Visual Performance, Satisfaction, and Spectacle Independence after Implantation of a New Hydrophobic Trifocal Intraocular Lens
Abstract
1. Introduction
2. Materials and Methods
2.1. Intraocular Lens
2.2. Clinical Procedures
2.3. Surgical Procedure
2.4. Post-Operative Assessment
2.5. Questionnaires
2.6. Statistical Analysis
3. Results
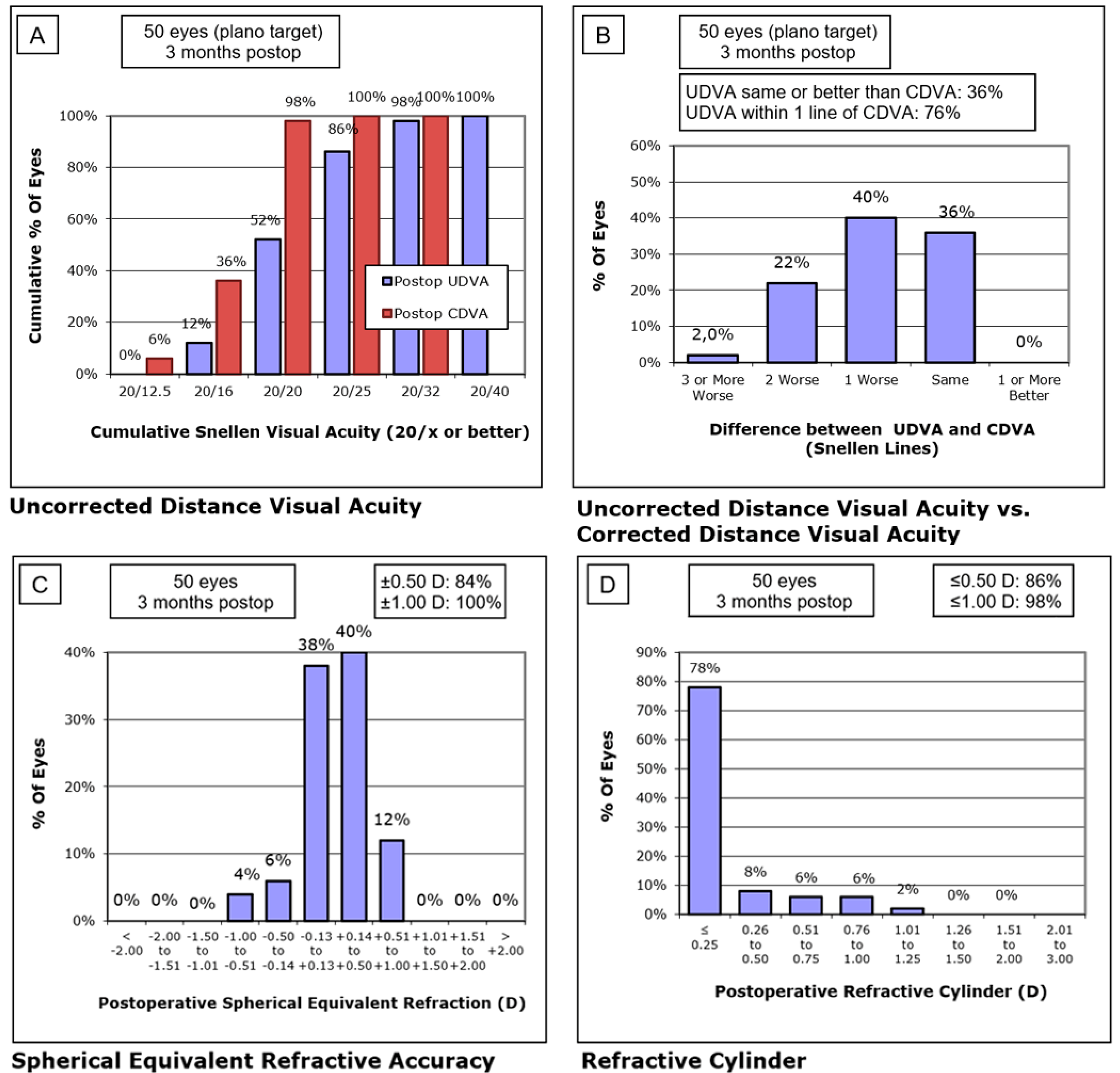
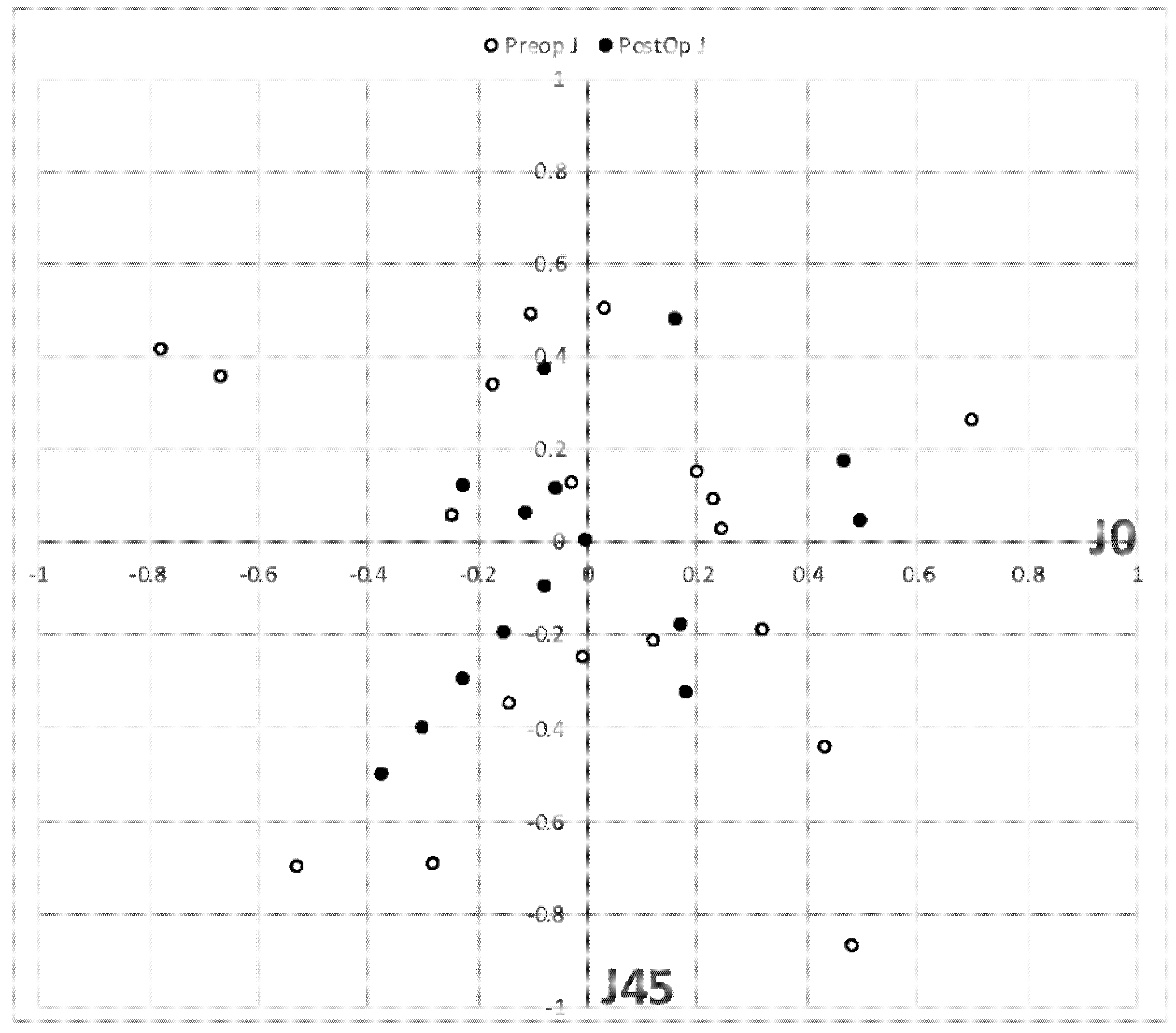
3.1. Post-Operative Refraction
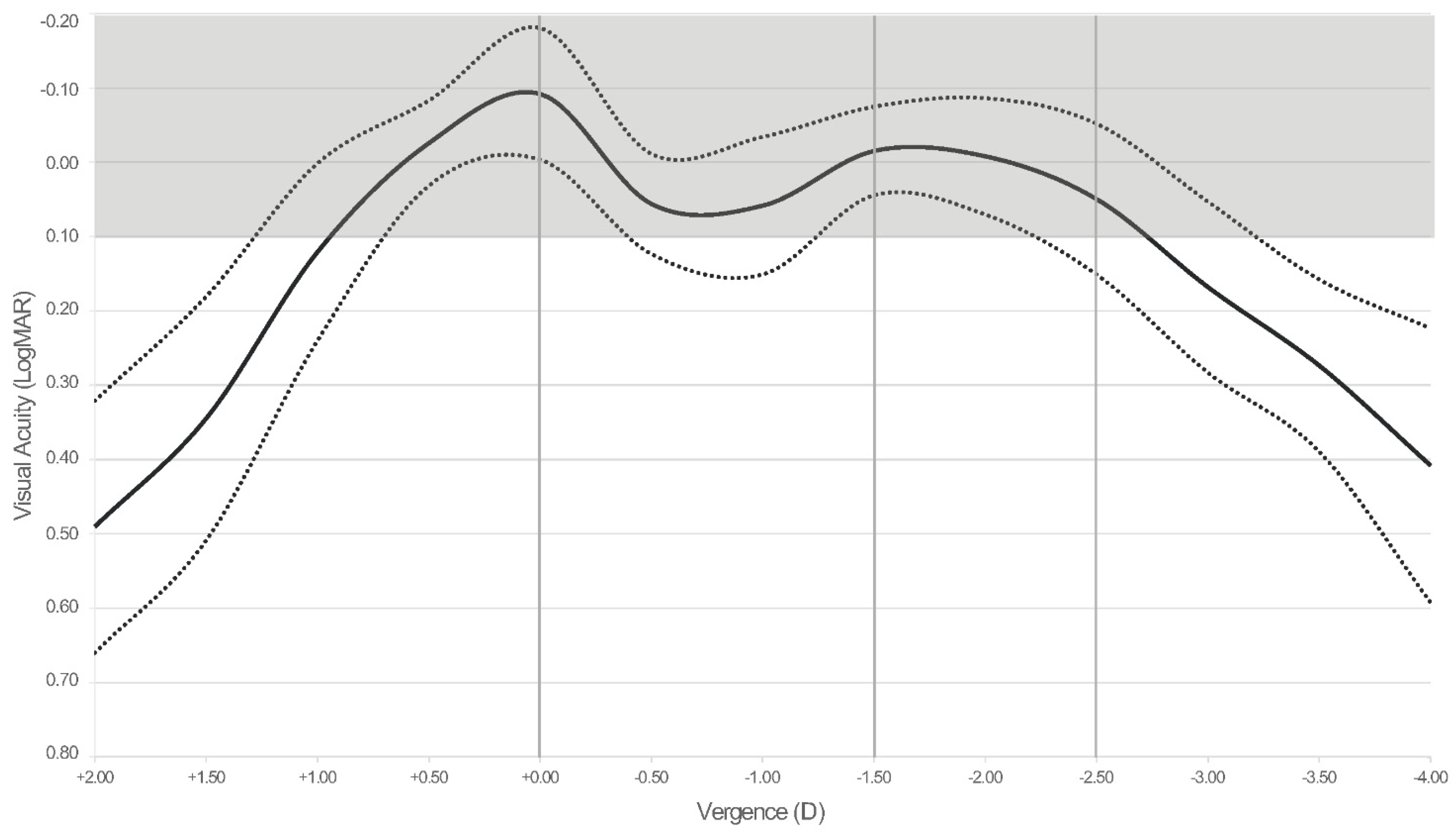
3.2. Visual Performance
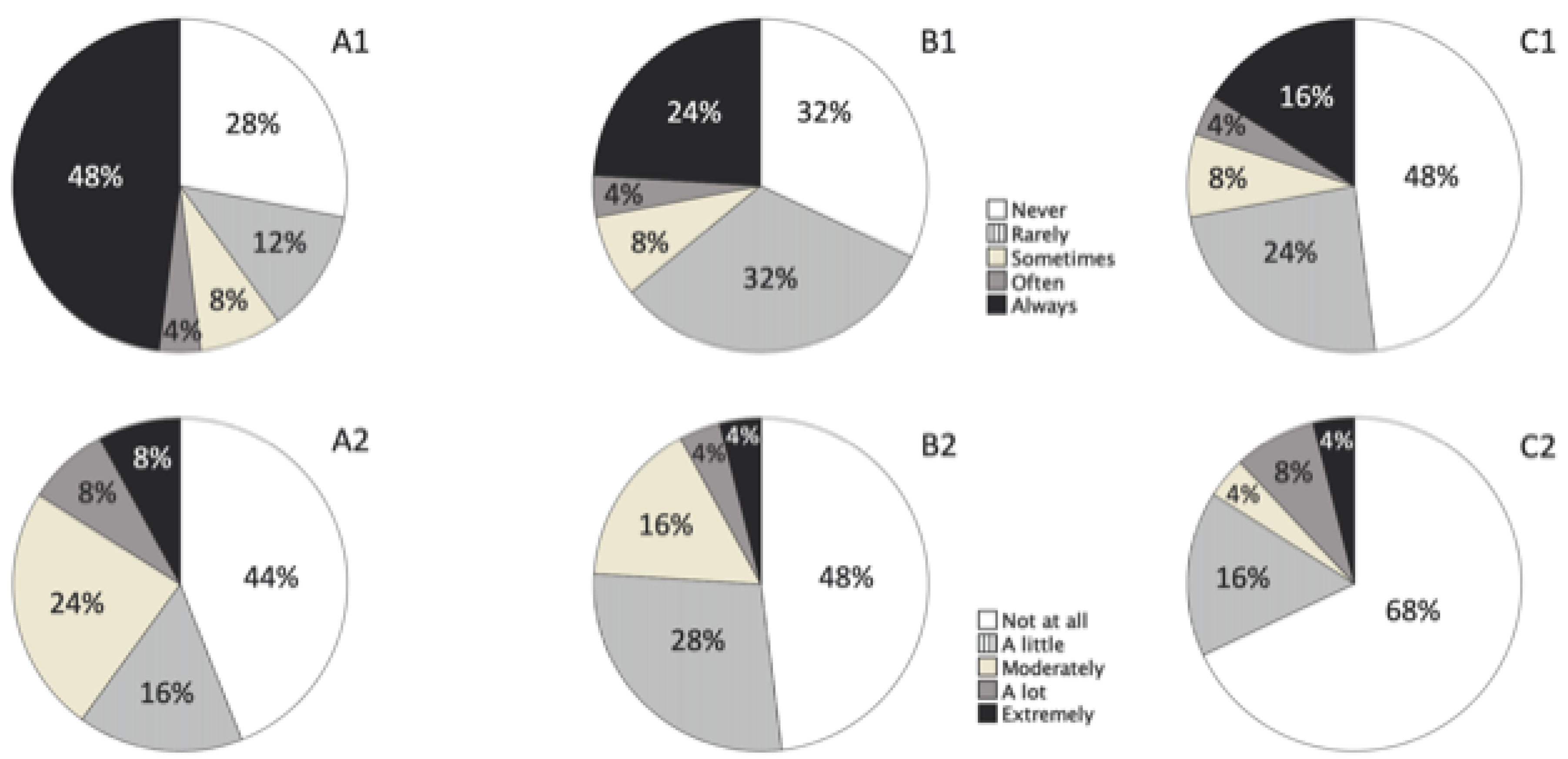
3.3. Outcomes of the Questionnaires
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shen, Z.; Lin, Y.; Zhu, Y.; Liu, X.; Yan, J.; Yao, K. Clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lenses: A systematic review and meta-analysis. Sci. Rep. 2017, 7, 45337. [Google Scholar] [CrossRef] [PubMed]
- Jin, S.; Friedman, D.S.; Cao, K.; Yusufu, M.; Zhang, J.; Wang, J.; Hou, S.; Zhu, G.; Wang, B.; Xiong, Y.; et al. Comparison of postoperative visual performance between bifocal and trifocal intraocular Lens based on randomized controlled trails: A meta-analysis. BMC Ophthalmol. 2019, 19, 78. [Google Scholar] [CrossRef]
- Zhong, Y.; Wang, K.; Yu, X.; Liu, X.; Yao, K. Comparison of trifocal or hybrid multifocal-extended depth of focus intraocular lenses: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 6699. [Google Scholar] [CrossRef]
- Escandón-García, S.; Ribeiro, F.J.; McAlinden, C.; Queirós, A.; González-Méijome, J.M. Through-Focus Vision Performance and Light Disturbances of 3 New Intraocular Lenses for Presbyopia Correction. J. Ophthalmol. 2018, 2018, 6165493. [Google Scholar] [CrossRef] [PubMed]
