Manual and Device-Assisted Hamstring Autograft Tensioning Yield Similar Outcomes following ACL Reconstruction
Abstract
:1. Introduction
2. Materials and Methods
2.1. Surgical Technique
2.2. Assessment of Clinical Outcomes and Postoperative Knee Stability
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Georgoulis, A.D.; Ristanis, S.; Moraiti, C.O.; Paschos, N.; Zampeli, F.; Xergia, S.; Georgiou, S.; Patras, K.; Vasiliadis, H.S.; Mitsionis, G. ACL injury and reconstruction: Clinical related in vivo biomechanics. Orthop. Traumatol. Surg. Res. 2010, 96 (Suppl. S8), S119–S128. [Google Scholar] [CrossRef] [Green Version]
- Ristanis, S.; Stergiou, N.; Siarava, E.; Ntoulia, A.; Mitsionis, G.; Georgoulis, A.D. Effect of femoral tunnel placement for reconstruction of the anterior cruciate ligament on tibial rotation. J. Bone Jt. Surg. Am. 2009, 91, 2151–2158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brady, M.F.; Bradley, M.P.; Fleming, B.C.; Fadale, P.D.; Hulstyn, M.J.; Banerjee, R. Effects of initial graft tension on the tibiofemoral compressive forces and joint position after anterior cruciate ligament reconstruction. Am. J. Sports Med. 2007, 35, 395–403. [Google Scholar] [CrossRef]
- Arneja, S.; McConkey, M.O.; Mulpuri, K.; Chin, P.; Gilbart, M.K.; Regan, W.D.; Leith, J.M. Graft tensioning in anterior cruciate ligament reconstruction: A systematic review of randomized controlled trials. Arthroscopy 2009, 25, 200–207. [Google Scholar] [CrossRef]
- Melby, A., 3rd; Noble, J.S.; Askew, M.J.; Boom, A.A.; Hurst, F.W. The effects of graft tensioning on the laxity and kinematics of the anterior cruciate ligament reconstructed knee. Arthroscopy 1991, 7, 257–266. [Google Scholar] [CrossRef]
- Numazaki, H.; Tohyama, H.; Nakano, H.; Kikuchi, S.; Yasuda, K. The effect of initial graft tension in anterior cruciate ligament reconstruction on the mechanical behaviors of the femur-graft-tibia complex during cyclic loading. Am. J. Sports Med. 2002, 30, 800–805. [Google Scholar] [CrossRef] [PubMed]
- Suggs, J.; Wang, C.; Li, G. The effect of graft stiffness on knee joint biomechanics after ACL reconstruction—A 3D computational simulation. Clin. Biomech. 2003, 18, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, S.J.; D’Amato, M.J.; Mullaney, M.J.; Tyler, T.F.; Kolstad, K.; McHugh, M.P. A prospectively randomized double-blind study on the effect of initial graft tension on knee stability after anterior cruciate ligament reconstruction. Am. J. Sports Med. 2004, 32, 1881–1886. [Google Scholar] [CrossRef]
- Kirwan, G.W.; Bourke, M.G.; Chipchase, L.; Dalton, P.A.; Russell, T.G. Graft tensioning practices in anterior cruciate ligament reconstruction amongst orthopaedic surgeons in Australia: A national survey. Arch. Orthop. Trauma Surg. 2015, 135, 1733–1741. [Google Scholar] [CrossRef] [PubMed]
