Prevalence of Sleep Disturbance and Its Risk Factors in Patients Who Undergo Surgical Treatment for Degenerative Spinal Disease: A Nationwide Study of 106,837 Patients
Abstract
1. Introduction
2. Patients and Methods
2.1. Database
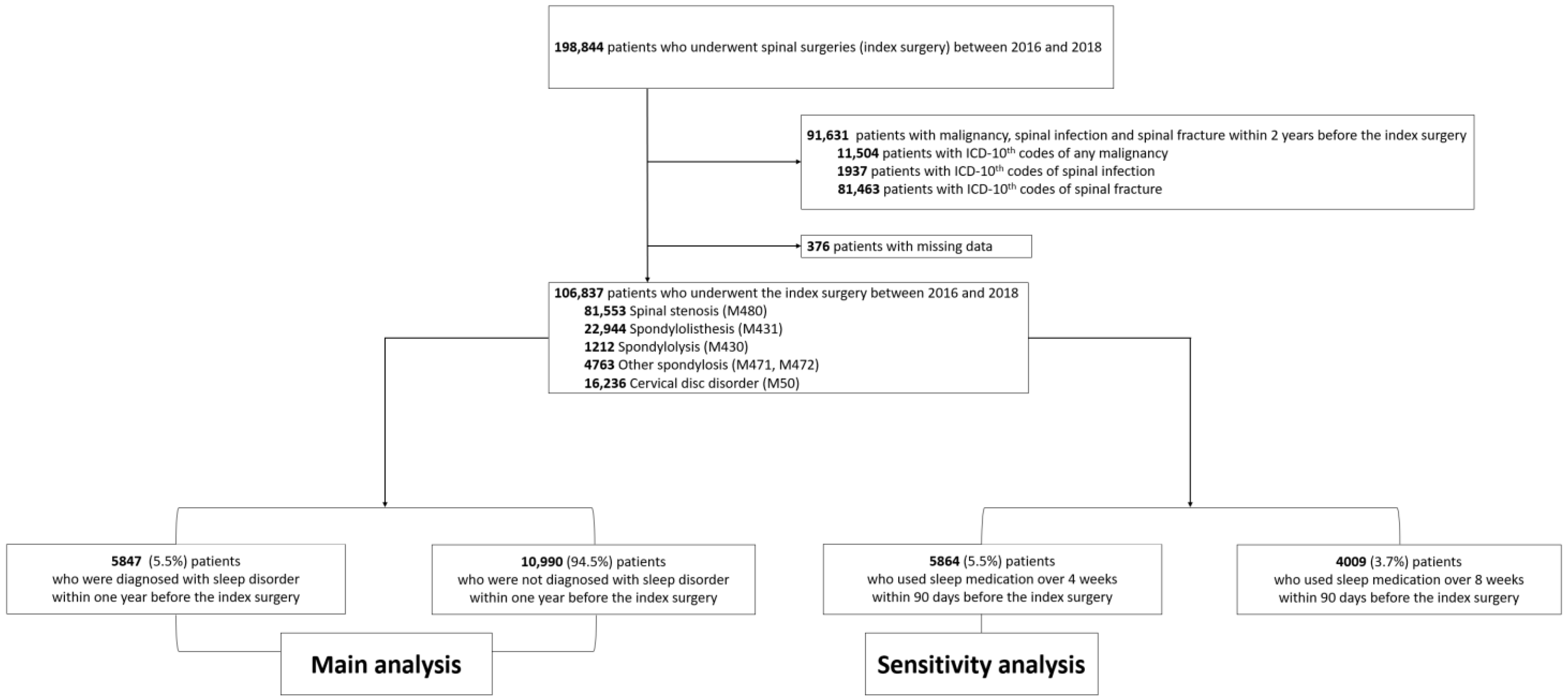
2.2. Study Patients
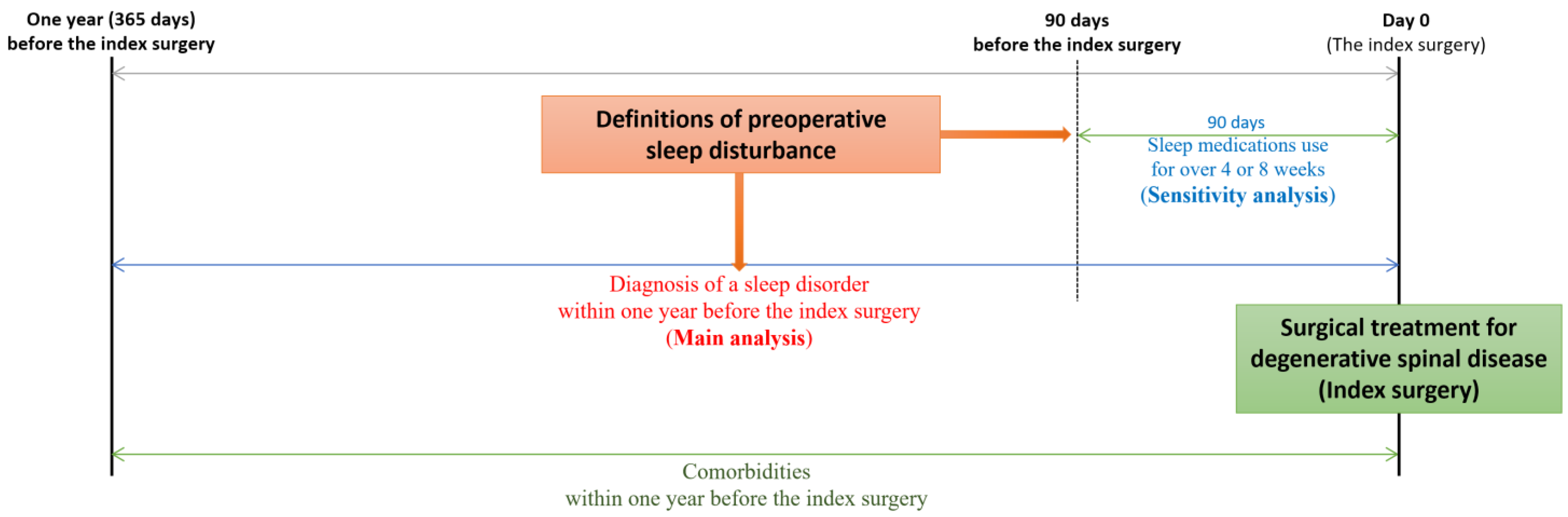
2.3. Definitions of Sleep Disturbance
2.4. Factors Associated with Sleep Disturbance
2.5. Statistical Analysis
3. Results
3.1. Annual Prevalence of Sleep Disturbance According to the Three Definitions
3.2. Prevalence of Sleep Disturbance According to the Baseline Characteristics and Comorbidities
3.3. Prevalence of Sleep Disturbance According to Spinal Regions
3.4. Prevalence of Sleep Disturbance According to Concurrent Neuropsychiatric Disorders and Osteoarthritis of Extremities
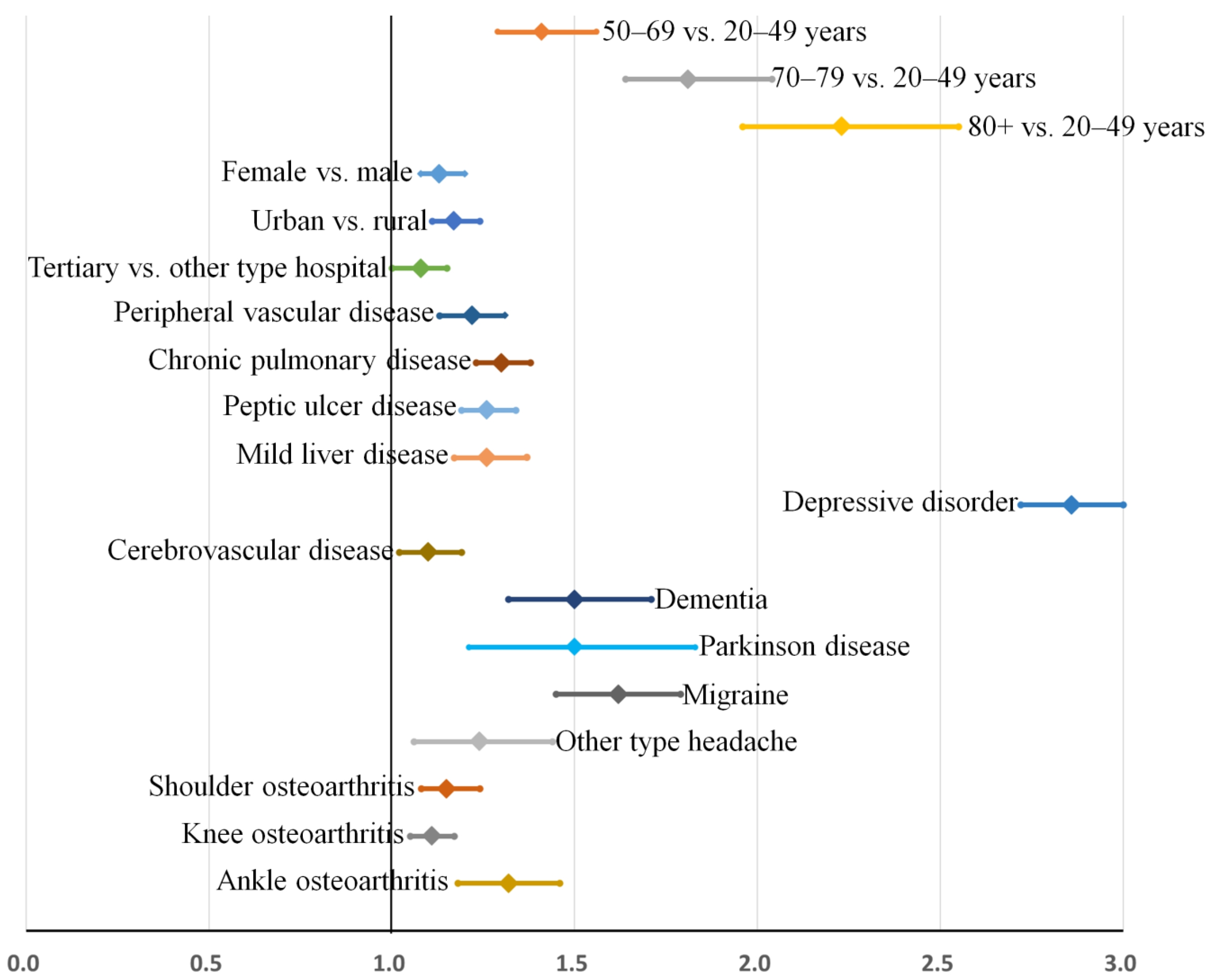
3.5. Risk Factors for Sleep Disorder: Main Analysis
3.6. Validation of Risk Factors: Sensitivity Analysis
3.7. Validation of Estimates: Bootstrap Sampling
4. Discussions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dattilo, M.; Antunes, H.K.; Medeiros, A.; Mônico Neto, M.; Souza, H.S.; Tufik, S.; de Mello, M.T. Sleep and muscle recovery: Endocrinological and molecular basis for a new and promising hypothesis. Med. Hypotheses 2011, 77, 220–222. [Google Scholar] [CrossRef] [PubMed]
- Cirelli, C.; Tononi, G. Is sleep essential? PLoS Biol. 2008, 6, e216. [Google Scholar] [CrossRef] [PubMed]
- Luyster, F.S.; Strollo, P.J., Jr.; Zee, P.C.; Walsh, J.K. Sleep: A health imperative. Sleep 2012, 35, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; Elia, L.; Strazzullo, P.; Miller, M.A. Sleep duration and all-cause mortality: A systematic review and meta-analysis of prospective studies. Sleep 2010, 33, 585–592. [Google Scholar] [CrossRef]
- Stranges, S.; Tigbe, W.; Gómez-Olivé, F.X.; Thorogood, M.; Kandala, N.B. Sleep problems: An emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep 2012, 35, 1173–1181. [Google Scholar] [CrossRef]
- Sutton, D.A.; Moldofsky, H.; Badley, E.M. Insomnia and health problems in Canadians. Sleep 2001, 24, 665–670. [Google Scholar] [CrossRef]
- Hossain, J.L.; Shapiro, C.M. The prevalence, cost implications, and management of sleep disorders: An overview. Sleep Breath 2002, 6, 85–102. [Google Scholar] [CrossRef]
- Burgess, H.J.; Burns, J.W.; Buvanendran, A.; Gupta, R.; Chont, M.; Kennedy, M.; Bruehl, S. Associations between sleep disturbance and chronic pain intensity and function: A test of direct and indirect pathways. Clin. J. Pain 2019, 35, 569–576. [Google Scholar] [CrossRef]
- Onen, S.H.; Onen, F. Chronic medical conditions and sleep in the older adult. Sleep Med. Clin. 2018, 13, 71–79. [Google Scholar] [CrossRef]