- Palomino-Bautista, C.; Sánchez-Jean, R.; Carmona-Gonzalez, D.; Piñero, D.P.; Molina-Martín, A. Depth of field measures in pseudophakic eyes implanted with different type of presbyopia-correcting IOLS. Sci. Rep. 2021, 11, 12081. [Google Scholar] [CrossRef]
- Palomino-Bautista, C.; Sánchez-Jean, R.; Carmona-González, D.; Piñero, D.P.; Molina-Martín, A. Subjective and objective depth of field measures in pseudophakic eyes: Comparison between extended depth of focus, trifocal and bifocal intraocular lenses. Int. Ophthalmol. 2020, 40, 351–359. [Google Scholar] [CrossRef]
- McAlinden, C.; Gothwal, V.K.; Khadka, J.; Wright, T.A.; Lamoureux, E.L.; Pesudovs, K. A Head-to-Head Comparison of 16 Cataract Surgery Outcome Questionnaires. Ophthalmology. 2011, 118, 2374–2381. [Google Scholar] [CrossRef]
- Khadka, J.; McAlinden, C.; Pesudovs, K. Quality Assessment of Ophthalmic Questionnaires. Optom. Vis. Sci. 2013, 90, 720–744. [Google Scholar] [CrossRef] [PubMed]
- Kabanovski, A.; Hatch, W.; Chaudhary, V.; El-Defrawy, S.; Reid, R.; Ahmed, I.I.K.; Schlenker, M.B. Validation and application of Catquest-9SF in various populations: A systematic review. Surv. Ophthalmol. 2020, 65, 348–360. [Google Scholar] [CrossRef] [PubMed]
- Mahmud, I.; Kelley, T.; Stowell, C.; Haripriya, A.; Boman, A.; Kossler, I.; Morlet, N.; Pershing, S.; Pesudovs, K.; Goh, P.P.; et al. A Proposed Minimum Standard Set of Outcome Measures for Cataract Surgery. JAMA Ophthalmol. 2015, 133, 1247. [Google Scholar] [CrossRef] [PubMed]
- Lundström, M.; Barry, P.; Brocato, L.; Fitzpatrick, C.; Henry, Y.; Rosen, P.; Stenevi, U. European registry for quality improvement in cataract surgery. Int. J. Health Care Qual. Assur. 2014, 27, 140–151. [Google Scholar] [CrossRef] [PubMed]
