Self-Injury in Adolescence Is Associated with Greater Behavioral Risk Avoidance, Not Risk-Taking
Abstract
:1. Introduction
2. Method
2.1. Participants
2.2. Measures
2.2.1. Clinical Assessment
2.2.2. Self-Report
2.2.3. Neuropsychological Testing
2.3. Analyses
2.3.1. Behavioral Impulsivity
2.3.2. Self-Report Impulsivity
3. Results
3.1. Demographic Information
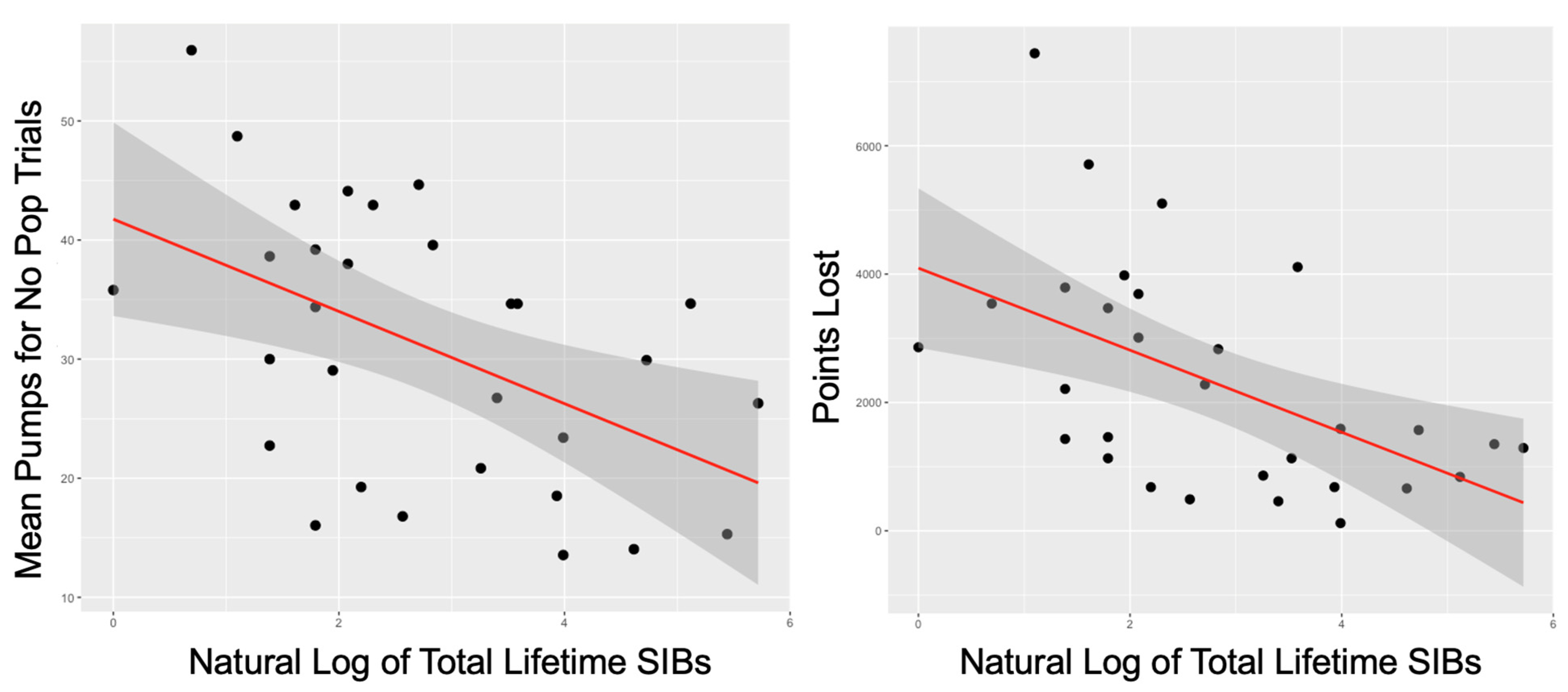
3.2. Behavioral Impulsivity
3.3. Self-Report Impulsivity and Rumination
3.4. Relations between Self-Report and Behavioral Impulsivity Measures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- CDC. WISQARS (Web-based Injury Statistics Query and Reporting System)|Injury Center|CDC. Available online: https://www.cdc.gov/injury/wisqars/index.html (accessed on 12 January 2021).