- Sasaki, E.; Tsuda, E.; Yamamoto, Y.; Maeda, S.; Inoue, R.; Chiba, D.; Okubo, N.; Takahashi, I.; Nakaji, S.; Ishibashi, Y. Nocturnal knee pain increases with the severity of knee osteoarthritis, disturbing patient sleep quality. Arthritis Care Res. 2014, 66, 1027–1032. [Google Scholar] [CrossRef]
- Khazzam, M.S.; Mulligan, E.P.; Brunette-Christiansen, M.; Shirley, Z. Sleep quality in patients with rotator cuff disease. J. Am. Acad. Orthop. Surg. 2018, 26, 215–222. [Google Scholar] [CrossRef]
- Kim, J.; Oh, J.K.; Kim, S.W.; Yee, J.S.; Kim, T.H. Risk factors for sleep disturbance in patients with cervical myelopathy and its clinical significance: A cross-sectional study. Spine J. 2021, 21, 96–104. [Google Scholar] [CrossRef]
- Kim, J.; Park, J.; Kim, S.W.; Oh, J.K.; Park, M.S.; Kim, Y.W.; Kim, T.H. Prevalence of sleep disturbance in patients with lumbar spinal stenosis and analysis of the risk factors. Spine J. 2020, 20, 1239–1247. [Google Scholar] [CrossRef]
- Kim, H.J.; Hong, S.J.; Park, J.H.; Ki, H. Sleep disturbance and its clinical implication in patients with adult spinal deformity: Comparison with lumbar spinal stenosis. Pain Res. Manag. 2020, 2020, 6294151. [Google Scholar] [CrossRef]
- Artner, J.; Cakir, B.; Spiekermann, J.-A.; Kurz, S.; Leucht, F.; Reichel, H.; Lattig, F. Prevalence of sleep deprivation in patients with chronic neck and back pain: A retrospective evaluation of 1016 patients. J. Pain Res. 2013, 6, 1–6. [Google Scholar] [CrossRef]
- Kim, J.; Kim, G.; Kim, S.W.; Oh, J.K.; Park, M.S.; Kim, Y.W.; Kim, T.H. Changes in sleep disturbance in patients with cervical myelopathy: Comparison between surgical treatment and conservative treatment. Spine J. 2021, 21, 586–597. [Google Scholar] [CrossRef]
- Kim, J.; Lee, S.H.; Kim, T.H. Improvement of sleep quality after treatment in patients with lumbar spinal stenosis: A prospective comparative study between conservative versus surgical treatment. Sci. Rep. 2020, 10, 14135. [Google Scholar] [CrossRef]
- Choi, H.; Youn, S.; Um, Y.H.; Kim, T.W.; Ju, G.; Lee, H.J.; Lee, C.; Lee, S.D.; Bae, K.; Kim, S.J.; et al. Korean Clinical Practice Guideline for the Diagnosis and Treatment of Insomnia in Adults. Psychiatry Investig. 2020, 17, 1048–1059. [Google Scholar] [CrossRef]
- Kim, J.; Ryu, H.; Kim, T.-H. Early reoperation rates and its risk factors after instrumented spinal fusion surgery for degenerative spinal disease: A nationwide cohort study of 65,355 patients. J. Clin. Med. 2022, 11, 3338. [Google Scholar] [CrossRef]