- Morlock, R.; Wirth, R.J.; Tally, S.R.; Garufis, C.; Heichel, C.W.D. Patient-Reported Spectacle Independence Questionnaire (PRSIQ): Development and Validation. Am. J. Ophthalmol. 2017, 178, 101–114. [Google Scholar] [CrossRef] [PubMed]
- Poyales, F.; Pérez, R.; López-Brea, I.; Zhou, Y.; Garzón, N. First Results after Implantation of Hydrophilic and Hydrophobic Trifocal Intraocular Lenses: Visual and Optical Performance. J. Ophthalmol. 2021, 2021, 3514577. [Google Scholar] [CrossRef] [PubMed]
- Nováček, L.V.; Němcová, M.; Sičová, K.; Tyx, K.; Rozsíval, P.; Němčanský, J.; Studený, P. Simultaneous Presbyopia and Astigmatism Correction with a Novel Trifocal Toric Intraocular Lens—A One-Year Follow-up. J. Clin. Med. 2022, 11, 4194. [Google Scholar] [CrossRef] [PubMed]
- Ramamurthy, D.; Vasavada, A.; Padmanabhan, P.; Reddy, J.C.; Shetty, N.; Dey, A.; Sudhir, R.R. Clinical Outcomes after Bilateral Implantation of a Trifocal Presbyopia-Correcting Intraocular Lens in an Indian Population. Clin. Ophthalmol. 2021, 15, 213–225. [Google Scholar] [CrossRef] [PubMed]
- Lundström, M.; Llovet, F.; Llovet, A.; del Pozo, M.M.; Mompean, B.; González, J.-V.; Pesudovs, K. Validation of the Spanish Catquest-9SF in patients with a monofocal or trifocal intraocular lens. J. Cataract Refract. Surg. 2016, 42, 1791–1796. [Google Scholar] [CrossRef] [PubMed]
