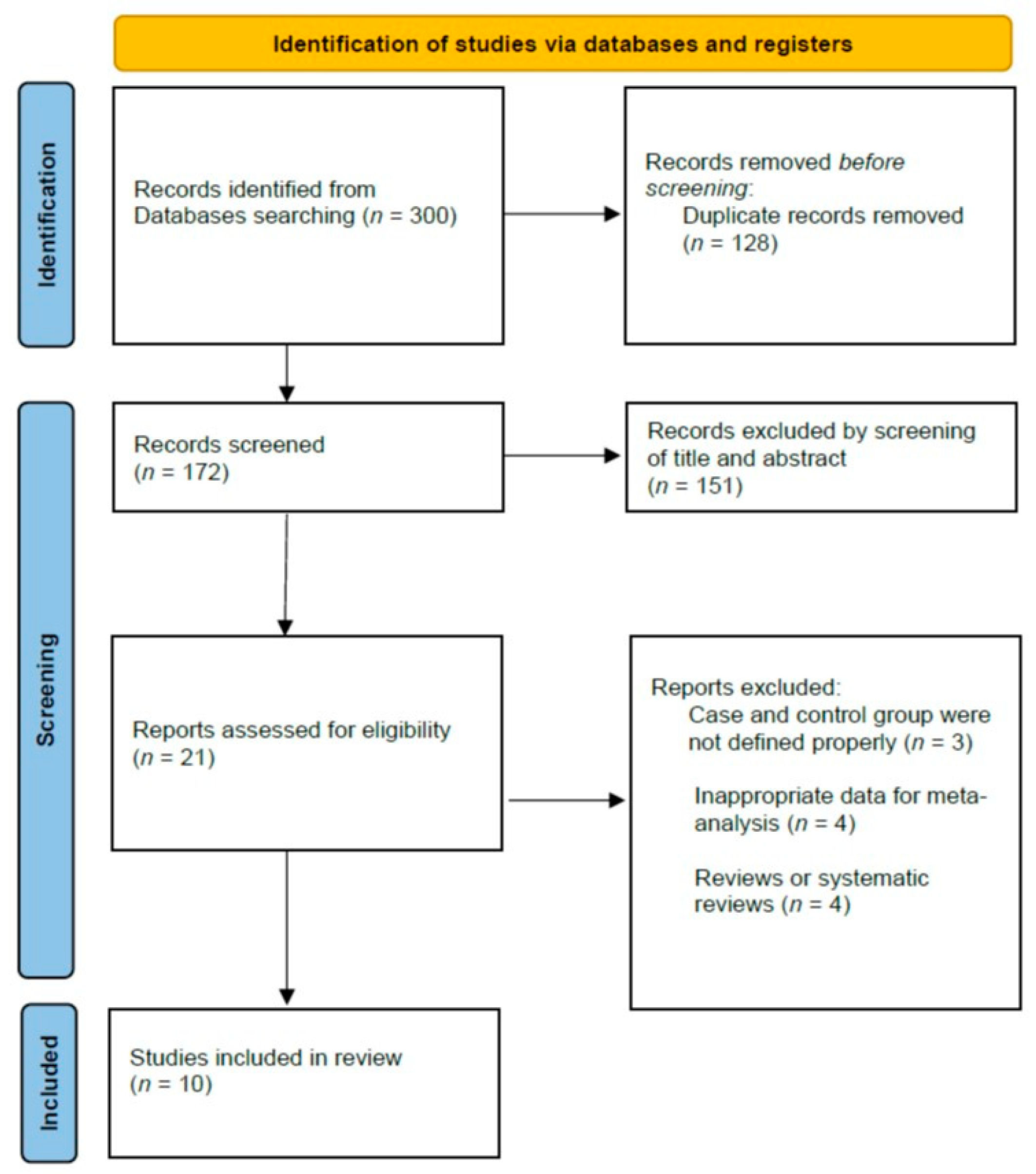
2.1. Literature Search Strategy and Study Selection
2.2. Data Extraction
2.3. Quality Assessment
2.4. Statistical Analyses
3. Results
3.1. Study Selection and Characteristics
3.2. Meta-Analysis Results
3.2.1. Functional Scores
3.2.2. Range of Motions
3.2.3. Complications and Reoperation
3.2.4. Publication Bias
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jordan, R.W.; Saithna, A.; Kimani, P.; Modi, C.; Drew, S.; Lawrence, T. Total elbow arthroplasty versus plate fixation for distal humeral fractures in elderly patients: A systematic review and meta-analysis. Curr. Orthop. Pract. 2018, 29, 384–399. [Google Scholar] [CrossRef]
- Korner, J.; Lill, H.; Müller, L.P.; Hessmann, M.; Kopf, K.; Goldhahn, J.; Gonschorek, O.; Josten, C.; Rommens, P.M. Distal humerus fractures in elderly patients: Results after open reduction and internal fixation. Osteoporos. Int. 2005, 16, S73–S79. [Google Scholar] [CrossRef] [PubMed]
- Palvanen, M.; Kannus, P.; Niemi, S.; Parkkari, J. Secular trends in the osteoporotic fractures of the distal humerus. Eur. J. Epidemiol. 1998, 14, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Hwang, I.-Y.; Park, J.; Park, S.-S.; Yang, J.; Kang, M.S. Injury Characteristics and Predisposing Effects of Various Outdoor Traumatic Situations in Children and Adolescents. Clin. Orthop. Surg. 2021, 13, 423. [Google Scholar] [CrossRef]
- Baik, J.S.; Lee, S.H.; Kang, H.T.; Song, T.H.; Kim, J.W. Comparison of open reduction and internal fixation with total elbow arthroplasty for intra-articular distal humeral fractures in older age: A retrospective study. Clin. Shoulder Elb. 2020, 23, 94–99. [Google Scholar]
- Shin, S.-J.; Sohn, H.-S.; Do, N.-H. A clinical comparison of two different double plating methods for intraarticular distal humerus fractures. J. Shoulder Elb. Surg. 2010, 19, 2–9. [Google Scholar] [CrossRef]
- Zalavras, C.G.; Vercillo, M.T.; Jun, B.-J.; Otarodifard, K.; Itamura, J.M.; Lee, T.Q. Biomechanical evaluation of parallel versus orthogonal plate fixation of intra-articular distal humerus fractures. J. Shoulder Elb. Surg. 2011, 20, 12–20. [Google Scholar] [CrossRef]
- Lee, S.K.; Kim, K.J.; Park, K.H.; Choy, W.S. A comparison between orthogonal and parallel plating methods for distal humerus fractures: A prospective randomized trial. Eur. J. Orthop. Surg. Traumatol. 2014, 24, 1123–1131. [Google Scholar] [CrossRef]
- Korner, J.; Lill, H.; Müller, L.P.; Rommens, P.M.; Schneider, E.; Linke, B.J.I. The LCP-concept in the operative treatment of distal humerus fractures—Biological, biomechanical and surgical aspects. Injury 2003, 34, B20–B30. [Google Scholar] [CrossRef]