- Lim, J.S.; Kim, T.-H. Recurrence rates and its associated factors after early spinal instrumentation for pyogenic spondylodiscitis: A nationwide cohort study of 2148 patients. J. Clin. Med. 2022, 11, 3356. [Google Scholar] [CrossRef]
- Kim, J.; Kim, T.-H. Risk factors for postoperative deep infection after instrumented spinal fusion surgeries for degenerative spinal disease: A nationwide cohort study of 194,036 patients. J. Clin. Med. 2022, 11, 778. [Google Scholar] [CrossRef]
- Park, H.-R.; Im, S.; Kim, H.; Jung, S.-Y.; Kim, D.; Jang, E.; Sung, Y.-K.; Cho, S.-K. Validation of algorithms to identify knee osteoarthritis patients in the claims database. Int. J. Rheum. Dis. 2019, 22, 890–896. [Google Scholar] [CrossRef]
- Koyanagi, A.; Stickley, A. The association between sleep problems and psychotic symptoms in the general population: A global perspective. Sleep 2015, 38, 1875–1885. [Google Scholar] [CrossRef]
- Kahneman, D. Thinking, Fast and Slow; Farrar, Straus and Giroux: New York, NY, USA, 2017. [Google Scholar]


| Year | Spinal Surgery (n) | Patients Diagnosed with Sleep Disorder within One Year from the Index Surgery | Prevalence According to Sleep Medication during the Preexisting 90 Days | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Over 4-Week Sleep Medication | Over 8-Week Sleep Medication | |||||||||
| (n) | Incidence (%) | 95% CI | (n) | Incidence (%) | 95% CI | (n) | Incidence (%) | 95% CI | ||
| 2016 | 35,507 | 1866 | 5.3% | [5.0–5.5] | 1839 | 5.2% | [4.9–5.4] | 1229 | 3.5% | [3.3–3.7] |
| 2017 | 35,459 | 1912 | 5.4% | [5.2–5.6] | 1932 | 5.4% | [5.2–5.7] | 1319 | 3.7% | [3.5–3.9] |
| 2018 | 35,871 | 2069 | 5.8% | [5.5–6.0] | 2093 | 5.8% | [5.6–6.1] | 1461 | 4.1% | [3.9–4.3] |
| All | 106,837 | 5847 | 5.5% | [5.3–5.6] | 5864 | 5.5% | [5.4–5.6] | 4009 | 3.8% | [3.6–3.9] |
| Variables | Categories | All | Patients Diagnosed with Sleep Disorder within One Year from the Index Surgery | Prevalence according to Sleep Medication during the Preexisting 90 days | ||||
|---|---|---|---|---|---|---|---|---|
| Over 4-Week Sleep Medication | Over 8-Week Sleep Medication | |||||||
| Number of Patients | 106,837 | 5847 | 5.5% | 5864 | 5.5% | 4009 | 3.8% | |
| Age | Mean ± SD | 62.9 ± 11.8 | 66.7 ± 10.5 | 66.9 ± 10.3 | 66.6 ± 10.4 | |||
| 20–49 | 14,014 | 378 | 2.7% | 358 | 2.6% | 266 | 1.9% | |
| 50–69 | 58,533 | 2857 | 4.9% | 2881 | 4.9% | 2007 | 3.4% | |
| 70–79 | 28,671 | 2115 | 7.4% | 2116 | 7.4% | 1393 | 4.9% | |
| 80+ | 5619 | 497 | 8.8% | 509 | 9.1% | 343 | 6.1% | |
| Sex | Male | 51,242 | 2298 | 4.5% | 2203 | 4.3% | 1503 | 2.9% |
| Female | 55,595 | 3549 | 6.4% | 3661 | 6.6% | 2506 | 4.5% | |
| Region | Urban | 88,826 | 4953 | 5.6% | 4903 | 5.5% | 3323 | 3.7% |
| Rural | 18,011 | 894 | 5.0% | 961 | 5.3% | 686 | 3.8% | |