- Galvis, V.; Escaf, L.C.; Tello, A.; Rodríguez, L.D.; Lapid-Gortzak, R.; Carreño, N.I.; Berrospi, R.D.; Niño, C.A.; Viberg, A.; Camacho, P.A. Visual and satisfaction results with implantation of the trifocal Panoptix® intraocular lens in cataract surgery. J. Optom. 2022, 15, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Rementería-Capelo, L.A.; Contreras, I.; García-Pérez, J.L.; Blázquez, V.; Ruiz-Alcocer, J. Visual quality and patient satisfaction with a trifocal intraocular lens and its new toric version. J. Cataract. Refract. Surg. 2019, 45, 1584–1590. [Google Scholar] [CrossRef] [PubMed]
- Fernández, J.; Rodríguez-Vallejo, M.; Martínez, J.; Burguera, N.; Piñero, D.P. Long-Term Efficacy, Visual Performance and Patient Reported Outcomes with a Trifocal Intraocular Lens: A Six-Year Follow-up. J. Clin. Med. 2021, 10, 2009. [Google Scholar] [CrossRef] [PubMed]
- Song, J.E.; Han, S.Y.; Khoramnia, R.; Tandogan, T.; Auffarth, G.U.; Choi, C.Y. Clinical Outcomes of Combined Implantation of an Extended Depth of Focus IOL and a Trifocal IOL in a Korean Population. J. Ophthalmol. 2021, 2021, 9034258. [Google Scholar] [CrossRef]
- Vargas, V.; Alio, J.L.; Oliveira, R.F.; Renna, A.; Yebana, P. Long-term objective and subjective outcomes following bilateral implantation of diffractive bifocal or trifocal intraocular lenses. Eur. J. Ophthalmol. 2021, 31, 1014–1020. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Xie, L.; Huang, Y. Comparison of the Visual Performance After Implantation of Bifocal and Trifocal Intraocular Lenses Having an Identical Platform. J. Refract. Surg. 2018, 34, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Mendicute, J.; Kapp, A.; Lévy, P.; Krommes, G.; Arias-Puente, A.; Tomalla, M.; Barraquer, E.; Rozot, P.; Bouchut, P. Evaluation of visual outcomes and patient satisfaction after implantation of a diffractive trifocal intraocular