- McKee, M.D.; Veillette, C.J.; Hall, J.A.; Schemitsch, E.H.; Wild, L.M.; McCormack, R.; Perey, B.; Goetz, T.; Zomar, M.; Moon, K.; et al. A multicenter, prospective, randomized, controlled trial of open reduction—Internal fixation versus total elbow arthroplasty for displaced intra-articular distal humeral fractures in elderly patients. J. Shoulder Elb. Surg. 2009, 18, 3–12. [Google Scholar] [CrossRef]
- Varecka, T.F.; Myeroff, C. Distal Humerus Fractures in the Elderly Population. J. Am. Acad. Orthop. Surg. 2017, 25, 673–683. [Google Scholar] [CrossRef] [PubMed]
- Kholinne, E.; Altamimi, L.A.; Aldayel, A.; AlSabti, R.; Kim, H.; Park, D.; Koh, K.-H.; Jeon, I.-H. Primary Linked Total Elbow Arthroplasty for Acute Distal Humerus Fracture Management: A Systematic Review of Clinical Outcome. Clin. Orthop. Surg. 2020, 12, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Prkić, A.; van Bergen, C.J.; The, B.; Eygendaal, D. Total elbow arthroplasty is moving forward: Review on past, present and future. World J. Orthop. 2016, 7, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Welsink, C.L.; Lambers, K.T.; Van Deurzen, D.F.; Eygendaal, D.; Van Den Bekerom, M.P.J. Total elbow arthroplasty: A systematic review. IBJS Rev. 2017, 5, e4. [Google Scholar] [CrossRef]
- Gschwend, N.; Scheier, N.H.; Baehler, A.R. Long-term results of the GSB III elbow arthroplasty. J. Bone Jt. Surgery. Br. Vol. 1999, 81, 1005–1012. [Google Scholar] [CrossRef]
- Voloshin, I.; Schippert, D.W.; Kakar, S.; Kaye, E.K.; Morrey, B.F. Complications of total elbow replacement: A systematic review. J. Shoulder Elb. Surg. 2011, 20, 158–168. [Google Scholar] [CrossRef]
- Little, C.P.; Graham, A.J.; Karatzas, G.; Woods, D.A.; Carr, A.J. Outcomes of Total Elbow Arthroplasty for Rheumatoid Arthritis: Comparative Study of Three Implants. J. Bone Jt. Surg. 2005, 87, 2439–2448. [Google Scholar] [CrossRef]
- Githens, M.; Yao, J.; Sox, A.H.S.; Bishop, J. Open Reduction and Internal Fixation Versus Total Elbow Arthroplasty for the Treatment of Geriatric Distal Humerus Fractures: A systematic review and meta-analysis. J. Orthop. Trauma 2014, 28, 481–488. [Google Scholar] [CrossRef]
- Schindelar, L.E.; Rondon, A.J.; Ilyas, A.M. Total Elbow Arthroplasty Versus Open Reduction and Internal Fixation for the Management of Distal Humerus Fractures in the Elderly. Orthopedics 2019, 42, 22–27. [Google Scholar] [CrossRef]
- Goyal, N.; Bohl, D.D.; Ong, K.L.; Lau, E.; Nicholson, G.P.; Wysocki, R.W. Reoperation Risk After Total Elbow Arthroplasty Versus Open Reduction Internal Fixation for Distal Humerus Fractures in Elderly Patients. J. Orthop. Trauma 2020, 34, 503–509. [Google Scholar] [CrossRef]
- Lopiz, Y.; Garríguez-Pérez, D.; García-Fernández, C.; del Baño, L.; Galán-Olleros, M.; Marco, F. Complex fractures of the distal humerus in the elderly: Primary total elbow arthroplasty or open reduction and internal fixation? Mid-term follow-up. Int. Orthop. 2021, 45, 2103–2110. [Google Scholar] [CrossRef] [PubMed]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef] [PubMed]
- Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ott. Hosp. Res. Inst. 2011, 2, 1–12. [Google Scholar]
- Frankle, M.A.; Herscovici, D.; DiPasquale, T.G.; Vasey, M.B.; Sanders, R.W. A Comparison of Open Reduction and Internal Fixation and Primary Total Elbow Arthroplasty in the Treatment of Intraarticular Distal Humerus Fractures in Women Older Than Age 65. J. Orthop. Trauma 2003, 17, 473–480. [Google Scholar] [CrossRef]
- Jost, B.; Adams, A.R.; Morrey, B.F. Management of acute distal humeral fractures in patients with rheumatoid arthritis: A case series. J. Bone Jt. Surg. 2008, 90, 2197–2205. [Google Scholar] [CrossRef]
- Egol, A.K.; Tsai, P.; Vazques, O.; Tejwani, N.C. Comparison of functional outcomes of total elbow arthroplasty vs plate fixation for distal humerus fractures in osteoporotic elbows. Am. J. Orthop. 2011, 40, 67–71. [Google Scholar]
- Ellwein, A.; Lill, H.; Voigt, C.; Wirtz, P.; Jensen, G.; Katthagen, J.C. Arthroplasty compared to internal fixation by locking plate osteosynthesis in comminuted fractures of the distal humerus. Int. Orthop. 2015, 39, 747–754. [Google Scholar] [CrossRef]
- Lovy, A.J.; Keswani, A.; Koehler, S.M.; Kim, J.; Hausman, M. Rehabilitation. Short-term complications of distal humerus fractures in elderly patients: Open reduction internal fixation versus total elbow arthroplasty. Geriatr. Orthop. Surg. Rehabil. 2016, 7, 39–44. [Google Scholar] [CrossRef]
- Medvedev, G.; Wang, C.; Amdur, R.; Neviaser, R.; Neviaser, A. Operative Distal Humerus Fractures in Older Patients: Predictors for Early Complications Based on a National Database. HSS J. Musculoskelet. J. Hosp. Spéc. Surg. 2017, 13, 212–216. [Google Scholar] [CrossRef]
- Sardelli, M.; Tashjian, R.Z.; MacWilliams, B.A. Functional Elbow Range of Motion for Contemporary Tasks. J. Bone Jt. Surg. 2011, 93, 471–477. [Google Scholar] [CrossRef]
- Masci, G.; Cazzato, G.; Milano, G.; Ciolli, G.; Malerba, G.; Perisano, C.; Greco, T.; Osvaldo, P.; Maccauro, G.; Liuzza, F. The stiff elbow: Current concepts. Orthop. Rev. 2020, 12, 8661. [Google Scholar] [CrossRef] [PubMed]




| Authors (Year) | Study Design (LOE) | Mean Age, Years | Mean FU, mo | Fracture Type | ORIF, n | TEA, n | Total, n | Elbow Prosthesis | Device for ORIF | Outcomes Recorded | NOS |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Frankle et al. (2003) [24] | Retrospective comparative (IV) | 70.2 | 51 | AO 13.C2, 13.C3 | 12 | 12 | 24 | Coonrad-Morrey Semiconstrained (Zimmer) | Non-locking plate | MEPS, ROM, complications | 8 (good) |
| Jost et al. (2008) [25] | Retrospective comparative (IV) | 63.4 | 59.6 | AO 13A, 13B, 13C | 6 | 10 | 16 | Coonrad-Morrey Semiconstrained (Zimmer) | Orthogonal or parallel configuration locking plates | MEPS, ROM, complications | 7 (good) |