| Hospital | Tertiary | 18,442 | 1154 | 6.3% | 1169 | 6.3% | 814 | 4.4% |
| General | 20,772 | 1257 | 6.1% | 1537 | 7.4% | 1072 | 5.2% | |
| Others | 67,623 | 3436 | 5.1% | 3158 | 4.7% | 2123 | 3.1% | |
| Variables | Categories | All | Patients Diagnosed with Sleep Disorder within One Year from the Index Surgery | Prevalence According to Sleep Medication during the Preexisting 90 Days | ||||
|---|---|---|---|---|---|---|---|---|
| Over 4-Week Sleep Medication | Over 8-Week Sleep Medication | |||||||
| Number of patients | 106,837 | 5847 | 5.5% | 5864 | 5.5% | 4009 | 3.8% | |
| Charlson comorbidity index score | Mean ± SD | 1.14 ± 1.28 | 1.56 ± 1.44 | 1.67 ± 1.52 | 1.66 ± 1.54 | |||
| 0–2 | 75,632 | 4551 | 6.0% | 4423 | 5.8% | 3028 | 4.0% | |
| 3–5 | 27,691 | 1195 | 4.3% | 1310 | 4.7% | 887 | 3.2% | |
| ≥6 | 3514 | 101 | 2.9% | 131 | 3.7% | 94 | 2.7% | |
| Comorbidities | Myocardial infarction | 967 | 72 | 7.4% | 73 | 7.5% | 51 | 5.3% |
| Congestive heart failure | 3394 | 286 | 8.4% | 314 | 9.3% | 217 | 6.4% | |
| Peripheral vascular disease | 12,062 | 969 | 8.0% | 934 | 7.7% | 644 | 5.3% | |
| Chronic pulmonary disease | 24,116 | 1867 | 7.7% | 1825 | 7.6% | 1227 | 5.1% | |
| Rheumatologic disease | 4010 | 292 | 7.3% | 298 | 7.4% | 198 | 4.9% | |
| Peptic ulcer disease | 17,189 | 1341 | 7.8% | 1331 | 7.7% | 905 | 5.3% | |
| Liver disease | ||||||||
| Mild | 6686 | 485 | 7.3% | 496 | 7.4% | 341 | 5.1% | |
| Moderate to severe | 83 | 7 | 8.4% | 9 | 10.8% | 5 | 6.0% | |
| Diabetes | ||||||||
| Uncomplicated | 23,105 | 1492 | 6.5% | 1660 | 7.2% | 1137 | 4.9% | |
| Complicated | 6733 | 434 | 6.4% | 559 | 8.3% | 362 | 5.4% | |
| Hemiplegia or paraplegia | 849 | 50 | 5.9% | 70 | 8.2% | 42 | 4.9% | |
| Renal disease | 2053 | 179 | 8.7% | 211 | 10.3% | 157 | 7.6% | |
| End stage renal disease | 379 | 39 | 10.3% | 57 | 15.0% | 39 | 10.3% | |
| Osteoporosis | 15,495 | 1185 | 7.6% | 1189 | 7.7% | 813 | 5.2% | |
| Concurrent neuropsychiatric disorders | Depressive disorder | 23,921 | 2818 | 11.8% | 3740 | 15.6% | 2806 | 11.7% |
| Cerebrovascular disease | 9502 | 808 | 8.5% | 971 | 10.2% | 695 | 7.3% | |
| Dementia | 1388 | 167 | 12.0% | 160 | 11.5% | 109 | 7.9% | |
| Parkinson disease | 875 | 100 | 11.4% | 175 | 20.0% | 152 | 17.4% | |
| Migraine | 3222 | 384 | 11.9% | 356 | 11.0% | 242 | 7.5% | |
| Tension type headache | 3011 | 343 | 11.4% | 329 | 10.9% | 219 | 7.3% | |
| Other-type headache | 4304 | 469 | 10.9% | 449 | 10.4% | 303 | 7.0% | |
| Concurrent osteoarthritis of extremities | Shoulder | 8503 | 674 | 7.9% | 648 | 7.6% | 450 | 5.3% |
| Elbow | 2276 | 141 | 6.2% | 121 | 5.3% | 86 | 3.8% | |
| Wrist | 2268 | 183 | 8.1% | 192 | 8.5% | 135 | 6.0% | |