lens. J. Cataract Refract. Surg. 2016, 42, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Buckhurst, P.J.; Naroo, S.A.; Davies, L.N.; Shah, S.; Drew, T.; Wolffsohn, J.S. Assessment of dysphotopsia in pseudophakic subjects with multifocal intraocular lenses. BMJ Open Ophthalmol. 2017, 1, e000064. [Google Scholar] [CrossRef]
- Alba-Bueno, F.; Garzón, N.; Vega, F.; Poyales, F.; Millán, M.S. Patient-Perceived and Laboratory-Measured Halos Associated with Diffractive Bifocal and Trifocal Intraocular Lenses. Curr. Eye Res. 2018, 43, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Teshigawara, T.; Meguro, A.; Mizuki, N. The Effect of Age, Postoperative Refraction, and Pre- and Postoperative Pupil Size on Halo Size and Intensity in Eyes Implanted with a Trifocal or Extended Depth-of-Focus Lens. Clin. Ophthalmol. 2021, 15, 4141–4152. [Google Scholar] [CrossRef]
- Rementería-Capelo, L.A.; Contreras, I.; García-Perez, J.L.; Carrillo, V.; Gros-Otero, J.; Ruiz-Alcocer, J. Tolerance to Residual Refractive Errors after Trifocal and Trifocal Toric Intraocular Lens Implantation. Eye Contact Lens Sci. Clin. Pract. 2021, 47, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Kohnen, T.; Suryakumar, R. Measures of visual disturbance in patients receiving extended depth-of-focus or trifocal intraocular lenses. J. Cataract Refract. Surg. 2021, 47, 245–255. [Google Scholar] [CrossRef] [PubMed]

| Min | Max | Mean ± SD | |
|---|---|---|---|
| Pre-Operative SE (D) | −4.25 | 7.38 | 1.52 ± 2.14 |
| Pre-Operative J0 (D) | −0.77 | 0.70 | −0.01 ± 0.31 |
| Pre-Operative J45 (D) | −0.87 | 0.50 | −0.01 ± 0.28 |
| AL (mm) | 20.37 | 27.02 | 22.92 ± 1.28 |