- Sherman, S.L.; Chalmers, P.N.; Yanke, A.B.; Bush-Joseph, C.A.; Verma, N.N.; Cole, B.J.; Bach, B.R., Jr. Graft tensioning during knee ligament reconstruction: Principles and practice. J. Am. Acad. Orthop. Surg. 2012, 20, 633–645. [Google Scholar] [CrossRef]
- Biau, D.J.; Katsahian, S.; Kartus, J.; Harilainen, A.; Feller, J.A.; Sajovic, M.; Ejerhed, L.; Zaffagnini, S.; Röpke, M.; Nizard, R. Patellar tendon versus hamstring tendon autografts for reconstructing the anterior cruciate ligament: A meta-analysis based on individual patient data. Am. J. Sports Med. 2009, 37, 2470–2478. [Google Scholar] [CrossRef]
- Magnussen, R.A.; Reinke, E.K.; Huston, L.J.; Hewett, T.E.; Spindler, K.P. Factors Associated With High-Grade Lachman, Pivot Shift, and Anterior Drawer at the Time of Anterior Cruciate Ligament Reconstruction. Arthroscopy 2016, 32, 1080–1085. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Neill, B.J.; Byrne, F.J.; Hirpara, K.M.; Brennan, W.F.; McHugh, P.E.; Curtin, W. Anterior cruciate ligament graft tensioning. Is the maximal sustained one-handed pull technique reproducible? BMC Res. Notes 2011, 4, 244. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoshiya, S.; Kurosaka, M.; Ouchi, K.; Kuroda, R.; Mizuno, K. Graft tension and knee stability after anterior cruciate ligament reconstruction. Clin. Orthop. Relat. Res. 2002, 394, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Grunau, P.D.; Arneja, S.; Leith, J.M. A Randomized Clinical Trial to Assess the Clinical Effectiveness of a Measured Objective Tensioning Device in Hamstring Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2016, 44, 1482–1486. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.M.; Hull, M.L.; Howell, S.M. Does a tensioning device pinned to the tibia improve knee anterior-posterior load-displacement compared to manual tensioning of the graft following anterior cruciate ligament reconstruction? A cadaveric study of two tibial fixation devices. J. Orthop. Res. 2006, 24, 1832–1841. [Google Scholar] [CrossRef]
- Morrison, L.; Haldane, C.; de Sa, D.; Findakli, F.; Simunovic, N.; Ayeni, O.R. Device-assisted tensioning is associated with lower rates of graft failure when compared to manual tensioning in ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3690–3698. [Google Scholar] [CrossRef]
- Hefti, F.; Muller, W.; Jakob, R.P.; Staubli, H.U. Evaluation of knee ligament injuries with the IKDC form. Knee Surg. Sports Traumatol. Arthrosc. 1993, 1, 226–234. [Google Scholar] [CrossRef]
