A Multicenter Network Analysis Examining the Psychological Effects of the COVID-19 Pandemic on Patients with Eating Disorders versus Their Healthy Siblings
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Assessment
2.3. Data Analysis
3. Results
3.1. Participants’ Characteristics
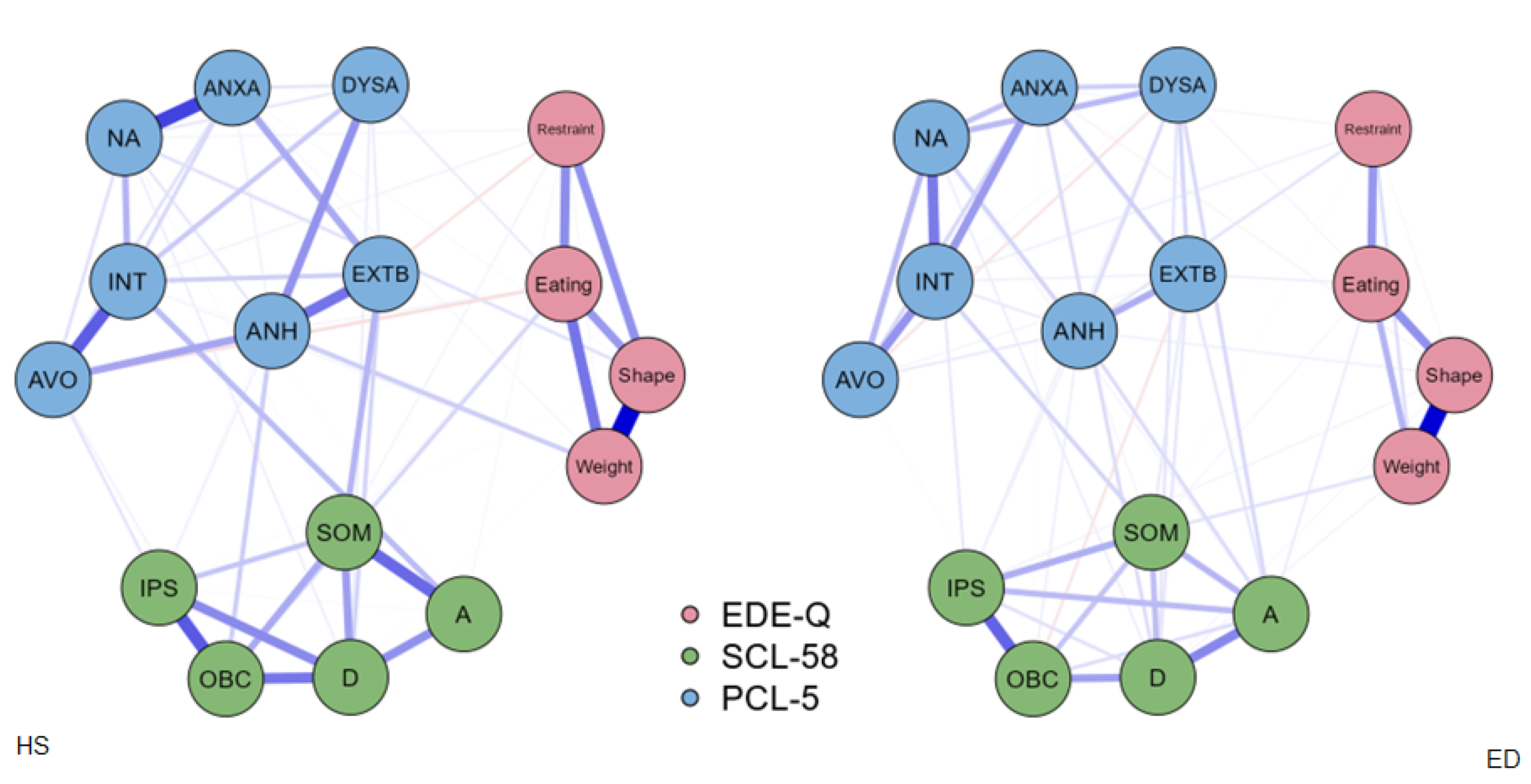
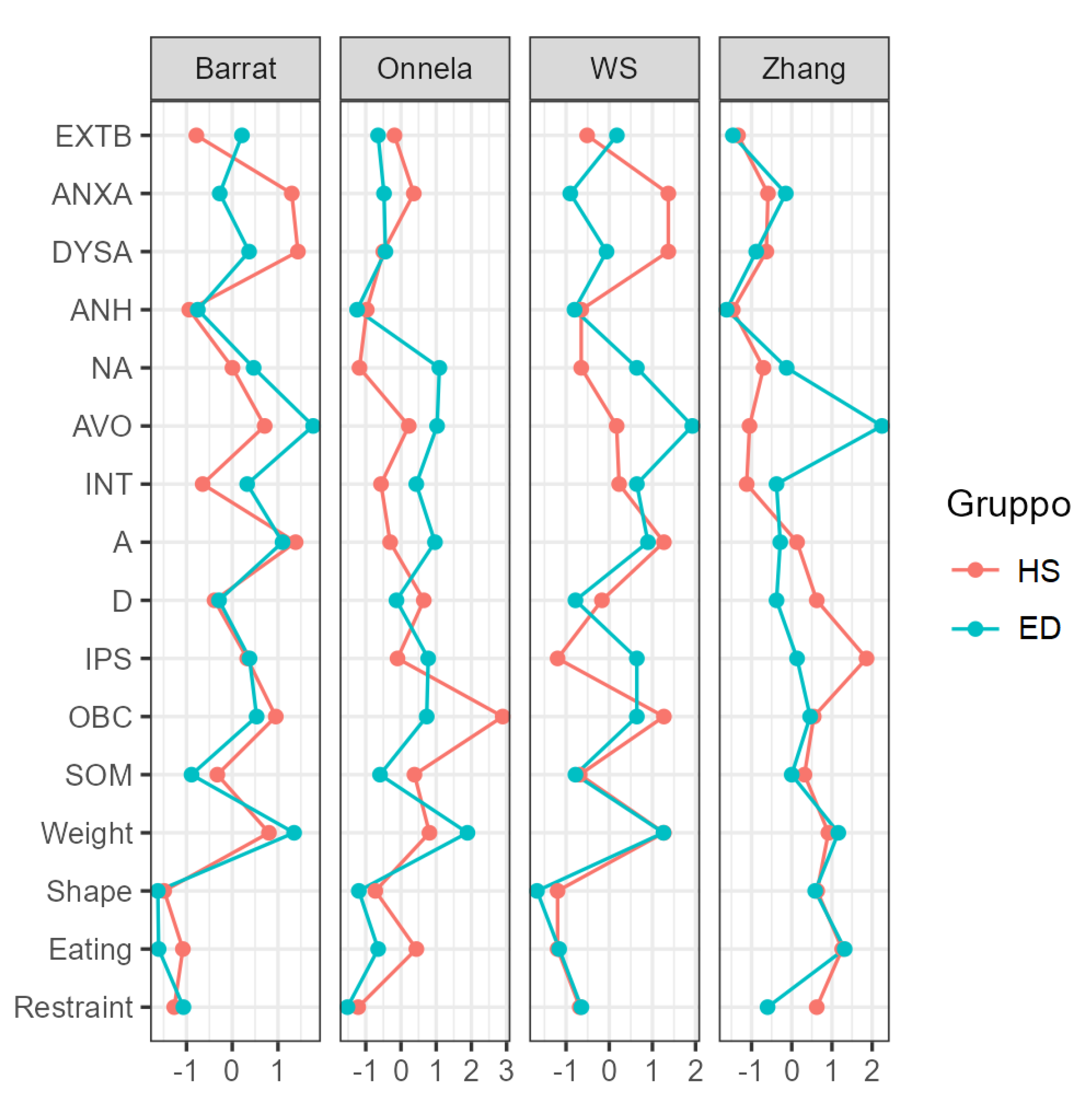
3.2. Network Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- van Hoeken, D.; Hoek, H.W. Review of the Burden of Eating Disorders: Mortality, Disability, Costs, Quality of Life and Family Burden. Curr. Opin. Psychiatry 2020, 33, 521. [Google Scholar] [CrossRef] [PubMed]
- Bakalar, J.L.; Shank, L.M.; Vannucci, A.; Radin, R.M.; Tanofsky-Kraff, M. Recent Advances in Developmental and Risk Factor Research on Eating Disorders. Curr. Psychiatry Rep. 2015, 17, 42. [Google Scholar] [CrossRef] [PubMed]
- Keel, P.K.; Brown, T.A. Update on Course and Outcome in Eating Disorders. Int. J. Eat. Disord. 2010, 43, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Favaro, A. Brain Development and Neurocircuit Modeling Are the Interface between Genetic/Environmental Risk Factors and Eating Disorders. A Commentary on Keel & Forney and Friederich et al. Int. J. Eat. Disord. 2013, 46, 443–446. [Google Scholar] [CrossRef] [PubMed]
- Hübel, C.; Marzi, S.J.; Breen, G.; Bulik, C.M. Epigenetics in Eating Disorders: A Systematic Review. Mol. Psychiatry 2019, 24, 901–915. [Google Scholar] [CrossRef]
- Grogan, K.; MacGarry, D.; Bramham, J.; Scriven, M.; Maher, C.; Fitzgerald, A. Family-Related Non-Abuse Adverse Life Experiences Occurring for Adults Diagnosed with Eating Disorders: A Systematic Review. J. Eat. Disord. 2020, 8, 36. [Google Scholar] [CrossRef]
- Maon, I.; Horesh, D.; Gvion, Y. Siblings of Individuals with Eating Disorders: A Review of the Literature. Front. Psychiatry 2020, 11, 604. [Google Scholar] [CrossRef]