| ACD (mm) | 2.31 | 3.67 | 3.05 ± 0.32 |
| K1 (D) | 39.14 | 47.10 | 43.67 ± 1.65 |
| K2 (D) | 39.41 | 47.95 | 44.19 ± 1.64 |
| IOL Power (D) | 17.00 | 32.00 | 23.29 ± 3.22 |
| Min | Max | Mean | SD | |
|---|---|---|---|---|
| Monocular UDVA | −0.10 | 0.30 | 0.05 | 0.09 |
| Monocular CDVA | −0.22 | 0.02 | −0.04 | 0.06 |
| Monocular UIVA | 0.00 | 0.20 | 0.07 | 0.08 |
| Monocular DCIVA | 0.00 | 0.30 | 0.08 | 0.10 |
| Monocular UNVA | 0.00 | 0.30 | 0.14 | 0.07 |
| Monocular DCNVA | 0.00 | 0.20 | 0.10 | 0.08 |
| Binocular UDVA | −0.22 | 0.20 | −0.02 | 0.09 |
| Binocular CDVA | −0.22 | 0.00 | −0.06 | 0.06 |
| Binocular UIVA | 0.00 | 0.20 | 0.06 | 0.08 |
| Binocular DCIVA | −0.10 | 0.28 | 0.02 | 0.09 |
| Binocular UNVA | 0.00 | 0.30 | 0.11 | 0.07 |
| Binocular DCNVA | 0.00 | 0.20 | 0.06 | 0.07 |
| Mean ± SD | Mode | Response Frequencies (%) | |||||
|---|---|---|---|---|---|---|---|
| R1 | R2 | R3 | R4 | R5 | |||
| 1. Within the last 7 days, how often did you wear glasses (including reading glasses) or CL? | |||||||
| A. To see at far distance (1.5 m or more) | 5.00 ± 0.00 | 5 | 0 | 0 | 0 | 0 | 100 |
| B. To see at intermediate distance (0.5–1.5 m) | 4.96 ± 0.20 | 5 | 0 | 0 | 0 | 4 | 96 |
| C. To see at near distance (less than 0.5 m) | 4.72 ± 0.89 | 5 | 4 | 0 | 4 | 4 | 88 |
| D. To see in general (all distances) | 4.84 ± 0.55 | 5 | 0 | 0 | 8 | 0 | 92 |
| 2. What is your level of satisfaction without glasses (including reading glasses) or CL? | |||||||
| A. To see at far distance (1.5 m or more) | 1.68 ± 0.63 | 2 | 40 | 52 | 8 | 0 | 0 |
| B. To see at intermediate distance (0.5–1.5 m)? | 1.80 ± 0.76 | 1 | 40 | 40 | 20 | 0 | 0 |