- Horwitz, A.G.; Czyz, E.K.; King, C.A. Predicting Future Suicide Attempts Among Adolescent and Emerging Adult Psychiatric Emergency Patients. J. Clin. Child Adolesc. Psychol. 2015, 44, 751–761. [Google Scholar] [CrossRef] [Green Version]
- Mars, B.; Heron, J.; Klonsky, E.D.; Moran, P.; O’connor, R.C.; Tilling, K.; Wilkinson, P.; Gunnell, D. Predictors of future suicide attempt among adolescents with suicidal thoughts or non-suicidal self-harm: A population-based birth cohort study. Lancet Psychiatry 2019, 6, 327–337. [Google Scholar] [CrossRef] [Green Version]
- Klonsky, E.D.; May, A. Rethinking Impulsivity in Suicide. Suicide Life-Threat. Behav. 2010, 40, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S.; Johnson, S.; Joormann, J.; Kim, Y.; Nam, J.Y. Serotonin Transporter Polymorphism Interacts With Childhood Adversity to Predict Aspects of Impulsivity. Psychol. Sci. 2011, 22, 589–595. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carver, C.S.; Voie, L.L.; Kuhl, J.; Ganellen, R.J. Cognitive Concomitants of Depression: A Further Ex-amination of the Roles of Generalization, High Standards, and Self-Criticism. J. Soc. Clin. Psychol. 2011, 7, 350–365. [Google Scholar] [CrossRef]
- Cyders, M.A.; Smith, G.T.; Spillane, N.S.; Fischer, S.; Annus, A.M.; Peterson, C. Integration of impulsivity and positive mood to predict risky behavior: Development and validation of a measure of positive urgency. Psychol. Assess. 2007, 19, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Whiteside, S.P.; Lynam, D.R. The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Pers. Individ. Differ. 2001, 30, 669–689. [Google Scholar] [CrossRef]
- Patton, J.H.; Stanford, M.S.; Barratt, E.S. Factor structure of the Barratt impulsiveness scale. J. Clin. Psychol. 1995, 51, 768–774. [Google Scholar] [CrossRef]
- Steinberg, L.; Sharp, C.; Stanford, M.S.; Tharp, A.T. New tricks for an old measure: The development of the Barratt Impulsiveness Scale–Brief (BIS-Brief). Psychol. Assess. 2013, 25, 216–226. [Google Scholar] [CrossRef]
- Maxfield, B.L.; Pepper, C.M. Impulsivity and Response Latency in Non-Suicidal Self-Injury: The Role of Negative Urgency in Emotion Regulation. Psychiatr. Q. 2017, 89, 417–426. [Google Scholar] [CrossRef]
- Lockwood, J.; Daley, D.; Townsend, E.; Sayal, K. Impulsivity and self-harm in adolescence: A systematic review. Eur. Child Adolesc. Psychiatry 2017, 26, 387–402. [Google Scholar] [CrossRef] [Green Version]
- Cassels, M.; Neufeld, S.; van Harmelen, A.-L.; Goodyer, I.; Wilkinson, P. Prospective Pathways From Impulsivity to Non-Suicidal Self-Injury Among Youth. Arch. Suicide Res. 2020, 1–14. [Google Scholar] [CrossRef]
- Janis, I.B.; Nock, M.K. Are self-injurers impulsive?: Results from two behavioral laboratory studies. Psychiatry Res. 2009, 169, 261–267. [Google Scholar] [CrossRef] [Green Version]
- Furnham, A.; Henderson, M. The good, the bad and the mad: Response bias in self-report measures. Pers. Individ. Differ. 1982, 3, 311–320. [Google Scholar] [CrossRef]
- van de Mortel, T.F. Faking It: Social Desirability Response Bias in Self-report Research|The Australian Journal of Advanced Nursing. Aust. J. Adv. Nurs. 2008, 25, 40–48. [Google Scholar]
- Hamza, C.A.; Willoughby, T.; Heffer, T. Impulsivity and nonsuicidal self-injury: A review and meta-analysis. Clin. Psychol. Rev. 2015, 38, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Hedge, C.; Powell, G.; Bompas, A.; Sumner, P. Self-reported impulsivity does not predict response caution. Pers. Individ. Differ. 2020, 167, 110257. [Google Scholar] [CrossRef] [PubMed]