| Hip | 7104 | 542 | 7.6% | 531 | 7.5% | 357 | 5.0% | |
| Knee | 24,338 | 1828 | 7.5% | 1898 | 7.8% | 1274 | 5.2% | |
| Ankle | 4024 | 368 | 9.1% | 353 | 8.8% | 239 | 5.9% | |
| Spinal Regions | According to Concurrent Neuropsychiatric Disorders | Cases (n) with Its Proportion (%) | Patients Diagnosed with Sleep Disorder within one Year from the Index Surgery | Prevalence According to Sleep Medication during the Preexisting 90 Days | |||||
|---|---|---|---|---|---|---|---|---|---|
| Over 4-Week Sleep Medication | Over 8-Week Sleep Medication | ||||||||
| Cervical | All cases | 18,819 | (100) | 837 | 4.4% | 812 | 4.3% | 563 | 3.0% |
| Depressive disorder | 3660 | 19.4% | 372 | 10.2% | 526 | 14.4% | 403 | 11.0% | |
| Cerebrovascular disease | 1380 | 7.3% | 107 | 7.8% | 136 | 9.9% | 97 | 7.0% | |
| Dementia | 103 | 0.5% | 10 | 9.7% | 14 | 13.6% | 11 | 10.7% | |
| Parkinson disease | 88 | 0.5% | 8 | 9.1% | 20 | 22.7% | 17 | 19.3% | |
| Migraine | 566 | 3.0% | 60 | 10.6% | 54 | 9.5% | 37 | 6.5% | |
| Tension type headache | 513 | 2.7% | 49 | 9.6% | 45 | 8.8% | 29 | 5.7% | |
| Other-type headache | 742 | 3.9% | 71 | 9.6% | 59 | 8.0% | 37 | 5.0% | |
| Thoracic | All cases | 1027 | (100) | 71 | 6.9% | 63 | 6.1% | 42 | 4.1% |
| Depressive disorder | 271 | 26.4% | 30 | 11.1% | 36 | 13.3% | 24 | 8.9% | |
| Cerebrovascular disease | 127 | 12.4% | 16 | 12.6% | 12 | 9.4% | 7 | 5.5% | |
| Dementia | 18 | 1.8% | 1 | 5.6% | 0 | 0.0% | 0 | 0.0% | |
| Parkinson disease | 6 | 0.6% | 1 | 16.7% | 2 | 33.3% | 2 | 33.3% | |
| Migraine | 24 | 2.3% | 2 | 8.3% | 3 | 12.5% | 2 | 8.3% | |
| Tension type headache | 31 | 3.0% | 3 | 9.7% | 2 | 6.5% | 1 | 3.2% | |
| Other-type headache | 45 | 4.4% | 3 | 6.7% | 3 | 6.7% | 1 | 2.2% | |
| Lumbar | All cases | 86,991 | (100) | 4939 | 5.7% | 4989 | 5.7% | 3404 | 3.9% |
| Depressive disorder | 19,990 | 23.0% | 2416 | 12.1% | 3178 | 15.9% | 2379 | 11.9% | |
| Cerebrovascular disease | 7995 | 9.2% | 685 | 8.6% | 823 | 10.3% | 591 | 7.4% | |
| Dementia | 1267 | 1.5% | 156 | 12.3% | 146 | 11.5% | 98 | 7.7% | |
| Parkinson disease | 781 | 0.9% | 91 | 11.7% | 153 | 19.6% | 133 | 17.0% | |
| Migraine | 2632 | 3.0% | 322 | 12.2% | 299 | 11.4% | 203 | 7.7% | |
| Tension type headache | 2467 | 2.8% | 291 | 11.8% | 282 | 11.4% | 189 | 7.7% | |
| Other-type headache | 3517 | 4.0% | 395 | 11.2% | 387 | 11.0% | 265 | 7.5% | |
| Spinal Regions | Categories | Extremities | Cases (n) with ItsProportion | Patients Diagnosed with Sleep Disorder within One Year from the Index Surgery | Prevalence According to Sleep Medication during the Preexisting 90 Days | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Over 4-Week Sleep Medication | Over 8-Week Sleep Medication | |||||||||
