An Attentional Bias Modification Task, through Virtual Reality and Eye-Tracking Technologies, to Enhance the Treatment of Anorexia Nervosa
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
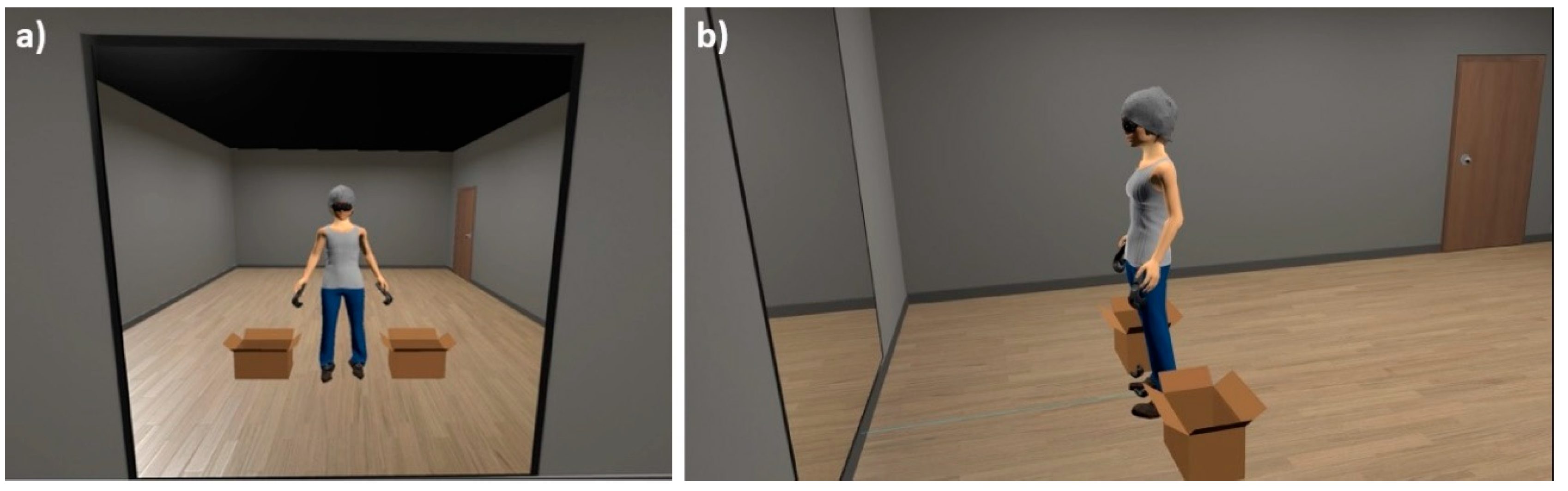
2.2. Instruments
2.3. Measures
2.3.1. Body-Related AB Assessment
2.3.2. User Experience
2.4. Procedure
2.5. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Keski-Rahkonen, A.; Mustelin, L. Epidemiology of eating disorders in Europe: Prevalence, incidence, comorbidity, course, consequences, and risk factors. Curr. Opin. Psychiatry 2016, 29, 340–345. [Google Scholar] [CrossRef] [PubMed]
- Russell, G.F. The changing nature of anorexia nervosa: An introduction to the conference. J. Psychiatr. Res. 1985, 19, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Linardon, J.; Phillipou, A.; Castle, D.; Newton, R.; Harrison, P.; Cistullo, L.L.; Griffiths, S.; Hindle, A.; Brennan, L. The relative associations of shape and weight over-evaluation, preoccupation, dissatisfaction, and fear of weight gain with measures of psychopathology: An extension study in individuals with anorexia nervosa. Eat. Behav. 2018, 29, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Calugi, S.; El Ghoch, M.; Conti, M.; Dalle Grave, R. Preoccupation with shape or weight, fear of weight gain, feeling fat and treatment outcomes in patients with anorexia nervosa: A longitudinal study. Behav. Res. Ther. 2018, 105, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Hagman, J.; Gardner, R.M.; Brown, D.L.; Gralla, J.; Fier, J.M.; Frank, G.K.W. Body size overestimation and its association with body mass index, body dissatisfaction, and drive for thinness in anorexia nervosa. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2015, 20, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Shafran, R. Information processing biases in eating disorders. Clin. Psychol. Rev. 2004, 24, 215–238. [Google Scholar] [CrossRef]
- Williamson, D.A.; White, M.A.; York-Crowe, E.; Stewart, T.M. Cognitive-Behavioral Theories of Eating Disorders. Behav. Modif. 2004, 28, 711–738. [Google Scholar] [CrossRef]
- Delinsky, S.S.; Wilson, G.T. Mirror exposure for the treatment of body image disturbance. Int. J. Eat. Disord. 2005, 39, 108–116. [Google Scholar]
- Vocks, S.; Wächter, A.; Wucherer, M.; Kosfelder, J. Look at yourself: Can body image therapy affect the cognitive and emotional response to seeing oneself in the mirror in eating disorders? Eur. Eat. Disord. Rev. 2008, 16, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Vocks, S.; Legenbauer, T.; Wächter, A.; Wucherer, M.; Kosfelder, J. What happens in the course of body exposure? Emotional, cognitive, and physiological reactions to mirror confrontation in eating disorders. J. Psychosom. Res. 2007, 62, 231–239. [Google Scholar] [CrossRef]