| Mckee et al. (2009) [10] | Randomized controlled trial (II) | 77 | 24 | AO 13C | 15 | 25 | 40 | Coonrad-Morrey Semiconstrained (Zimmer) | Orthogonal or parallel configuration locking plates | MEPS, DASH, complications | 9 (good) |
| Egol et al. (2011) [26] | Retrospective comparative (IV) | 77.4 | 14.8 | AO 13B, 13C | 11 | 9 | 20 | Semiconstrained Implant (Coonrad-Morrey or Solar) | orthogonal or parallel configuration locking plates | MEPS, DASH, ROM, complications | 7 (good) |
| Ellwein et al. (2014) [27] | Retrospective comparative (IV) | 72 | 26 | AO 13C | 11 | 8 | 19 | Semiconstrained, cemented (Latitude) | Orthogonal configuration locking plates | MEPS, DASH, ROM, complications | 8 (good) |
| Lovy et al. (2016) [28] | Retrospective comparative (IV) | 72.6 | NR | ICD-9 812.2, 812.40, 812.41 | 143 | 33 | 176 | NR | NR | complications | 8 (good) |
| Medvedev et al. (2017) [29] | Retrospective comparative (IV) | 78.1 | NR | ICD-9 812.4x, 812.5x | 216 | 65 | 281 | NR | NR | complications | 6 (good) |
| Baik et al. (2020) [5] | Retrospective comparative (IV) | 77.8 | 32.8 | AO 13C | 28 | 43 | 71 | Coonrad-Morrey semiconstrained prosthesis (Zimmer) | Double-locking plates | Pain, MEPS, DASH, ROM, complications | 9 (good) |
| Goyal et al. (2020) [20] | Retrospective comparative (IV) | At least 65 | NR | ICD-9: 812.40-3 | 522 | 142 | 664 | NR | NR | complications | 7 (good) |
| Lopiz et al. (2021) [21] | Retrospective comparative (IV) | 80 | 64 | AO 13C | 13 | 11 | 24 | Coonrad-Morrey semiconstrained (Zimmer) or the Link Endo-Model elbow prosthesis (Link®) | The Mayo Clinic Congruent elbow plate system (Acumed) | MEPS, DASH, ROM, complications | 9 (good) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seok, H.-G.; Park, J.-J.; Park, S.-G. Comparison of the Complications, Reoperations, and Clinical Outcomes between Open Reduction and Internal Fixation and Total Elbow Arthroplasty for Distal Humeral Fractures in the Elderly: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 5775. https://doi.org/10.3390/jcm11195775
Seok H-G, Park J-J, Park S-G. Comparison of the Complications, Reoperations, and Clinical Outcomes between Open Reduction and Internal Fixation and Total Elbow Arthroplasty for Distal Humeral Fractures in the Elderly: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2022; 11(19):5775. https://doi.org/10.3390/jcm11195775
Chicago/Turabian StyleSeok, Hyun-Gyu, Jeong-Jin Park, and Sam-Guk Park. 2022. "Comparison of the Complications, Reoperations, and Clinical Outcomes between Open Reduction and Internal Fixation and Total Elbow Arthroplasty for Distal Humeral Fractures in the Elderly: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 11, no. 19: 5775. https://doi.org/10.3390/jcm11195775