| Cervical | All cases | 18,819 | (100) | 837 | 4.4% | 812 | 4.3% | 563 | 3.0% | |
| Upper extremities | Shoulder | 2214 | 11.8% | 156 | 7.0% | 142 | 6.4% | 101 | 4.6% | |
| Elbow | 568 | 3.0% | 25 | 4.4% | 24 | 4.2% | 18 | 3.2% | ||
| Wrist | 532 | 2.8% | 39 | 7.3% | 42 | 7.9% | 27 | 5.1% | ||
| Lower extremities | Hip | 446 | 2.4% | 38 | 8.5% | 45 | 10.1% | 29 | 6.5% | |
| Knee | 2283 | 12.1% | 155 | 6.8% | 173 | 7.6% | 123 | 5.4% | ||
| Ankle | 459 | 2.4% | 46 | 10.0% | 38 | 8.3% | 31 | 6.8% | ||
| Thoracic | All cases | 1027 | (100) | 71 | 6.9% | 63 | 6.1% | 42 | 4.1% | |
| Upper extremities | Shoulder | 94 | 9.2% | 8 | 8.5% | 4 | 4.3% | 2 | 2.1% | |
| Elbow | 27 | 2.6% | 3 | 11.1% | 3 | 11.1% | 2 | 7.4% | ||
| Wrist | 25 | 2.4% | 2 | 8.0% | 3 | 12.0% | 2 | 8.0% | ||
| Lower extremities | Hip | 94 | 9.2% | 8 | 8.5% | 10 | 10.6% | 5 | 5.3% | |
| Knee | 334 | 32.5% | 31 | 9.3% | 34 | 10.2% | 23 | 6.9% | ||
| Ankle | 68 | 6.6% | 6 | 8.8% | 9 | 13.2% | 8 | 11.8% | ||
| Lumbar | All cases | 86,991 | (100) | 4939 | 5.7% | 4989 | 5.7% | 3404 | 3.9% | |
| Upper extremities | Shoulder | 6195 | 7.1% | 510 | 8.2% | 502 | 8.1% | 347 | 5.6% | |
| Elbow | 1681 | 1.9% | 113 | 6.7% | 94 | 5.6% | 66 | 3.9% | ||
| Wrist | 1711 | 2.0% | 142 | 8.3% | 147 | 8.6% | 105 | 6.1% | ||
| Lower extremities | Hip | 6564 | 7.5% | 496 | 7.6% | 476 | 7.3% | 323 | 4.9% | |
| Knee | 21,721 | 25.0% | 1642 | 7.6% | 1691 | 7.8% | 1128 | 5.2% | ||
| Ankle | 3497 | 4.0% | 316 | 9.0% | 306 | 8.8% | 200 | 5.7% | ||
| Variables | Categories | Model 1 (Univariable) | Model 2 (Fully Adjusted) | Model 3 (Bootstrap Validation after Fully Adjusted) | |||
|---|---|---|---|---|---|---|---|
| Odds Ratio (95% Confidence Interval) | p-Value | Adjusted Odds Ratio (95% Confidence Interval) | p-Value | Adjusted Odds Ratio (95% Confidence Interval) | Relative Bias (%) | ||
| Age | 50–69 vs. 20–49 years | 1.85 [1.66–2.06] | <0.001 | 1.40 [1.25–1.57] | <0.001 | 1.41 [1.29–1.56] | 2.21 |
| 70–79 vs. 20–49 years | 2.87 [2.57–3.21] | <0.001 | 1.80 [1.60–2.03] | <0.001 | 1.81 [1.64–2.04] | 0.89 | |
| 80+ vs. 20–49 years | 3.50 [3.05–4.02] | <0.001 | 2.22 [1.92–2.58] | <0.001 | 2.23 [1.96–2.55] | 0.80 | |
| Sex | Female vs. male | 1.45 [1.38–1.53] | <0.001 | 1.14 [1.07–1.21] | <0.001 | 1.13 [1.08–1.20] | −4.45 |
| Region | Urban vs. rural | 1.13 [1.05–1.22] | 0.001 | 1.18 [1.09–1.27] | <0.001 | 1.17 [1.11–1.24] | −2.97 |
| Hospital | Tertiary vs. others | 1.25 [1.16–1.34] | <0.001 | 1.08 [1.00–1.16] | 0.047 | 1.08 [1.00–1.15] | −3.33 |
| Comorbidities | Peripheral vascular disease | 1.61 [1.50–1.73] | <0.001 | 1.22 [1.13–1.32] | <0.001 | 1.22 [1.13–1.31] | 0.68 |