- Key, A.; George, C.L.; Beattie, D.; Stammers, K.; Lacey, H.; Waller, G. Body image treatment within an inpatient program for anorexia nervosa: The role of mirror exposure in the desensitization process. Int. J. Eat. Disord. 2002, 31, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Hildebrandt, T.; Loeb, K.; Troupe, S.; Delinsky, S. Adjunctive mirror exposure for eating disorders: A randomized controlled pilot study. Behav. Res. Ther. 2012, 50, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Jansen, A.; Voorwinde, V.; Hoebink, Y.; Rekkers, M.; Martijn, C.; Mulkens, S. Mirror exposure to increase body satisfaction: Should we guide the focus of attention towards positively or negatively evaluated body parts? J. Behav. Ther. Exp. Psychiatry 2016, 50, 90–96. [Google Scholar] [CrossRef]
- Jansen, A.; Nederkoorn, C.; Mulkens, S. Selective visual attention for ugly and beautiful body parts in eating disorders. Behav. Res. Ther. 2005, 43, 183–196. [Google Scholar] [CrossRef] [PubMed]
- Tuschen-Caffier, B.; Bender, C.; Caffier, D.; Klenner, K.; Braks, K.; Svaldi, J. Selective visual attention during mirror exposure in anorexia and bulimia nervosa. PLoS ONE 2015, 10, e0145886. [Google Scholar] [CrossRef]
- Bauer, S.; Schneider, S.; Waldorf, M.; Braks, K.; Huber, T.J.; Adolph, D.; Vocks, S. Selective visual attention towards oneself and associated state body satisfaction: An eye-tracking study in adolescents with different types of eating disorders. J. Abnorm. Child Psychol. 2017, 45, 1647–1661. [Google Scholar] [CrossRef]
- Rodgers, R.F.; Dubois, R.H. Cognitive biases to appearance-related stimuli in body dissatisfaction: A systematic review. Clin. Psychol. Rev. 2016, 46, 1–11. [Google Scholar] [CrossRef]
- Smeets, E.; Jansen, A.; Roefs, A. Bias for the (un)attractive self: On the role of attention in causing body (dis)satisfaction. Health Psychology 2011, 30, 360–367. [Google Scholar] [CrossRef]
- Porras-Garcia, B.; Ferrer-Garcia, M.; Yilmaz, L.; Sen, Y.O.; Olszewska, A.; Ghita, A.; Serrano-Troncoso, E.; Treasure, J.; Gutiérrez-Maldonado, J. Body-related attentional bias as mediator of the relationship between body mass index and body dissatisfaction. Eur. Eat Disord. Rev. 2020, 28, 454–464. [Google Scholar] [CrossRef]
- Hakamata, Y.; Lissek, S.; Bar-Haim, Y.; Britton, J.C.; Fox, N.A.; Leibenluft, E. Attention bias modification treatment: A meta-analysis toward the establishment of novel treatment for anxiety. Biol. Psychiatry 2010, 68, 982–990. [Google Scholar] [CrossRef]
- Renwick, B.; Campbell, I.; Schmidt, U. Attention bias modification: A new approach to the treatment of eating disorders? Int. J. Eat. Disord. 2013, 46, 496–500. [Google Scholar] [CrossRef] [PubMed]
- Barry, T.J.; Vervliet, B.; Hermans, D. An integrative review of attention biases and their contribution to treatment for anxiety disorders. Front. Psychol. 2015, 8, 968. [Google Scholar] [CrossRef]
- Mercado, D.; Schmidt, U.; O’Daly, O.G.; Campbell, I.C.; Werthmann, J. Food related attention bias modification training for anorexia nervosa and its potential underpinning mechanisms. J. Eat. Disord. 2020, 8, 1. [Google Scholar] [CrossRef] [PubMed]