| C. To see at near distance (less than 0.5 m)? | 2.32 ± 1.18 | 1 | 32 | 24 | 28 | 12 | 4 |
| D. To see in general (all distances)? | 1.72 ± 0.61 | 2 | 36 | 56 | 8 | 0 | 0 |
| 3. Generally, what is your level of satisfaction when performing these tasks? | |||||||
| A. Reading a menu in a restaurant with dimmed light | 2.28 ± 1.14 | 1 | 32 | 24 | 32 | 8 | 4 |
| B. Seeing objects or reading signs on the streets at sunset or at night | 2.16 ± 0.90 | 2 | 24 | 44 | 24 | 8 | 0 |
| C. Seeing steps or borders at sunset or at night | 1.88 ± 0.78 | 2 | 36 | 40 | 24 | 0 | 0 |
| D. Looking at photos on a smartphone or tablet | 1.84 ± 0.94 | 1 | 44 | 36 | 12 | 8 | 0 |
| E. Reading numbers and indicators from the car dashboard | 1.82 ± 0.79 | 1 | 36 | 32 | 20 | 0 | 0 |
| Mean ± SD | Mode | Response Frequencies (%) | |||||
|---|---|---|---|---|---|---|---|
| R1 | R2 | R3 | R4 | R5 | |||
| Do you find that your sight at present in some way causes you difficulty in your everyday life? | 3.80 ± 0.41 | 4 | 0 | 0 | 20 | 80 | 0 |
| Do you have difficulty… | |||||||
| …Reading text in newspapers? | 3.84 ± 0.47 | 4 | 0 | 0 | 20 | 76 | 4 |
| …Recognizing the faces of people you meet? | 3.80 ± 0.41 | 4 | 0 | 0 | 20 | 80 | 0 |
| …Seeing the prices of goods when shopping? | 3.76 ± 0.52 | 4 | 0 | 4 | 16 | 80 | 0 |
| …Seeing to walk on uneven surfaces? | 3.88 ± 0.33 | 4 | 0 | 0 | 12 | 88 | 0 |
| …Seeing to do handicrafts, woodwork, etc.? | 3.76 ± 0.66 | 4 | 0 | 4 | 24 | 64 | 8 |
| …Reading subtitles on TV? | 3.88 ± 0.33 | 4 | 0 | 0 | 12 | 88 | 0 |