- Alderson, R.M.; Rapport, M.D.; Kofler, M. Attention-Deficit/Hyperactivity Disorder and Behavioral Inhibition: A Meta-Analytic Review of the Stop-signal Paradigm. J. Abnorm. Child Psychol. 2007, 35, 745–758. [Google Scholar] [CrossRef] [PubMed]
- Bechara, A.; Damasio, H.; Tranel, D.; Damasio, A. The Iowa Gambling Task and the somatic marker hypothesis: Some questions and answers. Trends Cogn. Sci. 2005, 9, 159–162. [Google Scholar] [CrossRef] [PubMed]
- Lipszyc, J.; Schachar, R. Inhibitory control and psychopathology: A meta-analysis of studies using the stop signal task. J. Int. Neuropsychol. Soc. 2010, 16, 1064–1076. [Google Scholar] [CrossRef] [PubMed]
- Cyders, M.A.; Coskunpinar, A. Measurement of constructs using self-report and behavioral lab tasks: Is there overlap in nomothetic span and construct representation for impulsivity? Clin. Psychol. Rev. 2011, 31, 965–982. [Google Scholar] [CrossRef] [Green Version]
- Mc Closkey, M.S.; Look, A.E.; Chen, E.Y.; Pajoumand, G.; Berman, M.E. Nonsuicidal Self-Injury: Relationship to Behavioral and Self-Rating Measures of Impulsivity and Self-Aggression. Suicide Life-Threat. Behav. 2012, 42, 197–209. [Google Scholar] [CrossRef] [PubMed]
- Gunten, C.D.; Bartholow, B.D.; Martins, J.S. Inhibition Tasks are not Associated with a Variety of Behaviours in College Students. Eur. J. Pers. 2020, 34, 412–430. [Google Scholar] [CrossRef] [PubMed]
- Allen, K.J.; Hooley, J. Inhibitory control in people who self-injure: Evidence for impairment and enhancement. Psychiatry Res. 2015, 225, 631–637. [Google Scholar] [CrossRef]
- Aklin, W.M.; Lejuez, C.; Zvolensky, M.J.; Kahler, C.W.; Gwadz, M. Evaluation of behavioral measures of risk taking propensity with inner city adolescents. Behav. Res. Ther. 2005, 43, 215–228. [Google Scholar] [CrossRef]
- Lejuez, C.W.; Read, J.P.; Kahler, C.W.; Richards, J.B.; Ramsey, S.E.; Stuart, G.L.; Strong, D.R.; Brown, R.A. Evaluation of a behavioral measure of risk taking: The Balloon Analogue Risk Task (BART). J. Exp. Psychol. Appl. 2002, 8, 75–84. [Google Scholar] [CrossRef]
- Broos, N.; Schmaal, L.; Wiskerke, J.; Kostelijk, L.; Lam, T.; Stoop, N.; Goudriaan, A.E. The relationship between impulsive choice and impulsive action: A cross-species translational study. PLoS ONE 2012, 7, e36781. [Google Scholar] [CrossRef] [PubMed]
- Weafer, J.; Baggott, M.J.; de Wit, H. Test–retest reliability of behavioral measures of impulsive choice, impulsive action, and inattention. Exp. Clin. Psychopharmacol. 2013, 21, 475. [Google Scholar] [CrossRef] [PubMed]
- Ellingson, J.M.; Potenza, M.N.; Pearlson, G.D. Methodological factors as a potential source of discordance between self-report and behavioral measures of impulsivity and related constructs. Addict. Behav. 2018, 84, 126–130. [Google Scholar] [CrossRef]
- Hunt, M.K.; Hopko, D.R.; Bare, R.; Lejuez, C.; Robinson, E.V. Construct Validity of the Balloon Analog Risk Task (BART). Assessment 2005, 12, 416–428. [Google Scholar] [CrossRef]