- Werthmann, J.; Field, M.; Roefs, A.; Nederkoorn, C.; Jansen, A. Attention bias for chocolate increases chocolate consumption: An attention bias modification study. J. Behav. Ther. Exp. Psychiatry 2014, 45, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.; Rieger, E. The effect of attentional training on body dissatisfaction and dietary restriction. Eur. Eat. Disord. Rev. 2009, 17, 169–176. [Google Scholar] [CrossRef]
- Engel, N.; Waldorf, M.; Hartmann, A.; Voßbeck-Elsebusch, A.; Vocks, S. Is it possible to train the focus on positive and negative parts of one’s own body? A pilot randomized controlled study on attentional bias modification training. Front. Psychol. 2019, 10, 2890. [Google Scholar] [CrossRef] [PubMed]
- Fairburn, C.G.; Cooper, Z.; Shafran, R. Enhanced Cognitive Behavior Therapy for Eating Disorders (“CBT-E”): An Overview. In Cognitive Behavior Therapy and Eating Disorders; Fairburn, C.G., Ed.; Guilford Press: New York, NY, USA, 2008; pp. 23–34. [Google Scholar]
- Morgan, J.F.; Lazarova, S.; Schelhase, M.; Saeidi, S. Ten session body image therapy: Efficacy of a manualised body image therapy. Eur. Eat. Disord. Rev. 2013, 22, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Mountford, V.A.; Brown, A.; Bamford, B.; Saeidi, S.; Morgan, J.F.; Lacey, H. Bodywise: Evaluating a pilot body image group for patients with anorexia nervosa. Eur. Eat. Disord. Rev. 2014, 23, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Maldonado, J.; Wiederhold, B.K.; Riva, G. Future directions: How virtual reality can further improve the assessment and treatment of eating disorders and obesity. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 148–153. [Google Scholar] [CrossRef]
- Ferrer-Garcia, M.; Pla-Sanjuanelo, J.; Dakanalis, A.; Vilalta-Abella, F.; Riva, G.; Fernandez-Aranda, F.; Forcano, L.; Riesco, N.; Sánchez, I.; Clerici, M.; et al. A Randomized trial of virtual reality-based cue exposure second-level therapy and cognitive behavior second-level therapy for bulimia nervosa and binge-eating disorder: Outcome at six-month follow-up. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 60–68. [Google Scholar] [CrossRef]
- Ferrer-García, M.; Gutiérrez-Maldonado, J. Body image assessment software: Psychometric data. Behav. Res. Methods 2008, 40, 394–407. [Google Scholar] [CrossRef]
- Porras-Garcia, B.; Ferrer-Garcia, M.; Serrano-Troncoso, E.; Carulla-Roig, M.; Soto-Usera, P.; Miquel-Nabau, H.; Shojaeian, N.; de la Montaña Santos-Carrasco, I.; Borszewski, B.; Díaz-Marsá, M.; et al. Validity of virtual reality body exposure to elicit fear of gaining weight, body anxiety and body-related attentional bias in patients with anorexia nervosa. J. Clin. Med. 2020, 9, 3210. [Google Scholar] [CrossRef]
- Serino, S.; Pedroli, E.; Keizer, A.; Triberti, S.; Dakanalis, A.; Pallavicini, F.; Chirico, A.; Riva, G. Virtual reality body swapping: A tool for modifying the allocentric memory of the body. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 127–133. [Google Scholar] [CrossRef]
- Preston, C.; Ehrsson, H.H. Illusory changes in body size modulate body satisfaction in a way that is related to non-clinical eating disorder psychopathology. PLoS ONE 2014, 9, e85773. [Google Scholar] [CrossRef] [PubMed]