- Meneguzzo, P.; Cazzola, C.; Castegnaro, R.; Buscaglia, F.; Bucci, E.; Pillan, A.; Garolla, A.; Bonello, E.; Todisco, P. Associations Between Trauma, Early Maladaptive Schemas, Personality Traits, and Clinical Severity in Eating Disorder Patients: A Clinical Presentation and Mediation Analysis. Front. Psychol. 2021, 12, 661924. [Google Scholar] [CrossRef]
- Mitchell, K.S.; Scioli, E.R.; Galovski, T.; Belfer, P.L.; Cooper, Z. Posttraumatic Stress Disorder and Eating Disorders: Maintaining Mechanisms and Treatment Targets. Eat. Disord. 2021, 29, 292–306. [Google Scholar] [CrossRef]
- Rabito-Alcón, M.F.; Baile, J.I.; Vanderlinden, J. Mediating Factors between Childhood Traumatic Experiences and Eating Disorders Development: A Systematic Review. Children 2021, 8, 114. [Google Scholar] [CrossRef]
- Murray, S.L.; Holton, K.F. Post-Traumatic Stress Disorder May Set the Neurobiological Stage for Eating Disorders: A Focus on Glutamatergic Dysfunction. Appetite 2021, 167, 105599. [Google Scholar] [CrossRef]
- Rossi, E.; Cassioli, E.; Gironi, V.; Idrizaj, E.; Garella, R.; Squecco, R.; Baccari, M.C.; Maggi, M.; Vignozzi, L.; Comeglio, P.; et al. Ghrelin as a Possible Biomarker and Maintaining Factor in Patients with Eating Disorders Reporting Childhood Traumatic Experiences. Eur. Eat. Disord. Rev. 2021, 29, 588–599. [Google Scholar] [CrossRef]
- Meneguzzo, P.; Mancini, C.; Terlizzi, S.; Sales, C.; Francesconi, M.F.; Todisco, P. Urinary Free Cortisol and Childhood Maltreatments in Eating Disorder Patients: New Evidence for an Ecophenotype Subgroup. Eur. Eat. Disord. Rev. 2022, 30, 364–372. [Google Scholar] [CrossRef]
- Rodgers, R.F.; DuBois, R.; Thiebaut, S.; Jaussent, I.; Maimoun, L.; Seneque, M.; Lefebvre, P.; Renard, E.; Courtet, P.; Guillaume, S. Structural Differences in Eating Disorder Psychopathology After History of Childhood Abuse: Insights from a Bayesian Network Analysis. J. Abnorm. Psychol. 2019, 128, 795–805. [Google Scholar] [CrossRef]
- Monteleone, A.M. The Impact of the COVID-19 Pandemic on Eating Disorders: A Paradigm for an Emotional Post-Traumatic Stress Model of Eating Disorders. Eur. Neuropsychopharmacol. 2021, 51, 84–86. [Google Scholar] [CrossRef]