- Lynam, D.R.; Miller, J.D.; Miller, D.J.; Bornovalova, M.A.; Lejuez, C.W. Testing the relations between impulsivity-related traits, suicidality, and nonsuicidal self-injury: A test of the incremental validity of the UPPS model. Pers. Disord. Theory Res. Treat. 2011, 2, 151–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giannetta, M.M.; Betancourt, L.M.; Brodsky, N.L.; Wintersteen, M.B.; Romer, D.; Giannetta, J.M.; Hurt, H. Suicidal Ideation and Self-Harm Behavior in a Community Sample of Preadolescent Youth: A Case-Control Study. J. Adolesc. Heal. 2012, 50, 524–526. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watkins, E.R.; Roberts, H. Reflecting on rumination: Consequences, causes, mechanisms and treatment of rumination. Behav. Res. Ther. 2020, 127, 103573. [Google Scholar] [CrossRef] [PubMed]
- Nicolai, K.A.; Wielgus, M.D.; Mezulis, A. Identifying Risk for Self-Harm: Rumination and Negative Affectivity in the Prospective Prediction of Nonsuicidal Self-Injury. Suicide Life-Threat. Behav. 2016, 46, 223–233. [Google Scholar] [CrossRef] [PubMed]
- Selby, E.A.; Connell, L.D.; Joiner, T.E. The Pernicious Blend of Rumination and Fearlessness in Non-Suicidal Self-Injury. Cogn. Ther. Res. 2009, 34, 421–428. [Google Scholar] [CrossRef]
- Selby, E.A.; Franklin, J.; Carson-Wong, A.; Rizvi, S.L. Emotional Cascades and Self-Injury: Investigating Instability of Rumination and Negative Emotion. J. Clin. Psychol. 2013, 69, 1213–1227. [Google Scholar] [CrossRef]
- Miranda, R.; Nolen-Hoeksema, S. Brooding and reflection: Rumination predicts suicidal ideation at 1-year follow-up in a community sample. Behav. Res. Ther. 2007, 45, 3088–3095. [Google Scholar] [CrossRef] [Green Version]
- Rogers, M.L.; Joiner, T.E. Rumination, Suicidal Ideation, and Suicide Attempts: A Meta-Analytic Review. Rev. Gen. Psychol. 2017, 21, 132–142. [Google Scholar] [CrossRef]
- Buelens, T.; Luyckx, K.; Gandhi, A.; Kiekens, G.; Claes, L. Non-Suicidal Self-Injury in Adolescence: Longitudinal Associations with Psychological Distress and Rumination. J. Abnorm. Child Psychol. 2019, 47, 1569–1581. [Google Scholar] [CrossRef]
- Kaufman, J.; Birmaher, B.; Brent, D.; Rao, U.; Flynn, C.; Moreci, P.; Williamson, D.; Ryan, N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial Reliability and Validity Data. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 980–988. [Google Scholar] [CrossRef]
- Sheehan, D.V.; Sheehan, K.H.; Shytle, R.D.; Janavs, J.; Bannon, Y.; Rogers, J.E.; Milo, K.M.; Stock, S.L.; Wilkinson, B. Reliability and Validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). J. Clin. Psychiatry 2010, 71, 313–326. [Google Scholar] [CrossRef] [PubMed]
- Linehan, M.M.; Comtois, K.A. Lifetime Parasuicide History. 1996; Unpublished work. [Google Scholar]
- Nock, M.K.; Holmberg, E.B.; Photos, V.I.; Michel, B.D. Self-Injurious Thoughts and Behaviors Interview: Development, reliability, and validity in an adolescent sample. Psychol. Assess. 2007, 19, 309–317. [Google Scholar] [CrossRef]
- Treynor, W.; Gonzalez, R.; Nolen-Hoeksema, S. Rumination Reconsidered: A Psychometric Analysis. Cogn. Ther. Res. 2003, 27, 247–259. [Google Scholar] [CrossRef]
- Langenecker, S.A.; Zubieta, J.-K.; Young, E.A.; Akil, H.; Nielson, K. A task to manipulate attentional load, set-shifting, and inhibitory control: Convergent validity and test–retest reliability of the Parametric Go/No-Go Test. J. Clin. Exp. Neuropsychol. 2007, 29, 842–853. [Google Scholar] [CrossRef] [PubMed]
- Baek, K.; Kwon, J.; Chae, J.-H.; Chung, Y.A.; Kralik, J.D.; Min, J.-A.; Huh, H.; Choi, K.M.; An, C.Y.; Lee, N.-B.; et al. Heightened aversion to risk and loss in depressed patients with a suicide attempt history. Sci. Rep. 2017, 7, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Millner, A.J.; Ouden, H.E.M.D.; Gershman, S.J.; Glenn, C.R.; Kearns, J.C.; Bornstein, A.M.; Marx, B.P.; Keane, T.M.; Nock, M.K. Suicidal thoughts and behaviors are associated with an increased decision-making bias for active responses to escape aversive states. J. Abnorm. Psychol. 2019, 128, 106–118. [Google Scholar] [CrossRef]