- Serino, S.; Polli, N.; Riva, G. From avatars to body swapping: The use of virtual reality for assessing and treating body-size distortion in individuals with anorexia. J. Clin. Psychol. 2019, 75, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Keizer, A.; Van Elburg, A.; Helms, R.; Dijkerman, H.C. A virtual reality full body illusion improves body image disturbance in anorexia nervosa. PLoS ONE 2016, 11, e0163921. [Google Scholar] [CrossRef]
- Riva, G.; Malighetti, C.; Serino, S. Virtual reality in the treatment of eating disorders. Clin. Psychol. Psychother. 2021, 28, 477–488. [Google Scholar] [CrossRef]
- Magrini, M.; Curzio, O.; Tampucci, M.; Donzelli, G.; Cori, L.; Imiotti, M.C.; Maestro, S.; Moroni, D. Anorexia nervosa, body image perception and virtual reality therapeutic applications: State of the art and operational proposal. Int. J. Environ. Res. Public Health 2022, 19, 2533. [Google Scholar] [CrossRef]
- Gutiérrez-Maldonado, J.; Ferrer-García, M.; Dakanalis, A.; Riva, G. Virtual Reality: Applications to Eating Disorders. In The Oxford Handbook of Eating Disorders; Oxford University Press: Oxford, UK, 2018. [Google Scholar]
- Riva, G.; Serino, S.; Di Lernia, D.; Pavone, E.F.; Dakanalis, A. Embodied medicine: Mens sana in corpore virtuale sano. Front. Hum. Neurosci. 2017, 11, 120. [Google Scholar] [CrossRef]
- Riva, G.; Gutiérrez-Maldonado, J.; Dakanalis, A.; Ferrer-García, M. Virtual Reality in the Assessment and Treatment of Weight-Related Disorders. Virtual Reality for Psychological and Neurocognitive Interventions. In Virtual Reality Technologies for Health and Clinical Applications; Rizzo, A., Bouchard, S., Eds.; Springer: New York, NY, USA, 2019. [Google Scholar]
- Maselli, A.; Slater, M. The building blocks of the full body ownership illusion. Front. Hum. Neurosci. 2013, 7, 83. [Google Scholar] [CrossRef] [PubMed]
- García-Palacios, A.; Botella, C.; Hoffman, H.; Fabregat, S. Comparing acceptance and refusal rates of virtual reality exposure vs. In Vivo exposure by patients with specific phobias. Cyberpsychol. Behav. 2007, 10, 722–724. [Google Scholar] [CrossRef]
- Armstrong, T.; Olatunji, B.O. Eye tracking of attention in the affective disorders: A meta-analytic review and synthesis. Clin. Psychol. Rev. 2012, 32, 704–723. [Google Scholar] [CrossRef]
- Kerr-Gaffney, J.; Harrison, A.; Tchanturia, K. Eye-tracking research in eating disorders: A systematic review. Int. J. Eat. Disord. 2019, 52, 3–27. [Google Scholar] [CrossRef] [PubMed]
- Jiang, M.Y.W.; Vartanian, L.R. A review of existing measures of attentional biases in body image and eating disorders research. Aust. J. Psychol. 2018, 70, 3–17. [Google Scholar] [CrossRef]
- Stott, N.; Fox, J.R.E.; Williams, M.O. Attentional bias in eating disorders: A meta-review. Int. J. Eat. Disord. 2021, 54, 1377–1399. [Google Scholar] [CrossRef] [PubMed]
- Reed, D.L.; Thompson, J.K.; Brannick, M.T.; Sacco, W.P. Development and validation of the physical appearance state and trait anxiety scale (PASTAS). J. Anxiety Disord. 1991, 5, 323–332. [Google Scholar] [CrossRef]