- Devoe, D.J.; Han, A.; Anderson, A.; Katzman, D.K.; Patten, S.B.; Soumbasis, A.; Flanagan, J.; Paslakis, G.; Vyver, E.; Marcoux, G.; et al. The Impact of the COVID-19 Pandemic on Eating Disorders: A Systematic Review. Int. J. Eat. Disord. 2022. [Google Scholar] [CrossRef]
- Brown, S.; Opitz, M.-C.; Peebles, A.I.; Sharpe, H.; Duffy, F.; Newman, E. A Qualitative Exploration of the Impact of COVID-19 on Individuals with Eating Disorders in the UK. Appetite 2021, 156, 104977. [Google Scholar] [CrossRef]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Cohen Silver, R.; Everall, I.; et al. Multidisciplinary Research Priorities for the COVID-19 Pandemic: A Call for Action for Mental Health Science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Wang, Q.; Xu, R.; Volkow, N.D. Increased Risk of COVID-19 Infection and Mortality in People with Mental Disorders: Analysis from Electronic Health Records in the United States. World Psychiatry 2021, 20, 124–130. [Google Scholar] [CrossRef]
- De Girolamo, G.; Cerveri, G.; Clerici, M.; Monzani, E.; Spinogatti, F.; Starace, F.; Tura, G.; Vita, A. Mental Health in the Coronavirus Disease 2019 Emergency—The Italian Response. JAMA Psychiatry 2020, 77, 974–976. [Google Scholar] [CrossRef]
- Fernández-Aranda, F.; Casas, M.; Claes, L.; Bryan, D.C.; Favaro, A.; Granero, R.; Gudiol, C.; Jiménez-Murcia, S.; Karwautz, A.; Le Grange, D.; et al. COVID-19 and Implications for Eating Disorders. Eur. Eat. Disord. Rev. 2020, 28, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Castellini, G.; Cassioli, E.; Rossi, E.; Innocenti, M.; Gironi, V.; Sanfilippo, G.; Felciai, F.; Monteleone, A.M.; Ricca, V. The Impact of COVID-19 Epidemic on Eating Disorders: A Longitudinal Observation of Pre versus Post Psychopathological Features in a Sample of Patients with Eating Disorders and a Group of Healthy Controls. Int. J. Eat. Disord. 2020, 53, 1855–1862. [Google Scholar] [CrossRef] [PubMed]