| …Seeing to engage in an activity/hobby? | 3.76 ± 0.52 | 4 | 0 | 4 | 16 | 80 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cano-Ortiz, A.; Sánchez-Ventosa, Á.; González-Cruces, T.; Cerdán-Palacios, D.; Díaz-Mesa, V.; Gallego-Ordóñez, R.; Gálvez-Gómez, T.; García Parrizas, J.A.; Zurera Baena, J.; Villarrubia-Cuadrado, A. Visual Performance, Satisfaction, and Spectacle Independence after Implantation of a New Hydrophobic Trifocal Intraocular Lens. J. Clin. Med. 2022, 11, 5931. https://doi.org/10.3390/jcm11195931
Cano-Ortiz A, Sánchez-Ventosa Á, González-Cruces T, Cerdán-Palacios D, Díaz-Mesa V, Gallego-Ordóñez R, Gálvez-Gómez T, García Parrizas JA, Zurera Baena J, Villarrubia-Cuadrado A. Visual Performance, Satisfaction, and Spectacle Independence after Implantation of a New Hydrophobic Trifocal Intraocular Lens. Journal of Clinical Medicine. 2022; 11(19):5931. https://doi.org/10.3390/jcm11195931
Chicago/Turabian StyleCano-Ortiz, Antonio, Álvaro Sánchez-Ventosa, Timoteo González-Cruces, David Cerdán-Palacios, Vanesa Díaz-Mesa, Rubén Gallego-Ordóñez, Teresa Gálvez-Gómez, Jose A. García Parrizas, Javier Zurera Baena, and Alberto Villarrubia-Cuadrado. 2022. "Visual Performance, Satisfaction, and Spectacle Independence after Implantation of a New Hydrophobic Trifocal Intraocular Lens" Journal of Clinical Medicine 11, no. 19: 5931. https://doi.org/10.3390/jcm11195931
APA StyleCano-Ortiz, A., Sánchez-Ventosa, Á., González-Cruces, T., Cerdán-Palacios, D., Díaz-Mesa, V., Gallego-Ordóñez, R., Gálvez-Gómez, T., García Parrizas, J. A., Zurera Baena, J., & Villarrubia-Cuadrado, A. (2022). Visual Performance, Satisfaction, and Spectacle Independence after Implantation of a New Hydrophobic Trifocal Intraocular Lens. Journal of Clinical Medicine, 11(19), 5931. https://doi.org/10.3390/jcm11195931