- Porras-Garcia, B.; Ferrer-Garcia, M.; Serrano-Troncoso, E.; Carulla-Roig, M.; Soto-Usera, P.; Miquel-Nabau, H.; Fernández-Del castillo Olivares, L.; Marnet-Fiol, R.; de la Montaña Santos-Carrasco, I.; Borszewski, B.; et al. AN-VR-BE. A randomized controlled trial for reducing fear of gaining weight and other eating disorder symptoms in anorexia nervosa through virtual reality-based body exposure. J. Clin. Med. 2021, 10, 682. [Google Scholar] [CrossRef] [PubMed]
- Porras-Garcia, B.; Ferrer-Garcia, M.; Ghita, A.; Moreno, M.; López-Jiménez, L.; Vallvé-Romeu, A.; Serrano-Troncoso, E.; Gutiérrez- Maldonado, J. The influence of gender and body dissatisfaction on body-related attentional bias: An eye-tracking and virtual reality study. Int. J. Eat. Disord. 2019, 52, 1181–1190. [Google Scholar] [CrossRef]
- Rike-Arkenau, M.S.C.; Bauer, A.; Schneider, S. Gender differences in state body satisfaction, affect, and body-related attention patterns towards one’s own and a peer’s body: An Eye-Tracking Study with Women and Men. Cogn. Ther. Res. 2022, 46, 735–746. [Google Scholar] [CrossRef]
- Jacob, R.; Karn, K. Eye Tracking in Human-Computer Interaction and Usability Research: Ready to Deliver the Promises. In The Mind’s Eye: Cognitive and Applied Aspects of Eye Movement Research; Radach, R., Hyona, J., Deubel, H., Eds.; Elsevier Science BV: North Holland, The Netherlands, 2003; pp. 573–605. [Google Scholar]
- Gutierrez-Maldonado, J.; Clua i Sánchez, M.; Porras-Garcia, B.; Ferrer-Garcia, M.; Serrano, E.; Carulla, M.; Meschberger-Annweiler, F.A.; Ascione, M. Body-related attentional bias in anorexia nervosa and body dissatisfaction in females: An eye-tracking and virtual reality new paradigm. Lect. Notes Comput. Sci. 2022, 13317, 443–454. [Google Scholar]
- Lazarov, A.; Abend, R.; Bar-Haim, Y. Social anxiety is related to increased dwell time on socially threatening faces. J. Affect. Disord. 2016, 193, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Waechter, S.; Nelson, A.L.; Wright, C.; Hyatt, A.E.; Oakman, J.M. Measuring Attentional bias to threat: Reliability of dot probe and eye movement indices. Cogn. Ther. Res. 2014, 38, 313–333. [Google Scholar] [CrossRef]
- Sears, C.; Quigley, L.; Fernandez, A.; Newman, K.; Dobson, K. The reliability of attentional biases for emotional images measured using a free-viewing eye-tracking paradigm. Behav. Res. Methods 2019, 51, 2748–2760. [Google Scholar] [CrossRef] [PubMed]
- Skinner, I.W.; Hübscher, M.; Moseley, G.L.; Lee, H.; Wand, B.M.; Traeger, A.C.; Gustin, S.M.; McAuley, J.H. The reliability of eyetracking to assess attentional bias to threatening words in healthy individuals. Behav. Res. Methods 2018, 50, 1778–1792. [Google Scholar] [CrossRef]
- Brooke, J. SUS: A “Quick and Dirty” Usability Scale. In Usability Evaluation in Industry; Jordan, P.W., Thomas, B., Weerdmeester, B.A., McClelland, Eds.; Taylor and Francis: London, UK, 1996; pp. 189–194. [Google Scholar]