- Phillipou, A.; Meyer, D.; Neill, E.; Tan, E.J.; Toh, W.L.; Van Rheenen, T.E.; Rossell, S.L. Eating and Exercise Behaviors in Eating Disorders and the General Population during the COVID-19 Pandemic in Australia: Initial Results from the COLLATE Project. Int. J. Eat. Disord. 2020, 53, 1158–1165. [Google Scholar] [CrossRef] [PubMed]
- Termorshuizen, J.D.; Watson, H.J.; Thornton, L.M.; Borg, S.; Flatt, R.E.; MacDermod, C.M.; Harper, L.E.; van Furth, E.F.; Peat, C.M.; Bulik, C.M. Early Impact of COVID-19 on Individuals with Self-reported Eating Disorders: A Survey Of ~1000 Individuals in the United States and the Netherlands. Int. J. Eat. Disord. 2020, 53, 1780–1790. [Google Scholar] [CrossRef]
- Monteleone, A.M.; Cascino, G.; Marciello, F.; Abbate-Daga, G.; Baiano, M.; Balestrieri, M.; Barone, E.; Bertelli, S.; Carpiniello, B.; Castellini, G.; et al. Risk and Resilience Factors for Specific and General Psychopathology Worsening in People with Eating Disorders during COVID-19 Pandemic: A Retrospective Italian Multicentre Study. Eat. Weight Disord. 2021, 26, 2443–2452. [Google Scholar] [CrossRef]
- Monteleone, A.M.; Marciello, F.; Cascino, G.; Abbate-Daga, G.; Anselmetti, S.; Baiano, M.; Balestrieri, M.; Barone, E.; Bertelli, S.; Carpiniello, B.; et al. The Impact of COVID-19 Lockdown and of the Following “Re-Opening” Period on Specific and General Psychopathology in People with Eating Disorders: The Emergent Role of Internalizing Symptoms. J. Affect. Disord. 2021, 285, 77–83. [Google Scholar] [CrossRef]
- Baenas, I.; Caravaca-Sanz, E.; Granero, R.; Sánchez, I.; Riesco, N.; Testa, G.; Vintró-Alcaraz, C.; Treasure, J.; Jiménez-Murcia, S.; Fernández-Aranda, F. COVID-19 and Eating Disorders during Confinement: Analysis of Factors Associated with Resilience and Aggravation of Symptoms. Eur. Eat. Disord. Rev. 2020, 28, 855–863. [Google Scholar] [CrossRef]
- Touyz, S.; Lacey, H.; Hay, P. Eating Disorders in the Time of COVID-19. J. Eat. Disord. 2020, 8, 8–10. [Google Scholar] [CrossRef]