- Briggs, K.K.; Lysholm, J.; Tegner, Y.; Rodkey, W.G.; Kocher, M.S.; Steadman, J.R. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am. J. Sports Med. 2009, 37, 890–897. [Google Scholar] [CrossRef]
- Naik, A.K.; Jain, V.K.; Goyal, A.; Bhavani, P.; Shakya, M.; Sinha, S. Is in-vivo 80 N tensioned quadrupled hamstring graft better than conventional unmeasured pull for arthroscopic ACL reconstruction. J. Clin. Orthop. Trauma. 2020, 11 (Suppl. S5), S779–S783. [Google Scholar] [CrossRef]
- Mae, T.; Toritsuka, Y.; Nakamura, H.; Uchida, R.; Nakagawa, S.; Shino, K. Comparison of anterior knee laxity immediately after anatomic double-bundle anterior cruciate ligament reconstruction: Manual tensioning vs tensioning boot techniques. Asia Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2022, 28, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Tohyama, H.; Yasuda, K. Significance of graft tension in anterior cruciate ligament reconstruction. Basic background and clinical outcome. Knee Surg. Sports Traumatol. Arthrosc. 1998, 6 (Suppl. S1), S30–S37. [Google Scholar] [CrossRef] [PubMed]
- Lohmander, L.S.; Englund, P.M.; Dahl, L.L.; Roos, E.M. The long-term consequence of anterior cruciate ligament and meniscus injuries: Osteoarthritis. Am. J. Sports Med. 2007, 35, 1756–1769. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Øiestad, B.E.; Engebretsen, L.; Storheim, K.; Risberg, M.A. Knee osteoarthritis after anterior cruciate ligament injury: A systematic review. Am. J. Sports Med. 2009, 37, 1434–1443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoshiya, S.; Andrish, J.T.; Manley, M.T.; Bauer, T.W. Graft tension in anterior cruciate ligament reconstruction. An in vivo study in dogs. Am. J. Sports Med. 1987, 15, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Burks, R.T.; Leland, R. Determination of graft tension before fixation in anterior cruciate ligament reconstruction. Arthroscopy 1988, 4, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Bylski-Austrow, D.I.; Grood, E.S.; Hefzy, M.S.; Holden, J.P.; Butler, D.L. Anterior cruciate ligament replacements: A mechanical study of femoral attachment location, flexion angle at tensioning, and initial tension. J. Orthop. Res. 1990, 8, 522–531. [Google Scholar] [CrossRef]
- Beynnon, B.D.; Johnson, R.J.; Fleming, B.C.; Renström, P.A.; Nichols, C.E.; Pope, M.H.; Haugh, L.D. The measurement of elongation of anterior cruciate-ligament grafts in vivo. J. Bone Jt. Surg. Am. 1994, 76, 520–531. [Google Scholar] [CrossRef]
- Samitier, G.; Marcano, A.I.; Alentorn-Geli, E.; Cugat, R.; Farmer, K.W.; Moser, M.W. Failure of Anterior Cruciate Ligament Reconstruction. Arch. Bone Jt. Surg. 2015, 3, 220–240. [Google Scholar]