- Sauro, J. A Practical Guide to the System Usability Scale: Background, Benchmarks & Best Practices; Measuring Usability LLC.: Denver, CO, USA, 2011; ISBN 1461062705, 9781461062707. [Google Scholar]
- Bangor, A.; Kortum, P.T.; Miller, J.T. An empirical evaluation of the System Usability Scale. Int. J. Hum.-Comput. Interact. 2008, 24, 574–594. [Google Scholar] [CrossRef]
- Schmider, E.; Ziegler, M.; Danay, E.; Beyer, L.; Bühner, M. Is it really robust: Reinvestigating the robustness of ANOVA against violations of the normal distribution assumption. Methodology 2010, 6, 147–151. [Google Scholar] [CrossRef]
- Cicchetti, D.V. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol. Assess. 1994, 6, 284–290. [Google Scholar] [CrossRef]
- Weierich, M.R.; Treat, T.A.; Hollingworth, A. Theories and measurement of visual attentional processing in anxiety. Cogn. Emot. 2008, 22, 985–1018. [Google Scholar] [CrossRef]
- Calvo, M.G.; Avero, P. Time course of attentional bias to emotional scenes in anxiety: Gaze direction and duration. Cogn. Emot. 2005, 19, 433–451. [Google Scholar] [CrossRef] [PubMed]
- Folkvord, F.; Doeschka, J.; Anschütz, D.J.; Wiers, R.W.; Buijzen, M. The role of attentional bias in the effect of food advertising on actual food intake among children. Appetite 2015, 84, 251–258. [Google Scholar] [CrossRef]
- Bruce, A.S.; Lepping, R.J.; Bruce, J.M.; Cherry, B.C.; Martin, L.E.; Davis, A.M. Brain responses to food logos in obese and healthy weight children. J. Pediatr. 2012, 162, 759–764. [Google Scholar] [CrossRef] [PubMed]
- Murdaugh, D.L.; Cox, J.E.; Cook, E.W.; Weller, R.E. fMRI reactivity to high calorie food pictures predicts short- and long-term outcome in a weight-loss program. Neuroimage 2012, 59, 2709–2721. [Google Scholar] [CrossRef] [PubMed]
- Kellough, J.L.; Beevers, C.G.; Ellis, A.J.; Wells, T.T. Time course of selective attention in clinically depressed young adults: An eye tracking study. Behav. Res. Ther. 2008, 46, 1238–1243. [Google Scholar] [CrossRef]
- Waller, G.; Schmidt, U.; Treasure, J.; Murray, K.; Alenya, J.; Emanuelli, F. Problems across care pathways in specialist adult eating disorder services. Psych. Bull. 2009, 33, 26–29. [Google Scholar] [CrossRef]
- De Jong, H.; Broadbent, H.; Schmidt, U. A systematic review of dropout from treatment in outpatients with anorexia nervosa. Int. J. Eat. Disord. 2012, 45, 635–647. [Google Scholar] [CrossRef]
- Pike, K.M. Long-term course of anorexia nervosa: Response, relapse, remission and recovery. Clin. Psychol. Rev. 1998, 18, 447–475. [Google Scholar] [CrossRef] [PubMed]
- Beumont, P.; Russell, J.; Touyz, S. Treatment of anorexia nervosa. Lancet 1993, 341, 1635–1640. [Google Scholar] [CrossRef] [PubMed]
- Doran, D.; Smith, P. Measuring service quality provision within an eating disorders context. Int. J. Health Care Qual. Assur. Inc. Leadersh. Health Serv. 2004, 17, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Newton, T. Consumer involvement in the appraisal of treatment for people with eating disorders: A neglected area of research? Eur. Eat. Disord. Rev. 2001, 9, 301–308. [Google Scholar] [CrossRef]