- Meneguzzo, P.; Sala, A.; Merlino, L.; Ceccato, E.; Santonastaso, P. One Year of COVID-19 Pandemic on Patients with Eating Disorders, Healthy Sisters, and Community Women: Evidence of Psychological Vulnerabilities. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2022. [Google Scholar] [CrossRef]
- Monteleone, A.M.; Cascino, G. A Systematic Review of Network Analysis Studies in Eating Disorders: Is Time to Broaden the Core Psychopathology to Non Specific Symptoms. Eur. Eat. Disord. Rev. 2021, 29, 531–547. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5); American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Calugi, S.; Milanese, C.; Sartirana, M.; El Ghoch, M.; Sartori, F.; Geccherle, E.; Coppini, A.; Franchini, C.; Dalle Grave, R. The Eating Disorder Examination Questionnaire: Reliability and Validity of the Italian Version. Eat. Weight Disord. Anorex. Bulim. Obes. 2017, 22, 509–514. [Google Scholar] [CrossRef]
- Forte, G.; Favieri, F.; Tambelli, R.; Casagrande, M. COVID-19 Pandemic in the Italian Population: Validation of a Post-Traumatic Stress Disorder Questionnaire and Prevalence of PTSD Symptomatology. Int. J. Environ. Res. Public Health 2020, 17, 4151. [Google Scholar] [CrossRef]
- Derogatis, L.R.; Lipman, R.S.; Rickels, K.; Uhlenhuth, E.H.; Covi, L. The Hopkins Symptom Checklist (HSCL): A Self Report Symptom Inventory. Behav. Sci. 1974, 19, 1–15. [Google Scholar] [CrossRef]
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating Psychological Networks and Their Accuracy: A Tutorial Paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [CrossRef]
- Epskamp, S.; Cramer, A.O.J.; Waldorp, L.J.; Schmittmann, V.D.; Borsboom, D. Qgraph: Network Visualizations of Relationships in Psychometric Data. J. Stat. Softw. 2012, 48, 1–18. [Google Scholar] [CrossRef]
- Van Borkulo, C.D.; Epskamp, S.; Jones, P.; Haslbeck, J.; Millner, A. Package ‘NetworkComparisonTest’: Statistical Comparison of Two Networks Based on Three Invariance Measures. R Packag. Version 2016, 2. Available online: https://cran.r-project.org/web/packages/NetworkComparisonTest/NetworkComparisonTest.pdf (accessed on 30 September 2022).