| Chronic pulmonary disease | 1.66 [1.57–1.76] | <0.001 | 1.31 [1.23–1.40] | <0.001 | 1.30 [1.23–1.38] | −1.42 | |
| Peptic ulcer disease | 1.60 [1.50–1.70] | <0.001 | 1.26 [1.17–1.35] | <0.001 | 1.26 [1.19–1.34] | −0.91 | |
| Mild liver disease | 1.38 [1.26–1.52] | <0.001 | 1.27 [1.14–1.41] | <0.001 | 1.26 [1.17–1.37] | −1.68 | |
| Comorbidities associated neuropsychiatric disorders | Depressive disorder | 3.52 [3.34–3.72] | <0.001 | 2.86 [2.70–3.02] | <0.001 | 2.86 [2.72–3.00] | 0.03 |
| Cerebrovascular disease | 1.70 [1.58–1.84] | <0.001 | 1.12 [1.10–1.20] | 0.040 | 1.10 [1.02–1.19] | −16.00 | |
| Dementia | 2.41 [2.04–2.83] | <0.001 | 1.49 [1.26–1.78] | <0.001 | 1.50 [1.32–1.71] | 0.96 | |
| Parkinson disease | 2.25 [1.83–2.78] | <0.001 | 1.51 [1.22–1.88] | <0.001 | 1.50 [1.21–1.83] | −1.63 | |
| Migraine | 2.43 [2.18–2.71] | <0.001 | 1.61 [1.44–1.82] | <0.001 | 1.62 [1.45–1.79] | 1.76 | |
| Other-type headache | 2.21 [2.00–2.44] | <0.001 | 1.25 [1.03–1.52] | 0.023 | 1.24 [1.06–1.44] | −2.75 | |
| Concurrent osteoarthritis | Shoulder | 1.55 [1.43–1.69] | <0.001 | 1.15 [1.06–1.26] | 0.002 | 1.15 [1.08–1.24] | 1.17 |
| Knee | 1.59 [1.50–1.68] | <0.001 | 1.11 [1.04–1.18] | 0.002 | 1.11 [1.05–1.17] | −1.40 | |
| Ankle | 1.79 [1.60–2.00] | <0.001 | 1.32 [1.17–1.48] | <0.001 | 1.32 [1.18–1.46] | 0.67 | |
| Variables | Categories | Univariable | Model 2 (Fully Adjusted) | Model 3 (Bootstrap Validation after Fully Adjusted) | |||
|---|---|---|---|---|---|---|---|
| Odds Ratio (95% Confidence Interval) | p-Value | Adjusted Odds Ratio (95% Confidence Interval) | p-Value | Adjusted Odds Ratio (95% Confidence Interval) | Relative Bias (%) | ||
| Age | 50–69 vs. 20–49 years | 1.97 [1.77–2.21] | <0.001 | 1.32 [1.17–1.49] | <0.001 | 1.31 [1.19–1.44] | −2.60 |
| 70–79 vs. 20–49 years | 3.04 [2.71–3.41] | <0.001 | 1.54 [1.36–1.75] | <0.001 | 1.53 [1.37–1.71] | −0.78 | |
| 80+ vs. 20–49 years | 3.80 [3.31–4.37] | <0.001 | 1.95 [1.68–2.27] | <0.001 | 1.94 [1.71–2.22] | −0.69 | |
| Sex | Female vs. male | 1.57 [1.49–1.66] | <0.001 | 1.20 [1.13–1.27] | <0.001 | 1.19 [1.14–1.26] | −3.96 |
| Hospital | Tertiary vs. others | 1.38 [1.29–1.48] | <0.001 | 1.17 [1.08–1.15] | <0.001 | 1.16 [1.09–1.24] | −4.46 |
| General vs. others | 1.63 [1.53–1.74] | <0.001 | 1.38 [1.29–1.47] | <0.001 | 1.38 [1.30–1.46] | −0.34 | |
| Comorbidities | Congestive heart failure | 1.80 [1.60–2.03] | <0.001 | 1.16 [1.02–1.33] | 0.023 | 1.17 [1.06–1.32] | 6.99 |
| Peripheral vascular disease | 1.53 [1.42–1.65] | <0.001 | 1.09 [1.00–1.18] | 0.040 | 1.09 [1.01–1.18] | −0.67 | |
| Chronic pulmonary disease | 1.60 [1.51–1.69] | <0.001 | 1.21 [1.13–1.29] | <0.001 | 1.20 [1.13–1.27] | −4.26 | |