- Bell, L. What can we learn from consumer studies and qualitative research in the treatment of eating disorders? Eat. Weight Disord. 2003, 8, 181–187. [Google Scholar] [CrossRef]
- De la Rie, S.; Noordenbos, G.; Donker, M.; van Furth, E. Evaluating the treatment of eating disorders from the patient’s perspective. Int. J. Eat. Disord. 2006, 39, 667–676. [Google Scholar] [CrossRef]
- Smink, F.R.E.; Van Hoeken, D.; Hoek, H.W. Epidemiology of eating disorders: Incidence, prevalence and mortality rates. Curr. Psychiatry Rep. 2012, 14, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Favaro, A.; Caregaro, L.; Tenconi, E.; Bosello, R.; Santonastaso, P. Time trends in age at onset of anorexia nervosa and bulimia nervosa. J. Clin. Psychiatry 2009, 70, 1715–1721. [Google Scholar] [CrossRef] [PubMed]
- Serino, S.; Scarpina, F.; Dakanalis, A.; Keizer, A.; Pedroli, E.; Castelnuovo, G.; Chirico, A.; Catallo, V.; Di Lernia, D.; Riva, G. The role of age on multisensory bodily experience: An experimental study with a virtual reality full-body illusion. Cyberpsychol. Behav. Soc. Netw. 2018, 21, 304–310. [Google Scholar] [CrossRef]
- Szalma, J.L.; Warm, J.S.; Matthews, G. Effects of sensory modality and task duration on performance, workload, and stress in sustained attention. Hum. Factors 2004, 46, 219–233. [Google Scholar] [CrossRef] [PubMed]
- Waltemate, T.; Gall, D.; Roth, D.; Botsch, M.; Latoschik, M.E. The impact of avatar personalization and immersion on virtual body ownership, presence, and emotional response. IEEE Trans. Vis. Comput. Graph. 2018, 24, 1643–1652. [Google Scholar] [CrossRef]
- Cornelissen, K.K.; McCarty, K.; Cornelissen, P.L. Body size estimation in women with anorexia nervosa and healthy controls using 3D avatars. Sci. Rep. 2017, 7, 15773. [Google Scholar] [CrossRef] [PubMed]




| Overall (N = 58) | Grouping According to Complete Fixation Time | Grouping According to Number of Fixations | |||
|---|---|---|---|---|---|
| Weight-Oriented AB_CFT Women (n = 25) | Non-Weight-Oriented AB_CFT Women (n = 33) | Weight-Oriented AB_NF Women (n = 24) | Non-Weight-Oriented AB_NF Women (n = 34) | ||
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |
| Age | 24.93 (6.73) | 25.48 (7.62) | 24.52 (6.06) | 24.04 (2.46) | 25.56 (8.54) |
| BMI | 22.28 (3.27) | 22.67 (3.80) | 21.99 (2.82) | 22.63 (3.71) | 22.03 (2.95) |
| Baseline AB_CFT *** | −236 (6018) | 5135 (4404) | −4305 (3219) | 4606 (5063) | −3654 (3952) |
| Baseline AB_NF *** | −2.31 (12.40) | 7.72 (8.22) | −9.91 (9.23) | 9.17 (7.00) | −10.41 (8.26) |
| SUS | 67.46 (10.90) | 65.70 (10.47) | 68.79 (11.18) | 65.62 (10.51) | 68.75 (11.13) |
| AB_CFT Assessment Times | Weight-Oriented AB_CFT Women (n = 25) | Non-Weight-Oriented AB_CFT Women (n = 33) | |||
|---|---|---|---|---|---|
| (I) Time | (J) Time | MD (I-J) (ms) | 95% CI | MD (I-J) (ms) | 95% CI |
| 0 | 1 | 3616.04 | (−347.96, 7580.04) | −2334.70 | (−5784.92, 1115.52) |
| 2 | 4453.32 *** | (1434.96, 7471.68) | −4045.33 *** | (−6672.48, −1418.19) | |
| 3 | 5330.64 *** | (2178.41, 8482.87) | −4326.00 *** | (−7069.67, −1582.33) | |