- Cooper, M.; Reilly, E.E.; Siegel, J.A.; Coniglio, K.; Sadeh-Sharvit, S.; Pisetsky, E.M.; Anderson, L.M. Eating Disorders during the COVID-19 Pandemic and Quarantine: An Overview of Risks and Recommendations for Treatment and Early Intervention. Eat. Disord. 2022, 30, 54–76. [Google Scholar] [CrossRef]
- Karwautz, A.; Rabe-Hesketh, S.; Hu, X.; Zhao, J.; Sham, P.; Collier, D.A.; Treasure, J.L. Individual-Specific Risk Factors for Anorexia Nervosa: A Pilot Study Using a Discordant Sister-Pair Design. Psychol. Med. 2001, 31, 317–329. [Google Scholar] [CrossRef]
- Klump, K.L.; Wonderlich, S.; Lehoux, P.; Lilenfeld, L.R.R.R.; Bulik, C. Does Environment Matter? A Review of Nonshared Environment and Eating Disorders. Int. J. Eat. Disord. 2002, 31, 118–135. [Google Scholar] [CrossRef]
- Taquet, M.; Geddes, J.R.; Luciano, S.; Harrison, P.J. Incidence and Outcomes of Eating Disorders during the COVID-19 Pandemic. Br. J. Psychiatry 2022, 220, 262–264. [Google Scholar] [CrossRef]
- Trott, M.; Johnstone, J.; Pardhan, S.; Barnett, Y.; Smith, L. Changes in Body Dysmorphic Disorder, Eating Disorder, and Exercise Addiction Symptomology during the COVID-19 Pandemic: A Longitudinal Study of 319 Health Club Users. Psychiatry Res. 2021, 298, 113831. [Google Scholar] [CrossRef] [PubMed]
- Kurisu, K.; Matsuoka, M.; Sato, K.; Hattori, A.; Yamanaka, Y.; Nohara, N.; Otani, M.; Yoshiuchi, K. Increased Prevalence of Eating Disorders in Japan since the Start of the COVID-19 Pandemic. Eat. Weight Disord. Anorex. Bulim. Obes. 2022, 27, 2251–2255. [Google Scholar] [CrossRef] [PubMed]
- Favreau, M.; Hillert, A.; Osen, B.; Gärtner, T.; Hunatschek, S.; Riese, M.; Hewera, K.; Voderholzer, U. Psychological Consequences and Differential Impact of the COVID-19 Pandemic in Patients with Mental Disorders. Psychiatry Res. 2021, 302, 114045. [Google Scholar] [CrossRef] [PubMed]
- Haddad, C.; Zakhour, M.; Haddad, R.; Al Hachach, M.; Sacre, H.; Salameh, P. Association between Eating Behavior and Quarantine/Confinement Stressors during the Coronavirus Disease 2019 Outbreak. J. Eat. Disord. 2020, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Dodd, D.; Smith, A.; Bodell, L. Restraint Feeds Stress: The Relationship between Eating Disorder Symptoms, Stress Generation, and the Interpersonal Theory of Suicide. Eat. Behav. 2014, 15, 567–573. [Google Scholar] [CrossRef][Green Version]
- Monteleone, P. Eating Disorders in the Era of the COVID-19 Pandemic: What Have We Learned? Int. J. Environ. Res. Public Health 2021, 18, 12381. [Google Scholar] [CrossRef]
- Costa, M.L.; Costa, M.G.O.; de Souza, M.F.C.; da Silva, D.G.; dos Santos Vieira, D.A.; Mendes-Netto, R.S. Cognitive Restraint, Emotional Eating and Uncontrolled Eating: Exploring Factors Associated with the Cycle of Behaviors during the COVID-19 Pandemic. Food Qual. Prefer. 2022, 100, 104579. [Google Scholar] [CrossRef]
- Ramalho, S.M.; Trovisqueira, A.; de Lourdes, M.; Gonçalves, S.; Ribeiro, I.; Vaz, A.R.; Machado, P.P.P.; Conceição, E. The Impact of COVID-19 Lockdown on Disordered Eating Behaviors: The Mediation Role of Psychological Distress. Eat. Weight Disord. 2022, 27, 179–188. [Google Scholar] [CrossRef]
- Gonzalez-Garcia, V.; Exertier, M.; Denis, A. Anxiety, post-traumatic stress symptoms, and emotion regulation: A longitudinal study of pregnant women having given birth during the COVID-19 pandemic. Eur. J. Trauma Dissociation 2021, 5, 100225. [Google Scholar] [CrossRef]