- Easom, J.C.; Goradia, V.K.; Pearson, S.E.; Wiley, W.B. Anterior cruciate ligament tensioning: KT-1000 measurements after anterior cruciate ligament reconstruction and tensioning (SS-68). Arthroscopy 2004, 20, e32. [Google Scholar] [CrossRef]
- Kim, S.G.; Kurosawa, H.; Sakuraba, K.; Ikeda, H.; Takazawa, S. The effect of initial graft tension on postoperative clinical outcome in anterior cruciate ligament reconstruction with semitendinosus tendon. Arch. Orthop. Trauma Surg. 2006, 126, 260–264. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, K.; Tsujino, J.; Tanabe, Y.; Kaneda, K. Effects of initial graft tension on clinical outcome after anterior cruciate ligament reconstruction. Autogenous doubled hamstring tendons connected in series with polyester tapes. Am. J. Sports Med. 1997, 25, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Kayaalp, M.E.; Collette, R.; Kruppa, P.; Flies, A.; Schaser, K.D.; Wulsten, D.; Duda, G.N.; Becker, R.; Kopf, S. A Higher Initial Tensioning Force of an ACL Graft Results in a Higher Graft Force After Screw Fixation Irrespective of the Screw Diameter: A Biomechanical Study. Am. J. Sports Med. 2021, 49, 3825–3832. [Google Scholar] [CrossRef] [PubMed]
- Nishizawa, Y.; Hoshino, Y.; Nagamune, K.; Araki, D.; Nagai, K.; Kurosaka, M.; Kuroda, R. Comparison Between Intra- and Extra-articular Tension of the Graft During Fixation in Anterior Cruciate Ligament Reconstruction. Arthroscopy 2017, 33, 1204–1210. [Google Scholar] [CrossRef] [PubMed]
- Chahal, J.; Whelan, D.B.; Hoit, G.; Theodoropoulos, J.; Ajrawat, P.; Betsch, M.; Docter, S.; Dwyer, T. Anterior Cruciate Ligament Patellar Tendon Autograft Fixation at 0° Versus 30° Results in Improved Activity Scores and a Greater Proportion of Patients Achieving the Minimal Clinical Important Difference For Knee Injury and Osteoarthritis Outcome Score Pain: A Randomized Controlled Trial. Arthroscopy 2022, 38, 1969–1977. [Google Scholar]
- Amis, A.A.; Jakob, R.P. Anterior cruciate ligament graft positioning, tensioning and twisting. Knee Surg. Sports Traumatol. Arthrosc. 1998, 6 (Suppl. S1), S2–S12. [Google Scholar] [CrossRef]
- Cunningham, R.; West, J.R.; Greis, P.E.; Burks, R.T. A survey of the tension applied to a doubled hamstring tendon graft for reconstruction of the anterior cruciate ligament. Arthroscopy 2002, 18, 983–988. [Google Scholar] [CrossRef]



| Group A | Group Β | Total | p-Value | |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | ||
| Gender | 0.226 | |||
| Men | 25 (86.2) | 25 (71.4) | 50 (78.1) | |
| Women | 4 (13.8) | 10 (28.6) | 14 (21.9) | |
| Mean (SD) | Mean (SD) | Mean (SD) | p-Value | |
| Age (years) | 28.7 (9.4) | 29.9 (9.5) | 29.3 (9.4) | 0.680 |