| 4 | 2881.80 | (−892.14, 6655.74) | −2291.06 | (−5575.86, 993.74) | |
| 1 | 2 | 837.28 | (−2964.86, 4639.42) | −1710.64 | (−5019.98, 1598.70) |
| 3 | 1714.60 | (−2769.44, 6198.64) | −1991.30 | (−5894.16, 1911.55) | |
| 4 | −734.24 | (−5283.27, 3814.79) | 43.64 | (−3915.78, 4003.06) | |
| 2 | 3 | 877.32 | (−2555.24, 4309.88) | −280.67 | (−3268.33, 2706.99) |
| 4 | −1571.52 | (−5326.34, 2183.30) | 1754.27 | (−1513.88, 5022.43) | |
| 3 | 4 | −2448.84 | (−6243.37, 1345.69) | 2034.94 | (−1267.77, 5337.65) |
| AB_NF Assessment Times | Weight-Oriented AB_NF Women (n = 24) | Non-Weight-Oriented AB_NF Women (n = 34) | |||
|---|---|---|---|---|---|
| (I) Time | (J) Time | MD (I-J) (ms) | 95% CI | MD (I-J) (ms) | 95% CI |
| 0 | 1 | 4.42 | (−3.45, 12.28) | −6.09 | (−12.70, 0.52) |
| 2 | 5.12 | (−2.82, 13.07) | −8.32 ** | (−15.00, −1.65) | |
| 3 | 10.00 ** | (1.84, 18.16) | −8.18 ** | (−15.03, −1.32) | |
| 4 | 1.75 | (−7.28, 10.78) | −6.24 | (−13.82, 1.35) | |
| 1 | 2 | 0.71 | (−8.14, 9.56) | −2.24 | (−9.67, 5.20) |
| 3 | 5.58 | (−2.78, 13.94) | −2.09 | (−9.11, 4.94) | |
| 4 | −2.67 | (−10.90, 5.57) | −0.15 | (−7.07, 6.77) | |
| 2 | 3 | 4.87 | (−3.06, 12.81) | 0.15 | (−6.52, 6.81) |
| 4 | −3.37 | (−12.19, 5.44) | 2.09 | (−5.32, 9.49) | |
| 3 | 4 | −8.25 * | (−16.03, −0.47) | 1.94 | (−4.59, 8.48) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meschberger-Annweiler, F.-A.; Ascione, M.; Porras-Garcia, B.; Ferrer-Garcia, M.; Moreno-Sanchez, M.; Miquel-Nabau, H.; Serrano-Troncoso, E.; Carulla-Roig, M.; Gutiérrez-Maldonado, J. An Attentional Bias Modification Task, through Virtual Reality and Eye-Tracking Technologies, to Enhance the Treatment of Anorexia Nervosa. J. Clin. Med. 2023, 12, 2185. https://doi.org/10.3390/jcm12062185
Meschberger-Annweiler F-A, Ascione M, Porras-Garcia B, Ferrer-Garcia M, Moreno-Sanchez M, Miquel-Nabau H, Serrano-Troncoso E, Carulla-Roig M, Gutiérrez-Maldonado J. An Attentional Bias Modification Task, through Virtual Reality and Eye-Tracking Technologies, to Enhance the Treatment of Anorexia Nervosa. Journal of Clinical Medicine. 2023; 12(6):2185. https://doi.org/10.3390/jcm12062185
Chicago/Turabian StyleMeschberger-Annweiler, Franck-Alexandre, Mariarca Ascione, Bruno Porras-Garcia, Marta Ferrer-Garcia, Manuel Moreno-Sanchez, Helena Miquel-Nabau, Eduardo Serrano-Troncoso, Marta Carulla-Roig, and José Gutiérrez-Maldonado. 2023. "An Attentional Bias Modification Task, through Virtual Reality and Eye-Tracking Technologies, to Enhance the Treatment of Anorexia Nervosa" Journal of Clinical Medicine 12, no. 6: 2185. https://doi.org/10.3390/jcm12062185
APA StyleMeschberger-Annweiler, F.-A., Ascione, M., Porras-Garcia, B., Ferrer-Garcia, M., Moreno-Sanchez, M., Miquel-Nabau, H., Serrano-Troncoso, E., Carulla-Roig, M., & Gutiérrez-Maldonado, J. (2023). An Attentional Bias Modification Task, through Virtual Reality and Eye-Tracking Technologies, to Enhance the Treatment of Anorexia Nervosa. Journal of Clinical Medicine, 12(6), 2185. https://doi.org/10.3390/jcm12062185