- Hoffart, A.; Johnson, S.U.; Ebrahimi, O.V. Metacognitive Beliefs, Maladaptive Coping Strategies, and Depressive Symptoms: A Two-Wave Network Study of the COVID-19 Lockdown and Reopening. J. Psychiatr. Res. 2022, 152, 70–78. [Google Scholar] [CrossRef]
- Linardon, J.; Messer, M.; Rodgers, R.F.; Fuller-Tyszkiewicz, M. A Systematic Scoping Review of Research on COVID-19 Impacts on Eating Disorders: A Critical Appraisal of the Evidence and Recommendations for the Field. Int. J. Eat. Disord. 2022, 55, 3–38. [Google Scholar] [CrossRef]

| ED n = 141 | HS n = 99 | t | p | |
|---|---|---|---|---|
| Age | 21.81 (7.19) | 23.75 (8.40) | −1.917 | 0.056 |
| BMI | 19.70 (5.62) | 21.48 (3.34) | −3.067 | 0.002 |
| Female (%) | 133 (94.3%) | 89 (89.9%) | 1.643 * | 0.302 |
| Years of education | 11.58 (3.35) | 12.52 (3.37) | −1.790 | 0.075 |
| EDE-Q | ||||
| Restraint | 2.83 (1.79) | 0.71 (1.25) | 10.768 | <0.001 |
| Eating concern | 3.05 (1.64) | 0.74 (1.21) | 12.515 | <0.001 |
| Shape concern | 4.26 (1.66) | 1.69 (1.71) | 11.649 | <0.001 |
| Weight concern | 3.55 (1.86) | 1.30 (1.42) | 10.567 | <0.001 |
| SCL-58 | ||||
| Somatization | 1.60 (0.84) | 0.79 (0.76) | 7.951 | <0.001 |
| Obsessive-compulsive | 1.53 (0.98) | 0.80 (0.80) | 6.312 | <0.001 |
| Interpersonal sensitivity | 1.42 (0.91) | 0.74 (0.73) | 6.462 | <0.001 |
| Depression | 1.66 (0.88) | 0.86 (0.70) | 7.851 | <0.001 |
| Anxiety | 1.66 (0.94) | 0.98 (0.76) | 6.195 | <0.001 |
| PCL-5 | ||||
| Intrusion | 1.69 (1.02) | 1.06 (0.99) | 4.739 | <0.001 |
| Avoidance | 1.79 (1.06) | 1.09 (1.00) | 5.175 | <0.001 |
| Negative affect | 1.71 (1.18) | 1.01 (0.95) | 5.079 | <0.001 |
| Anhedonia | 2.24 (1.15) | 1.33 (1.15) | 6.006 | <0.001 |
| Dysphoric arousal | 1.48 (1.12) | 0.91 (0.89) | 4.405 | <0.001 |
| Anxious arousal | 1.68 (1.11) | 1.12 (0.97) | 4.084 | <0.001 |
| Externalizing behavior | 1.91 (1.18) | 1.37 (1.17) | 3.511 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meneguzzo, P.; De Mico, A.; Gori, P.; Ajello, A.; Ceccato, E.; Consolati, M.D.; Vita, A.; Sala, A.; Santonastaso, P. A Multicenter Network Analysis Examining the Psychological Effects of the COVID-19 Pandemic on Patients with Eating Disorders versus Their Healthy Siblings. J. Clin. Med. 2022, 11, 7187. https://doi.org/10.3390/jcm11237187
Meneguzzo P, De Mico A, Gori P, Ajello A, Ceccato E, Consolati MD, Vita A, Sala A, Santonastaso P. A Multicenter Network Analysis Examining the Psychological Effects of the COVID-19 Pandemic on Patients with Eating Disorders versus Their Healthy Siblings. Journal of Clinical Medicine. 2022; 11(23):7187. https://doi.org/10.3390/jcm11237187
Chicago/Turabian StyleMeneguzzo, Paolo, Alberto De Mico, Pietro Gori, Alessio Ajello, Enrico Ceccato, Mauro Domenico Consolati, Antonio Vita, Alessandra Sala, and Paolo Santonastaso. 2022. "A Multicenter Network Analysis Examining the Psychological Effects of the COVID-19 Pandemic on Patients with Eating Disorders versus Their Healthy Siblings" Journal of Clinical Medicine 11, no. 23: 7187. https://doi.org/10.3390/jcm11237187
APA StyleMeneguzzo, P., De Mico, A., Gori, P., Ajello, A., Ceccato, E., Consolati, M. D., Vita, A., Sala, A., & Santonastaso, P. (2022). A Multicenter Network Analysis Examining the Psychological Effects of the COVID-19 Pandemic on Patients with Eating Disorders versus Their Healthy Siblings. Journal of Clinical Medicine, 11(23), 7187. https://doi.org/10.3390/jcm11237187