| Weight (kg) | 72.4 (7.0) | 72.4 (5.3) | 72.4 (6.1) | 0.991 |
| Height (cm) | 173.2 (7.0) | 173.1 (6.2) | 173.1 (6.5) | 0.945 |
| ΒΜΙ (kg/m2) | 24.1 (1.2) | 24.2 (1.1) | 24.1 (1.1) | 0.819 |
| Group A | Group Β | Total | ||
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | p-Value | |
| Anterior laxity (mm) | 10.2 (2.9) | 10.8 (2.5) | 10.6 (2.7) | 0.378 |
| Side-to-side anterior laxity (mm) | 3.6 (1.6) | 3.8 (1.9) | 3.7 (1.7) | 0.576 |
| IKDC | 49.3 (7.5) | 49.1 (7.9) | 49.2 (7.6) | 0.922 |
| LYSHOLM knee score | 55.5 (4.8) | 57.5 (4.1) | 56.6 (4.5) | 0.076 |
| TEGNER activity scale score | 5.1 (0.7) | 5.0 (0.8) | 5.0 (0.7) | 0.598 |
| Group A | Group Β | ||
|---|---|---|---|
| Mean (SD) | Mean (SD) | p-Value | |
| Side-to-side anterior laxity (mm) | |||
| Pre-op | 3.6 (1.6) | 3.8 (1.9) | 0.576 |
| Under GA | 4.5 (1.8) | 4.2 (2.0) | 0.523 |
| Post-op | 1.8 (1.3) | 2.0 (1.7) | 0.896 |
| Post-op 3 mo | 1.3 (0.9) | 1.3 (1.1) | 0.983 |
| Post-op 6 mo | 1.5 (1.2) | 1.1 (1.0) | 0.323 |
| IΚDC | |||
| Pre-op | 49.3 (7.5) | 49.1 (7.9) | 0.922 |
| Post-op 6 mo | 83.9 (4.3) | 85.4 (3.6) | 0.132 |
| Post-op 12 mo | 89.6 (2.5) | 90.0 (2.5) | 0.517 |
| Post-op 24 mo | 91.4 (3.0) | 91.5 (2.7) | 0.915 |
| LYSHOLM knee score | |||
| Pre-op | 55.5 (4.8) | 57.5 (4.1) | 0.076 |
| Post-op 6 mo | 80.3 (5.2) | 80.4 (5.4) | 0.930 |
| Post-op 12 mo | 90.0 (3.6) | 89.7 (4.0) | 0.605 |
| Post-op 24 mo | 90.2 (3.7) | 89.9 (4.1) | 0.614 |
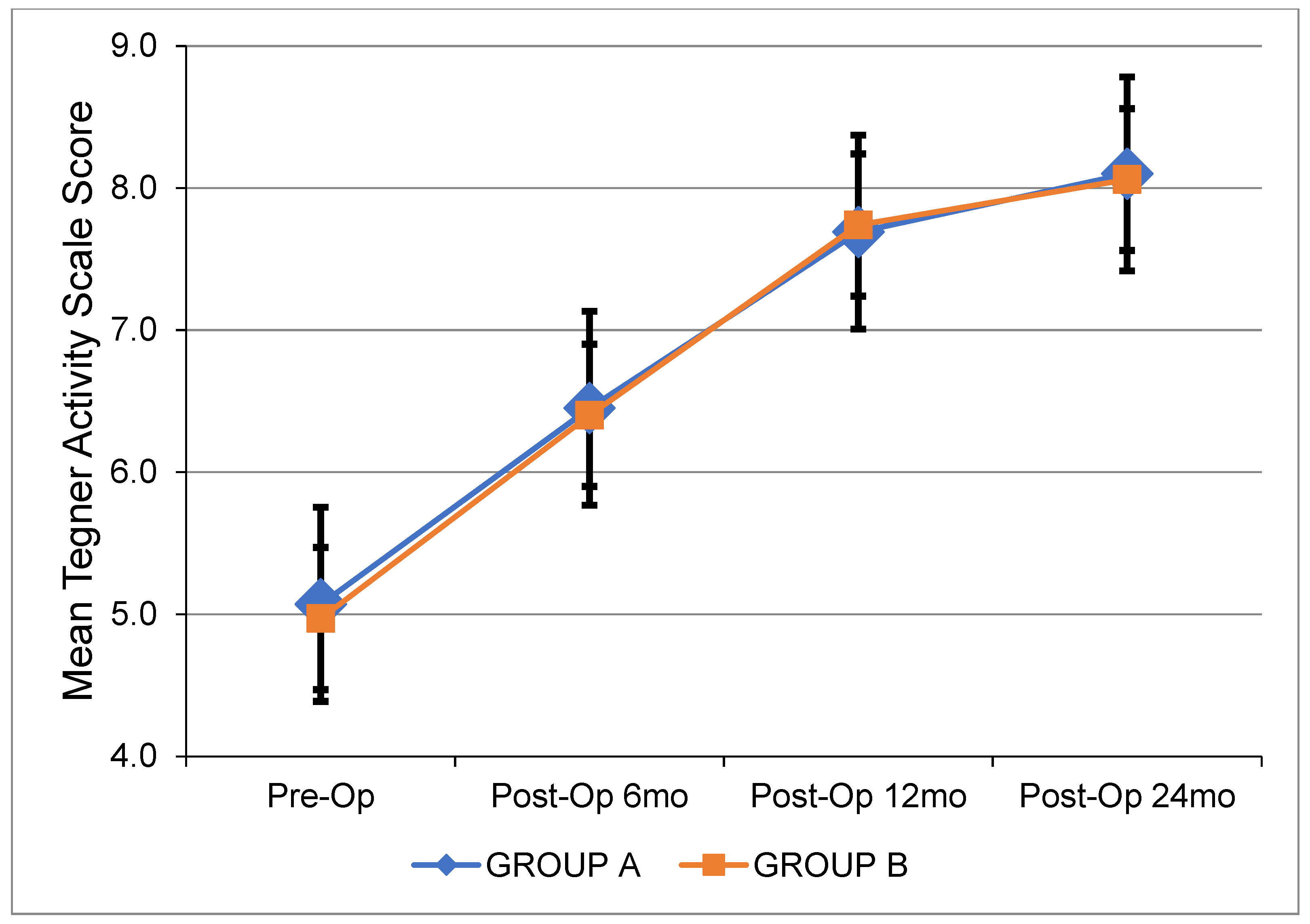
| TEGNER activity scale score | |||
| Pre-op | 5.1 (0.7) | 5.0 (0.8) | 0.514 |
| Post-op 6 mo | 6.5 (1.0) | 6.4 (1.1) | 0.856 |
| Post-op 12 mo | 7.7 (1.1) | 7.7 (0.9) | 0.938 |
| Post-op 24 mo | 8.1 (1.1) | 8.1 (0.8) | 0.813 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piskopakis, A.; Totlis, T.; Achlatis, V.; Zampeli, F.; Georgoulis, J.D.; Hantes, M.; Piskopakis, N.; Vekris, M. Manual and Device-Assisted Hamstring Autograft Tensioning Yield Similar Outcomes following ACL Reconstruction. J. Clin. Med. 2023, 12, 4623. https://doi.org/10.3390/jcm12144623
Piskopakis A, Totlis T, Achlatis V, Zampeli F, Georgoulis JD, Hantes M, Piskopakis N, Vekris M. Manual and Device-Assisted Hamstring Autograft Tensioning Yield Similar Outcomes following ACL Reconstruction. Journal of Clinical Medicine. 2023; 12(14):4623. https://doi.org/10.3390/jcm12144623
Chicago/Turabian StylePiskopakis, Andreas, Trifon Totlis, Vlasios Achlatis, Frantzeska Zampeli, Jim Dimitris Georgoulis, Michael Hantes, Nikolaos Piskopakis, and Marios Vekris. 2023. "Manual and Device-Assisted Hamstring Autograft Tensioning Yield Similar Outcomes following ACL Reconstruction" Journal of Clinical Medicine 12, no. 14: 4623. https://doi.org/10.3390/jcm12144623