| Study 1 | Study 2 | Study 3 | Present Sample | |
|---|---|---|---|---|
| Inclusion Criteria |
|
|
|
|
| Exclusion Criteria |
|
|
|
|
| Self-report and Interview Measures |
|
|
|
|
| General Demographics | ||||
|---|---|---|---|---|
| SIBs (n = 31) | No SIBs (n = 14) | Total (n = 45) | ||
| Age | M(SD) | 15.77 (1.09) | 15.93 (1.00) | 15.82 (1.05) |
| Sex | Male | 9 | 4 | 13 |
| Female | 22 | 10 | 32 | |
| Race | White | 28 | 14 | 42 |
| Asian | 1 | 0 | 1 | |
| Native Hawaiian/Pacific Islander | 1 | 0 | 1 | |
| American Indian/Alaskan Native | 1 | 0 | 1 | |
| Total | 31 | 14 | 45 | |
| Ethnicity | Hispanic | 5 | 0 | 5 |
| Not Hispanic | 26 | 14 | 40 | |
| Total | 31 | 14 | 45 | |
| Clinical Characteristics | ||||
| MDD Status | Remitted | 26 | 14 | 40 |
| Active | 4 | 0 | 4 | |
| No MDD | 1 | 0 | 1 | |
| Total | 31 | 14 | 45 | |
| Lifetime SIBs M(SD) | Raw Total | 44.3 (72.27) | N/A | 44.3 (72.27) |
| Log Transformed | 2.76 (1.46) | N/A | 2.76 (1.46) | |
| Self-Reported Impulsivity M(SD) | UPPS-P: Positive Urgency | 18.9 (6.11) | 17.43 (5.39) | 18.29 (5.79) |
| UPPS-P: Negative Urgency | 22.65 (4.31) | 19.00 (4.71) | 21.15 (4.77) | |
| Behavioral Impulsivity M(SD) | BART: NPMP | 30.95 (11.43) | 35.34 (7.42) | 32.13 (10.42) |
| PGNG: PCIT 2 Target | 0.79 (.25) | 0.70 (0.27) | 0.76 (0.26) | |
| PGNG: PCIT 3 Target | 0.61 (0.19) | 0.59 (0.26) | 0.60 (0.21) | |
| Lifetime Self-Injurious Behaviors (Natural Log Transformed) | Rumination | |
|---|---|---|
| No Pop Mean Pumps | −0.498 ** | −0.219 |
| Points Lost | −0.532 ** | −0.123 |
| Points Won | −0.312 | −0.190 |
| 2T PCIT | 0.203 | 0.063 |
| 3T PCIT | 0.291 | −0.222 |
| Negative Urgency | 0.532 * | 0.539 ** |
| Positive Urgency | 0.691 *** | 0.285 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dillahunt, A.K.; Feldman, D.A.; Thomas, L.R.; Farstead, B.W.; Frandsen, S.B.; Lee, S.; Pazdera, M.; Galloway, J.; Bessette, K.L.; Roberts, H.; et al. Self-Injury in Adolescence Is Associated with Greater Behavioral Risk Avoidance, Not Risk-Taking. J. Clin. Med. 2022, 11, 1288. https://doi.org/10.3390/jcm11051288
Dillahunt AK, Feldman DA, Thomas LR, Farstead BW, Frandsen SB, Lee S, Pazdera M, Galloway J, Bessette KL, Roberts H, et al. Self-Injury in Adolescence Is Associated with Greater Behavioral Risk Avoidance, Not Risk-Taking. Journal of Clinical Medicine. 2022; 11(5):1288. https://doi.org/10.3390/jcm11051288
Chicago/Turabian StyleDillahunt, Alina K., Daniel A. Feldman, Leah R. Thomas, Brian W. Farstead, Summer B. Frandsen, Somi Lee, Myah Pazdera, Jennica Galloway, Katie L. Bessette, Henrietta Roberts, and et al. 2022. "Self-Injury in Adolescence Is Associated with Greater Behavioral Risk Avoidance, Not Risk-Taking" Journal of Clinical Medicine 11, no. 5: 1288. https://doi.org/10.3390/jcm11051288
APA StyleDillahunt, A. K., Feldman, D. A., Thomas, L. R., Farstead, B. W., Frandsen, S. B., Lee, S., Pazdera, M., Galloway, J., Bessette, K. L., Roberts, H., Crowell, S. E., Watkins, E. R., Langenecker, S. A., & Westlund Schreiner, M. (2022). Self-Injury in Adolescence Is Associated with Greater Behavioral Risk Avoidance, Not Risk-Taking. Journal of Clinical Medicine, 11(5), 1288. https://doi.org/10.3390/jcm11051288