| Peptic ulcer disease | 1.58 [1.48–1.68] | <0.001 | 1.20 [1.11–1.29] | <0.001 | 1.20 [1.13–1.29] | −0.34 | |
| Mild liver disease | 1.42 [1.29–1.56] | <0.001 | 1.27 [1.14–1.40] | <0.001 | 1.27 [1.17–1.39] | −0.13 | |
| Uncomplicated diabetes | 1.46 [1.38–1.55] | <0.001 | 1.12 [1.04–1.20] | 0.002 | 1.11 [1.05–1.19] | −4.17 | |
| Renal disease | 2.01 [1.74–2.32] | <0.001 | 1.23 [1.01–1.49] | 0.042 | 1.22 [1.01–1.48] | −5.03 | |
| End stage renal disease | 3.07 [2.31–4.07] | <0.001 | 1.97 [1.39–2.79] | <0.001 | 1.96 [1.45–2.71] | −0.76 | |
| Comorbidities associated neuropsychiatric disorders | Depressive disorder | 7.05 [6.67–7.45] | <0.001 | 5.84 [5.51–6.18] | <0.001 | 5.84 [5.57–6.16] | 0.01 |
| Cerebrovascular disease | 2.15 [2.00–2.31] | <0.001 | 1.28 [1.18–1.39] | <0.001 | 1.28 [1.19–1.38] | 0.54 | |
| Dementia | 2.28 [1.93–2.69] | <0.001 | 1.33 [1.11–1.59] | 0.002 | 1.32 [1.13–1.55] | −1.68 | |
| Parkinson disease | 4.41 [3.73–5.21] | <0.001 | 2.80 [2.34–3.36] | <0.001 | 2.83 [2.46–3.32] | 1.00 | |
| Migraine | 2.21 [1.98–2.48] | <0.001 | 1.30 [1.15–1.47] | <0.001 | 1.31 [1.18–1.44] | 1.88 | |
| Concurrent osteoarthritis | Shoulder | 1.47 [1.35–1.60] | <0.001 | 1.08 [1.02–1.17] | 0.013 | 1.08 [1.01–1.17] | 3.82 |
| Knee | 1.68 [1.58–1.77] | <0.001 | 1.14 [1.06–1.21] | <0.001 | 1.13 [1.07–1.19] | −5.13 | |
| Ankle | 1.70 [1.52–1.90] | <0.001 | 1.19 [1.06–1.35] | 0.004 | 1.20 [1.09–1.32] | 5.14 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.; Kang, M.S.; Kim, T.-H. Prevalence of Sleep Disturbance and Its Risk Factors in Patients Who Undergo Surgical Treatment for Degenerative Spinal Disease: A Nationwide Study of 106,837 Patients. J. Clin. Med. 2022, 11, 5932. https://doi.org/10.3390/jcm11195932
Kim J, Kang MS, Kim T-H. Prevalence of Sleep Disturbance and Its Risk Factors in Patients Who Undergo Surgical Treatment for Degenerative Spinal Disease: A Nationwide Study of 106,837 Patients. Journal of Clinical Medicine. 2022; 11(19):5932. https://doi.org/10.3390/jcm11195932
Chicago/Turabian StyleKim, Jihye, Min Seong Kang, and Tae-Hwan Kim. 2022. "Prevalence of Sleep Disturbance and Its Risk Factors in Patients Who Undergo Surgical Treatment for Degenerative Spinal Disease: A Nationwide Study of 106,837 Patients" Journal of Clinical Medicine 11, no. 19: 5932. https://doi.org/10.3390/jcm11195932
APA StyleKim, J., Kang, M. S., & Kim, T.-H. (2022). Prevalence of Sleep Disturbance and Its Risk Factors in Patients Who Undergo Surgical Treatment for Degenerative Spinal Disease: A Nationwide Study of 106,837 Patients. Journal of Clinical Medicine, 11(19), 5932. https://doi.org/10.3390/jcm11195932





